Abstract
Upper gastrointestinal (GI) complaints are common among patients in a GI clinic. Outside of typical gastroesophageal reflux disease (GERD) symptoms that are treated with medication, the symptom presentations of esophageal patients, particularly those with functional conditions, are often difficult to treat and account for high healthcare utilization. This manuscript describes the role of a health psychologist in the treatment of esophageal disorders using behavioral medicine interventions. Observations over the course of a 1-year period indicate that the sample presents with a relatively low level of psychological distress, but reports negative effects of their symptoms on health related quality of life. Five case examples of commonly treated disorders (globus, non-cardiac chest pain, functional dysphagia, rumination syndrome, supragastric belching) are described to highlight how behavioral treatment can improve patients’ symptoms, decrease healthcare utilization, and improve overall quality of life in a timely and relatively simple manner. Successful treatment outcomes are associated with a collaborative working alliance between patient, health psychologist and gastroenterologist. Results indicate the benefit of referring appropriate esophageal patients to a health psychologist with specialization in gastroenterology.
Keywords: behavioral medicine, health psychology, esophageal symptoms, cognitive behavioral therapy, medical hypnosis
Introduction
Individuals with esophageal disorders account for a significant proportion of health care utilization, with gastroesophageal reflux disease (GERD) as the leading diagnosis, explaining approximately 9,000,000 visits to outpatient clinics in 2009.1 Nearly 70% of GERD patients have normal endoscopic results2 and 40% do not achieve adequate results with traditional medical treatments.3 A significant proportion of these patients have functional upper gastrointestinal (GI) conditions, including functional heartburn, non-cardiac chest pain (NCCP), dysphagia and globus. Functional gastrointestinal disorders (FGIDs) can have a significant impact on patient’s quality of life (QOL) and interfere with daily functioning, including work/school absenteeism, difficulty with household chores, and decreased involvement in social and leisure activities.4,5 Patients often complain of these QOL impairments and report fear of having a life threatening condition during visits to the emergency room, primary care settings or gastroenterology clinics.4 In the absence of reliable biomarkers or abnormal structural or biochemical findings on exam, accurate diagnosis of functional upper GI conditions can be challenging. Providers may have difficulty discerning whether symptoms are due to GERD, abnormalities in esophageal motility or are indicative of a FGID. Diagnoses are further complicated by the lack of correlation between symptoms and pathophysiological findings.6 Traditional medical treatments are often inadequate for managing refractory functional gastrointestinal conditions,8 resulting in high healthcare utilization.4,7,8 Psychological interventions (e.g., cognitive behavioral therapy (CBT), hypnosis) are well-established, effective treatments for numerous functional GI conditions, and there is a growing body of research supporting the use of these treatments for esophageal patients8. Widely cited is the impact of psychosocial stressors which provoke and exacerbate symptom presentation,8–11 while effectively learning to cope with stress can aid in the alleviation of globus10 and NCCP symptoms.6,12 Researchers also find a high rate of comorbid psychiatric disorders in the functional GI patient population which can affect the outcome of treatment, especially if generalized anxiety or depression are left untreated.13 With limited treatment options for functional esophageal symptoms, the most promising interventions are medications and psychological treatments aimed at targeting esophageal hypersensitivity. Hypnosis has been shown to reduce pain sensitivity14–15 and somatization16 of IBS patients, and has similarly been used to modify hypervigilance for visceral sensations experienced in globus,10 NCCP,17 and rumination.18–19 Finally, randomized controlled trials have shown brief courses of CBT, hypnosis, interpersonal psychotherapy, relational therapy, and biofeedback have positively impacted quality of life, emotional wellbeing, and symptomatology in this population.8
Despite advances, treatment options for functional esophageal disorders are limited and first line treatment typically involves medication such as proton pump inhibitor (PPI) therapy, but these medications are not effective for all patients. There is a limited body of research examining treatment options for rumination syndrome and supragastric belching. Anecdotal evidence and case studies indicate that behavioral interventions (i.e. diaphragmatic breathing) can be effective treatment for rumination20–22 and in reducing the rate of swallowing in supragastric belching patients18, 23 [See Figure 1].
Figure 1.
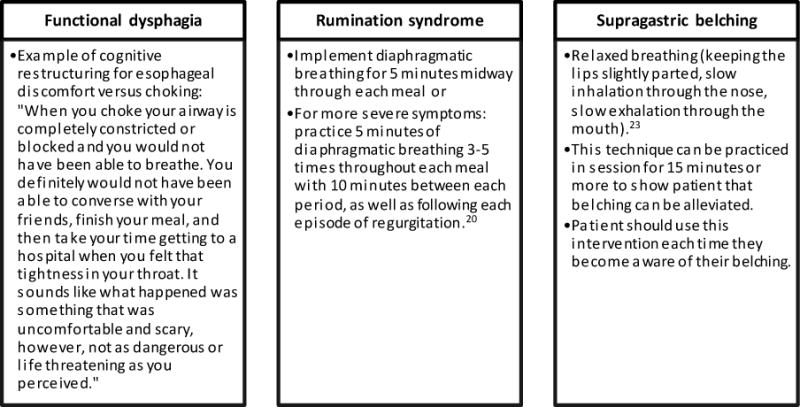
Behavioral interventions for the treatment of dysphagia, rumination, and belching
Objective
The objective of this paper is to describe the potential role of a health psychologist in a comprehensive Esophageal Center (EC). We will characterize patients referred to a health psychologist (MR) working within the EC over a 1-year period and feature 5 cases that highlight our treatment approach with the most common functional esophageal disorders [See Figure 2].
Figure 2.
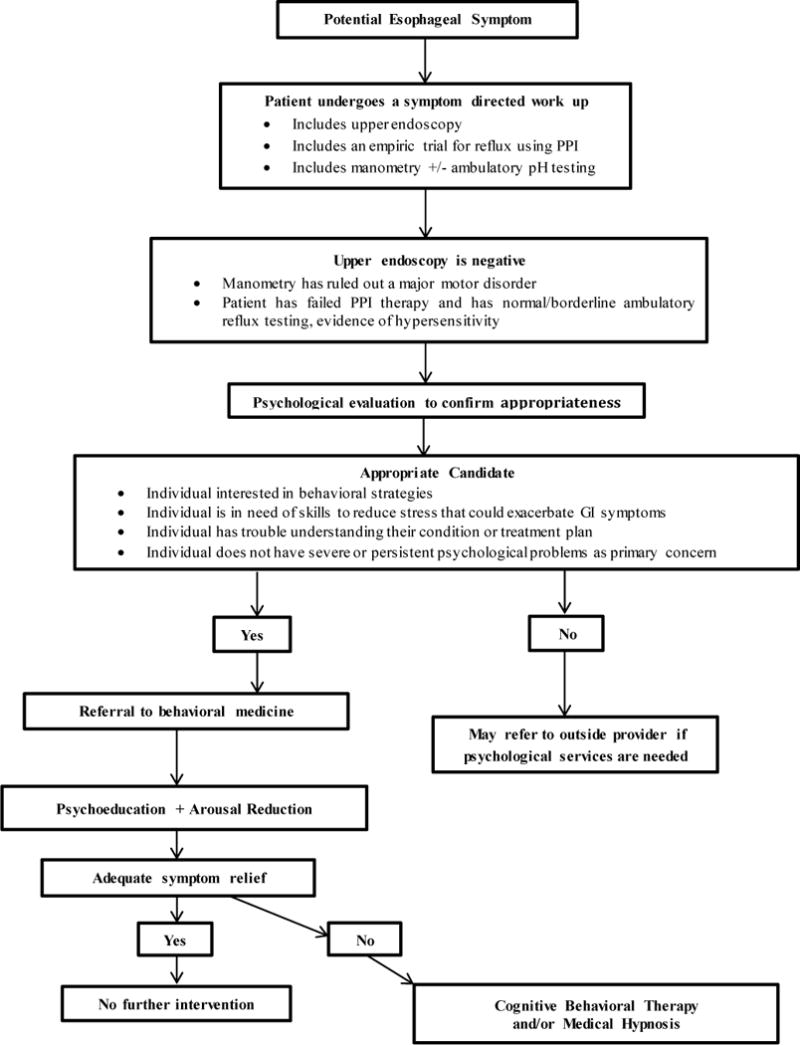
Referral algorithm for patients with esophageal complaints
Methods
Patients with esophageal complaints are seen in our EC, staffed by internationally recognized esophagologists, nurses and technicians. The EC supports a nutritionist and a health psychologist (MR) as part of its commitment to comprehensive care. All patients seen in the EC undergo a thorough work-up by their gastroenterologist, including careful clinical history and any necessary procedures (e.g., endoscopy, manometry, dilation, pH impedance). As part of this comprehensive assessment, patients are considered for potential psychological management and referred by their physicians accordingly. When one of the esophagologists determines a patient may benefit from a behavioral intervention, s/he will place an order in the patient’s electronic medical record (EMR) and a patient liaison will contact the patient to set up an evaluation with our dedicated esophageal health psychologist. Health psychologists have specialized Health and Behavior billing codes that allow for behavioral interventions to be billed under the patient’s medical insurance. This is a revenue generating service at our EC and most major insurance carriers, including Medicare, cover this service.
Psychological Evaluation of Esophageal Patients
The purpose of the psychological evaluation is to identify the role of psychosocial factors in the patient’s symptom presentation and to determine his/her appropriateness for behavioral intervention. At the time of the intake consultation with the health psychologist, patients complete the following questionnaire data:
Demographic and clinical information. Patients provide their name, age, marital status, occupation, and highest level of education completed. Next, patients are asked to report their weight, height and type of GI diagnosis. Patients are provided space to describe their current symptoms and current medications.
Psychosocial checklist. Patients are asked to identify as many that apply in a list of 36 current or past psychosocial stressors. Examples of the psychosocial stressors listed include: work problems, caregiver stress, difficulties with communication, loss of a loved one, anxiety, nightmares, sexual dysfunction, chronic pain, thoughts of self-harm, abuse/trauma, eating disorder and addiction.
Concomitant treatment form. Each individual is asked to list other medical and/or psychiatric conditions they currently have and the approximate date of diagnosis.
Brief Symptom Inventory - 18 (BSI-18).24 The BSI-18 is a reliable measure of general psychological distress in medical populations. Patients are asked to rate how much of each problem distressed them “during the last 7 days including today,” using a 5-point Likert scale. A single item assesses suicide risk. The BSI subscales capture clinically significant depression, anxiety and somatization in addition to the Global Severity Index (GSI). The subscale scores range from 0–24, and the GSI is a sum of the three scores ranging from 0–72. Raw scores are converted to T-scores: GSI T-scores greater than or equal to 63 are considered significantly distressed (greater than or equal to 90th percentile).
Quality of Life in Reflux and Dyspepsia (QOLRAD).25 The QOLRAD is a brief, validated, disease specific measure developed to identify health related QOL impairment in patients with heartburn and dyspepsia. Each of the 25 questions is scored on a 7-point Likert scale with a lower score indicating a more severe impact on daily functioning. An average of the 25 question’s scores can produce a score ranging from 0 to 7.
Rating of symptom severity. Patients are asked to rate the severity of their last symptom flare-up on a 10-point Likert scale with higher scores indicating greater symptom severity.
Psychosocial intake interview. The initial psychological evaluation is structured to build therapeutic rapport, provide patients with feedback regarding the impact of their current functioning on their symptoms, determine if behavioral medicine is an appropriate treatment approach for their current medical complaints, assess whether a psychiatric co-morbidity is a primary concern, as well as to assess the level of insight a patient has into how psychological factors might impact GI symptoms. At the conclusion of the one-hour intake consultation, the patient is provided with a treatment plan. If a severe psychiatric co-morbidity (severe depression or anxiety, psychosis, axis II personality disorder, eating disorder) is present, the patient is provided with an appropriate referral to a community-based clinical psychologist. If psychiatric co-morbidity of a lesser degree is present (depression, generalized anxiety disorder, panic disorder, post-traumatic stress disorder) and the primary concern, the patient is also referred to an outside provider.
Treatment Approach
While therapy is tailored to individual patient needs, all patients receive 2 core elements.
Psychoeducation
All patients receive psychoeducation regarding their medical condition and the impact of psychosocial stressors on their symptom presentation. The psychoeducation component provides an opportunity for patients to ask questions, achieve buy-in, gain insight into ways to reduce stressors and behaviorally modify certain aspects of their lifestyle to accommodate symptom alleviation (i.e. increase exercise, identify dietary modifications, improve sleep hygiene, increase relaxation). For example, for patients with functional heartburn or non-cardiac chest pain, we typically deliver a brief description of what esophageal hypersensitivity is and how it may be impacting their symptoms. Patients find this information helpful in understanding why proton pump inhibitor medication may not be helping their symptoms and therefore, why behavioral medicine or medical hypnosis is warranted as an effective treatment for decreasing their perception of pain in the esophageal region.
Modification of arousal
The second core element of our service is relaxation. At the first session, all patients are taught diaphragmatic breathing to effectively decrease physiological arousal in the body. The individual typically leaves the first session knowing why this intervention is important for their treatment as well as how and when to use it. Other forms of relaxation skills training such as guided imagery or progressive muscle relaxation may be incorporated later in treatment. The course of treatment is then dependent on several factors [See Figure 2]. If the patient’s condition is appropriate for medical hypnosis, and the patient is interested in this form of therapeutic intervention, then it is utilized. In our sample, 19 of 37 (51%) esophageal patients received some form of hypnosis using an evidenced-based protocol for their specific condition or tailoring a hypnosis session to their needs. Many patients benefit from the incorporation of these skills into their daily lives, especially in times of symptom flare-up and stress.
In most cases, psychoeducation, combined with some modification of arousal technique (diaphragmatic breathing, relaxation skills training or medical hypnosis) is sufficient.
Cognitive-behavioral therapy is a component of treatment for select patients. CBT is commonly used with medical populations and is an evidence-based treatment for functional bowel disorders. The use of CBT with functional bowel patients is based on the premise that these patients have specific skills deficits, including faulty thinking or beliefs (e.g. catastrophizing, symptom hypervigilance) that exacerbate symptoms or impair coping. The goal of CBT is to remediate these deficits through techniques such as cognitive restructuring, problem solving and worry control. If patients with esophageal complaints demonstrate similar skills deficits, then these techniques are incorporated into treatment. CBT is practical for patients who learn quickly, are engaged in their treatment and are open to practicing new ways of thinking and reacting to their symptoms.
The following case examples describe our approach to 5 esophageal conditions commonly seen in our behavioral medicine clinic: globus, non-cardiac chest pain, functional dysphagia, rumination syndrome, and supragastric belching [summarized in Table 1].
Table 1.
Summary of Case Examples and Outcomes
| Presenting problem | Treatment components | No. sessions† | Post-treatment | |||
|---|---|---|---|---|---|---|
| Symptom improvement (%)‡ | Productivity improvement (%)§ | Decrease in medication?¶ | Improve QOL?†† | |||
| Globus |
|
5 | 70 | 100 | No | Yes |
| Non-cardiac chest pain |
|
8 | 90 | 90 | Yes | Yes |
| Functional dysphagia |
|
6 | 90 | 90 | Yes | Yes |
| Rumination syndrome |
|
4 | 100 | 90 | Yes | Yes |
| Supragastric belching |
|
2 | 75 | 75 | Yes | Yes |
No. Sessions was the total number of sessions the patient presented in the case study example engaged in.
Symptom Improvement (%) was assessed by asking the patient: “On a scale of 0 to 100%, with 0 being no improvement and 100 being complete improvement, please rate the % of improvement in your GI symptoms since beginning treatment.”
Productivity improvement (%) was assessed by asking the patient: “On a scale of 0 to 100%, with 0 being no improvement and 100 being complete improvement, please rate the % of improvement in your productivity at work or home since beginning treatment.”
Decrease in medication was assessed by asking the patient: “Has your medication use decreased?” (Yes or No).
Improve QOL was assessed by asking the patient: “Has your quality of life improved since beginning services with your provider?”.
Case Examples
Globus Sensation
Presenting Complaint
A 19-year-old male was referred for globus sensation that was interrupting his ability to focus in school and extracurricular activities. His current medication use was 40mg of esomeprazole once per day.
Treatment and intervention
This patient was provided detailed information describing the nature of globus (i.e., that it is typically benign), and the rationale behind behavioral treatment options. One goal was to decrease physiological arousal and address visceral hypersensitivity contributing to his esophageal discomfort. The patient was instructed to practice diaphragmatic breathing one time per day for approximately 10 minutes. The patient then engaged in esophageal focused hypnotherapy for globus based on a protocol developed within our group.10
Treatment Outcome
After 5 sessions of hypnosis the patient reported adequate alleviation of the globus sensation and no pain or discomfort in his throat most days. By completion of treatment he had resumed all school and extracurricular activities. Three months after treatment the patient’s results were maintained and he continued to utilize diaphragmatic breathing on a regular basis.
Non-cardiac chest pain
Presenting complaint
A 68-year-old retired male was referred with complaints of burning in his throat, severe chest pain, and shortness of breath. The patient had a history of reflux and underwent Nissen fundoplication 3 years ago. He had seen numerous gastroenterologists for his chest pain symptoms and undergone an extensive GI work-up, which was normal and did not explain his symptoms. His current medications included finasteride, fluticasone, atorvastatin, and over the counter proton pump inhibitor medications that he regularly took during symptom flare-ups.
Treatment and Intervention
An initial goal of therapy was to aid the patient in gaining insight into the negative emotional and physiological consequences of stress on the exacerbation and maintenance of his GI symptoms. Session #1 included education regarding the nature of esophageal hypersensitivity. Treatment also incorporated cognitive therapy techniques to address cognitive distortions (i.e. rigid thinking, catastrophizing, filtering) that were contributing to anxiety about his symptoms (e.g., “I have to be productive at all times, I can’t relax”). Follow-up treatment incorporated guided relaxation training as well as a behavioral treatment plan to replace unhealthy activities with relaxation strategies such as the diaphragmatic breathing, progressive muscle relaxation, guided imagery, meditation, and exercise.
Treatment Outcome
The patient reported significant improvement in mood and reduction in the severity and frequency of chest pain after 8 sessions. He engaged in on-going daily practice of relaxation skills. Emotionally, the patient reported more control over his anxiety and developed a more realistic outlook toward his health. The patient decreased his medication use and has not needed to return to his gastroenterologist outside of regular checkups. At the three-month follow-up the patient reported maintaining his health improvements and continued use of behavior modification strategies.
Functional Dysphagia
Presenting complaint
A 29-year-old male presented with dysphagia for liquids and solids. The patient initially presented to the emergency room due to fears that he would choke and had also been evaluated in our outpatient GI clinic. This patient arrived at our intake interview stating that he had stopped eating alone for fear of choking, and had many other catastrophic thoughts regarding his esophagus and body functioning. This provider developed a treatment plan to address his esophageal health concerns, while also recommending the patient to psychotherapy with another professional to address generalized anxiety.
Treatment and Intervention
Initially, it was important that the patient be validated, in that his instances of dysphagia were scary for him. Documentation of his negative endoscopy with biopsies and a negative manometry report were used to reassure the patient. Traditional behavioral techniques might approach this problem with biofeedback focused around the mechanics of swallowing. However, in this case, maladaptive beliefs seemed to drive symptoms. Cognitive behavioral therapy was used to reframe his perception of symptoms as uncomfortable, but not life threatening [See Figure 1]. As the negative cognitions around choking (“I could choke and die.”) were alleviated, treatment shifted to developing coping skills to manage future symptoms of dysphagia, including relaxation techniques, positive self-talk, coping statements, and distraction. For example, he counted slowly to ten, while breathing deeply and slowly, and then reminded himself, “This is uncomfortable, but this is not permanent and I am not choking. I will be okay!”. Treatment also targeted eating behaviors and self-care, including taking time to sit down for meals, taking smaller bites, chewing food more thoroughly, and incorporating exercise.
Treatment Outcome
At completion of 5 sessions, patient reported increased self-efficacy and confidence to manage daily stress and esophageal symptoms. The patient resumed normal eating behaviors, and reported significant improvements in his QOL. In addition, he began psychotherapy with another provider to address generalized anxiety. At a three-month follow-up the symptoms remained manageable and he had continued to use adaptive coping skills.
Rumination Syndrome
Presenting complaint
A 33-year-old female was referred with symptoms of nausea and involuntary regurgitation of liquids and food approximately ten times throughout the day. The patient subconsciously engaged in a physiological sequence of behaviors (contraction of the abdominal muscles and the voluntary relaxation of the LES) that allowed food and liquid to be regurgitated when she experienced any abdominal discomfort. She was taking domperidone, lorazepam, a proton pump inhibitor, and ondansetron at the time of intake. The patient had a history of depression, generalized anxiety and an eating disorder (in remission for ten years); however, there was no indication of clinically significant psychological problems at the time of intake. The patient was under the established care of a clinical psychologist to aid with stress management and current symptoms of anxiety. As a result of her current rumination symptoms she was on medical leave, but needed to return to work within a one-month period.
Treatment and Intervention
The primary treatment intervention began with psychoeducation to teach the patient that her body was capable of withstanding abdominal discomfort; followed by diaphragmatic breathing training as a habit reversal strategy as described by Chitkara and colleagues [See Figure 1].20
Treatment Outcome
The patient reported significant reduction in frequency of regurgitation (reduced from 10 times per day to one episode every few days) after 4 sessions. The patient learned to become tolerant of abdominal discomfort/nausea and over time became less sensitive and aware of those feelings. She discontinued all medications except her proton pump inhibitor, and returned back to work. The patient reported significant improvement in her QOL, as she gained strength to return to regular exercise and was able to re-engage in social activities. Three months after termination the patient no longer needed to implement diaphragmatic breathing throughout her meals, but she used the skill as a relaxation technique.
Supragastric Belching
Presenting complaint
A retired, 69-year-old male was referred with persistent belching that spontaneously began five months prior. The patient had seen several specialists and tried several medications including metoclopramide, lorazepam, amitriptyline, and a series of proton pump inhibitors that did not alleviate symptoms. There was evidence of air swallowing that preceding the patient’s belching.
Treatment and Intervention
The patient was provided with current literature on supragastric belching and then instructed in ways to decondition the behavior. The notion that his behavior was learned was demonstrated by having him lean back and open his mouth to make it very difficult to swallow (this stops the behavior) [See Figure 1]. He became encouraged by the idea that his behavior was voluntary and thus could begin to control his symptoms. To facilitate cue-controlled relaxation (i.e. belching serves as cue to open mouth and stop swallowing air), we created a coping card with behaviors (relaxed breathing, opening his mouth or yawning, asking others to remind him to keep his mouth open, and passive muscle relaxation) to implement when he became aware of the belching behavior.
Treatment Outcome
After 1 session, the patient felt more confident in his ability to manage the belching with the tools he had developed to keep his mouth open. The patient decreased medication use and had become more engaged in social activities. At the three-month follow-up, the patient indicated that his symptoms improved by 75% and had most significantly improved while he was at home.
For a summary of case examples see Table 2.
Table 2.
Summary of upper-GI patients appropriate for psychological intervention by presenting problem (N = 37)†
| Characteristic | All | Presenting Problem
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| GERD | Globus | Func HB‡ | NCCP§ | Rumination | Nausea/vomiting | Dysphagia | Belching¶ | ||
| Gender (n) | |||||||||
| Male | 4 | 1 | 1 | 3 | 0 | 2 | 1 | 2 | |
| Female | 5 | 5 | 5 | 0 | 4 | 2 | 2 | 0 | |
| Age (M) | 50.9 | 46 | 37.8 | 67 | 29.5 | 46.8 | 50.3 | 64.5 | |
| No. sessions (Mdn)†† | 7 | 5.5 | 6 | 5 | 3 | 5.5 | 7 | 2 | |
N = 37: Only the 37 patients with upper GI complaints as the primary presenting problem are presented here. The remaining 11 patients who received treatment, presented with lower GI complaints as their presenting problem.
Func HB is functional heartburn.
NCCP is non-cardiac chest pain.
Belching is supragastric belching.
No. sessions was the median number of sessions for each diagnosis.
Results
Of 85 patients referred to the esophageal health psychologist, 48 patients (56%) were good candidates and chose to pursue psychological treatment for their GI complaint. Of the 48 patients (28 female, 20 male), 37 patients (77%) had an upper GI complaint as the primary presenting problem [See Table 2]. Thirty-one of the 37 (83%) upper GI patients attended therapy for 10 sessions or less, while 6 (16%) patients received 11 sessions or more.
The following comments reflect baseline data that was collected through observation and anecdotal patient reflections. For the purposes of this paper, original data collected and described in the methods section is not included in this preliminary work. As evidenced by baseline data collection, our upper GI patient population (N=37) varied in terms of QOL impairment and psychosocial distress. Patients with rumination syndrome reported the greatest level of QOL impairment while individuals with a diagnosis of globus reported the least. This may not be surprising given the characteristics of globus that typically do not include painful heartburn or regurgitation; while regurgitation or vomiting is one of the primary complaints made by our rumination patients and they often report these symptoms as embarrassing and distressing.
In terms of psychological distress, this sample was variable. Overall, this is a psychologically healthy sample. While patients reported experiencing lifetime psychosocial stressors prior to beginning treatment (i.e. work problems, relationship problems, distrust of others, difficulties with communication, abuse, anxiety, etc) their psychological functioning was not significantly impaired. The functional heartburn patient group appeared to be the most distressed. They showed the most significant negative impact of symptoms on their health related QOL, experienced higher levels of psychological distress than other patient groups and had poor responses to medical treatment. However, this functional heartburn patient sample had a positive response to health psychology treatment in a short period of time (median number of sessions: 6) despite these higher levels of distress.
Gender may be an important factor in psychological treatment for esophageal disorders as well. In this sample, our rumination patients were all female (n=4) with an average age of 29.5 years. Given their life stage, the social, professional and emotional toll of their symptoms for these young, female patients may be particularly impactful. Two of the 4 women were on a medical leave of absence from their jobs. Impressively, significant symptom alleviation was reported after a short number of sessions (median: 3) allowing these patients to return to work as well as noting other social and emotional improvements. Alternatively, patients engaging in treatment for supragastric belching (n=2) and NCCP (n=3) were all older males ranging in age from 62–76. All 5 men greatly benefited from psychoeducation regarding the benign nature of their symptoms, which quickly alleviated worry regarding “something worse” (i.e. heart attack). Psychoeducation and behavior modification for supragastric belching patients over the course of 2 sessions proved adequate for symptom improvement. Further, for the men with NCCP, diaphragmatic breathing and relaxation training served as an effective coping strategy in times of symptom flare, as they could quickly notice physiological changes in their chest pain as they released tension and stress from the body. The median number of sessions for these 3 patients was 5.
Our sample of GERD patients reported their symptoms as only mildly impacting their health related QOL, commonly citing periodic sleep difficulties due to reflux symptoms, or frustration with the inability to tolerate some foods. This patient group also exhibited lower levels of psychological distress (i.e. lower levels of anxiety, less cognitive distortions, adequate social support). These patients were offered behavioral medicine services at the recommendation of their gastroenterologist and they were typically receptive to learning alternative forms of treatment for their reflux symptoms. These patients often benefit from simple, time-limited interventions that include behavioral modification and relaxation skills to improve stress management as well as psychoeducation regarding the importance of diet and exercise.
A limitation to working with this patient population was the ability to collect outcome data. Ideally patients would fill out a treatment feedback form reporting the level of symptom improvement, whether their medication use had been impacted, had there been improvement in QOL, their comments about treatment, etc. However, within a medical population, when patient’s symptoms improve they often do not return for follow-up appointments unless they have a recurrence. The collection of routine outcome data is not easy to accomplish and more likely to be collected informally via follow-up phone calls. This was the method used to obtain follow-up data for the patients presented in the case examples included in this paper. Further research will benefit from obtaining more comprehensive follow-up data on patients.
Discussion
This paper highlights the benefit of having a health psychologist with specific training and specialization in gastroenterology as a resource to GI patients and gastroenterologists. Successful treatment outcomes are associated with a collaborative working alliance between patient, health psychologist and gastroenterologist. Many patients were receptive to working with a health psychologist, interested in behavioral treatment and often times, excited to have the opportunity. It appears that gender, age, and disease presentation influence the health related QOL and distress levels of this patient population and more research will be important to better understand the role that these variables play in predicting response to treatment. While complete alleviation from symptoms may not always be achieved, behavioral treatments can reduce the severity of symptoms and improve QOL for many patients. Many of the behavioral interventions learned in session are relatively simple for patients to implement and can be effectively applied to various aspects of day-to-day life. Understanding the basic mechanisms of functional GI disorders, being prepared to cope with the frustration a patient may feel by the time they reach your office, and the ability to foster a quick and collaborative therapeutic relationship will aid a health psychologist in developing appropriate and effective treatment plans.
Integrating a GI health psychologist into a patient’s treatment team is beneficial for many reasons. Having an on-site health psychologist decreases stigma of receiving behavioral medicine services, improves collaboration with the gastroenterologist, and patients can use their medical insurance with our health and behavior billing codes. Medical providers report greater patient treatment compliance, less burden on physicians and nurses, and improved patient satisfaction when patients are under the care of a health psychologist. Even though we have scientific support for the use of psychological treatment for functional GI disorders, these treatments have not been well disseminated and there is a need for more integrated treatment models to make these treatments available and accessible to patients.
Acknowledgments
We would like to thank the behavioral medicine team at the Center for Psychosocial Research in GI for assistance and consultation; and the gastroenterologists in the Division of Gastroenterology at Northwestern Medical Faculty Foundation for providing referrals for behavioral intervention.
Support: No direct support was received for this work. Drs Pandolfino and Keefer are supported by 1R01DK092217.
Footnotes
All behavioral medicine interventions were conducted at the Esophageal Center at Northwestern, 676 North Saint Clair Street, Suite 1400, Chicago, Illinois 60611 USA.
Author contributions: Megan E. Riehl, PsyD, provided behavioral medicine services and contributed to data collection and analysis, manuscript preparation and editing.
Sarah Kinsinger, PhD, contributed to manuscript preparation and editing.
Peter Kahrilas, MD, contributed as a referring esophagologist and manuscript preparation and editing.
John Pandolfino, MD, contributed as a referring esophagologist and manuscript preparation and editing.
Laurie Keefer, PhD, contributed to manuscript preparation and editing.
References
- 1.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States – 2012 update. Gastroenterology. 2012;143:1179–87. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martinez SD, Malagon IB, Cui H, et al. Non-erosive reflux disease (NERD) – acid reflux and symptom patterns. Aliment Pharmacol Ther. 2003;17:527–45. doi: 10.1046/j.1365-2036.2003.01423.x. [DOI] [PubMed] [Google Scholar]
- 3.di Pietro M, Fitzgerald R. Research advances in esophageal disease - bench to bedside. F1000Prime Reports. 2013;5:44. doi: 10.12703/P5-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Camilleri M, Dubois D, Coulie B, et al. Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States - results of the US Upper Gastrointestinal Study. Clin Gastroenterol Hepatol. 2005;3:543–52. doi: 10.1016/s1542-3565(05)00153-9. [DOI] [PubMed] [Google Scholar]
- 5.Drossman DA. The functional gasterointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377–90. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Kumar AR, Katz PO. Functional esophageal disorders - a review of diagnosis and management. Expert Rev Gastroenterol Hepatol. 2013;7:453–61. doi: 10.1586/17474124.2013.811028. [DOI] [PubMed] [Google Scholar]
- 7.Gyawali P. Esophageal hypersensitivity. Gastroenterol Hepatol (N Y) 2010;6:497–500. [PMC free article] [PubMed] [Google Scholar]
- 8.Palsson OS, Whitehead WE. Psychological treatments in functional gastrointestinal disorders: A primer for the gastroenterologist. Clin Gastroenterol Hepatol. 2013;11:208–216. doi: 10.1016/j.cgh.2012.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitehead WE. Psychosocial aspects of functional gastrointestinal disorders. Gastroenterol Clin North Am. 1996;25(1):21–34. doi: 10.1016/s0889-8553(05)70363-0. [DOI] [PubMed] [Google Scholar]
- 10.Kiebles JL, Kwiatek MA, Pandolfino JE, et al. Do patients with globus sensation respond to hypnotically assisted relaxation therapy? - a case series report. Dis Esophagus. 2010;23:545–53. doi: 10.1111/j.1442-2050.2010.01064.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee BE, Kim GH. Globus pharyngeus: a review of its etiology, diagnosis and treatment. World J Gastroenterol. 2012;18:2462–71. doi: 10.3748/wjg.v18.i20.2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galmiche JP, Clouse RE, Balint A, et al. Functional esophageal disorders. Gastroenterology. 2006;130:1459–65. doi: 10.1053/j.gastro.2005.08.060. [DOI] [PubMed] [Google Scholar]
- 13.Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002;122(4):1140–56. doi: 10.1053/gast.2002.32392. [DOI] [PubMed] [Google Scholar]
- 14.Houghton LA, Larder SA, Lee R, et al. Gut focused hypnotherapy normalizes rectal hypersensitivity in patients with irritable bowel syndrome (IBS) Gastroenterology. 1999;116:A1009. [Google Scholar]
- 15.Lea R, Houghton LA, Calvert EL, et al. Gut-focused hypnotherapy normalizes disordered rectal sensitivity in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2003;17:635–42. doi: 10.1046/j.1365-2036.2003.01486.x. [DOI] [PubMed] [Google Scholar]
- 16.Palsson OS, Turner MJ, Johnson DA, et al. Hypnosis treatment for severe irritable bowel syndrome: investigation of mechanism and effects of symptoms. Dig Dis Sci. 2002;47:2605–14. doi: 10.1023/a:1020545017390. [DOI] [PubMed] [Google Scholar]
- 17.Jones H, Cooper P, Miller V, et al. Treatment of no-cardiac chest pain: a controlled trial of hypnotherapy. Gut. 2006;55:1403–08. doi: 10.1136/gut.2005.086694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calloway SP, Fonagy P, Pounder RE, et al. Behavioral techniques in the management of aerophagia in patients with hiatus hernia. J Psychosom Res. 1983;27:499–502. doi: 10.1016/0022-3999(83)90039-9. [DOI] [PubMed] [Google Scholar]
- 19.Spiegel SB. Uses of hypnosis in the treatment of uncontrollable belching - a case report. Am J Clin Hypn. 1996;38:263–70. doi: 10.1080/00029157.1996.10403350. [DOI] [PubMed] [Google Scholar]
- 20.Chitkara DK, Bredenoord AJ, Talley NJ, et al. Aerophagia and rumination - recognition and therapy. Curr Treat Options Gastroenterol. 2006;9:305–13. doi: 10.1007/s11938-006-0012-9. [DOI] [PubMed] [Google Scholar]
- 21.Prather CM, Litzinger KL, Camilleri M, et al. An open trial of cognitive behavioral intervention in the treatment of rumination syndrome. Gastroenterology. 1997;112:A808. [Google Scholar]
- 22.Wagaman JR, Williams DE, Camilleri M. Behavioral intervention for the treatment of rumination. J Pediatr Gastroenterol Nutr. 1998;27(5):596–8. doi: 10.1097/00005176-199811000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Cigrang JA, Hunter CM, Peterson AL. Behavioral treatment of chronic belching due to aerophagia in a normal adult. Behav Modif. 2006;30:341–51. doi: 10.1177/0145445504264746. [DOI] [PubMed] [Google Scholar]
- 24.Derogatis LR, Melisaratos N. The brief symptom inventory. An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- 25.Wiklund IK, Junghard O, Grace E, et al. Quality of life in reflux and dyspepsia patients. Psychometric documentation of a new disease-specific questionnaire (QOLRAD) Eur J Surg. 1998;(suppl 583):41–9. [PubMed] [Google Scholar]


