Abstract
Falls among people aged ≥65 years are the leading cause of both injury deaths and emergency department visits for trauma. Research shows that many falls are preventable. In the clinical setting, an effective fall intervention involves assessing and addressing an individual’s fall risk factors. This individualized approach is recommended in the American and British Geriatrics Societies’ (AGS/BGS) practice guideline. This article describes the development of STEADI (Stopping Elderly Accidents, Deaths, and Injuries), a fall prevention tool kit that contains an array of health care provider resources for assessing and addressing fall risk in clinical settings. As researchers at the Centers for Disease Control and Prevention’s Injury Center, we reviewed relevant literature and conducted in-depth interviews with health care providers to determine current knowledge and practices related to older adult fall prevention. We developed draft resources based on the AGS/BGS guideline, incorporated provider input, and addressed identified knowledge and practice gaps. Draft resources were reviewed by six focus groups of health care providers and revised. The completed STEADI tool kit, Preventing Falls in Older Patients—A Provider Tool Kit, is designed to help health care providers incorporate fall risk assessment and individualized fall interventions into routine clinical practice and to link clinical care with community-based fall prevention programs.
Keywords: falls, fall prevention, elderly, older adults, clinical care
INTRODUCTION
Falls among older adults (people aged ≥65 years) are the leading cause of both injury deaths and emergency department visits for trauma (Centers for Disease Control and Prevention [CDC], 2012). Falls can have devastating and long-term consequences including reduced mobility, loss of independence, and premature death (Sterling, O’Connor, & Bonadies, 2001). Each year, falls are responsible for more than 20,000 deaths and 2.3 million emergency department visits nationwide (CDC, 2012) and incur more than $30 billion (in 2010 dollars) in direct medical costs (Stevens, Corso, Finkelstein, & Miller, 2006).
BACKGROUND
Falls are a major threat to older adults’ health and quality of life, and as the U.S. population ages, it becomes increasingly important to find ways to reduce the frequency of these events. Epidemiological studies have identified numerous fall risk factors (Masud & Morris, 2001). These can be classified as either intrinsic (i.e., originating within the person, such as age, female gender, leg weakness, balance disorders, and poor vision) or extrinsic (i.e., originating outside the body, such as environmental hazards). However, most falls result from the interaction of multiple risk factors (Rubenstein & Josephson, 2006). In an early study of community-dwelling older adults, Tinetti, Speechley, and Ginter (1988) found that the likelihood of falling increased linearly with the increasing number of risk factors present. The proportion of older people who fell in one year increased from 19% for those with one risk factor to 32% for two risk factors, 60% for three risk factors, and 78% for four or more risk factors.
A meta-analysis of randomized controlled trials of fall interventions concluded that, in the clinical setting, assessing and addressing an older person’s fall risk factors, in addition to identifying and treating symptoms of chronic conditions, can reduce falls (Gillespie et al., 2012; American Geriatrics Society/British Geriatrics Society [AGS/BGS], 2010). A systematic review of interventions suitable for primary care settings, conducted by the U.S. Preventive Services Task Force, also found that interventions implemented through primary care, including exercise or physical therapy, reduced older adult falls (Moyer, 2012). Such interventions could include referral to community programs, but this linkage has not been put into practice.
The AGS/BGS published a clinical practice guideline to promote fall risk assessment and management (AGS/BGS, 2010). It recommends that health care providers ask all older adults if they have fallen in the past year. People who have fallen two or more times or who are experiencing difficulties with walking or balance should receive a multifactorial fall risk assessment. Such an assessment would include taking a fall history; reviewing all medications; testing gait, balance, neurological function, lower extremity muscle strength, cardiovascular status, and visual acuity; assessing activities of daily living including the use of mobility aids and fear of falling; and evaluating the condition of the feet and usual footwear. Fall interventions would include medical management tailored to the identified risk factors, including appropriate referrals, coupled with a suitable exercise program (AGS/BGS, 2010).
Primary care physicians (PCPs) have been slow to put the AGS/BGS guideline into clinical practice because many feel they do not know how to conduct fall risk assessments or do not have adequate knowledge about fall prevention (Chou, Tinetti, King, Irwin, & Fortinsky, 2006; Fortinsky et al., 2004; Rubenstein, Solomon, & Roth, 2004). To fill these knowledge and practice gaps, CDC’s Injury Center developed a suite of materials to help health care providers incorporate fall risk assessment, treatment, and referral into clinical practice and to facilitate patient referrals to community-based fall prevention programs.
METHOD
In addition to the AGS/BGS guideline, two conceptual models informed the development of the tool kit. Wagner’s Chronic Care Model (Wagner, 1998) was selected because fall risk can be conceptualized as a chronic state, similar to other chronic conditions. And Prochaska’s Transtheoretical Stages of Change Model (Prochaska & Velicer, 1997) was chosen because staging algorithms are easily adopted into clinical practice (Sutton et al., 2003; Vallis et al., 2003) and fall prevention frequently involves behavioral change.
To understand health care providers’ knowledge and clinical practices regarding older adult falls, we began by reviewing the literature. We found that community physicians did not adequately identify falls and gait disorders or evaluate patients who reported falling (Rubenstein et al., 2004). Only 37% of older persons in primary care were even asked about falls (Chou, Tinetti, King, Irwin, & Fortinsky, 2006). Of 68 PCPs, only 8% used clinical guidelines on fall prevention (Jones, Ghosh, Horn, Smith, & Vogt, 2011). However, PCPs who treated many geriatric patients did express considerable interest in learning about fall risk assessment and risk reduction (Robinson, Barry, Renick, Bergen, & Stratos, 2001).
In-Depth Interviews
Following the literature review, we conducted in-depth interviews with health care providers. Potential participants were identified using two nationally representative randomized lists provided by a recruitment firm. One list was made up of 5,000 physicians and the other of 5,000 registered nurses (RNs) and nurse practitioners (NPs). Provider information included name, address, telephone number, age, years of practice, type of practice setting, and geographic location.
Using these lists, a contractor contacted a random sample of 216 physicians and 120 RNs or NPs and recruited 18 participants. To be eligible, providers had to currently work in their specified health care field, have practiced in their field at least 2 years, primarily see outpatients in their principal work setting, spend at least 70% of their professional time in clinical work, and devote between 25% and 80% of their clinical work to patients aged ≥65 years. Twelve (6%) physicians and six (3%) RNs or NPs met the inclusion criteria, were geographically diverse, and agreed to be interviewed. Because this was an evaluation project, it was exempt from institutional review board review.
We conducted 60-minute structured in-depth telephone interviews with 18 health care professionals: six geriatricians (one female and five males), six PCPs (three females and three males), four RNs (all female), and two NPs (one female and one male).
Participants were asked about their perceptions of falls as a health issue and their current practices related to discussing falls with their patients, conducting fall risk assessments, using standardized gait and balance tests, talking about fall prevention with patients, their awareness of fall prevention guidelines, the perceived barriers to implementing fall risk assessment and prevention strategies, and the challenges to obtaining reimbursement for fall risk assessment and prevention activities. Participants also were asked to suggest types and formats of materials they would like to have to help them incorporate fall risk assessment and fall prevention into their practice and to educate patients about preventing falls. Interviews were recorded and transcribed, and the major ideas were summarized in a report. Examples of responses are provided in the Results section.
We used the results from the in-depth interviews, in conjunction with the theoretical frameworks, the AGS/BGS clinical practice guideline, and input from four subject matter experts, including the two authors of this article, to guide the development of draft materials for STEADI (Stopping Elderly Accidents, Deaths, and Injuries), a fall prevention tool kit for health care providers. Two were geriatricians and all were nationally recognized experts and researchers in older adult fall prevention.
Some of the STEADI components were developed in response to suggestions from the providers who were interviewed or to address knowledge gaps, whereas others were considered, a priori, to be necessary for integrating the AGS/BGS fall prevention recommendations into routine clinical care.
The draft STEADI materials were reviewed by six focus groups of health care providers from around the country. The purpose of the focus groups was to learn providers’ reactions to and preferences for different design elements (e.g., the most convenient packaging for the tool kit, the title, the designs of one-page fact sheets, and pocket guide size). We wanted the focus groups to reflect the variety of health care providers who practice in diverse clinical settings and to include both gender and geographic diversity. Providers were identified from a nationally representative randomized list of 5,250 records that included five categories: general medicine and family medicine practitioners, geriatricians, PAs, RNs, and NPs. To be eligible to participate in the focus groups, providers had to currently work in their specified health care field; have practiced in their specified field for at least 2 years; work in private practice (i.e., as an independent provider rather than as a salaried employee), health clinic, or hospital; primarily see outpatients in their principal work setting; spend at least 70% of their professional time in clinical work; and spend 25% to 80% of their clinical time with patients aged ≥65 years. All 5,250 people on the list were contacted; 54 (10.3%) were eligible and agreed to participate in a 90-minute telephone focus group.
Each focus group included nine persons and represented a single type of health care provider: geriatricians (three females and six males), PCPs who worked in small group practices (defined as <5 physicians; two females and eight males), PCPs who worked in large group practices (defined as ≥5 physicians; three females and six males), PAs (three females and three males), RNs (nine females), and NPs (nine females and one male).
The focus groups reviewed 19 draft items including the tool kit title, cover and folder, the flow chart algorithm, three fact sheets, four fall risk assessment tools, a summary risk factor checklist, a wall chart, guidelines for talking with patients, a case study, the pocket guide, two referral forms, and a patient brochure on hypotension. Because of time constraints, each group reviewed only five or six pieces, based on their relevance to those types of providers, (e.g., nurse practitioners reviewed several assessment tests and PCPs reviewed the pocket guide and a case study). Most items were reviewed by at least two focus groups. Reactions to each item were compiled and general themes were identified. Examples of responses are provided in the Results section. Finally, all materials were revised based on the feedback from the focus groups.
RESULTS
In-Depth Interview Results
A summary of the key findings from 60-minute in-depth telephone interviews is shown in Table 1. Seventy-two percent (13/18) of the providers recognized that falls were a serious threat for their older patients.
TABLE 1.
Characteristics and Key Findings From 60-Minute In-Depth Interviews With 18 Health Care Providers
| Type of Provider | Male | Female |
|---|---|---|
| Primary care physician | 3 | 3 |
| Geriatrician | 5 | 1 |
| Registered nurse | 4 | 0 |
| Nurse practitioner | 1 | 1 |
| Key Findings | ||
| ||
It’s a big issue… . I see a lot of folks with problems with their gait, light headedness, especially when they get up quickly. Side effects of medications sometimes contribute to the problem. (Primary Care Physician)
Falls? Oh, huge, huge. I tell my patients that their biggest enemy is injury. (Geriatrician)
However, practitioners reported that they lacked information about standardized methods for assessing fall risk and evidence-based fall prevention strategies. Providers tended to be reactive rather than proactive in addressing falls. About 94% (17/18) of the providers were unaware of the AGS/BGS clinical guidelines. Most (12/18) did not routinely ask about a patient’s fall history unless the patient had visible signs of a recent fall or if the patient was obviously at high risk.
I’m looking for bruises or difficulty ambulating, anxiety, fear of falling. (Geriatrician)
Like I said, if there is an issue that would make them more likely to fall or to have a detriment from it such as osteoporosis or balance issues that are obvious.” (Primary Care Physician)
When you’ve got a patient with multiple comorbidities and you know you’ve got just a limited amount of time with that patient, it is difficult sometimes to prioritize … depending on the acuity of the patient and their current chief complaint. (Nurse)
Fall risk assessments were informal and usually prompted by a patient’s recent fall.
If somebody brings to my attention that their balance is very poor, I’ll do some kind of mild testing in the office like heel to toe walking, the so-called Romberg test, that sort of thing. (Geriatrician)
But if they look like—if I see a walker or cane and they just look frail, then I would have them walk or either watch them walk out of the room. (Primary Care Provider)
During the in-depth interviews, health care providers said they would appreciate and use simple, straightforward materials designed for both themselves and their patients. These materials should be direct, concise, and easy to read. The suggested content included information about fall risk factors, fall risk assessment tests and protocols, guidelines, and suggestions for conversation starters with patients. Preferred formats included checklists, one-pagers, and online information. Materials for patients included brochures, pamphlets, and one-pagers that patients could take home.
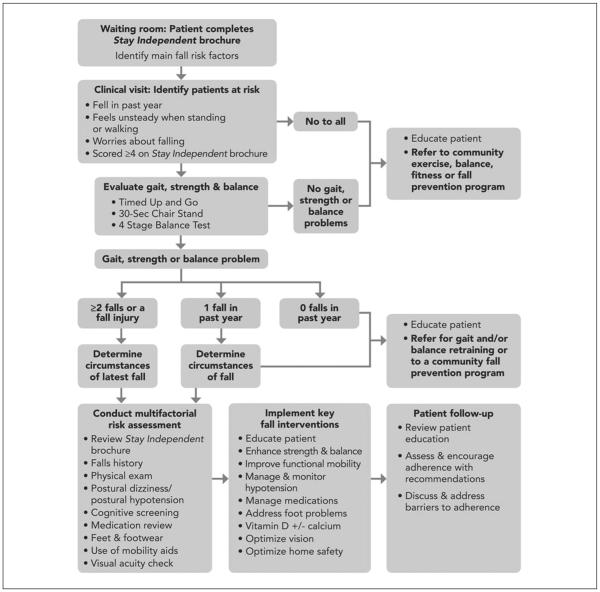
In conjunction with the in-depth interview results, we used the AGS/BGS clinical guideline to develop a simplified flow chart algorithm for fall risk assessment, treatment, and referral (Figure 1).
FIgure 1.
Algorithm for Fall risk Assessment, Treatment, and Referral
The algorithm in Figure 1 and the interview results guided our selection of materials that were developed and then reviewed by the focus groups. These materials included standardized instructions for three gait, strength, and balance assessment tests; a pocket guide with key fall prevention information; guidance on talking about fall prevention with patients; and a patient brochure on managing hypotension.
Focus Group Results
Feedback from the provider focus groups was used to identify the most appealing title cover design, refine all the materials, and select the size of the pocket guide. A summary of the responses to the tool kit materials overall and to specific components is provided below.
The geriatrician and PCPs’ focus groups preferred a tool kit cover design that clearly indicated it was for providers, and a folder that was less bulky than a 3-ring binder but with a spine that could be read if it was placed on a bookshelf. With this in mind, we designed a compact folder with a Velcro® closure and a 1/2 in. spine with the title, Preventing Falls in Older Patients—A Provider Tool Kit. The folder neatly packages the provider resources and patient educational materials. The folder and all components for providers display the STEADI and CDC logos, whereas the materials intended for patients display only the CDC logo.
Overall, all the focus groups except the geriatricians responded favorably to the tool kit materials. The geriatricians reported that they were already familiar with fall risk assessment and included fall prevention in their practices, whereas the reactions of the remaining five groups were more positive.
I’m not familiar with the guidelines but this chart is kind of next to worthless. Number one, what is selfassessment? Number two, I think everybody should have gait and balance evaluations and not based upon a fall history. (Geriatrician)
My first impression was this [specialist referral form] is kind of insulting… . I guess the concept is for the nongeriatrician. (Geriatrician)
The two PCP groups and the geriatricians, who reviewed the flowchart algorithm, thought it was too simple, so the final version was revised to include specific details (e.g., we added a list of specific items in the box labeled, “Conduct multifactorial risk assessment” [Figure 1]).
I think it’s a good guideline to start with. It simplifies it quite a bit but it’s a nice place to start. (Primary Care Physician)
I’m not convinced that the flowchart is very helpful. It’s the kind of stuff that you would do anyway. (Geriatrician)
The PAs, RNs, and NPs liked the format and information provided in the fact sheets and thought the patient education brochure about hypotension was both appropriate and helpful.
I thought it was very informative for the patient because when you’re doing a lot of patient education, a lot of times it’s just overwhelming for them. (Registered Nurse)
The RNs and NPs also liked the directions for the gait, strength, and balance assessment tests, and especially the instructions for measuring orthostatic blood pressure.
I like that the time frames are down here. That’s excellent because there are a lot of people that seem to have questions about that. (Registered Nurse)
The PCPs were enthusiastic about the sample case study.
I actually love this. It’s something I fully support and I think (case studies) can help in a great way. (Primary Care Physician)
The geriatricians, PAs, and NPs, who reviewed the Fall Risk Checklist and the two referral forms, were uncertain how useful these would be in their practice settings. We tried to address these concerns by expanding the list of risk factors in the Checklist and revising the referral form, Recommended Fall Prevention Programs, to include community exercise programs.
This (fall risk checklist) is very useful for me. It summarizes everything you see on a daily basis. (Physician Assistant)
Talking about Fall Prevention with Your Patient was reviewed by geriatricians, PCPs, RNs, and NPs and responses differed by type of provider. The geriatricians and PCPs did not think the guidelines for talking with patients about falls were useful or that the Stages of Change Model was applicable, whereas the RNs and NPs thought it was very pertinent.
I felt it was kind of a stretch to use this for this particular topic, because it does not seem to me that you are going to have quite as much of the resistance (as quitting smoking). (Primary Care Physician)
I would not have thought of this model in relation to falls. It sort of gives you an idea where your patient lies in their current state. (Nurse Practitioner)
I liked this piece of information. It gave me a lot of good ideas to improve what I’m already, you know, trying to do. (Registered Nurse)
Finally, based on feedback from the PCPs, RNs, and NPs, the wall chart, Integrating Fall Prevention into Practice, was modified so that fall prevention activities could be adapted more easily to various types and sizes of practices.
I think it is a very good explanation of who can or should do what… . I can see this in the exam room. (Nurse Practitioner)
You could put this not only in the clinics but in every department because it’s user friendly. It’s really informative. (Primary Care Physician)
The provider resources and patient educational materials in the completed STEADI tool kit are described in Table 2. All tool kit components and other supporting materials such as relevant research articles will be available at: www.cdc.gov/injury/STEADI.
TABLE 2.
Contents of the STEADI Fall Prevention Tool Kit for Health Care Providers
| Title | Description |
|---|---|
| Provider resources | |
| Algorithm for fall risk assessment and interventions | Simple algorithm based on the AGS/BGS clinical guideline |
| Three fact sheets | Statistics about falls, information about fall risk factors, and medications associated with falls |
| Three case studies | Illustrates patients with low, moderate, and high fall risk |
| Fall risk checklist | Summarizes a patient’s fall risk assessment results. It would become part of his or her medical record |
| Talking about fall prevention with your patients | Provides guidelines and examples of conversations with patients based on the Stages of Change Model (Prochaska & Velicer, 1997) |
| Measuring orthostatic blood pressure | Standardized instructions for measuring orthostatic blood pressure (Sclater & Alagiakrishnan, 2004) |
Three assessments
|
Standardized and validated gait, strength and balance assessments (Guralnik et al., 1994; Rikli & Jones, 1999; Vicarro, Perera, & Studenski, 2011) |
| Fall prevention patient referral form | A form to refer patients to relevant specialists such as neurologists and physical therapists |
| Recommended fall prevention programs | A form to refer patients to recommended community fall prevention or exercise programs |
| 3.5 in. × 5.5 in. pocket guide | Contains the algorithm as well as other key information that a provider might want to have readily available |
| 11 in. × 14 in. wall chart, Integrating Fall
Prevention into Practice |
Wall chart designed to help providers in various size practices plan how they will accomplish fall risk assessment and management in the context of their particular practice setting |
| Patient educational materials | |
| Stay Independent Brochure | Validated self-risk assessment brochure (Rubenstein, Vivrette, Harker, Stevens, & Kramer, 2011) |
| What YOU Can Do to Prevent Falls | CDC educational brochure |
| Check for Safety | CDC home safety brochure |
| Postural Hypotension: What It Is and How to Manage It |
Educational brochure |
| Chair Rise Exercise | One-page exercise handout |
NOTE: STEADI = Stopping Elderly Accidents, Deaths, and Injuries; AGS/BGS = American Geriatrics Society/British Geriatrics Society; CDC = Centers for Disease Control and Prevention.
DISCUSSION
The STEADI tool kit addresses identified knowledge gaps among primary health care providers regarding fall risk assessment, treatment, and referrals. It provides information and resources designed to help health care providers incorporate fall prevention into their clinical practice as well as a tool for linking primary care with community fall prevention and exercise programs.
This tool kit is unique in a number of ways. First, it translates the fall prevention process into specific activities that can fit into a variety of clinical settings. As shown in Figure 1, the STEADI tool kit algorithm can be used to assess and treat patients with all levels of fall risk. Although it largely follows the AGS/BGS clinical guideline, the STEADI tool kit also incorporates primary fall prevention. Low-risk older patients (those who have not fallen and/or do not have gait or balance problems) would be educated about how to prevent falls and referred to a community-based exercise program that emphasizes strength and balance.
Second, the tool kit is theory-driven and applies concepts from Wagner’s Chronic Care Model (Wagner, 1998) to fall risk. The Chronic Care Model identifies the essential elements of a health care system that encourages high-quality preventive as well as chronic disease care (Glasgow, Orleans, & Wagner, 2001).
These elements, as incorporated in the STEADI tool kit, include the health system (by embedding evidence-based guidelines into clinical practice through the chart, Integrating Fall Prevention into Practice); selfmanagement support (by emphasizing the patient’s role in managing their fall risk), delivery system design (by defining roles and distributing tasks among health care team members and implementing evidence-based interventions), decision support (by sharing evidence-based guidelines and information with patients to encourage their participation, and by using the Stay Independent self-risk assessment brochure); and the community (by linking primary health care referrals to community programs).
Fall prevention frequently requires that an individual change his or her behavior, and two components of the STEADI tool kit address this issue. One is the Stay Independent brochure that enables older persons to assess their personal fall risk and to initiate conversations about falling with their health care providers. The second component, Talking about Fall Prevention with Your Patient, is designed to help providers discuss fall prevention by applying Prochaska’s Transtheoretical Stages of Change Model (Prochaska & Velicer, 1997). Fall prevention requires behavioral change, and this model is a good fit because it depicts change as a “process involving progress through a series of stages.” Talking about Fall Prevention with Your Patient addresses four of the five stages of this model: precontemplation (not ready to change behavior), contemplation (preparing to change), preparation (ready to take action in the immediate future), and action (modifying behavior or acquiring new healthy behaviors). The maintenance stage was not included because older adults are most often in the early stages of behavior change for fall prevention. This may be because many older adults believe that falls just happen, falling is the result of “bad luck,” and/or are unaware that falls can be prevented (Stevens, Noonan, & Rubenstein, 2010).
For each stage, Talking about Fall Prevention with Your Patient provides a brief statement about how to move the patient to the next stage (i.e., “To move the patient to the preparation stage, make specific suggestions, be encouraging, and enlist support from the family”). It also provides real-world examples of patient–provider conversations for each of the four stages and offers possible responses to frequently heard statements.
The STEADI tool kit has a number of strengths. It incorporated input from a variety of health care providers at each stage of development; it is based on current evidence of what works to prevent falls (AGS/BGS, 2010; Gillespie et al., 2003; Michael et al., 2010) and emphasizes identifying and addressing modifiable fall risk factors; it is simple and practical, focusing on achieving fall risk assessment and management within the context of busy primary care practices; and it addresses communication barriers that can prevent patients from acting on fall prevention advice. In addition, some of the STEADI components may be applicable to settings outside of primary health care (e.g., Talking about Fall Prevention with Your Patients may be relevant and useful to health care professionals in the emergency department, particularly with patients who are treated and released; or in the hospital, with patients who have sustained a serious fall-related injury, to begin to address these patients’ underlying fall risk factors). Finally, all or part of the STEADI tool kit could be incorporated into electronic health records, to more easily integrate fall assessment, treatment, and referral into the clinical (electronic) workflow.
Limitations of the STEADI tool kit include lack of field testing of the various components in health care practice settings. This important next step is being undertaken as part of CDC-funded fall prevention cooperative agreements with the state health departments of Colorado, New York, and Oregon. Additional qualitative research with older adults to evaluate the patient educational materials also is needed. Finally, evaluating the STEADI tool kit using the Delphi method would ensure internal validity.
It should be noted that risk assessment alone does not decrease falls. Clinical assessment must be followed by individualized interventions to be effective. Finally, the patient educational materials are meant to supplement, not replace, the health care providers’ fall prevention activities. Health education by itself is not an effective fall intervention.
CONCLUSION
The STEADI tool kit is a broad, evidence-based resource designed with input from health care providers and intended to help them incorporate fall risk assessment and individualized fall interventions into clinical practice. Next steps will focus on pilot testing the tool kit in three states, including training providers in its use and evaluating its adoption and impact. Future activities may include incorporating STEADI into electronic medical records systems and/or creating an electronic application for handheld devices that can be used by physicians and other health care providers.
REFERENCES
- The American Geriatrics Society/British Geriatrics Society AGS/BGS clinical practice guideline: Prevention of falls in older persons. 2010 Retrieved from www.americangeriatrics.org/education/prevention_of_falls.shtml.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control Web-based Injury Statistics Query and Reporting System (WISQARS) 2012 Retrieved from www.cdc.gov/ncipc/wisqars.
- Chou WC, Tinetti ME, King MB, Irwin I, Fortinsky RH. Perceptions of physicians on the barriers and facilitators to integrating fall risk evaluation and management into practice. Journal of General Internal Medicine. 2006;21:117–122. doi: 10.1111/j.1525-1497.2005.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortinsky RH, Iannuzzi-Sucich M, Baker DI, Gottschalk M, King MB, Brown CJ, Tinetti ME. Fall-risk assessment and management in clinical practice: Views from healthcare providers. Journal of the American Geriatrics Society. 2004;52:1522–1526. doi: 10.1111/j.1532-5415.2004.52416.x. [DOI] [PubMed] [Google Scholar]
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community (Review) Cochrane Database of Systematic Reviews. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Quarterly. 2001;79:579–612. doi: 10.1111/1468-0009.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Wallace RB. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 1994;49A:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Jones TS, Ghosh TS, Horn K, Smith J, Vogt RL. Primary care physicians perceptions and practices regarding fall prevention in adults 65 years and older. Accident Analysis and Prevention. 2011;43:1605–1609. doi: 10.1016/j.aap.2011.03.013. [DOI] [PubMed] [Google Scholar]
- Michael YL, Whitlock EP, Lin JS, Fu R, O’Connor EA, Gold R. Primary care-relevant interventions to prevent falling in older adults: A systematic evidence review for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2010;153:815–825. doi: 10.7326/0003-4819-153-12-201012210-00008. [DOI] [PubMed] [Google Scholar]
- Masud T, Morris RO. Epidemiology of falls. Age and Ageing. 2001;30(Suppl. 4):3–7. doi: 10.1093/ageing/30.suppl_4.3. [DOI] [PubMed] [Google Scholar]
- Moyer VA. Prevention of falls in community-dwelling older adults: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2012;157:197–204. doi: 10.7326/0003-4819-157-3-201208070-00462. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American Journal of Health Promotion. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Rikli R, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. Journal of Aging and Physical Activity. 1999;7:129–161. [Google Scholar]
- Robinson BE, Barry PP, Renick N, Bergen MR, Stratos GA. Physician confidence and interest in learning more about common geriatric topics: A needs assessment. Journal of the American Geriatrics Society. 2001;49:963–967. doi: 10.1046/j.1532-5415.2001.49188.x. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: What does the evidence show? Medical Clinics of North America. 2006;90:807–824. doi: 10.1016/j.mcna.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Solomon DH, Roth CO. Detection & management of falls & instability among vulnerable elders by community physicians. Journal of the American Geriatrics Society. 2004;52:1527–1531. doi: 10.1111/j.1532-5415.2004.52417.x. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Vivrette R, Harker JO, Stevens JA, Kramer BJ. Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults. Journal of Safety Research. 2011;42:493–499. doi: 10.1016/j.jsr.2011.08.006. [DOI] [PubMed] [Google Scholar]
- Sclater A, Alagiakrishnan K. Orthostatic hypotension: A primary care primer for assessment and treatment. Geriatrics. 2004 Aug;59:22–27. [PubMed] [Google Scholar]
- Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. Journal of Trauma. 200150:116–119. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- Stevens JA, Corso PS, Finkelstein EA, Miller TR. Cost of fatal and nonfatal falls among older adults. Injury Prevention. 2006;12:290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Noonan RK, Rubenstein LZ. Older adult fall prevention: Perceptions, beliefs, and behaviors. American Journal of Lifestyle Medicine. 2010;4:16–20. doi: 10.1177/1559827616687263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton K, Logue E, Jarjoura D, Baughman K, Smucker W, Capers C. Assessing dietary and exercise stage of change to optimize weight loss interventions. Obesity Research. 2003;11:641–652. doi: 10.1038/oby.2003.92. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. New England Journal of Medicine. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- Vallis M, Ruggiero L, Greene G, Jones H, Zinman B, Rossi S, Prochaska JO. Stages of change for healthy eating in diabetes: Relation to demographic, eating-related, health care utilization, and psychosocial factors. Diabetes Care. 2003;26:1468–1474. doi: 10.2337/diacare.26.5.1468. [DOI] [PubMed] [Google Scholar]
- Vicarro LJ, Perera S, Studenski SA. Is Timed Up and Go better than gait speed in predicting health, function and falls in older adults? Journal of the American Geriatrics Society. 2011;59:887–892. doi: 10.1111/j.1532-5415.2011.03336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice. 1998;1:2–4. [PubMed] [Google Scholar]