Abstract
Objectives
Few evidence-based fall prevention programs have been evaluated for adoption in clinical settings. This study investigated the dissemination potential of a Tai Ji Quan-based program, previously shown efficacious for reducing risk of falls in older adults, through outpatient clinical settings.
Design
A single-group pre-post design in which participants attended a twice weekly Tai Ji Quan training program for 24 weeks.
Setting
Communities in Lane County, Oregon.
Participants
Referral patients (N = 379) aged 65 and older living independently.
Measurements
Using the RE-AIM framework, the primary outcome was the proportion of participating healthcare providers who made referrals. Secondary outcomes were the proportion of referred patients agreeing to participate and enrolling in the program, and measures of program implementation, maintenance, and effectiveness (on measures of falls, balance, gait, physical performance, and balance efficacy).
Results
Of the 252 providers invited to participate, 157 made referrals (62% adoption rate). Of 564 patients referred, 379 (67% reach) enrolled in the program, which was successfully implemented in senior/community centers with good fidelity. Of the total number of participants, 283 completed the program (75% retention) and 212 of these attended ≥75% of the total (48) sessions. Participants reported a reduction in falls with an incidence rate of 0.13 falls per person-month and showed significant improvement from baseline in all outcome measures. A 3-month post-intervention follow-up indicated encouraging levels of program maintenance among providers, patients, and community centers.
Conclusion
A protocol to refer patients at increased risk of falling to a Tai Ji Quan-based program was successfully implemented among healthcare providers. The evidence-based program appears readily scalable and exportable with potential for substantial clinical and public health impact.
Keywords: Dissemination, RE-AIM, older adults
INTRODUCTION
Unintentional falls among older adults in the United States have increasingly been recognized by public health officials and medical authorities as a serious public health issue.1–5 Falls, especially injurious falls, can have significant serious consequences on older adults, leading to decreased functional abilities, loss of independence, and early admission to nursing homes.6–8 Healthcare services and direct medical costs are subsequently impacted.2 Despite the significance of this problem, older-adult fall risk is not being adequately addressed in clinical practice.9 With increasing evidence that exercise-based interventions can prevent falls and reduce fall risk,10–14 efforts are needed to understand how these effective interventions can be routinely incorporated into clinical settings.
Tai Ji Quan, a balance training exercise based on martial arts movements, has proven effective in randomized controlled trials to reduce the risk of falling in community-dwelling older adults15–17 and people with Parkinson’s disease who experience postural instability.18 Subsequently, efforts have been made to put these findings into practice and an initial translational study has shown that this evidence-based program can be effectively implemented in community settings in terms of program adoption, outreach to the target population, and efficacy.19,20 However, the extent to which referral to an evidence-based fall prevention program can be integrated into routine clinical care of older persons who have a history (or a high risk) of falling is unclear. Addressing this issue is clinically important if the potential of fall screening and referral to preventative activities and targeted treatment through clinical care and/or health services1,5 is to be fully utilized.
To bridge this research-to-clinical-practice gap, the primary aim of this study was to evaluate the dissemination potential of Tai Ji Quan: Moving for Better Balance (formerly known as Tai Chi: Moving for Better Balance)19,20 through healthcare providers in outpatient settings. The secondary aims were to evaluate: a) the reach of the program to older adult patients, b) community-based class implementation, c) effectiveness of Tai Ji Quan-based movement practice in reducing falls, and d) maintenance of referral (by healthcare providers) and continued (post-program) practice (by participants). Accordingly, the RE-AIM framework21,22 was used to evaluate the study aims. On the basis of information derived from focus groups involving target healthcare providers, we predicted 20% of solicited providers would refer their qualified patients to the program.
METHODS
Study Area
The study area included 6 of 12 incorporated cities (Eugene, Springfield, Junction City, Veneta, Cottage Grove, Florence) in Lane County, Oregon. The county has a total population of 353,416, of which 54,426 are persons 65 years old and over (per U.S. Census 2011 estimates) living in both rural (Junction City, Veneta, Cottage Grove, Florence) and urban communities (Eugene, Springfield). The study area covered 64% of the county’s older adult population. The average annual (unintentional) fall fatality rate between 2000 and 2006 in individuals 65 years and older in the county was 45.3 per 100,000, compared to the national rate of 38.3 per 100,000 ages.23 There were 11 local senior and community centers within the study area that provided services for older people. These centers constituted target locations for implementing the program. The study protocol was approved by the Institutional Review Board of Oregon Research Institute, and informed consent was obtained from all participants.
Program Adopters and Study Population
The inclusion criteria for target adopters were local healthcare providers who worked with older adults (i.e., primary care physicians and other medical specialists, including physical therapists and nurse practitioners). In 2010, information on provider names and their specialties was obtained through the following professional organizations: (a) Oregon Medical Association (with specialties in family medicine, internal medicine, geriatric medicine, rehabilitation medicine, and general medicine), (b) Oregon Physical Therapist Licensing Board, and (c) Oregon State Board of Nursing. Names and status of practicing providers were further verified via e-mail contacts or provider websites throughout the active project period (2010–2012). A total of 323 providers, working in 63 clinics (i.e., medical, physical therapy, occupational therapy) within the study area were identified and met the inclusion criteria. Of these, 194 were medical doctors, 109 were physical therapists, and 20 were nurse practitioners.
The referral population was community-dwelling older adults who were (a) 65 years of age or over, (b) deemed at risk of falling (as judged by their healthcare providers using existing guidelines1), (c) physically mobile (i.e., could walk with or without an assistive device), (d) without severe cognitive deficits,24 and (e) referred by a healthcare provider to the program.
Recruitment Process for Patient Participants
Referrals
Initially a member of the investigative team contacted the administrators, managers, or providers of group-based and independent clinics within the study area. For providers who expressed interest, a follow-up meeting was arranged at the provider’s clinic to explain the intent of the program and its recruitment and class enrollment procedures in detail. Clinicians who were not available at the group meeting were subsequently reached on an individual basis. Referral forms with patient eligibility guidelines and materials (i.e., program brochures, exam room flyers, prescription/recommendation pads) were provided to the participating providers as an initial point of outreach to the target population and supplied throughout the project period (April 2010 to January 2012).
Class enrollment
Enrollment in this translational program was free to all referrals. Patients who received a referral from their providers were asked to call the research office and were then contacted by a research assistant, who conducted a brief phone screening (i.e., verification of age, fall history, mobility status) and scheduled an appointment for an in-office visit. At this visit, details about the program were described, and informed consent procedures and baseline assessments (involving a health survey, and balance, gait, and physical performance) were conducted. Trained research assistants, who were not blinded to study condition, conducted all assessments per established protocols.
Once sufficient patient referrals were received, local senior and/or community activity facilities were contacted to set up class logistics, followed by the implementation of the program described below.
Tai Ji Quan Program and Community Delivery
The Tai Ji Quan: Moving for Better Balance program, derived from the simplified 24-form Tai Ji Quan,25 consists of an 8-form core routine with a variety of built-in practice variations and a subroutine of Tai Ji Quan - Mini Therapeutic Movements. In contrast to prior training approaches involving Tai Ji Quan in fall prevention,15,16,26,27,28 this program employed an enhanced protocol in which the Tai Ji Quan movements were transformed into therapeutic training for balance and integrated into the daily functioning and clinical rehabilitation of participants. Specifically, the program involved a set of tailored Tai Ji Quan-based activities that focused on stimulating and integrating musculoskeletal and sensory systems via self-initiated movements such as ankle sways with feet planted, weight-shifting, trunk rotation/flexion/extension, and coordinated eyes-head-hand movements.29,30 The goals of the training were to improve postural stability and orientation, pelvic mobility and stability, control of body positioning, gait initiation and locomotion, gaze stability, and movement symmetry and coordination; to increase range of motion around the ankle joints; and to build lower-extremity strength. Chair-supported progressions, from completely seated, through sit-and-stand, to chair-assisted, were also included as part of the protocol.
Protocol
The program was delivered in two 1-hour sessions each week for 24 weeks. Each session consisted of: (a) warm-up exercises, (b) core practices, which included a mix of practice of forms, variations of forms, and mini-therapeutic movements, and (c) brief cool-down exercises. In terms of core exercises, during the initial 2–3 weeks practice time was spent on learning and drilling 2–3 forms in sets of 2–3, which progressively increased to 3–5 sets in later weeks. The protocol required that instructors: (a) complete teaching all 8 forms within 10–14 weeks, (b) teach each session with a mix of exercises that integrated the core components indicated above, and (c) include movements while seated, standing, or stepping, with varying speeds, ranges of motion, sensory inputs, and bases of support. Home practice was encouraged but not monitored.
Delivery
Community centers were first contacted for availability. The project staff and managers/supervisors worked together to develop an implementation plan that covered room size, number of participants, instructors, and schedule for class sessions. Classes were delivered by instructors trained by the first author during a 2-day workshop that covered: (a) background on clinical and translation research in Tai Ji Quan, (b) an orientation to falls in older adults and postural control mechanisms, (c) teaching and practicing core program routines, including forms, variations in forms, and mini-therapeutic movements, and (d) program instructions and implementation.
Evaluation
Adoption
This component was evaluated in two ways: (a) the proportion of providers approached by program personnel who agreed to participate and (b) the proportion of participating providers who made referrals during the active referral period (i.e., between April 2010 and January 2012). The representativeness of specialty care categories was evaluated by examining the percentage of participating providers in each category who were eligible to participate in the study area.
Reach
Reach was evaluated by dividing the number of patients who were enrolled by the total number of all referrals made during the entire study period.
Implementation
This was assessed by the extent to which instructors successfully implemented the various pre-specified program protocol components, that is, (a) delivered twice weekly 60-minute sessions across a 6-month period, (b) adhered to the teaching and training protocols (as verified by a program fidelity checklist), and (c) achieved participation and retention rates of 75% or better. The components in (b) focused primarily on (1) delivery - teaching emphases and movement execution, (2) integration - blending of forms, variations of forms, and mini-therapeutic movements, and (3) practice time - at least 40–45 minutes spent on core movements. The in-class fidelity check was conducted bi-monthly by the first author or experienced peer instructors.
Effectiveness
The primary endpoint was reduction in monthly falls frequency during the 24-week program implementation. Falls were reported by participants using falls calendars15 and verified by research assistants during a monthly phone call. Secondary endpoints included the change from baseline to 24 weeks in: (a) limits of stability (Maximum Excursion, Movement Control) measured by a Balance Master® System, (b) gait measures of stride length and walking velocity (GAITRite, CIR Systems), (c) Functional Reach,31 (d) Timed Up and Go,32 (e) time to rise from a chair,33 and balance efficacy assessed by a modified Activities-Specific Balance Confidence (ABC) scale, which measures confidence in one’s ability to avoid falling during the performance of activities of daily living.34 Both baseline and the 6-month follow-up assessments were conducted by trained research assistants in a research laboratory at the Oregon Research Institute. Participants who travelled more than 15 miles to the laboratory were paid $25 to complete the assessment.
Maintenance
Maintenance was defined as (a) clinician willingness to continue to make referrals after the translational study was completed (i.e., after 24 weeks) and (b) the percentage of participants who continued their Tai Ji Quan practice during the 12 weeks following the end of the 24-week program.
Data Analysis
Descriptive statistics are reported as the mean and standard deviation or percentage for all outcome measures, unless otherwise noted. The difference between the proportions of referrals between medical specialties was evaluated using the independent t-test for proportions. The fall incidence rate was determined as the number of falls that occurred during the study period divided by the total follow-up time in months (person-months of follow-up). Paired t-tests were conducted to examine change in the functional outcomes among participants from baseline to program termination at 6 months. We used SPSS version 18 for all calculations.
RESULTS
Adoption
Of 323 eligible providers, 252 agreed to participate. Of the remaining 71 providers, 10 did not provide a response and 61 could not be reached. Between March 2010 and January 2012, 157 of the participating clinicians referred patients to the program. Thus, 78% (252/323) of clinicians approached agreed to participate in the program, and 62% (157/252) actually made referrals (i.e., adopted the program). Participation by specialty and the proportion of each medical specialty that made referrals is summarized in Table 1.
Table 1.
Healthcare Provider Participation and Referral Status
| Specialty | No. of qualified providers* (N=323) |
No. of providers accepting† (N=252) |
Percent of representation by specialty‡ |
No. of providers making referrals (N=157) |
Percent of providers making referrals by specialty§ |
|---|---|---|---|---|---|
| Family medicine | 136 | 94 | 69 | 60 | 64 |
| Internal medicine | 53 | 44 | 83 | 35 | 80 |
| Geriatric medicine | 5 | 5 | 100 | 5 | 100 |
| Physical therapy‖ | 109 | 91 | 83 | 47 | 52 |
| Nurse practitioner¶ | 20 | 18 | 90 | 10 | 56 |
Number of eligible providers within Lane County, Oregon.
Providers who expressed interest in participating.
Calculated as number of accepting providers divided by the number of target providers.
Calculated as number of referring providers divided by the number of accepting providers.
Physical therapy included physical medicine (n=7) and occupational therapy (n=1).
Nurse practitioners included adult nurse practitioners (n=5), family nurse practitioners (n=11), and general nurse practitioners (n=4).
There was a significantly higher referral proportion from physicians (i.e., the combined specialties of family medicine, internal medicine, and geriatric medicine) than from physical therapists (0.69 vs. 0.51, P<0.05). In comparing internal medicine and family medicine providers, internal medicine doctors had a significantly higher referral proportion than family medicine doctors (0.80 vs. 0.63, P<0.05). Furthermore, providers (n=121), regardless of specialty, practicing in urban areas had a higher referral proportion (71%) than those practicing in rural areas (19%).
Reach
A total of 564 patients were referred during the active referral period. Of these, 185 (33%) did not enroll in the program for various reasons (i.e., could not commit to the length of the program = 105; class time conflict = 23; poor health or change in health conditions = 16; late referral = 25; others = 16). Most of these un-enrolled individuals (126/185=0.68) were living in rural areas. A total of 379 patients agreed to participate, completed the baseline assessment, and subsequently enrolled in classes, resulting in a 67% reach.
Population characteristics of the study sample are shown in Table 2. The mean age was 74 years (SD=8), 71% were women, and 95% were white, which approximates the population demographics in Lane County (91%). In all, 276 patients (73%) reported having two or more chronic conditions, 192 (51%) were taking two or more prescribed medications, and 221 (58%) reported having fallen at least once in the previous 3 months, with more than 60% of those having fallen two or more times. A total of 298 participants (78%) reported being afraid of falling. Participants’ overall physical activity levels prior to starting the class were below the recommended guidelines for moderate (i.e., 150 minutes per week) and vigorous (75 minutes per week) activity.35
Table 2.
Enrolled Patient Characteristics at Baseline (N=379)
| Measure | Study Estimate |
|---|---|
| Female, no. (%) | 269 (71) |
| Age in years, mean (SD) | 74 (8) |
| White, no. (%) | 360 (95) |
| Hispanic/Latino, no. (%) | 6 (2) |
| Education attainment, no. (%) | |
| High school diploma or lower | 224 (59) |
| College degree or higher | 155 (41) |
| Household income, no. (%) | |
| Less than $10,000 | 14 (3.7) |
| $10,000 to $14,999 | 52 (13.7) |
| $15,000 to $24,999 | 64 (16.9) |
| $25,000 to $34,999 | 101 (26.6) |
| ≥ $35,000 | 148 (39.1) |
| Body mass index, no. (%) | |
| <25 | 91 (24) |
| 25–29 | 135 (36) |
| ≥30 | 153 (40) |
| Resting blood pressure in mm Hg, mean (SD) | |
| Systolic | 134 (20) |
| Diastolic | 77 (11) |
| Falls in past 3 months, no. (%) | |
| No falls | 158 (42) |
| One fall | 83 (22) |
| Two falls | 77 (20) |
| Three falls | 31 (8) |
| Four or more falls | 30 (8) |
| Afraid of falling, no. (%) | |
| Yes | 298 (78) |
| No | 81 (22) |
| Health status, no. (%) | |
| Poor or fair | 49 (13) |
| Good | 167 (44) |
| Very good or excellent | 163 (43) |
| Chronic medical conditions,* no. (%) | |
| 0 | 24 (6) |
| 1 | 79 (21) |
| 2 | 81 (21) |
| ≥ 3 | 195 (52) |
| Number of medications taking, no. (%) | |
| 0 | 72 (19) |
| 1 | 116 (31) |
| 2 | 85 (22) |
| ≥3 | 107 (28) |
| Weekly physical activity, mean (SD) min/wk | |
| Moderate | 141 (154) |
| Vigorous | 22 (57) |
| Walking | 91 (114) |
These included arthritis, heart disease, high blood pressure, lung disease, diabetes, osteoporosis, depression, chronic back pain, and cancer.
Implementation
The 24-week program was successfully implemented in five senior centers, six community centers, one church, one dance studio, and one rehabilitation center. Each class progressed as designed and all instructors (n=6) successfully taught the required program routine.
A total of 283 participants completed the 24-week program, resulting in a 75% retention rate. There were no differences at baseline between those who completed the program and those who did not complete on characteristics of gender, age (65–74 years vs. 75–85+ years), health status, and risk factors of falls or fear of falling. There were also no differences between these two subgroups on falls and physical measures across the 24-week program implementation period.
The program included a total of 48 sessions. The median class attendance, including dropout participants, was 36 sessions (range, 1 to 48). Of those who completed the program, 212 participants (75%) attended 36 or more sessions (≥75% of the total).
Effectiveness
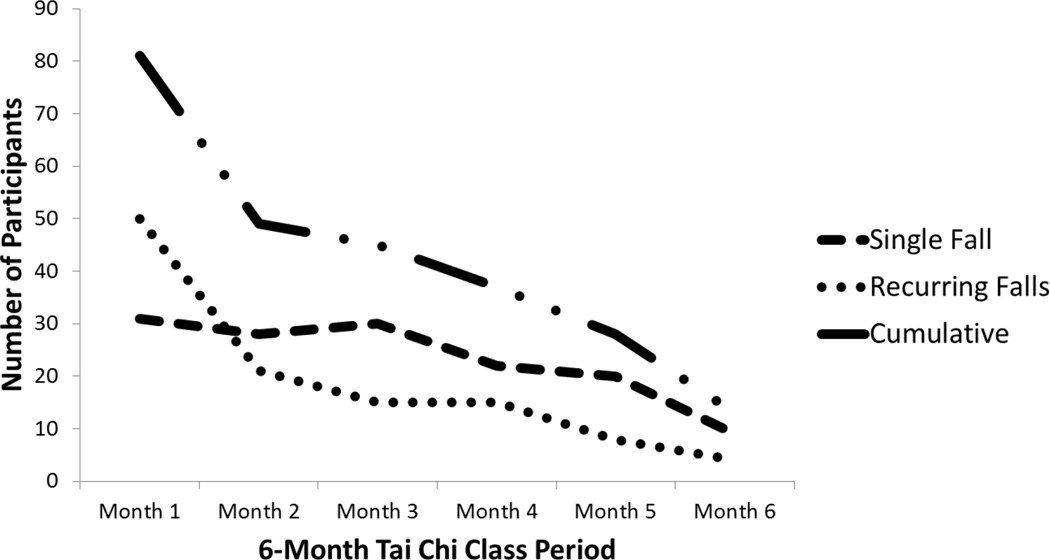
During the 24-week period, a total of 261 falls were reported by 119 participants (31%) over 1,995 person-months of follow-up, resulting in a fall-incidence rate of 0.13 falls per person-month. Of those who fell, 63 fell once and 56 fell two or more times. Of those reporting one or more falls at baseline (n=221), 127 participants (58%) reported no falls during the study period. The average time from baseline to first fall was 0.79 months (interquartile range: 1 month). Figure 1 shows fall incidence data across the 6-month study period. Falls shown included all falls that took place either during class sessions (3 minor falls recorded during warm-ups) or outside classes (all falls were verified as falls occurring in the home). As shown in Table 3, compared to baseline, at the end of the 24-week training program participants exhibited significant improvements in all secondary outcome measures.
Figure 1.
Incidence of Falls across the 24-Week Program Period (the number accounts for loss to follow-up). Note: Falls shown include those observed during class sessions or at home as reported by the participants.
Table 3.
Change in Outcome Measures from Baseline to 6 Months (N=379)
| Outcome Measures* | Baseline | 6-Montha | Mean Difference between Baseline and 6-Month |
P† |
|---|---|---|---|---|
| Maximum excursion, ‡ % (SD) | 63.69 (18.93) | 70.35 (15.67) | 6.66 (13.43) | ≤ 0.001 |
| Movement control, § % (SD) | 62.14 (22.75) | 69.19 (19.82) | 7.05 (14.08) | ≤ 0.001 |
| Stride length, mean ‖ (SD), cm | 106.12 (19.26) | 112.35 (19.94) | 6.23 (8.04) | ≤ 0.001 |
| Walking velocity, ¶ mean (SD), cm/s | 95.89 (23.52) | 103.93 (23.22) | 8.04 (10.30) | ≤ 0.001 |
| Functional Reach, # mean (SD), cm | 20.26 (6.68) | 23.38 (6.48) | 3.12 (5.0) | ≤ 0.001 |
| Timed Up and Go, ** mean (SD), sec. | 10.03 (4.79) | 8.83 (2.14) | −1.20 (3.85) | ≤ 0.001 |
| Chair-stands, †† mean (SD), sec. | 14.16 (6.56) | 12.93 (6.11) | −1.23 (3.09) | ≤ 0.001 |
| Balance efficacy, mean (SD) §§ | 3.67 (0.67) | 4.0 (0.76) | 0.33 (0.67) | ≤ 0.001 |
Missing values at all follow-ups were substituted by baseline values.
Paired t-tests
A measure of limits of stability that assesses the farthest distance displaced by a participant’s center of gravity while performing leaning/reaching tasks. Values range from 0% to 100%, with higher percentages indicating better balance. This is measured by a Balance Master® System.
A measure of limits of stability in which the amount of movement in the intended direction (toward the target) is compared to the amount of extraneous movement (away from the target), defined by the ratio of (amount of intended movement − amount of extraneous movement)/(amount of intended movement), expressed in percentage accuracy. The scores range from 0% to 100%, with higher percentages indicating better movement control. This is measured by a Balance Master® System.
Measures the distance between the heel points of two consecutive footprints of the same foot with the unit of measure being centimeters. Higher scores indicate greater stride length.
Measured by dividing the distance traveled by the ambulation time, with the unit of measure in centimeters per second. Higher scores indicate greater gait (walking) velocity.
Measures the maximal distance a participant can reach forward beyond arm’s length while maintaining a fixed base of support in a standing position. Higher scores indicate better balance.
Measures the time taken to rise from a chair, walk 10 feet (3 meters), return, and sit down. Lower scores indicate better mobility.
Measures lower-extremity strength by having participants perform 5 repetitions of sit-to-stand as quickly possible. Lower scores indicate better strength.
Modified Activities-Specific Balance Confidence (ABC) scale. The scores range from 1 (not confident) to 5 (completely confident) with higher scores indicating higher confidence.
Adverse event
Three falls that occurred during warm-up sessions were reported, but the participants sustained no injuries and continued the classes. There were no major adverse events, such as injurious falls or severe muscular pain, resulting from Tai Ji Quan exercises during any class.
Maintenance
A brief post-program survey was conducted at the end of the project. Of the 157 providers who referred patients, 121 (77%) responded, 32 did not respond (20%), 3 had relocated (2%), and 1 had retired. Of the respondents, 114 (94%) planned to continue encouraging their patients to participate in Tai Ji Quan. The level of continued interest and support by participating clinicians is demonstrated by the fact that in the first 8 months following the end of the study, 179 patients were referred by 79 providers to the project for placement in a class.
A follow-up participant survey conducted 3 months after the end of the intervention found that 173 participants (61% of those who completed the program) reported continuing weekly Tai Ji Quan practice, either on their own (n=20) or by attending a class (n=153; verified by class attendance sheets), for a median of 104 minutes each week (range: 15 to 315 minutes), which equated to the recommended 20–30 minutes of daily practice. All of the community centers where this program was implemented expressed strong interest in continuing to offer classes, and as of 1 year after the completion of the study all were still offering the program.
DISCUSSION
During the active enrollment period, the study demonstrated a substantially better-than-projected adoption rate of 62% by a variety of medical providers in terms of patient referrals to the Tai Ji Quan program. Of the different specialties, internal medicine physicians demonstrated the highest referral rate. Physicians generally had a higher rate than physical therapists, suggesting that, at least from this study, providers with medical degrees tend to be more likely to adopt. With respect to settings of clinical practice, providers with a practice in urban areas tended to have a higher referral rate compared to those in rural areas.
Of the total number of patients referred, 67% were enrolled in the 6-month community-based Tai Ji Quan class. The fall profiles of the participants indicated that high-risk patients were referred appropriately. Over 50% of the participants reported falling in the month prior to the start of the program; the majority of participants reported multiple falls (60%) and fear of falling (78%). This suggests that the current study was able to reach a high-risk patient population.
To maximize program dissemination potential, classes were delivered primarily through senior and community activity centers that provided senior services and could be easily accessed by community-dwelling older adults. Of the 11 centers approached, all expressed interest in offering room space (100% adoption) and willingness to assist in planning and scheduling classes. These findings are consistent with a prior community-based study.19
Trained instructors successfully implemented the program, with good fidelity with respect to program compliance and adherence to and completion of the training protocol. As was the case in prior work,15,19 at the end of the program participants demonstrated improved balance, gait, and mobility; falls efficacy; and fewer falls. Despite the longer duration of the current study (6 months vs. 3 months in a community centers outreach study19), there were comparable rates of class participation (75%) and program retention (75%) using the clinical referral method of recruitment compared to the community centers-based promotion and public advertisement method (75% for class participation, 80% class attendance, respectively). Data from a 3-month follow-up in the present study indicated sustainability in that the majority of participants continued their Tai Ji Quan practice, a general phenomenon observed in prior studies.15,16,19,26
In the exit survey, providers indicated that they intended to continue referring patients and encouraging them to do the Tai Ji Quan exercises. The fact that this project continued to receive referrals after the active enrollment period ended indicated good sustainability. It also suggested that once providers are made aware of community resources for fall prevention, they are likely to continue using these avenues to support their patients. Thus, community-based programs can become an integral component of clinical falls-risk screening/assessment and intervention.
A challenge to sustainability is how to keep providers informed about resources, such as evidence-based classes, that are available in their community so that they can continue referring patients. Experience with this project suggests that communicating frequently with clinicians and program implementers, offering educational outreach workshops, and even providing training in Tai Ji Quan to clinicians may facilitate the referral process. For example, offering physical and occupational therapists the opportunity to undertake the training program as part of their continuing education helped increase referrals during the study period. Additionally, these clinicians applied components of the program, for example, the mini-therapeutic movements, in their clinical practice. However, the feasibility of training clinicians to improve adoption and sustainability of evidence-based programs in clinical practice was not explicitly evaluated in this study but is important and therefore requires formal evaluation in future studies.
Practical Implications
This study has some clinical implications. First, with national guidelines recommending Tai Ji Quan exercises for prevention of falls,1,5 results from this study suggest it is feasible to engage healthcare providers to make evidence-based recommendations for the management of falls and/or balance-related issues in older adults. Second, it suggests that, in addition to using recruitment resources from the community (e.g., senior centers or services), involving clinicians through a simple referral system is likely to maximize older adult participation in community-based fall prevention programs. Lastly, because Tai Ji Quan programs involve relatively little cost (instructor salary; facilities rental) and are easy to implement (i.e., non-equipment dependent, simple practice arrangement), a variety of funding models, ranging from self-supporting user fees to government grants or health reimbursement programs,36, 37 can be used to establish them in community and clinical settings. For example, in the United States the average cost of a self-support-model Tai Ji Quan class is $3–$5 per person per class.19,38 The Administration on Aging has supported state-wide implementation of evidence-based health and prevention programs, including falls prevention,39 through grants to local Area Agencies on Aging.
Study Limitations
The lack of information about the process that clinicians used to decide whether or not to make a referral is a limitation in the current study. Such information would be useful in determining how to increase appropriate referrals to fall prevention programs. A second limitation is that there was no mechanism in place to provide patient-specific feedback to individual referring providers. This information could be useful for providers in re-evaluating patient fall-risk. A third limitation is the lack of a comparison group to measure effectiveness. However, it is important to note that the primary purpose of the study was to examine the dissemination potential of an evidence-based program that had demonstrated effectiveness, and the results of the secondary outcomes of falls, balance, gait, and physical function further strengthened previous findings of its effectiveness. A fourth limitation is that generalizability of the results may be limited to access to senior and community activity centers that were the primary settings for classes in this study. However, it should be noted that this program has also been successfully implemented in a variety of community-accessible facilities including YMCA/YWCA and churches. Finally, research assessors were aware of participant intervention status, which was a potential source of bias in the outcome assessments. However, none of the research assistants were aware of the study hypotheses, knew any of the participants’ previous measurement scores, or were involved in any data entry or analyses.
Conclusion
This study demonstrates that the evidence-based Tai Ji Quan: Moving for Better Balance fall prevention program can be successfully disseminated by having clinicians refer their patients at risk of falling directly to this community-based program. Future studies should investigate mechanisms that would enhance the connections and coordination between healthcare providers and community programs, as well as explore the feasibility of implementing the program through healthcare systems.36, 37 Additionally, the plausibility of maximizing sustainability by providing incentives and opportunities for clinical referrals (e.g., reimbursement, education, training)10 should be explored in future studies.
ACKNOWLEDGMENTS
We wish to thank all of the participants for their support and dedication to this research project, as well as the healthcare providers who referred their patients to participate in it. Appreciation is also extended to the project instructors and staff.
The project reported in this manuscript was supported through a cooperative agreement with the Centers for Disease Control and Prevention (No. 5R18CE001723).
F. Li - paid by a CDC grant (5R18CE001723)
P. Harmer - paid by a CDC grant (5R18CE001723)
R Stock - paid by a CDC grant (5R18CE001723)
K. Fitzgerald - paid by a CDC grant (5R18CE001723)
Sponsor’s Role: None.
Appendix
No financial conflicts of interest was reported by the authors of this paper.
Conflict of Interest Disclosures:
| Elements of Financial/Personal Conflicts |
*Author 1 – FL | Author 2 – PH | Author 3 – RS |
Author 4 – KF | ||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | No | No | No | No | ||||
| Grants/Funds | Yes | Yes | No | No | ||||
| Honoraria | No | No | No | No | ||||
| Speaker Forum | No | No | No | No | ||||
| Consultant | No | No | Yes | Yes | ||||
| Stocks | No | No | No | No | ||||
| Royalties | No | No | No | No | ||||
| Expert Testimony | No | No | No | No | ||||
| Board Member | No | No | No | No | ||||
| Patents | No | No | No | No | ||||
| Personal Relationship | No | No | No | No | ||||
| Elements of Financial/Personal Conflicts |
*Author 5 - JS | Author 6 - MG | Author 7 - LC |
Author 8 - KC | ||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | No | No | No | No | ||||
| Grants/Funds | No | No | No | No | ||||
| Honoraria | No | No | No | No | ||||
| Speaker Forum | No | No | No | No | ||||
| Consultant | No | No | No | No | ||||
| Stocks | No | No | No | No | ||||
| Royalties | No | No | No | No | ||||
| Expert Testimony | No | No | No | No | ||||
| Board Member | No | No | No | No | ||||
| Patents | No | No | No | No | ||||
| Personal Relationship | No | No | No | No | ||||
| Elements of Financial/Personal Conflicts |
*Author 9 - JV | |
|---|---|---|
| Yes | No | |
| Employment or Affiliation | No | |
| Grants/Funds | No | |
| Honoraria | No | |
| Speaker Forum | No | |
| Consultant | No | |
| Stocks | No | |
| Royalties | No | |
| Expert Testimony | No | |
| Board Member | No | |
| Patents | No | |
| Personal Relationship | No | |
Authors can be listed by abbreviations of their names.
For all “Yes” responses, provide a brief explanation here:
Author Contributions:
F. Li originated the study, supervised all aspects of its implementation, performed data analysis, and wrote the article. P. Harmer assisted with the implementation, analysis, interpretation, and the writing of this article. R. Stock and K. Fitzgerald contributed to the concept and design of this research project. J. Stevens, M. Gladieux, L-S Chou, K. Carp, and J. Voit contributed substantively to the interpretation of the study outcomes and writing and revisions of the article.
Contributor Information
Fuzhong Li, Oregon Research Institute, Eugene, OR
Peter Harmer, Department of Exercise Science, Willamette University, Salem, OR.
Ronald Stock, Oregon Health & Science University, Portland, OR.
Kathleen Fitzgerald, Oregon Medical Group, Eugene, OR.
Judy Stevens, Centers for Disease Control and Prevention, Atlanta, GA.
Michele Gladieux, Outpatient Rehabilitation Services, Sacred Heart Medical Center, Peace Health, Eugene, OR.
Li-Shan Chou, University of Oregon, Eugene, OR
Kenji Carp, Cooperative Performance & Rehabilitation, Eugene, OR.
Jan Voit, Harborview Medical Center, Seattle, WA.
REFERENCES
- 1.American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2011;49:664–672. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Falls among older adults: an overview. 2012 www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html.
- 3.Fuller G. Falls in the Elderly. Am Fam Physician. 2000;61(7):2159–2168. [PubMed] [Google Scholar]
- 4.National Institutes of Health. Falls and older adults. Accessed at: http://nihseniorhealth.gov/falls/aboutfalls/01.html on 5 January 2013.
- 5.Moyer VA. Preventing Falls in Older Adults Who Live in Community Settings: U.S. Preventive Services Task Force Recommendation. Ann Intern Med. 2012;157:197–204. doi: 10.7326/0003-4819-157-3-201208070-00468. [DOI] [PubMed] [Google Scholar]
- 6.Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82:1020–1023. doi: 10.2105/ajph.82.7.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50:116–119. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Tinetti TE, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 9.Järvinen T, Sievanen H, Khan K, et al. Shifting the focus in fracture prevention from osteoporosis to falls. Br Med J. 2008;336:124–126. doi: 10.1136/bmj.39428.470752.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noonan RK, Stevens JA, Baldwin G. The public health approach to older adult fall prevention: Comments from the U.S. Centers for Disease Control and Prevention. Open Longevity Sci. 2011;5:26–31. [Google Scholar]
- 11.Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ. 2004;328:680–688. doi: 10.1136/bmj.328.7441.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. 2012;(9) doi: 10.1002/14651858.CD007146.pub3. Art. No. : CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sherrington C, Julie C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JCT. Effective Exercise for the Prevention of Falls: A Systematic Review and Meta-Analysis. J Am Geriatr Soc. 2008;56:2234–2243. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 14.Stevens JA, Sogolow ED. A CDC Compendium of Effective Community-Based Interventions from Around the World. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2008. Preventing falls: What works. [Google Scholar]
- 15.Li F, Harmer P, Fisher KJ, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60:187–194. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 16.Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 17.Wolf SL, Sattin RW, Kutner M, et al. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 2003;51:1693–1701. doi: 10.1046/j.1532-5415.2003.51552.x. [DOI] [PubMed] [Google Scholar]
- 18.Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J, Maddalozzo G, Batya S. Tai Chi and postural stability in patients with Parkinson’s disease. N Engl J Med. 2012;366 doi: 10.1056/NEJMoa1107911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li F, Harmer P, Glasgow R, Mack KA, Sleet D, Fisher KJ, Kohn MA, Millet LM, Mead J, Xu J, Lin ML, Yang T, Sutton B, Tompkins Y. Translation of an effective Tai Chi intervention into a community-based falls prevention program. Am J Pub Health. 2008;98(7):1195–1198. doi: 10.2105/AJPH.2007.120402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li F, Harmer P, Mack KA, Sleet D, Fisher KJ, Kohn MA, Millet LM, Xu J, Yang T, Sutton B, Tompkins Y. Tai Chi: Moving for Better Balance – Development of a community-based falls prevention program. J Phy Acti Health. 2008;5:445–455. doi: 10.1123/jpah.5.3.445. [DOI] [PubMed] [Google Scholar]
- 21.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Pub Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 22.Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) [Accessed January 2013]; Available at: www.re-aim.org. [Google Scholar]
- 23.Centers for Disease Control and Prevention. [Accessed January 2013];Fatal injury data. Available at: http://www.cdc.gov/injury/wisqars/fatal.html.
- 24.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatric Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 25.China National Sports Commission. Simplified Taijiquan. Beijing, China: People’s Sports; 1983. [Google Scholar]
- 26.Taylor D, Hale L, Schluter P, Waters DL, Binns EE, McCracken H, McPherson K, Wolf SL. Effectiveness of Tai Chi as a Community-Based Falls Prevention Intervention: A Randomized Controlled Trial. J Am Geriatr Soc. 2012;60:841–848. doi: 10.1111/j.1532-5415.2012.03928.x. [DOI] [PubMed] [Google Scholar]
- 27.Logghe IHJ, Zeeuwe PEM, Verhagen AP, et al. Lack of effect of tai chi chuan in preventing falls in elderly people living at home: A randomized clinical trial. J Am Geriatr Soc. 2009;57:70–75. doi: 10.1111/j.1532-5415.2008.02064.x. [DOI] [PubMed] [Google Scholar]
- 28.Voukelatos A, Cumming R, Lord S, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: The Central Sydney tai chi trial. J Am Geriatr Soc. 2007;55:1185–1191. doi: 10.1111/j.1532-5415.2007.01244.x. [DOI] [PubMed] [Google Scholar]
- 29.Li F. Transforming Traditional Tai Ji Quan techniques into integrative movement therapy. J Sport Health Sci. doi: 10.1016/j.jshs.2013.11.002. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li F. Tai Ji Quan exercise for people with Parkinson’s disease and other neurodegenerative movement disorders. International J Integ Med. 2013;1:4–8. doi: 10.5772/56243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duncan PW, Weiner DK, Chandler J, et al. Functional reach: A new clinical measure of balance? J Gerontol: Med Sci. 1990;45:M192–M197. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- 32.Podsiadlo D, Richardson S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 33.Lord SR, Murray SM, Chapman K, et al. Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol: Med Sci. 2002;57:539–543. doi: 10.1093/gerona/57.8.m539. [DOI] [PubMed] [Google Scholar]
- 34.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol: Med Sci. 2005;50:M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 35.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;8:1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 36.Tinetti ME, Brach JS. Translating the fall prevention recommendations into a covered service: Can it be done, and who should do it? Ann Inter Med. 2012;157:213–214. doi: 10.7326/0003-4819-157-3-201208070-00014. [DOI] [PubMed] [Google Scholar]
- 37.Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med. 2010;363:1296–1299. doi: 10.1056/NEJMp1008560. [DOI] [PubMed] [Google Scholar]
- 38.Li F, Harmer P, McAuley E, Duncan TE, Duncan SC, Chaumeton NR, Fisher J. An evaluation of the effects of Tai Chi exercise on physical function among older persons: a randomized controlled trial. An Beh Med. 2001;2:89–101. doi: 10.1207/S15324796ABM2302_9. [DOI] [PubMed] [Google Scholar]
- 39.Administration on Aging. Accessed at: http://www.aoa.gov/AoARoot/AoA_Programs/HCLTC/Evidence_Based/ on 5 July 2013.