INTRODUCTION
Falls: Definition and Magnitude of the Problem
Falls occur more often with advancing age. Each year, approximately 30% to 40% of people aged 65 years and older who live in the community fall.1 Roughly half of all falls result in an injury,2 of which 10% are serious,3 and injury rates increase with age.4 The direct medical costs for falls total nearly $30 billion annually.5
Falls in the outpatient setting are usually defined as “coming to rest unintentionally on the ground or lower level, not due to an acute overwhelming event”6 (eg, stroke, seizure, loss of consciousness) or external event to which any person would be susceptible.
Falls are a major threat to older adults’ quality of life, often causing a decline in self-care ability and participation in physical and social activities. Fear of falling, which develops in 20% to 39% of people who fall, can lead to further limiting activity, independent of injury.7
Fall Risk Factors
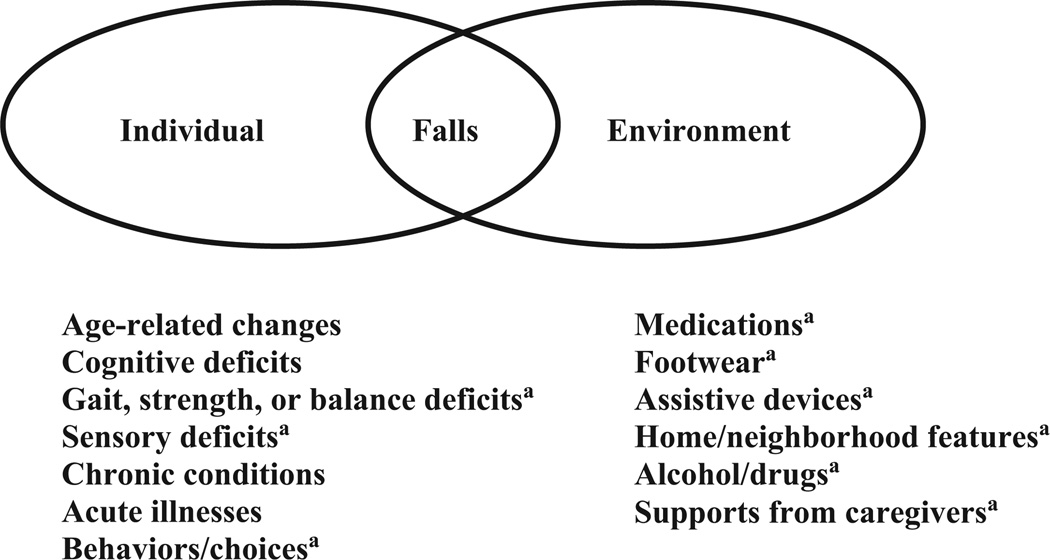
Fall risk factors increase the likelihood that a person will fall. These risk factors can be categorized as extrinsic (external to the individual) and intrinsic (within-person) (Fig. 1). Intrinsic factors include several age-related physiologic changes, as summarized in Table 1.
Fig. 1.
Falls result from an interaction between factors in the individual (intrinsic) and the environment (extrinsic). a Factors that may be modifiable with intervention.
Table 1.
Aging-related physiologic changes in organ systems that affect fall risk
| Organ System | Physiologic Change |
|---|---|
| Muscular system | Decreased muscle strength |
| Nervous System | |
| Balance | Increased postural sway Slowed righting reflexes |
| Gait | Decreased step height Decreased proprioception |
| Vision | Reduced papillary response to light variation Thickening and loss of elasticity of lens |
Many falls result from interactions among multiple risk factors, and the risk of falling increases linearly with the number of risk factors.1 However, even among community-dwelling people aged 75 years and older without risk factors, approximately 10% fall during any given year.1 Therefore, all older adults should be recognized as being at some increased risk for falling.
Falls from Older Adults’ Perspective
Older adults frequently think that falls are inevitable with aging8 but underestimate their personal risk of falling.9 Environmental and behavioral factors (eg, rushing, being distracted) are most often seen as causing falls; intrinsic (personal/health) factors are rarely recognized. Thus, primary care providers (PCPs) have a crucial role in helping patients understand the importance of intrinsic factors in causing falls.
Few older adults use proven fall prevention strategies such as balance exercises.10 When asked what they are doing to prevent future falls, people commonly report being more careful.11 However, there is no evidence that being more careful alone prevents falls.
Less than half of older adults who fall talk with their health care providers about it.12 Therefore, guidelines specify that providers should ask all their patients aged 65 years and older about falls at least annually.13 By evaluating patients for fall risk and encouraging them to adopt evidence-based prevention strategies, PCPs can help patients reduce their chances of falling and experiencing functional decline, injury, or death.
FALL RISK ASSESSMENT
Clinical Practice Guideline
A 2012 Cochrane Systematic Review reported that clinical assessment by a health care provider combined with individualized treatment of identified risk factors, referral if needed, and follow-up reduced the rate of falls by 24%.14 Similarly, the US Preventive Services Task Force found that multifactorial clinical assessment and management, combined with follow-up, was effective in reducing falls.15
The American Geriatrics Society and British Geriatrics Society (AGS/BGS) have published a clinical practice guideline on fall risk screening, assessment, and management. 13 The AGS/BGS guideline13 recommends screening all adults aged 65 years and older for fall risk annually. This screening consists of asking patients whether they have fallen 2 or more times in the past year or sought medical attention for a fall, or, if they have not fallen, whether they feel unsteady when walking. Patients who answer positively to any of these questions are at increased risk for falls and should receive further assessment. People who have fallen once without injury should have their balance and gait evaluated; those with gait or balance abnormalities should receive additional assessment. A history of 1 fall without injury and without gait or balance problems does not warrant further assessment beyond continued annual fall risk screening.13
A fall risk assessment is required as part of the Welcome to Medicare examination. PCPs can receive reimbursement for fall risk assessment through the Medicare Annual Wellness visit and incentive payments for assessing and managing fall risk through voluntary participation in the Physician Quality Reporting System.
Implementing Screening and Assessment
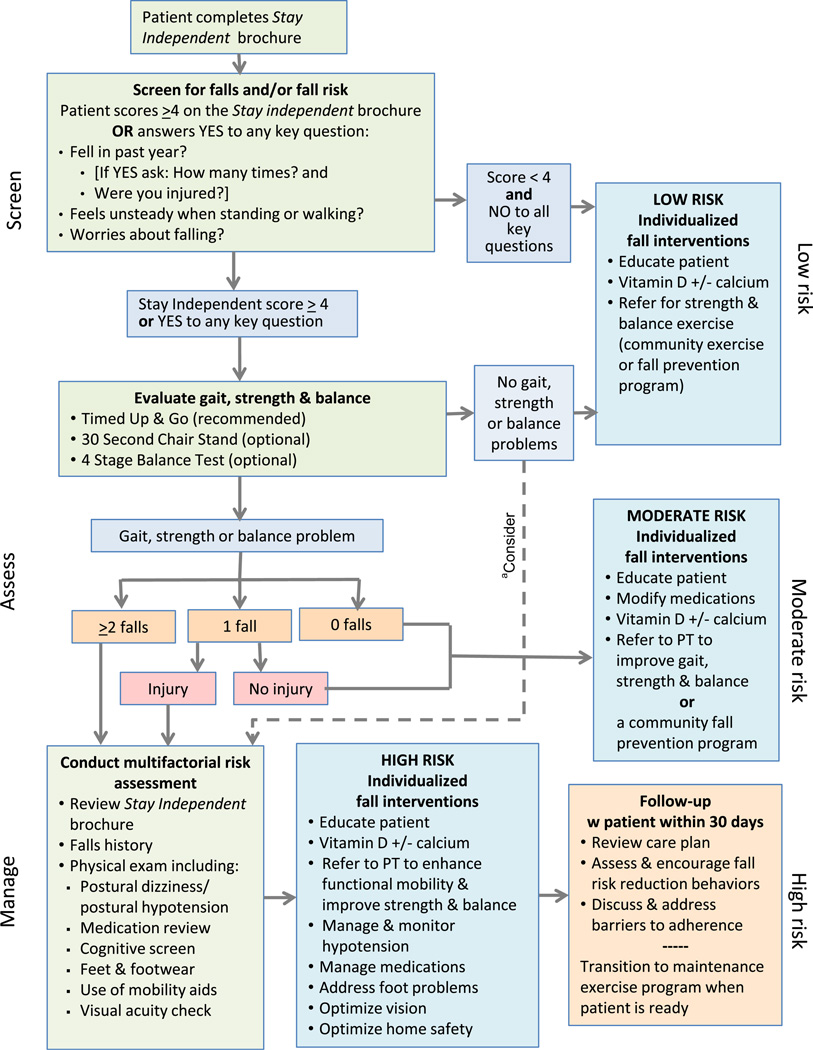
The US Centers for Disease Control and Prevention (CDC) has developed an algorithm that details each step of screening and assessment and guides interventions based on each individual’s level of risk (Fig. 2).
Fig. 2.
STEADI (Stopping Elderly Accidents, Deaths, and Injuries) algorithm. a For patients who screen positive for falls but have no gait, strength, or balance problems, consider additional risk assessment (eg, medication review, cognitive screen, syncope). PT, physical therapist. (From Centers for Disease Control and Prevention. Algorithm for fall risk assessment & interventions. Available at: http://www.cdc.gov/homeandrecreationalsafety/pdf/steadi/algorithm_fall_risk_assessment.pdf. Accessed November 11, 2014.)
This algorithm is part of a tool kit called STEADI (Stopping Elderly Accidents, Deaths, and Injuries).16 Based on the AGS/BGS guideline13 with input from practicing clinicians, STEADI was designed to help health care providers integrate falls assessment and management into their practice. The algorithm highlights that even individuals at low risk (no history of falls, no problems with gait or balance) can benefit from a primary prevention approach, namely education about fall risk factors, strength and balance exercises, and vitamin D supplementation.15 The recommended dose of vitamin D for fall prevention is 1000 IU of cholecalciferol daily.17
Fall Risk Assessment
A risk assessment consists of a falls history, medication review, physical examination, and functional and environmental assessments.
The falls history
A falls history should include determining the number of falls in the past year as well as their circumstances, including any premonitory symptoms, location, activity, footwear, use of assistive device (if prescribed), use of glasses (if typically used), ability to get up after the fall, time of day, any injuries sustained, and any medical treatment received. Corroboration by a witness can be helpful in cases of recurrent, unexplained falls, because such falls may be caused by unrecognized syncope.18 Documenting a falls history is one of the quality indicators for fall prevention and management.19
Medications and falls
A critical part of risk assessment is a medication review. Several classes of medications increase fall risk (Table 2). Psychoactive medications in particular are independent predictors of falls.20 These medications tend to be sedating, alter the sensorium, and impair balance and gait. Other medications (eg, antihypertensives, nonsteroidal antiinflammatory drugs, diuretics) are more weakly associated with falls.21
Table 2.
Medications that increase the risk of falls
| Medication Class | Odds Ratio (95% CI) |
|---|---|
| Psychoactive Medications | |
| Antidepressants | 1.68 (1.47–1.91) |
| Antipsychotics | 1.59 (1.37–1.83) |
| Sedative hypnotics | 1.47 (1.35–1.62) |
| Benzodiazepines | 1.57 (1.43–1.72) |
| Other Medications | |
| Antihypertensives | 1.24 (1.01–1.50) |
| Nonsteroidal antiinflammatory drugs | 1.21 (1.01–1.44) |
| Diuretics | 1.07 (1.01–1.14) |
Abbreviation: CI, confidence interval.
Data from Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 2009;169:1957.
A key strategy is to reduce the dose of any indicated medications that contribute to fall risk and to taper and stop any medications that are no longer indicated.22 Nonpharmacologic approaches (eg, sleep hygiene measures for insomnia) are often a useful alternative.
Postural hypotension
Postural hypotension is defined as a reduction in systolic blood pressure of at least 20 mm Hg or in diastolic blood pressure of at least 10 mm Hg within 3 minutes of standing. Postural hypotension affects approximately 30% of community-dwelling older adults23 and is a fall risk factor. Patients may experience lightheadedness, blurred vision, headache, fatigue, weakness, or syncope within 1 to several minutes of standing up, or they may be asymptomatic. In contrast, patients may experience postural lightheadedness without a measured blood pressure reduction; this should be considered equivalent to postural hypotension for fall risk. Postural hypotension can often be alleviated by reducing the dosage of blood pressure–lowering medications and/or stopping medications that have orthostatic hypotension as a side effect. Use of above-the-knee support hose and sleeping with the head of the bed elevated may also reduce postural reductions in blood pressure.
Fall-focused physical examination
The recommended elements of a fall-focused physical examination are shown in Box 1. An essential exam element is assessment of the patient’s gait and balance. Three quick gait, strength, and balance tests are the Timed Up-and-Go (TUG), the 30-Second Chair Stand test, and the 4-Stage Balance test. These tests are described in the STEADI tool kit and shown in online instructional videos at: http://www.cdc.gov/homeandrecreationalsafety/Falls/steadi/index.html.
Box 1: Key elements of fall-focused physical examinations.
Examination element
Orthostatic vital signs
Distance visual acuity
Cardiac examination (rate, rhythm, murmurs)
Gait and balance evaluationa
Musculoskeletal examination of back and lower extremities
Neurologic examination
Cognitive screen
Sensation
Proprioception
Muscle bulk, tone, strength, reflexes, and range of motion
Higher neurologic function (cerebellar, motor cortex, basal ganglia)
a Recommended evaluations include the Timed Up-and-Go, 30-Second Chair Stand, and 4-Stage Balance tests.
The TUG, a test of functional mobility, involves timing a person standing up from a chair with armrests (using their assistive device if they normally use one), walking 3 m (10 feet) at their usual pace, turning, returning to the chair, and sitting down. A TUG time greater than or equal to 12 seconds suggests high fall risk.24
The 30-Second Chair Stand test assesses lower extremity strength and balance. Being unable to stand up from a chair of knee height without using one’s arms indicates increased fall risk.20
The 4-Stage Balance test assesses static balance by having the patient stand in 4 positions, each progressively more challenging. Positions include the parallel, semi-tandem, tandem, and single-leg stand.25 Inability to perform a tandem stand (ie, heel of one shoe touching toe of the other) for 10 seconds predicts falls, and the inability to stand on 1 leg unassisted for 5 seconds predicts injurious falls.26
Cognitive testing is also an important part of the fall-related physical examination and may consist of a brief cognitive screen such as the Mini-Cog.27 People with moderate to severe cognitive impairment are at high risk of falls.
Functional assessment
Assessing a patient’s level of functioning is usually accomplished by asking standardized questions about difficulties with performing activities of daily living and instrumental activities of daily living. The risk of falling and the circumstances and location of falls vary by functional ability.28 People who are healthier are more likely to fall on stairs, away from home, and during displacing activities (eg, bending over, reaching up), and are more likely to be seriously injured if they fall.28 By contrast, people with functional limitations are more likely to fall at home during routine activities. Gauging functional ability can help determine the degree of fall and injury risk, indicate risk factors, and suggest interventions.
Laboratory tests and imaging
A comprehensive assessment may involve laboratory tests. These tests could include thyroid-stimulating hormone, vitamin B12 level, complete blood count, 25-hydroxy vitamin D level, and other laboratory tests if clinically indicated.29
A dual-energy x-ray absorptiometry scan should be done if bone mineral density has not been assessed. No other radiographic imaging study is routinely necessary. However, based on signs and symptoms, such as evidence of head injury or a new focal neurologic deficit, computed tomography or MRI of the brain may be indicated. An assessment for causes of syncope should be conducted only if there is strong suspicion, as in the case of recurrent, unexplained falls.
Environmental assessment
Environmental assessment, which is typically conducted by a trained health professional (eg, occupational therapist [OT]) on referral from the PCP, is intended to identify hazardous conditions within the home, such as obstacles in pathways or on stairs, unsupportive or ill-fitting footwear, unsuitable assistive devices, inadequate lighting, and slippery surfaces. It also identifies hazards outside the home, such as cracked pavement or sloped yards. Identifying and modifying environmental factors is an effective intervention as part of a comprehensive multifactorial approach to preventing falls.13 It is also effective as a single intervention when delivered by an OT.14 OTs consider behavioral factors that affect fall risk as well as adaptations that older adults can make to function safely in and around their homes.30
MANAGEMENT OF FALL RISK
Management Goals for Older Adults at Risk of Falls
Goals for fall risk management include (1) reduce the chances of falling, (2) reduce the risk of injury, (3) maintain the highest possible level of mobility, and (4) ensure ongoing follow-up.
Clinical Approach to Managing Fall Risk
Collaborate with patients and their caregivers to address fall risk factors
Providers should explore older adults’ perceptions of the causes of their falls and willingness to make changes to reduce their risk of falling again. Approaches that facilitate behavior change include presenting the information that falls can be prevented, providing choices, personalizing options, and focusing strategies on enhancing quality of life (eg, maintaining independence).8 The STEADI tool kit16 includes guidance on talking about fall prevention with patients. There are examples of patients in various stages of readiness to make changes to reduce their fall risk, with possible provider responses for each stage.
Discuss the importance of strength and balance exercise
Exercise interventions that focus on improving strength and balance are the most effective single intervention for reducing falls and fall-related injuries.14 Most older adults do not routinely practice these types of exercises.31 Other forms of exercise (eg, stretching, walking) have not been shown to reduce falls.32
To be effective, exercise must (1) focus on improving balance, (2) be of moderate to high challenge and progress in difficulty, and (3) be practiced a minimum of 50 hours, which equates to 2 hours weekly for 25 weeks.32 PCPs can educate patients about exercise that prevents falls and refer to appropriate resources (eg, physical therapists [PTs], community fall prevention programs) to initiate it. It is important to emphasize that the effects of exercise will not be apparent for several months, and that practice must be ongoing in order to maintain the benefits.
Evidence-based exercise programs may be either home based (eg, Otago Exercise Program33) or group classes offered in community settings (eg, tai chi34).
Prioritize interventions for modifiable risk factors
Because the risk of falling increases with the number of risk factors, risk can be reduced by modifying even a few contributing factors. Three key risk factors (balance, medications, and home safety) should be addressed in everyone at high risk.35 In addition, if the PCP suspects that a cataract is affecting vision, it is beneficial to refer the patient for cataract extraction, assuming that the patient is a surgical candidate, because first eye cataract surgery decreases falls.13,14
In our experience, most high-risk patients are amenable to decreasing medication dosages and appreciate having their physician reduce the number of prescription medications. Most older adults are willing to consider balance training, especially if the instructions are not complicated and the exercises can be done at home.36 A referral from a health care provider, particularly a physician, encourages follow-through with environmental assessment and modifications.8
Address fall injury risk
To reduce the chances of a fall injury, optimize bone health by recommending calcium and vitamin D supplementation and evaluating and treating osteoporosis.15 Strengthening lower extremity muscles and teaching older adults how to get up from the ground after a fall may prevent a so-called long lie (remaining on the ground involuntarily because of inability to get up without help) with its associated medical complications. 37 High-risk patients should carry a cellular phone or wear a personal medical alert device to reduce the risk of a long lie in the event of a fall.
Involve relevant professional disciplines
Physical therapists
PTs assess and treat balance, strength, and gait deficits. Table 3 lists several tests that are typically done by PTs as part of a comprehensive gait and balance assessment.
Table 3.
Tests for evaluation of gait and balance in people at risk of falls
| Test | Purpose |
|---|---|
| Dynamic Gait Index43 | Gait with head turns, speed changes, and pivot turns; stepping over and around obstacles; chair-climbing |
| TUG Cognitive24 | Gait with divided attention |
| Berg Balance Scale44 | Balance with sitting, standing, transferring, reaching, and turning |
| Functional Reach45 | Postural stability |
| Four Square Step Test46 | Dynamic balance |
PTs can design an exercise program to reduce fall risk that takes into consideration an individual’s goals and functional abilities. The exercise program should be individually tailored to challenge balance. It may include static and dynamic activities as well as functional balance activities (eg, dual attention tasks, reaching and turning, weight shifting).
PTs work with older adults to improve their balance and mobility to the point where they can safely participate in a home or community exercise program. A PCP should initially refer a patient to a PT for a 3-month period of fall prevention exercise training. However, continued therapy beyond 3 months is frequently necessary before patients can successfully transition to a community program.38
With a referral from the PCP, PTs can determine whether patients require a mobility aid. PTs select and fit an assistive device and teach patients how to use it correctly.
Occupational therapists
OTs assess the home environment and evaluate older adults’ capacities (eg, vision, cognition) and deficits in relation to functioning safely within their homes. OTs elicit a falls history, individuals’beliefsabout causes of falls, their understanding of environmental risks and perceived ability to negotiate those risks, and patterns of home use and community access.30 OTs help older adults change their behavior to prevent falls; for example, by helping them create new routines during daily activities and identifying adaptive behaviors (eg, scanning ahead for hazards when walking). Like outpatient PT services, outpatient OT services are a covered Medicare Part B benefit. If patients meet Medicare’s definition of homebound, they can receive home health services that can include a home safety evaluation by an OT under Medicare Part A.
Connect patients to evidence-based community fall prevention programs
Several effective fall prevention programs are becoming available in the community. For example, tai chi has been shown to reduce fall risk by 29%.14 Some YMCAs are offering the tai chi program, Y-Moving for Better Balance. Stepping On, a 7-week workshop that teaches strength and balance exercises and behavior changes to prevent falls,39 is also being disseminated (see https://wihealthyaging.org/stepping-on). Local public health departments and Area Agencies on Aging typically collaborate in community-level efforts to address falls.
Considerations for patients with dementia
Dementia impairs gait, balance, and hazard recognition. About half of community-dwelling older adults with dementia experience a fall every year.1 Few randomized intervention studies have included people with dementia, and so current evidence is insufficient to recommend for or against a particular fall prevention intervention.13 However, recent evidence suggests that the mobility and balance deficits seen in dementia may be improved through exercise.40
Working with the patient’s caregiver becomes important in addressing fall risk in patients with dementia.41 The caregiver can help by modifying the environment to improve safety and the way in which older adults with dementia perform mobility-related activities (eg, dressing, toileting, housekeeping) in and around the home. In some cases, it may be necessary to provide assistance with activities that the older adult can no longer safely perform. Their caregivers also may help older adults with dementia perform a set of basic exercises42 or consistently use an assistive device. An evaluation by an OT is critical and should include observing how the patient performs mobility-related tasks in the home.
Offer ongoing monitoring and follow-up
Reducing falls using the clinical approach described herein requires ongoing monitoring by the providers.35 Providers’ active involvement can help ensure that patients act on recommendations. Providers can receive reimbursement for providing medically necessary fall-related services by using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code R29.6 for repeated falls.
For high-risk patients with multiple modifiable risk factors, it may be necessary to address each risk factor individually over time so as not to confuse or overwhelm the patient. These patients typically have multiple health issues and may see several specialists, all of whom make suggestions, adjust medications, and schedule the patient for follow-up visits.
A PCP managing a high-risk patient may complete assessments and recommend interventions over a 3-month period,19 or longer if intercurrent health problems interfere. In this case, reassess the patient and recommend interventions at 4 to 6 months and as part of routine follow-up visits thereafter. Follow-up by other providers, (eg, nurse, PT, or OT) can augment the PCP’s care.
Resources for clinical practice
Several resources can facilitate integrating fall prevention into practice (Table 4).
Table 4.
Resources for health care providers
| Source | Item | Location |
|---|---|---|
| American Geriatrics Society |
Clinical practice guideline on fall prevention |
http://www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/prevention_of_falls_summary_of_recommendations |
| CDC | STEADI tool kit | www.cdc.gov/injury/steadi |
| Centers for Medicare and Medicaid Services |
Welcome to Medicare (Initial Preventive Physical Examination) visit |
www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/MPS_QRI_IPPE001a.pdf |
| Centers for Medicare and Medicaid Services |
Annual Wellness visit | www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/AWV_Chart_ICN905706.pdf |
| National Council on Aging |
Fact sheets about Medicare coverage for fall-related clinical services |
www.ncoa.org/improve-health/falls-prevention |
| National Institute on Aging |
Go4Life exercise DVD and manual |
http://go4life.nia.nih.gov |
SUMMARY
Falls and their associated injuries are common and usually result from interactions among multiple fall risk factors, many of which may be modifiable. PCPs play a critical role in reducing fall risk factors among their older patients. Guidelines recommend annual screening to identify patients at increased risk of falling and comprehensive risk assessment and management of modifiable fall risk factors for high-risk patients. Regular exercise that improves strength and balance, along with vitamin D supplementation, can reduce falls and are appropriate prevention strategies even for low-risk patients. Understanding older adults’ perspective and how to facilitate their involvement in fall prevention activities is critical to the success of provider efforts in this area.
KEY POINTS.
Falls are common and have adverse consequences, but are often preventable.
Current guidelines specify that primary care providers should screen older adults for falls and risk for falling at least once a year by asking about falls and unsteadiness when walking.
Multifactorial interventions that address many predisposing factors are appropriate for people at high risk and can decrease falls by approximately 25%.
Three key risk factors (balance, medications, and home safety) should be addressed in everyone at high risk.
Primary care providers should refer patients to clinical and community resources to address modifiable risk factors.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 2.King MB, Tinetti ME. Falls in community-dwelling older persons. J Am Geriatr Soc. 1995;43:1146–1154. doi: 10.1111/j.1532-5415.1995.tb07017.x. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Doucette J, Claus E, et al. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43:1214–1221. doi: 10.1111/j.1532-5415.1995.tb07396.x. [DOI] [PubMed] [Google Scholar]
- 4.Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001–2003. Vol. 392. Hyattsville, MD: National Center for Health Statistics Advance data from vital and health statistics; 2007. [PubMed] [Google Scholar]
- 5.Stevens JA, Corso PS, Finkelstein EA, et al. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan Med Bull. 1987;34:1–24. [PubMed] [Google Scholar]
- 7.Scheffer AC, Schuurmans MJ, van Dijk N, et al. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37:19–24. doi: 10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- 8.Bunn F, Dickinson A, Barnett-Page E, et al. A systematic review of older people’s perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing Soc. 2008;28:449–472. [Google Scholar]
- 9.Yardley L, Bishop FL, Beyer N, et al. Older people’s views of falls-prevention interventions in six European countries. Gerontologist. 2006;46:650–660. doi: 10.1093/geront/46.5.650. [DOI] [PubMed] [Google Scholar]
- 10.Boyd R, Stevens JA. Falls and fear of falling: burden, beliefs and behaviours. Age Ageing. 2009;38:423–428. doi: 10.1093/ageing/afp053. [DOI] [PubMed] [Google Scholar]
- 11.Calhoun R, Meischke H, Hammerback K, et al. Older adults’ perceptions of clinical fall prevention programs: a qualitative study. J Aging Res. 2011;2011:867341. doi: 10.4061/2011/867341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevens JA, Ballesteros MF, Mack KA, et al. Gender differences in seeking care for falls in the aged Medicare population. Am J Prev Med. 2012;43:59–62. doi: 10.1016/j.amepre.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Panel on Prevention of Falls in Older Persons. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 14.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;(9):CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moyer VA. Prevention of falls in community-dwelling older adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:197–204. doi: 10.7326/0003-4819-157-3-201208070-00462. [DOI] [PubMed] [Google Scholar]
- 16.Stevens JA, Phelan EA. Development of STEADI: a fall prevention resource for health care providers. Health Promot Pract. 2013;14:706–714. doi: 10.1177/1524839912463576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Geriatrics Society Workgroup on Vitamin D Supplementation for Older Adults. Recommendations abstracted from the American Geriatrics Society Consensus Statement on vitamin D for Prevention of Falls and Their Consequences. J Am Geriatr Soc. 2014;62:147–152. doi: 10.1111/jgs.12631. [DOI] [PubMed] [Google Scholar]
- 18.Richardson DA, Bexton RS, Shaw FE, et al. Prevalence of cardioinhibitory carotid sinus hypersensitivity in patients 50 years or over presenting to the accident and emergency department with “unexplained” or “recurrent” falls. Pacing Clin Electrophysiol. 1997;20:820–823. doi: 10.1111/j.1540-8159.1997.tb03912.x. [DOI] [PubMed] [Google Scholar]
- 19.Chang JT, Ganz DA. Quality indicators for falls and mobility problems in vulnerable elders. J Am Geriatr Soc. 2007;55(Suppl 2):S327–S334. doi: 10.1111/j.1532-5415.2007.01339.x. [DOI] [PubMed] [Google Scholar]
- 20.Ganz DA, Bao Y, Shekelle PG, et al. Will my patient fall? JAMA. 2007;297:77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 21.Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 22.Tinetti ME, Baker DI, McAvay G, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331:821–827. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- 23.Poon IO, Braun U. High prevalence of orthostatic hypotension and its correlation with potentially causative medications among elderly veterans. J Clin Pharm Ther. 2005;30:173–178. doi: 10.1111/j.1365-2710.2005.00629.x. [DOI] [PubMed] [Google Scholar]
- 24.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 25.Rossiter-Fornoff JE, Wolf SL, Wolfson LI, et al. A cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Gerontol A Biol Sci Med Sci. 1995;50:M291–M297. doi: 10.1093/gerona/50a.6.m291. [DOI] [PubMed] [Google Scholar]
- 26.Vellas BJ, Wayne SJ, Romero L, et al. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45:735–738. doi: 10.1111/j.1532-5415.1997.tb01479.x. [DOI] [PubMed] [Google Scholar]
- 27.Borson S, Scanlan JM, Chen P, et al. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51:1451–1454. doi: 10.1046/j.1532-5415.2003.51465.x. [DOI] [PubMed] [Google Scholar]
- 28.Speechley M, Tinetti M. Falls and injuries in frail and vigorous community elderly persons. J Am Geriatr Soc. 1991;39:46–52. doi: 10.1111/j.1532-5415.1991.tb05905.x. [DOI] [PubMed] [Google Scholar]
- 29.Tinetti ME. Preventing falls in elderly persons. N Engl J Med. 2003;348:42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 30.Peterson EW, Clemson L. Understanding the role of occupational therapy in fall prevention for community-dwelling older adults. OT Practice. 2008;13:CE1–CE8. [Google Scholar]
- 31.Merom D, Pye V, Macniven R, et al. Prevalence and correlates of participation in fall prevention exercise/physical activity by older adults. Prev Med. 2012;55:613–617. doi: 10.1016/j.ypmed.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Sherrington C, Whitney JC, Lord SR, et al. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56:2234–2243. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 33.Campbell AJ, Robertson MC, Gardner MM, et al. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–1069. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li F, Harmer P, Fisher KJ, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60:187–194. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 35.Tinetti ME, Kumar C. The patient who falls: “It’s always a trade-off”. JAMA. 2010;303:258–266. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yardley L, Kirby S, Ben-Shlomo Y, et al. How likely are older people to take up different falls prevention activities? Prev Med. 2008;47:554–558. doi: 10.1016/j.ypmed.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 37.Mallinson WJ, Green MF. Covert muscle injury in aged patients admitted to hospital following falls. Age Ageing. 1985;14:174–178. doi: 10.1093/ageing/14.3.174. [DOI] [PubMed] [Google Scholar]
- 38.Shubert TE. Evidence-based exercise prescription for balance and falls prevention: a current review of the literature. J Geriatr Phys Ther. 2011;34:100–108. doi: 10.1519/JPT.0b013e31822938ac. [DOI] [PubMed] [Google Scholar]
- 39.Clemson L, Cumming RG, Kendig H, et al. The effectiveness of a community-based program for reducing the incidence of falls in the elderly: a randomized trial. J Am Geriatr Soc. 2004;52:1487–1494. doi: 10.1111/j.1532-5415.2004.52411.x. [DOI] [PubMed] [Google Scholar]
- 40.Suttanon P, Hill K, Said C. Can balance exercise programme improve balance and related physical performance measures in people with dementia? A systematic review. Eur Rev Aging Phys Act. 2010;7:13–25. [Google Scholar]
- 41.Mahoney JE, Shea TA, Przybelski R, et al. Kenosha County Falls Prevention Study: a randomized, controlled trial of an intermediate-intensity, community-based multifactorial falls intervention. J Am Geriatr Soc. 2007;55:489–498. doi: 10.1111/j.1532-5415.2007.01144.x. [DOI] [PubMed] [Google Scholar]
- 42.Logsdon RG, McCurry SM, Teri L. A home health care approach to exercise for persons with Alzheimer’s disease. Care Manag J. 2005;6:90–97. doi: 10.1891/cmaj.6.2.90. [DOI] [PubMed] [Google Scholar]
- 43.VanSwearingen JM, Paschal KA, Bonino P, et al. Assessing recurrent fall risk of community-dwelling, frail older veterans using specific tests of mobility and the physical performance test of function. J Gerontol A Biol Sci Med Sci. 1998;53:M457–M464. doi: 10.1093/gerona/53a.6.m457. [DOI] [PubMed] [Google Scholar]
- 44.Berg KO, Wood-Dauphinee SL, Williams JI, et al. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(Suppl 2):S7–S11. [PubMed] [Google Scholar]
- 45.Duncan PW, Weiner DK, Chandler J, et al. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45:M192–M197. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- 46.Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil. 2002;83:1566–1571. doi: 10.1053/apmr.2002.35469. [DOI] [PubMed] [Google Scholar]