This study compares the average degree of spinal instability between patients with spinal metastases referred for surgery or for radiotherapy and evaluate whether this difference changed after introduction of the Spinal Instability Neoplastic Score (SINS) in clinical practice. The introduction of SINS led to a decrease in SINSs for both groups, suggesting that using SINS in metastatic spinal disease increases awareness for instability, resulting in earlier referrals for surgical intervention.
Keywords: Spinal metastases, Cancer, Spine, Spinal neoplasms, Radiation oncology, Instability
Abstract
Background.
Stable spinal metastases are effectively treated with radiotherapy, whereas unstable spinal metastases often need surgical fixation followed by radiotherapy for local control. The Spinal Instability Neoplastic Score (SINS) was developed as a tool to assess spinal neoplastic related instability with the goal of helping to guide referrals among oncology specialists. We compare the average degree of spinal instability between patients with spinal metastases referred for surgery or for radiotherapy and evaluate whether this difference changed after introduction of the SINS in clinical practice.
Methods.
All patients with spinal metastases treated with palliative surgery or radiotherapy in the period 2009–2013 were identified in two spine centers. For all patients, the SINS was scored on pretreatment imaging. The SINS before and after introduction of the SINS in 2011 were compared within the surgical and radiotherapy group. Furthermore, the overall SINS was compared between the two groups.
Results.
The overall SINS was significantly higher in the surgical group, with a mean SINS of 10.7 (median 11) versus 7.2 (median 8) for the radiotherapy group. The mean SINS decreased significantly for both groups after introduction of the SINS in clinical practice from 11.2 to 10.3 in the surgical group and from 8.4 to 7.2 in the radiotherapy group.
Conclusion.
The SINS differed significantly between patients treated with surgery or radiotherapy. The introduction of SINS led to a decrease in SINS score for both groups, suggesting that using SINS in metastatic spinal disease increases awareness for instability and may subsequently result in earlier referrals for surgical intervention.
Implications for Practice:
Spinal metastases can present with varying degrees of mechanical instability. Because unstable spinal metastases may respond insufficiently to palliative radiotherapy and can lead to loss of ambulation, timely detection and appropriate referral are important. The Spinal Instability Neoplastic Score (SINS) may help physicians caring for patients with metastasized disease to identify spinal instability before the onset of neurological deficits. In this study, it was shown that the introduction of SINS in routine practice led to a decrease in spinal instability in radiotherapy and surgical cohorts. The use of SINS may increase awareness of instability and subsequently result in earlier referrals.
Introduction
The skeleton is the most common site of metastases in advanced cancer, with the spine being the most frequent location [1]. The median survival time of patients with bone metastases has substantially improved over the last decades, mostly because of advances in oncological treatment options [2]. Bone metastases greatly increase the risk of skeletal-related events, which have a substantial negative impact on quality of life and daily functioning [3, 4]. Because the presence of spinal metastases represents advanced cancer, the goal of treatment shifts from long-term survival to preservation of quality of life for the remaining lifetime by retaining function and relieving symptoms [2].
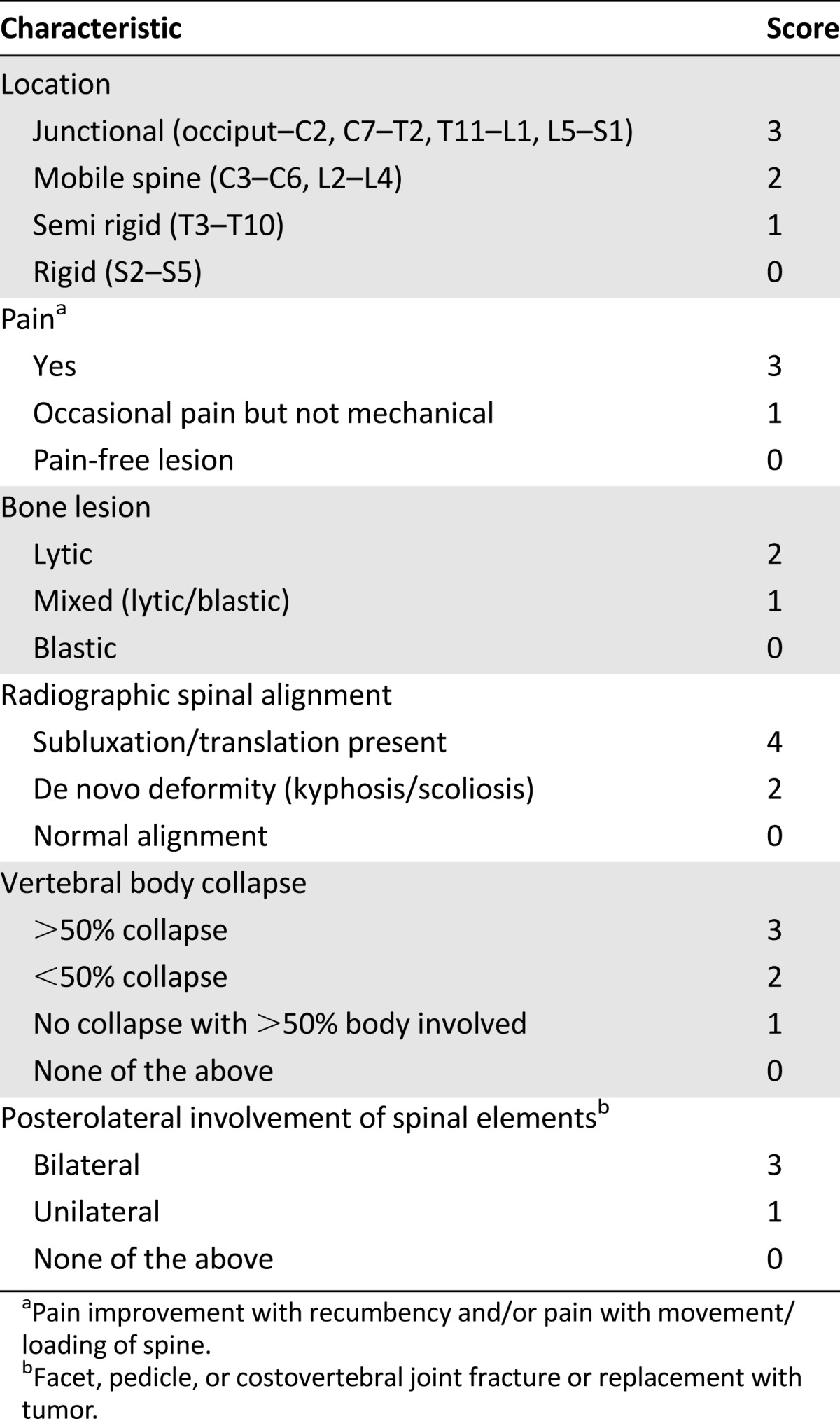
External beam radiotherapy has been the cornerstone of palliative treatment for painful spinal metastases and has been reported to be effective in 50%–80% of patients [5]. For more complex cases, such as patients with spinal cord compression, neurological deficits, and/or spinal mechanical instability, medical oncologists, radiation oncologists, and spinal surgeons need to collaborate to provide the best supportive care possible [6]. Neurological deficits and spinal cord compression are relatively easy to assess with physical/neurological examination and appropriate imaging. In contrast, evaluating spinal instability is more demanding, especially for nonspine surgeons, yet it is important because spinal instability increases the risk for neurological compromise and persisting disabling pain [7]. Considering the potential prognostic implications, spinal instability should be suspected in every patient with a proven malignancy and spinal complaints. To help direct referrals to a radiation oncologist or spine surgeon, the Spine Oncology Study Group (SOSG) developed the Spinal Instability Neoplastic Score (SINS) in 2010 to assess the degree of spinal (in)stability caused by metastatic disease [7]. The score consists of the sum of 5 radiographical and 1 clinical parameter, resulting in a total (summed) score between 0 and 18 points (Table 1) [7]. The total score is divided in three categories of spinal stability: stable (0–6 points), impending/potentially unstable (7–12 points), and unstable (13–18 points) [7]. The SINS does not provide a treatment recommendation, but consultation of a spinal surgeon is currently advised for SINS scores equal to or greater than 7 points [7]. The SINS has undergone extensive reliability testing among different oncology specialists and radiologists, reflecting the multidisciplinary aspect of care for cancer patients [8–10]. Excellent agreement was found between radiation oncologists, radiologists, and spinal surgeons for the differentiation between stable and (impending) unstable cases [9, 10]. With the repeatability of the SINS confirmed to assess spinal instability, the next step would be to determine the influence of implementing the SINS in routine clinical practice for patients with spinal metastases. After the introduction and application of the SINS in clinical practice, a change in referral pattern should be expected, with a decrease in inappropriate and/or late referrals. Therefore the aim of this study was to compare the average degree of spinal instability in patients with spinal metastases referred for surgery or radiotherapy before and after introduction of the SINS in clinical practice.
Table 1.
SINS according to Fisher et al. [7]
Methods
An international retrospective review was performed of patients who underwent stabilizing surgery or radiotherapy for spinal metastases in two tertiary academic centers between January 2009 and December 2013. Both spine centers are tertiary referral centers specializing in spinal oncology. The time frame was chosen because the SINS was introduced in August 2011 in our institutions, resulting in an equal distribution of time before and after introduction of the SINS. The SINS was introduced among the oncologists and radiation oncologists through an instructional lecture and/or by providing pocket cards with SINS methodology for clinical use. Surgical referral was recommended for patients with a SINS of 7 or above. Indications for treatment of patients with spinal metastases were comparable for both spine centers. The study was approved by the institutional review board of both participating centers.
Study Population
Patients were included if they were diagnosed with spinal metastases, were treated with radiotherapy or surgery, and were neurologically minimally impaired or intact. Neurological status was classified according to the American Spinal Injury Association (ASIA) classification [11], with ASIA E representing normal neurological function and ASIA D without progressive neurological deficits being interpreted as minimally impaired neurological function. All surgical patients presented with symptoms warranting palliative surgical intervention including pathological fracture, intractable back pain, and impending deterioration of neurological status.
Surgical patients were included in both spine centers and compared with patients from a cohort of radiotherapy patients with spinal metastases who underwent palliative radiotherapy at the European center. Patients in the radiotherapy group that would never have been surgical candidates based on their limited prognosis (as reflected by their short follow-up time) were excluded. For this purpose, we required radiotherapy patients to have the same follow-up time as the surgical group or at least 12 months of follow-up. Because the number of patients treated with radiotherapy exceeded the number of surgically treated patients, a random sample of 160 patients was selected from the radiotherapy group to equal the number of surgically treated patients.
The exclusion criteria were the presence of a primary spinal tumor, intradural tumor, epidural metastasis without bony involvement, or progressive neurological impairment. Patients classified with progressive neurological impairment were excluded to eliminate neurological compromise as primary indication for treatment.
Outcomes
Demographic characteristics and clinical data were collected from medical charts. Governmental databases were accessed to retrieve information regarding vital statistics. The SINS was calculated for each patient using pretreatment computed tomography (CT) scans. Pretreatment CT scans were obtained using 16 detector row CT scanners or superior (Philips Medical Systems, Eindhoven, The Netherlands, http://www.medical.philips.com) for adequate visualization of the spinal column. All CT scans were reviewed using the same window and level settings: window level +300 Hounsfield units (HU) and window width +1,000 HU.
In case of multiple spinal metastases, the SINS was calculated for each lesion in the treatment area, and the lesion with the highest SINS was used for analysis. Information regarding the pain component was retrieved from the medical chart and was scored with identical criteria for both groups: 3 points whenever pain was continuously present and 1 point when pain was occasionally present or of nonmechanical origin [6]. The SINS was scored by one observer experienced in assessing spinal stability; in ambiguous cases, a spine surgeon with a special focus on spinal oncology was consulted for consensus on the final SINS. The observers were blinded for patient characteristics but not for treatment type.
Statistical Analysis
Patients treated with surgery or radiotherapy were compared for age, gender, primary tumor type, disease extent, pain symptoms, neurological status (ASIA score), total SINS (continuous score), and categorical SINS (stable, potentially unstable, unstable). In addition, the SINS scores before and after introduction of the SINS in routine clinical practice were compared within the two cohorts. The chi-square and Fisher exact tests were used for categorical variables and the independent sample t test for continuous variables. p < .05 defined statistical significance All statistical analyses were performed using SPSS 21.0 (IBM Corp., Armonk, NY, http://www-01.ibm.com/software/analytics/spss/).
Results
Patient Characteristics
A total of 1,509 patients were identified; 160 underwent stabilizing surgery and 1,349 received radiotherapy. From the radiotherapy cohort, 160 patients were randomly selected for analysis. Of the surgically treated patients, 84 were treated in Europe, and 76 were treated in North America. Surgical patients were younger (p = .002), had less often a primary breast, prostate, or lung tumor (p < .001), had a shorter time between diagnosis of spinal metastases and treatment (p = .013), and were more often classified as ASIA D (p < .001) compared with radiotherapy patients (Table 2).
Table 2.
Baseline characteristics
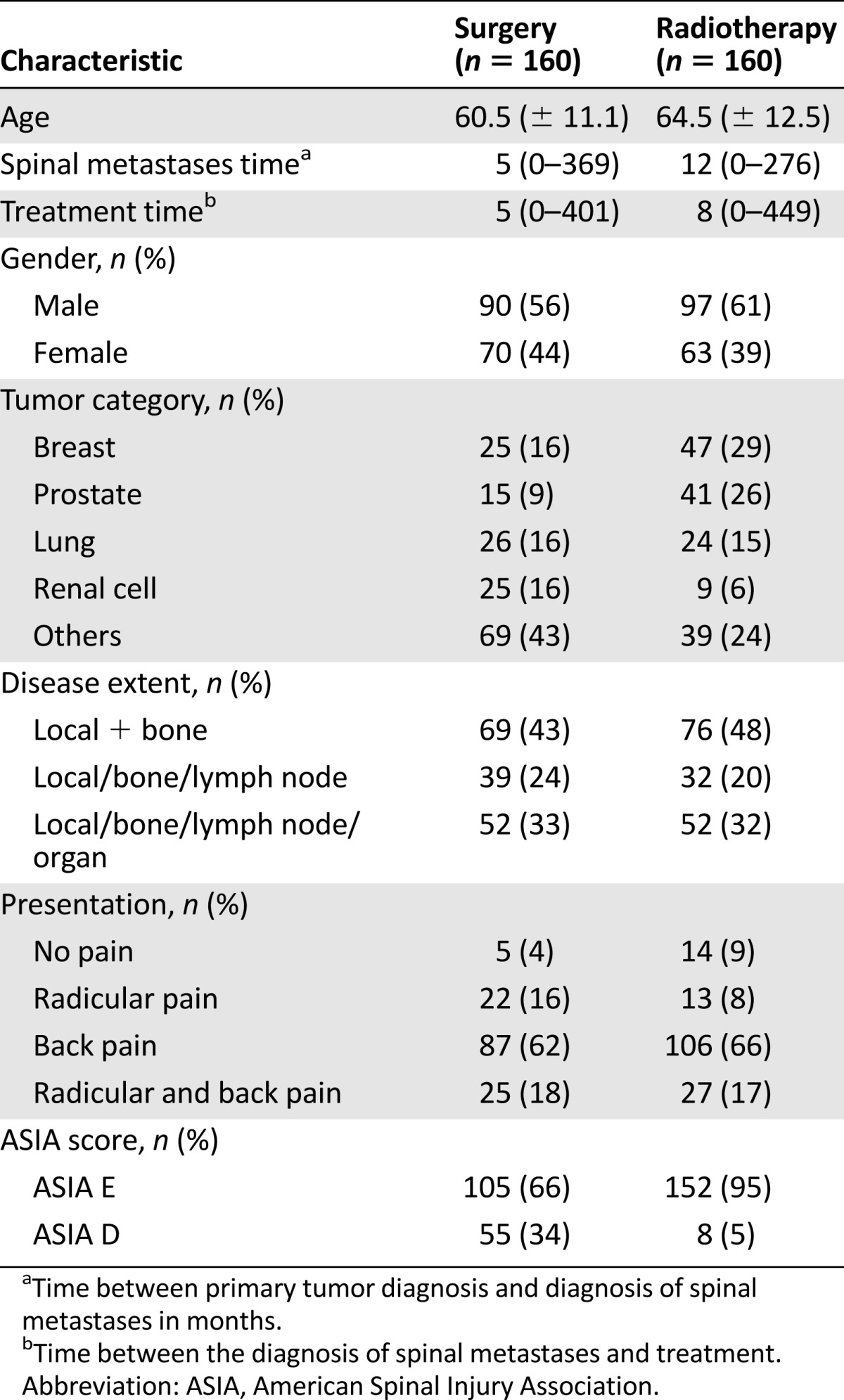
No significant differences in demographic characteristics were found between the surgical cohorts from the two spine centers. Breast, renal cell, lung, and prostate were the most common primary tumor types. Median follow-up time was 10 months (range 0–67) in the surgical cohort and 11 months (range 0–66) in the radiotherapy cohort. During follow-up, 210 (66%) of the patients died: 112 patients (70%) of the radiotherapy cohort and 98 patients (61%) of the surgical cohort.
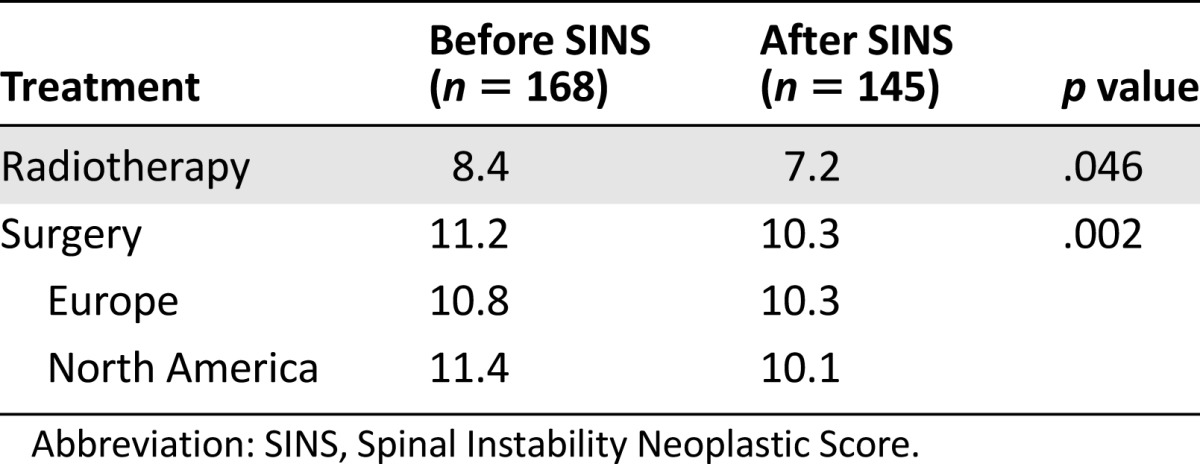
SINS
The majority of patients (73%) were treated for a lesion in the junctional or semirigid spine, and mechanical pain was present in 63% of the patients (Table 3). The mean SINS was significantly (p < .001) higher for the surgical patients (10.7; median 11; range 3–17) compared with those receiving radiotherapy (7.2; median 8; range 2–14). The mean SINS in both groups decreased significantly after introduction of the SINS in routine clinical practice, from 11.2 to 10.3 in the surgical group and from 8.4 to 7.2 in the radiotherapy group (Table 4).
Table 3.
Baseline SINS characteristics
Table 4.
Mean SINS scores before and after introduction of the SINS in clinical care
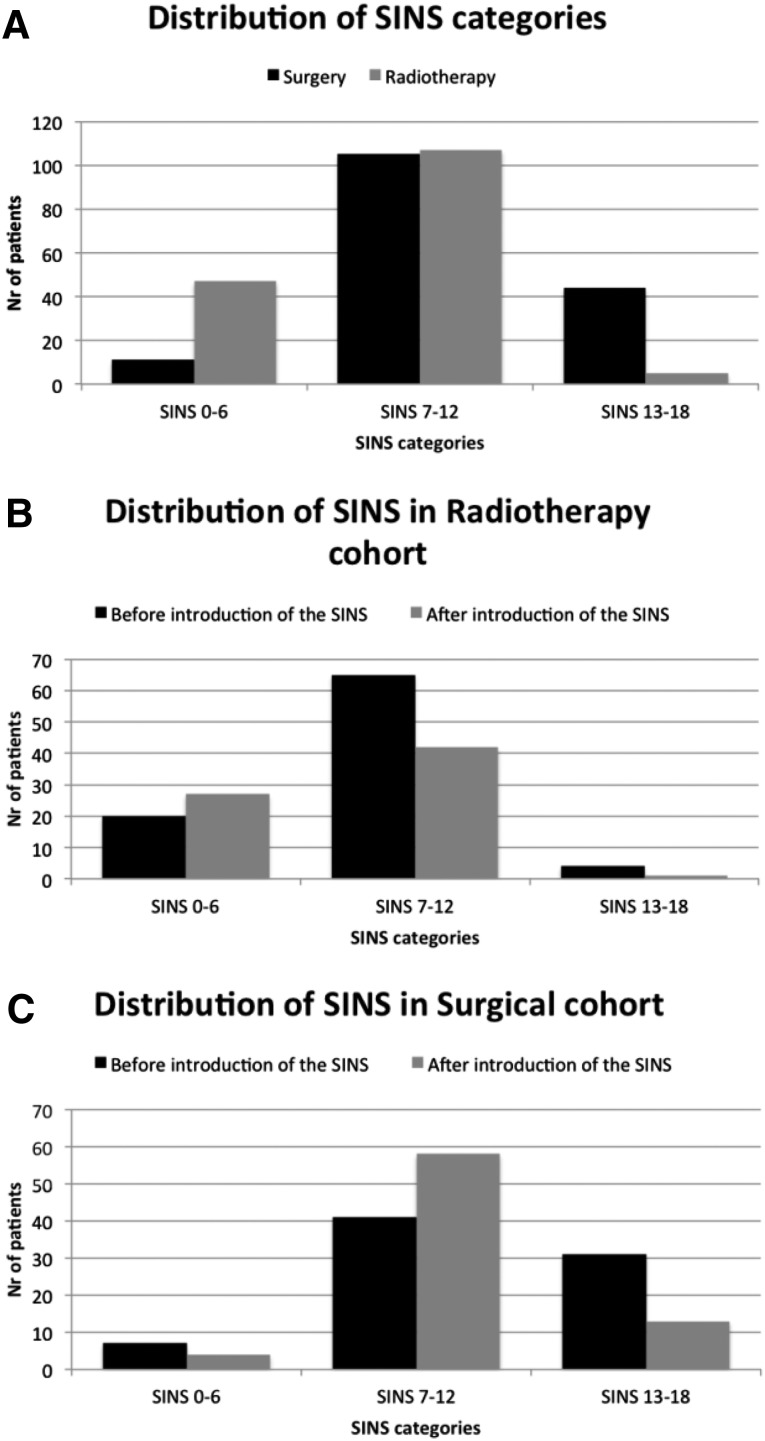
Evaluation of the SINS score by category of stability showed a significant (p < .001) difference between the surgical and radiotherapy group, with more unstable lesions (28%) in the surgical group than in the radiotherapy group (3%). Additionally, 107 (67%) of the radiotherapy patients and 105 (66%) of the surgical patients fell in the category of impending instability (7–12 points) (Fig. 1A).
Figure 1.
Distribution of SINS categories. (A): Distribution of SINS categories for surgical and radiotherapy cohort. (B): Distribution of SINS categories within radiotherapy cohort. (C): Distribution of SINS categories within surgery cohort.
Abbreviations: Nr, number; SINS, Spinal Instability Neoplastic Score.
Twenty (23%) patients treated with radiotherapy had a SINS below 7 before introduction of the SINS compared with 27 (39%) after introduction. Furthermore, 65 (73%) of the radiotherapy patients had a SINS between 7 and 12 before introduction, and 42 (60%) patients had a SINS between 7 and 12 after introduction of the SINS (Fig. 1B). In comparison, 31 (39%) of the surgically treated patients had a SINS above 12 before introduction and 13 (17%) after introduction of the SINS. Forty-one (52%) of the surgically treated patients were within the category of impending instability before introduction and 57 (77%) after introduction of the SINS (Fig. 1C).
Eleven (7%) of the surgically treated patients were in the stable category comprising 1 patient with a SINS of 3, 1 patient with a SINS of 4, and 9 patients with a SINS of 6. The 2 patients with a SINS score of 3 and 4 points were operated to avoid further neurological compromise but were without progressive neurological deficits at the time of consultation. The 9 patients with a SINS score of 6 consisted of 6 patients with minimal neurological impairment (ASIA D) but no signs of progressive neurological deficits; 5 patients had lesions in the thoracolumbar or lumbosacral junction, combined with the presence of mechanical pain; or occasional pain and a lytic lesion. The remaining 4 patients had a lesion in the semirigid region, occasional pain, vertebral body collapse, and unilateral involvement of the posterior elements.
Discussion
This study demonstrated a significant decrease in mean and median SINS in both the surgical and radiotherapy groups after introduction of the SINS in routine clinical practice. In addition, a significant difference in overall mean, median, and categorical SINS between the surgical and radiotherapy cohort was found. The decrease in SINS may be explained by increased awareness of neoplastic-related spinal instability and earlier and more appropriate referral to the spine surgeon after introduction of the SINS in clinical practice. The SINS classification system was developed to classify spinal instability caused by metastatic disease and to provide a tool to guide referrals among the different specialists involved in the care of cancer patients. Evaluation of the SINS has until now been limited to reliability and validity testing on selected case series [8–10, 12, 13]. This study is the first to determine the influence of the SINS in a clinical setting with a substantial number of patients.
At baseline, significant differences were found between the surgical and radiotherapy cohorts for age at time of treatment, primary tumor type, time between the diagnosis of spinal metastases and treatment, and neurological status. Although breast, prostate, lung, and renal cell carcinoma represented more than 50% of the primary tumors in both the surgical and radiotherapy cohort, the surgical cohort contained significantly more (46%) “other” primary tumor types compared with the radiotherapy cohort. This may be explained by aggressiveness of other tumor types warranting earlier surgical intervention in patients still fit for surgery. In addition, the neurological status differed significantly between the two cohorts, with the surgical cohort containing more patients classified as ASIA D. This may be explained by the choice for a more aggressive (surgical) approach, in case a patient presents with the combination of (impending) spinal instability and minimal nonprogressive neurological deficits. Furthermore, radiation oncologists refer patients with neurological deficits in an earlier stage for surgical evaluation, because neurological compromise is one of the key indications for surgical intervention [14].
The decrease in mean SINS scores in both groups after introduction of the SINS may be explained by the reverse of the “Will-Rogers phenomenon” [15], an apparent epidemiological paradox named after comedian Will Rogers based on his quotation: “When the Oakies left Oklahoma and moved to California, they raised the average intelligence level in both states” [15]. This term has been used to describe stage migration in cancer patients, a change in diagnostic criteria, or the improved sensitivity of diagnostic techniques to stage cancer results in the migration of patients with a better prognosis into a stage of patients with a worse prognosis, resulting in improved survival rates for both groups [15]. Similarly, in our study patients with the highest SINS scores in the radiotherapy cohort, yet still in the lower range of spinal instability, shifted from the radiotherapy group to the surgical group, resulting in decreased mean SINS scores in both cohorts. More patients with a score of impending spinal instability and an indication for surgical stabilization were operated. Minimally invasive procedures can effectively be used to treat impending instability, whereas gross spinal instability requires extensive open surgery, which is less desirable in this fragile patient category. Increased awareness of (impending) spinal instability and earlier and more appropriate referral by different oncology specialists after the introduction of the SINS in clinical practice may account for these changes.
Considering the three different categories of spinal stability, it is known that most stable spinal metastases can effectively be treated with radiation therapy and that gross spinal instability is best treated with surgical stabilization provided the patient is fit for surgery [5, 8]. However, it is unknown what the optimal treatment is for patients with impending spinal instability. This is reflected by the large number of patients with impending instability in both the radiotherapy (66%) and surgical cohorts (67%). Although radiotherapy is effective in 50%–80% of the patients, a substantial number of patients do not gain any pain relief [16, 17]. It is not completely understood why some patients respond to radiotherapy and others do not. The current authors hypothesize that “metastatic bone pain, if predominantly caused by mechanical instability of the spine responds less well to radiotherapy than metastatic bone pain caused by local tumor activity” [18]. This was confirmed by a study from Huisman et al. [18] demonstrating a relationship between the risk on radiotherapy failure and a higher SINS; every point increase in SINS increased the risk of radiotherapy failure with 30%. Patients with a high SINS should therefore not be subjected to radiotherapy before consultation of a spine surgeon to reduce the risk of radiotherapy failure and having to perform surgery after irradiation with its inherent risks around wound healing. However, this was a retrospective study with radiotherapy failure defined as the need for retreatment on the index site rather than using international consensus guidelines for radiotherapy response.
The SOSG recommends consultation of a spine surgeon for all patients with a SINS of 7 or greater [7]. In view of the increased burden of extra hospital visits for cancer patients to consult a spine surgeon and the fact that more than 60% of the patients in the radiotherapy cohort have a SINS score above 7, increasing the threshold of the SINS may be considered before recommending surgical consultation. Furthermore, considering the limited resources and increasing costs of health care [19, 20], it may be useful to increase the threshold of the SINS to limit the number of inappropriate referrals. To find the optimal cut-off value, a step-wedge study design using different cut-off values in different centers should be performed.
Although this study demonstrated a significant difference in spinal stability between the surgical and radiotherapy groups and within the individual groups before and after introduction of the SINS, some study limitations can be identified. First, because of the retrospective nature of the study, scoring of the pain component is less reliable. According to the SOSG, spinal instability is strongly related to the presence of mechanical pain as defined by presence of movement-related pain improving with recumbency [7]. Scoring of the pain component was done with identical criteria in the radiotherapy and surgery cohort to score the pain component uniformly. Any over- or underestimation would therefore be equal in both groups. However, this may have influenced the overall SINS scores for both groups to some extent. Second, the observer was not blinded for the treatment strategy of the patients, which could have biased scoring of the SINS. Furthermore, the SINS was scored by one rater. However, previous testing of the reliability of the SINS has demonstrated excellent inter- and intraobserver reliability to distinguish between the three different categories of spinal instability [8], and the judgment of one observer experienced with the SINS methodology was therefore deemed sufficient. Moreover, a spine surgeon was consulted in ambiguous cases to reach consensus.
Conclusion
This is the first study to evaluate the effect of the introduction of the SINS in clinical practice. The SINS was developed to evaluate the degree of spinal instability, improve communication, and facilitate appropriate referrals among spine oncology specialists. Treatment of patients with spinal metastases is multidisciplinary, and evaluation of spinal instability is only one of several factors that are taken into account. Our study demonstrated a significant decrease in mean SINS after the introduction of the SINS in clinical practice. This may be explained by increased awareness of spinal neoplastic related instability and earlier and more appropriate referral of patients to a spinal surgeon after introduction of the SINS. Future studies are needed to determine the optimal threshold to recommend surgical consultation to balance under- and over-referral, considering that most of the surgical and radiotherapy patients have a score of impending instability.
Footnotes
For Further Reading:Adam N. Wallace, Clifford G. Robinson, Jeffrey Meyer et al. The Metastatic Spine Disease Multidisciplinary Working Group Algorithms. The Oncologist 2015;20:1205–1215.
Implications for Practice:The Metastatic Spine Disease Multidisciplinary Working Group algorithms can facilitate interdisciplinary referrals by providing physicians with straightforward recommendations regarding available treatment options, including emerging modalities such as stereotactic body radiation therapy and percutaneous tumor ablation.
Author Contributions
Conception/Design: Anne L. Versteeg, Jorrit-Jan Verlaan
Provision of study material or patients: Anne L. Versteeg, Joanne M. van der Velden
Collection and/or assembly of data: Anne L. Versteeg
Data analysis and interpretation: Anne L. Versteeg, Joanne M. van der Velden, Helena M. Verkooijen, Marco van Vulpen, F. Cumhur Oner, Charles G. Fisher, Jorrit-Jan Verlaan
Manuscript writing: Anne L. Versteeg, Joanne M. van der Velden, Helena M. Verkooijen, Marco van Vulpen, F. Cumhur Oner, Charles G. Fisher, Jorrit-Jan Verlaan
Final approval of manuscript: Anne L. Versteeg, Joanne M. van der Velden, Helena M. Verkooijen, Marco van Vulpen, F. Cumhur Oner, Charles G. Fisher, Jorrit-Jan Verlaan
Disclosures
F. Cumhur Oner: DePuy-Synthes (RF); Charles G. Fisher: Medtronic, Nuvasive (C/A), OREF (RF), Medtronic (other). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res. 2006;12:6243s–6249s. doi: 10.1158/1078-0432.CCR-06-0931. [DOI] [PubMed] [Google Scholar]
- 2.Poon M, Zeng L, Zhang L, et al. Incidence of skeletal-related events over time from solid tumour bone metastases reported in randomised trials using bone-modifying agents. Clin Oncol (R Coll Radiol) 2013;25:435–444. doi: 10.1016/j.clon.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Henry DH, Costa L, Goldwasser F, et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol. 2011;29:1125–1132. doi: 10.1200/JCO.2010.31.3304. [DOI] [PubMed] [Google Scholar]
- 4.Weinfurt KP, Li Y, Castel LD, et al. The significance of skeletal-related events for the health-related quality of life of patients with metastatic prostate cancer. Ann Oncol. 2005;16:579–584. doi: 10.1093/annonc/mdi122. [DOI] [PubMed] [Google Scholar]
- 5.Lutz S, Berk L, Chang E, et al. Palliative radiotherapy for bone metastases: An ASTRO evidence-based guideline. J Radiat Oncol Biol Phys. 2011;79:965–976. doi: 10.1016/j.ijrobp.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 6.Laufer I, Rubin DG, Lis E, et al. The NOMS framework: Approach to the treatment of spinal metastatic tumors. The Oncologist. 2013;18:744–751. doi: 10.1634/theoncologist.2012-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher CG, DiPaola CP, Ryken TC, et al. A novel classification system for spinal instability in neoplastic disease: An evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine. 2010;35:E1221–E1229. doi: 10.1097/BRS.0b013e3181e16ae2. [DOI] [PubMed] [Google Scholar]
- 8.Fourney DR, Frangou EM, Ryken TC, et al. Spinal Instability Neoplastic Score: An analysis of reliability and validity from the spine oncology study group. J Clin Oncol. 2011;29:3072–3077. doi: 10.1200/JCO.2010.34.3897. [DOI] [PubMed] [Google Scholar]
- 9.Fisher CG, Versteeg AL, Schouten R, et al. Reliability of the spinal instability neoplastic scale among radiologists: An assessment of instability secondary to spinal metastases. AJR Am J Roentgenol. 2014;203:869–874. doi: 10.2214/AJR.13.12269. [DOI] [PubMed] [Google Scholar]
- 10.Fisher CG, Schouten R, Versteeg AL, et al. Reliability of the Spinal Instability Neoplastic Score (SINS) among radiation oncologists: An assessment of instability secondary to spinal metastases. Radiat Oncol. 2014;9:69. doi: 10.1186/1748-717X-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirshblum SC, Burns SP, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury (revised 2011) J Spinal Cord Med. 2011;34:535–546. doi: 10.1179/204577211X13207446293695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Campos M, Urrutia J, Zamora T, et al. The Spine Instability Neoplastic Score: An independent reliability and reproducibility analysis. Spine J. 2014;14:1466–1469. doi: 10.1016/j.spinee.2013.08.044. [DOI] [PubMed] [Google Scholar]
- 13.Teixeira WG, Coutinho PR, Marchese LD, et al. Interobserver agreement for the varies according to the experience of the evaluator. Clinics (Sao Paulo) 2013;68:213–218. doi: 10.6061/clinics/2013(02)OA15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: A randomised trial. Lancet. 2005;366:643–648. doi: 10.1016/S0140-6736(05)66954-1. [DOI] [PubMed] [Google Scholar]
- 15.Feinstein AR, Sosin DM, Wells CK. The Will Rogers phenomenon: Stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. N Engl J Med. 1985;312:1604–1608. doi: 10.1056/NEJM198506203122504. [DOI] [PubMed] [Google Scholar]
- 16.Sze WM, Shelley M, Held I, et al. Palliation of metastatic bone pain: Single fraction versus multifraction radiotherapy: A systematic review of the randomised trials. Cochrane Database Syst Rev. 2004;(2):CD004721. doi: 10.1002/14651858.CD004721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chow E, Zeng L, Salvo N, et al. Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol) 2012;24:112–124. doi: 10.1016/j.clon.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Huisman M, van der Velden JM, van Vulpen M, et al. Spinal instability as defined by the Spinal Instability Neoplastic Score is associated with radiotherapy failure in metastatic spinal disease. Spine J. 2014;14:2835–2840. doi: 10.1016/j.spinee.2014.03.043. [DOI] [PubMed] [Google Scholar]
- 19.Barlev A, Song X, Ivanov B, et al. Payer costs for inpatient treatment of pathologic fracture, surgery to bone, and spinal cord compression among patients with multiple myeloma or bone metastasis secondary to prostate or breast cancer. J Manag Care Pharm. 2010;16:693–702. doi: 10.18553/jmcp.2010.16.9.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hess G, Barlev A, Chung K, et al. Cost of palliative radiation to the bone for patients with bone metastases secondary to breast or prostate cancer. Radiat Oncol. 2012;7:168. doi: 10.1186/1748-717X-7-168. [DOI] [PMC free article] [PubMed] [Google Scholar]