Abstract
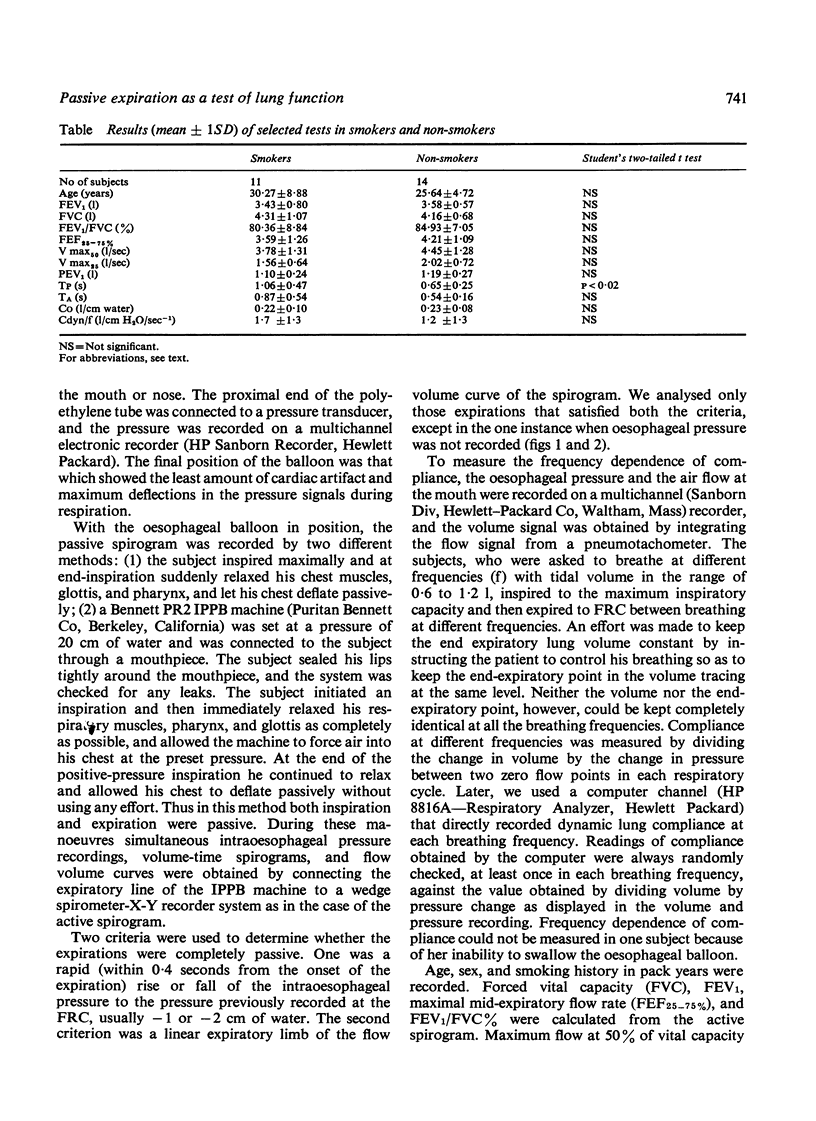
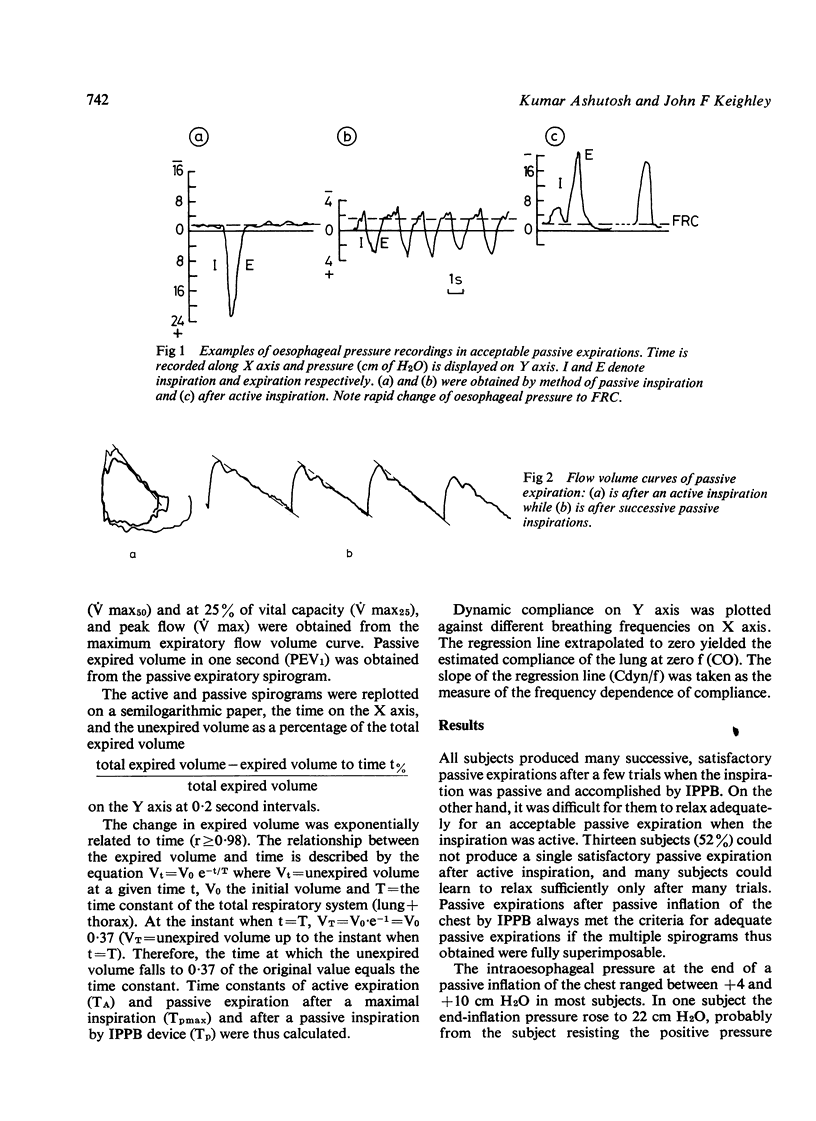
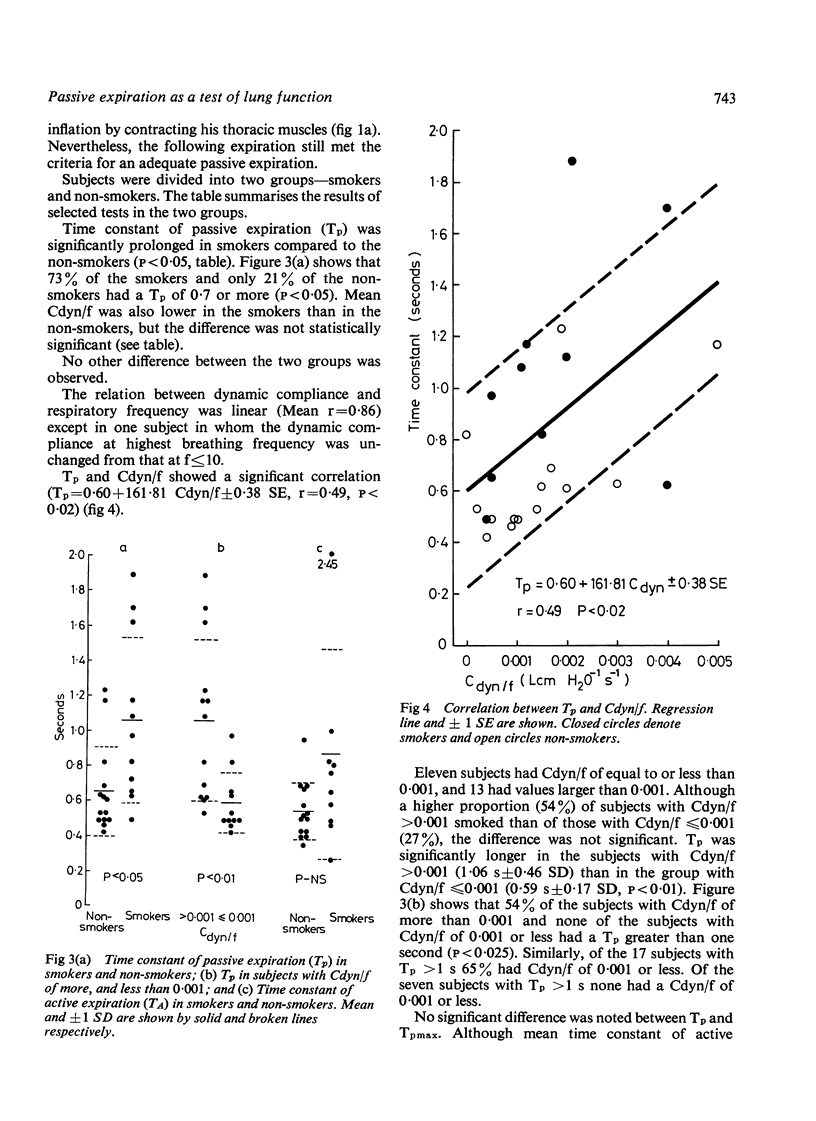
Twenty-five normal subjects, 14 non-smokers and 11 smokers, passively expired into a spirometer after a maximal active inspiration, and after a passive inflation of the chest by a pressure cycled intermittent positive-pressure breathing (IPPB) machine. Acceptable passive expirations could be performed by all subjects after a passive inspiration but by only 12 after an active inspiration. Expired volume was found to change exponentially with time (r greater than 0.98), and the time constant of passive expiration (Tp) was obtained. There was no significant difference between the smokers and non-smokers in age, sex, forced vital capacity, FEV1 FEV1/FVC%, maximum mid-expiratory flow rate, maximum expiratory flow at 50% and 25% of the vital capacity, or the magnitude of the fall in the dynamic compliance with increasing frequency of breathing (Cdyn/f). Tp in smokers (1.06 +/- 0.47 SD) was significantly longer than in the non-smokers (0.65 +/- 0.25 SD P less than 0.02). Tp had a significant correlation with Cdyn/f(Tp = 0.6 + 161.81 Cdyn/f +/- 0.38 SE, r = 0.49, P less than 0.02). We conclude that satisfactory passive expiratory spirograms can be easily obtained after a mechanically assisted passive inspiration. Tp thus obtained is determined by the intrinsic properties of the respiratory system (lung plus thorax), and is significantly prolonged in smokers compared with non-smokers when other studies of pulmonary function including frequency dependence of compliance are unchanged.
Full text
PDF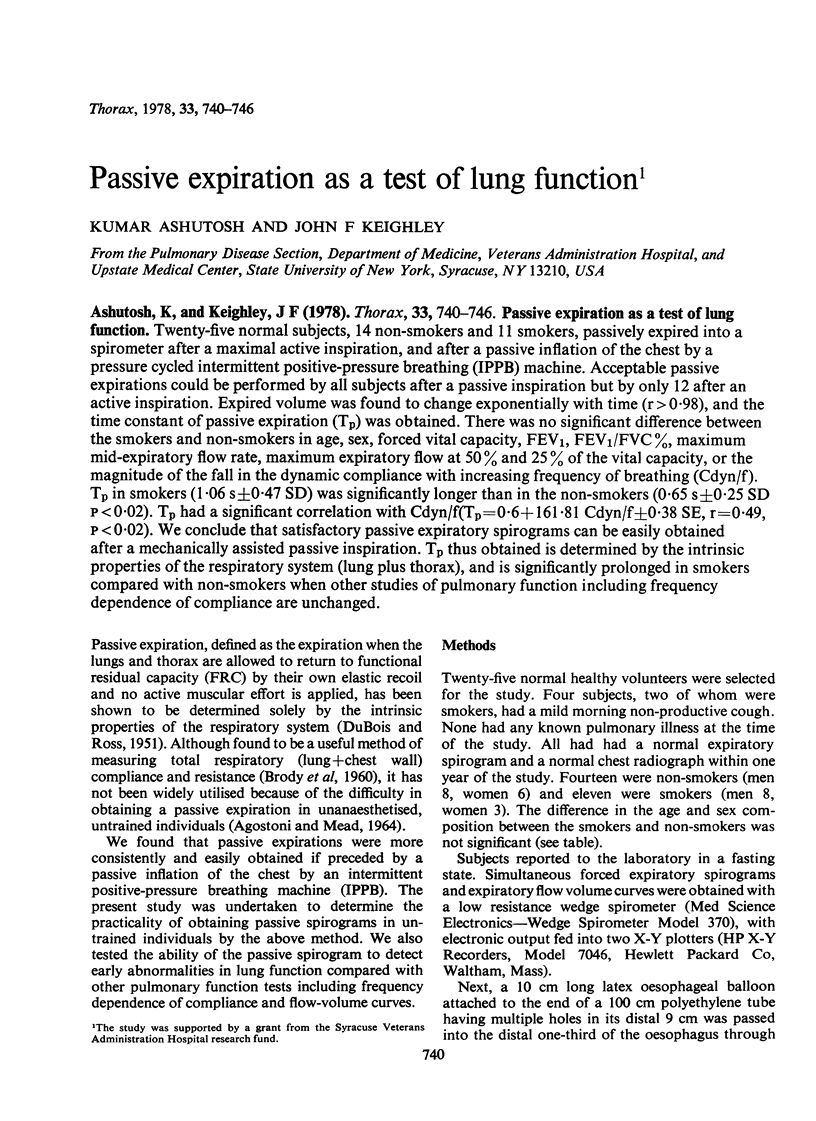
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BRODY A. W. Mechanical compliance and resistance of the lung-thorax calculated from the flow recorded during passive expiration. Am J Physiol. 1954 Aug;178(2):189–196. doi: 10.1152/ajplegacy.1954.178.2.189. [DOI] [PubMed] [Google Scholar]
- COMROE J. H., Jr, NISELL O. I., NIMS R. G. A simple method for concurrent measurement of compliance and resistance to breathing in anesthetized animals and man. J Appl Physiol. 1954 Sep;7(2):225–228. doi: 10.1152/jappl.1954.7.2.225. [DOI] [PubMed] [Google Scholar]
- DUBOIS A. B., ROSS B. B. A new method for studying mechanics of breathing using cathode ray oscillograph. Proc Soc Exp Biol Med. 1951 Nov;78(2):546–549. doi: 10.3181/00379727-78-19135. [DOI] [PubMed] [Google Scholar]
- Dixon W. E. Contributions to the physiology of the lungs: Part I. The bronchial muscles, their innervation, and the action of drugs upon them. J Physiol. 1903 Mar 16;29(2):97–173. doi: 10.1113/jphysiol.1903.sp000947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dosman J., Bode F., Urbanetti J., Martin R., Macklem P. T. The Use of a Helium-Oxygen Mixture during Maximum Expiratory Flow to Demonstrate Obstruction in Small Airways in Smokers. J Clin Invest. 1975 May;55(5):1090–1099. doi: 10.1172/JCI108010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt A. R., Siddorn J. A., Brash H. M., Flenley D. C. Reproducibility of dynamic compliance and flow-volume curves in normal man. J Appl Physiol. 1975 Sep;39(3):341–348. doi: 10.1152/jappl.1975.39.3.341. [DOI] [PubMed] [Google Scholar]
- Ingram R. H., Jr, O'Cain C. F. Frequency dependence of compliance in apparently healthy smokers versus non-smokers. Bull Physiopathol Respir (Nancy) 1971 Jan-Feb;7(1):195–212. [PubMed] [Google Scholar]
- Ingram R. H., Jr, Schilder D. P. Association of a decrease in dynamic compliance with a change in gas distribution. J Appl Physiol. 1967 Dec;23(6):911–916. doi: 10.1152/jappl.1967.23.6.911. [DOI] [PubMed] [Google Scholar]
- MILLS R. J., CUMMING G., HARRIS P. FREQUENCY-DEPENDENT COMPLIANCE AT DIFFERENT LEVELS OF INSPIRATION IN NORMAL ADULTS. J Appl Physiol. 1963 Nov;18:1061–1064. doi: 10.1152/jappl.1963.18.6.1061. [DOI] [PubMed] [Google Scholar]
- Marco M., Minette A. Lung function changes in smokers with normal conventional spirometry. Am Rev Respir Dis. 1976 Oct;114(4):723–738. doi: 10.1164/arrd.1976.114.4.723. [DOI] [PubMed] [Google Scholar]
- McFadden E. R., Jr, Kiker R., Holmes B., DeGroot W. J. Small airway disease. An assessment of the tests of peripheral airway function. Am J Med. 1974 Aug;57(2):171–182. doi: 10.1016/0002-9343(74)90441-0. [DOI] [PubMed] [Google Scholar]
- NEWMAN H. C., CAMPBELL E. J., DINNICK O. P. A simple method of measuring the compliance and the nonelastic resistance of the chest during anaesthesia. Br J Anaesth. 1959 Jul;31:282–289. doi: 10.1093/bja/31.7.282. [DOI] [PubMed] [Google Scholar]
- NISELL O. I., DUBOIS A. B. Relationship between compliance and FRC of the lungs in cats, and measurement of resistance to breathing. Am J Physiol. 1954 Aug;178(2):206–210. doi: 10.1152/ajplegacy.1954.178.2.206. [DOI] [PubMed] [Google Scholar]
- OTIS A. B., FENN W. O., RAHN H. Mechanics of breathing in man. J Appl Physiol. 1950 May;2(11):592–607. doi: 10.1152/jappl.1950.2.11.592. [DOI] [PubMed] [Google Scholar]
- PIERCE J. A. Studies of free collapse in the intact human lung. J Lab Clin Med. 1959 Jul;54(1):96–106. [PubMed] [Google Scholar]
- Saibene F., Mead J. Frequency dependence of pulmonary quasi-static hysteresis. J Appl Physiol. 1969 Jun;26(6):732–737. doi: 10.1152/jappl.1969.26.6.732. [DOI] [PubMed] [Google Scholar]
- Tockman M., Menkes H., Cohen B., Permutt S., Benjamin J., Ball W. C., Jr, Tonascia J. A comparison of pulmonary function in male smokers and nonsmokers. Am Rev Respir Dis. 1976 Oct;114(4):711–722. doi: 10.1164/arrd.1976.114.4.711. [DOI] [PubMed] [Google Scholar]
- Woolcock A. J., Vincent N. J., Macklem P. T. Frequency dependence of compliance as a test for obstruction in the small airways. J Clin Invest. 1969 Jun;48(6):1097–1106. doi: 10.1172/JCI106066. [DOI] [PMC free article] [PubMed] [Google Scholar]


