Abstract
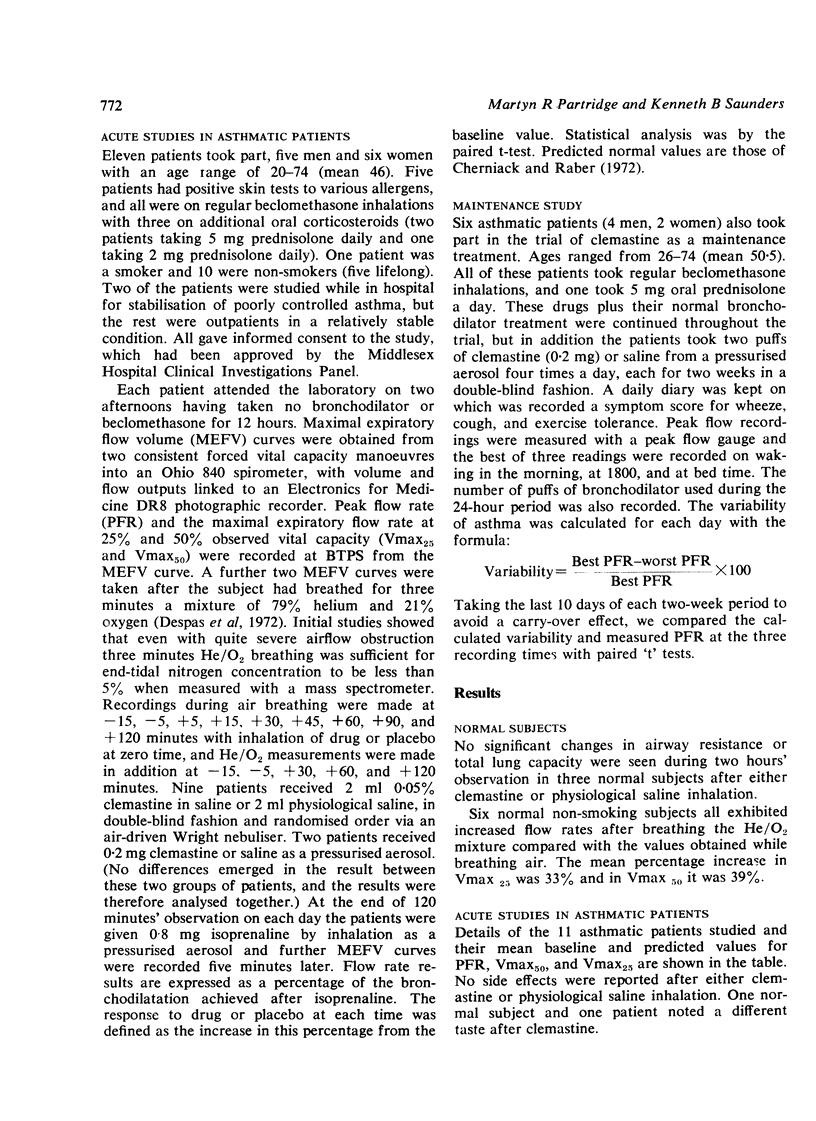
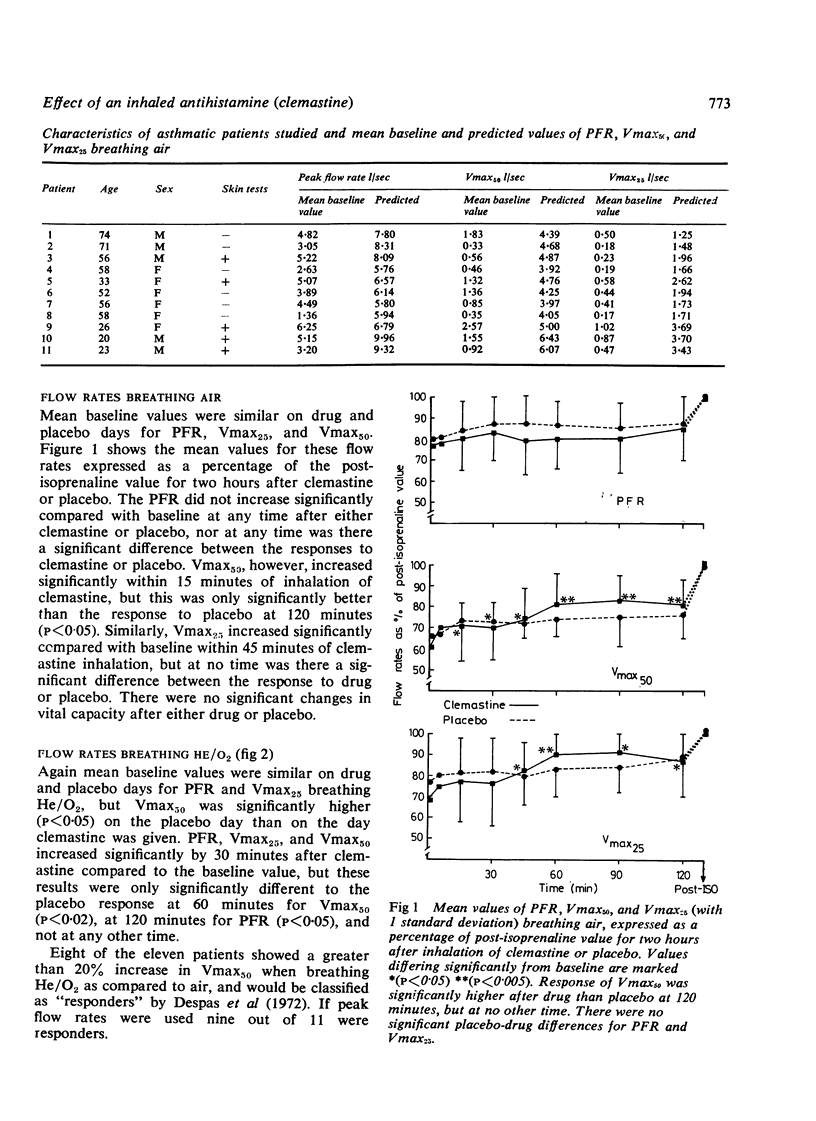
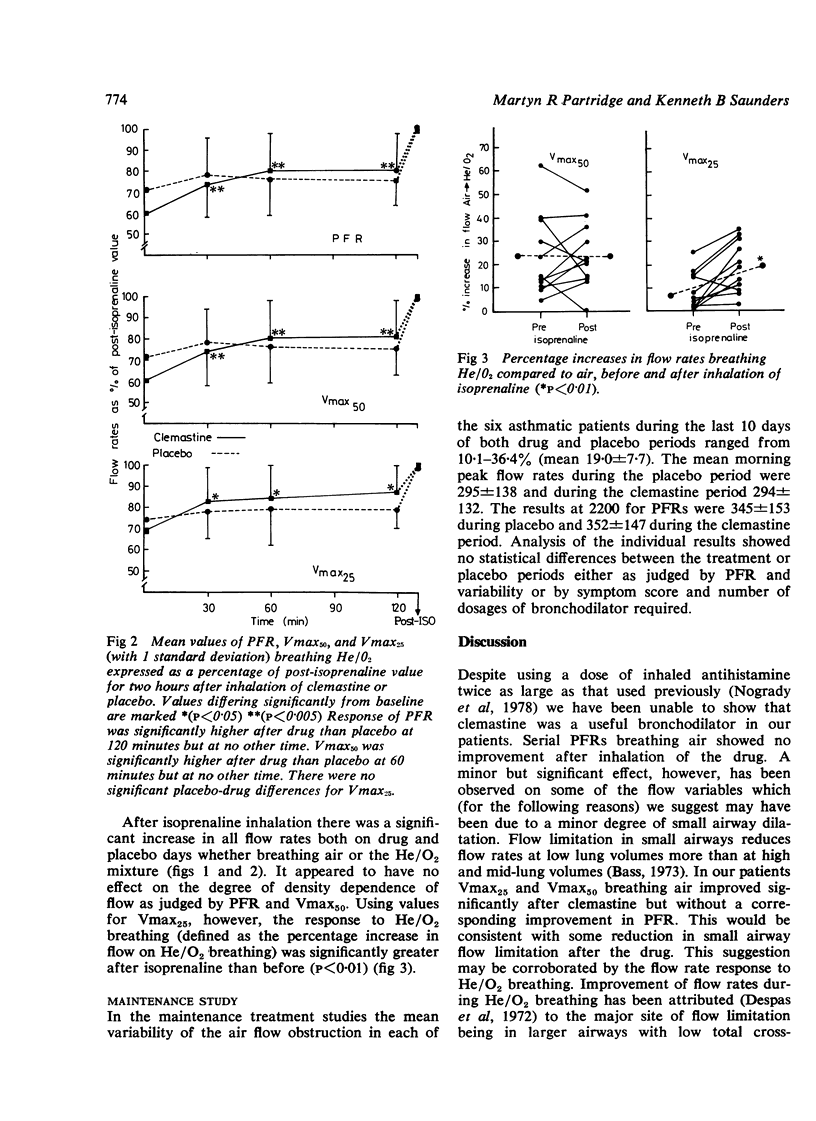
Although intravenous chlorpheniramine can cause bronchodilatation, oral and parenteral antihistamines have not proved useful in treating asthma. Inhaled antihistamines may cause throat irritation, but a recent study of the antihistamine, clemastine, showed it to be an effective bronchodilator without irritant effects. We have extended these studies to determine the site of action of inhaled clemastine and to assess its potential usefulness both as a bronchodilator and as a maintenance treatment. Eleven stable asthmatic patients received inhaled clemastine and placebo and the effect was assessed by serial maximum expiratory flow volume (MEFV) curves breathing air and a helium/oxygen (He/O2) mixture. There was no significant improvement in peak flow rates during air breathing after clemastine and no significant difference between the responses to drug and placebo. Minor but significant changes were seen in some flow measurements on the downslope of the MEFV curve during air and He/O2 breathing, and these are tentatively ascribed to a dilating effect of clemastine on peripheral airways where flow is laminar. Subsequent administration of inhaled isoprenaline showed the patients to be still capable of significant bronchodilatation. The addition of clemastine, from a pressurised aerosol, to the patients' therapeutic regimen for two weeks was no more effective than placebo in controlling airflow obstruction, and did not reduce the need for standard bronchodilators. In our patients clemastine was not a clinically useful bronchodilator either acutely or as a maintenance treatment for asthma.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bass H. The flow volume loop: normal standards and abnormalities in chronic obstructive pulmonary disease. Chest. 1973 Feb;63(2):171–176. doi: 10.1378/chest.63.2.171. [DOI] [PubMed] [Google Scholar]
- Chan-Yeung M., Abboud R., Tsao M. S., Maclean L. Effect of helium on maximal expiratory flow in patients with asthma before and during induced bronchoconstriction. Am Rev Respir Dis. 1976 Apr;113(4):433–443. doi: 10.1164/arrd.1976.113.4.433. [DOI] [PubMed] [Google Scholar]
- Cherniack R. M., Raber M. B. Normal standards for ventilatory function using an automated wedge spirometer. Am Rev Respir Dis. 1972 Jul;106(1):38–46. doi: 10.1164/arrd.1972.106.1.38. [DOI] [PubMed] [Google Scholar]
- Despas P. J., Leroux M., Macklem P. T. Site of airway obstruction in asthma as determined by measuring maximal expiratory flow breathing air and a helium-oxygen mixture. J Clin Invest. 1972 Dec;51(12):3235–3243. doi: 10.1172/JCI107150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram R. H., Jr, Wellman J. J., McFadden E. R., Jr, Mead J. Relative contributions of large and small airways to flow limitation in normal subjects before and after atropine and isoproterenol. J Clin Invest. 1977 Apr;59(4):696–703. doi: 10.1172/JCI108688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nogrady S. G., Bevan C. Inhaled antihistamines--bronchodilatation and effects on histamine- and methacholine-induced bronchoconstriction. Thorax. 1978 Dec;33(6):700–704. doi: 10.1136/thx.33.6.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nogrady S. G., Hartley J. P., Handslip P. D., Hurst N. P. Bronchodilatation after inhalation of the antihistamine clemastine. Thorax. 1978 Aug;33(4):479–482. doi: 10.1136/thx.33.4.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popa V. T. Bronchodilating activity of an H1 blocker, chlorpheniramine. J Allergy Clin Immunol. 1977 Jan;59(1):54–63. doi: 10.1016/0091-6749(77)90177-4. [DOI] [PubMed] [Google Scholar]
- Wellman J. J., McFadden E. R., Jr, Ingram R. H., Jr Density-dependence of maximal expiratory flow rates before and after bronchodilators in patients with obstructive airways disease. Clin Sci Mol Med. 1976 Aug;51(2):133–139. doi: 10.1042/cs0510133. [DOI] [PubMed] [Google Scholar]


