Abstract
Persistent pulmonary hypertension of the newborn (PPHN) is often secondary to parenchymal lung disease (such as meconium aspiration syndrome) or lung hypoplasia (with congenital diaphragmatic hernia) but can also be idiopathic. PPHN is characterized by elevated pulmonary vascular resistance, resulting in right-to-left shunting of blood and hypoxemia. The diagnosis of PPHN is based on clinical evidence of labile hypoxemia often associated with differential cyanosis and confirmed by echocardiography. Lung volume recruitment with optimal use of positive end-expiratory pressure or mean airway pressure and/or surfactant is very important in secondary PPHN due to parenchymal lung disease. Other management strategies include optimal oxygenation, avoiding respiratory and metabolic acidosis, blood pressure stabilization, sedation, and pulmonary vasodilator therapy. Failure of these measures leads to consideration of extracorporeal membrane oxygenation, although this rescue therapy is needed less frequently with advances in medical management. Randomized clinical trials with long-term follow-up are required to evaluate various therapeutic strategies in PPHN.
Introduction
Successful adaptation to extrauterine life requires a rapid increase in pulmonary blood flow at birth to establish the lungs as the site of gas exchange. Persistent pulmonary hypertension of the newborn (PPHN) is secondary to failure of normal circulatory transition at birth. It is a syndrome characterized by elevated pulmonary vascular resistance (PVR) that causes labile hypoxemia due to decreased pulmonary blood flow and right-to-left shunting of blood. Its incidence has been reported as 1.9 per 1,000 live births (0.4–6.8 per 1,000 live births) in the United States and 0.43 to 6 per 1,000 live births in the United Kingdom, with mortality rates ranging from 4% to 33%. (1)(2)
Fetal and Transitional Circulation
Pulmonary hypertension with reduced pulmonary blood flow is a normal physiologic state in the fetus because the placenta, not the lungs, serves as the organ of gas exchange. Most of the right ventricular output crosses the ductus arteriosus to the aorta, and only approximately 8% to 10% of combined ventricular output in an ovine fetus and 13% to 21% in human fetuses perfuse the fetal lungs due to high PVR. (3)(4) Mechanical factors such as fluid-filled lungs, hypoxic pulmonary vasoconstriction, and circulating vasoconstrictors such as endothelin 1, and products of the prostaglandin pathway (ie, leukotriene and thromboxane) all play a significant role in maintaining high fetal PVR. (5) Serotonin increases fetal PVR, and the use of selective serotonin reuptake inhibitors during the last half of pregnancy has been associated with an increased incidence of PPHN, although recent studies have questioned this association.
A series of circulatory events take place at birth to ensure a smooth transition from fetal to extrauterine life. Clamping of the umbilical cord removes the low-resistance placental circulation, increasing systemic arterial pressure. Various mechanisms operate simultaneously to rapidly reduce pulmonary resistance and increase pulmonary blood flow. The most important stimulus to promote pulmonary vasodilation appears to be ventilation of the lungs and an increase in oxygen tension. (5) An 8-fold increase in pulmonary blood flow occurs, which raises left atrial pressure, closing the foramen ovale. Because PVR decreases lower than systemic vascular resistance, flow reverses across the ductus arteriosus (from the aorta to the pulmonary artery or left to right). The increase in arterial oxygen saturation leads to closure of the ductus arteriosus and ductus venosus.
Endothelium-Derived Mediators and Circulatory Transition at Birth
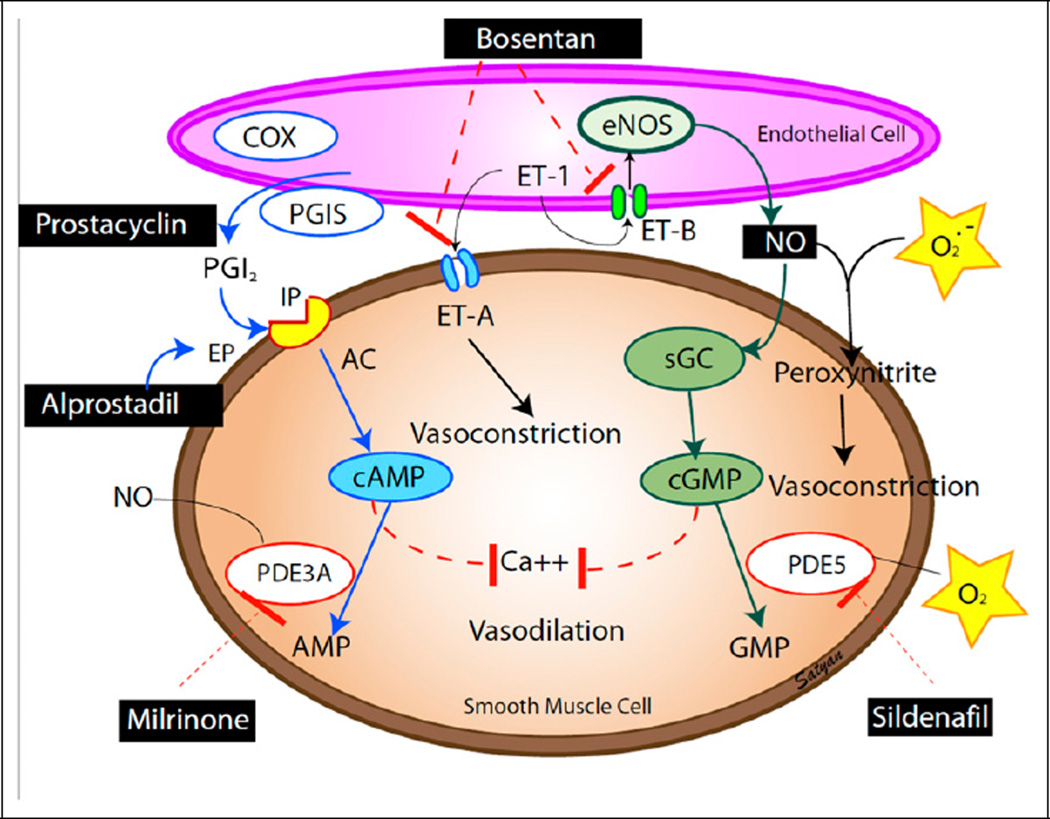
Vascular endothelium releases several vasoactive products that play a primary role in cardiopulmonary transition at birth. Pulmonary endothelial nitric oxide production increases markedly at the time of birth. The shear stress that results from increased pulmonary blood flow and increased oxygenation also induces endothelial nitric oxide synthase (eNOS) expression, thus contributing to nitric oxide–mediated pulmonary vasodilation after birth. (5) Nitric oxide exerts its action through soluble guanylate cyclase and cyclic guanosine monophosphate (Fig 1). The arachidonic acid–prostacyclin pathway also plays an important role; prostaglandins activate adenylate cyclase to increase cyclic adenosine monophosphate concentrations in vascular smooth muscle cells (Fig 1). Inhibition of prostacyclin production by nonsteroidal anti-inflammatory drugs during late pregnancy has been associated with PPHN, (7) although this association has also been recently called into question. (8)
Figure 1.
Endothelium-derived mediators: the vasodilators prostacyclin (PGI2) and nitric oxide (NO) and the vasoconstrictor endothelin (ET-1). Cyclooxygenase (COX) and prostacyclin synthase (PGIS) are involved in the production of prostacyclin. Prostacyclin acts on its receptor (IP) in the smooth muscle cell and stimulates adenylate cyclase (AC) to produce cyclic adenosine monophosphate (cAMP). cAMP is broken down by phosphodiesterase 3A (PDE3A). Milrinone inhibits PDE3A and increases cAMP levels in arterial smooth muscle cells and cardiac myocytes. Endothelin acts on ET-A receptors causing vasoconstriction. A second endothelin receptor (ET-B) on the endothelial cell stimulates NO release and vasodilation. Endothelial nitric oxide synthase (eNOS) produces NO, which stimulates soluble guanylate cyclase (sGC) enzyme to produce cyclic guanosine monophosphate (cGMP). cGMP is broken down by PDE5 enzyme. Sildenafil inhibits PDE5 and increases cGMP levels in pulmonary arterial smooth muscle cells. cAMP and cGMP reduce cytosolic ionic calcium concentrations and induce smooth muscle cell relaxation and pulmonary vasodilation. NO is a free radical and can avidly combine with superoxide anions to form the toxic vasoconstrictor peroxynitrite. Medications used in PPHN are shown in black boxes. Modified from Sharma et al. (6) Copyright Satyan Lakshminrusimha.
Etiology and Pathophysiology of PPHN
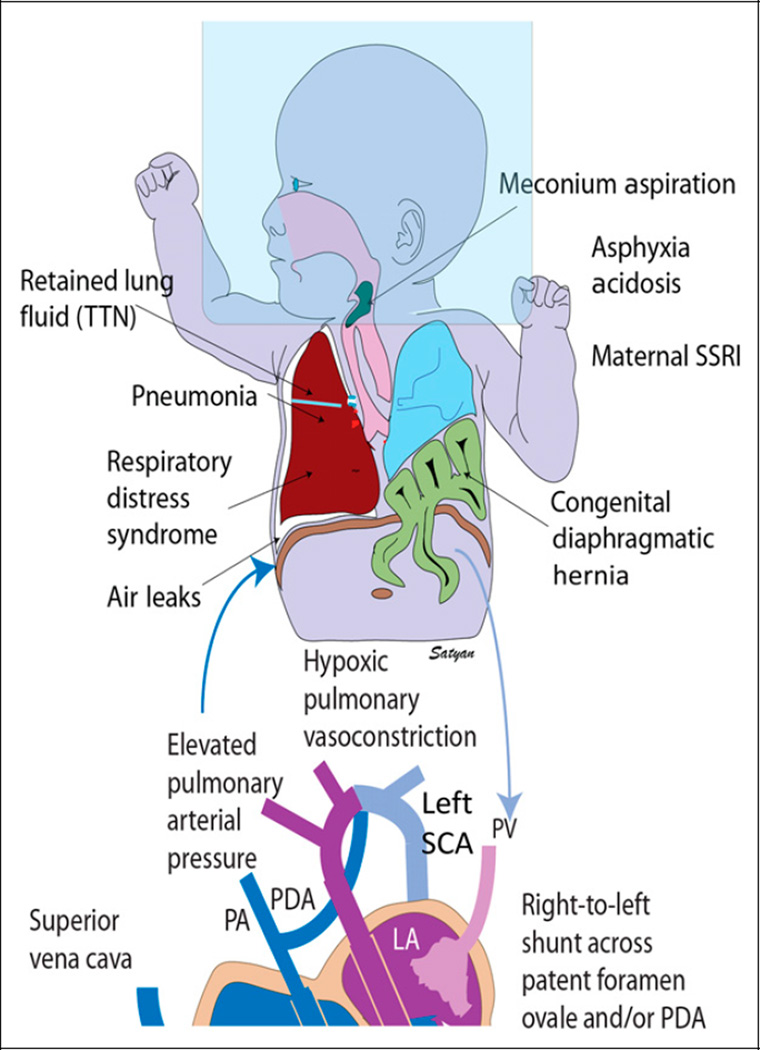
PPHN can be secondary to lung parenchymal diseases, such as meconium aspiration syndrome (with or without asphyxia), respiratory distress syndrome (RDS), or pneumonia or sepsis (maladaptation of pulmonary vasculature); remodeled pulmonary vasculature (maldevelopment) with normal lung parenchyma (primary or idiopathic); or lung hypoplasia (underdevelopment) due to oligohydramnios or congenital diaphragmatic hernia (CDH) or intrinsic obstruction (polycythemia with hyperviscosity). Disruption of normal neonatal circulatory transition due to these factors results in failure to resolve fetal pulmonary hypertension and leads to the persistence of fetal pulmonary hypertension or PPHN. High PVR decreases the blood flow to the lungs because the blood takes the path of least resistance, which is the systemic circulation. Ventilation-perfusion mismatch and extrapulmonary right-to-left shunting of deoxygenated blood across the patent foramen ovale (PFO) and patent ductus arteriosus (PDA) result in cyanosis. Differential cyanosis (saturation in the lower limb is >5%–10% lower than right upper limb) occurs due to pulmonary artery to aorta shunt through the PDA. If the PDA is closed and the shunt exclusively is at the PFO level, the degree of cyanosis is similar in both the upper and lower limbs. Labile hypoxemia (marked change in oxygen saturation with minimal or no change in ventilator settings or fraction of inspired oxygen [FIO2]) is characteristic of PPHN and is due to change in the volume of right-to-left shunt secondary to subtle changes in the delicate balance between PVR and systemic vascular resistance. A few clinically important conditions associated with PPHN are outlined below.
Malignant TTN
Transient tachypnea of newborn (TTN) has been associated with PPHN. For example, after elective cesarean delivery, newborns with TTN who have hypoxemia may be given high concentrations of inspired oxygen (approximately 100%) by hood or nasal cannula (without any positive pressure). In these cases, absorption atelectasis can develop, resulting in increasing oxygen requirements and respiratory failure (Fig 2). Furthermore, the formation of reactive oxygen species from the high alveolar oxygen can lead to increased pulmonary vascular reactivity, thereby contributing to PPHN. (9)(10) The term malignant TTN has been used to describe severe respiratory morbidity and subsequent mortality in newborns delivered by elective cesarean delivery who developed PPHN. (11) One possible strategy when managing these newborns (and to prevent malignant TTN) may be early use of distending pressure (such as continuous positive airway pressure when FIO2 exceeds 0.5–0.6) to inflate and recruit the lungs vs merely administering high amounts of oxygen without positive pressure.
Figure 2.
Etiology and pathophysiology of persistent pulmonary hypertension of the newborn (PPHN). Secondary PPHN can be due to various lung diseases, such as retained lung fluid or transient tachypnea of newborn (TTN), pneumonia, aspiration syndromes, respiratory distress syndrome (RDS), and congenital diaphragmatic hernia with lung hypoplasia. Use of high concentrations of inspired oxygen (approximately 100%) without positive pressure (oxygen hood) can lead to absorption atelectasis and worsening of ventilation-perfusion mismatch. Lung disease and V/Q mismatch result in hypoxemia. Increased pulmonary vascular resistance results in reduced pulmonary blood flow and right-to-left shunt through patent ductus arteriosus (PDA) and/or patent foramen ovale (PFO). Pulmonary hypertension is often associated with systemic hypotension with deviation of the interventricular septum to the left. The right subclavian artery (SCA) (and blood flowing to the right upper extremity) is always preductal. The left SCA may be preductal, juxtaductal, or postductal. Hence, preductal oxygen saturations should be obtained from the right upper extremity and compared with lower extremity to assess differential cyanosis.
LA = left atrium; LV = left ventricle; PA = pulmonary artery; RA = right atrium RV = right ventricle; TR = tricuspid regurgitation. Copyright Satyan Lakshminrusimha.
Pulmonary Hypertension in Premature Infants
Although PPHN is traditionally considered a disease of-term and late preterm infants, it is increasingly being diagnosed in extremely preterm infants. Some preterm infants with RDS present with PPHN in the first few days after birth, (12) whereas preterm infants with bronchopulmonary dysplasia (BPD) may be diagnosed as having pulmonary hypertension later in the hospital course or after discharge from the NICU. Pulmonary artery hypertension complicating BPD is a process somewhat distinct from PPHN and tends to run a much more protracted course. It appears to be a consequence of the reduced pulmonary capillary bed secondary to the simplified lung of new BPD and pulmonary vascular remodeling. Pulmonary vascular disease is challenging to treat and significantly increases morbidity and mortality in BPD. (13)
Preterm infants with fetal growth restriction and those who are born after prolonged rupture of membranes with varying degrees of pulmonary hypoplasia are at higher risk of developing pulmonary hypertension.
Congenital Diaphragmatic Hernia
CDH is a developmental defect in the diaphragm that separates the thorax and the abdomen and is the most important cause of pulmonary hypoplasia resulting in PPHN. CDH has a mortality rate of 20% to 30%, and the degree of associated pulmonary hypoplasia and the severity of pulmonary hypertension remain the major determinants of survival. Despite marked improvement in survival of PPHN resulting from other causes, the mortality and need for extracorporeal membrane oxygenation (ECMO) remain high in infants with CDH.
Alveolar Capillary Dysplasia
Alveolar capillary dysplasia is generally associated with malalignment of the pulmonary veins. It presents with respiratory failure and unremitting PPHN early in life and carries a mortality rate that approaches 100%. (14) Histologic examination of lung tissue remains the gold standard for diagnosis. A lung biopsy to rule out alveolar capillary dysplasia should be considered for neonates who do not respond to conventional medical management or fail attempts at ECMO decannulation.
Diagnosis
In a hypoxemic neonate, differentiating cyanotic congenital heart disease from PPHN is of paramount importance. The initial evaluation should include a thorough history and physical examination, simultaneous measurement of preductal and postductal oxygen saturation, chest radiography, and arterial blood gas tests. Hypoxemia disproportionate to the severity of parenchymal disease on chest radiography should suggest idiopathic PPHN(or cyanotic heart disease). Preductal and postductal oxygen saturation and PaO2 measurements are used to differentiate PPHN from structural heart disease. Saturation differences of greater than 5% to 10% or PaO2 differences of 10 to 20 mm Hg between right upper limb and lower limbs are considered significant. In neonates with PPHN and atrial-level right-to-left shunting without a significant ductal shunt, both the right arm and the right leg saturations will be low. Conversely, infants with PDA and coarctation of the aorta might have differential cyanosis. In PPHN, hypoxemia is often labile unlike fixed hypoxemia seen in cyanotic congenital heart disease. Hyperoxia testing (obtaining an arterial gas measurement after 15 minutes of exposure to 100% oxygen) and hyperoxia-hyperventilation (hyperoxia and alkalosis to induce pulmonary vasodilation and improve PaO2) are no longer widely practiced because of the known adverse effects of hyperoxia and alkalosis. These tests can be avoided by confirming elevated pulmonary pressures by early echocardiography, when available.
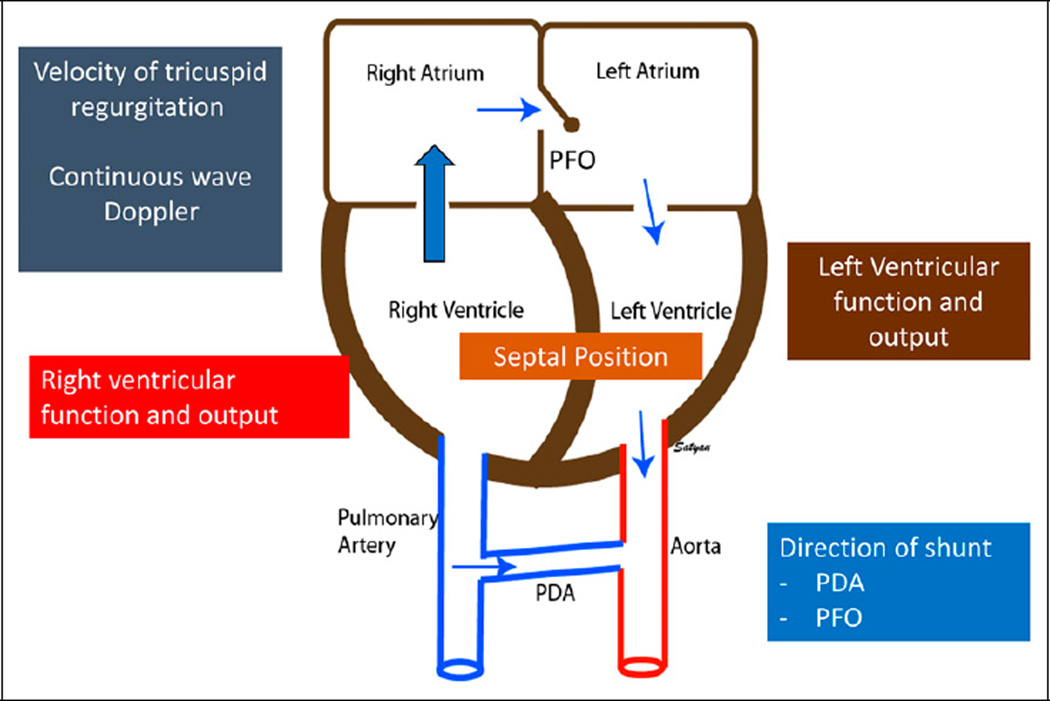
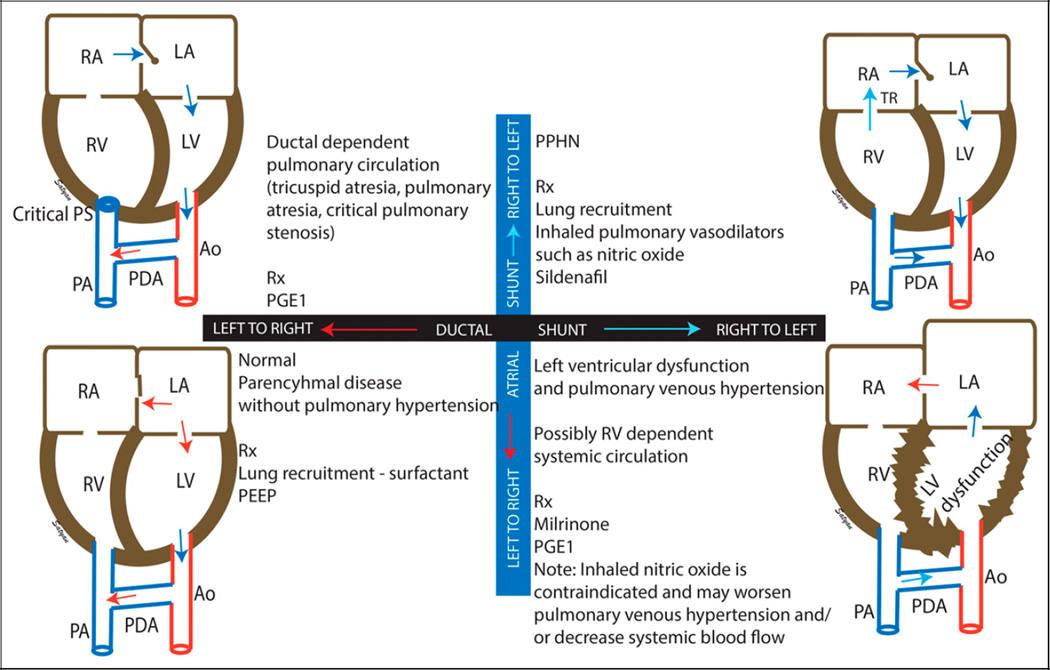
Echocardiography is the gold standard to confirm the diagnosis and to monitor the efficacy of specific therapeutic interventions in PPHN (Fig 3). Measurement of the direction of the ductal and foramen ovale shunt (Fig 4), flattening or left deviation of the interventricular septum, and tricuspid regurgitation velocity on continuous wave Doppler with simultaneous systemic blood pressure measurement provides an indication of right-sided pressures and hemodynamic physiologic mechanisms. Evaluation of right and left ventricular function will guide the choice of appropriate pulmonary vasodilator.
Figure 3.
Echocardiographic features of persistent pulmonary hypertension of the newborn (PPHN): high right ventricular pressure results in tricuspid regurgitation (TR) and deviation of the interventricular septum to the left. Assessment of tricuspid regurgitation velocity by continuous wave Doppler is used to calculate systolic pulmonary arterial pressure. The presence of right-to-left shunt at patent foramen ovale (PFO) and patent ductus arteriosus (PDA) is commonly observed in infants with severe PPHN. Impaired right and left ventricular function is associated with poor outcome in PPHN. Copyright Satyan Lakshminrusimha.
Figure 4.
Echocardiographic evaluation of neonatal hypoxemia based on ductal (black bar) and atrial (blue bar) shunts. Left-to-right shunt at the ductal and atrial level is considered normal but can also be seen in the presence of parenchymal lung disease, resulting in hypoxemia in the absence of persistent pulmonary hypertension of the newborn (PPHN) (lower left quadrant). The presence of right-to-left shunt at the atrial and ductal levels is associated with PPHN (upper right quadrant). Right-to-left shunt at the ductal level but a left-to-right shunt at the atrial level is associated with left ventricular dysfunction, pulmonary venous hypertension, and ductal-dependent systemic circulation (lower right quadrant) and is a contraindication for inhaled pulmonary vasodilators, such as inhaled nitric oxide. In patients with right-sided obstruction (such as critical pulmonary stenosis [PS]), right atrial blood flows to the left atrium through the PFO. Pulmonary circulation is dependent on a left-to-right shunt at the patent ductus arteriosus (PDA) (upper left quadrant).
Ao = aorta; LA = left atrium; LV = left ventricle; PA = pulmonary artery; PGE1 = prostaglandin E1; RA = right atrium; RV = right ventricle; Rx = treatment; TR = tricuspid regurgitation.
Modified from Nair and Lakshminrusimha. (15) Copyright Satyan Lakshminrusimha.
Management
Supportive Therapy
The severity of PPHN can range from mild hypoxemia with minimal respiratory distress to severe hypoxemia and cardiopulmonary instability that requires intensive care support. Infants with PPHN require supportive care, including optimal temperature and nutritional support, avoidance of stress, and handling with sedation and analgesia as needed. Paralysis should be avoided if possible because it has been associated with increased mortality. (1) Additional therapy should target the underlying disease (such as antibiotics for pneumonia or sepsis) (Fig 5).
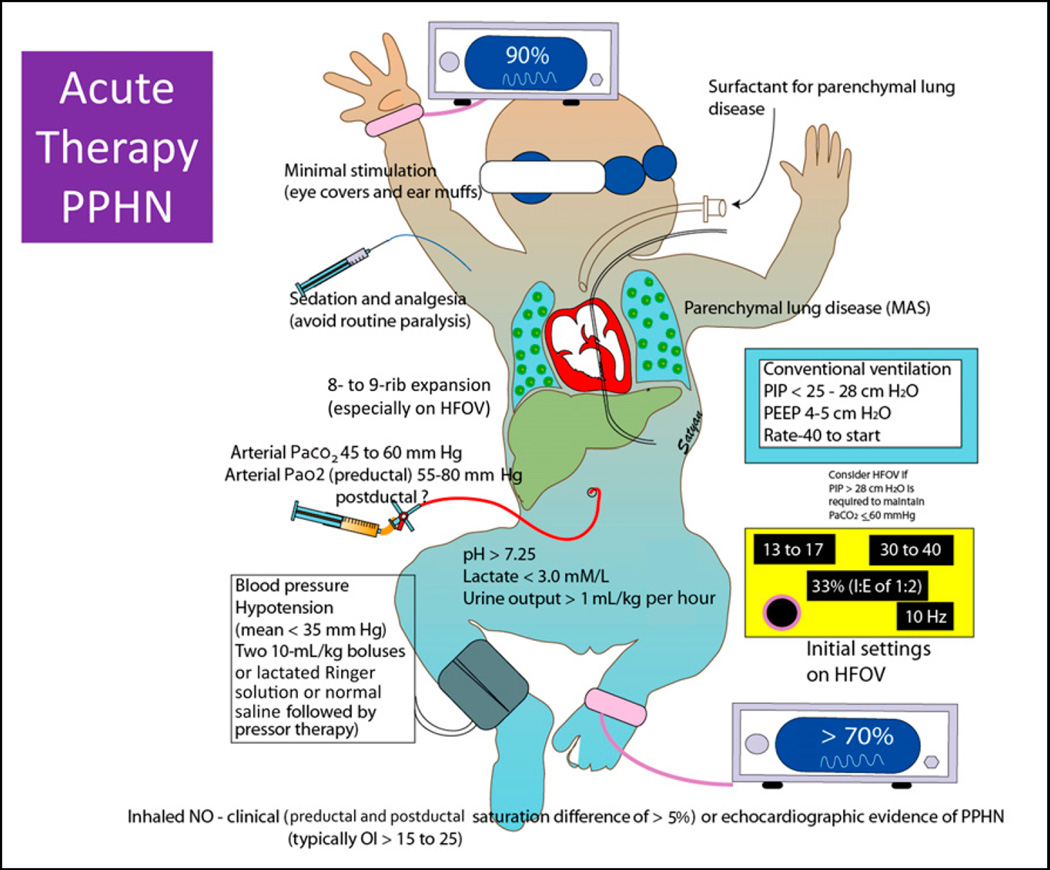
Figure 5.
Management of acute persistent pulmonary hypertension of the newborn (PPHN) (suggested guidelines as recommended by the authors are shown in this figure): (1) minimal stimulation with the use of eye covers and ear muffs; (2) sedation and analgesia with a narcotic agent and a benzodiazepine (avoid muscle paralysis if possible); (3) maintain preductal oxygen saturation in the low to mid-90s and postductal saturations above 70% as long as metabolic acidosis, lactic acidosis, and/or oliguria are not present; (4) lung recruitment with adequate positive end-expiratory pressure (PEEP) or mean airway pressure and/or surfactant to maintain 8- to 9-rib expansion during inspiration; and (5) maintain adequate blood pressure and avoid supraphysiological systemic pressure. See text for details.
HFOV = high frequency oscillatory ventilation; MAS = meconium aspiration syndrome; OI = oxygenation index; PIP = peak inspiratory pressure.
Modified from Nair and Lakshminrusimha. (15) Copyright Satyan Lakshminrusimha.
Mild cases of PPHN with minimal or no respiratory distress may be detected in the newborn nursery either after a desaturation episode or by low postductal oxygen saturation detected on critical congenital heart disease screening. (16) These infants can be managed with supportive care and oxygen supplementation. Close monitoring is important because some of these infants may rapidly deteriorate and require noninvasive ventilation or intubation and mechanical ventilation.
Hyperventilation and infusion of alkali were used in the past but should be avoided because of adverse effects on cerebral perfusion and increased risk of sensorineural deafness. (17)(18) Alkali infusion was associated with increased use of ECMO and need for oxygen at 28 days. (1) Most centers avoid acidosis based on animal studies that found exaggerated hypoxic pulmonary vasoconstriction with pH less than 7.25. (19) We recommend maintaining pH greater than 7.25, preferably 7.30 to 7.40, during the acute phase of PPHN.
Mechanical Ventilation
Optimal lung recruitment (8- to 9-rib expansion on an inspiratory chest radiograph) with the use of positive end-expiratory pressure (PEEP) or mean airway pressure decreases PVR. Both underinflation and overinflation of the lung will lead to elevation of PVR. Gentle ventilation strategies with optimal PEEP, relatively low peak inflation pressure or tidal volume, and a degree of permissive hypercapnia are recommended to ensure adequate lung expansion while limiting barotrauma and volutrauma. (20) In newborns with severe lung disease, high-frequency ventilation is frequently used to optimize lung inflation and minimize lung injury. (21) If a peak inflation pressure of greater than 25 to 28 cm H2O or tidal volumes greater than 6 mL/kg are required to maintain a PaCO2 less than 60 mm Hg on conventional ventilation, we recommend switching to high-frequency (jet or oscillator) ventilation. In clinical studies using inhaled nitric oxide (iNO), the combination of high-frequency ventilation and iNO resulted in the greatest improvement in oxygenation in PPHN associated with diffuse parenchymal lung disease, such as RDS and pneumonia, but had no benefit in idiopathic PPHN or CDH. (22)
Oxygen is a specific and potent pulmonary vasodilator but may be detrimental if used in excess. Mechanical ventilation with high concentrations of oxygen used to be a mainstay of PPHN management. More recently, it has been found that brief exposure to 100% oxygen in newborn lambs results in increased contractility of pulmonary arteries, (9) reduces response to iNO, (23) and increases the potential for oxidative stress. We recommend maintaining preductal oxygen saturations in the low to mid-90s with PaO2 levels between 55 and 80 mm Hg during management of infants with PPHN. If the serum lactate levels are normal (<3 mM/L) and urine output is adequate (≥1 mL/kg per hour), postductal oxygen saturations in the 70s and 80s may be acceptable especially in infants with CDH.
Surfactant
In patients with PPHN secondary to parenchymal lung disease, early administration of surfactant and lung recruitment is associated with better outcome with reduced risk of ECMO or death. (24)(25) Surfactant inactivation and deficiency are observed in many neonatal respiratory disorders, such as pneumonia, RDS, and meconium aspiration syndrome. We recommend that infants with PPHN secondary to parenchymal lung disease receive a dose of surfactant rich in surfactant protein B, such as calfactant or poractant alfa. It is not clear whether surfactant therapy is beneficial in infants with CDH. Animal studies reveal benefit, but a review of the CDH registry did not support the use of surfactant. (26) We recommend administration of surfactant only in the presence of clinical, radiologic, or biochemical evidence of surfactant deficiency in CDH and administer only 50% of the dose because of pulmonary hypoplasia.
Pulmonary Vasodilator Therapy
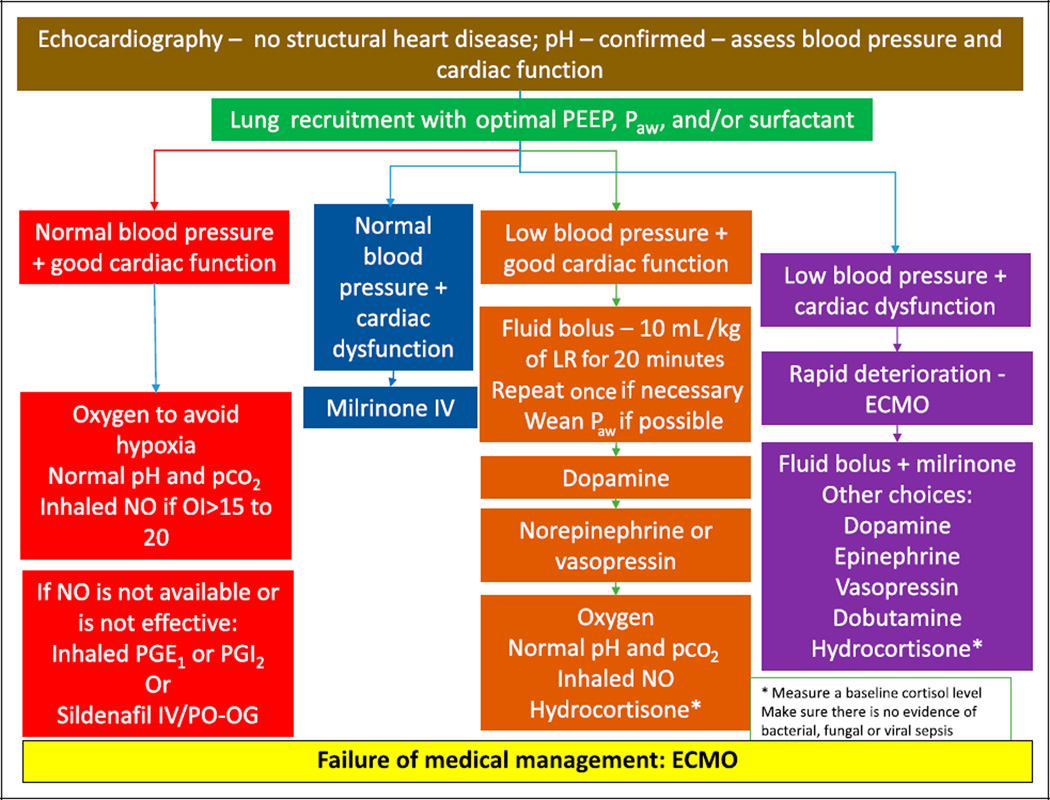
After achieving lung recruitment with and without surfactant therapy, further management should be based on oxygenation status, systemic blood pressure, and cardiac and ventricular function on echocardiography (Fig 6). Various therapeutic strategies outlined in this figure are described below.
Figure 6.
Algorithm showing practical approach to persistent pulmonary hypertension of the newborn (PPHN) based on oxygenation, systemic blood pressure, and cardiac function. See text for details.
ECMO = extracorporeal membrane oxygenation; IV = intravenous; LR = lactated ringers solution; NO = nitric oxide; OI=oxygenation index; Paw = mean airway pressure; PEEP = positive end-expiratory pressure; PGE1 = prostaglandin E1; PGI2 = prostaglandin I2; PO-OG = per oral or orogastric.
Copyright Satyan Lakshminrusimha.
iNO is a potent and selective pulmonary vasodilator without a significant decrease in systemic blood pressure (selective effect of iNO). iNO is also preferentially distributed to the ventilated segments of the lung, resulting in increased perfusion of the ventilated segments, optimizing ventilation-perfusion match (microselective effect of iNO). Studies have found that iNO therapy causes marked improvement in oxygenation in term newborns with PPHN. (27) Multicenter randomized clinical studies subsequently confirmed that iNO therapy reduces the need for ECMO in term neonates with hypoxemic respiratory failure. (28) (29)(30) iNO therapy is the only therapy approved by the US Food and Drug Administration for clinical use in term or near-term newborn infants (>34 weeks’ gestation) with PPHN. Konduri et al initially found that earlier initiation of iNO with an oxygenation index (OI) of 15 to 25 did not reduce the need for ECMO but may have a tendency to reduce the risk of progression to severe hypoxemic respiratory failure. (31) Post hoc analysis of the same study suggested that the use of surfactant before randomization and enrollment (and use of iNO) at an OI of 20 or less was associated with reduced incidence of ECMO or death. (25) A dose of 20 ppm results in improved oxygenation and the most optimal decrease in pulmonary to systemic arterial pressure ratio (32) and is the typical starting dose. Higher doses are not recommended because they are associated with increased levels of nitrogen dioxide and methemoglobin. (27) To summarize, we recommend initiation of iNO if the OI is approximately 20 at a dose of 20 ppm. A complete response to iNO is defined as an increase in Pao2/FIO2 ratio of 20 mm Hg or more (20-20-20 rule for initiation of iNO). Methemoglobin levels are monitored at 2 hours, 8 hours after initiation of iNO, and then once a day for the duration of iNO therapy. Some centers stop checking methemoglobin levels after the first couple of days if levels are low (<2%) and iNO dose remains less than 20 ppm.
Weaning iNO is a gradual process to minimize the risk of rebound vasoconstriction and resultant pulmonary hypertension associated with abrupt withdrawal. Weaning in steps from 20 ppm gradually for a period before its discontinuation prevents the rebound effect. (33) If there is oxygenation response, inspired oxygen concentration is first weaned below 60%, and then iNO is weaned only if PaO2 can be maintained at 60 mm Hg or higher (or preductal oxygen saturation as measured by pulse oximetry ≥90%) for 60 minutes (60-60-60 rule of weaning iNO). Our practice is to wean iNO at a rate of 5 ppm every 4 hours. Once iNO dose is 5 ppm, gradual weaning by 1 ppm every 2 to 4 hours is performed. Continuing iNO in infants unresponsive to iNO or failure to wean iNO can potentially lead to prolonged dependence on iNO due to suppression of endogenous eNOS. (34)(35)
If iNO is not effective or not available and if hypoxemia persists, further management is based on systemic blood pressure and ventricular function on echocardiography:
-
If blood pressure is relatively stable but hypoxemia persists, consider the use of phosphodiesterase (PDE) 5 inhibitors, especially in the presence of a right-to-left shunt at the PFO and/or PDA levels with good ventricular function (Fig 4). Sildenafil, administered by intravenous (preferred) or oral route, is usually the firstline agent. Sildenafil is metabolized by the liver, and severe hepatic dysfunction may impair its metabolism. On the basis of pharmacokinetic data in neonates with PPHN, intravenous sildenafil is administered as a load of 0.42 mg/kg for 3 hours (0.14 mg/kg per hour) followed by 1.6 mg/kg per day as a continuous maintenance infusion (0.07 mg/kg per hour). Careful monitoring of systemic blood pressure is necessary during sildenafil therapy. Studies have found that oral sildenafil (dose range, 1–2 mg/kg every 6 hours) improves oxygenation and reduces mortality in centers limited by nonavailability of iNO and ECMO. (36)(37) Neonatal clinicians should be aware of the current US Food and Drug Administration safety warning in the pediatric population based on a dose escalation pediatric trial (all infants were older than 1 year) that demonstrated a higher mortality in the high-dose group. (38)
Alternate agents (not approved by the US Food and Drug Administration) for iNO-resistant PPHN include aerosolized prostaglandin E1 at 150 to 300 ng/kg per minute diluted in saline to provide 4 mL/h (39) and inhaled prostaglandin I2 at a dose of 50 ng/kg per minute. (40) The intravenous formulation epoprostenol sodium is dissolved in 20 mL of manufacturer’s diluent (a glycine buffer, pH – 10). Fresh solution is added to the nebulization chamber every 4 hours. (40) The effect of such alkaline pH on neonatal respiratory tract is not known. Iloprost is a synthetic prostacyclin that can also be delivered by aerosolization (1–2.5 µg/kg every 2–4 hours) (41) or by intravenous route (dose of 0.5 to 3 ng/kg perminute and titrated to 1–10 ng/kg per minute) (42) and improves oxygenation in PPHN.
If blood pressure is normal but there is evidence of ventricular dysfunction, an inodilator such as milrinone might be the preferred therapeutic agent in PPHN. (43) For example, if left ventricular dysfunction is associated with high left atrial pressures and a left-to-right shunt at the level of the foramen ovale in the presence of a right-to-left shunt at the ductus arteriosus (Fig 4), iNO is contraindicated because it may precipitate pulmonary edema and respiratory deterioration. Milrinone inhibits PDE3 and increases concentration of cyclic adenosine monophosphate in pulmonary and systemic arterial smooth muscle and in cardiac muscle. (44) A loading dose (50 µg/kg for 30–60 minutes) followed by a maintenance dose (0.33 µg/kg per minute and escalated to 0.66 and then to 1 µg/kg per minute based on response) are commonly used. The loading dose is not recommended in the presence of systemic hypotension. As with any systemic vasodilator, hypotension is a clinical concern, and blood pressure needs to be closely monitored. A fluid bolus (10mL/kg of lactated Ringer solution or normal saline) before a loading dose may decrease the risk of hypotension.
In the presence of systemic hypotension and good cardiac function, 1 or 2 fluid boluses (10 mL/kg of lactated Ringer solution or saline) followed by dopamine are recommended. Some centers prefer the use of norepinephrine or vasopressin because these agents are thought to be more selective systemic vasoconstrictors. If high doses of vasopressors are needed, a cortisol level is measured in these patients. If the levels are low relative to the infant’s stress level and there is no evidence of infection (viral, bacterial or fungal), the authors recommend a stress dose of hydrocortisone.
Hypotension is associated with cardiac dysfunction, and rapid deterioration with hemodynamic instability should precipitate cannulation for ECMO(or immediate transfer to an ECMO center).
Chronic Pulmonary Hypertension in Neonates
Neonates with CDH and BPD can have pulmonary hypertension lasting for weeks or months. In the hospital setting, these patients are often managed with supplemental oxygen, iNO (sometimes through a nasal cannula), and oral pulmonary vasodilators, such as sildenafil or bosentan. Because of its high cost, long-term therapy with iNO is cost prohibitive, and most patients can be successfully transitioned to sildenafil after a few days.
Bosentan is an endothelin 1 receptor blocker (Fig 1) that may be beneficial in the management of PPHN. (45) However, the results of a multicenter, randomized, doubleblind, placebo-controlled exploratory trial of bosentan (2 mg/kg per dose twice daily) did not have any additive effect on the top of iNO in term neonates with PPHN. (46)
ECMO is a modified cardiopulmonary bypass used for a prolonged period to support heart and lung function. The use of neonatal ECMO has decreased from a peak of more than 1,500 cases per year in the early 1990s to approximately 750 cases per year. This decline is likely due to improvements in both perinatal care and availability of advanced therapies for neonatal hypoxemic respiratory failure, including high-frequency ventilators, surfactant, and iNO. Generally accepted criteria to start ECMO are persistent hypoxemia (with an OI of >40 or alveolar-arterial gradient >600 despite aggressive medical management of PPHN with mechanical ventilation and iNO) and the presence of hemodynamic instability (Fig 6).
Neurodevelopmental Outcome in NICU Graduates With Severe PPHN
The infants with PPHN who survive and are discharged from the NICU have long-term consequences, such as neurodevelopmental, cognitive, and hearing abnormalities. (47)(48)(49) Thus, it is essential to provide long-term multidisciplinary follow-up after discharge. In their long-term follow-up of infants randomized to early iNO in PPHN, Konduri et al noted neurodevelopmental impairment in approximately 25% of infants and hearing impairment in approximately 23%. (47) The UK collaborative trial randomized critically ill neonates into transfer to a regional center for ECMO or continued conventional care at the local NICU. At 7-year follow-up, mortality remained significantly lower in the ECMO group, with no increase in disability. (50) The presence of neurodevelopmental and medical disabilities may reflect the severity of the underlying illnesses experienced by these infants rather than complications of iNO or ECMO.
Conclusion
The management of PPHN has significantly improved during the last 2 decades. The emphasis has shifted from hyperoxygenation-hyperventilation-alkalosis to improved gentle ventilation strategies to optimize lung recruitment and minimize oxygen toxic effects and permissive hypercapnia paired with the therapeutic use of surfactant and iNO. These changes have led to a substantial decrease in the number of neonatal PPHN patients requiring ECMO for respiratory disorders. Two remaining challenges where large knowledge gaps persist include management of pulmonary hypoplasia and pulmonary hypertension in CDH and BPD-associated pulmonary hypertension in the premature infant. Newer pulmonary vasodilators, such as antioxidants (superoxide dismutase), soluble guanylate cyclase activators, and rho-kinase inhibitors, are currently under investigation. At the same time, many nurseries around the world cannot afford proven but expensive therapies such as iNO and ECMO. Further research to develop appropriate cost-effective strategies to ameliorate pulmonary vascular disease associated with conditions such as pneumonia and asphyxia and meconium aspiration, common in developing countries, is warranted.
Educational Gap.
Complete understanding of the complex pathophysiology and optimal management of persistent pulmonary hypertension remains elusive.
Persistent pulmonary hypertension among extremely preterm infants and infants with congenital diaphragmatic hernia is associated with high morbidity and mortality.
Objectives.
After completing this article, readers should be able to:
Understand the origin of persistent pulmonary hypertension of the newborn (PPHN) and hypoxemic respiratory failure.
Optimize the use of oxygen during management of PPHN.
Outline the importance of lung recruitment using positive end-expiratory pressure or mean airway pressure and/or surfactant in PPHN.
Rationalize the choice of inhaled, intravenous, and oral pulmonary vasodilators.
American Board of Pediatrics Neonatal-Perinatal Content Specifications.
Know the pathogenesis, pathophysiology, pathologic features, and risk factors for persistent pulmonary hypertension.
Recognize the clinical features and differential diagnosis of persistent pulmonary hypertension.
Recognize the laboratory, imaging, and other diagnostic features of persistent pulmonary hypertension.
Know the management of persistent pulmonary hypertension including assisted ventilation, pharmacologic approaches, and ECMO.
Acknowledgments
Ikaria had no role in the preparation of the manuscript. He was supported by grant HD072929 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development during the preparation of the manuscript.
Footnotes
AUTHOR DISCLOSURE
Dr Lakshminrusimha has disclosed that he was previously a member of the speaker bureau for Ikaria (until October 2014), manufacturer of inhaled nitric oxide. He also declares that he has no competing interest in published data. Dr Keszler has disclosed no financial relationships relevant to this article.
This commentary does contain a discussion of an unapproved/ investigative use of a commercial product/ device.
References
- 1.Walsh-Sukys MC, Tyson JE, Wright LL, et al. Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics. 2000;105(1, pt 1):14–20. doi: 10.1542/peds.105.1.14. [DOI] [PubMed] [Google Scholar]
- 2.Bendapudi P, Rao GG, Greenough A. Diagnosis and management of persistent pulmonary hypertension of the newborn. Paediatr Respir Rev. 2015;16(3):157–161. doi: 10.1016/j.prrv.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Dawes GS. Pulmonary circulation in the foetus and new-born. Br Med Bull. 1966;22(1):61–65. doi: 10.1093/oxfordjournals.bmb.a070439. [DOI] [PubMed] [Google Scholar]
- 4.Rasanen J, Wood DC, Weiner S, Ludomirski A, Huhta JC. Role of the pulmonary circulation in the distribution of human fetal cardiac output during the second half of pregnancy. Circulation. 1996;94(5):1068–1073. doi: 10.1161/01.cir.94.5.1068. [DOI] [PubMed] [Google Scholar]
- 5.Lakshminrusimha S, Steinhorn RH. Pulmonary vascular biology during neonatal transition. Clin Perinatol. 1999;26(3):601–619. [PubMed] [Google Scholar]
- 6.Sharma V, Berkelhamer SK, Lakshminrusimha S. Persistent pulmonary hypertension of the newborn. Matern Health Neonatol Perinatol. BMC. 2015;1(14):1–18. doi: 10.1186/s40748-015-0015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alano MA, Ngougmna E, Ostrea EM, Jr, Konduri GG. Analysis of nonsteroidal antiinflammatory drugs in meconium and its relation to persistent pulmonary hypertension of the newborn. Pediatrics. 2001;107(3):519–523. doi: 10.1542/peds.107.3.519. [DOI] [PubMed] [Google Scholar]
- 8.Van Marter LJ, Hernandez-Diaz S, Werler MM, Louik C, Mitchell AA. Nonsteroidal antiinflammatory drugs in late pregnancy and persistent pulmonary hypertension of the newborn. Pediatrics. 2013;131(1):79–87. doi: 10.1542/peds.2012-0496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lakshminrusimha S, Russell JA, Steinhorn RH, et al. Pulmonary arterial contractility in neonatal lambs increases with 100% oxygen resuscitation. Pediatr Res. 2006;59(1):137–141. doi: 10.1203/01.pdr.0000191136.69142.8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramachandrappa A, Jain L. Elective cesarean section: its impact on neonatal respiratory outcome. Clin Perinatol. 2008;35(2):373–393. vii. doi: 10.1016/j.clp.2008.03.006. [vii.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keszler M, Carbone MT, Cox C, Schumacher RE. Severe respiratory failure after elective repeat cesarean delivery: a potentially preventable condition leading to extracorporeal membrane oxygenation. Pediatrics. 1992;89(4, pt 1):670–672. [PubMed] [Google Scholar]
- 12.Kumar VH, Hutchison AA, Lakshminrusimha S, Morin FC, III, Wynn RJ, Ryan RM. Characteristics of pulmonary hypertension in preterm neonates. J Perinatol. 2007;27(4):214–219. doi: 10.1038/sj.jp.7211673. [DOI] [PubMed] [Google Scholar]
- 13.Mourani PM, Abman SH. Pulmonary vascular disease in bronchopulmonary dysplasia: pulmonary hypertension and beyond. Curr Opin Pediatr. 2013;25(3):329–337. doi: 10.1097/MOP.0b013e328360a3f6. [DOI] [PubMed] [Google Scholar]
- 14.Deutsch GH, Young LR, Deterding RR, et al. Pathology Cooperative Group; ChILD Research Co-operative. Diffuse lung disease in young children: application of a novel classification scheme. Am J Respir Crit Care Med. 2007;176(11):1120–1128. doi: 10.1164/rccm.200703-393OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nair J, Lakshminrusimha S. Update on PPHN: mechanisms and treatment. Semin Perinatol. 2014;38(2):78–91. doi: 10.1053/j.semperi.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manja V, Mathew B, Carrion V, Lakshminrusimha S. Critical congenital heart disease screening by pulse oximetry in a neonatal intensive care unit. J Perinatol. 2014 doi: 10.1038/jp.2014.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bifano EM, Pfannenstiel A. Duration of hyperventilation and outcome in infants with persistent pulmonary hypertension. Pediatrics. 1988;81(5):657–661. [PubMed] [Google Scholar]
- 18.Hendricks-Muñoz KD, Walton JP. Hearing loss in infants with persistent fetal circulation. Pediatrics. 1988;81(5):650–656. [PubMed] [Google Scholar]
- 19.Rudolph AM, Yuan S. Response of the pulmonary vasculature to hypoxia and H+ ion concentration changes. J Clin Invest. 1966;45(3):399–411. doi: 10.1172/JCI105355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wung JT, James LS, Kilchevsky E, James E. Management of infants with severe respiratory failure and persistence of the fetal circulation, without hyperventilation. Pediatrics. 1985;76(4):488–494. [PubMed] [Google Scholar]
- 21.Kinsella JP, Abman SH. Clinical approaches to the use of high-frequency oscillatory ventilation in neonatal respiratory failure. J Perinatol. 1996;16(2, pt 2) suppl:S52–S55. [PubMed] [Google Scholar]
- 22.Kinsella JP, Truog WE, Walsh WF, et al. Randomized, multicenter trial of inhaled nitric oxide and high-frequency oscillatory ventilation in severe, persistent pulmonary hypertension of the newborn. J Pediatr. 1997;131(1, pt 1):55–62. doi: 10.1016/s0022-3476(97)70124-0. [DOI] [PubMed] [Google Scholar]
- 23.Lakshminrusimha S, Swartz DD, Gugino SF, et al. Oxygen concentration and pulmonary hemodynamics in newborn lambs with pulmonary hypertension. Pediatr Res. 2009;66(5):539–544. doi: 10.1203/PDR.0b013e3181bab0c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lotze A, Mitchell BR, Bulas DI, Zola EM, Shalwitz RA, Gunkel JH Survanta in Term Infants Study Group. Multicenter study of surfactant (Beractant) use in the treatment of term infants with severe respiratory failure. J Pediatr. 1998;132(1):40–47. doi: 10.1016/s0022-3476(98)70482-2. [DOI] [PubMed] [Google Scholar]
- 25.Konduri GG, Sokol GM, Van Meurs KP, et al. Impact of early surfactant and inhaled nitric oxide therapies on outcomes in term/late preterm neonates with moderate hypoxic respiratory failure. J Perinatol. 2013;33(12):944–949. doi: 10.1038/jp.2013.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Meurs K Congenital Diaphragmatic Hernia Study Group. Is surfactant therapy beneficial in the treatment of the term newborn infant with congenital diaphragmatic hernia? J Pediatr. 2004;145(3):312–316. doi: 10.1016/j.jpeds.2004.04.056. [DOI] [PubMed] [Google Scholar]
- 27.Davidson D, Barefield ES, Kattwinkel J, et al. The I-NO/PPHN Study Group. Inhaled nitric oxide for the early treatment of persistent pulmonary hypertension of the term newborn: a randomized, double-masked, placebo-controlled, dose-response, multicenter study. Pediatrics. 1998;101(3, pt 1):325–334. doi: 10.1542/peds.101.3.325. [DOI] [PubMed] [Google Scholar]
- 28.Clark RH, Kueser TJ, Walker MW, et al. Clinical Inhaled Nitric Oxide Research Group. Low-dose nitric oxide therapy for persistent pulmonary hypertension of the newborn. N Engl J Med. 2000;342(7):469–474. doi: 10.1056/NEJM200002173420704. [DOI] [PubMed] [Google Scholar]
- 29.Neonatal Inhaled Nitric Oxide Study Group. Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure [erratum appears in N Engl J Med. 1997; 337 (6):434] N Engl J Med. 1997;336(9):597–604. doi: 10.1056/NEJM199702273360901. [DOI] [PubMed] [Google Scholar]
- 30.Roberts JD, Jr, Fineman JR, Morin FC, III, et al. The Inhaled Nitric Oxide Study Group. Inhaled nitric oxide and persistent pulmonary hypertension of the newborn. N Engl J Med. 1997;336(9):605–610. doi: 10.1056/NEJM199702273360902. [DOI] [PubMed] [Google Scholar]
- 31.Konduri GG, Kim UO. Advances in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatr Clin North Am. 2009;56(3):579–600. doi: 10.1016/j.pcl.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tworetzky W, Bristow J, Moore P, et al. Inhaled nitric oxide in neonates with persistent pulmonary hypertension. Lancet. 2001;357(9250):118–120. doi: 10.1016/S0140-6736(00)03548-0. [DOI] [PubMed] [Google Scholar]
- 33.Sokol GM, Fineberg NS, Wright LL, Ehrenkranz RA. Changes in arterial oxygen tension when weaning neonates from inhaled nitric oxide. Pediatr Pulmonol. 2001;32(1):14–19. doi: 10.1002/ppul.1083. [DOI] [PubMed] [Google Scholar]
- 34.Sheehy AM, Burson MA, Black SM. Nitric oxide exposure inhibits endothelial NOS activity but not gene expression: a role for superoxide. Am J Physiol. 1998;274(5 Pt 1):L833–L841. doi: 10.1152/ajplung.1998.274.5.L833. [DOI] [PubMed] [Google Scholar]
- 35.Black SM, Heidersbach RS, McMullan DM, Bekker JM, Johengen MJ, Fineman JR. Inhaled nitric oxide inhibits NOS activity in lambs: potential mechanism for rebound pulmonary hypertension. Am J Physiol. 1999;277(5 Pt 2):H1849–H1856. doi: 10.1152/ajpheart.1999.277.5.H1849. [DOI] [PubMed] [Google Scholar]
- 36.Baquero H, Soliz A, Neira F, Venegas ME, Sola A. Oral sildenafil in infants with persistent pulmonary hypertension of the newborn: a pilot randomized blinded study. Pediatrics. 2006;117(4):1077–1083. doi: 10.1542/peds.2005-0523. [DOI] [PubMed] [Google Scholar]
- 37.Vargas-Origel A, Gomez-Rodriguez G, Aldana-Valenzuela C, Vela-Huerta MM, Alarcon-Santos SB, Amador-Licona N. The use of sildenafil in persistent pulmonary hypertension of the newborn. Am J Perinatol. 2009;27(3):225–230. doi: 10.1055/s-0029-1239496. [DOI] [PubMed] [Google Scholar]
- 38.Abman SH, Kinsella JP, Rosenzweig EB, et al. Pediatric Pulmonary Hypertension Network (PPHNet) Implications of the U.S. Food and Drug Administration warning against the use of sildenafil for the treatment of pediatric pulmonary hypertension. Am J Respir Crit Care Med. 2013;187(6):572–575. doi: 10.1164/rccm.201210-1928PP. [DOI] [PubMed] [Google Scholar]
- 39.Sood BG, Keszler M, Garg M, et al. Inhaled PGE1 in neonates with hypoxemic respiratory failure: two pilot feasibility randomized clinical trials. Trials. 2014;15(1):486. doi: 10.1186/1745-6215-15-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelly LK, Porta NF, Goodman DM, Carroll CL, Steinhorn RH. Inhaled prostacyclin for term infants with persistent pulmonary hypertension refractory to inhaled nitric oxide. J Pediatr. 2002;141(6):830–832. doi: 10.1067/mpd.2002.129849. [DOI] [PubMed] [Google Scholar]
- 41.Kahveci H, Yilmaz O, Avsar UZ, et al. Oral sildenafil and inhaled iloprost in the treatment of pulmonary hypertension of the newborn. Pediatr Pulmonol. 2014;49(12):1205–1213. doi: 10.1002/ppul.22985. [DOI] [PubMed] [Google Scholar]
- 42.Janjindamai W, Thatrimontrichai A, Maneenil G, Chanvitan P, Dissaneevate S. Effectiveness and safety of intravenous iloprost for severe persistent pulmonary hypertension of the newborn. Indian Pediatr. 2013;50(10):934–938. doi: 10.1007/s13312-013-0263-1. [DOI] [PubMed] [Google Scholar]
- 43.Lakshminrusimha S, Steinhorn RH. Inodilators in nitric oxide resistant persistent pulmonary hypertension of the newborn. Pediatr Crit Care Med. 2013;14(1):107–109. doi: 10.1097/PCC.0b013e318250af44. [DOI] [PubMed] [Google Scholar]
- 44.McNamara PJ, Shivananda SP, Sahni M, Freeman D, Taddio A. Pharmacology of milrinone in neonates with persistent pulmonary hypertension of the newborn and suboptimal response to inhaled nitric oxide. Pediatr Crit Care Med. 2013;14(1):74–84. doi: 10.1097/PCC.0b013e31824ea2cd. [DOI] [PubMed] [Google Scholar]
- 45.Mohamed WA, Ismail M. A randomized, double-blind, placebo-controlled, prospective study of bosentan for the treatment of persistent pulmonary hypertension of the newborn. J Perinatol. 2012;32(8):608–613. doi: 10.1038/jp.2011.157. [DOI] [PubMed] [Google Scholar]
- 46.Steinhorn RH, Fineman J, Kusic-Pajic A, et al. Bosentan as adjunctive therapy for persistent pulmonary hypertension of the newborn: results of the FUTURE-4 study. Circulation. 2014;130:A13503. doi: 10.1016/j.jpeds.2016.06.078. [DOI] [PubMed] [Google Scholar]
- 47.Konduri GG, Vohr B, Robertson C, Sokol GM, Solimano A, Singer J, et al. Early inhaled nitric oxide therapy for term and near-term newborn infants with hypoxic respiratory failure: neurodevelopmental follow-up. J Pediatr. 2007;150(3):235–240. 240 e231. doi: 10.1016/j.jpeds.2006.11.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Robertson CM, Tyebkhan JM, Hagler ME, Cheung PY, Peliowski A, Etches PC. Late-onset, progressive sensorineural hearing loss after severe neonatal respiratory failure. Otol Neurotol. 2002;23(3):353–356. doi: 10.1097/00129492-200205000-00022. [DOI] [PubMed] [Google Scholar]
- 49.Lipkin PH, Davidson D, Spivak L, Straube R, Rhines J, Chang CT. Neurodevelopmental and medical outcomes of persistent pulmonary hypertension in term newborns treated with nitric oxide. J Pediatr. 2002;140(3):306–310. doi: 10.1067/mpd.2002.122730. [DOI] [PubMed] [Google Scholar]
- 50.McNally H, Bennett CC, Elbourne D, Field DJ Group UKCET; UK Collaborative ECMO Trial Group. United Kingdom collaborative randomized trial of neonatal extracorporeal membrane oxygenation: follow-up to age 7 years. Pediatrics. 2006;117(5):e845–e854. doi: 10.1542/peds.2005-1167. [DOI] [PubMed] [Google Scholar]