Abstract
Objective
Bullying is a common childhood experience with enduring psychosocial consequences. The aim of this study was to test whether bullying increases risk for eating disorder symptoms.
Method
Ten waves of data on 1420 participants between ages 9 and 25 were used from the prospective population-based Great Smoky Mountains Study. Structured interviews were used to assess bullying involvement and symptoms of anorexia nervosa and bulimia nervosa as well as associated features. Bullying involvement was categorized as not involved, bully only, victim only, or both bully and victim (bully-victims).
Results
Within childhood/adolescence, victims of bullying were at increased risk for symptoms of anorexia nervosa and bulimia nervosa as well as associated features. These associations persisted after accounting for prior eating disorder symptom status as well as preexisting psychiatric status and family adversities. Bullies were at increased risk of symptoms of bulimia and associated features of eating disorders, and bully-victims had higher levels of anorexia symptoms. In terms of individual items, victims were at risk for binge eating and bully-victims had more binge eating and use of vomiting as a compensatory behavior. There was little evidence in this sample that these effects differed by sex. Childhood bullying status was not associated with increased risk for persistent eating disorder symptoms into adulthood (ages 19, 21, and 25).
Discussion
Bullying predicts eating disorder symptoms for both bullies and victims. Bullying involvement should be a part of risk assessment and treatment planning for children with eating problems.
Keywords: Eating behavior, Body Image, Bullying, Epidemiology, Childhood, Adolescence, Psychosocial, Stress
Bullying involves targeting an individual perceived to be vulnerable for repeated mistreatment (1). Bullying is a common childhood experience with enduring social and psychological consequences (e.g., (2–4)). Victims of bullying are at increased risk of physical health problems (5), behavior and emotional problems (6), suicidality (7), psychotic symptoms (8) and poor school achievement (9). Victims who also bully others (so-called bully-victims) have the worst outcomes (2, 3). Despite widespread evidence that bullying negatively affects childhood functioning, few studies have explored whether the negative effects of bullying extend to eating problems.
Eating behavior may be affected by bullying for several reasons. First, bullying may increase negative perceptions of one’s body either directly via teasing about one’s weight/appearance (10) or indirectly through its effects on general self-esteem and emotional problems (11). Most studies of body dissatisfaction and disordered eating have focused on teasing that is appearance or weight-related (12). These studies suggest moderate associations of teasing with body dissatisfaction, dietary restraint, and bulimic behaviors(13). The associations, however, are attenuated in longitudinal studies that account for prior levels of body dissatisfaction/disordered eating, and almost no studies have accounted for other preexisting family and individual factors that increase risk for being teased in the first place (14). As such, questions remain about the role of childhood teasing in eating disorder-related problems.
Bullying involves a range of forms of peer victimization beyond weight/appearance-related teasing (e.g., overt aggression, social exclusion, and rumor mongering) (15). Studies of teasing that is not appearance/weight related suggest negative effects on body esteem both cross-sectionally (12, 16) and over time (17, 18), with stronger effects in girls than boys. Studies that used broad measures of bullying also suggested associations with disordered eating (19, 20). Bullying often co-occurs with disordered eating, but it is not at all clear whether it is a risk factor or predicts such problems (21).
The aim of the current study is to test whether broadly defined bullying—rather than specific appearance or weight-related teasing—is a risk factor for eating disorder symptoms. The study uses a representative sample repeatedly assessed to test whether bullying increases risk for eating disorder symptoms after accounting for preexisting levels of eating disorder symptoms. This design allows us to test if observed effects on eating disorder symptoms are a direct effect of bullying or mediated by the changes to emotional symptoms that are known to increase in response to bullying. We hypothesize that victims will be at increased risk for eating disorder symptoms and that a portion of this effect will be accounted for by increases in negative affect. This hypothesis is based on the previous evidence on the effects of weight/body-related teasing (13, 22), associations between bullying and eating/weight outcomes (18, 19), and the effects of bullying on a range of related childhood/adolescent outcomes (5, 6, 23). Finally, as the prevalence estimates of both bullying involvement and eating disorder outcomes vary by sex (3, 15, 24, 25) we will test whether sex differences exist in any observed associations.
Finally, few studies to date have considered the perpetrators of bullying – the bullies themselves. Bullies have been reported to enjoy high social standing and low levels of emotional distress while having more conduct related problems (26). At the same time, the need to solidify one’s status by harming or humiliating others, may be indicative of low self-esteem or poor self-image (27). Furthermore, bullies commonly report regret following bullying incidents, even if this is not sufficient to change their future behavior (28). Given these findings, we predict bullies may also display increased disordered eating.
Methods and Materials
Participants
The Great Smoky Mountains Study (GSMS) is a longitudinal study of the development of psychiatric disorders and the need for mental health services in rural and urban youth (29). A representative sample of three cohorts of children, age 9, 11, and 13 at intake, was recruited from 11 counties in western North Carolina. All children scoring above a predetermined cut point (the top 25% of the total scores) on a screener, plus a 1 - in - 10 random samples of the remaining 75% of the total scores, were recruited for detailed interviews. This oversampling approach allows us to estimate prevalence of common psychiatric disorders. By applying weights inversely proportional to selection probability, results are unbiased and representative of the population (30). About 8% of the area residents and the sample are African American, less than 1% are Hispanic, and 3% are American Indian. Of all participants recruited, 80% (N=1420) agreed to participate. Participants were assessed annually to age 16 then again at ages 19, 21 and 25. Across all waves, participation rates averaged 84% (range: 74–94%).
Procedures
The parent (biological mother for 83% of interviews) and participant were interviewed by trained interviewers separately until the participant was 16, and participants only thereafter. Before the interviews began, parent and child signed informed consent approved by the Duke University Medical Center Institutional Review Board. Each parent and child received an honorarium for their participation.
Assessment
Childhood bullying involvement
Bullying involvement required the child (or another child in the case of bullies) to be a particular and preferred object of mockery, physical attacks or threats. At each assessment between ages 9 and 16, the child and parent reported on whether the child had been bullied/teased multiple times or bullied others in the 3 months immediately prior to the interview as part of the Child and Adolescent Psychiatric Assessment (CAPA) (31). Participants were categorized as victims, bullies, both (i.e., bully-victims) or neither. A bully-victim group was included rather than simply modeling joint exposure with an interaction term as prior work suggests that this group has a different pattern of correlates and outcomes than either bullies or victims (2, 3, 32–34). Appendix A provides definitions for these categories as well as interview probes uses. Being bullied or bullying others was counted if reported by either the parent or the child. If the informant reported that the participant had been bullied or bullied others, then the informant was asked separately how often the bullying occurred in the prior 3 months in the following three settings: home, school, and the community. The focus in the current paper is on peer bullying in the school context only as this is the most common setting for bullying (3). Weight/appearance-related teasing was not assessed separately from bullying. Parent and child agreement (kappa=0.24) was similar to that of other bullying measures (8). Parents were more likely to report their child was either a bully or victim than the child themselves (62.2% and 55.2% of total cases, respectively). We have found similar associations between parent- and child- reporting bullying involvement and long-term outcomes in prior work (2, 3, 35).
Childhood bullying-related covariates
To clarify that bullying involvement is an independent risk factor for eating disorder symptoms, it is necessary to account for preexisting family and individual factors that might predict bullying involvement and eating disorder symptoms. Childhood psychiatric and family hardships variables (except where indicated) were assessed by parent and self-report using the Child and Adolescent Psychiatric Assessment (CAPA) (31). Childhood psychiatric variables included any anxiety disorder, any depressive disorder, any behavioral disorder (conduct disorder, attention-deficit hyperactivity disorder, and oppositional defiant disorder) and any substance abuse or dependence. See (36) for additional details. Four types of family hardships were assessed: low socioeconomic status (SES; including family poverty, low parental educational attainment, and low parental occupational prestige), unstable family structure (indicators include single parent, divorce, parental separation, presence of step-parent, or change in parent structure), family dysfunction (including inadequate parental supervision, domestic violence, parental over involvement, maternal depression, marital relationship characterized by apathy, indifference, or high conflict, and high conflict between parent and child) and maltreatment (including physical abuse, sexual abuse, parental neglect). Additional details are provided in Appendix B. All bully-related covariates have been shown to be related to both bully and victim status in previous work (3).
Eating disorder symptoms and associated features
All items were assessed as part of a module on eating behavior and eating disorders in the Child and Adolescent Psychiatric Assessment (ages 9 to 16) and its upward extension the Young Adult Psychiatric Assessment (ages 19, 21, and 25). The CAPA is a structured diagnostic interview that was used in this epidemiologic study to obtain prevalence estimates of various common childhood disorders. The eating disorder module and associated glossary are included in the appendices. An item was counted as present if reported by either parent or child or both, as is standard in child and adolescent epidemiological studies, approximating the process of combining information from multiple informants in clinical practice. Two-week test-retest reliability of CAPA diagnoses in children aged 10 through 18 is comparable to that of other structured child psychiatric interviews (37, 38). Construct validity as judged by 10 different criteria including comparison to other interviews and ability to predict mental health service use is good to excellent (39).
The CAPA/YAPA eating disorder module assesses all DSM-III-R and IV symptoms of anorexia nervosa and bulimia nervosa. Associated eating disorder related features are also assessed. This included increased appetite or decreased appetite (defined as a definite change in food intake because of an appetite change that has persisted for at least a week) and a preoccupation with eating/food (defined as an unusual and excessive amount of time spent thinking or worrying about food and eating). In GSMS, it was rare for participants to meet full criteria for an eating disorder (40). As such, the focus of this analysis is on individual symptoms of anorexia nervosa and bulimia nervosa and associated features. Two items were too rare to study individually: Amenorrhea (anorexia) and use of medications to control weight (bulimia). Individual items were summed into scales for anorexia, bulimia, and associated features. Finally height and weight measures were collected at each observation and overweight and obesity status was calculated using conventional BMI cutoffs.
Analytic framework
All models used SAS PROC GENMOD to run weighted regression models with robust variance (sandwich type) estimates derived from generalized estimating equations to adjust the standard errors for the stratified design and repeated observations. Sampling weights were applied to ensure results are representative of the population from which the sample was drawn. Odds/means ratios (OR/MR), 95% confidence intervals (CI), and p values are provided for all analyses.
The primary analysis tested whether recent bullying involvement (the participant’s status at the most recent observation) predicted eating disorder symptom/features within childhood/adolescence (ages 9 and 16). This simple model included a dummy variable for comparing the bullying group (bullies, victims, and bully-victims) to a group not involved in bullying and status on the eating disorder symptom/feature at the prior observation (typically 1 year prior). Adjusted models also included covariates for sex, age, and psychiatric status and family adversities at the prior observation (low SES, family instability, family dysfunction, maltreatment, depressive disorders, anxiety disorders, disruptive behavior disorders or substance disorders). A similar series of models tested whether having ever been involved in bullying in childhood or adolescence (ages 9 to 16) predicted eating disorder related outcomes in young adulthood (ages 19, 21, and 25).
Results
Descriptive information
A total of 6674 assessments were completed on the 1420 participants between ages 9 and 16 years (median of 5 observations per subject). This was 84.4% of possible interviews during this period. No bullying involvement was reported at 5800 person-observations, bullying only at 204, being bullied (victims) at 616, and 54 reported both bullying others and being bullied (bully-victim). Neither bullying role nor eating disorder symptoms were associated with missing prior or subsequent interviews (bullies: p = 0.42; victims: p = 0.76; bully-victims: p = 0.10; anorexia symptoms: p = 0.56; bulimia symptoms: p = 0.38; associated features symptoms: p = 0.79).
Both bullies and bully-victims were less likely to be female than those uninvolved in bullying (Bullies: 31.0% vs. 50.1%, p < 0.001; Bully-victims: 22.4% vs. 50.1%, p < 0.001). Victims were not more or less likely to be female (44.2% vs. 50.1%, p = 0.74). Neither victim, bully, nor bully-victim status was related to being overweight or obese, but victims were more likely to be underweight than those uninvolved in bullying (46.7% vs. 36.1%, p <0.001; results available upon request from first author).
Short-term associations
Table 1 provides prevalence estimates of childhood/adolescent (ages 9 to 16) eating disorder symptoms and associated features for different bullying groups (columns 2 to 5) and associations adjusted for status on the eating disorder symptom/feature at the prior observation (columns 6 to 11). Not surprising, the single best predictor of one’s current level of eating disorder symptoms was the level of symptoms at the most recent observation. (e.g., distorted body image at one observation tended to predict a distorted body image at the next observation). By adjusting for prior status, our model is testing whether recent bullying involvement predicts a change in eating disorder symptoms/features from the prior observation.
Table 1.
Associations between childhood bully/victim groups and eating disorder related cognitions and behaviors adjusting for prior status
| Neither N=5816 |
Bully only N=204 |
Victim only N=616 |
Bully/ Victim N=54 |
Victims vs. neither |
Bullies vs. neither |
Bully/victims vs. neither |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | OR/MR (95%CI) | p value | OR/MR (95%CI) | p value | OR/MR (95%CI) | p value | |
| Any anorexia symptom | 5.6 | 8.6 | 11.2 | 22.8 | 1.8 (1.1–3.0) | 0.02 | 1.1 (0.3–3.6) | 0.87 | 4.6 (1.8–11.4) | 0.001 |
| Underweight for height/age | 2.2 | 1.1 | 4.0 | 0.0 | 2.2 (1.0–5.0) | 0.05 | 0.8 (0.3–1.9) | 0.62 | -- | -- |
| Fear of gaining weight | 1.5 | 2.3 | 6.0 | 6.0 | 3.8 (2.0–7.1) | <0.001 | 0.9 (0.2–4.3) | 0.88 | 4.3 (1.6–11.9) | 0.005 |
| Distorted body image | 2.6 | 6.3 | 3.4 | 18.1 | 1.1 (0.5–2.5) | 0.85 | 1.7 (0.4–7.8) | 0.53 | 7.6 (2.5–22.4) | <0.001 |
| Any bulimia symptom | 17.6 | 30.8 | 27.9 | 28.4 | 1.5 (1.1–2.1) | 0.007 | 1.7 (1.0–2.7) | 0.04 | 1.7 (0.6–5.2) | 0.34 |
| Binge eating | 0.4 | 0.9 | 1.6 | 4.8 | 4.6 (1.5–14.8) | 0.01 | 2.3 (0.6–8.8) | 0.22 | 14.2 (4.0–50.8) | <0.001 |
| Attempts to cut weight | 17.0 | 29.3 | 26.1 | 24.9 | 1.5 (1.1–2.0) | 0.02 | 1.6 (1.0–2.6) | 0.07 | 1.5 (0.4–4.9) | 0.54 |
| Diet | 7.8 | 18.8 | 13.8 | 19.8 | 1.6 (1.0–2.4) | 0.04 | 2.3 (1.1–4.8) | 0.03 | 2.9 (0.9–9.3) | 0.08 |
| Exercise | 14.1 | 24.6 | 22.4 | 9.9 | 1.5 (1.1–2.1) | 0.01 | 1.6 (0.9–2.8) | 0.12 | 0.5 (0.1–1.9) | 0.33 |
| Vomiting | 0.3 | 0.3 | 0.2 | 2.4 | 0.9 (0.2–3.2) | 0.83 | 0.5 (0.0–8.5) | 0.63 | 9.3 (1.7–50.2) | 0.01 |
| Overconcern with body | 1.9 | 5.3 | 8.0 | 9.6 | 3.6 (2.2–6.0) | <0.001 | 1.9 (0.3–11.8) | 0.51 | 5.6 (2.6–12.1) | <0.001 |
| Any associated features | 28.2 | 43.3 | 42.5 | 33.6 | 1.8 (1.4–2.3) | <0.001 | 1.8 (1.1–3.0) | 0.02 | 1.3 (0.5–2.9) | 0.61 |
| Preoccupied with eating | 0.8 | 4.1 | 4.9 | 4.8 | 6.1 (3.0–12.5) | <0.001 | 5.6 (1.3–23.6) | 0.02 | 6.0 (2.0–17.6) | 0.001 |
| Decreased appetite | 7.8 | 12.9 | 13.6 | 15.5 | 1.9 (1.2–2.9) | 0.003 | 1.6 (0.7–4.1) | 0.28 | 2.4 (0.6–10.2) | 0.24 |
| Increased appetite | 20.7 | 28.1 | 28.0 | 14.5 | 1.5 (1.1–2.0) | 0.01 | 1.4 (0.8–2.3) | 0.22 | 0.6 (0.2–1.6) | 0.29 |
All bullying groups were at increased risk for reporting eating disorder symptoms or associated features as compared to those uninvolved in bullying. Victims of bullying were at increased risk for reporting a symptom of anorexia, bulimia, or an associated feature. Specific symptoms that victims were at risk for included fear of gaining weight, failing to maintain weight, binge eating, a preoccupation with food/eating, and changes in appetite. Bully-victims were only at increased risk for reporting an anorexic symptom, but they did have elevated prevalence of specific bulimic symptoms, namely binge eating, use of vomiting to control weight, or overconcern with body shape/weight. Finally, bullies were at risk for both bulimic symptoms and associated features.
Including all individual items and bullying groups, 17 of 34 independent tests of associations were statistically significant. The likelihood of this occurring by chance is 4.1×10−14, suggesting this is nonrandom.
This pattern of associations is suggestive. It is necessary, however, to account for preexisting individual and family factors that might increase risk for both bullying involvement and eating disorder symptoms/features (possible confounders). Table 2 presents results from models testing associations between bullying and these outcomes adjusted for sex, preexisting individual psychiatric problems (depression, anxiety, behavior problems and substance use), preexisting family adversities (maltreatment, family instability, family dysfunction, and low SES), in addition to the covariates from the simple models. Associations between bullying groups and the likelihood of having any symptoms/features were largely unchanged. A few individual associations were no longer statistically significant (victims and binge-eating). Figure 1 provides that adjusted mean scores for sum scales of anorexic and bulimic symptoms and associated features within childhood/adolescence by bullying group. Supplemental figure 1 provides adjusted mean scores for the sum scales when the sample is restricted to those with no eating disorder symptoms at the prior wave. This analysis specifically tests whether bullying predicts new symptoms in previously asymptomatic individuals. The pattern of results is similar to that observed for the entire sample.
Table 2.
Associations between childhood bully/victim groups and eating disorder symptoms/features adjusted for sex, age, race, prior levels of eating symptoms/features, preexisting psychiatric status and family adversities
| Victims vs. neither | Bullies vs. neither | Bully/victims vs. neither | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR/MR (95%CI) | p value | Sig. Covariates |
OR/MR (95%CI) |
p value | Sig. Covariates |
OR/MR (95%CI) | p value | Sig. Covariates |
|
| Any anorexia symptom | 1.9 (1.2–3.2) | 0.01 | 1,2,5,8,11 | 1.3 (0.4–3.2) | 0.64 | 1,2,5,8,11 | 5.7 (2.0–16.7) | 0.001 | 1,2,5,8,11 |
| Underweight for height/age | 2.1 (0.9–5.1) | 0.09 | 1,2,6 | 0.8 (0.2–2.7) | 0.73 | 1,2,6 | -- | -- | |
| Fear of gaining weight | 4.5 (2.5–8.0) | <0.001 | 1,8 | 1.2 (0.4–3.8) | 0.74 | 1,8 | 4.9 (1.2–19.3) | 0.02 | 1,8 |
| Distorted body image | 1.1 (0.5–2.3) | 0.89 | 1,2,5,8 | 2.1 (0.4–10.0) | 0.35 | 1,2,5,8 | 8.2 (2.4–28.5) | <0.001 | 1,2,5,8 |
| Any bulimia symptom | 1.5 (1.1–2.1) | 0.02 | 1,2,11 | 1.8 (1.1–3.0) | 0.03 | 1,2,11 | 1.6 (0.5–5.4) | 0.44 | 1,2,11 |
| Binge eating | 3.7 (1.1–12.0) | 0.03 | 3 | 2.1 (0.5–8.2) | 0.31 | 3 | 11.1 (3.1–40.3) | <0.001 | 3 |
| Attempts to cut weight | 1.4 (1.0–2.0) | 0.04 | 1,2,11 | 1.7 (1.0–2.9) | 0.05 | 1,2,11 | 1.4 (0.4–5.0) | 0.64 | 1,2,11 |
| Diet | 1.5 (1.0–2.4) | 0.07 | 1 | 2.5 (1.1–5.6) | 0.02 | 1 | 2.9 (0.9–9.9) | 0.08 | 1 |
| Exercise | 1.5 (1.1–2.2) | 0.03 | 1,2,11 | 1.7 (0.9–3.1) | 0.10 | 1,2,11 | 0.5 (0.1–1.9) | 0.28 | 1,2,11 |
| Vomiting | 0.7 (0.1–4.4) | 0.72 | 1,3,8,9 | 1.2 (0.2–8.6) | 0.84 | 1,3,8,9 | 42.5 (6.6–271.5) | <0.001 | 1,3,8,9 |
| Overconcern with body | 3.8 (2.3–6.3) | <0.001 | 1,8 | 2.5 (0.6–10.6) | 0.22 | 1,8 | 5.6 (2.1–15.1) | <0.001 | 1,8 |
| Any associated features | 1.7 (1.3–2.2) | <0.001 | 1,2,6 | 1.7 (1.1–2.8) | 0.03 | 1,2,6 | 1.2 (0.6–2.8) | 0.60 | 1,2,6 |
| Preoccupied with eating | 4.4 (2.3–8.4) | <0.001 | 1,3,6,9 | 6.0 (1.4–26.0) | 0.02 | 1,3,6,9 | 4.4 (1.2–15.3) | 0.02 | 1,3,6,9 |
| Decreased appetite | 2.2 (1.4–3.5) | <0.001 | 1,3 | 2.1 (0.8–5.2) | 0.12 | 1,3 | 3.5 (0.8–14.5) | 0.09 | 1,3 |
| Increased appetite | 1.4 (1.0–1.8) | 0.05 | 1,2,3 | 1.2 (0.8–2.0) | 0.39 | 1,2,3 | 0.5 (0.2–1.3) | 0.16 | 1,2,3 |
Bolded ORs significant at p<0.05. OR = odds ratio; 95%CI=95 percent confidence interval. Too few participants used medications to control weight or reported amenorrhea for these analyses. Childhood psychiatric and family hardships and other covariates: 1=Sex; 2=Race; 3=Age; 4 = Low SES; 5 = Family instability; 6 = Family dysfunction; 7 = Maltreatment; 8 = Depressive disorders; 9 = Anxiety disorders; 10 = Disruptive disorders; 11 = Substance disorder.
Figure 1.
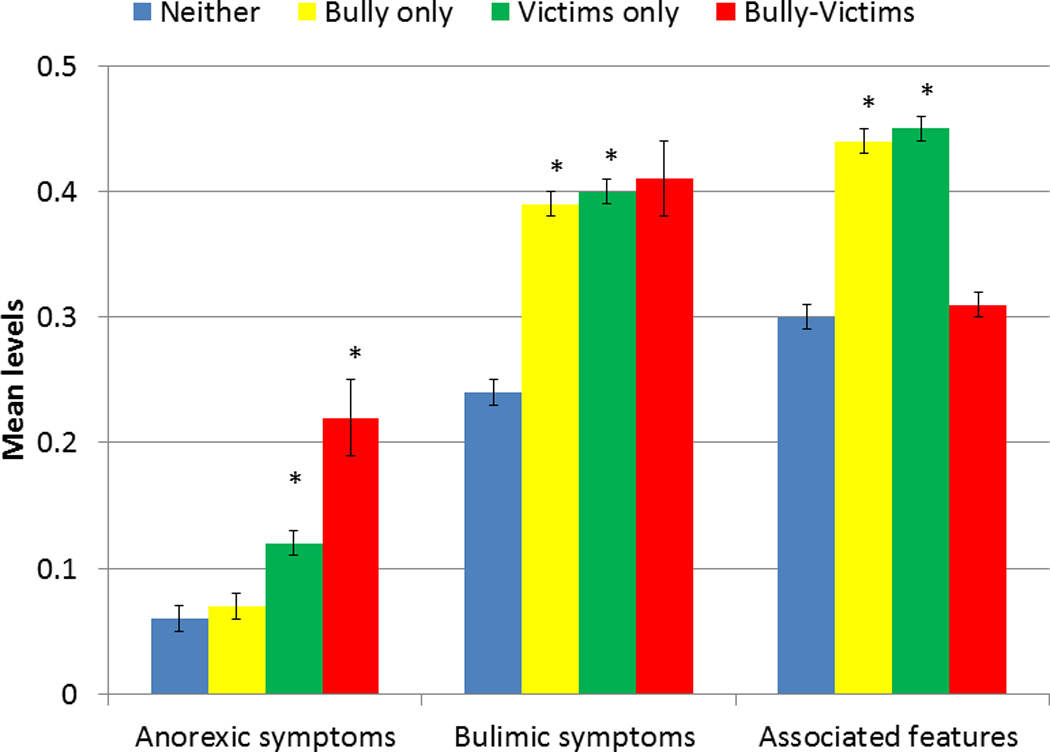
Adjusted means scores for sum scales of eating disorder symptoms/features within childhood and adolescence by bully/victims status. Means are adjusted for prior levels of eating symptoms/features as well as sex, race, age, and preexisting psychiatric status and family adversities. Bars indicate the standard error of the mean. Starred bars indicate groups that are different from those uninvolved in bullying (see table 2 for means ratios, confidence intervals and p values).
Are these associations sex-specific?
The most common significant covariate in multivariable models was sex. It is not surprising that prevalence estimates of these outcomes vary by sex, but do the associations between bullying and eating disorder related outcomes vary between boys and girls? To test for moderation by sex, all models in table 2 were rerun including an interaction term between sex and bully status. There was not evidence to suggest widespread moderation by sex: the interaction terms were not significant for any of the summary scales (9 models) and only two of the individual indicators (34 models), consistent with chance findings.
Are these associations mediated by changes in emotional distress?
We hypothesized that these associations could be explained in part by the well-established emotional sequelae of bullying involvement such as anxiety or depressive symptoms. This is particularly the case with victims and bully-victims who are at risk for elevated depression and anxiety (3, 6).
Five criteria had to be met to demonstrate mediation by either anxiety or depressive symptoms: 1) the bullying group was associated with the outcome; 2) the bullying group was associated with mediator (table 4, column 1); 3) In models adjusting for the bullying group, the mediator was associated with outcome (column 2); 4) In models adjusting for mediator, the association between the bully group and outcome was either no longer statistically significant or attenuated (column 3); and 5) A statistically significant indirect path existed between the bully group variable and the eating disorder outcome through the mediator, as measured by the Sobel test (41) (column 4). Table 4 and appendix C tested mediation of the associations between bully group and different symptom scales by depressive and anxiety symptoms, respectively. In every case, the indirect path from bullying status to the eating disorder symptom scale was statistically significant. This is consistent with a common pathway by which bully status may affect eating disorder symptoms through emotional symptoms.
Table 4.
Tests of depressive symptoms as a mediator of the association between bullying groups and eating disorder symptoms/features
| 1. Predictors to mediator | 2. Mediator to outcome |
3. Predictor to Outcome |
4. Sobel test | ||
|---|---|---|---|---|---|
| Predictor | Outcome | β (SE) | β (SE) | β (SE) | p |
| Victim | Anorexic symptoms | 0.45 (0.09)§ | 0.35(0.05)§ | 0.38 (0.23) | <0.001 |
| Victim | Bulimic symptoms | 0.45 (0.09)§ | 0.18 (0.03)§ | 0.35 (0.13)‡ | <0.001 |
| Victim | Ass. Features | 0.45 (0.09)§ | 0.47 (0.03)§ | 0.11 (0.08) | <0.001 |
| Bullies | Bulimic symptoms | 0.61 (0.13)§ | 0.18 (0.03)§ | 0.36 (0.27) | <0.001 |
| Bullies | Ass. Features | 0.61 (0.13)§ | 0.47 (0.03) | 0.15 (0.16) | <0.001 |
| Bully-victims | Anorexic symptoms | 0.85 (0.18)§ | 0.33(0.05)§ | 0.85 (0.43)† | <0.001 |
Models were tested with Poissona regression.
Columns numbered 2 and 3 provide results from models in which both predictor and potential mediator predicted eating outcome status. Models adjusted for demographics, prior levels of eating symptoms/features, prior psychiatric status and family adversities. Sobel test assess significance of indirect pathway.
P≤0.05;
P≤0.01;
P≤0.0001.
Long-term associations
Finally, do these apparent effects of bullying on eating disorder symptoms persist long-term into adulthood? Here, our goal was to test whether bullying involvement was a risk factor for problems in young adulthood beyond one’s childhood status on eating disorder related measures. Table 3 presents results predicting sum scales of young adult (ages 19, 21, and 25) eating disorder symptoms and associated features from childhood bullying involvement (ages 9 to 16). The first set of models is only adjusted for childhood levels of disordered eating sum scales. The second set adjusts for prior status, but also childhood psychiatric status and family adversities. Overall, there was little evidence that bullying involvement is a risk factor beyond childhood status on eating disorder symptoms.
Table 3.
Associations between childhood bully/victim groups and young adult eating disorder related behaviors and cognitions (ages 19, 21, and 25)
| Victims vs. neither | Bullies vs. neither | Bully/victims vs. neither | ||||
|---|---|---|---|---|---|---|
| MR (95%CI) | p value | MR (95%CI) | p value | MR (95%CI) | p value | |
| Total anorexia symptoms | ||||||
| Adjusted for childhood status | 0.9 (0.5–1.6) | 0.68 | 1.4 (0.4–4.3) | 0.58 | 1.0 (0.6–1.6) | 0.88 |
| Adjusted for psychiatric status and adversities | 0.9 (0.5–1.7) | 0.71 | 1.7 (0.7–4.1) | 0.29 | 1.1 (0.7–1.9) | 0.69 |
| Total bulimia symptoms | ||||||
| Adjusted for childhood status | 0.8 (0.6–1.2) | 0.38 | 1.2 (0.7–2.1 | 0.59 | 0.8 (0.4–1.7) | 0.60 |
| Adjusted for psychiatric status and adversities | 1.0 (0.7–1.5) | 0.90 | 1.6 (0.9–3.0) | 0.12 | 1.3 (0.5–3.4) | 0.57 |
| Total associated features | ||||||
| Adjusted for childhood status | 1.3 (1.0–1.8) | 0.08 | 1.3 (0.7–2.5) | 0.42 | 1.7 (1.2–2.6) | 0.01 |
| Adjusted for psychiatric status and adversities | 1.3 (1.0–1.8) | 0.09 | 1.3 (0.7–2.6) | 0.39 | 1.5 (0.9–2.6) | 0.09 |
Of the total young adult observations, 1993 involved participants never involved in bullying, 243 involved participants that were bullies only, 774 involved victims only, and 205 involved bully-victims. Bolded MRs significant at p<0.05. OR = means ratio; 95%CI=95 percent confidence interval. Childhood psychiatric and family hardships and other covariates include sex, low SES, family instability, family dysfunction, maltreatment, depressive disorders, suicidality, anxiety disorders, disruptive disorders, substance disorders, and age.
Discussion
Eating disorders are relatively rare but even subthreshold presentations are associated with significant morbidity and impairment (24, 25). This study used a community sample repeatedly assessed to test whether symptoms of eating disorders increase following bullying involvement. All bullying groups – victims, bullies, and bully-victims – saw increases in at least one type of eating disorder symptom even after accounting for prior eating problems and preexisting psychiatric status and family adversities. Victims displayed the most pervasive pattern with increases in anorexic and bulimic symptoms as well as associated features. Bully-victims had high prevalence of both binge eating and vomiting, and victims were at increased risk for binge eating. In all cases there was evidence that these associations might be mediated by increased depressive and anxiety symptoms. Childhood/adolescent bullying involvement, however, did not increase risk for eating problems in young adulthood.
The findings in relation to victims and bully-victims should not be surprising given previous evidence on the effects of weight/body-related teasing (13, 22), associations between bullying and eating/weight outcomes (18, 19), and the effects of bullying on a range of related childhood/adolescent outcomes (5, 6, 23). At the same time, the strength of our findings rests on the following features of this study. First, the repeated assessments across childhood and adolescence allowed us to predict changes in eating disorder outcomes associated with recent bullying involvement. As such, all analyses accounted for the most potent predictor of current behavior, namely, past behavior. Second, the prospective design also allowed us to account for preexisting individual and family factors that might increase risk for both bullying involvement and eating disorder outcomes. This allowed us to make the strong inferences about bullying playing predicting subsequent eating disorder outcomes within the context of an observational study. Our distinction between victims and bully-victims allowed us to identify a small group at high risk of problems that are of greatest clinical concern (binge eating and vomiting). Finally, studying this in the context of a broader study of emotional and behavioral functioning allowed us to test mood changes as a candidate mediator of the observed associations. Together, these considerations allowed us to build on our understanding of how being bullied affects eating disorder outcomes.
The finding of increased risk of bulimic symptoms and associated features for bullies is both surprising and novel. Bullies, like victims and bully-victims, had increased eating disorder outcomes, despite being perpetrators and presumably seeing bullying as way to access resources. More surprisingly, observed associations were not attenuated in models accounting for preexisting status, suggesting the experience of bullying itself may affect subsequent behaviors. This presents a few nonexclusive explanations. First, weight loss efforts may be strategies to maintain the social influence/dominance acquired through bullying. If bullying is viewed as a tool of social control, then eating behaviors and cognitions may be an extension of these efforts to master oneself and one’s environment. Second, the experience of criticizing/teasing others (possible weight or body-related) may sensitize bullies to their own physical attributes and shortcomings. Third, bullies may experience regret or guilt following bullying incidents and this contributes to impulsive eating behaviors and cognitions. Finally, bullying others may be triggered by experiences (unmeasured here) that adversely affect one’s self-image. At the minimum, these findings suggest that the experience of bullies may be more complex than previously suggested and simple notions of ‘hale and hearty’ perpetrators are incomplete.
Two other surprising findings were the lack of evidence of sex-specific associations and the lack of long-term effects. In this study, bullies and bully-victims were more likely to be boys and it is well-established that eating problems, weight loss efforts, and negative body-image are more common in females (25). Despite the mismatch of sex differences between the prevalence of the risk factor and outcome, the associations were similar for males and females in this study. The absence of sex differences serves as a useful corrective against assessment or treatment planning based on gender-typical expectations.
Finally, the bullying-related increased risk for eating problems in adolescence did not extend into young adulthood. This is surprising as we have observed long-term effects of bullying on emotional functioning in this sample (3). On the one hand, it is relatively uncommon for childhood risk factors to affect long-term functioning. It is possible that adult eating disorder symptoms are affected by a more proximal set of risk factors, than is the case for emotional problems. It is also still possible (and perhaps likely) that bullying involvement in adulthood may affect eating outcomes. This should be a priority area of work for prospective studies with adult samples.
Strengths and Limitations
As reviewed above, the GSMS has the strengths of prospective design, longitudinal assessment, and representative sampling. In addition, the study has maintained consistently high participation rates across time to minimize selective attrition and used multiple informants across childhood and adolescence. Limitations must also be considered. The sample is not representative of the U.S. population with Native Americans overrepresented and African Americans and Latinos underrepresented. The oversampling approach is useful for insuring an adequate number of cases for risk analyses, but does require use of weighting to obtain population-based estimates. The time between assessments was never less than a year, yet both bullying involvement and eating disorder symptoms may vary over shorter periods. Because this is a population-based study, the rates of DSM diagnosable eating disorders are very low. As such, we are unable to study whether the bullying related-changes in eating disorder symptoms results in more children meeting criteria for eating disorders. In looking at these associations, it would be helpful to know the precise nature of the bullying behavior (e.g., weight/body related, physical vs. relational). To the extent that such specific aspect of bullying would have a stronger effect on the outcomes studied here, our findings may underestimate true associations. As an observation cohort study it is not possible to support causal inferences in terms of risk factor-outcome associations (42). Inferences in this study are limited by possible confounding between time-varying predictors (43). Finally, the mediation analysis tested a plausible model of how bullying may affect eating disorder symptoms. At the same time, these results may be bias due to potential confounding of the mediator-outcome association and should be interpreted cautiously.
Eating disorders are costly (44) and incur considerable morbidity and mortality (24, 45). Moreover, bulimia and binge eating disorder lead to impairment and decrements in role attainment in adulthood (46). This study does not suggest that bullying prevention would eliminate eating problems, but it does identify a common, highly visible, childhood experience that may predict such problems for some and exacerbate such problems for others. Bullying can be assessed and monitored by parents, health professionals and school personnel and bullying prevention programs that reduce victimization are available (47). The most successful efforts to reduce bullying typically involve improved supervision and surveillance from school personnel and parents, firm discipline for the perpetrators, and a collective understanding that bullying is not tolerable or a common rite of passage. Finally, bullying involvement (including perpetration) should be part of the assessment armamentarium of clinicians working with patients struggling with eating problems. Cognitive and emotional responses to such experiences provide a clear target for established cognitive-behavioral treatment strategies.
Supplementary Material
Supplemental Figure 1. Adjusted means scores for sum scales of eating disorder symptoms/features within childhood and adolescence by bully/victims status for those with no eating disorder symptoms at the prior wave. Means are adjusted for sex, race, age, and preexisting psychiatric status and family adversities. Bars indicate the standard error of the mean. Starred bars indicate groups that are different from those uninvolved in bullying (see table 2 for means ratios, confidence intervals and p values).
Acknowledgements
The work presented here was supported by the National Institute of Mental Health (MH63970, MH63671, MH48085, and MH080230), the National Institute on Drug Abuse (DA/MH11301), NARSAD (Early Career Award to First Author), the William T. Grant Foundation, and the Economic and Social Research Council (ESRC) in the UK (ES/K003593/1).
Footnotes
Financial Disclosures
Dr. Bulik is a consultant for Shire Pharmaceuticals. No other authors report a biomedical financial interest or potential conflict of interest.
No authors have any conflicts of interest to report.
Contributor Information
William E. Copeland, Department of Psychiatry and Behavioral Sciences at Duke Medical Center.
Cynthia M. Bulik, Department of Psychiatry and the Department of Nutrition at the University of North Carolina at Chapel Hill and in the Department of Medical Epidemiology and Biostatistics at the Karolinska Institutet, Stockholm, Sweden.
Nancy Zucker, Department of Psychiatry and Behavioral Sciences at Duke Medical Center.
Dieter Wolke, Department of Psychology and Division of Mental Health and Well-being at the University of Warwick.
Suzet Tanya Lereya, Department of Psychology and Division of Mental Health and Well-being at the University of Warwick.
E. Jane Costello, Department of Psychiatry and Behavioral Sciences at Duke Medical Center.
References
- 1.Olweus D. Bullying at school: What we know and what we can do. Wiley-Blackwell; 1993. [Google Scholar]
- 2.Wolke D, Copeland WE, Angold A, Costello E. Impact of Bullying in Childhood on Adult Health, Wealth, Crime and Social Outcomes. Psychological Science. 2013;24(10):1958–1970. doi: 10.1177/0956797613481608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Copeland W, Wolke D, Angold A, Costello E. Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence. JAMA Psychiatry. 2013:1–8. doi: 10.1001/jamapsychiatry.2013.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sourander AMD, Multimaki PMD, Nikolakaros GMD, Haavisto AMD, Ristkari TMNS, Helenius HMS, et al. Childhood Predictors of Psychiatric Disorders Among Boys: A Prospective Community-Based Follow-up Study From Age 8 Years to Early Adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(8):756–767. doi: 10.1097/01.chi.0000164878.79986.2f. [DOI] [PubMed] [Google Scholar]
- 5.Gini G, Pozzoli T. Association between bullying and psychosomatic problems: A meta-analysis. Pediatrics. 2009;123(3):1059–1065. doi: 10.1542/peds.2008-1215. [DOI] [PubMed] [Google Scholar]
- 6.Reijntjes A, Kamphuis JH, Prinzie P, Telch MJ. Peer victimization and internalizing problems in children: A meta-analysis of longitudinal studies. Child Abuse & Neglect. 2010;34(4):244–252. doi: 10.1016/j.chiabu.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Brunstein Klomek A, Sourander A, Gould MS. The association of suicide and bullying in childhood to young adulthood: a review of cross-sectional and longitudinal research findings. Canadian Journal of Psychiatry. 2010;55(5):282–288. doi: 10.1177/070674371005500503. [DOI] [PubMed] [Google Scholar]
- 8.Schreier A, Wolke D, Thomas K, Horwood J, Hollis C, Gunnell D, et al. Prospective Study of Peer Victimization in Childhood and Psychotic Symptoms in a Nonclinical Population at Age 12 Years. Arch Gen Psychiatry. 2009;66(5):527–536. doi: 10.1001/archgenpsychiatry.2009.23. [DOI] [PubMed] [Google Scholar]
- 9.Nakamoto J, Schwartz D. Is Peer Victimization Associated with Academic Achievement? A Meta-analytic Review. Social Development. 2010;19(2):221–242. [Google Scholar]
- 10.Thompson JK, Coovert MD, Richards KJ, Johnson S, Cattarin J. Development of body image, eating disturbance, and general psychological functioning in female adolescents: Covariance structure modeling and longitudinal investigations. International Journal of Eating Disorders. 1995;18:221–236. doi: 10.1002/1098-108x(199511)18:3<221::aid-eat2260180304>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 11.Perry DG, Hodges EV, Egan SK. Determinants of chronic victimization by peers. Peer harassment in school: The plight of the vulnerable and victimized. 2001:73–104. [Google Scholar]
- 12.Lunde C, Frisén A, Hwang CP. Is peer victimization related to body esteem in 10-year-old girls and boys? Body Image. 2006;3(1):25–33. doi: 10.1016/j.bodyim.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Menzel JE, Schaefer LM, Burke NL, Mayhew LL, Brannick MT, Thompson JK. Appearance-related teasing, body dissatisfaction, and disordered eating: A meta-analysis. Body Image. 2010;7(4):261–270. doi: 10.1016/j.bodyim.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Eisenberg M, Neumark-Sztainer D. Peer harassment and disordered eating. International journal of adolescent medicine and health. 2008;20(2):155–164. doi: 10.1515/ijamh.2008.20.2.155. [DOI] [PubMed] [Google Scholar]
- 15.Wolke D, Stanford K. Developmental psychology. London: Arnold; 1999. Bullying in school children; pp. 341–360. [Google Scholar]
- 16.Farrow CV, Fox CL. Gender differences in the relationships between bullying at school and unhealthy eating and shape-related attitudes and behaviours. British journal of educational psychology. 2011;81(3):409–420. doi: 10.1348/000709910X525804. [DOI] [PubMed] [Google Scholar]
- 17.Lunde C, Frisén A, Hwang CP. Ten-year-old girls’ and boys’ body composition and peer victimization experiences: Prospective associations with body satisfaction. Body Image. 2007;4(1):11–28. doi: 10.1016/j.bodyim.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Lunde C, Frisén A. On being victimized by peers in the advent of adolescence: Prospective relationships to objectified body consciousness. Body Image. 2011;8(4):309–314. doi: 10.1016/j.bodyim.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 19.Kaltiala-Heino R, RimpelÄ M, Rantanen P, RimpelÄ A. Bullying at school—an indicator of adolescents at risk for mental disorders. Journal of Adolescence. 2000;23(6):661–674. doi: 10.1006/jado.2000.0351. [DOI] [PubMed] [Google Scholar]
- 20.Striegel-Moore RH, Fairburn CG, Wilfley DE, Pike KM, Dohm F-A, Kraemer HC. Toward an understanding of risk factors for binge-eating disorder in black and white women: a community-based case-control study. Psychological Medicine. 2005;35(06):907–917. doi: 10.1017/s0033291704003435. [DOI] [PubMed] [Google Scholar]
- 21.Kraemer H, Stice E, Kazdin A, Offord D, Kupfer DJ. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 22.Thompson JK, Coovert MD. Body image, social comparison, and eating disturbance: A covariance structure modeling investigation. International Journal of Eating Disorders. 1999;26(1):43–51. doi: 10.1002/(sici)1098-108x(199907)26:1<43::aid-eat6>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 23.Zwierzynska K, Wolke D, Lereya TS. Peer victimization in childhood and internalizing problems in adolescence: a prospective longitudinal study. Journal of Abnormal Child Psychology. 2013;41(2):309–323. doi: 10.1007/s10802-012-9678-8. [DOI] [PubMed] [Google Scholar]
- 24.Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents: results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry. 2011;68(7):714. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The Prevalence and Correlates of Eating Disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juvonen J, Graham S, Schuster MA. Bullying among young adolescents: the strong, the weak, and the troubled. Pediatrics. 2003;112(6):1231–1237. doi: 10.1542/peds.112.6.1231. [DOI] [PubMed] [Google Scholar]
- 27.Cook CR, Williams KR, Guerra NG, Kim TE, Sadek S. Predictors of bullying and victimization in childhood and adolescence: A meta-analytic investigation. School Psychology Quarterly. 2010;25(2):65. [Google Scholar]
- 28.Borg MG. The emotional reactions of school bullies and their victims. Educational Psychology. 1998;18(4):433–444. [Google Scholar]
- 29.Costello EJ, Angold A, Burns B, Stangl D, Tweed D, Erkanli A, Worthman C. The Great Smoky Mountains Study of Youth: Goals, designs, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 30.Pickles A, Dunn G, Vazquez-Barquero J. Screening for stratification in two-phase ('two-stage') epidemiological surveys. Statistical Methods in Medical Research. 1995;4(1):73–89. doi: 10.1177/096228029500400106. [DOI] [PubMed] [Google Scholar]
- 31.Angold A, Costello E. The Child and Adolescent Psychiatric Assessment (CAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 32.Veenstra R, Lindenberg S, Oldehinkel AJ, De Winter AF, Verhulst FC, Ormel J. Bullying and victimization in elementary schools: A comparison of bullies, victims, bully/victims, and uninvolved preadolescents. Developmental Psychology. 2005;41(4):672–681. doi: 10.1037/0012-1649.41.4.672. [DOI] [PubMed] [Google Scholar]
- 33.Wolke D, Woods S, Bloomfield L, Karstadt L. The Association between Direct and Relational Bullying and Behaviour Problems among Primary School Children. Journal of Child Psychology and Psychiatry. 2000;41(8):989–1002. [PubMed] [Google Scholar]
- 34.Lereya S, Copeland W, Zammit S, Wolke D. Bully/victims: a longitudinal, population-based cohort study of their mental health. European Child & Adolescent Psychiatry. 2015:1–11. doi: 10.1007/s00787-015-0705-5. [DOI] [PubMed] [Google Scholar]
- 35.Copeland WE, Wolke D, Lereya ST, Shanahan L, Worthman C, Costello EJ. Childhood bullying involvement predicts low-grade systemic inflammation into adulthood. Proceedings of the National Academy of Sciences. 2014 doi: 10.1073/pnas.1323641111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative Prevalence of Psychiatric Disorders by Young Adulthood: A Prospective Cohort Analysis From the Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(3):252–261. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Angold A, Costello EJ. A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C) Psychological Medicine. 1995;25:755–762. doi: 10.1017/s0033291700034991. [DOI] [PubMed] [Google Scholar]
- 38.Angold A, Erkanli A, Copeland W, Goodman R, Fisher PW, Costello EJ. Psychiatric Diagnostic Interviews for Children and Adolescents: A Comparative Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(5):506–517. doi: 10.1016/j.jaac.2012.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 40.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 41.Sobel ME. Asymptomic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982:290–312. (S. Leinhardt) [Google Scholar]
- 42.De Stavola BL, Nitsch D, dos Santos Silva I, McCormack V, Hardy R, Mann V, et al. Statistical issues in life course epidemiology. American Journal of Epidemiology. 2006;163(1):84–96. doi: 10.1093/aje/kwj003. [DOI] [PubMed] [Google Scholar]
- 43.Diggle P, Heagerty P, Liang K-Y, Zeger S. Analysis of longitudinal data. Oxford University Press; 2002. [Google Scholar]
- 44.Agras WS. The consequences and costs of the eating disorders. Psychiatric Clinics of North America. 2001;24(2):371–379. doi: 10.1016/s0193-953x(05)70232-x. [DOI] [PubMed] [Google Scholar]
- 45.Root TL, Pisetsky EM, Thornton L, Lichtenstein P, Pedersen NL, Bulik CM. Patterns of co-morbidity of eating disorders and substance use in Swedish females. Psychological Medicine. 2010;40(1):105. doi: 10.1017/S0033291709005662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kessler R, Shahly V, Hudson J, Supina D, Berglund P, Chiu W, et al. A comparative analysis of role attainment and impairment in binge-eating disorder and bulimia nervosa: results from the WHO World Mental Health Surveys. Epidemiology and psychiatric sciences. 2013:1–15. doi: 10.1017/S2045796013000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ttofi MM, Farrington DP. Effectiveness of school-based programs to reduce bullying: a systematic and meta-analytic review. J Exp Criminol. 2011;7(1):27–56. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Adjusted means scores for sum scales of eating disorder symptoms/features within childhood and adolescence by bully/victims status for those with no eating disorder symptoms at the prior wave. Means are adjusted for sex, race, age, and preexisting psychiatric status and family adversities. Bars indicate the standard error of the mean. Starred bars indicate groups that are different from those uninvolved in bullying (see table 2 for means ratios, confidence intervals and p values).


