Abstract
Objective
Emergency Medical Services (EMS) workers are shift workers in a high-risk, uncontrolled occupational environment. EMS-worker fatigue has been associated with self-reported injury, but the influence of extended weekly work hours is unknown.
Methods
A retrospective cohort study was designed using historical shift schedules and occupational injury and illness reports. Using multilevel models, we examined the association between weekly work hours, crew familiarity, and injury or illness.
Results
In total, 966,082 shifts and 950 reports across 14 EMS agencies were obtained over a 1-3 year period. Weekly work hours were not associated with occupational injury or illness. Schedule characteristics that yield decreased exposure to occupational hazards, such as part-time work and night work, conferred reduced risk of injury or illness.
Conclusions
Extended weekly work hours were not associated with occupational injury or illness. Future work should focus on transient exposures and agency-level characteristics that may contribute to adverse work events.
Keywords: Emergency Medical Services, Shift work, Occupational injury
Introduction
The average weekly hours of work for all occupations in the US is approximately 39 hours.[2014a] As a process of scheduling or voluntary overtime, healthcare workers commonly work beyond the weekly average, contributing to shorter sleep duration, increased sleepiness, and fatigue.[Sallinen and Kecklund 2010, Virtanen, et al. 2009] Evidence links extended weekly work hours and extended shifts (e.g., ≥12-hours) to increased risks of poor worker performance, health, and safety.[Caruso 2014, Williamson, et al. 2011] Emergency Medical Services (EMS) clinicians typically work 12 or 24-hour shifts. Approximately half of EMS workers exceed 45 hours of work per week, with many working more than one EMS job.[Brown, et al. 2002a, Frakes and Kelly 2007] More than half of EMS workers also report work-related fatigue.[Patterson, et al. 2010b, Patterson, et al. 2012a] Concern for EMS shift work, shift length, and work hours has risen, due in part to recent data linking EMS worker fatigue to negative safety outcomes.[Patterson, et al. 2012a, Patterson, et al. 2012b] Despite these data, research on the link between EMS worker weekly hours, shift work, and occupational injury is limited.
EMS workers are vulnerable to negative safety outcomes. The setting for work can be hazardous and the workload and demands are often unpredictable. Over half of EMS workers report being assaulted at work, and 5-10% of all calls involve a violent patient.[Corbett, et al. 1998, Grange and Corbett 2002, Mock, et al. 1998] Exposure to blood and infectious illness was reported by 20% of providers nationally in a single year.[Boal, et al. 2010] Greater than 1% of EMS providers reported being involved in an ambulance collision in just a 3-month time period.[Cone, et al. 2015]
Approximately 20,000 non-fatal injuries are reported each year in the EMS setting; a rate three times that of all private industry occupations.[Maguire, et al. 2005, Maguire and Smith 2013, Reichard, et al. 2011] The rate of non-fatal injuries is disproportionately high in EMS compared to other public safety sectors with similar risk profiles, such as police or fire.[Suyama, et al. 2009] While shift work is a known factor in safety outcomes for other occupations, its role in safety for EMS workers remains unclear.[Patterson, et al. 2012b]
There is reason to believe that lack of familiarity between EMS workers combined with excessive fatigue due to extended shift work may result in greater incidence of work related injury.[Patterson, et al. 2011, Salas and Fiore 2004] Communication and trust are key factors in teamwork and team performance.[Baker, et al. 2007, Salas, et al. 2005] When fatigued, communication and trust may be negatively affected, raising the risk of a negative outcome.[Anderson and Dickinson 2010] EMS workers have limited opportunities to develop positive teamwork behaviors due to working on average with four different partners every 10 shifts.[Patterson, et al. 2011, Patterson, et al. 2012c] Lack of familiarity between teammates/partners is associated with poor performance and negative outcomes.[Foushee, et al. 1986, NTSB 1994, Thomas and Petrilli 2006]
The objective of this work is to determine if occupational injury is associated with weekly hours of work for EMS providers, while controlling for familiarity between EMS crewmembers (teammates). We hypothesize that increased weekly work hours would significantly increase the likelihood of occupational injury and illness.
Materials and Methods
This study followed a retrospective cohort study design, utilizing information available from 14 geographically distinct EMS agencies with 37 individual base sites. Participating agencies provided a convenience sample of historical scheduling records and occupational injury and illness reports for a period of 1-3 years. The unit of analysis was a work shift. Each shift was characterized as exposed or unexposed to extended weekly work hours based on the hours of work in the 7 days preceding each shift (weekly work hours).
Study Protocol
Agencies provided historical administrative records of employee shift schedules and Occupational Safety Health Association (OSHA) occupational injury or illness reports. OSHA reports were matched to specific work shifts using date, location (agency/base site), and employee identification number. If the employee and location matched the injury record but the date did not, the report was matched to the employee's most proximal previous work shift provided the shift occurred within 4 days of the reported injury or illness. The limit of 4 days was used to maximize the likelihood that the OSHA report be matched to the shift on which the incident occurred. Shift records were excluded when designated for non-clinical tasks, such as billing staff or vehicle service technician.
Outcome Variable of Interest
The outcome of interest was OSHA-reportable work-related injury or illness. We measured injury and illness using a standardized reporting record of injuries; the OSHA form 300 log of work-related injuries and illnesses (available at https://www.osha.gov/recordkeeping/RKforms.html). The OSHA form 300A was obtained from each of the participating EMS agencies for all 37 base sites for each year of participation. The OSHA form contains a description of the event along with the assignment of the event into specific categories of injury or illness. Two investigators reviewed each reported injury or illness and determined if the report met the OSHA definitions and criteria for occupational injury or illness. Reports were excluded if they did not meet the benchmark for OSHA recording. We reviewed each record to minimize potential biases that could be present in cases of differential thresholds for reporting injuries or illnesses across agencies and individuals.
Independent Variables of Interest
We extracted all independent variables of interest from historical shift schedules. The primary independent variable of interest was weekly work hours. Weekly work hours was treated as a time-varying covariate and defined as the cumulative hours of work in the 7 days preceding each shift. Weekly work hours was categorized for practical interpretation of the findings, as well as for comparison with prior benchmarking publications.[Alterman, et al. 2013] The categories of weekly work hours were <48 hrs, 48-59 hrs, and ≥60 hrs. Shifts with <48 hrs of work in the previous 7 days were considered the unexposed referent group in the cohort analysis.
The total number of shifts the employee worked with the partner(s) assigned to the shift of the interest in the 8 weeks preceding each shift was calculated and referred to as teammate familiarity. The familiarity variable was categorized using quartiles. The 8 week interval was chosen based on prior literature suggesting that significant decay in the recall of team interactions is observed after 8 weeks.[Jenkins, et al. 2002, Landen and Hendricks 1995]
The shift records were utilized to capture other variables and concepts that could potentially confound the association between weekly work hours and the outcome. These covariates include the time period prior to the shift available for recovery, the proportion of the shift occurring over night hours, part-time vs. full-time employee status, and the number of shifts worked over the past month.
Recovery time was treated as a binary variable - situations where the end of the most recent shift occurred less than 11 hours prior to the shift of interest were considered to have short recovery periods.[Eldevik, et al. 2013] Night hours were defined as hours of work from 10pm until 6am. The proportion of night hours was calculated as the shift duration in hours divided by the number of night hours. Part-time employees were defined in accordance with the Bureau of Labor Statistics (BLS) standard.[2014b] According to the BLS, part-time employees average no more than 34 weekly work hours. We calculated the average hours worked per week for each month of the study – employees averaging at or below 34 hours per week for that month were considered to be part-time employees for all shifts within that month. The number of shifts in a month was calculated as the number of shifts worked in the 4 weeks immediately preceding the shift start date, not including the shift of interest.
Workforce size has been associated with injury reporting in other settings.[Azaroff, et al. 2002, Oleinick, et al. 1995] The number of unique employees working a shift during the midpoint month of data collection was used to estimate the number of workers employed by each agency.
Statistical Analysis
Variables of interest are described using mean and standard deviation when normality is present, and with median and interquartile range otherwise. The rate of OSHA reports was calculated as the number of reports per 100 Full-time Equivalent (FTE). An FTE was defined as 2000 hours of work per year.
Multivariable mixed effects logistic models were constructed for hypothesis testing. The fixed effects were specified as hours of work in the previous 7 days, categorical quartile of familiarity of crew on the shift, binary recovery less than 11 hours, continuous number of shifts in the month, and the percentage of work hours occurring between the hours of 10pm and 6am. A random agency effect was implemented to account for the clustering of EMS workers within agencies and a random worker effect to account for the correlation between repeated measures within worker. The analysis was performed using Stata version 12.1 MP, College Station, TX: StataCorp LP.
The primary outcome was the presence/absence of an OSHA reportable occupational injury or illness. A sensitivity analysis was performed to assess changes in the observed associations after excluding reports classified as illness, to explore the possibility that reports of illness may not share the same relationship between exposure and outcome.
Ethical Statement
This study was reviewed and approved by the University of Pittsburgh Institutional Review Board.
Results
Study Sample
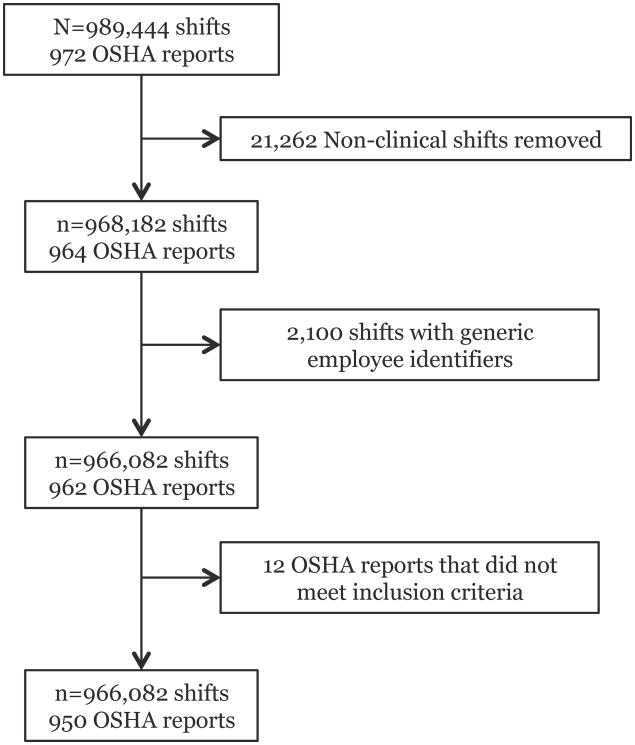
Administrative shift scheduling and injury data was obtained from 14 EMS organizations, ranging in size from 96 to 348 EMS worker employees. Data are representative of 4,382 employees and 966,082 total work shifts (Figure 1). Total workdays varied by organization from 388 to 1,048. EMS workers in this sample averaged 39 hours of work per week (SD 17). (Table I)
Figure 1.
Table I. Sampling frame and agency-level characteristics.
| Years of data | Cumulative hours of work | OSHA reports | OSHA rate (per 100 FTE per Year) | Midpoint workforce size | Hours of work per employee per week (Mean, SD) | |
|---|---|---|---|---|---|---|
| Location | ||||||
| Agency 1 | 2.50 | 1,773,139 | 90 | 10.2 | 348 | 40.0 (15.3) |
| Agency 2 | 1.08 | 219,762 | 23 | 20.9 | 132 | 35.2 (14.9) |
| Agency 3 | 2.50 | 778,834 | 26 | 6.7 | 170 | 33.9 (11.3) |
| Agency 4 | 2.76 | 820,096 | 68 | 16.6 | 145 | 44.0 (20.8) |
| Agency 5 | 2.67 | 832,416 | 20 | 4.8 | 117 | 50.2 (20.7) |
| Agency 6 | 2.91 | 1,600,990 | 136 | 17.0 | 255 | 41.0 (15.5) |
| Agency 7 | 2.91 | 1,097,959 | 51 | 9.3 | 186 | 40.9 (14.9) |
| Agency 8 | 2.52 | 461,899 | 40 | 17.3 | 96 | 38.3 (12.8) |
| Agency 9 | 2.00 | 777,045 | 219 | 56.4 | 255 | 35.6 (19.7) |
| Agency 10 | 2.91 | 718,311 | 36 | 10.0 | 148 | 38.4 (17.5) |
| Agency 11 | 2.85 | 1,179,573 | 50 | 8.5 | 220 | 38.4 (20.9) |
| Agency 12 | 2.91 | 1,015,161 | 23 | 4.5 | 222 | 34.8 (13.9) |
| Agency 13 | 1.82 | 384,328 | 156 | 81.2 | 138 | 33.7 (14.7) |
| Agency 14 | 1.83 | 524,790 | 12 | 4.6 | 174 | 33.9 (19.0) |
| Total | 34.17 | 12,184,303 | 950 | 15.6 | 2,606 | 38.8 (17.0) |
Weekly Work Hours
Among EMS workers in the cohort, the mean weekly work hours was 39 (SD 17) and the mean number of shifts per work week was 3.2 (SD 1.4). Over 1/3 of shifts were worked with the employee having already logged at least 48 cumulative hours of work in the previous 7 days (n=345,595), and over 10% of shifts came after 60 hours of work in the previous 7 days. (Table II)
Table II. Distribution of covariates across exposure categories.
| <48 hours (n=620,487) | 48-59 hours (n=233,221) | ≥60 hours (n=112,374) | Total (n=966,082) | |
|---|---|---|---|---|
| Familiarity (past 8 weeks) | ||||
| Median (P25-75) | 7 (1-20) | 8 (1-19) | 5 (1-17) | 7 (1-19) |
| Hours of recovery | ||||
| Median (P25-P75) | 19 (12-84) | 12 (12-36.5) | 12 (11.5-24) | 16 (12-60) |
| Number of shifts in the month | ||||
| Mean (SD) | 12.1 (4.6) | 13.6 (4.0) | 16.0 (4.8) | 12.9 (4.7) |
| Proportion night hours | ||||
| Mean (SD) | 0.25 (0.29) | 0.29 (0.27) | 0.31 (0.26) | 0.27 (0.28) |
|
| ||||
| Unique employees | 4,382 | 3,562 | 2,810 | 4,382 |
| Part-time employees | 4,380 | 3,332 | 1,551 | 4,380 |
|
| ||||
| Injuries (n (%)) | 637 (0.10) | 202 (0.09) | 111 (0.10) | 950 (0.10) |
| Injuries with work restriction only | 137 (0.02) | 54 (0.02) | 21 (0.02) | 212 (0.02) |
| Injuries requiring time away from work | 91 (0.01) | 22 (0.01) | 8 (0.01) | 121 (0.01) |
Crewmember/Teammate Familiarity
Nearly 75% of shifts (n=715,768) were comprised of a two-person crew, while 17.4% (n=168,090) were single-person assignments. Twenty-three percent of all shifts were staffed by a crew who had not worked together in the previous 8 weeks. The mean number of shifts worked together over an 8-week period was 10 (SD 10), with a median of 7 (IQR 1-19). (Table II)
Injuries and Illnesses
A total of 1,128 occupational illnesses and injuries were documented by the EMS agencies. We matched 86.2% of reports to a historical work shift (n=972). After removal of non-clinical workers and review of eligibility criteria, 950 reports of occupational illness or injury were included in the analysis. The analysis was performed on 705 occupational injuries and 245 occupational illnesses. (Figure 1) Among employees reporting an injury, 27% reported multiple injuries or illnesses. The overall rate of reported injury or illness was 15.6 per 100 FTE, and ranged from 4.5 to 81.2 per 100 FTE across agencies. (Table I)
Hypothesis Testing
Bivariate analyses revealed that none of the covariates of interest were associated with OSHA reports of occupational injury or illness. (Table III) In a multivariate model controlling for other work schedule characteristics, familiarity of crewmembers, time of day, and agency size, weekly work hours were not associated with OSHA report. (Table III)
Table III. Mixed effects logistic regression model results.
| Unadjusted RR Injury | p-Value | Adjusted RR Injury | p-value | |
|---|---|---|---|---|
| Hours of work previous 7 days | ||||
| <48 hrs | Referent | --- | Referent | --- |
| 48-59 hrs | 0.93 (0.79-1.10) | 0.61 | 0.92 (0.78-1.09) | 0.36 |
| ≥60 hrs | 1.04 (0.84-1.28) | 1.12 (0.89-1.41) | 0.33 | |
|
| ||||
| Crewmember Familiarity | ||||
| 0-1 shifts | Referent | --- | Referent | --- |
| 2-7 shifts | 1.04 (0.88-1.23) | 0.63 | 1.05 (0.89-1.25) | 0.54 |
| 8-19 shifts | 1.11 (0.93-1.33) | 1.13 (0.94-1.36) | 0.19 | |
| ≥20 shifts | 1.12 (0.91-1.38) | 1.18 (0.95-1.47) | 0.15 | |
|
| ||||
| Short Recovery (<11 hrs) | 0.93 (0.76-1.13) | 0.46 | 0.95 (0.77-1.17) | 0.60 |
|
| ||||
| Number of shifts in a month | 0.99 (0.97-1.00) | 0.08 | 0.96 (0.94-0.98) | <0.0001 |
|
| ||||
| Proportion of night hours | 0.80 (0.63-1.00) | 0.05 | 0.78 (0.61-0.98) | 0.03 |
|
| ||||
| Employment status | ||||
| Full-time | Referent | --- | Referent | --- |
| Part-time | 0.90 (0.77-1.04) | 0.15 | 0.70 (0.58-0.86) | 0.001 |
|
| ||||
| Midpoint Agency Size(20 person units) | 0.99 (0.88-1.11) | 0.84 | 0.99 (0.87-1.12) | 0.84 |
Familiarity of crewmembers was not significantly associated with the outcome (p=0.44). Part-time worker status was protective against occupational injury or illness (OR 0.70; 95% CI 0.58-0.86). For each additional shift worked in the previous 4 weeks, the odds of an OSHA report decreased by 4% (OR 0.96; 95% CI 0.94-0.98). Results of a model excluding illnesses are very similar. (Appendix A)
Discussion
In this study population of EMS workers and diverse EMS organizations, there was no association between weekly work hours, crewmember familiarity, and occupational injury or illness. Our findings differ from the general population captured via the National Health Interview Survey, which detected an increasing incidence of injury for 40-50, 50-60, and greater than 60 weekly work hours.[Lombardi, et al. 2010] Research of 11,516 nurses, who often face similar shift work challenges to EMS, concluded that working more than 40 hours per week on average was significantly associated with work-related injuries.[Olds and Clarke 2010] Regarding the role of familiarity, our findings show no association between weekly work hours, familiarity, and injury. This differs from what we hypothesized based on findings from previous research.[NTSB 1994] To the best of our knowledge, our study is one of the first to investigate this relationship in an EMS population.
There are several potential explanations for our findings. It is possible that in the EMS setting, work-related exposures other than weekly work hours are more important drivers of adverse workplace events. The occurrence of an occupational injury or illness can be likened to Reason's Swiss cheese model of system accidents.[Reason 2000] Deficits in performance due to prolonged weekly work hour may be mitigated by downstream layers of the model. Layers of defense against an injury or illness may be positive safety culture, certain agency policies, or the presence of equipment designed to encourage safety when lifting and moving patients.[Oginski, et al. 2000]
EMS care can be characterized as intermittent (episodic) in nature, - specifically, EMS work is episodic in that paramedics and other EMS workers perform patient care when dispatched to do so. This care is not scheduled and can be characterized as unpredictable. Care episodes are separated by periods of rest and precipitated by sensory activations such as alarms, lights, and sirens, which may encourage wakefulness.[Tassi, et al. 1992] There may be a correlation between the preferred work schedule of an individual and their tolerance to chronic partial sleep restriction.[Wehrens, et al. 2012] Workers who gravitate to this profession may also maintain vigilance effectively in stressful situations – which may also partially explain the lack of association between familiarity and injury.[Rose 1992]
We observed decreased risk of occupational injury or illness for shifts where the previous week of work included a higher percentage of night hours, and also for shifts worked by part-time employees. Workers on night shifts may be more susceptible to sleepiness, disrupted circadian rhythms, and have less oversight from management.[Kilpatrick and Lavoie-Tremblay 2006] At the same time, EMS workers may receive sufficient rest during overnight shifts to maintain high performance.[Guyette, et al. 2013] Call volume is often lowest during night hours[Channouf, et al. 2007] and exposure to occupational hazards most often occurs when workers are active. This is also relevant when considering the part-time worker finding. Part-time workers are potentially exposed to a lesser extent to the occupational hazards of emergency medical services work.
Shift work, fatigue, and safety are visible and contentious issues in the EMS community. This analysis contributes to the understanding of these issues by examining nearly 1 million shift records and 1,000 reports of occupational illness or injury. Our findings, while in contrast to prior efforts in other settings, raise important questions which merit further research in the EMS domain. Namely – staffing requirements and the safety of those staffing structures vary by population density, service area, and job tasks. What is a safe and sustainable amount of weekly work in each setting, assuming a given workload and cognitive demand? Also, are historical OSHA 300 log records representative of the burden of injury in a workplace? Further research should seek to utilize and grow data sources to inform these questions.
Limitations
This is a secondary analysis of administrative data. The dataset lacks potential explanatory information on work activities, including unit hour utilization (a measure of available ambulances and activations over time), work environment, and agency culture. Important individual confounding variables are also unavailable – such as medical conditions, dietary habits, and sleep behaviors. The dataset lacks providers' certification level and experience in EMS. Previous literature suggests many EMS workers work multiple jobs.[Frakes and Kelly 2007, Patterson, et al. 2012a] Any hours worked outside of agencies participating in data collection are not captured in the analysis. Detail regarding the situation and events surrounding the injuries and illnesses was often missing, precluding potential subgroup analyses.
We consider use of a large dataset of shift schedules as one of several strengths of our study over that of previous research. This may be the largest dataset and analysis of work hours in EMS workers. Our findings suggests that EMS workers work a similar amount of hours per week (39 on average) in comparison to the general working population at their primary job (39 hours). Previous research has relied primarily on self-report and cross-sectional surveys. These prior studies suggest that EMS workers accumulate greater than or equal to 48-hours per week. Specifically, in the LEADS survey (Longitudinal Emergency Medical Technician Attributes and Demographics Study – a national survey of EMS providers constructed by sampling from providers with active national certifications), respondents were asked the number of hours they were available for an EMS response during a typical week. The median value for EMT-Basics was 48.1 hours, compared to 51.8 hours for EMT-Paramedics.[Brown, et al. 2002b] Several studies suggest EMS workers often maintain employment at multiple organizations.[Frakes and Kelly 2007, Patterson, et al. 2012a] Differences between our findings and previous research may be due to lack of capture of all EMS worker shifts. Future studies should determine how to include both secondary and self-report data to obtain the most accurate measurement of weekly work hours.
Research in other settings using OSHA 300 logs suggests that they are commonly an underestimate of the true burden of injury. The degree to which they underestimate injury rates is thought be between 20 and 70%.[Ruser 2008, Tucker, et al. 2014] The extent of underreporting varies widely across occupational setting, and has not been quantified in an EMS setting.[Fan, et al. 2006] Previous studies have found that organizational safety culture is associated with injury reporting. Organizations with negative safety climate had significantly higher rates of underreporting of OSHA eligible injury or illness.[Probst, et al. 2008] We have previously found wide variation in safety climate scores and safety culture as a whole across EMS agencies nationally.[Patterson, et al. 2010a] We observed an 18-fold difference in OSHA reporting rates across the participating EMS organizations. We attempted to remove potential agency-level confounding by including a random-effect for agency in the multivariable model.
Conclusion
Weekly work hours are not associated with OSHA-reportable occupational injury and illness in this national cohort of EMS providers. Future research should explore the impact of momentary exposures such as unit hour utilization, transient sleepiness and fatigue, as well as incorporate information regarding agency policies and safety culture.
Supplementary Material
Acknowledgments
None
Disclosure of Grant Funding: Work performed on this study was supported by a grant from the National Institute for Occupational Safety and Health (NIOSH), Grant #1R21OH010025-01A1.
Footnotes
Institution at which work was performed: University of Pittsburgh, School of Medicine, Department of Emergency Medicine
Authorship Contributions: MDW and PDP conceived the study and acquired the data. All authors contributed to the analysis and interpretation of data. MDW drafted the work. All authors contributed critical revisions and important intellectual content. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics Review and Approval: This study was reviewed and approved by the University of Pittsburgh IRB (PRO12060296).
References
- Bureau of Labor Statistics Series Report. United States Department of Labor; 2014a. [Google Scholar]
- Labor Force Characteristics (CPS) Bureau of Labor Statistics; 2014b. Labor Force Statistics from the Current Population Survey. [Google Scholar]
- Alterman T, Luckhaupt SE, Dahlhamer JM, Ward BW, Calvert GM. Prevalence rates of work organization characteristics among workers in the U.S.: data from the 2010 National Health Interview Survey. Am J Ind Med. 2013;56:647–659. doi: 10.1002/ajim.22108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson C, Dickinson DL. Bargaining and trust: the effects of 36-h total sleep deprivation on socially interactive decisions. J Sleep Res. 2010;19:54–63. doi: 10.1111/j.1365-2869.2009.00767.x. [DOI] [PubMed] [Google Scholar]
- Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: conceptual filters explain underreporting. American journal of public health. 2002;92:1421–1429. doi: 10.2105/ajph.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DP, Salas E, Barach P, Battles J, King H. The relation between teamwork and patient safety. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety Mahwah. New Jersey: Lawrence Erlbaum Associates (LEA); 2007. pp. 259–271. [Google Scholar]
- Boal WL, Leiss JK, Ratcliffe JM, Sousa S, Lyden JT, Li J, Jagger J. The national study to prevent blood exposure in paramedics: rates of exposure to blood. Int Arch Occup Environ Health. 2010;83:191–199. doi: 10.1007/s00420-009-0421-x. [DOI] [PubMed] [Google Scholar]
- Brown W, Dickison P, Misselbeck W, Levine R. Longitudinal Emergency Medical Technician Attribute and Demographic Study (LEADS): An interim report. Prehosp Emerg Care. 2002a;6:433–439. doi: 10.1080/10903120290938085. [DOI] [PubMed] [Google Scholar]
- Brown WE, Jr, Dickison PD, Misselbeck WJ, Levine R. Longitudinal Emergency Medical Technician Attribute and Demographic Study (LEADS): an interim report. Prehosp Emerg Care. 2002b;6:433–439. doi: 10.1080/10903120290938085. [DOI] [PubMed] [Google Scholar]
- Caruso CC. Negative impacts of shiftwork and long work hours. Rehabil Nurs. 2014;39:16–25. doi: 10.1002/rnj.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Channouf N, L'Ecuyer P, Ingolfsson A, Avramidis AN. The application of forecasting techniques to modeling emergency medical system calls in Calgary, Alberta. Health Care Manag Sci. 2007;10:25–45. doi: 10.1007/s10729-006-9006-3. [DOI] [PubMed] [Google Scholar]
- Cone DC, Brice JH, Delbridge TR, Myers JB. Emergency medical services : clinical practice and systems oversight. Second. Chichester, West Sussex; Hoboken: John Wiley & Sons Inc; 2015. [Google Scholar]
- Corbett SW, Grange JT, Thomas TL. Exposure of prehospital care providers to violence. Prehosp Emerg Care. 1998;2:127–131. doi: 10.1080/10903129808958856. [DOI] [PubMed] [Google Scholar]
- Eldevik MF, Flo E, Moen BE, Pallesen S, Bjorvatn B. Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PLoS One. 2013;8:e70882. doi: 10.1371/journal.pone.0070882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan ZJ, Bonauto DK, Foley MP, Silverstein BA. Underreporting of work-related injury or illness to workers' compensation: individual and industry factors. J Occup Environ Med. 2006;48:914–922. doi: 10.1097/01.jom.0000226253.54138.1e. [DOI] [PubMed] [Google Scholar]
- Foushee HC, Lauber JK, Baetge MM, Acomb DB. Crew Factors in Flight Operations: III The Operational Significance of Exposure to Short-Haul Air Transport Operations. Moffett Field, California: National Aeronautics and Space Administration; 1986. [Google Scholar]
- Frakes MA, Kelly JG. Sleep debt and outside employment patterns in helicopter air medical staff working 24-hour shifts. Air Med J. 2007;26:45–49. doi: 10.1016/j.amj.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Grange JT, Corbett SW. Violence against emergency medical services personnel. Prehosp Emerg Care. 2002;6:186–190. doi: 10.1080/10903120290938526. [DOI] [PubMed] [Google Scholar]
- Guyette FX, Morley JL, Weaver MD, Patterson PD, Hostler D. The effect of shift length on fatigue and cognitive performance in air medical providers. Prehosp Emerg Care. 2013;17:23–28. doi: 10.3109/10903127.2012.710719. [DOI] [PubMed] [Google Scholar]
- Jenkins P, Earle-Richardson G, Slingerland DT, May J. Time dependent memory decay. Am J Ind Med. 2002;41:98–101. doi: 10.1002/ajim.10035. [DOI] [PubMed] [Google Scholar]
- Kilpatrick K, Lavoie-Tremblay M. Shiftwork: what health care managers need to know. Health Care Manag (Frederick) 2006;25:160–166. doi: 10.1097/00126450-200604000-00009. [DOI] [PubMed] [Google Scholar]
- Landen DD, Hendricks S. Effect of recall on reporting of at-work injuries. Public Health Rep. 1995;110:350–354. [PMC free article] [PubMed] [Google Scholar]
- Lombardi DA, Folkard S, Willetts JL, Smith GS. Daily sleep, weekly working hours, and risk of work-related injury: US National Health Interview Survey (2004-2008) Chronobiol Int. 2010;27:1013–1030. doi: 10.3109/07420528.2010.489466. [DOI] [PubMed] [Google Scholar]
- Maguire BJ, Hunting KL, Guidotti TL, Smith GS. Occupational injuries among emergency medical services personnel. Prehospital Emergency Care. 2005;9:405–411. doi: 10.1080/10903120500255065. [DOI] [PubMed] [Google Scholar]
- Maguire BJ, Smith S. Injuries and Fatalities among Emergency Medical Technicians and Paramedics in the United States. Prehospital and disaster medicine. 2013:1–7. doi: 10.1017/S1049023X13003555. [DOI] [PubMed] [Google Scholar]
- Mock EF, Wrenn KD, Wright SW, Eustis TC, Slovis CM. Prospective field study of violence in emergency medical services calls. Ann Emerg Med. 1998;32:33–36. doi: 10.1016/s0196-0644(98)70096-4. [DOI] [PubMed] [Google Scholar]
- NTSB. A Review of Flightcrew-Involved Major Accidents of U S Air Carriers, 1978 through 1990. Washington, D.C.: National Transportation Safety Board; 1994. [Google Scholar]
- Oginski A, Oginska H, Pokorski J, Kmita W, Gozdziela R. Internal and external factors influencing time-related injury risk in continuous shift work. International journal of occupational safety and ergonomics : JOSE. 2000;6:405–421. doi: 10.1080/10803548.2000.11076464. [DOI] [PubMed] [Google Scholar]
- Olds DM, Clarke SP. The effect of work hours on adverse events and errors in health care. J Safety Res. 2010;41:153–162. doi: 10.1016/j.jsr.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oleinick A, Gluck JV, Guire KE. Establishment size and risk of occupational injury. Am J Ind Med. 1995;28:1–21. doi: 10.1002/ajim.4700280102. [DOI] [PubMed] [Google Scholar]
- Patterson PD, Arnold RM, Abebe K, Lave JR, Krackhardt D, Carr M, Weaver MD, Yealy DM. Variation in emergency medical technician partner familiarity. Health services research. 2011;46:1319–1331. doi: 10.1111/j.1475-6773.2011.01241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson PD, Huang DT, Fairbanks RJ, Simeone S, Weaver M, Wang HE. Variation in emergency medical services workplace safety culture. Prehosp Emerg Care. 2010a;14:448–460. doi: 10.3109/10903127.2010.497900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson PD, Suffoletto BP, Kupas DF, Weaver MD, Hostler D. Sleep quality and fatigue among prehospital providers. Prehosp Emerg Care. 2010b;14:187–193. doi: 10.3109/10903120903524971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson PD, Weaver MD, Frank RC, Warner CW, Martin-Gill C, Guyette FX, Fairbanks RJ, Hubble MW, Songer TJ, Callaway CW, Kelsey SF, Hostler D. Association between poor sleep, fatigue, and safety outcomes in emergency medical services providers. Prehosp Emerg Care. 2012a;16:86–97. doi: 10.3109/10903127.2011.616261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson PD, Weaver MD, Hostler D, Guyette FX, Callaway CW, Yealy DM. The shift length, fatigue, and safety conundrum in EMS. Prehosp Emerg Care. 2012b;16:572–576. doi: 10.3109/10903127.2012.704491. [DOI] [PubMed] [Google Scholar]
- Patterson PD, Weaver MD, Weaver SJ, Rosen MA, Todorova G, Weingart LR, Krackhardt D, Lave JR, Arnold RM, Yealy DM, Salas E. Measuring teamwork and conflict among emergency medical technician personnel. Prehosp Emerg Care. 2012c;16:98–108. doi: 10.3109/10903127.2011.616260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst TM, Brubaker TL, Barsotti A. Organizational injury rate underreporting: the moderating effect of organizational safety climate. J Appl Psychol. 2008;93:1147–1154. doi: 10.1037/0021-9010.93.5.1147. [DOI] [PubMed] [Google Scholar]
- Reason J. Human error: models and management. BMJ. 2000;320:768–770. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichard AA, Marsh SM, Moore PH. Fatal and nonfatal injuries among emergency medical technicians and paramedics. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2011;15:511–517. doi: 10.3109/10903127.2011.598610. [DOI] [PubMed] [Google Scholar]
- Rose DA. Personality type and perception of the work environment in career paramedics. Ball State University; 1992. [Google Scholar]
- Ruser JW. Examining evidence on whether BLS undercounts workplace injuries and illnesses. Mon Labor Rev. 2008;131:20–32. [Google Scholar]
- Salas E, Fiore SM. Team cognition : understanding the factors that drive process and performance. 1st. Washington, DC: American Psychological Association; 2004. p. xi, 268. [Google Scholar]
- Salas E, Sims DE, Burke CS. Is there a “Big Five” in Teamwork? Small Group Research. 2005;36:555–599. [Google Scholar]
- Sallinen M, Kecklund G. Shift work, sleep, and sleepiness - differences between shift schedules and systems. Scandinavian journal of work, environment & health. 2010;36:121–133. doi: 10.5271/sjweh.2900. [DOI] [PubMed] [Google Scholar]
- Suyama J, Rittenberger JC, Patterson PD, Hostler D. Comparison of public safety provider injury rates. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2009;13:451–455. doi: 10.1080/10903120903144908. [DOI] [PubMed] [Google Scholar]
- Tassi P, Nicolas A, Dewasmes G, Eschenlauer R, Ehrhart J, Salame P, Muzet A, Libert JP. Effects of noise on sleep inertia as a function of circadian placement of a one-hour nap. Percept Mot Skills. 1992;75:291–302. doi: 10.2466/pms.1992.75.1.291. [DOI] [PubMed] [Google Scholar]
- Thomas MJ, Petrilli RM. Crew familiarity: operational experience, non-technical performance, and error management. Aviat Space Environ Med. 2006;77:41–45. [PubMed] [Google Scholar]
- Tucker S, Diekrager D, Turner N, Kelloway EK. Work-related injury underreporting among young workers: Prevalence, gender differences, and explanations for underreporting. J Safety Res. 2014 doi: 10.1016/j.jsr.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Virtanen M, Ferrie JE, Gimeno D, Vahtera J, Elovainio M, Singh-Manoux A, Marmot MG, Kivimaki M. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep. 2009;32:737–745. doi: 10.1093/sleep/32.6.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehrens SM, Hampton SM, Kerkhofs M, Skene DJ. Mood, alertness, and performance in response to sleep deprivation and recovery sleep in experienced shiftworkers versus non-shiftworkers. Chronobiol Int. 2012;29:537–548. doi: 10.3109/07420528.2012.675258. [DOI] [PubMed] [Google Scholar]
- Williamson A, Lombardi DA, Folkard S, Stutts J, Courtney TK, Connor JL. The link between fatigue and safety. Accid Anal Prev. 2011;43:498–515. doi: 10.1016/j.aap.2009.11.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.