Abstract
Introduction
A nonrecurrent laryngeal nerve (NRLN) is a rare anatomical variation in which the nerve enters the larynx directly off the cervical vagus nerve.
Case Report
We present 2 patients who underwent thyroid surgery for benign disease. Intraoperatively, type 2a and 1 NRLN were identified. Due to the frequent association with a vascular abnormality, an ultrasound and a computed tomography were performed which showed a right aberrant subclavian artery with a retroesophageal course and a common trunk of the common carotids in both patients.
Discussion and Conclusion
The presence of an NRLN is a major risk during surgical procedures and the surgeon should be aware of the possibility of its existence. NRLN may be associated with rare vascular anomalies, such as arteria lusoria and a bicarotid trunk. This paper reveals this association in 2 patients for the first time.
Key Words: Recurrent laryngeal nerve, Thyroid surgery, Vascular anomalies, Prediction
What Is Known about This Topic?
• The presence of a nonrecurrent laryngeal nerve is a major risk during surgical procedures and may be associated with rare vascular anomalies.
What Does This Case Report Add?
• This paper reports an association between a nonrecurrent laryngeal nerve and rare vascular anomalies, such as arteria lusoria and a bicarotid trunk: the first 2 cases of patients in the literature.
Introduction
The recurrent laryngeal nerve (RLN) is a branch of the vagus nerve providing motor and sensitive function to the larynx [1]. It usually describes a loop as it turns upward, passing under the subclavian artery on the right and recurring around the ligamentum arteriosum on the left. A nonrecurrent laryngeal nerve (NRLN) is a rare anatomical variation in which the nerve enters the larynx directly from the cervical vagus nerve, without descending to the thoracic level [2]. It has been reported in 0.3-0.8% of the population on the right side, being extremely rare on the left side (0.004%) [3].
This anomaly promotes a high susceptibility to damage during thyroid surgery [2], potentially resulting in permanent hoarseness, and, if bilateral, could lead to aphonia or life-threatening dyspnea [4]. Preoperative ultrasound or computed tomography may provide clues about the existence of an NRLN, thus avoiding iatrogenic injury to the nerve [5].
This paper reports 2 cases of intraoperative NRLN identification and describes the relevant radiological and anatomical features of this anomaly.
Case Report
Written informed consent was obtained from the patients for publication of this case report and its accompanying images.
The first patient was a 56-year-old asymptomatic woman sent to our department with a 20-mm follicular neoplasm (Bethesda classification) in the right lobe of the thyroid and an adjacent, not biopsied, nodule of 9 mm. The previous history and physical examination were unremarkable and thyroid function was normal.
The second patient was a 55-year-old woman with multinodular goiter. She had a family history of thyroid surgery and presented with 3-cm, bilateral, elastic nodules on physical examination and ultrasonography, with normal thyroid function. Biopsies revealed colloid nodules.
The first patient underwent a right thyroid lobectomy and isthmectomy and the second underwent a total thyroidectomy. During the procedure, the thyroid gland and blood vessels were exposed. As it was not possible to identify the RLN on the right side using the usual anatomical landmarks, the possibility of an NRLN was raised.
In the first patient, we identified a branch of the right vagus nerve, entering the larynx beside Berry's ligament, almost at a right angle, without any apparent recurrence (fig. 1a). The nerve was compatible with a type 2a NRLN, as defined by Toniato et al. [6]. In the second patient, we found an NRLN showing a course parallel to the upper pole vessels (fig. 1b), compatible with a type 1 NRLN.
Fig. 1.

Surgery in the first patient (a) and the second patient (b). 1 = Right NRLN; 2 = thyroid nodule; 3 = right hemithyroid.
After dissecting the thyroid from the trachea and Berry's ligament, we successfully completed the surgery. The histopathological report showed a 1.1-cm, partially cystic follicular adenoma in the first case and an adenomatous multinodular goiter in the second. The postoperative period was uneventful in both patients.
Due to the frequent association of NRLN with vascular abnormalities, an ultrasound and a computed tomography were postoperatively performed and in both patients we found a common trunk of the 2 common carotids and a right aberrant subclavian artery with a retroesophageal course (fig. 2).
Fig. 2.
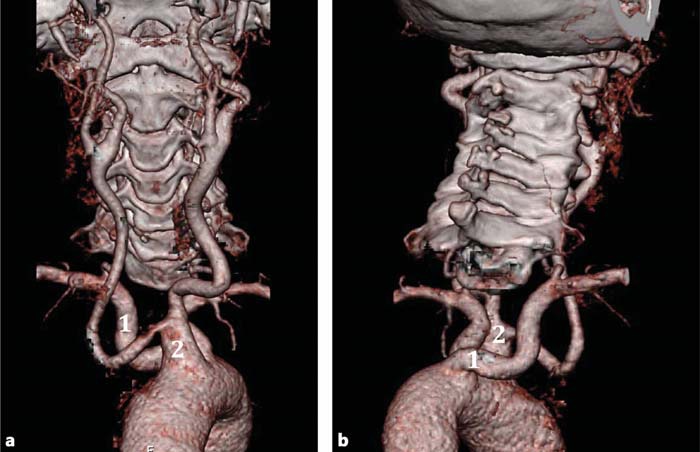
Computed tomography: anterior (a) and posterior (b) views. 1 = Right aberrant subclavian artery with a retroesophageal course; 2 = common trunk of the 2 common carotids.
Because the 2 patients were asymptomatic, no additional measures were considered in this regard. They were informed of the congenital abnormality and about the eventual symptomatology in the future.
Discussion
There are many descriptions of variations of the RLN. The RLN usually runs in the tracheoesophageal groove (50-77%), the paratracheal area (17-40%), and the paraesophageal area (6%) or within thyroid parenchyma (4%) and it can divide into 2 or 3 branches before entering the larynx [7]. On the other hand, cases of an NRLN, first reported by Stedman [8] in 1823, wherein the nerve enters the larynx directly from the vagus nerve without recurring have been often found incidentally during thyroid surgery. All of these variations increase the risk of nerve injury during thyroidectomy.
In studies on cadavers, the nonrecurrent inferior laryngeal nerve occurs very rarely, with an incidence of 0.3-0.8% [9,10]. In the largest series reported, including 6,637 observations of the RLN during neck surgery, the frequency of an NRLN was 0.54% (17 cases in 3,098) on the right side and 0.07% on the left (2 cases in 2,846), corresponding to a global prevalence of 0.32% [2]. However, the true incidence of NRLN may be higher (6%) than expected, as suggested by intraoperative neuromonitoring studies [11].
The RLN is the nerve of the 6th branchial arch, which, with the descent of the heart, passes beneath the 6th aortic arch and ascends to the larynx. On the right side, the distal portion of the 6th and 5th aortic arches disappears and the nerve moves up beneath the 4th aortic arch, which becomes the future subclavian artery. Occasionally, the 4th arch disappears and the subclavian artery arises directly from the aorta (aberrant subclavian artery or arteria lusoria), distally to the normally positioned left subclavian artery, and crosses retroesophageally to the (right) upper limb. In these cases the nerve moves cranially and originates directly from the vagus where it becomes an NRLN [12]. The incidence of this vascular malformation is reportedly as high as 0.5-2% of the general population. Even though it is usually asymptomatic, nearly 5% of these patients experience dysphagia (dysphagia lusoria) or symptoms related to arterial tortuosity, premature atherosclerosis, and rarely aneurism formation [13]. It may be associated with several congenital cardiovascular anomalies and chromosomal and other syndromes. Anatomical variations associated with arteria lusoria include the abnormal origin of the right vertebral artery from the aorta or from the right common carotid artery, the presence of a common carotid trunk, a right-sided thoracic duct, and a right NRLN. The combination of an arteria lusoria and a bicarotid trunk appears rarely in the population. This trunk, another aortic arch branching variation, arises from the aortic arch and then bifurcates into the right and left common carotid arteries, thus creating a common origin for the 2 common carotid arteries [14]. According to the classification of Piersol [15], in which aortic anomalies are classified into 5 groups, this case belongs to group 2 (right aberrant subclavian artery) plus group 5 (common trunk of common carotids). To our knowledge, these anatomical variations have only been described in cadavers, this being the first time these vascular anomalies have been associated with an NRLN in patients. On the left side, the NRLN occurs less frequently and is usually associated with situs inversus or a right aortic arch [12].
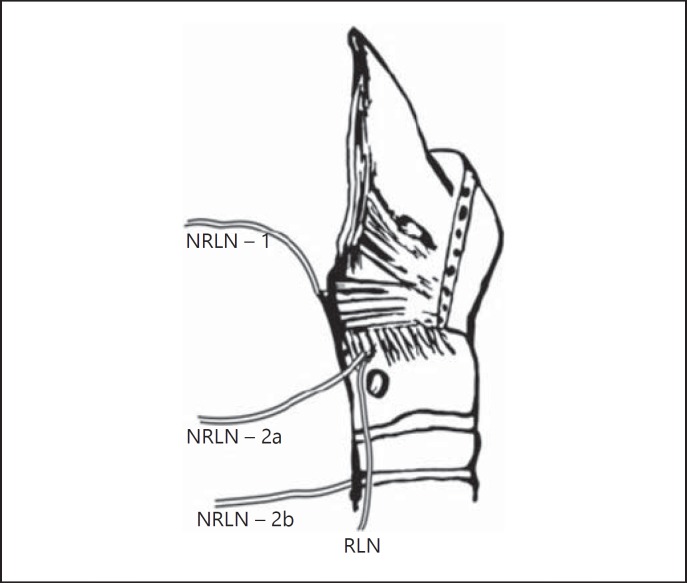
In addition, 3 types of NRLN have been described (fig. 3). In type 1, the nerve runs with the superior vascular pedicle of the thyroid gland. In type 2a, it runs above the trunk of the inferior thyroid artery. In type 2b, it runs below the trunk or between the branches of the inferior thyroid artery [6].
Fig. 3.
Relationship of the NRLN to the laryngeal framework. 1, 2a, and 2b correspond to the type of nerve course. Adapted from Varghese et al. [21].
Considering the probability of damaging the nerve during surgery, some guidelines were developed to prevent a major surgical risk. The best way to avoid damage to the nerve during thyroidectomy is to identify the nerve with systematic diligent dissection based on the usual anatomical landmarks and keeping always in mind the possibility of an anatomic variation. Liu et al. [16] suggested that any transverse bond (with the exception of the middle thyroid vein) should not be cut unless the RLN is identified and preserved, thus preventing postoperative vocal fold paresis. Intraoperative neuromonitoring may also be a useful tool for understanding the anatomy and physiology of the inferior laryngeal nerve [11].
Preoperative diagnosis of NRLN and its associated arterial abnormalities is also theoretically possible with imaging studies [17,18]. Some studies have reported 100% accuracy for ultrasonography in detecting NRLN-associated vascular anomalies [19,20], allowing earlier nerve identification and prevention of injuries [19]. Computed tomography is also being used as a routine examination before thyroid surgery in some institutions for this purpose [5]. Nevertheless, systematic preoperative use of imaging methods is not yet recommended.
Conclusion
The presence of an NRLN is a major risk during surgical procedures. Its damage should be avoided by intraoperative nerve identification, with systematic diligent dissection based on the usual anatomical landmarks and awareness of the possibility of its existence.
NRLN may be associated with rare vascular anomalies, such as arteria lusoria and a bicarotid trunk. These findings have been previously described in cadavers, but this paper reveals this association in 2 patients for the first time. Thorough preoperative knowledge of the radiological and surgical anatomy seems very important for the improvement of surgical outcomes.
Disclosure Statement
The authors declare that they have no competing interests.
References
- 1.Khaki AA, et al. An unusual course of the left recurrent laryngeal nerve. Clin Anat. 2007;20:344–346. doi: 10.1002/ca.20341. [DOI] [PubMed] [Google Scholar]
- 2.Henry JF, et al. The nonrecurrent inferior laryngeal nerve: review of 33 cases, including two on the left side. Surgery. 1988;104:977–984. [PubMed] [Google Scholar]
- 3.Mahmodlou R, Aghasi MR, Sepehrvand N. Identifying the non-recurrent laryngeal nerve: preventing a major risk of morbidity during thyroidectomy. Int J Prev Med. 2013;4:237–240. [PMC free article] [PubMed] [Google Scholar]
- 4.Lee MS, et al. Relative direction and position of recurrent laryngeal nerve for anatomical configuration. Surg Radiol Anat. 2009;31:649–655. doi: 10.1007/s00276-009-0494-y. [DOI] [PubMed] [Google Scholar]
- 5.Watanabe A, et al. Preoperative computed tomography diagnosis of non-recurrent inferior laryngeal nerve. Laryngoscope. 2001;111:1756–1759. doi: 10.1097/00005537-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Toniato A, et al. Identification of the nonrecurrent laryngeal nerve during thyroid surgery: 20-year experience. World J Surg. 2004;28:659–661. doi: 10.1007/s00268-004-7197-7. [DOI] [PubMed] [Google Scholar]
- 7.Zambudio AR, et al. Prospective study of postoperative complications after total thyroidectomy for multinodular goiters by surgeons with experience in endocrine surgery. Ann Surg. 2004;240:18–25. doi: 10.1097/01.sla.0000129357.58265.3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stedman G. A singular distribution of some of the nerves and arteries of the neck and the top of the thorax. Edinb Med Surg J. 1823;19:564–565. [PMC free article] [PubMed] [Google Scholar]
- 9.Asgharpour E, et al. Recurrent laryngeal nerve landmarks revisited. Head Neck. 2012;34:1240–1246. doi: 10.1002/hed.21882. [DOI] [PubMed] [Google Scholar]
- 10.Coady MA, et al. Nonrecurrent laryngeal nerve during carotid artery surgery: case report and literature review. J Vasc Surg. 2000;32:192–196. doi: 10.1067/mva.2000.105680. [DOI] [PubMed] [Google Scholar]
- 11.Donatini G, Carnaille B, Dionigi G. Increased detection of non-recurrent inferior laryngeal nerve (NRLN) during thyroid surgery using systematic intraoperative neuromonitoring (IONM) World J Surg. 2013;37:91–93. doi: 10.1007/s00268-012-1782-y. [DOI] [PubMed] [Google Scholar]
- 12.Nagayama I, et al. Importance of pre-operative recognition of the nonrecurrent laryngeal nerve. J Laryngol Otol. 1994;108:417–419. doi: 10.1017/s0022215100126957. [DOI] [PubMed] [Google Scholar]
- 13.Attmann T, et al. Two-stage surgical and endovascular treatment of an aneurysmal aberrant right subclavian (lusoria) artery. Eur J Cardiothorac Surg. 2005;27:1125–1127. doi: 10.1016/j.ejcts.2005.02.029. [DOI] [PubMed] [Google Scholar]
- 14.Natsis K, et al. A bicarotid trunk in association with an aberrant right subclavian artery: report of two cases, clinical impact, and review of the literature. Folia Morphol (Warsz) 2011;70:68–73. [PubMed] [Google Scholar]
- 15.Piersol G. Human Anatomy. ed 5. Philadelphia: Lippincott; 1916. pp. 724–727. [Google Scholar]
- 16.Liu LX, et al. The importance of nonrecurrent laryngeal nerve in thyroid surgery (in Chinese) Zhonghua Wai Ke Za Zhi. 2006;44:904–906. [PubMed] [Google Scholar]
- 17.Abboud B. Preoperative diagnosis of right nonrecurrent inferior laryngeal nerve by CT scan: report of a case and review of the literature. J Med Liban. 2007;55:46–49. [PubMed] [Google Scholar]
- 18.Guerreiro S, et al. The non-recurrent laryngeal nerve: an anatomical ‘trap’. Rev Port Endocrinol Diabetes Metab. 2014;9:84–87. [Google Scholar]
- 19.Iacobone M, et al. The usefulness of preoperative ultrasonographic identification of nonrecurrent inferior laryngeal nerve in neck surgery. Langenbecks Arch Surg. 2008;393:633–638. doi: 10.1007/s00423-008-0372-9. [DOI] [PubMed] [Google Scholar]
- 20.Yetisir F, et al. Efficacy of ultrasonography in identification of non-recurrent laryngeal nerve. Int J Surg. 2012;10:506–509. doi: 10.1016/j.ijsu.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Varghese BT, Desai KP, Ramachandran A. Pre-operative prediction of a right non-recurrent laryngeal nerve by computed tomography. J Laryngol Otol. 2013;127:525–527. doi: 10.1017/S0022215113000054. [DOI] [PubMed] [Google Scholar]