Abstract
Background
Male involvement in maternal health is recommended as one of the interventions to improve maternal and newborn health. There have been challenges in realising this action, partly due to the position of men in society and partly due to health system challenges in accommodating men. The aim of this study was therefore to evaluate the effect of Home Based Life Saving Skills training by community health workers on improving male involvement in maternal health in terms of knowledge of danger signs, joint decision-making, birth preparedness, and escorting wives to antenatal and delivery care in a rural community in Tanzania.
Design
A community-based intervention consisting of educating the community in Home Based Life Saving Skills by community health workers was implemented using one district as the intervention district and another as comparison district. A pre-/post-intervention using quasi-experimental design was used to evaluate the effect of Home Based Life Saving Skills training on male involvement and place of delivery for their partners. The effect of the intervention was determined using difference in differences analysis between the intervention and comparison data at baseline and end line.
Results
The results show there was improvement in male involvement (39.2% vs. 80.9%) with a net intervention effect of 41.1% (confidence interval [CI]: 28.5–53.8; p <0.0001). There was improvement in the knowledge of danger signs during pregnancy, childbirth, and postpartum periods. The proportion of men accompanying their wives to antenatal and delivery also improved. Shared decision-making for place of delivery improved markedly (46.8% vs. 86.7%), showing a net effect of 38.5% (CI: 28.0–49.1; p <0.0001). Although facility delivery for spouses of the participants improved in the intervention district, this did not show statistical significance when compared to the comparison district with a net intervention effect of 12.2% (95% CI: −2.8–27.1: p=0.103).
Conclusion
This community-based intervention employing community health workers to educate the community in the Home Based Life Saving Skills programme is both feasible and effective in improving male involvement in maternal healthcare.
Keywords: community-based intervention, home-based life saving skills, male involvement, rural Tanzania
Introduction
Male involvement in maternal health is recommended as one of the interventions to improve maternal and newborn health (1). As early as 1994, the International Conference on Population and Development (ICPD) in Cairo endorsed the principles of involving men in maternal, neonatal, and reproductive health as well as research that explores the effects of gender roles on health outcomes (2). The action plan stresses the importance of men as partners with shared responsibilities towards sexual and reproductive health. There have been challenges in realising this plan, partly due to gender structures in society and partly due to health system challenges in accommodating men in areas of sexual and reproductive health (3).
Many societies and cultures assume that pregnancy is solely a women's issue and this may have contributed to men not being invited to learn about and engage in matters related to women's and children's health (4). In addition, due to gender structures, men are mostly considered to be the decision-makers in many patriarchal families. They decide when and where the woman can go to access skilled antenatal care (ANC), delivery, and postpartum care, as well as child care (5, 6). This might take the form of deciding how their partners use health services, for example, whether to provide financial support for transportation to access the services (7) or deciding whether a pregnant woman can travel to a referral facility (8–10). At the same time, men, who hold both the economic and decision-making power, are not knowledgeable about complications that can occur during pregnancy and childbirth (11, 12). This can make an impact on women's health when a need arises to take quick actions in seeking expert care (13, 14).
Despite challenges in implementing the ICPD plan of action, there has been some progress made in the increase in male involvement in ANC attendance in areas related to HIV prevention, such as mother-to-child transmission of HIV. This shift in custom has been shown to improve knowledge, adherence to treatment regimen, and rates of exclusive breastfeeding (15–17). Family planning use was also shown to improve in studies where men were included in counselling sessions with their partners (18, 19). Encouraging outcomes have also been recently reported in male involvement in maternal health, including increased access to antenatal and postnatal care (20), reduced maternal smoking, reduced maternal depression, and reduced risk of preterm birth and infant mortality (21–24).
Other interventions, however, have been shown to have negative effects in improving male involvement in reproductive and maternal healthcare. A study completed in Tanzania on counselling for HIV testing, where pregnant women were asked to return to clinic together with their husbands for couple counselling, resulted in women not returning for the second visit (25). Similarly, it was shown in a recent review on male involvement and prevention of mother-to-child transmission (PMTCT) of HIV that uptake of PMTCT was low if unmarried women were obliged to come with their partners (26). Barriers impeding women to reach adequate services have been shown to occur because of gender inequality, such as heavy household workload and having no decision-making power, and inaccessibility to health-related resources, all of which affect child survival (27). Interventions that promoted gender equality and treated men as agents of change, such as making joint decisions and sharing household chores, have been shown to improve interspousal communication, reduce maternal workload, and lead to more involvement in birth preparedness (4, 28, 29). In contrast, if studies are designed in such a way that they consider men's only duty to be a provider of money (i.e. men as instrumental), there is a risk of perpetuating women's disempowerment in relation to health seeking (30, 31). Therefore, it is important to design programmes with strategies that are gender sensitive and can reduce gender inequality (32–35).
In Tanzania, as part of the policy of focused antenatal care (FANC) for the care of pregnant women during ANC, men are encouraged to attend with their spouses. During ANC, the health worker is supposed to discuss birth preparedness and complication readiness (BP/CR) with the couple, as well as general care of the pregnant woman at home (36). In addition, part of the PMTCT national policy is male involvement in voluntary counselling and testing (VCT) and in the overall prevention of perinatal and sexual transmission of HIV. Pregnant women are encouraged to inform their husbands and request that they attend antenatal clinics for HIV-VCT (37). Despite these policies, however, there is no specific strategy to implement this policy.
A way to involve men in sexual and reproductive health is to increase the knowledge of both men and women in the community. Home Based Life Saving Skills (HBLSS) is a programme developed and introduced by the American College of Nurse Midwives (ACNM), which involves the joint training of the pregnant woman, her husband, and other family members (38). The aim is to equip the immediate family members with knowledge in order to recognise life-threatening danger signs, make birth preparedness arrangements, promote health-seeking behaviour, and acquire skills to help the woman if any problem occurs at home. The training encourages dialogue and thus making joint informed decisions when the need for action arises. As such, this is a gender-sensitive programme in that it accommodates both men and women in the intervention.
The aim of this study was to evaluate the effect of HBLSS training in a rural community in Tanzania in improving male involvement in maternal healthcare.
Materials and methods
Study design
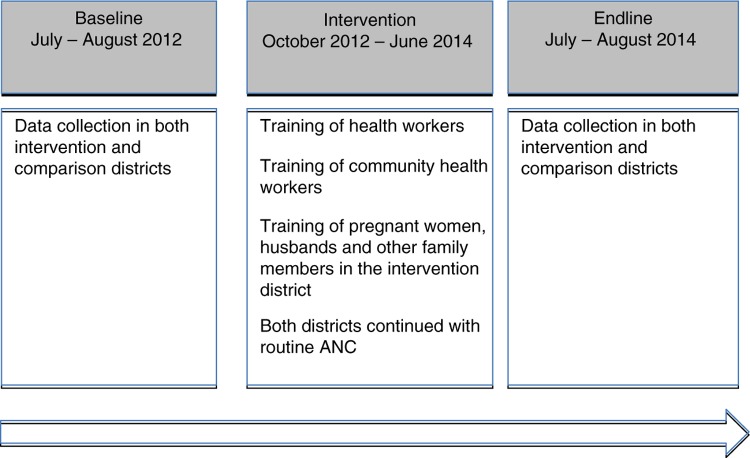
A quasi-experimental study (non-equivalent group) using pretest–post-test comparison was conducted to evaluate the effect of HBLSS training in the community on male involvement in maternal health in a rural area (Fig. 1).
Fig. 1.
Phases of the intervention.
Study setting
The study was conducted in two districts in the Pwani Region, Rufiji and Mkuranga, in the south part of Tanzania. Both districts have approximately 222,000 inhabitants, half of them male and half female. Rufiji has a population of 217,274 (108,024 males; 109,250 females), whereas Mkuranga, the comparison district, has a population of 222,921 (104,851 males, 118,070 females). The male literacy rate in the Pwani Region was reported to be 73.2% and the female literacy rate was 66.9% (39). As in Rufiji, agriculture is the main economic activity in Mkuranga District. Common food crops cultivated are cassava, rice, and beans. The main cash crop is cashew nuts. Two hospitals, four health centres, and fifty-two dispensaries serve the population in Rufiji District. Mkuranga has one hospital, five health centres, and fifty-three dispensaries. Clinical officers with 2 years’ training in clinical medicine, registered midwives and enrolled nurses, public health nurses, and maternal and child health aiders provide maternal health services in the health facilities. These include ANC and delivery care services. Men are encouraged to attend the ANC clinic together with their wives (36). Rufiji District was chosen as the intervention district because previous studies completed in the area demonstrated that pregnant women had low awareness of danger signs (40). Mkuranga was chosen as a comparison district due to its comparable population size and socio-demographic characteristics.
Intervention
The HBLSS education programme covers core topics such as the following: the importance of attending ANC early; recognition of danger signs during pregnancy, delivery, and postpartum and for the newborn; actions to take in case of danger; sharing household chores; making joint decisions on the place to deliver; and identifying skilled care for delivery. Furthermore, the concept of knowledge and actions for BP/CR were included in the educational visits, which relates to saving money, identifying transport, identifying where to go in case of emergency, identifying a skilled attendant, and the preparation of birth kits. Birth kits in this study include buying sterile gloves, surgical blades, a cord tie, and clean clothes. The promotion of health-seeking behaviour to avoid maternal morbidity and deaths was also discussed. The content of the home visits is shown in Table 1. Education was provided to currently pregnant women, their husbands, and other family members. The teaching was done through the use of checklists, skill acquisition, and Take Action cards. These cards consist of images that represent the various problems on one side and which action to take on the other side. The family members are given the cards to keep at the end of each session.
Table 1.
Training of pregnant women, husbands, and family members on Home Based Life Saving Skills
| Visit 1 | Visit 2 | Visit 3 | Visit 4 |
|---|---|---|---|
| Importance of attending antenatal care early | Recognition of maternal danger signs and actions to take | Recognition of danger signs and actions to take for early referral | Recognition of maternal and newborn danger signs and actions to take |
| Recognition of maternal danger signs and actions to take | Birth preparedness and complication readiness | Birth preparedness and complication readiness | Birth preparedness and complication readiness |
| Importance of rest and nutrition during pregnancy | Importance of skilled care for delivery and joint decision-making in seeking delivery care | Importance of skilled care for delivery and joint decision-making in seeking delivery care | |
| Importance of helping the woman with household chores |
Twenty-four health workers from selected health facilities were trained by a master trainer (the first author), who was trained by the ACNM to use the HBLSS concept. The training duration was 1 week. These health workers then trained 66 community health workers (CHWs) for 2 weeks under the supervision of the master trainer. The content of the training included the HBLSS curriculum and BP/CR messages. Refresher training was conducted every 2 months for 1 day to ensure that the education programme was correctly provided. CHWs are trusted men and women in their villages who have completed primary school, are able to read and write, and regularly assist in public health programmes on a voluntary basis. The CHWs were provided with bicycles for easy outreach in this rural community. CHWs identified pregnant women in the community and were asked to make at least four visits to the family throughout the pregnancy. The visits lasted between 60 and 90 minutes. Arrangements were made in advance for a convenient time when the husband and other family members would be available for the educational session. Both the intervention and comparison districts continued to receive the usual services provided by trained health workers at health facilities.
Sampling and sample size
A two-stage cluster sampling strategy was employed to select a representative sample from the two districts. First, all health facilities (56 in Rufiji District and 58 in Mkuranga District) were listed and then 14 health facilities were randomly selected using the ballot method. In Rufiji District, four health centres and ten dispensaries were randomly selected, whereas in Mkuranga, five health centres and nine dispensaries were randomly selected. Next, two villages forming the catchment population of the health facilities were randomly selected. All men who had partners who had delivered in the last 2 years were selected to participate in the study. The estimated sample size was 1,300 (650 per district). This was based on the assumption of detecting a 10% effect from proportion of male involvement in accompanying spouses of 65.3% (41), considering the power of 80% with 5% significant level, a design effect of 1.5 and non-response rate of 20%. The same procedure was used at baseline and end line, and participants were not necessarily the same during the two surveys.
Data collection
Before the start of the intervention, a baseline survey was conducted in both districts during 2 months in 2012. An end line survey was conducted 2 years later. Research assistants who had recently graduated from medical school, with experience in conducting interviews, were trained for 5 days before the start of data collection. The questionnaire used in the study was adapted from a questionnaire on BP/CR developed by JHPIEGO, an affiliate of Johns Hopkins University (42). The questionnaire was adapted to fit the Tanzanian context, specifically for the rural areas. A pilot test using 20 questionnaires was conducted in a separate but similar district in the same region. A few alterations were made to the questionnaire following the pilot test. An example of the modifications made is the addition of a question about purchasing birth materials (birth kit), as this was mentioned as a common BP/CR practice. Data were collected under the supervision of the first author. The questionnaire was used to collect information on socio-demographic characteristics, knowledge of danger signs, knowledge and practice of BP/CR components, and place of delivery (Table 2).
Table 2.
Summary of items used to identify knowledge of danger signs, knowledge on BP/CR, and actions taken
| Danger signs | ||||
|---|---|---|---|---|
|
| ||||
| During pregnancy | During childbirth | During postpartum period | Knowledge of BP/CR | Actions taken on BP/CR |
| Excessive vaginal bleeding | Excessive vaginal bleeding | Excessive vaginal bleeding | Saving money | Saving money |
| Convulsions | Convulsions | Convulsions | Identifying transport | Identifying transport |
| Fever | Delay in placenta delivery | Foul-smelling discharge | Identify where to go in case of emergency | Identifying where to go in case of emergency |
| Blurred vision | Fever | Difficulty breathing | Identifying skilled birth attendant | Identifying skilled birth attendant |
| Difficulty breathing | Preterm rupture of membranes | Abdominal pain | Identifying blood donor | Identifying blood donor |
| Swelling of hands and feet | Prolonged labour | Pain in the perineum | Identifying birth kit | Identifying birth kit |
| Severe abdominal pain | Body weakness | |||
| Dizziness | Swollen or tender breasts | |||
| Reduced or increased foetal movements | ||||
| Ruptured membranes before delivery | ||||
BP/CR, birth preparedness and complication readiness.
Outcome measures
The main outcome in this study was male involvement. There are no standard criteria in the literature for what is considered to be male involvement. Some authors use criteria such as escorting their partner to ANC or childbirth as a measure of male involvement. Others have used a composite score of several indicators to assess male involvement (43, 44). In our study, we defined male involvement using a composite scoring system. The male involvement score was based on a yes/no answer to the following five components: 1) men escorting their wives to ANC; 2) men escorting their wives to delivery; 3) joint decision-making on where to deliver; 4) knowledge of at least three or more danger signs in each of the phases (pregnancy, childbirth, and the postpartum period), although items to identify knowledge were not ranked according to importance; and 5) at least three BP/CR actions having been taken. A composite index for male involvement was based on the participants having taken three out of the five above actions. The knowledge of danger signs and BP/CR was obtained by asking the participants to mention danger signs without giving any options (Table 2). All variables were measured dichotomously (yes/no). These variables were selected in congruence with previous studies conducted in Uganda and Nigeria that used them to indicate male involvement (13, 43, 44). In addition, the location of the last delivery was recorded. The outcomes were compared before and after the intervention and between the two districts.
Data analysis
Data were entered into SPSS and cleaned, and in case of any discrepancies the original questionnaire was consulted for cross-checking. Characteristics of the participants were described by using descriptive statistics. An estimated proportion of outcome variables and its variance were calculated according to the cluster sampling design for each group (pretest–post-test intervention) and time point (baseline/end line).
The net intervention effect (NIE) was estimated as the difference between baseline and end line in the intervention group minus the difference between baseline and end line in the comparison group regarding changes in proportions from baseline to end line. This effect is a linear combination of four independent estimates. p-values from a Z-test and 95% confidence intervals for the intervention effect were calculated based on a normal distribution assumption. A statistically significant effect was considered if p<0.05. Statistical analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC, USA).
Ethical approval
Ethical approval to conduct the study was obtained from the Muhimbili University of Health and Allied Sciences from the Senate Research and Publication Committee (Ref. No. MU/RP/AEC/Vol XIII). Permission to conduct the study in the area was given by the offices of the district executive directors and the village executive officers. The aim of the study was explained to the participants along with their rights in relation to continuing or withdrawing from the study. Informed consent was obtained after participants received the information regarding the aim and objectives of the study. Upon agreeing to participate in the study, participants signed the informed consent form. A thumbprint was accepted for those who could not read or write.
Results
A total of 1,378 men were interviewed for the study in the intervention district (baseline and end line) and 1,359 in the comparison district (baseline and end line). There was no significant difference in terms of age, marital status, education level, or wife's education level (Table 3).
Table 3.
Socio-demographic characteristics of participants in the intervention and comparison districts at baseline and end line
| Baseline | End line | |||||
|---|---|---|---|---|---|---|
| n=725 | n=701 | n=653 | n=658 | |||
| Intervention, n (%) | Comparison, n (%) | p | Intervention, n (%) | Comparison, n (%) | p | |
| Age of participants | 0.832 | 0.614 | ||||
| <21 | 28 (3.9) | 29 (4.2) | 13 (2.0) | 5 (0.8) | ||
| 21–25 | 111 (15.3) | 88 (12.5) | 103 (15.8) | 89 (13.5) | ||
| 26–30 | 177 (24.4) | 140 (20.0) | 110 (16.8) | 98 (14.9) | ||
| 31–35 | 143 (19.7) | 147 (21.0) | 114 (17.5) | 150 (22.8) | ||
| >35 | 266 (36.7) | 297 (42.4) | 313 (47.9) | 316 (48.0) | ||
| Marital status | 0.173 | 0.581 | ||||
| Single | 49 (6.8) | 35 (5.0) | 22 (3.4) | 26 (4.0) | ||
| Married/cohabiting | 676 (93.2) | 666 (95.0) | 631 (96.6) | 632 (96.0) | ||
| Education level | 0.159 | 0.748 | ||||
| No school | 150 (20.7) | 146 (21.0) | 136 (20.8) | 128 (19.5) | ||
| Primary incomplete | 64 (8.8) | 67 (9.5) | 85 (13.0) | 47 (7.1) | ||
| Primary completed | 450 (62.1) | 440 (62.7) | 352 (53.9) | 415 (63.1) | ||
| Secondary or higher | 60 (8.3) | 48 (6.8) | 80 (12.3) | 68 (10.3) | ||
| Wife's education level | 0.416 | 0.693 | ||||
| No school | 191 (26.3) | 228 (32.5) | 194 (29.7) | 222 (33.7) | ||
| Primary incomplete | 88 (12.1) | 65 (9.3) | 67 (10.3) | 51 (7.8) | ||
| Primary completed | 408 (56.3) | 379 (54.1) | 347 (53.1) | 345 (52.4) | ||
| Secondary or higher | 38 (5.3) | 29 (4.1) | 45 (6.9) | 40 (6.1) | ||
| Asset quintile | 0.207 | 0.357 | ||||
| A1 (poorest) | 21.8 | 18.5 | 23.1 | 18.9 | ||
| A2 | 20.6 | 22.7 | 19.5 | 23.2 | ||
| A3 | 21.7 | 19.2 | 20.2 | 18.7 | ||
| A4 | 18.5 | 21.3 | 17.5 | 21.3 | ||
| A5 (least poor) | 17.4 | 18.3 | 19.7 | 17.9 | ||
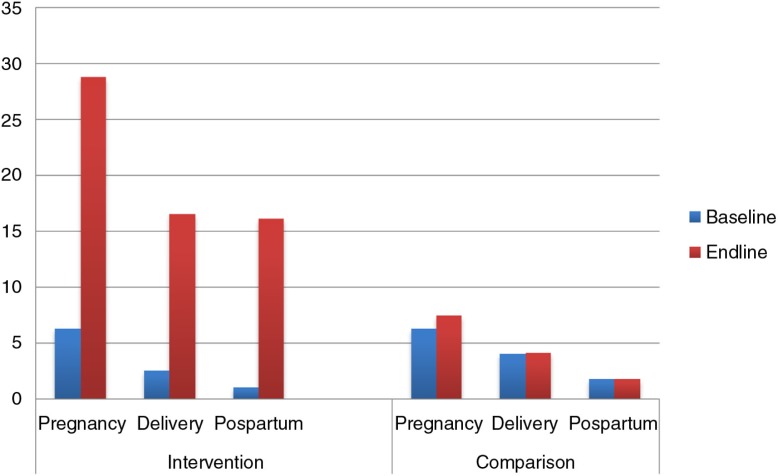
Table 4 presents the effect of the intervention on knowledge of danger signs, knowledge of BP/CR and facility delivery. There was significant improvement in knowledge of danger signs across all the phases, during pregnancy, childbirth, and postpartum (Fig. 2). The knowledge of three or more dangers signs during pregnancy increased significantly by a factor of 4 (6.3% vs. 28.8%) with an NIE of 21.3% (95% CI: 13.7–28.9; p<0.0001) compared to the comparison district. The proportion of men who mentioned three or more danger signs during childbirth improved in the intervention area (2.5% vs. 16.5%) with an NIE of 13.9% (95% CI: 10.5–17.4; p<0.0001). Knowledge of three or more danger signs in the postpartum period also showed improvement in the intervention area compared to the comparison area (1.0% vs. 16.1%) with an NIE of 15.1% (95% CI: 9.2–21: p<0.0001). There was improvement in the spouses’ facility delivery in the intervention area as compared to the comparison area, but with non significant estimate of 12.2% (95% CI: −2.8–27.1: p=0.103).
Table 4.
Effect of the intervention on women's facility delivery, knowledge of danger signs, and knowledge of birth preparedness in intervention and comparison districts at baseline and end line
| Intervention (N=798) | Comparison | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n=725 | n=653 | n=701 | n=658 | ||||||
| Baseline, n (%) | End line, n (%) | Difference (%) | Baseline, n (%) | End line, n (%) | Difference (%) | NIE (%) | 95% CI | p | |
| Wife's facility delivery | 559 (77.1) | 579 (88.7) | 11.6 | 492 (70.2) | 458 (69.6) | −0.6 | 12.2 | −2.8 to 27.1 | 0.103 |
| Knowledge of danger signs | |||||||||
| Knowledge of at least 3 during pregnancy | 46 (6.3) | 188 (28.8) | 22.4 | 44 (6.3) | 49 (7.4) | 1.1 | 21.3 | 13.7 to 28.9 | <0.0001 |
| Knowledge of at least 3 during childbirth (out of 10) | 18 (2.5) | 108 (16.5) | 14.1 | 28 (4.0) | 27 (4.1) | 0.1 | 13.9 | 10.5 to 17.4 | <0.0001 |
| Knowledge of at least 3 during postpartum | 7 (1.0) | 105 (16.1) | 15.1 | 12 (1.8) | 12 (1.8) | 0 | 15.1 | 9.2 to 21 | <0.0001 |
| Knowledge of BP/CR | |||||||||
| Knowledge of at least 3 | 61 (8.4) | 223 (34.9) | 26.5 | 54 (7.7) | 68 (10.3) | 2.6 | 23.9 | 19.7 to 26.3 | 0.0029 |
Significant at p<0.01.
Fig. 2.
Knowledge of three or more danger signs among men in the intervention and comparison districts at baseline and end line.
Table 5 shows the effect of the intervention on male involvement. The proportion of men who accompanied their spouses to ANC improved (51.9% vs. 72.1%) with an NIE of 16.4% (95% CI: 5.6–27.2; p=0.002). For the men accompanying their spouses to delivery, the proportion improved with an NIE of 33.1% (95% CI: 24.1–42.1; p<0.0001). Improvement was observed in shared decision-making about place of delivery in the intervention area compared to the comparison area (46.8% vs. 86.7%), showing a net effect of 38.5% (CI: 28.0–49.1; p<0.0001). Knowledge of at least three danger signs in each phase during pregnancy, three during childbirth, and three during postpartum increased with a net effect of 27% (CI: 15.3–38.5; p<0.0001). The proportion of men who made three or more BP/CR actions increased twofold with an NIE of 26.8% (CI: 15.3–38.2; p<0.0001). Overall, the composite index for male involvement (at least three actions taken out of five possible options: escorting the wife to ANC; escorting the wife to delivery; joint discussion on where to deliver; knowledge of at least three danger signs in each phase during pregnancy, delivery, and postpartum; and practice of at least three BP/CR) improved twofold (39.2% vs. 80.9%), showing an intervention effect of 41.1% (95% CI: 28.5–53.8; p<0.0001).
Table 5.
Effect of the intervention on male involvement in intervention and comparison districts at baseline and end line
| Intervention | Comparison | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n=725 | n=653 | n=701 | n=658 | ||||||
| Baseline, n (%) | End line, n (%) | Difference (%) | Baseline, n (%) | End line, n (%) | Difference (%) | NIE (%) | 95% CI | p | |
| Escorted wife to ANC | 376 (51.9) | 471 (72.1) | 20.3 | 321 (53.4) | 402 (57.3) | 3.9 | 16.4 | 5.6–27.2 | 0.002 |
| Escorted wife to delivery | 339 (46.8) | 526 (80.6) | 33.8 | 289 (48.1) | 342 (48.8) | 0.7 | 33.1 | 24.1–42.1 | <0.0001 |
| Shared decision-making for delivery | 339 (46.8) | 566 (86.7) | 39.9 | 251 (41.8) | 303 (43.2) | 1.4 | 38.5 | 28.0–49.1 | <0.0001 |
| Knowledge of at least 3 danger signs in each of the phases | 322 (44.4) | 471 (72.1) | 27.7 | 236 (33.7) | 226 (34.4) | 0.7 | 27 | 15.5–38.5 | <0.0001 |
| Three or more BP/CR actions | 158 (21.8) | 293 (44.8) | 22.9 | 175 (25.0) | 139 (21.1) | −3.8 | 26.8 | 15.3–38.2 | <0.0001 |
| Male involvement score | 284 (39.2) | 528 (80.9) | 41.7 | 239 (34.1) | 228 (34.7) | 0.5 | 41.1 | 28.5–53.8 | <0.0001 |
NIE, net intervention effect; CI, confidence interval; ANC, antenatal care; BP/CR, birth preparedness and complication readiness.
Significant at p<0.01.
Discussion
This study aimed to evaluate the use of HBLSS training by CHWs to improve male involvement in a rural community in Tanzania. Our study shows that there was a significant improvement in male involvement in matters related to maternal health, such as more men accompanying their wives to ANC and for childbirth. Substantial improvement of their knowledge of obstetric danger signs was observed. Couples’ shared decision-making increased as well, as did making preparations for childbirth and for the possibility of obstetric emergency. Although the wives’ facility delivery rate did increase, it was not significant in relation to the comparison district.
Attending ANC is considered to be one of the most important interventions in reducing maternal morbidity and mortality (45). It is the first step that a pregnant woman takes to make contact with the health system during pregnancy. Men have also been encouraged to attend the visits, as they can obtain information regarding the pregnancy. Our intervention improved the proportion of men who accompanied their wives for ANC visits. A study completed in Pakistan showed similar findings (46). The Pakistani study was a community-based randomised trial using volunteers to disseminate audiocassettes and booklets on maternal and newborn danger signs. It demonstrated that more men accompanied their wives to ANC after the intervention. Acquired knowledge on the importance of ANC conveyed by both male and female CHWs using HBLSS could have contributed to this finding. A recent systematic literature review on the impact of male accompaniment to ANC showed that there is an increase in women's knowledge of danger signs, increased facility delivery, and mixed effects on BP/CR. They argued that the effect could be due to the retention of knowledge of essential information and increased communication between couples (47). These findings suggest the importance of male involvement in maternal healthcare and that strategies such as the community-based training of HBLSS should be advocated.
In many societies, men are seen as decision-makers in matters related to health, nutrition, and access to skilled care for their pregnant spouses. With their power to decide, they need to make informed decisions by acquiring knowledge about recognising danger signs, how to prepare for childbirth, and knowing the importance of ANC and institutional delivery care. Furthermore, involving them can contribute to preventing delays in seeking or reaching care (48). It has been observed in other studies that when men possess this kind of information related to pregnancy and knowledge of danger signs, they stress the importance of their wives delivering in a health facility (41, 49). Evidence from our intervention shows that there was significant improvement in the knowledge of danger signs and knowledge on BP/CR. Similar findings were observed in a study conducted in Nepal (29) where pregnant women were counselled in the health facility together with their husbands. In contrast, randomised controlled studies completed in India and South Africa did not show any improvement of men's knowledge of the women's issues if women and their husbands were counselled together (28, 50). The difference in effect between our Tanzanian study and the others from South Africa and India (28, 50) could be related to the fact that only one-third of men who were invited accompanied their spouses to ANC. In addition, the counselling was done in group sessions and not in sessions with individual couples, which could have contributed to the lack of effect. Hence, those who were not exposed to the intervention could have diluted the effect.
The proportion of men who took more BP/CR actions, such as identifying transport, saving money, and identifying a blood donor, improved significantly in our study. A study conducted in Indonesia called Suami SIAGI used a multimedia entertainment education intervention. The study, which targeted men, showed similar improvement in men making more preparations for birth (51). A higher proportion of South African women who participated in a randomised controlled trial described receiving more assistance from partners in case of an emergency in terms of arranging transport or taking the woman to the doctor if they had received couples’ counselling at the health facility during ANC (28). In this South African study, although the results showed that men did not significantly improve in knowledge of danger signs, there was improvement in BP/CR. This finding can be explained by the fact that the pregnant women received an enhanced ANC package, were provided with booklets that contained information on ANC, and were encouraged to discuss BP/CR with their partners. In a similar study involving Nepalese men and women in ANC counselling provided at a healthcare facility, no improvement was demonstrated in women making more birth preparations (29). The lack of significant effect in the study in Nepal could be due to the mode of education, which was provided at the health facility. Furthermore, the acquisition of knowledge may not translate into taking desired actions. The mixed effects among the studies indicate the need to perform research that investigates the effect of multiple strategies to improve male involvement.
Our findings show improvement in shared decision-making for determining the place of childbirth. This result is quite encouraging, and it has also been shown elsewhere that male involvement leads to more informed couples, for example, in El Salvador (19). When couples discuss issues together it is easier to make decisions regarding, for example, the use of contraceptives, as was seen in the Malawi Male Motivator project (52) and in India (50). In addition, increased couple communication is associated with increased knowledge of maternal and reproductive health services (53). This is important, as fixed gender norms, where the man is the sole decision-maker, are not reinforced and hence health-seeking behaviour is improved (33).
Facility deliveries increased significantly in the intervention area, but compared to the control district the net effect was not significant. An increase in institutional deliveries has also been observed in other intervention studies where couples are counselled together during ANC visits in hospital settings, for example, in Nepal (29). Contrary to this finding, a community-based intervention in Pakistan (46) did not demonstrate any effect on facility deliveries. A plausible explanation for the non-significant increase in facility deliveries compared to the comparison district in our study could be that the delivery rate at baseline was already high and hence no effect could be detected. In contrast, cross-sectional studies have shown that when men accompany their spouses to ANC there is an increased likelihood of facility delivery (41, 47). More research is needed to rigorously evaluate the mechanisms of including men in ANC and the effect on birth preparedness and facility delivery.
This study has shown that gender norms can be challenged when education is provided in a family setting where both men and women are involved. There was improved joint decision-making, and this aspect is important, especially when seeking care. Joint decision-making may imply good relational and spousal communication. Increased male attendance at ANC may also pose a challenge to the health workers at the health facility. The health facility must be able to accommodate men in terms of infrastructure and privacy. Furthermore, training of health workers on how to counsel couples in terms of understanding that health behaviours and outcomes are a result of social norms and socio-economic relationships could be beneficial. Studies on exploring perceptions of men and women in changing gender norms could help in improving such interventions.
Strengths and limitations
It is important to use caution while interpreting the results. Because this was a pretest–post-test quasi-experimental study, there was a risk that bias could have been introduced when interpreting the findings. Employing a cluster-randomised trial method could have avoided this bias. The length of time that elapsed between the events and completion of the questionnaire means that participants' responses might be subject to recall bias. Furthermore, the use of a composite score for male involvement that is not universally defined could also be a limitation. It is important to find a common way of describing male involvement in maternal health so as to be able to compare results with other studies.
One of the strengths of this study was the use of both CHWs and health workers. CHWs are also members of the community and therefore are acceptable for providing the HBLSS education. Training of the health workers could have helped them to improve their day-to-day work and hence may provide improved and more appropriate services for ANC.
Conclusion
Our study has shown that employing CHWs and educating the community using the HBLSS programme improves male involvement in this rural community of Tanzania. The use of CHWs increased men's knowledge of maternal healthcare, improved joint decision-making, and increased accompaniment of spouses to ANC and delivery. It would be possible to scale up this community-based intervention by making home-based ANC visits conducted by CHWs. By increasing health facility deliveries and access to skilled birth attendants, this intervention will make a positive impact on maternal and newborn care.
Acknowledgements
Our special gratitude goes to the Swedish International Development Cooperation Agency for the financial support provided through the Muhimbili University of Health and Allied Sciences. We also thank all of the participants who agreed to be part of the study.
Authors' contributions
FA, ABP, RM, PA, and ED designed the study. FA, ABP, and RM collected the data. FA, ABP, and RM conducted the data analysis. FA wrote the first draft of the manuscript. All authors read the draft and contributed to interpretation of the results. All authors read and approved the final manuscript for submission.
Conflict of interest and funding
The authors declare they have no conflicts of interest.
References
- 1.WHO. WHO recommendations on health promotion interventions for maternal and newborn health. Geneva: WHO; 2015. [PubMed] [Google Scholar]
- 2.UNFPA. International Conference on Population and Development Program of Action 1994. Available from: http://www.un.org/popin/icpd/conference/offeng/poa.html [cited 13 September 2015]
- 3.Promundo, MenEngage, UNFPA. Engaging men and boys in gender equality and health: a global toolkit for action. Rio de Janeiro: UNFPA; 2010. [Google Scholar]
- 4.Davis J, Luchters S, Holmes W. Men and maternal and newborn health: benefits, harms, challenges and potential strategies for engaging men. Melbourne, Australia: Compass: Women's and Children's Health Knowledge Hub; 2012. [Google Scholar]
- 5.Gross K, Alba S, Glass TR, Schellenberg JA, Obrist B. Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy Childbirth. 2012;12:16. doi: 10.1186/1471-2393-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waiswa P, Kemigisa M, Kiguli J, Naikoba S, Pariyo G, Peterson S. Acceptability of evidence-based neonatal care practices in rural Uganda – implications for programming. BMC Pregnancy Childbirth. 2008;8:21. doi: 10.1186/1471-2393-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olayemi O, Bello F, Aimakhu C, Obajimi G, Adekunle A. Male participation in pregnancy and delivery in Nigeria: a survey of antenatal attendees. J Biosoc Sci. 2009;41:493–503. doi: 10.1017/S0021932009003356. [DOI] [PubMed] [Google Scholar]
- 8.Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19:69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- 9.Aarnio P, Chipeta E, Kulmala T. Men's perceptions of delivery care in rural Malawi: exploring community level barriers to improving maternal health. Health Care Women Int. 2013;34:419–39. doi: 10.1080/07399332.2012.755982. [DOI] [PubMed] [Google Scholar]
- 10.Pembe AB, Urassa DP, Darj E, Carlsted A, Olsson P. Qualitative study on maternal referrals in rural Tanzania: decision making and acceptance of referral advice. Afr J Reprod Health. 2008;12:120–31. [PubMed] [Google Scholar]
- 11.August F, Pembe AB, Kayombo E, Mbekenga C, Axemo P, Darj E. Birth preparedness and complication readiness – a qualitative study among community members in rural Tanzania. Glob Health Action. 2015;8 doi: 10.3402/gha.v8.26922. 26922, doi: http://dx.doi.org/10.3402/gha.v8.26922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.August F, Pembe AB, Mpembeni R, Axemo P, Darj E. Men's knowledge of obstetric danger signs, birth preparedness and complication readiness in rural Tanzania. PLoS One. 2015;10:e0125978. doi: 10.1371/journal.pone.0125978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iliyasu Z, Abubakar IS, Galadanci HS, Aliyu MH. Birth preparedness, complication readiness and fathers’ participation in maternity care in a northern Nigerian community. Afr J Reprod Health. 2010;14:21–32. [PubMed] [Google Scholar]
- 14.Dudgeon MR, Inhorn MC. Men's influences on women's reproductive health: medical anthropological perspectives. Soc Sci Med. 2004;59:1379–95. doi: 10.1016/j.socscimed.2003.11.035. [DOI] [PubMed] [Google Scholar]
- 15.Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr. 2004;37:1620–6. doi: 10.1097/00126334-200412150-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peltzer K, Sikwane E, Majaja M. Factors associated with short-course antiretroviral prophylaxis (dual therapy) adherence for PMTCT in Nkangala district, South Africa. Acta Paediatr. 2011;100:1253–7. doi: 10.1111/j.1651-2227.2011.02253.x. [DOI] [PubMed] [Google Scholar]
- 17.Weiss SM, Karl P, Olga V-L, Shikwane ME, Ryan C, Jones DL. Improving PMTCT uptake in rural South Africa. J Int Assoc Provid AIDS Care. 2014;13:269–76. doi: 10.1177/2325957413488203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Exner T, Mantell J, Adeokun L, Udoh I, Ladipo O, Delano G. Mobilizing men as partners: the results of an intervention to increase dual protection among Nigerian men. Heal Educ Res. 2009;24:846–54. doi: 10.1093/her/cyp021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lundgren RI, Gribble JN, Greene ME, Emrick GE, de Monroy M. Cultivating men's interest in family planning in rural El Salvador. Stud Fam Plann. 2005;36:173–88. doi: 10.1111/j.1728-4465.2005.00060.x. [DOI] [PubMed] [Google Scholar]
- 20.Redshaw M, Henderson J. Fathers’ engagement in pregnancy and childbirth: evidence from a national survey. BMC Pregnancy Childbirth. 2013;13:70. doi: 10.1186/1471-2393-13-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carter M. Husbands and maternal health matters in rural Guatemala: wives’ reports on their spouses’ involvement in pregnancy and birth. Soc Sci Med. 2002;55:437–50. doi: 10.1016/s0277-9536(01)00175-7. [DOI] [PubMed] [Google Scholar]
- 22.Yargawa J, Leonardi-Bee J. Male involvement and maternal health outcomes: systematic review and meta-analysis. J Epidemiol Community Health. 2015;69:604–12. doi: 10.1136/jech-2014-204784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alio A, Lewis C, Scarborough K, Harris K, Fiscella K. A community perspective on the role of fathers during pregnancy: a qualitative study. BMC Pregnancy Childbirth. 2013;13:60. doi: 10.1186/1471-2393-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alio A, Mbah A, Kornosky J, Wathington D, Marty P, Salihu H. Assessing the impact of paternal involvement on racial/ethnic disparities in infant mortality rates. J Community Health. 2011;36:63–8. doi: 10.1007/s10900-010-9280-3. [DOI] [PubMed] [Google Scholar]
- 25.Becker S, Mlay R, Schwandt H, Lyamuya E. Comparing couples’ and individual voluntary counseling and testing for HIV at antenatal clinics in Tanzania: a randomized trial. AIDS Behav. 2010;14:558–66. doi: 10.1007/s10461-009-9607-1. [DOI] [PubMed] [Google Scholar]
- 26.Brusamento S, Ghanotakis E, Tudor Car L, Van-Velthoven M, Majeed A, Car J. Male involvement for increasing the effectiveness of prevention of mother-to-child HIV transmission (PMTCT) programmes. Cochrane Database Syst Rev. 2012;10:CD009468. doi: 10.1002/14651858.CD009468.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.UNICEF and Liverpool School of Tropical Medicine. Gender influences on child survival, health and nutrition: a narrative review. New York, NY: UNICEF; 2011. [Google Scholar]
- 28.Kunene B, Beksinska M, Zondi S, Mthembu M, Mullick S, Ottolenghi E. Involving men in maternity care: South Africa. Washington, DC: Population Council; 2004. [Google Scholar]
- 29.Mullany BC, Becker S, Hindin MJ. The impact of including husbands in antenatal health education services on maternal health practices in urban Nepal: results from a randomized controlled trial. Health Educ Res. 2007;22:166–76. doi: 10.1093/her/cyl060. [DOI] [PubMed] [Google Scholar]
- 30.Mullany BC, Hindin MJ, Becker S. Can women's autonomy impede male involvement in pregnancy health in Kathmandu, Nepal? Soc Sci Med. 2005;61:1993–2006. doi: 10.1016/j.socscimed.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 31.Barker G, Das A. Men and sexual and reproductive health: the social revolution. Int J Mens Health. 2004;3:147–53. [Google Scholar]
- 32.Greene ME, Mehta M, Pulerwitz J, Wulf D, Bankole A, Singh S. Involving men in reproductive health: contributions to development. UN Millennium Project; 2004. [Google Scholar]
- 33.Barker G, Ricardo C, Nascimento M. Engaging men and boys in changing gender-based inequity in health: evidence from programme interventions. Geneva: World Health Organization; 2007. [Google Scholar]
- 34.Barker G, Ricardo C, Nascimento M, Olukoya A, Santos C. Questioning gender norms with men to improve health outcomes: evidence of impact. Glob Public Health. 2010;5:539–53. doi: 10.1080/17441690902942464. [DOI] [PubMed] [Google Scholar]
- 35.Kraft JM, Wilkins KG, Morales GJ, Widyono M, Middlestadt SE. An evidence review of gender-integrated interventions in reproductive and maternal-child health. J Health Commun. 2014;19(Suppl 1):122–41. doi: 10.1080/10810730.2014.918216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.MoHSW. Focused antenatal care, malaria and syphilis in pregnancy: orientation package for service providers. Dar es Salaam, Tanzania: MOHSW; 2002. [Google Scholar]
- 37.MOH. National guidelines for prevention of mother to child transmission of HIV. Tanzania: MOH; 2004. [Google Scholar]
- 38.Sibley L, Buffington ST, Beck D, Armbruster D. Home based life saving skills: promoting safe motherhood through innovative community-based interventions. J Midwifery Women's Health. 2001;46:258–66. doi: 10.1016/s1526-9523(01)00139-8. [DOI] [PubMed] [Google Scholar]
- 39.NBS. Population and housing census. Dar es Salaam, Tanzania: National Bureau of Statistics (NBS); 2013. [Google Scholar]
- 40.Pembe A, Urassa D, Carlstedt A, Lindmark G, Nystrom L, Darj E. Rural Tanzanian women's awareness of danger signs of obstetric complications. BMC Pregnancy Childbirth. 2009;9:12. doi: 10.1186/1471-2393-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tweheyo R, Konde-Lule J, Tumwesigye NM, Sekandi JN. Male partner attendance of skilled antenatal care in peri-urban Gulu district, Northern Uganda. BMC Pregnancy Childbirth. 2010;10:53. doi: 10.1186/1471-2393-10-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.JHPIEGO. Monitoring birth preparedness and complication readiness: tools and indicators for maternal and newborn health. Baltimore, MD: JHPIEGO; 2004. [Google Scholar]
- 43.Byamugisha R, Astrom AN, Ndeezi G, Karamagi CA, Tylleskar T, Tumwine JK. Male partner antenatal attendance and HIV testing in eastern Uganda: a randomized facility-based intervention trial. J Int AIDS Soc. 2011;14:43. doi: 10.1186/1758-2652-14-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ampt F, Mon MM, Than KK, Khin MM, Agius PA, Morgan C, et al. Correlates of male involvement in maternal and newborn health: a cross-sectional study of men in a peri-urban region of Myanmar. BMC Pregnancy Childbirth. 2015;15:122. doi: 10.1186/s12884-015-0561-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gupta S, Yamada G, Mpembeni R, Frumence G, Callaghan-Koru JA, Stevenson R, et al. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS One. 2014;9:e101893. doi: 10.1371/journal.pone.0101893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Midhet F, Becker S. Impact of community-based interventions on maternal and neonatal health indicators: Results from a community randomized trial in rural Balochistan, Pakistan. Reprod Health. 2010;7:30. doi: 10.1186/1742-4755-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aguiar C, Jennings L. Impact of male partner antenatal accompaniment on perinatal health outcomes in developing countries: a systematic literature review. Matern Child Health J. 2015;19:2012–19. doi: 10.1007/s10995-015-1713-2. [DOI] [PubMed] [Google Scholar]
- 48.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 49.Aparajita C. Men in maternal care: evidence from India. J Biosoc Sci. 2012;44:129–53. doi: 10.1017/S0021932011000502. [DOI] [PubMed] [Google Scholar]
- 50.Varkey L, Mishra A, Das A, Ottolenghi E, Huntington D, Adamchak S. Involving men in maternity care in India. New Delhi: Population Council; 2004. [Google Scholar]
- 51.Shefner-Rogers C, Sood S. Involving husbands in safe motherhood: effects of the SUAMI SIAGA campaign in Indonesia. J Health Commun. 2004;9:233–58. doi: 10.1080/10810730490447075. [DOI] [PubMed] [Google Scholar]
- 52.Shattuck D, Kerner B, Gilles K, Hartmann M, Ng'ombe T, Guest G. Encouraging contraceptive uptake by motivating men to communicate about family planning: the Malawi Male Motivator project. Am J Public Health. 2011;101:1089–95. doi: 10.2105/AJPH.2010.300091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mutombo N, Bakibinga P, Mukiira C, Kamande E. Benefits of family planning: an assessment of women's knowledge in rural Western Kenya. BMJ Open. 2014;4:e004643. doi: 10.1136/bmjopen-2013-004643. [DOI] [PMC free article] [PubMed] [Google Scholar]