Abstract
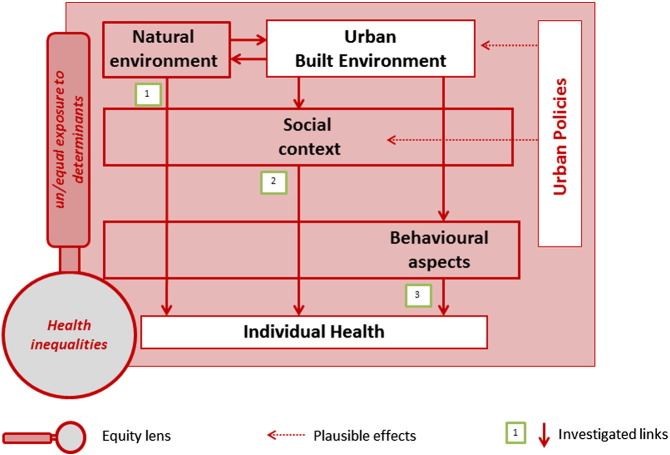
Objective: The Health in All Policies strategy aims to engage every policy domain in health promotion. The more socially disadvantaged groups are usually more affected by potential negative impacts of policies if they are not health oriented. The built environment represents an important policy domain and, apart from its housing component, its impact on health inequalities is seldom assessed. Methods: A scoping review of evidence on the built environment and its health equity impact was carried out, searching both urban and medical literature since 2000 analysing socio-economic inequalities in relation to different components of the built environment. Results: The proposed explanatory framework assumes that key features of built environment (identified as density, functional mix and public spaces and services), may influence individual health through their impact on both natural environment and social context, as well as behaviours, and that these effects may be unequally distributed according to the social position of individuals. Conclusion: In general, the expected links proposed by the framework are well documented in the literature; however, evidence of their impact on health inequalities remains uncertain due to confounding factors, heterogeneity in study design, and difficulty to generalize evidence that is still very embedded to local contexts.
Keywords: Built environment, Health inequalities, Urban health, Neighbourhood, Equity, Health in All Policies
Introduction
A large proportion of the world population is presently living in urban areas, and this trend is going to increase in the future (Global health Observatory GHO data, 2014). According to Barton et al. (2003) urban design is related to inhabitants' health, and its primary objective should be quality of life. It is nowadays fundamental to understand how the urban environment, including physical and social contexts, affects people's health and how this impact varies according to personal characteristics such as social position (O'Donoghue, 2007).
Such health variations are interpreted as social inequalities in health when they affect the poor more than the rich and could be avoidable. In 1991, Dahlgren and Whitehead published a framework that described the role of social determinants of health assuming a progressive influence from general socioeconomic cultural and environmental conditions to individual, through several layers, including the urban environment. Urban setting can be assumed as a field for increasing public health and reducing health inequalities: Barton (2005) explored the effects of planning practice and urban policy-making on health and wellbeing, highlighting the impact of urban built environment on the other components of neighbourhood ecosystems, including both upper (natural resources) and lower layer (local activities, community and people). He endorsed a comprehensive and integrated vision of human settlements as eco-systems, proposing a framework to help urban planners understand the complexity of settlements, and providing an “ecosystem health map”: he set the stage for interdisciplinarity as a need in urban planning practices.
While knowledge on the effects of urban built environment on health starts to be quite developed, with a great attention for physical activity and mental health as the most explored pathways, up to now only few researchers have reviewed impacts of the built environment on health inequalities, and a comprehensive picture based on evidence is missing. Some authors reviewed the literature, but they mainly focused on the effects of some specific urban policies, as Thomson (2008) did with Area based Initiatives in the UK, but some contradictory results emerged mainly because of the macro level of analysis. Northridge and Freeman (2011) deliver a picture of the complexity of causal pathways, comprehensive not only of built environment (specifically ‘urban form’), but collecting evidence also on environmental hazards, social segregation, food environments: they also highlight a strong incoherence in what is known, which may require a lower scale analysis (municipality or neighbourhood) and a focus on specific mechanisms. Starting from this background, we will try to shed a light on specific pathways linking urban environment components to health inequalities.
Objectives
The aim of this work is to identify the most meaningful relationships between built environment and health inequalities in urban areas, in order to provide a logical foundation for both scientific research and policy making.
We attempt to answer to the following questions: does the built environment have any effect on health inequalities by influencing natural environment (link 1), social context (link 2), and behavioural aspects (link 3)?
Built environment is meant here as the space, the physical settlement, where all the activities related to the city take place: it may be described as the complex of buildings, streets, greenspace and infrastructure, considered in its form, networks and aesthetic character. Urban policies go beyond the aim of this article: the status quo of a city is our main object, and we look for evidence limited to socio-economic inequalities.
Methods
Whitehead and Dahlgren (1991)'s framework was the reference model for the scheme used to examine possible links between urban design and health inequalities. The new framework underwent an iterative process of progressive adjustments operated by a multidisciplinary team of experts in urban planning, public health, social and political sciences, based on both literature research and interdisciplinary consensus. According to Whitehead and colleagues, we kept, even if in another graphic shape, the four level over the individual characteristics (namely 1. individual lifestyles factors, 2. social and community networks, 3. living and working conditions – in which we added our focus, the built environment – and 4. general socioeconomic, cultural and environmental conditions). Specifically, we wanted to restrict our attention to a single segment of the third arch (built environment) and to physical conditions of the fourth one (natural environment); due to the tight connections between the two we preferred to put both on the same level. Differently from the reference model, the main causal flows are depicted.
To emphasize the effects on health inequalities we followed a broad scoping approach for searching the literature, adopting selective criteria for articles inclusion, keeping only those really focused on inequalities.
The main effort was in conciliating different approaches to research and knowledge: urban planning literature normally adopts a deductive, expert opinion based method, while public health is grounded in an evidence-based, empirical approach. Because of these two different epistemological approaches, different search methodologies were followed. When looking for characteristics of urban design and their impacts on risk factors, we searched the best literature available on urban field databases (EBSCO, Google scholar, and others) and articles suggested by experts, which helped to focus on mechanisms and their description. When looking for health outcomes, the most common databases belonging to public health domains were searched (Medline, Cihnal, Embase, Cochrane Library): when indexation (Mesh) was available, priority was given to indexed words, otherwise related terms would be searched as text words. Considering the medical competence of these archives, the terms used were related to structural determinants (for example “urban”[tw], “neighbourhood”[tw], “Residential characteristics”[Mesh], “built environment”[tw], “cities”[Mesh]) and to socioeconomic determinants (“socioeconomic factors” [Mesh], “equity”[tw], “health disparities”[Mesh], “inequalities”[tw]), not explicitly to health, which was considered to be intrinsic to the nature of the storage. Related articles were also searched for (without temporal limits). We include papers 1) inquiring about the research questions, 2) reporting any quantitative data about outcomes, 3) concerning residents in urban setting, 4) dealing with high income countries' towns (any size), 5) published after 2000. A synoptic picture of the selection's steps of literature included in the equity focus is shown in Table 1.
Table 1.
Selection process for the review.
| Number of articles | Selected on title | Selected on abstract | Final selection | |
|---|---|---|---|---|
| Link 1 | 2175 | 198 | 37 | 8 |
| Link 2 | 84 | 15 | 7 | 1 |
| Link 3 | 19,252 | 350 | 66 | 10 |
| Reviews (all themes) | 201 | 41 | 18 | 4 |
| Total | 21,712 | 604 | 128 | 23 |
Due to the large amount of articles about all the components of our framework, a systematic approach was beyond our resources. Therefore, this must be considered a scoping review of literature: according to the methodological approach proposed by Anderson et al. (2001), we examined the literature under the guidance of the logical framework, which, in turn, has been modified according to the evidence when necessary.
Reviews of studies were given priority in the selection and, if not available, primary studies were searched. In a complex field like this, we realized that reviews tend to be more generic than specific studies and usually they don't deal with specific topics as those represented in the three links of our model.
Specific attention was paid to inequalities, investigated both as variation in exposure and as an interaction term, and not only as a confounder. Each link was explored looking firstly at the effect of built environment on residents health (non-systematic way) in order to explain the general mechanisms and, secondly, at its effect according to their individual socioeconomic characteristics; this second group of studies was collected more systematically, and is presented in the ‘equity lens’ focus at the end of each link description (Results Section), where any measure of socioeconomic level – simple or composite, aggregated or individual – was considered. We didn't investigate other kind of inequalities (e.g. gender or ethnicity).
Results
We present the review's findings according to the explanatory framework (Fig. 1) that assumes different pathways from the urban built environment to health inequalities. The city, considered as a whole in its physical structure, society and governance (urbs, civitas, polis), is a complex unicum in which places, people and organizations represent the living context. The health of a person, indeed, is influenced by a chain of possible mechanisms: living conditions contribute to define one's health status.
Fig. 1.
Theoretical framework.
People may be differently exposed to health determinants related to the built environment, depending on their location in the city. Neighbourhoods may get unequal resources, opportunities, and capacities as a result of policies (affecting structural and social aspects) according to administrative and political priorities. Inequalities in health may be enhanced when the direction and intensity of the effect of each pathway changes according to individual or aggregate social position.
The first research question tries to explore the link (1) City – Nature – Health. The urban form and natural environment are the physical setting in which people live: living in a healthy or unhealthy environment is often related to socioeconomic conditions.
Individuals are involved in a social network: according to social norms of each neighbourhood, citizens shape their lifestyle and use the city in a heterogeneous way. The second research question investigates the link (2) City – Social Context – Health.
Furthermore, the residents may live in the same city in completely different ways: individual characteristics and behaviour are key factors in health. The third research question investigates the link (3) City – Behavioural Aspects – Health, trying to detect which features of urban design can promote a more equal healthy lifestyle.
This is, of course, a necessary simplification. Actually, no pathway can be completely isolated: confounding, modification effects, intermediate steps are present, with a mutual interference. In the framework, the passage of the arrows through the boxes symbolizes these intermediate steps on the pathways from the built environment to individual health.
Each link includes an equity-focused paragraph: it presents results of studies affording the connection between a structural element of the built environment and health inequalities, investigated at individual level.
Methodological aspects of equity-oriented studies included in the review are synthesised in Table 2. Here, primary studies are separated from reviews. The level of the study area is reported. Variables or indexes that describe the socioeconomic status (SES) are outlined in the Equity Lens column, separating aggregate and individual indicators. The last three columns relate built environment determinants, intermediate risk factors and health outcomes: missing elements are graphically identified as//. Up and down arrows show the direction of exposure to risk or health damage (increasing or decreasing) in low SES in comparison to high SES individuals/groups.
Table 2.
Equity — oriented articles.
| Author year | Setting | Area level | Equity lens — socioeconomic indicator | Built environment determinant | Risk factor | Health outcome |
|---|---|---|---|---|---|---|
| Exposure to risk or health damage for low Socio Economic Status (SES) compared to high SES ↑ increased/ ↓ decreased ↔ no differences* //no measurement *the effect direction is clearly recognizable in primary studies only |
||||||
| Reviews | ||||||
| Laurent et al. (2007) | Worldwide | Town — subareas | Various socioeconomic variables | // | Air pollution | Short term Long term |
| Rosenthal et al. (2007) | USA (New York) | Metropolitan area | Poverty | Town characteristics (built environment) | Heat waves | Cardiovascular death |
| McClellan et al. (2012) | Worldwide | National | Poverty | Healthcare services availability Physical attributes of place (climate, altitude, built environment) |
// | Prevalence of chronic kidney disease |
| White et al. (2012) | USA | Neighbourhood | Ethnicity, income, education | Health care accessibility | // | // |
| Primary studies | ||||||
| Link 1 | ||||||
| Teschke et al. (2010) | Canada | Neighbourhood (census block) | Income | Water provision and sewage disposal | Organic water pollution | Endemic intestinal infectious diseases ↑ |
| Limousi et al. (2014) | France | Neighbourhood (statistical blocks INSEE) | SES (Townsend index 1988) (hospital record) | // | Chemical water pollution | Prevalence of small for gestational age neonates ↑ |
| Havard et al. (2011) | France | Neighbourhood | Income, employment, education, human development index (RECORD cohort Study) | Traffic streets' characteristics | Noise pollution ↓ | // |
| Laussmann et al. (2013) | Germany | Neighbourhood (self reported) Individual (self reported) |
Education, employment, income (DEGSI survey) | Road and air traffic Neighbourhood social characteristics |
Noise pollution | Perceived annoyance ↑ |
| Bocquier et al. (2013) | France | Neighbourhood census block | SES (Havard 2008) | // | Noise pollution ↓ | // |
| Maas et al. (2006) | Netherland | Municipal | Education, ethnicity, employment, health insurance | Availability of green spaces | // | Perceived good general health ↑ |
| Michelozzi et al. (2005) | Italy | Census block | Education (Turin) SES Braga 2001 (Rome) |
// | Heat waves | Death ↑ |
| Reid et al. (2009) | USA | Neighbourhood (census block) | Education, poverty, ethnicity | Lack of green spaces | Heat waves ↑ | // |
| Link 2 | ||||||
| De Donder et al. (2005) | Belgium West Flanders |
Neighbourhood | Income | Neighbourhood structural characteristics | Negative social characteristics ↑ | // |
| Link 3 | ||||||
| Estabrooks et al. (2003) | USA | Neighbourhood (census block) | Employment, income, poverty threshold | Lack of resources for physical activity ↑ | // | // |
| van Lenthe et al. (2005) | Netherland Eindhoven |
Neighbourhood | Education, work, employment (A) | Lack of resources for physical activity | Lack of physical activity ↑ | // |
| Tucker-Seeley et al. (2009) | USA | Neighbourhood | Income, education (RAND 2008) | Lack of safety | Lack of physical activity (HRS) ↔ | // |
| Taylor et al. (2012) | USA | Neighbourhood | Income | Lack of resources for physical activity ↔ | // | // |
| Ellaway et al. (2010) | UK (Scotland) | Neighbourhood | SES (SIMD 2006) | Alcohol outlets ↔ | // | // |
| Schneider and Gruber (2013) | Germany Cologne | Neighbourhood (social area) | Income proxies, employment | Tobacco, alcohol, fast food outlets ↑ | // | // |
| Svastisalee et al. (2012) | Denmark | Neighbourhood | Parental occupational class | Fast food outlets and lack of supermarket near schools | Lack of fruit and vegetable intake (HBSC) of children ↑ | // |
| Chi and Leroux (2012) | USA | County | Poverty, unemployment, food assistance | Lack of healthcare services ↑ | // | // |
| Macintyre et al. (2008) | UK (Scotland) | Neighbourhood (postal code area) | SES (SIMD 2006)(A) | Public services availability ↔ | // | // |
| Edwards et al. (2008) | USA | Neighbourhood (census block) | SES (IMD2004) (A) | // | // | Serious injuries in children pedestrian and cyclists ↑ |
Link 1: Influence of built environment on natural conditions and related effects on health inequalities
We use the definition of natural environment given by European Directive 337/85 on Environmental Impact Assessment1 (ecosystems radiation are not considered for lack of evidence).
Air quality
Density is the main feature of built environment related to air quality in the literature, even if evidence collected is contradictory: it can exacerbate exposure to harmful emission within central areas due to traffic congestion (Frank and Engelke, 2005), but buildings' position, height and permeability are able to favour air movement at ground level, removing pollutants and heat (Ng, 2009). This channelling effect improves also ventilation in residential units at lower floors.
At the same time, some studies showed that worse air quality is found in lower density areas. In the US, where urban sprawl is shaping the majority of cities, Stone (2008) showed that low density metropolitan areas present ozone peaks more often than dense urban areas. This phenomenon persists even when controlling for population size, average temperature and regional emissions of nitrogen oxides and volatile organic compounds.
Equity lens
In the review of Laurent et al. (2007) three studies reported short-term effects on health using socioeconomic variables at very coarse geographic resolutions, but none found differences according to socioeconomic variables, despite very large populations. The studies at finer geographic resolutions produced mixed results: five out of six studies which analysed individual socioeconomic variables reported stronger pollution-mortality associations for people with low SES, even adjusting for behavioural and occupational risk factors (Zanobetti and Schwartz, 2000, Wojtyniak et al., 2001, Filleul et al., 2004, Zeka et al., 2006, included in the Laurent's review).
Climate characteristics
Air temperatures in dense urban areas are generally higher than temperatures in the surrounding rural country (Santamouris et al., 2001). The lack of greenery, the density of particulates' emissions and excessive built surface are the main reasons for higher summer temperatures in denser cities. Solar radiation incident on urban surfaces is absorbed and then transformed into sensible heat, while natural evapotranspiration (typically guaranteed by trees) is impeded. Urban surfaces have also low capability for retaining water, then there are lower levels of evaporation and less cooling near the ground (Kuttler, 2008). Gas emissions from transport and factories and heat production from air conditioning systems worsen the process. As collected in the Basu and Samet review (2002) “persons living in urban environments may be at particularly increased risk for mortality from ambient heat exposure, since urban areas typically have higher heat indexes (combinations of temperature and humidity)” (Lee, 1980) than surrounding suburban or rural areas, a phenomenon known as the “urban heat island effect” (Landsberg, 1981).
Equity lens
Four factors could explain heat waves' effect on health: social vulnerability (education, poverty, ethnicity),social isolation, lack of green spaces, access to air conditioning, and clinical frailty in the elderly (Reid et al., 2009) increasing cardiovascular risks and distress from pre-existing respiratory conditions (Rosenthal et al., 2007). Socioeconomic inequalities in mortality, caused by 2003 heat wave in Italy, were demonstrated in Rome, Turin (Michelozzi et al., 2005) and Barcelona (Borrell et al., 2006).
Soil and water pollution
Soil pollution can result in water pollution if contamination reaches the superficial ground water aquifer. This contamination may occur in both higher and lower density cities: in urban areas, runoff from wide roads and parking lots was found to be the largest source of water pollution (Bannerman et al., 1993); in suburbs, the largest source were chemicals such as those used in lawn care. High numbers of roadways and vehicles contribute to water pollution through contaminants that gather onto impervious surfaces, are washed away by rain and enter a water source through groundwater or streams and rivers. Rains are often acid due to high levels of pollution and the soil is already loaded with hydrocarbons and organic waste which pollute the water. Another cause of water contamination is related to excessive and uncontrolled sewage drainage in over populated areas.
Equity lens
In developed countries, access to drinking water is available to everybody: nonetheless, in some cases, bottled water consumption instead of tap water might lead to different exposure to chemical and bacteriological risk due to the socioeconomic level of people. Contradicting what we could expect, Limousi et al. (2014) demonstrates in a French town a stronger effect of nitrates in drinking tap water among women of the less deprived neighbourhoods during the second trimester of pregnancy and a reduction in their baby's growth. Water supply can be a source of communicable diseases in a rich country such as Canada, and some socio-demographic variables are associated with higher risk, as being females, very young or elder, and to reside in low income areas (Teschke et al., 2010).
Noise pollution
The principal cause of noise pollution reported in urban settings is traffic, followed by neighbours' noise, flights, manufacturing activities and rail transport; noise pollution is associated with hypertension and cardiovascular events (Van Kempen and Babisch, 2012).
Equity lens
In Europe, noise pollution seems to be unequally distributed among socioeconomic groups, with different patterns of inequalities among cities; while in a study conducted in Germany it was found to affect low socioeconomic groups (Laussmann et al., 2013), according to French studies at local level it has greater impact on high and medium SES people (Bocquier et al., 2013, Havard et al., 2011). Research on noise impacts with an equity focus is still an underexplored topic, and evidence is not univocal.
Availability of green areas
In urban areas, attention must be directed towards avoiding potential hazards and coping with noise and visual stimuli; this can lead to mental fatigue, a lowered ability to perform cognitive tasks (Tzoulas et al., 2007). Exposure to nature and wilderness settings can improve cognitive function (Maller et al., 2006), social cohesion, recovery from stress (Van den Berg et al., 2007), mental wellbeing (Coley et al., 1997, Keniger et al., 2013, Jackson, 2003) and pregnancy outcomes (Agay-Shay et al., 2014). Equal opportunities to enjoy green areas are linked to landscape design, pleasantness, vegetation density and maintenance (Jansson et al., 2013), which are related to sense of security and willingness to use parks.
Equity lens
The proportion of green space in people's living environment shows a positive association (stronger in urban areas) with perceived good health of residents: the relation between green space and health could be somewhat stronger for lower socioeconomic groups. According to Maas et al. (2006), residents in large cities with secondary school diploma benefit more from green areas in their living environment. People with primary or no education benefit at an intermediate level (more than higher, less than secondary) from access to green areas.
Link 2: Influences of built environment on social conditions and effects on health inequalities
People's social interactions may influence health either directly, e.g. through biological responses to stress, or indirectly, through healthy behaviours; some studies show different effects of psychosocial factors on different socioeconomic groups (Egan et al., 2008). Proximity and mix of functions are key elements to determine these interactions.
Urban sprawl hinders the use of public spaces and reduces opportunities for casual encounters, weakening social ties and increasing isolation. While those living in historical centres tend enjoy greater social participation (Leyden, 2003), sprawl forces people to commute: those who need to cover long distances to reach their workplace often do not have time and energy to develop meaningful social relationships with neighbours; even family relationships can sustain negative impacts of commuting (Frumkin, 2002, Putnam, 2000) and mental wellbeing may be reduced (Frumkin et al., 2004).
Functional mix, more likely found in denser settlements, generates crossing flows of different city users: people passing by with different destinations discourages ‘ghettoization’ and produces a spontaneous control on the street over the daytime. Availability of public space and green spaces may influence social capital by providing a meeting place for users (Lee and Maheswaran, 2010) and adequate local infrastructures – schools, libraries, leisure facilities – are the first protection against violence: they increase sense of community and opportunities for social cohesion (Moeller, 1997).
The quality of public space contributes to increase the feeling of belonging to a community and influences the perception of crime's risk (Schweitzer et al., 1999): while in private houses locks, fencing or secure entry systems reduce fear, in public space such measures may increase it. Well-designed public lighting can reduce sense of unsafety: it increases visibility, gives a more pleasant impression of the environment, suggests the presence of other people. Bad state of maintenance, dirt, graffiti, litter and other signs of environmental neglect are drivers of fear, reducing the use of common grounds: these are associated with environmental indicators of socio-economic disadvantage as part of a more general sense of ‘rough’ areas (Lorenc et al., 2013).
Environmental and social characteristics of a neighbourhood are able to influence mental health (De Silva et al., 2005, Truong, 2006), causing unhealthy behaviours dictated by fear (lack of physical activity and reduced social relationships) (Stafford et al., 2007, Mair et al., 2009), worsening the social and economic situation of deprived areas in a vicious circle. Where social capital is weak, there are greater chances of contracting illness, since individualism, lack of communication and control networks impede prevention activities and quick therapeutic interventions (De Donder et al., 2005).
Equity lens
Measuring the fear of crime, De Donder et al. (2005) demonstrated that the effect of a spoiled neighbourhood on this feeling is stronger on worse off residents. This is the only article found which analyses the differential effect of built environment through social elements among different groups.
Link 3: Influences of built environment on behaviours and effects on health inequalities
Humans adapt their behaviour to different settings, in order to survive and reproduce. Even if each person reacts differently to external structural and social stimuli, built environment heavily influences behaviour and lifestyles.
Physical activity and active mobility
The built environment influences the need for car use, traffic accidents (Ewing et al., 2003, Mohamed et al., 2014, Dissanayake et al., 2009, Wei and Lovegrove, 2012) and the opportunities for daily physical activity (Ewing et al., 2014, Li et al., 2005, Yen et al., 2009) mainly when it sprawls, invading the land.
Other factors influencing active mobility and physical activity include perceived accessibility, park maintenance and size, availability of amenities, aesthetic features and safety (Wallmann et al., 2012): in adults (Humpel et al., 2002, De Bourdeaudhuij et al., 2003) and adolescents (De Meester et al., 2013, Mota et al., 2005) good perceived quality of outdoor spaces has a relevant effect on active behaviour, even if social factors usually explain greater variability (Van Holle et al., 2012). Watts et al. (2013) highlights the importance of proximity of green spaces to enable physical activity of deprived neighbourhoods' residents, but this results is contradictory with other studies which report that people of low socioeconomic level are less prone to use recreational facilities when available (Giles-Corti and Donovan, 2002).
Equity lens
People living in disadvantaged neighbourhoods often lack access to safe and pleasant green areas, and seem to be therefore less likely to participate in physical activities than those in more affluent neighbourhoods. This is especially evident among worse off elders (Tucker-Seeley et al., 2009). The increased probability of almost never walking, cycling and gardening in leisure time in the most disadvantaged neighbourhoods is partly explained by a poorer urban design (van Lenthe et al., 2005, Estabrooks et al., 2003).
Alcohol drinking and smoking
Neighbourhood characteristics have an independent effect on smoking and drinking behaviours. They act on three mechanisms at least: alcohol and cigarettes' outlets density, social norms and the effects of built environmental quality on the psychological status of residents. The association among outlet density and several kinds of trauma are evident: the availability of alcoholic beverages increases, especially among young people, suicide and mental illness (Pereira et al., 2013), car accidents and criminal assaults (Gruenewald et al., 2006, Campbell et al., 2009) and, at the domestic level, intimate partner violence (McKinney et al., 2012). Furthermore, the feeling of social abandonment generated by areas of decay, seems to induce a tendency towards alcoholism through anxiety and depression (Hill and Angel, 2005).
Equity lens
Ellaway et al. (2010) showed a socio-spatial distribution of outlets in some UK areas, non systematically favouring consumption in low socioeconomic neighbourhoods. The situation seems to be clearer in the study of Schneider and Gruber (2013) in Germany, where the availability of addictive substances seems to have a contextual effect on individual lifestyles.
Eating habits
Neighbourhoods influences eating habits through the availability of healthy food outlets: their distribution in the city may differ according to the area economic level and zoning rules. By functional zoning we mean one function concentrated in one area, as it may happen with concentrated food distribution such as in shopping malls (which is normally accompanied by scarcity of smaller local shops): many people are excluded from access to food by not owning a motor vehicle. Associations were found between individual characteristics and the likelihood of being obese in neighbourhoods with a high-density of fast food restaurants, in comparison with those with a low density (Li et al., 2009).
Equity lens
In some European towns, as area affluence declines, the availability of some potentially health damaging sources (such as cigarettes, alcohol and fast food outlets) increases (Schneider and Gruber, 2013) and when children and youth belonging to low socioeconomic groups have easier access to unhealthy food outlets, they worsen their food habits (Svastisalee et al., 2012).
Care seeking behaviour
Low density areas are significantly correlated with increased response times by the emergency services, accentuated during night hours and by worse road conditions (Trowbridge et al., 2009). Programmed visits for existing health conditions may be reduced (Teach et al., 2006), increasing hospital admissions for acute episodes. The distance from services might also influence compliance with treatment and regular checks, as well as emergency admissions (Graves, 2008) characterised by geographical and structural inequity. Even in denser areas a difficult access to services, determined by the physical characteristics of the city, affects the most disadvantaged groups (especially older people): this may imply diagnostic and therapeutic delays for any conditions, either acute or chronic.
Equity lens
The socioeconomic and environmental context of neighbourhoods may be shaped by segregation and limited opportunities to obtain equitable health care independent of individual-level factors: deprived neighbourhoods may have difficulty in attracting primary- and specialty-care physicians in countries with a strong private component of health care (White et al., 2012). In the same contexts also dental care can be affected by strong inequalities in access due to shortage and geographically unbalanced services allocation (Chi and Leroux, 2012). The role of the built environment and accessibility to health care centres in chronic kidney disease was investigated by McClellan et al. (2012), who reported no significant evidence of inequalities.
Discussion
The explanatory framework (Fig. 1) identifies the more relevant mechanisms through which the built environment might influence health and its social distribution according to the literature.
All the articles reviewed could be placed into the framework, and the pathways followed from the built environment to any health equity effect through natural environment, social context and behaviours, seem to be all connected, partially or totally, to one of the following components: density (e.g. concentration of buildings and population in an area), availability of public spaces and facilities, and integration of different functions within the same neighbourhood. These three components deserve specific attention because of their implications for urban policies, and this can be considered a first finding of our work.
Relatively high density is related with a more efficient use of soil, and with a provision of services accessible to a greater proportion of the population: density often implies proximity (to services, to workplaces, to family and friends). However, when density is too high and uncontrolled, it can lead to overcrowding and congestion, lack of green spaces and higher noise pollution. On the other hand, development spread out over a region (urban sprawl) causes high consumption of land for road infrastructure, environmental decay caused by noise and air pollution. Such a type of development is often related with poor functional mix and low accessibility to primary facilities: significant use of individuals' time, increased risks of accidents and stress, reduced opportunities for daily social and physical activities are often associated with low density (Ewing et al., 2014).
Public space is the place of civic life, where people can exercise their rights and duties (Borja and Muxí, 2003). Wide access to green areas, a careful distribution of services as schools, administrative offices, clinics, hospitals, transport, theatres, and sport facilities offer every citizen the opportunity to equally enjoy the city which foster wellbeing and human development. Public gardens and parks play an important role in relation to health, as they offer a place to meet and to do sports; they improve air quality and users' mental wellbeing (Macintyre and Ellaway, 2000).
Mixed and diverse functions (functional integration), as well as multiplicity of users, encourage the presence of different actors in public space during the whole day and set the basis for safety, control, and integration (Jacobs, 1961). Assorted activities enable people to use common spaces, facilitating a wide open fruition of the city.
The second finding which emerges is that, applying the equity lens to the literature, built environment seems able to influence health inequalities in two ways. Firstly, because people in lower social position who live in more deprived areas are more exposed to the health damaging mechanisms. Secondly, because the health status of socially disadvantaged individuals may reduce the resilience to health damaging factor. The only example where the built environment worsens the living conditions of the more socially advantaged is related to noise pollution in France (Bocquier et al., 2013). The health outcomes identified in these pathways are many and their list may help health monitoring systems to better focus indicators in equity audits of urban policies.
Some limitations arise from this review. In many studies health inequalities are not the main objective of research and assessing health equity impacts requires a multi-step approach to research, measuring inequalities in each layer of the possible causal chain. Moreover, the strength of evidence available in the literature is still inadequate, due to limitations in the quality of study design and in controlling confounding and interaction. The external validity of these studies is questionable: due to the significant effect of context, local research should be accepted for its local validity and should be promoted, without losing the internal validity principia, as a scientific foundation for policy making.
The review explores a maybe too short time period. It demonstrates a large heterogeneity among studies in the way socio-economic level is measured, the level of the geographical aggregate that is considered, and the confounders accounted for. An effort should be made to introduce comparable indicators.
A further lesson of this review is the importance of multidisciplinarity, necessary to go in depth and understanding important pathways linking different domains (urban planning, transport, sociology, environmental psychology, public health and others); as Barton and Tsourou (2000) reported, chief planners from cities participating in the European Healthy Cities movement considered that many planning policies (involving urban form, transport, traffic and social integration) were actually incompatible with health. The reason highlighted by some of them is that “planning focus on the private profit of market interests was at the expense of the everyday needs of citizens” (cited in Barton, 2005).
Beside this need in everyday practice, we noticed while conducting this review that also research is lacking an integration in methods: in order to validate the explanatory framework, a complementary connection between urban planning, that follows experience-based/deductive approach, and the empirical/inductive methods of health research is needed. These two epistemologically different ways of building new knowledge require a compromise between different methods, but they can also offer a logical and evidence based background for both researchers and policy makers.
Conclusions
The main conclusion is that the logical framework (Fig. 1) adequately identifies the more relevant mechanisms through which the built environment may influence health and its social distribution according to the literature. The framework seems particularly useful for both orienting health equity impact assessments of urban policies, and for addressing urban policies to equity, such as required by the Health in All Policies strategy. The literature neither states the relative proportion of health inequalities explained by the built environment effect, nor identifies the more powerful mechanisms contributing to such inequalities; as Northridge and Freeman already noticed in 2011, “the relationship between urban form and health equity is unresolved in the scientific literature likely because the available evidence is narrow in concept and scale” (p.587): this lack of evidence prevents any possibility to set priorities and targets.
However, in many European cities, poorer neighbourhoods have been the target of policies aiming to promote equal access to recreational facilities, to markets and other core public services (Macintyre et al., 2008); the review suggests that ‘equal’ may not be enough. Deprived neighbourhoods may need more tailored investments (on urban policies but also on social and educational interventions) for giving everybody the same advantages afforded by the health promoting role of urban density, public spaces and functional mix.
In any attempt to develop evidence-based policy, decision makers would find in this field of knowledge a fundamental basis to manage both the built and natural environment, and to provide their citizen with safety and wellbeing: research focused on local contexts is interesting for public health staff and local administrators involved in urban planning and land protection in order to guarantee healthy places to live for future generations.
Conflict of interest
The authors declare there is no conflict of interest.
Acknowledgments
This work was supported by the European Community's Seventh Framework Programme (FP7/2007–2013) under grant agreement 278173 (SOPHIE project).
Footnotes
The elements listed in the European Directive 337/85 are: air (quality and climate characteristics, i.e. heath waves), water (ground and underground), soil (geology, geomorphology, pedology, and as non-renewable energy source), natural environment and ecosystems, noise and vibrations, radiation (ionizing or not), landscape (as cultural value).
Contributor Information
Elena Gelormino, Email: gelormino.elena@aslto5.piemonte.it.
Giulia Melis, Email: giulia.melis@siti.polito.it.
Cristina Marietta, Email: cristina.marietta@polito.it.
Giuseppe Costa, Email: giuseppe.costa@unito.it.
References
- Agay-Shay K., Peled A., Valentín Crespo A. Green spaces and adverse pregnancy outcomes. Occup. Environ. Med. 2014;71:562–569. doi: 10.1136/oemed-2013-101961. [DOI] [PubMed] [Google Scholar]
- Anderson L.M., Petticrew M., Rehfuess E. Using logic models to capture complexity in systematic reviews. Res. Synth. Methods. 2001;2:33–42. doi: 10.1002/jrsm.32. [DOI] [PubMed] [Google Scholar]
- Bannerman R.T., Owens D.W., Dodds R.B. Sources of pollutants in Wisconsin stormwater. Water Sci. Technol. 1993;28:241–259. [Google Scholar]
- Barton H. A health map for urban planners: towards a conceptual model for healthy, sustainable settlements. Plann. Healthy Towns Cities. 2005;31(4):339–355. [Google Scholar]
- Barton H., Tsourou C. Spon/WHO; London/Copenhagen: 2000. Health Urban Planning: A WHO Guide to Planning for People. [Google Scholar]
- Barton H., Grant M., Guise R. Taylor & Francis; 2003. Shaping Neighbourhoods: A Guide for Health, Sustainability and Vitality. [Google Scholar]
- Basu R., Samet J.M. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol. Rev. 2002;24:190–202. doi: 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- Bocquier A., Cortaredona S., Boutin C. Small-area analysis of social inequalities in residential exposure to road traffic noise in Marseilles, France. Eur. J. Pub. Health. 2013;23(4):540–546. doi: 10.1093/eurpub/cks059. [DOI] [PubMed] [Google Scholar]
- Borja J., Muxí Z. Electa; Barcelona: 2003. El espacio público: ciudad y ciudadanía. [Google Scholar]
- Borrell C., Marí-Dell'Olmo M., Rodríguez-Sanz M. Socioeconomic position and excess mortality during the heat wave of 2003 in Barcelona. Eur. J. Epidemiol. 2006;21(9):633–640. doi: 10.1007/s10654-006-9047-4. [DOI] [PubMed] [Google Scholar]
- Campbell C.A., Hahn R.A., Elder R. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am. J. Prev. Med. 2009;37(6):556–569. doi: 10.1016/j.amepre.2009.09.028. [DOI] [PubMed] [Google Scholar]
- Chi D.L., Leroux B. County-level determinants of dental utilization for Medicaid- enrolled children with chronic conditions: how does place affect use? Health Place. 2012;18(6):1422–1429. doi: 10.1016/j.healthplace.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coley R., Sullivan W., Kuo F. Where does community grow? The social context created by nature in urban public housing. Environ. Behav. 1997;29:468–494. [Google Scholar]
- De Bourdeaudhuij I., Sallis J., Saelens B. Environmental correlates of physical activity in a sample of Belgian adults. Am. J. Health Promot. 2003;18(1):83–92. doi: 10.4278/0890-1171-18.1.83. [DOI] [PubMed] [Google Scholar]
- De Donder L., Vertè D., Messelis E. Fear of crime and elderly people: key factors that determine fear of crime among elderly people in West Flanders. Ageing Int. 2005;30:363–376. [Google Scholar]
- De Meester F., Van Dyck D., De Bourdeaudhuij I. Does the perception of neighborhood built environmental attributes influence active transport in adolescents. Int. J. Behav. Nutr. Phys. Act. 2013;10:38. doi: 10.1186/1479-5868-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva M., Mc Kenzie K., Harpham T. Social capital and mental illness: a systematic review. J. Epidemiol. Community Health. 2005;59:619–627. doi: 10.1136/jech.2004.029678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dissanayake D., Aryaija J., Wedagama D. Modelling the effects of land use and temporal factors on child pedestrian casualties. Accid. Anal. Prev. 2009;41:1016–1024. doi: 10.1016/j.aap.2009.06.015. [DOI] [PubMed] [Google Scholar]
- Edwards P., Green J., Lachowycz K. Serious injuries in children: variation by area deprivation and settlement type. Arch. Dis. Child. 2008;93(6):485–489. doi: 10.1136/adc.2007.116541. [DOI] [PubMed] [Google Scholar]
- Egan M., Tannahill C., Petticrew M. Psychosocial risk factors in home and community settings and their associations with population health and health inequalities: a systematic meta-review. BMC Public Health. 2008;16:239. doi: 10.1186/1471-2458-8-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellaway A., Macdonald L., Forsyth A., Macintyre S. The socio-spatial distribution of alcohol outlets in Glasgow city. Health Place. 2010;16(1):167–172. doi: 10.1016/j.healthplace.2009.08.007. [DOI] [PubMed] [Google Scholar]
- Estabrooks P.A., Lee R.E., Gyurcsik N.C. Resources for physical activity participation: does availability and accessibility differ by neighborhood socioeconomic status? Ann. Behav. Med. 2003;25(2):100–104. doi: 10.1207/S15324796ABM2502_05. [DOI] [PubMed] [Google Scholar]
- Ewing R., Schieber R., Zegeer C. Urban sprawl as risk factor in motor vehicle occupant and pedestrian fatalities. Am. J. Public Health. 2003;93:1541–1545. doi: 10.2105/ajph.93.9.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing R., Meakins G., Hamidi S. Relationship between urban sprawl and physical activity, obesity, and morbidity — update and refinement. Health Place. 2014;26:118–126. doi: 10.1016/j.healthplace.2013.12.008. [DOI] [PubMed] [Google Scholar]
- Filleul L., Rondeau V., Cantagrel A. Do subject characteristics modify the effects of particulate air pollution on daily mortality among the elderly? J. Occup. Environ. Med. 2004;46(11):1115–1122. doi: 10.1097/01.jom.0000144998.82543.9d. [DOI] [PubMed] [Google Scholar]
- Frank L.D., Engelke P. Multiple impacts of the built environment on public health: walkable places and the exposure to air pollution. Int. Reg. Sci. Rev. 2005;28 193-16. [Google Scholar]
- Frumkin H. Urban sprawl and public health. Public Health Rep. 2002;117 doi: 10.1093/phr/117.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frumkin H., Lawrence F., Richard J. Island Press; Washington DC: 2004. Urban Sprawl and Public Health, Designing, Planning, and Building for Healthy Communities. [Google Scholar]
- Giles-Corti B., Donovan R.J. Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Prev. Med. 2002;35:601–611. doi: 10.1006/pmed.2002.1115. [DOI] [PubMed] [Google Scholar]
- Graves B. Integrative literature review: a review of literature related to geographical information systems, healthcare access, and health out come. Perspect. Health Inf. Manag. 2008;5:11. [PMC free article] [PubMed] [Google Scholar]
- Gruenewald P., Freisthler B., Remer L. Ecological models of alcohol outlets and violent assaults: crime potentials and geospatial analysis. Addiction. 2006;101:666–677. doi: 10.1111/j.1360-0443.2006.01405.x. [DOI] [PubMed] [Google Scholar]
- Havard S., Reich B., Bean K. Social inequalities in residential exposure to road traffic noise: an environmental justice analysis based on the RECORD cohort study. Occup. Environ. Med. 2011;68:366–374. doi: 10.1136/oem.2010.060640. [DOI] [PubMed] [Google Scholar]
- Hill T., Angel R. Neighborhood disorders, psychological distress and heavy drinking. Soc. Sci. Med. 2005;61:965–975. doi: 10.1016/j.socscimed.2004.12.027. [DOI] [PubMed] [Google Scholar]
- Humpel N., Owen N., Leslie E. Environmental factors associated with adults' participation in physical activity: a review. Am. J. Prev. Med. 2002;22:188–199. doi: 10.1016/s0749-3797(01)00426-3. [DOI] [PubMed] [Google Scholar]
- Jackson L. The relationship of urban design to human health and condition. US Environmental Protection Agency. Landsc. Urban Plan. 2003;64:191–200. [Google Scholar]
- Jacobs J. Vintage. 1961. The death and life of great American cities. [Google Scholar]
- Jansson M., Fors H., Lindgren T. Vol. 12. 2013. Perceived personal safety in relation to urban woodland vegetation — a review; pp. 127–133. [Google Scholar]
- Keniger L., Gaston K., Irvine K. Review: what are the benefits of interacting with nature? Int. J. Environ. Res. Public Health. 2013;10:913–935. doi: 10.3390/ijerph10030913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuttler W. The urban climate — basic and applied aspects. In: Marzluff J.L., editor. Urban Ecology. 2008. pp. 233–248. [Google Scholar]
- Landsberg H.E. Academic Press, Inc.; New York, NY: 1981. The Urban Climate. [Google Scholar]
- Laurent O., Bard D., Filleul L. Effect of socioeconomic status on the relationship between atmospheric pollution and mortality. J. Epidemiol. Community Health. 2007;61:665–675. doi: 10.1136/jech.2006.053611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laussmann D., Haftenberger M., Lampert T. Social inequities regarding annoyance to noise and road traffic intensity: results of the German Health Interview and Examination Survey for Adults (DEGS1) Bundesgesundheitsbl. Gesundheitsforsch. Gesundheitsschutz. 2013;56(5-6):822–831. doi: 10.1007/s00103-013-1668-7. [DOI] [PubMed] [Google Scholar]
- Lee D.H. Seventy-five years of searching for a heat index. Environ. Res. 1980;22:331–356. doi: 10.1016/0013-9351(80)90146-2. [DOI] [PubMed] [Google Scholar]
- Lee A., Maheswaran R. The health benefits of urban green spaces: a review of the evidence. J. Public Health. 2010;33(2):212–222. doi: 10.1093/pubmed/fdq068. [DOI] [PubMed] [Google Scholar]
- Leyden K. Social capital and built environment: the importance of walkable neighborhoods. Am. J. Public Health. 2003;93:1546–1551. doi: 10.2105/ajph.93.9.1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F., Fisher K., Bauman A. Neighborhood influences on physical activity in middle-aged and older adults: a multilevel perspective. J. Aging Phys. Act. 2005;13(1):87–114. doi: 10.1123/japa.13.1.87. [DOI] [PubMed] [Google Scholar]
- Li F., Harmer P., Cardinal B. Obesity and the built environment: does the density of neighborhood fast-food outlets matter? Am. J. Health Promot. 2009;23(3):203–209. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limousi F., Albouy-Llaty M., Carles C. Does area deprivation modify the association between exposure to a nitrate and low-dose atrazine metabolite mixture in drinking water and small for gestational age? A historic cohort study. Environ. Sci. Pollut. Res. Int. 2014;21(7):4964–4973. doi: 10.1007/s11356-013-1893-5. [DOI] [PubMed] [Google Scholar]
- Lorenc T., Petticrew M., Whitehead M. Fear of crime and the environment: systematic review of UK qualitative evidence. BMC Public Health. 2013;13:496. doi: 10.1186/1471-2458-13-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas J., Verheij R., Groenewegen P. Green space, urbanity, and health: how strong is the relation? J. Epidemiol. Community Health. 2006;60:587–592. doi: 10.1136/jech.2005.043125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S., Ellaway A. Ecological approaches: rediscovering the role of the physical and social environment. Soc. Epistemol. 2000;332–348 [Google Scholar]
- Macintyre S., Macdonald L., Ellaway A. Do poorer people have poorer access to local resources and facilities? The distribution of local resources by area deprivation in Glasgow, Scotland. Soc. Sci. Med. 2008;67(6):900–914. doi: 10.1016/j.socscimed.2008.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C., Diez Roux A., Shen M. Cross-sectional and longitudinal association of neighborhood cohesion and stressors with depressive symptoms in the Multiethnic Study of Atherosclerosis (MESA) Ann. Epidemiol. 2009;19:49–57. doi: 10.1016/j.annepidem.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maller C., Townsend M., Pryor A. Healthy nature healthy people: ‘contact with nature’ as an upstream health promotion intervention for populations. Health Promot. Int. 2006;21(1) doi: 10.1093/heapro/dai032. [DOI] [PubMed] [Google Scholar]
- McClellan A., Plantinga L., McClellan W. Epidemiology, geography and chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 2012;21(3):323–328. doi: 10.1097/MNH.0b013e3283521dae. [DOI] [PubMed] [Google Scholar]
- McKinney C., Chartier K., Caetano R. Alcohol availability and neighborhood poverty and their relationship to binge drinking and related problems among drinkers in committed relationships. J. Interpers. Violence. 2012;27(13):2703–2727. doi: 10.1177/0886260512436396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michelozzi P., de Donato F., Bisanti L. The impact of the summer 2003 heat waves on mortality in four Italian cities. Euro Surveill. 2005;10(7):161–165. [PubMed] [Google Scholar]
- Moeller D. Harvard University Press; Cambridge: 1997. Environmental Health. [Google Scholar]
- Mohamed R., Vom Hofe R., Mazumder S. Jurisdictional spillover effects of sprawl on injuries and fatalities. Accid. Anal. Prev. 2014;72C:9–16. doi: 10.1016/j.aap.2014.05.028. [DOI] [PubMed] [Google Scholar]
- Mota J., Almeida M., Santos P. Perceived neighbourhood environment and physical activity in adolescent. Prev. Med. 2005;41:834–836. doi: 10.1016/j.ypmed.2005.07.012. [DOI] [PubMed] [Google Scholar]
- Ng E. Policies and technical guidelines for urban planning of high-density cities-air ventilation assessment (AVA) of Hong Kong. Build. Environ. 2009;44(7):1478–1488. doi: 10.1016/j.buildenv.2008.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northridge M., Freeman L. Urban planning and health equity journal of urban health. Bull. N. Y. Acad. Med. 2011;88(3) doi: 10.1007/s11524-011-9558-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donoghue L. Determining indigenous health: opening address to the social determinants of indigenous health short-course, Darwin, 8–12 march 2004. In: Carson B., Dunbar T., Cenhall R., Bailie R., editors. Social Determinants of Indigenous Health. Allen & Unwin; Crows Nest, NSW: 2007. [Google Scholar]
- Pereira G., Wood L., Foster S., Haggar F. Access to alcohol outlets, alcohol consumption and mental health. PLoS One. 2013;8(1) doi: 10.1371/journal.pone.0053461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam R. Simon & Schuster; New York: 2000. Bowling Alone the Collapse and Revival of the American Community. [Google Scholar]
- Reid C.E., O'Neill M.S., Gronlund C.J. Mapping community determinants of heat vulnerability. Environ. Health Perspect. 2009;117(11):1730–1736. doi: 10.1289/ehp.0900683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal J., Sclar E., Kinney P. Links between the built environment, climate and population health: interdisciplinary environmental change research in New York City. Ann. Acad. Med. Singap. 2007;36:834–846. [PubMed] [Google Scholar]
- Santamouris M., Papanikolaou N., Livada I. On the impact of urban climate on the energy consumption of buildings. Sol. Energy. 2001;70(3):201–216. [Google Scholar]
- Schneider S., Gruber J. Neighbourhood deprivation and outlet density for tobacco, alcohol and fast food: first hints of obesogenic and addictive environments in Germany. Public Health Nutr. 2013;16(7):1168–1177. doi: 10.1017/S1368980012003321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweitzer J., Kim J., Mackin J. The impact of the built environment on crime and fear of crime in urban neighbourhoods. J. Urban Technol. 1999;6:59–73. [Google Scholar]
- Stafford M., Chandola T., Marmot M. Association between fear of crime and mental health and physical functioning. Am. J. Public Health. 2007;97:2076–2081. doi: 10.2105/AJPH.2006.097154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone B. Urban sprawl and air quality in large US cities. J. Environ. Manag. 2008;86(4):688–698. doi: 10.1016/j.jenvman.2006.12.034. [DOI] [PubMed] [Google Scholar]
- Svastisalee C., Holstein B., Due P. Fruit and vegetable intake in adolescents: association with socioeconomic status and exposure to supermarkets and fast food outlets. J. Nutr. Metab. 2012;2012 doi: 10.1155/2012/185484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor W.C., Franzini L., Olvera N., Poston W.S.C., Lin G. Environmental audits of friendliness toward physical activity in three income levels. J. Urban Health. 2012;89(2):296–307. doi: 10.1007/s11524-011-9663-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teach S., Guagliardo M., Crain E. Spatial accessibility of primary care pediatric services in an urban environment: association with asthma management and outcome. Pediatrics. 2006;117:4. doi: 10.1542/peds.2005-2000E. [DOI] [PubMed] [Google Scholar]
- Teschke K., Bellack N., Shen H. Water and sewage systems, socio-demographics, and duration of residence associated with endemic intestinal infectious diseases: a cohort study. BMC Public Health. 2010;10:767. doi: 10.1186/1471-2458-10-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson H. A dose of realism for healthy urban policy: lessons from area-based initiatives in the UK. J. Epidemiol. Community Health. 2008;62:932–936. doi: 10.1136/jech.2007.068775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trowbridge M.J., Gurka M.J., O'connor R.E. Urban sprawl and delayed ambulance arrival in the US. Am. J. Prev. Med. 2009;37(5):428–432. doi: 10.1016/j.amepre.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Truong K. A systematic review of relations between neighborhoods and mental health. J. Ment. Health Policy Econ. 2006;9:137–154. [PubMed] [Google Scholar]
- Tucker-Seeley R.D., Subramanian S.V., Li Y., Sorensen G. Neighborhood safety, socioeconomic status, and physical activity in older adults. Am. J. Prev. Med. 2009;37(3):207–213. doi: 10.1016/j.amepre.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzoulas K., Korpela K., Venn S. Promoting ecosystem and human health in urban areas using Green Infrastructure: a literature review. Landsc. Urban Plan. 2007;81:167. [Google Scholar]
- Van den Berg A., Hartig T., Staats H. Preference for nature in urbanized societies: stress, restoration, and the pursuit of sustainability. J. Soc. Issues. 2007;63:79–96. [Google Scholar]
- Van Holle V., Deforche B., Van Cauwenberg J. Relationship between the physical environment and different domains of physical activity in European adults: a systematic review. BMC Public Health. 2012;12:807. doi: 10.1186/1471-2458-12-807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Kempen E., Babisch W. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J. Hypertens. 2012;30(6):1075–1086. doi: 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- van Lenthe F.J., Brug J., Mackenbach J.P. Neighbourhood inequalities in physical inactivity: the role of neighbourhood attractiveness, proximity to local facilities and safety in the Netherlands. Soc. Sci. Med. 2005;60(4):763–775. doi: 10.1016/j.socscimed.2004.06.013. [DOI] [PubMed] [Google Scholar]
- Wallmann B., Bucksch J., Froboese I. The association between physical activity and perceived environment in German adults. Eur. J. Pub. Health. 2012;22(4):502–508. doi: 10.1093/eurpub/ckr069. [DOI] [PubMed] [Google Scholar]
- Watts P., Phillips G., Petticrew M. Physical activity in deprived communities in London: examining individual and neighbourhood-level factors. PLoS One. 2013;8(7) doi: 10.1371/journal.pone.0069472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei V., Lovegrove G. Sustainable road safety: a new (?) neighbourhood road pattern that saves VRU lives. Accid. Anal. Prev. 2012;44(1):140–148. doi: 10.1016/j.aap.2010.12.005. [DOI] [PubMed] [Google Scholar]
- White K., Haas J.S., Williams D.R. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv. Res. 2012;47(3 pt2):1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead M., Dahlgren G. What can be done about inequalities in health? Lancet. 1991;338(8774):1059–1063. doi: 10.1016/0140-6736(91)91911-d. [DOI] [PubMed] [Google Scholar]
- Wojtyniak B., Rabczenko D., Stokwiszewski J. Does air pollution has respect for socio-economic status of people [abstract] Epidemiology. 2001;12:S64. [Google Scholar]
- Yen I., Michael Y., Perdue L. Neighbourhood environment in studies of health of older adults. Am. J. Prev. Med. 2009;37(5):455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanobetti A., Schwartz J. Race, gender, and social status as modifiers of the effects of PM10 on mortality. J. Occup. Environ. Med. 2000;42(5):469–474. doi: 10.1097/00043764-200005000-00002. [DOI] [PubMed] [Google Scholar]
- Zeka A., Zanobetti A., Schwartz J. Individual-level modifiers of the effects of particulate matter on daily mortality. Am. J. Epidemiol. 2006;163(9):849–859. doi: 10.1093/aje/kwj116. [DOI] [PubMed] [Google Scholar]