Abstract
Background: Over one-third of the world’s population is exposed to household air pollution (HAP) but the separate effects of cooking with solid fuel and kerosene on childhood mortality are unclear.
Objectives: To evaluate the effects of both solid fuels and kerosene on neonatal (0-28 days) and child (29 days-59 months) mortality.
Methods: We used Demographic and Health Surveys from 47 countries and calculated adjusted relative risks (aRR) using Poisson regression models.
Results: The aRR of neonatal and child mortality in households exposed to solid fuels were 1.24 (95% CI: 1.14, 1.34) and 1.21 (95% CI: 1.12, 1.30), respectively, and the aRR for neonatal and child mortality in households exposed to kerosene were 1.34 (95% CI: 1.18, 1.52) and 1.12 (95% CI: 0.99, 1.27), controlling for individual, household, and country-level predictors of mortality.
Conclusions: Kerosene should not be classified as a clean fuel. Neonates are at risk for mortality from exposure to solid fuels and kerosene.
Keywords: Biomass, Child mortality, Cooking fuel, Household air pollution, Indoor air pollution, Neonatal mortality, Low and middle income countries, Solid fuels
Introduction
Household air pollution (HAP) from cooking with solid fuels (i.e. coal and biomass) in low and lower middle income countries is associated with adverse health outcomes, particularly for pregnant women, young mothers, and young children.1–3 Mothers and their young children are at disproportionate risk of exposure to HAP because of the increased time that they spend inside the house.4,5 The consequences of HAP begin even before birth. Incomplete combustion from burning solid fuels releases harmful pollutants such as carbon monoxide and polycyclic aromatic hydrocarbons (PAH) into the environment.6,7 Exposure to these pollutants results in intrauterine growth restriction, preterm birth, and low birth weight, which in turn increase the risk of mortality throughout the first 5 years of life.8,9 Children under age 5 who are exposed to particulate matter from HAP are also at increased risk of lower respiratory infections and mortality from pneumonia.10–14
Millenium Development Goal (MDG) 4 is to reduce by two-thirds the 1990 under-five child mortality rate by 2015. Substantial progress has been made toward achieving MDG 4 with a decline in the global under-five mortality rate between 1990 and 2013 from 90 to 46 deaths per 1 000 live births.15 However, there are considerable differences in under-five mortality rates between countries and regions, and greater attention needs to be brought to reducing mortality in the first 28 days of life.15,16Understanding the contribution of HAP to mortality in children under-five is important because HAP exposure is potentially modifiable and reducing exposure could be a method for accelerating progress toward reducing under-five mortality, particularly as HAP is now ranked fourth as a risk factor of mortality worldwide and first in South Asia.17
In September 2010, the United Nations Foundation announced the Global Alliance for Clean Cook Stoves, a public–private partnership to save lives, empower women, improve livelihoods, and combat climate change by creating a thriving global market for clean and efficient household cooking solutions. The Alliance's “100 by 20” goal calls for 100 million homes to adopt clean, efficient stoves and fuels by 2020. Already there is a great urgency to implement improved stoves and fuels and so there is an imminent need to evaluate whether these new stoves actually save lives.18 To do so, it is important to understand the magnitude of the effect of HAP on mortality before new stoves are introduced. Although this has been addressed in several published studies,17,19,20 the recent recognition of the harmful effects of exposure to kerosene has raised questions about the magnitude of the effect of HAP on mortality when kerosene has been categorized as a clean fuel.21,22 Therefore, we reevaluated the relationship between type of cooking fuel used in the household and neonatal and post-neonatal under-five mortality, comparing the effects of kerosene and solid fuels separately with clean fuels (electricity or gas) using data from the Demographic and Health Surveys (DHS).
Methods
DHS are nationally representative surveys conducted approximately every 5 years in many low and lower-middle income countries using multistage stratified probabilistic sampling. Macro International implements DHS with support from in-country data collection agencies and funding largely provided by the United States Agency for International Development. Trained interviewers use model survey questionnaires to attain standardization and comparability across countries. The Household Questionnaire is used to collect information on demographic and health information of household residents and visitors as well as household characteristics, including type of cooking fuel used by the household. The Women's Questionnaire collects a birth history from reproductive-aged women (15–49 years in many countries) including information on age at death of all live-born children; stillbirths are not included in the birth history. All variables in our analysis came from the Household or Women's Questionnaires.
The most recent DHS at the time of analysis from countries with data on household cooking fuel were considered for the analysis. Of 56 country surveys, nine were excluded because they had missing information on whether the mother smoked cigarettes. Data from 47 surveys conducted between 2001 and 2012 were included in the study (Table 1). The 47 countries were categorized into four global regions: Americas, Asia, North Africa and Europe, and Sub-Saharan Africa.
Table 1.
Characteristics of demographic and health surveys participants and households
| Country | Survey year | Household response rate, % | Women response rate, % | Neonatal sample size | Child sample size | Neonatal deaths | Child deaths |
|---|---|---|---|---|---|---|---|
| Americas | |||||||
| Bolivia | 2008 | 98·8 | 95·9 | 17 297 | 16 831 | 466 | 623 |
| Dominican Republic | 2007 | 97·0 | 93·1 | 19 841 | 19 463 | 378 | 291 |
| Guyana | 2009 | 93·2 | 90·1 | 4 214 | 4 128 | 86 | 51 |
| Haiti | 2012 | 99·7 | 98·7 | 11 847 | 11 494 | 353 | 628 |
| Honduras | 2011–2012 | 98·3 | 93·2 | 19 033 | 18 734 | 299 | 247 |
| Nicaragua | 2001 | 94·5 | 92·5 | 13 779 | 13 544 | 235 | 336 |
| Peru | 2012 | 99·0 | 97·3 | 18 247 | 18 013 | 234 | 197 |
| Total | 104 258 | 102 207 | 2 051 | 2 373 | |||
| Asia | |||||||
| Cambodia | 2010 | 99·0 | 97·5 | 15 362 | 14 932 | 430 | 540 |
| India | 2005–2006 | 97·7 | 94·5 | 99 687 | 96 142 | 3 545 | 2 994 |
| Indonesia | 2012 | 99·0 | 95·9 | 34 123 | 33 444 | 679 | 775 |
| Maldives | 2009 | 90·3 | 85·3 | 6 772 | 6 672 | 100 | 62 |
| Nepal | 2006 | 99·6 | 98·4 | 10 969 | 10 581 | 388 | 408 |
| Philippines | 2008 | 99·3 | 98·3 | 12 347 | 12 154 | 193 | 246 |
| Timor Leste | 2009–2012 | 98·2 | 95·2 | 18 620 | 18 146 | 474 | 804 |
| Total | 197 880 | 192 071 | 5 809 | 5 829 | |||
| North Africa and Europe | |||||||
| Albania | 2008–2009 | 97·9 | 98·1 | 3 943 | 3 907 | 36 | 54 |
| Armenia | 2010 | 95·1 | 97·7 | 2 707 | 2 683 | 24 | 28 |
| Egypt | 2005 | 98·9 | 99·5 | 24 685 | 24 203 | 482 | 567 |
| Jordan | 2009 | 97·3 | 97·2 | 17 197 | 16 957 | 240 | 169 |
| Moldova | 2005 | 95·2 | 95·1 | 2 915 | 2 886 | 29 | 27 |
| Ukraine | 2007 | 95·1 | 92·0 | 2 431 | 2 403 | 28 | 20 |
| Total | 53 878 | 53 039 | 839 | 865 | |||
| Sub-Saharan Africa | |||||||
| Benin | 2006 | 99·1 | 94·4 | 26 373 | 25 495 | 878 | 2 161 |
| Burkina Faso | 2010 | 99·2 | 98·4 | 26 672 | 25 862 | 810 | 2 426 |
| Burundi | 2010 | 99·1 | 96·4 | 13 174 | 12 745 | 429 | 823 |
| Congo (Brazzaville) | 2011–2012 | 99·8 | 98·0 | 14 017 | 13 708 | 309 | 716 |
| Congo DR | 2007 | 99·3 | 96·7 | 14 738 | 14 232 | 506 | 1 491 |
| Cote d'Ivoire | 2011–2012 | 98·1 | 92·7 | 12 067 | 11 546 | 521 | 875 |
| Ethiopia | 2011 | 98·1 | 95·0 | 21 503 | 20 679 | 824 | 1 246 |
| Gabon | 2012 | 99·3 | 98·2 | 8 775 | 8 600 | 175 | 361 |
| Ghana | 2008 | 98·9 | 96·5 | 5 018 | 4 860 | 158 | 238 |
| Guinea | 2005 | 99·2 | 97·2 | 11 324 | 10 719 | 605 | 1 311 |
| Kenya | 2008–2009 | 97·7 | 96·3 | 10 387 | 10 072 | 315 | 467 |
| Lesotho | 2009 | 97·6 | 97·9 | 6 092 | 5 871 | 221 | 357 |
| Malawi | 2010 | 98·1 | 96·9 | 34 887 | 33 893 | 994 | 2 385 |
| Mali | 2006 | 98·8 | 96·6 | 25 248 | 23 930 | 1 318 | 3 055 |
| Mozambique | 2011 | 99·8 | 99·1 | 18 074 | 17 532 | 542 | 1 076 |
| Namibia | 2006–2007 | 97·8 | 94·7 | 6 887 | 6 709 | 178 | 349 |
| Niger | 2006 | 97·9 | 95·6 | 16 665 | 16 104 | 561 | 2 068 |
| Nigeria | 2008 | 98·3 | 96·5 | 49 067 | 46 979 | 2 088 | 5 148 |
| Rwanda | 2010 | 99·8 | 99·1 | 16 041 | 15 612 | 429 | 860 |
| Sao Tome | 2008–2009 | 94·2 | 89·8 | 3 284 | 3 230 | 54 | 138 |
| Senegal | 2010–2011 | 98·4 | 92·7 | 20 218 | 19 586 | 632 | 920 |
| Sierra Leone | 2008 | 97·6 | 94·0 | 9 438 | 8 962 | 476 | 1 017 |
| Swaziland | 2006–2007 | 95·2 | 94·1 | 4 194 | 4 097 | 97 | 372 |
| Tanzania | 2010 | 98·8 | 96·4 | 12 914 | 12 587 | 327 | 642 |
| Uganda | 2011 | 95·3 | 93·8 | 12 909 | 12 527 | 382 | 836 |
| Zambia | 2007 | 97·8 | 96·5 | 10 290 | 9 946 | 344 | 835 |
| Zimbabwe | 2010–2011 | 96·0 | 93·3 | 8 366 | 8 171 | 195 | 364 |
| Total | 418 622 | 404 254 | 14 368 | 32 537 | |||
| World | |||||||
| 774 638 | 751 571 | 23 067 | 41 604 |
The outcomes of interest were neonatal (0–28 days) and child (from 29 days to 59 months) mortality. All children alive at the start of the age interval were included in the risk set. The exposure of interest was type of fuel the household “mainly use[s] for cooking,” categorized into clean fuels (electricity, liquid petroleum gas, natural gas, and biogas), kerosene, and solid fuels (coal, charcoal, and biomass such as wood, crop waste, and dung).
We limited the population to singleton births living with their birth mothers at the house surveyed so that type of fuel used in the household was the relevant exposure. We excluded all visitors. The population included children born in the 10 years before the survey to minimize nondifferential misclassification of exposure and incorrect recall of age at death (n = 776 520). Children with missing information on household cooking fuel use (n = 586), whose households responded “other” (n = 415) or “no food cooked in household” (n = 475) to type of cooking fuel used, children with missing information on any covariate (n = 118), and children with inconsistent or unknown ages at death (n = 288) were excluded from the analysis. The final analytic sample size for the neonatal population was 774 638 children from 47 countries representing a weighted sample of 770 577 children; and the final analytic sample size for the child population was 751 571 children from 47 countries representing a weighted sample of 746 616 children.
Individual, household, and country-level characteristics included in the analysis as confounding variables were: sex, birth order, mother's education, mother's age at birth, whether or not she currently smokes cigarettes, household wealth index, urban versus rural residence, and country. All covariates were included as categorical variables. We chose not to include birth weight as a covariate because it is likely on the causal pathway between exposure to HAP and mortality, especially neonatal mortality.23–25 Wealth index is calculated by DHS using principal components analysis to create a country-relative variable that places households into quintiles based on household assets, materials for housing construction, and access to water and sanitation.
We used Poisson regression models that account for survey design, adjusted for clustering effects and individual, household, and country-level characteristics to compare neonatal and child mortality in households using solid fuels and in households using kerosene versus households using clean fuels in each of the four study regions as well as an estimate that combines data from all 47 countries. All analyses were done using STATA software version 12SE. Sampling weights were used to adjust for differences in the probability of household selection and nonresponse, and a domain analysis accounted for analyzing a subpopulation. We used Poisson regression with robust error variance to correct for overestimation of binary data. Results are presented as relative risks with a value of one indicating equal risk of mortality between children living in households using solid fuels or kerosene and children living in households using clean fuels while values greater than one indicate increased risk of mortality among children living in households using solid fuels or kerosene.
Results
The unweighted number of children included in the analysis was 774 638 for the neonatal population and 751 571 for the child population, out of which there were 23 067 (3%) neonatal and 41 604 (6%) child deaths (Table 1). North Africa and Europe had the smallest study populations followed by the Americas, Asia, and Sub-Saharan Africa, which had the largest study populations.
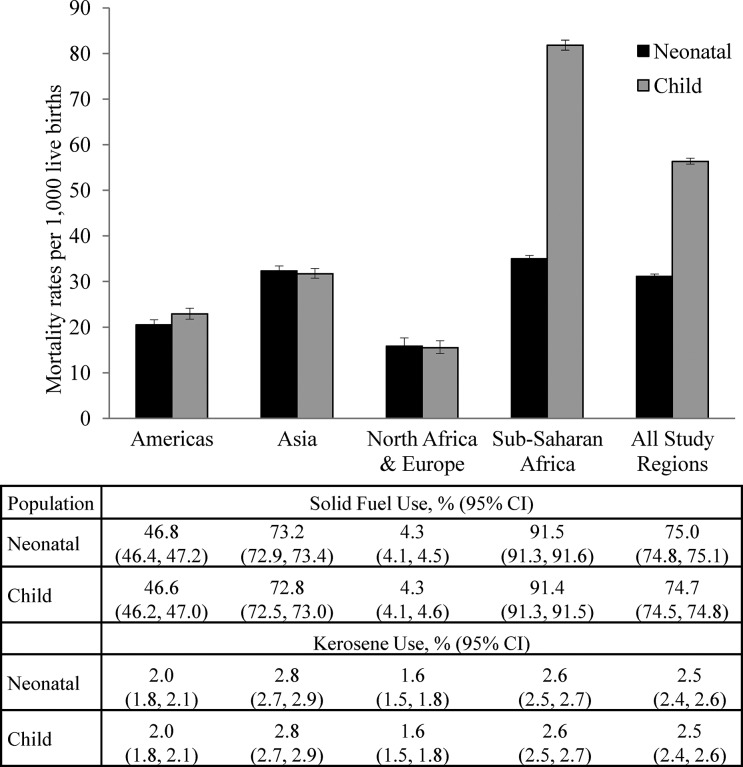
The distribution of fuel use was similar for the neonatal and child populations, with approximately 22.5% of the populations using clean fuels, 2.5% using kerosene, and 75% using solid fuels. The region with the lowest solid fuel and kerosene use was North Africa and Europe (Fig. 1). Sub-Saharan Africa had the highest solid fuel use and Asia had the highest kerosene use. In general, mothers from households using solid fuels were younger, had fewer years of education, and had given birth to more children than mothers from households using clean fuels or kerosene (Table 2). Households using predominantly solid fuels had a lower wealth index and were more often rural compared to households using clean fuels or kerosene.
Figure 1.
Mortality rates and fuel use by region
Table 2.
Weighted distribution of demographic, socioeconomic, and health variables in the neonatal and child populations
| Neonatal population | Child population | |||||
|---|---|---|---|---|---|---|
| Characteristic | Clean fuel 173 824 | Kerosene 19 161 | Solid fuel 577 592 | Clean fuel 170 701 | Kerosene 18 567 | Solid fuel 557 348 |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Maternal education | ||||||
| Secondary or more | 118 407 (68·1) | 11 956 (62·4) | 95 270 (16·5) | 116 548 (68·3) | 11 597 (62·5) | 92 673 (16·6) |
| Primary | 38 561 (22·2) | 4 815 (25·1) | 198 808 (34·4) | 37 694 (22·1) | 4 671 (25·2) | 192 628 (34·6) |
| None | 16 856 (9·7) | 2 389 (12·5) | 283 514 (49·1) | 16 458 (9·6) | 2 299 (12·4) | 272 047 (48·8) |
| Mother's age at childbirth | ||||||
| < 17 | 4 363 (2·5) | 547 (2·9) | 26 665 (4·6) | 4 246 (2·5) | 514 (2·8) | 24 711 (4·4) |
| 18–24 | 73 024 (42·0) | 8 019 (41·9) | 245 498 (42·5) | 71 648 (42·0) | 7 761 (41·8) | 236 522 (42·4) |
| >25 | 96 437 (55·5) | 10 595 (55·3) | 305 430 (52·9) | 94 807 (55·5) | 10 291 (55·4) | 296 115 (53·1) |
| Maternal cigarette smoking | ||||||
| No | 168 193 (96·8) | 18 902 (98·7) | 568 201 (98·4) | 165 196 (96·8) | 18 316 (98·7) | 548 324 (98·4) |
| Yes | 5 631 (3·2) | 259 (1·4) | 9 391 (1·6) | 5 505 (3·2) | 251 (1·4) | 9 025 (1·6) |
| Birth order | ||||||
| First | 59 971 (34·5) | 5 969 (31·2) | 124 019 (21·5) | 58 882 (34·5) | 5 741 (30·9) | 117 923 (21·2) |
| Second or third | 78 562 (45·2) | 8 391 (43·8) | 205 304 (35·5) | 77 324 (45·3) | 8 197 (44·2) | 199 427 (35·8) |
| Fourth born or after | 35 290 (20·3) | 4 800 (25·1) | 248 269 (43·0) | 34 495 (20·2) | 4 628 (24·9) | 239 999 (43·1) |
| Sex of child | ||||||
| Male | 89 319 (51·4) | 9 687 (50·6) | 295 660 (51·2) | 87 510 (51·3) | 9 352 (50·4) | 283 998 (51·0) |
| Female | 84 505 (48·6) | 9 474 (49·4) | 281 932 (48·8) | 83 191 (48·7) | 9·215 (49·6) | 273 351 (49·0) |
| Wealth index | ||||||
| Poorest | 14 642 (8·4) | 1 865 (9·7) | 166 647 (28·9) | 14 351 (8·4) | 1 824 (9·8) | 160 497 (28·8) |
| Poorer | 24 481 (14·1) | 1 796 (9·4) | 142 641 (24·7) | 24 000 (14·1) | 1 760 (9·5) | 137 486 (24·7) |
| Middle | 32 539 (18·7) | 2 829 (14·8) | 120 970 (20·9) | 31 903 (18·7) | 2 753 (14·8) | 116 757 (21·0) |
| Richer | 43 814 (25·2) | 4 955 (25·9) | 94 447 (16·4) | 43 050 (25·2) | 4 778 (25·7) | 91 290 (16·4) |
| Richest | 58 347 (33·6) | 7 716 (40·3) | 52 887 (9·2) | 57 397 (33·6) | 7 453 (40·1) | 51 319 (9·2) |
| Place of residence | ||||||
| Urban | 122 839 (70·7) | 13 216 (69·0) | 109 179 (18·9) | 120 634 (70·7) | 12 800 (68·9) | 105 814 (19·0) |
| Rural | 50 985 (29·3) | 5 945 (31·0) | 468 413 (81·1) | 50 067 (29·3) | 5 767 (31·1) | 451 534 (81·0) |
Mortality rates were lowest in North Africa and Europe and highest in Sub-Saharan Africa with average mortality rates for all regions of 31.1 per 1 000 live births for the neonatal period (0–28 days) and 56.3 per 1 000 live births for the child period (from 29 days to 4 years) (Fig. 1). The unadjusted risk of mortality among neonates living in homes using solid fuels, compared to clean fuels, ranged from 0.59 (0.37, 0.95) in North Africa and Europe to 2.18 (1.97, 2.40) in Asia with a combined risk for all regions of 1.95 (1.85, 2.06); and among children living in homes using solid fuels, compared to clean fuels, the unadjusted risk of mortality ranged from 1.27 (0.90, 1.78) in North Africa and Europe to 2.82 (2.51, 3.16) in Asia with a combined risk for all regions of 3.97 (3.77, 4.18) (Table 3). The unadjusted risk of mortality among neonates living in homes using kerosene, compared to clean fuels, ranged from 1.08 (0.72, 1.62) in the Americas to 1.57 (1.25, 1.96) in Asia with a combined risk for all regions of 1.73 (1.53, 1.94). The risk among children living in homes using kerosene, compared to clean fuels, ranged from 0.88 (0.49, 1.58) in the Americas to 3.86 (2.76, 5.39) in North Africa and Europe with a combined risk for all regions of 2.22 (1.97, 2.50) (Table 4). For all regions combined, the risk of mortality among neonates living in homes using solid fuels, compared to clean fuels, adjusted for individual, household, and country-level characteristics was 1.24 (1.14, 1.34) and the adjusted risk of child mortality was 1.21 (1.12, 1.30). The adjusted risk of mortality among neonates living in homes using kerosene, compared to clean fuel, was 1.34 (1.18, 1.52) and the adjusted risk of child mortality was 1.12 (0.99, 1.27) (Table 5).
Table 3.
Risk of mortality among neonates and children living in homes using solid fuels versus clean fuels by geographic region
| Neonatal mortality | Child mortality | ||||
|---|---|---|---|---|---|
| RR* | 95% CI | p-value | RR* | 95% CI | p-value |
| Unadjusted | |||||
| Americas | |||||
| 1·31 | (1·16, 1·47) | < 0·001 | 2·35 | (2·09, 2·64) | < 0·001 |
| Asia | |||||
| 2·18 | (1·97, 2·40) | < 0·001 | 2·82 | (2·51, 3·16) | < 0·001 |
| North Africa and Europe | |||||
| 0·59 | (0·37, 0·95) | 0·030 | 1·27 | (0·90, 1·78) | 0·171 |
| Sub-Saharan Africa | |||||
| 1·50 | (1·34, 1·69) | < 0·001 | 2·31 | (2·10, 2·53) | < 0·001 |
| All study regions | |||||
| 1·95 | (1·85, 2·06) | < 0·001 | 3·97 | (3·77, 4·18) | < 0·001 |
| Adjusted† | |||||
| Americas | |||||
| 1·20 | (1·01, 1·44) | 0·040 | 1·41 | (1·18, 1·69) | < 0·001 |
| Asia | |||||
| 1·28 | (1·10, 1·49) | 0·001 | 1·14 | (0·97, 1·34) | 0·105 |
| North Africa and Europe | |||||
| 0·77 | (0·44, 1·37) | 0·377 | 1·41 | (0·89, 2·23) | 0·147 |
| Sub-Saharan Africa | |||||
| 1·06 | (0·92, 1·21) | 0·430 | 1·02 | (0·92, 1·13) | 0·713 |
| All study regions | |||||
| 1·24 | (1·14, 1·34) | < 0·001 | 1·21 | (1·12, 1·30) | < 0·001 |
Relative risks, where values greater than 1 indicate increased risk among polluting fuel users.
Adjusted for maternal education, mother's age at birth, if the mother smokes cigarettes, birth order, sex of child, wealth index, urban vs. rural residence, and country of residence.
Table 4.
Risk of mortality among neonates and children living in homes using kerosene versus clean fuels by geographic region
| Neonatal mortality | Child mortality | ||||
|---|---|---|---|---|---|
| RR* | 95% CI | p-value | RR* | 95% CI | p-value |
| Unadjusted | |||||
| Americas | |||||
| 1·08 | (0·72, 1·62) | 0·722 | 0·88 | (0·49, 1·58) | 0·655 |
| Asia | |||||
| 1·57 | (1·25, 1·96) | < 0·001 | 1·47 | (1·06, 2·05) | 0·023 |
| North Africa and Europe | |||||
| 1·41 | (0·77, 2·57) | 0·263 | 3·86 | (2·76, 5·39) | < 0·001 |
| Sub-Saharan Africa | |||||
| 1·52 | (1·27, 1·81) | < 0·001 | 1·39 | (1·20, 1·62) | < 0·001 |
| All study regions | |||||
| 1·73 | (1·53, 1·94) | < 0·001 | 2·22 | (1·97, 2·50) | < 0·001 |
| Adjusted† | |||||
| Americas | |||||
| 0·87 | (0·52, 1·45) | 0·592 | 0·88 | (0·44, 1·74) | 0·707 |
| Asia | |||||
| 1·37 | (1·08, 1·73) | 0·010 | 1·01 | (0·72, 1·41) | 0·959 |
| North Africa and Europe | |||||
| 1·04 | (0·56, 1·92) | 0·898 | 1·56 | (1·10, 2·21) | 0·012 |
| Sub-Saharan Africa | |||||
| 1·22 | (1·01, 1·48) | 0·041 | 0·91 | (0·78, 1·07) | 0·264 |
| All study regions | |||||
| 1·34 | (1·18, 1·52) | < 0·001 | 1·12 | (0·99, 1·27) | 0·073 |
Relative risks, where values greater than 1 indicate increased risk among polluting fuel users.
Adjusted for maternal education, mother's age at birth, if the mother smokes cigarettes, birth order, sex of child, wealth index, urban vs. rural residence, and country of residence.
Table 5.
Multivariate analysis of risk factors of neonatal and child mortality
| Characteristic | Neonatal mortality | Child mortality | ||||
|---|---|---|---|---|---|---|
| RR* | 95% CI | p value | RR* | 95% CI | p value | |
| Household air pollution | ||||||
| Clean fuel | 1 | 1 | ||||
| Kerosene | 1.34 | (1.18, 1.52) | < 0.001 | 1.12 | (0.99, 1.27) | 0.073 |
| Solid fuel | 1.24 | (1.14, 1.34) | < 0.001 | 1.21 | (1.12, 1.30) | < 0.001 |
| Maternal education | ||||||
| Secondary or more | 1 | 1 | ||||
| Primary | 1.22 | (1.15, 1.29) | < 0.001 | 1.42 | (1.36, 1.49) | < 0.001 |
| None | 1.29 | (1.21, 1.37) | < 0.001 | 1.72 | (1.64, 1.81) | < 0.001 |
| Mother's age at childbirth | ||||||
| < 17 | 1 | 1 | ||||
| 18–24 | 0.62 | (0.58, 0.66) | < 0.001 | 0.62 | (0.59, 0.65) | < 0.001 |
| >25 | 0.54 | (0.50, 0.59) | < 0.001 | 0.48 | (0.45, 0.51) | < 0.001 |
| Maternal cigarette smoking | ||||||
| No | 1 | 1 | ||||
| Yes | 1.20 | (1.05, 1.37) | 0.008 | 1.55 | (1.40, 1.71) | < 0.001 |
| Birth order | ||||||
| First born | 1 | 1 | ||||
| Second or third born | 0.68 | (0.65, 0.71) | < 0.001 | 1.08 | (1.04, 1.12) | < 0.001 |
| Fourth or later | 0.83 | (0.78, 0.88) | < 0.001 | 1.30 | (1.25, 1.36) | < 0.001 |
| Sex of child | ||||||
| Male | 1 | 1 | ||||
| Female | 0.77 | (0.75, 0.80) | < 0.001 | 0.98 | (0.95, 1.00) | 0.027 |
| Wealth index | ||||||
| Poorest | 1 | 1 | ||||
| Poorer | 0.98 | (0.93, 1.02) | 0.297 | 0.95 | (0.92, 0.98) | 0.001 |
| Middle | 0.95 | (0.90, 0.99) | 0.035 | 0.88 | (0.85, 0.91) | < 0.001 |
| Richer | 0.91 | (0.86, 0.96) | 0.001 | 0.83 | (0.80, 0.87) | < 0.001 |
| Richest | 0.83 | (0.77, 0.90) | < 0.001 | 0.65 | (0.61, 0.69) | < 0.001 |
| Place of residence | ||||||
| Urban | 1 | 1 | ||||
| Rural | 1.02 | (0.97, 1.07) | 0.393 | 1.00 | (0.96, 1.03) | 0.852 |
Relative risks.
Model also includes country of residence.
Other independent predictors of neonatal and child mortality were male sex, fewer years of maternal education, younger age of the mother at birth, whether the mother smokes cigarettes, and poorer wealth status (Table 5). Being the first born child was predictive of neonatal mortality while being the second born or later was predictive of child mortality.
Discussion
Our study showed that neonatal mortality was increased in households using kerosene and in households using solid fuels, compared to households using gas or electricity. In the post-neonatal period, child mortality through 5 years of age was increased in households using solid fuels, but in households using kerosene the trend toward increased child mortality did not achieve statistical significance. These findings confirm that kerosene should not be categorized as a clean fuel. The data further suggest that the neonatal period is a higher risk period for the effects of exposure to HAP on mortality.
The predominant type of solid fuel used in our study population was wood, which accounted for over 80% of the solid fuel group. Because coal and other forms of biomass (e.g. animal dung and crop waste) comprised a relatively small percentage of the solid fuel group, the effects seen in our study are likely attributable to wood smoke. While assessing exposure to HAP by type of cooking fuel used in the household is a crude estimate of exposure, having a high percentage of wood use within the solid fuel group eliminates some of the heterogeneity from categorizing all solid fuels together.26
Our findings are consistent with other studies that found exposure to HAP is associated with an increased risk of under-five mortality. Bruceet al. (2013) published a systematic review of outcomes associated with HAP for children 0–59 months.19 They found that exposure to HAP and all-cause mortality had a pooled odds ratio of 1.27 (1.07, 1.50), however the five studies that were included varied in the age of the study population (all ranging from 0 to 59 months) and differed in the grouping of kerosene with the clean fuel versus solid fuel group. Our study differed from those of Bruceet al. because we found a strong association between exposure to both solid fuels and kerosene and neonatal mortality. In Bruce's systematic review, both of the studies included in the pooled analysis of neonatal mortality included kerosene in the clean fuel group, which may explain the lack of association between HAP and neonatal mortality.
Our findings on kerosene are similar to those of Epsteinet al., who studied the risk of neonatal mortality from exposure to HAP in India separating out the effects of kerosene, biomass, and coal from the effects of gas.21 In adjusted models, there were significant associations between exposure to kerosene and coal with neonatal mortality but there was not an association between exposure to biomass and neonatal mortality. As discussed previously, it is likely that the effect of solid fuels on mortality in the current study is driven by wood smoke, but since we did not separate the effects of the solid fuel group we cannot comment on whether our results confirm or contradict Epstein's findings on biomass and coal.
Our study confirms previous findings that male gender, fewer years of maternal education, younger age of the mother, maternal smoking, and poorer wealth status are predictors of neonatal and child mortality.21,27–29 Being the firstborn child was protective for child mortality while it was a risk factor for neonatal mortality in our study. Urban versus rural status was not predictive of mortality for either age group.
The biological basis for HAP increasing the risk of mortality in neonates and young children includes increased risk of low birth weight, preterm birth, and pneumonia, which is still the leading cause of death in children under-five.30 Among the pollutants released by insufficient burning of solid fuels are PAH.7 PAH inhaled by a mother enter the blood stream and are able to cross the placenta and reach fetal organs.9 Pereraet al. (1998) found that neonates with increased levels of PAH-DNA adducts (biomarkers for the biologically effective dose of PAH) had decreased birth weight, height, and head circumference.9 Additionally, PAH can trigger oxidative stress leading to an inflammatory response.31 Increased levels of proinflammatory cytokines can trigger preterm birth.32 Carbon monoxide is another pollutant released by insufficient burning of solid fuels.6 Increased exposure to carbon monoxide reduces oxygen in the mother's blood and ultimately oxygen delivery to the placenta.8 Insufficient oxygen during fetal development can lead to intrauterine growth restriction, preterm birth, and low birth weight.8 Finally, exposure to particulate matter from HAP increases the risk of pneumonia in children under-five.10–14
Our study has several strengths. The large study population allowed us to separately analyze the effects of exposure to solid fuels and kerosene. This is of particular importance as many prior studies categorized kerosene with clean fuels. More recently, the harmful effects of kerosene have been recognized. We were also able to assess the separate effects of exposure on neonates and on older infants and children. Finally, we were able to evaluate geographic variation in prevalence of fuel use and effects of HAP.
Our study also has limitations. Our outcome of interest, mortality, is likely underestimated in our population.33 Underreporting of child deaths on the DHS is most common for deaths occurring in early infancy, making the current study sample susceptible to omitted deaths, especially the neonatal population.34 Omission of deaths occurs more frequently among economically and socially disadvantaged groups, who are also more likely to use solid fuels.35 The consequences of underreporting of deaths in our study would bias toward underestimating an association between exposure to solid fuels and mortality. Underreporting of deaths could have affected results such as the adjusted relative risk (aRR) of mortality in Sub-Saharan Africa where solid fuel use was the highest but the 95% confidence interval spanned one for both age groups. Another instance where underreporting of deaths could have affected results is among those living in rural households. Mothers living in rural areas tend to have lower socioeconomic status than mothers in urban areas, and it is possible that mothers living in rural areas underreported deaths more frequently than mothers from urban areas and as a result we did not find an association between rural households and mortality.
The amount of missing data within the DHS limited the covariates that we could include in the analysis. Other predictors of mortality, such as vaccination status and access to healthcare, had up to 80% missing data and were therefore not included. Residual confounding could remain from factors that affect mortality but were not included in the analysis. If there is residual confounding, it could make the effect of solid fuel use and kerosene on mortality appear greater than the true effect.
Finally, exposure to HAP based on predominant type of fuel used for cooking may result in misclassification of exposure, particularly if households predominantly using clean fuel also use solid fuels or kerosene, and vice versa, or if the type of fuel has changed over time. It is likely that further advances in understanding of the health consequences of exposure to HAP will require measurement of household pollutants and this will be particularly important as new stoves and fuels are introduced.
Disclaimer Statements
Contributors Lauren Kleimola was responsible for conceiving and designing the study, obtaining ethics approval, analyzing the data, interpreting the data, drafting, critical revision, and final approval of the article. Archana Patel was responsible for conceiving and designing the study, interpreting the data, critical revision, and final approval of the article. Jitesh Borkar was responsible for analyzing the data and final approval of the article. Patricia Hibberd was responsible for conceiving and designing the study, interpreting the data, drafting, critical revision, and final approval of the article. Lauren Kleimola is the guarantor.
Conflicts of interest The authors have no conflicts of interest to disclose.
Ethics approval
DisclosureThis study uses the existing survey data with all identifying information removed. The ORC Macro institutional review board and the appropriate regulatory board within each country approve the DHS before data collection. Informed consent was obtained from each survey respondent. Approval to use the data for this study was obtained from Measure DHS, and the Partners Human Research Committee, which approves all human-subject research conducted by Partners investigators, reviewed the study and determined that the research was exempt because it did not meet the definition of human subjects research.
References
- 1.Fullerton DG, Bruce N, Gordon SB. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans R Soc Trop Med Hyg. 2008;102(9):843–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bruce N, Perez-Padilla R, Albalak R. Indoor air pollution in developing countries: a major environmental and public health challenge. Bull World Health Organ. 2000;78(9):1078–92. [PMC free article] [PubMed] [Google Scholar]
- 3.Bonjour S, Adair-Rohani H, Wolf J, Bruce NG, Mehta S, Pruss-Ustun A, et al. Solid fuel use for household cooking: country and regional estimates for 1980-2010. Environ Health Perspect. 2013;121(7):784–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Behera D, Dash S, Malik SK. Blood carboxyhaemoglobin levels following acute exposure to smoke of biomass fuel. Indian J Med Res. 1988;88:522–4. [PubMed] [Google Scholar]
- 5.Bruce N, McCracken J, Albalak R, Schei MA, Smith KR, Lopez V et al. , Impact of improved stoves, house construction and child location on levels of indoor air pollution exposure in young Guatemalan children. J Expo Anal Environ Epidemiol. 2004;14:S26–S33. [DOI] [PubMed] [Google Scholar]
- 6.Zhang J, Smith KR, Uma R, Ma Y, Kishore VVN, Lata K et al. , Carbon monoxide from cookstoves in developing countries: 1.Emission factors. Chemosphere Global Change Sci. 1999;1(1–3):353–66. [Google Scholar]
- 7.Bostrom CE, Gerde P, Hanberg A, Jernstrom B, Johansson C, Kyrklund T et al. , Cancer risk assessment, indicators, and guidelines for polycyclic aromatic hydrocarbons in the ambient air. Environ Health Perspect. 2002;110(Suppl 3):451–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Longo LD. The biological effects of carbon monoxide on the pregnant woman, fetus, and newborn infant. Am J Obstet Gynecol. 1977;129(1):69–103. [DOI] [PubMed] [Google Scholar]
- 9.Perera FP, Whyatt RM, Jedrychowski W, Rauh V, Manchester D, Santella RM et al. , Recent developments in molecular epidemiology: a study of the effects of environmental polycyclic aromatic hydrocarbons on birth outcomes in Poland. Am J Epidemiol. 1998;147(3):309–14. [DOI] [PubMed] [Google Scholar]
- 10.Smith KR, McCracken JP, Weber MW, Hubbard A, Jenny A, Thompson LM,et al. . Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised controlled trial. Lancet. 2011;378(9804):1717–26. [DOI] [PubMed] [Google Scholar]
- 11.Misra P, Srivastava R, Krishnan A, Sreenivaas V, Pandav CS. Indoor air pollution-related acute lower respiratory infections and low birthweight: a systematic review. J Trop Pediatr. 2012;58(6):457–66. [DOI] [PubMed] [Google Scholar]
- 12.Smith KR. Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax. 2000;55(6):518–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M, Bruce N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ. 2008;86(5):390C–8C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson AW, Osinusi K, Aderele WI, Gbadero DA, Olaleye OD, Adeyemi-Doro FA. Etiologic agents and outcome determinants of community-acquired pneumonia in urban children: a hospital-based study. J Natl Med Assoc. 2008;100(4):370–85. [DOI] [PubMed] [Google Scholar]
- 15.Wardlaw T, You D, Hug L, Amouzou A, Newby H. UNICEF report: enormous progress in child survival but greater focus on newborns urgently needed. Reprod Health. 2014;11(1):82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lozano R, Wang H, Foreman KJ, Rajaratnam JK, Naghavi M, Marcus JR,et al. . Progress towards millennium development goals 4 and 5 on maternal and child mortality: an updated systematic analysis. Lancet. 2011;378(9797):1139–65. [DOI] [PubMed] [Google Scholar]
- 17.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H,et al. . A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin WJ. Household air pollution in low- and middle-income countries: health risks and research priorities. PLoS Med. 2013;10(6):e1001455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bruce NG, Dherani MK, Das JK, Balakrishnan K, Adair-Rohani H, Bhutta ZA,et al. . Balakrishnan K, Adair-Rohani H, Bhutta ZA,et al. Control of household air pollution for child survival: estimates for intervention impacts. BMC Public Health. 2013;13(Suppl 3):S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pandey S, Lin Y. Adjusted effects of domestic violence, tobacco use, and indoor air pollution from use of solid fuel on child mortality. Matern Child Health J. 2013;17(8):1499–507. [DOI] [PubMed] [Google Scholar]
- 21.Epstein MB, Bates MN, Arora NK, Balakrishnan K, Jack DW, Smith KR. Household fuels, low birth weight, and neonatal death in India: the separate impacts of biomass, kerosene, and coal. Int J Hyg Environ Health. 2013;216(5):523–32. [DOI] [PubMed] [Google Scholar]
- 22.Lam NL, Smith KR, Gauthier A, Bates MN. Kerosene: a review of household uses and their hazards in low- and middle-income countries. J Toxicol Environ Health B Crit Rev. 2012;15(6):396–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.VanderWeele TJ, Mumford SL, Schisterman EF. Conditioning on intermediates in perinatal epidemiology. Epidemiology. 2012;23:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilcox AJ, Weinberg CR, Basso O. On the pitfalls of adjusting for gestational age at birth. Am J Epidemiol. 2011;174:1062–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hernandez-Diaz S, Schisterman EF, Hernan MA. The birth weight “paradox” uncovered? Am J Epidemiol. 2006;164:1115–20. [DOI] [PubMed] [Google Scholar]
- 26.Clark ML, Peel JL, Balakrishnan K, Breysse PN, Chillrud SN, Naeher LP,et al. . Health and household air pollution from solid fuel use: the need for improved exposure assessment. Environ Health Perspect. 2013;121(10):1120–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kazembe L, Clarke A, Kandala NB. Childhood mortality in sub-Saharan Africa: a cross-sectional insight into small-scale geographical inequalities from census data. BMJ Open. 2012;2(5):e001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jehan I, Harris H, Salat S, Zeb A, Mobeen N, Pasha O,et al. . Neonatal mortality, risk factors and causes: a prospective population-based cohort study in urban Pakistan. Bull World Health Organ. 2009;87(2):130–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh R, Tripathi V. Maternal factors contributing to under-five mortality at birth order 1 to 5 in India: a comprehensive multivariate study. Singerplus. 2013;2:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE,et al. . Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61. [DOI] [PubMed] [Google Scholar]
- 31.Nel AE, Diaz-Sanches D, Li N. The role of particulate pollutants in pulmonary inflammation and asthma: evidence for the involvement of organic chemicals and oxidative stress. Curr Opin Pulm Med. 2001;7(1):20–6. [DOI] [PubMed] [Google Scholar]
- 32.Engel SA, Erichsen HC, Savitz DA, Thorp J, Chanock SJ, Olshan AF. Risk of spontaneous preterm birth is associated with common proinflammatory cytokine polymorphisms. Epidemiology. 2005;16(4):469–77. [DOI] [PubMed] [Google Scholar]
- 33.Wang H, Liddell CA, Coates MM, Mooney MD, Levitz CE, Schumacher AE. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9947):957–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mwale MW. National Statistics Office [Malawi], ORC Macro. Infant and child mortality. National Statistics Office [Malawi], ORC Macro, eds. Malawi Demographic and Health Survey 2004:123–132. [Google Scholar]
- 35.National Statistical Office (NSO) [Malawi], and ORC Macro 2005. Malawi Demographic and Health Survey 2004. Calverton, Maryland: NSO and ORC Macro. [Google Scholar]
- 36.Hobcraft JN, McDonald JW, Rutstein SO. Socio-economic factors in infant and child mortality: a cross-national comparison. Popul Stud (Camb). 1984;38:193–223. [PubMed] [Google Scholar]