Abstract
Three phenylpropanoid dimers (1−3) including two new metabolites were isolated from the extract of the twigs of Nectandra leucantha using antileishmanial bioassay-guided fractionation. The in vitro antiparasitic activity of the isolated compounds against Leishmania donovani parasites and mammalian cytotoxicity and immunomodulatory effects were evaluated. Compounds 1−3 were effective against the intracellular amastigotes within macrophages, with IC50 values of 26.7, 17.8, and 101.9 μM, respectively. The mammalian cytotoxicity, given by the 50% cytotoxic concentration (CC50), was evaluated against peritoneal macrophages. Compounds 1 and 3 were not toxic up to 290 μM, whereas compound 2 demonstrated a CC50 value of 111.2 μM. Compounds 1−3 also suppressed production of disease exacerbatory cytokines IL-6 and IL-10 but had minimal effect on nitric oxide production in L. donovani-infected macrophages, indicating that antileishmanial activity of these compounds is mediated via an NO-independent mechanism. Therefore, these new natural products could represent promising scaffolds for drug design studies for leishmaniasis.
Graphical abstract
Leishmaniasis is a neglected tropical disease that affects up to 10% of the world’s population in more than 98 countries or territories, most of which are either poorly developed or developing countries.1 Human visceral leishmaniasis (VL) is the most severe clinical form of leishmaniasis and is potentially fatal. More than 90% of VL cases occur in India, Bangladesh, Nepal, Sudan, and Brazil.2 Current treatment against VL in most endemic countries includes mainly the highly toxic pentavalent antimonials, which have been used in the treatment of all forms of leishmaniasis worldwide as first-line drugs where drug resistance is not present.3–5 Amphotericin B and oral miltefosine have also been used for the treatment of VL.6 However, amphotericin B therapy may be associated with toxicity, and VL relapses have been reported within 6−12 months after miltefosine treatment.7 Owing to these limitations of current therapies for VL, the identification of novel drugs and biochemical targets is essential. Natural products are potential sources of new and selective agents for the treatment of neglected tropical diseases, especially those caused by protozoans.8 Between 1981 and 2006, 1184 new drugs were registered, 28% of which were natural products or derivatives. Another 24% of these new drugs had pharmacophores derived from natural products.9
Lauraceae is one of the major groups of flowering plants (Angiosperms), being predominantly an arboreous family. Distributed throughout tropical and subtropical forests of Southeast Asia and Central/South America, particularly Brazil, Lauraceae contains 68 genera and about 2900 species.10 Phytochemically, this family is known to be a source of alkaloids, phenylpropanoids, lignans, neolignans, nitro derivatives, benzyl esters, pyrones, and flavonoids.11–15 To discover new bioactive antiparasitic compounds from the Brazilian biodiversity, the phytochemical composition of the n-hexane extract of the twigs of Nectandra leucantha Nees & Mart (Lauraceae), which displayed activity against promastigote forms of Leishmania donovani, was investigated. The anti-parasitic activity of metabolites 1−3 (Figure 1) against intracellular L. donovani in macrophages and their in vitro immunomodulatory activity and toxicity against mammalian cells were also assessed.
Figure 1.
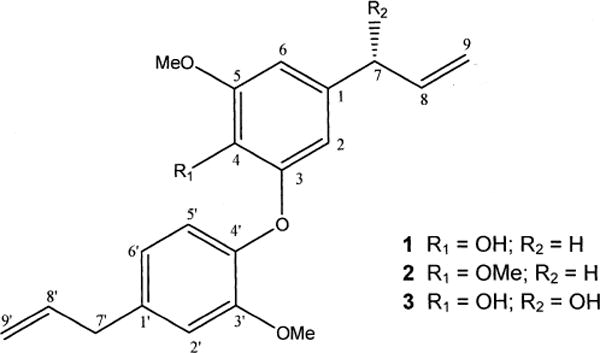
Chemical structures of isolated metabolites 1−3.
RESULTS AND DISCUSSION
The antileishmanial activity of the n-hexane extract of the twigs of N. leucantha was evaluated against promastigotes of L. donovani, demonstrating 100% of parasite death at 200 μg/mL. The crude extract was subjected to a bioguided chromatographic fractionation to afford three bioactive metabolites (1−3).
Compound 1 was identified as dehydrodieugenol B (1-(8-propenyl)-3-[1′-(8′-propenyl)-3′-methoxyphenoxy]-4-hydroxy-5-methoxybenzene), previously isolated from Ocotea cymbarum,16 by comparison of reported 1H NMR and HREIMS data associated with 13C NMR data recorded here for the first time.
Compound 2, isolated as a yellowish oil, showed pseudomolecular ion peaks at m/z 341.1753 [M + H]+ and 363.1585 [M + Na]+ in the HRESIMS, which in conjunction with 13C NMR data corresponded to the molecular formula C21H24O4. This compound showed virtually identical NMR spectra to 1 but displayed additional peaks at δH 3.87 and δC 61.0, attributed to a hindered methoxy group at C-4. Therefore, the structure of compound 2 may be defined as 1-(8-propenyl)-3-[3′-methoxy-1′-(8-propenyl)phenoxy]-4,5-dimethoxybenzene.
Compound 3, isolated as a brownish oil, displayed pseudomolecular HRESIMS ion peaks at m/z 325.1343 [M − H2O + H]+ and 365.1241 [M + Na]+, corresponding to a molecular formula of C20H22O5. The 1H NMR spectrum displayed similarities to that of 1, except for the signal attributed to H-7, which was observed at δ 5.04 (d, J = 6.0 Hz, 1H) and those assigned to H-9 at δ 5.28 (dt, J = 17.0 and 1.5 Hz, H-9a) and 5.14 (dt, J = 10.5 and 1.5 Hz, H-9b). These data suggested the presence of an additional hydroxy group at the allyl side chain. The 13C NMR data displayed the sp2 carbons of the aromatic rings/olefinic functions was well as an oxymethine signal at δ 75.0 (CH), confirming the presence of an additional hydroxy group. Its location at C-7 was determined by analysis of the 2J and 3J HMBC spectrum, which showed correlations between the signal at δ 5.04 (H-7) and those at δ 110.0 (C-6), 104.9 (C-2), and 115.1 (C-9). This spectrum also showed cross-peaks between the signal at δH 3.85 (OCH3) and δC 150.3 (C-3′) as well as between the signal at δH 3.90 (OCH3) and δC 148.1 (C-5), confirming the position of methoxy groups at C-5 and C-3′. The configuration of C-7 was tentatively proposed as R on the basis of comparison of ECD data with those for (R)-phenylethanol,17 including the negative Cotton effect at 260−280 nm. Therefore, the structure of compound 3 was defined as 1-(7R-hydroxy-8-propenyl)-3-[3′-methoxy-1′-(8′-propenyl)-phenoxy]-4-hydroxy-5-methoxybenzene.
The antiparasitic activities of metabolites 1−3 were determined by flow cytometry, and their cytotoxicities were evaluated in peritoneal macrophages by the colorimetric MTT method.18 The in vitro study against the extracellular forms demonstrated that only compound 2 showed activity against the promastigotes, with an IC50 value of 111.8 μM (CI 95% 94.0 to 132.6 μM). Conversely, when 1−3 were tested against the amastigotes, all compounds selectively eliminated the intracellular parasites, but 1 and 2 showed the most promising IC50 values of 26.7 μM (CI 95% 13.8 to 31.7 μM) and 17.8 μM (CI 95% 15.3 to 20.8 μM), respectively, when compared to the standard drug sodium stibogluconate (IC50 13.3 μM).19 Compound 3 also demonstrated activity but to a lesser extent, with an IC50 value of 101.9 μM (CI 95% 80.3 to 129.7 μM). Compound 2 showed toxicity against peritoneal macrophages, with a 50% cytotoxic concentration (CC50) of 111.2 μM (CI 95% 100.5 to 122.8 μM) (Table 1). Furthermore, compounds 1 and 3 showed no toxicity to mammalian cells at concentrations up to >290 μM. Considering the mammalian cytotoxicity and the effectiveness against the intracellular amastigotes, given by the selectivity index (SI), compound 1 showed the most promising value of >11.0. Natural phenylpropanoids have shown antiprotozoal activities, including in vitro antileishmanial activity of the six phenylpropanoids isolated from Smirnowia iranica, with IC50 values ranging from 77 to 880 μM against L. donovani amastigotes and moderate mammalian cytotoxicity.20 The anti-Trypanosoma cruzi activity of other phenylpropanoid derivatives has also been reported.21−27
Table 1.
Anti-L. donovani Activity (IC50) and Cytotoxicity (CC50) against Mammalian Cells (Peritoneal Macrophages) of Metabolites 1−3
| compound | IC50 (μM) CI 95%
|
CC50 (μM) CI 95%
|
||
|---|---|---|---|---|
| promastigotes | amastigotes | mammalian cells | SI | |
| 1 | NA | 26.7 (13.8 to 31.7) | >293.8 | >11.0 |
| 2 | 111.8 (94.0 to 132.6) | 17.8 (15.3 to 20.8) | 111.2 (100.5 to 122.8) | 6.25 |
| 3 | NA | 101.9 (80.3 to 129.7) | >292.1 | >2.9 |
IC50: 50% inhibitory concentration; CC50: 50% cytotoxic concentration (mammalian cells); CI 95%: 95% confidence interval; SI: selectivity index (CC50 mammalian cells/IC50 Leishmania amastigotes); NA: not active. Sodium stibogluconate values:19 IC50 promastigotes (306.8 μM), amastigotes (13.3 μM); CC50 53.4 μM.
Considering the poor or lack of activity of 1 and 3 against the extracellular promastigotes, but a considerable selectivity toward the parasites inside the macrophages, the possible immunomodulatory effects of the phenylpropanoids in Leishmania-infected bone marrow-derived macrophages were investigated.28 The Leishmania-mediated killing could be an event associated with the up-regulation of nitric oxide (NO) by macrophages, induced by different natural metabolites, as described for quinazolinone alkaloids and glycoside derivatives.29,30 However, other natural phenylpropanoids showed inhibitory effects on nitric oxide synthase or even inhibitory effects on the production of NO by macrophages.31,32 In this study, compounds 1−3 induced limited and nonsignificant production of NO in macrophages (data not shown). Thus, their antileishmanial activity could not be ascribed to a direct NO toxicity toward intracellular amastigotes.
Macrophages are the major effector cells responsible for elimination of parasites, which can be activated by distinct signals, leading to their development into functionally distinct subsets with different disease outcomes. Thus, appropriate activation of macrophages is crucial for eliminating this intracellular pathogen.33 Cytokines such as IL-6 and IL-10 play a critical role in regulating macrophage activation. Several clinical as well as experimental studies show that both IL-6 and IL-10 are involved in pathogenesis of VL. For example, high levels of IL-6 are associated with a preceding death event in patients with VL.34 Conversely, Murray has shown that lack of IL-6 accelerates control of VL in IL-6−/− mice.35 It has also been reported that patients with active VL have high serum levels of IL-10 and IL-6 and a higher percentage of IL-10 prior to treatment, indicating their association with disease persistence.36,37 Similarly, in canine VL, disease outcomes correlated with a positive correlation of IL-10 levels in the spleen.38 In the present study, metabolites 1−3 inhibited production of both IL-6 and IL-10 in Leishmania-infected macrophages (Figure 2A and B). Taken together, these findings suggest that antiparasitic activity of the metabolites 1 and 3 could be partly mediated by their ability to down-regulate production of VL-exacerbating cytokines IL-6 and IL-10.
Figure 2.
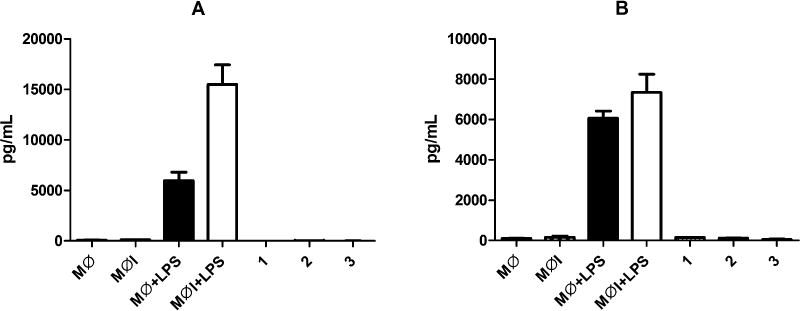
Effect of treatment with metabolites 1−3 isolated from N. leucantha in bone marrow-derived macrophages (BMDMs) infected with L. donovani parasites. MØ (macrophages); MØI (infected macrophages); MØ+LPS (macrophages plus LPS); MØI+LPS (infected macrophages plus LPS). IL-6 (A) and IL-10 (B) cytokines levels were measured by ELISA in supernatant from BMDMs treated for 72 h. Mean cytokine level was expressed as pg/mL ± SE.
Considering the effective antileishmanial activity of the phenylpropanoid dimer 1 against intracellular amastigotes, without considerable mammalian toxicity and its promising immunomodulatory activity on macrophages, these results suggest this compound as a candidate for future experimental preclinical assays against VL. Further studies may be necessary to investigate the possible metabolism of these phenylpropanoid derivatives by macrophages, to support the hypothesis of a prodrug effect.39
EXPERIMENTAL SECTION
General Experimental Procedures
Optical rotations were measured on a JASCO DIP-370 digital polarimeter (Na filter, λ = 588 nm), and electronic circular dichroism (ECD) analysis was performed using MeOH on a JASCO J-720 spectropolarimeter. UV spectra were recorded on a UV/visible Shimadzu 1650-PC spectrophotometer. IR spectra were obtained on a Shimadzu IR Prestige-21 spectrophotometer. 1D and 2D NMR spectra were recorded at 300 and 75 MHz on a Bruker Ultrashield 300 Avance III spectrometer. CDCl3 (Aldrich) was used as the solvent with TMS as the internal standard. HRESIMS spectra were measured on a Bruker Daltonics MicroTOF QII spectrometer. Silica gel (Merck, 230−400 mesh) was used for column chromatography (CC), and silica gel 60 PF254 (Merck) was used for analytical and preparative TLC separations. For all extraction and chromatography procedures, analytical grade solvents (Labsynth Ltd.) were used.
Plant Material
Twigs of Nectandra leucantha Nees & Mart (Lauraceae) were collected in Cubatão, São Paulo, Brazil, in December 2012, and the plant species was identified by Euder G. A. Martins. A voucher specimen (EM357) has been deposited in the Herbarium of the Institute of Biosciences, University of São Paulo, SP, Brazil.
Extraction and Isolation
The air-dried twigs of N. leucantha (320 g) were powdered and exhaustively extracted with n-hexane. This material was filtered and concentrated under vacuum to afford 10 g of n-hexane extract. Part of this (9 g) was subjected to column chromatography over silica gel (400 g, 60 × 5.5 cm) using increasing amounts of EtOAc in n-hexane and MeOH in EtOAc to afford 12 fractions (A to L). After antiparasitic evaluation, fractions C (eluted with n-hexane/EtOAc, 9:1, 1 g), F (eluted with n-hexane/EtOAc, 7:3, 1.52 g), and I (eluted with n-hexane/EtOAc, 1:1, 250 mg) displayed activity and were submitted to further purification procedures. Part of fraction C (40 mg), F (40 mg), and I (60 mg) were subjected to SiO2 preparative TLC (n-hexane/EtOAc, 7:3) to afford, respectively, 2 (25 mg), 1 (29 mg), and 3 (30 mg).
1-(8-Propenyl)-3-[1′-(8′-propenyl)-3′-methoxyphenoxy]-4-hydroxy-5-methoxybenzene (1, dehydrodieugenol B): brownish oil; UV (MeOH) λmax (log ɛ) 215 (3.2), 280 (2.3) nm; 1H NMR (CDCl3, 300 MHz) δ 6.89 (1H, d, J = 8.1 Hz, H-5′), 6.79 (1H, d, J = 2.0 Hz, H-2′), 6.70 (1H, dd J = 8.1 and 2.0 Hz, H-6′), 6.49 (1H, J = 1.8 Hz, H-2), 6.40 (1H, d, J = 1.8 Hz, H-6), 5.93 (1H, m, H-8′), 5.92 (1H, m, H-8), 5.06 (2H, m, H-9a and H-9′), 3.89 (3H, s, 5-OCH3), 3.86 (3H, s, 3′-OCH3), 3.36 (1H, d, J = 6.6 Hz, H-7′), 3.24 (1H, d, J = 6.6 Hz, H-7); 13C NMR (CDCl3, 75 MHz) δ 150.4 (C, C-3′), 147.8 (C, C-5), 144.4 (C, C-3), 144.2 (C, C-4′), 137.4 (CH, C-8′), 137.2 (CH, C-8), 136.4 (C, C-1′), 135.2 (C, C-4), 131.0 (C, C-1), 120.8 (CH, C-6′), 119.5 (C, C-5′), 116.0 (CH2, C-9′), 115.7 (CH2, C-9), 112.9 (CH, C-2′), 111.8 (CH, C-6), 107.3 (CH, C-2), 56.2 (CH3, 5-OCH3), 55.9 (CH3, 3′-OCH3), 40.0 (CH2, C-7), 39.9 (CH2, C-7′); HRESIMS m/z 327.1595 [M + H]+ and 349.1423 [M + Na]+ (calculated for C20H23O4, 327.1596 and for C20H22O4Na, 349.1416).
1-(8-Propenyl)-3-[3′-methoxy-1′-(8-propenyl)phenoxy]-4,5-dimethoxybenzene (2): yellowish oil; UV (MeOH) λmax (log ɛ) 220 (3.2), 280 (2.5) nm; IR (KBr) νmax 2955, 2850, 1642, 1510, 1460, 1384, 1163, 978, 915, 832, 724, 593 cm−1; 1H NMR (CDCl3, 300 MHz) δ 6.81 (1H, d, J = 8.1 Hz, H-5′), 6.69 (1H, dd J = 8.1 and 2.0 Hz, H-6′), 6.79 (1H, d, J = 2.0 Hz, H-2′), 6.48 (1H, J = 1.8 Hz, H-2), 6.27 (1H, d, J = 1.8 Hz, H-6), 5.93 (2H, m, H-8 and H-8′), 5.06 (2H, m, H-9a and H-9′), 3.87 (6H, s, 4-OCH3/3′-OCH3), 3.83 (3H, s, 5-OCH3), 3.37 (1H, d, J = 6.6 Hz, H-7′), 3.24 (1H, d, J = 6.6 Hz, H-7); 13C NMR (CDCl3, 75 MHz) δ 153.5 (C, C-3′), 150.6 (C, C-5/C-4′), 144.1 (C, C-3), 138.1 (C, C-4), 137.4 (CH, C-8), 137.1 (CH, C-8′), 136.0 (C, C-1′), 135.5 (C, C-1), 120.7 (CH, C-6′), 119.4 (C, C-5′), 115.9 (CH2, C-9/C-9′), 113.1 (CH, C-2′), 111.4 (CH, C-6), 107.3 (CH, C-2), 61.0 (CH3, 4-OCH3), 56.1 (CH3, 5-OCH3), 56.0 (CH3, 3′-OCH3), 40.1 (CH2, C-7′), 40.0 (CH2, C-7); HRESIMS m/z 341.1753 [M + H]+ and 363.1585 [M + Na]+ (calculated for C21H25O4, 341.1753 and for C21H24O4Na, 363.1572).
1-[(7R)-Hydroxy-8-propenyl]-3-[3′-methoxy-1′-(8′-propenyl)-phenoxy]-4-hydroxy-5-methoxybenzene (3): brownish oil; [α]25D −0.01 (c 0.01, MeOH); UV (MeOH) λmax (log ɛ) 275 (4.0), 285 (3.9), 325 (3.7) nm; IR (film) νmax 2928, 2852, 1640, 1508, 1463,1365, 1130, 996, 918, 831, 745, 540 cm−1; 1H NMR (CDCl3, 300 MHz) δ 6.90 (1H, d, J = 8.1 Hz, H-5′), 6.79 (1H, d, J = 2.0 Hz, H-2′), 6.71 (1H, dd, J = 8.1 and 2.0 Hz, H-6′), 6.70 (1H, J = 2.0 Hz, H-2), 6.56 (1H, d, J = 2.0 Hz, H-6), 5.96 (2H, m, H-8 and H-8′), 5.28 (1H, dt, J = 17.0 and 1.5 Hz, H-9a), 5.14 (1H, dt, J = 10.5 and 1.5 Hz, H-9b), 5.09 (1H, m, H-9′), 5.04 (1H, d, J = 6.0 Hz, H-7), 3.90 (3H, s, 5-OCH3), 3.85 (3H, s, 3′-OCH3), 3.37 (1H, d, J = 6.6 Hz, H-7′); 13C NMR (CDCl3, 75 MHz) δ 150.3 (C, C-3′), 148.1 (C, C-5), 144.5 (C, C-3), 144.0 (C, C-4′), 140.0 (CH, C-8), 137.4 (CH, C-8′), 136.6 (C, C-1′), 136.4 (C, C-4), 133.8 (C, C-1), 120.9 (CH, C-6′), 119.9 (C, C-5′), 116.0 (CH2, C-9′), 115.1 (CH2, C-9), 113.0 (CH, C-2′), 110.0 (CH, C-6), 104.9 (CH, C-2), 75.0 (CH, C-7), 56.3 (CH3, 5-OCH3), 56.0 (CH3, 3′-OCH3), 39.9 (CH2, C-7′); HRESIMS m/z 325.1343 [M − H2O + H]+ and 365.1241 [M + Na]+ (calculated for C20H21O4, 325.1440 and C20H22O5Na, 365.1365).
Mice
C57BL/6 and BALB/c mice were purchased from Harlan Laboratories (Indianapolis, IN, USA). The mice were maintained in a pathogen-free animal facility at The Ohio State University (Columbus, OH, USA) in accordance with U.S. National Institutes of Health and Institutional guidelines.
Parasites
Dsred2-L. donovani were previously generated from L. donovani strain LV82 expressing firefly luciferase and a red fluorescent protein.40 Parasites were maintained by serial passage of amastigotes isolated from the spleen of BALB/c mice previously infected. The animals were infected with 1 × 107 Dsred2-L. donovani amastigotes in 100 μL by intravenous route into the tail vein.
Evaluation of in Vitro Anti-L. donovani Activity
DsRed2-L. donovani promastigotes (1 × 106) were incubated in the presence of the isolated metabolites 1−3, dissolved in DMSO and diluted in M-199 medium supplemented with 10% of FCS, at 28 °C for 48 h. Parasites were incubated in the presence of increasing concentrations of compounds: 5 to 300 μM. After 48 h, parasites were centrifuged at 1250g for 5 min and resuspended in 500 μL of PBS, and the parasite viability was measured by flow cytometry to quantify the proportion of dead/live parasites assessed by the loss of fluorescence. Untreated or control treated with DMSO (0.5%) parasites were used as live cell control; parasites treated with 66.68 μM saponin from Q. saponaria (Sigma-Aldrich) were incubated for 30 min and used as an internal control for permeabilization.
Bone Marrow-Derived Macrophages (BMDMs) and in Vitro Infection
BMDMs were isolated from long bones (femurs and tibias) of C57BL/6 mice.41 The differentiated cells (macrophages) were seeded into the 24-well plate at 3.5 × 106/well. After 24 h, DsRed2-L. donovani promastigotes were used to infect BMDMs at a 1:10 ratio (1 macrophage/10 promastigotes), and the extracellular parasites were washed twice with fresh warm media. Infected macrophages were incubated in the presence of increasing concentrations of all compounds: 5 to 300 μM. After 72 h, supernatants were collected to perform the cytokine ELISA and NO assays. Infected BMDMs were centrifuged at 1250g for 10 min and resuspended in 500 μL of PBS, and the quantification of infected cells was measured by flow cytometry as previously described. Control treated with DMSO (0.5%) macrophages infected with DsRed2-L. donovani were used as controls.
Evaluation of in Vitro Mammalian Toxicity
Peritoneal macrophages from BALB/c mice were seeded at 1 × 105 cells/well in 96-well microplates and incubated with all compounds in the presence of increasing concentrations (0.2 to 600 μM) for 48 h at 37 °C in a 5% CO2 incubator. The quantification of viable cells was assessed by measuring the cleavage of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT; Sigma-Aldrich) as previously described.18 The formazan extraction was carried out with 10% (v/v) sodium dodecyl sulfate for 18 h (100 μL/well) at 24 °C. After 24 h, the microplate was read at 570 nm using a FilterMax F5Multi-Mode microplate reader. The selectivity index was determined considering the following equation: CC50 against macrophages/IC50 against amastigotes.
Cytokine ELISA
BMDMs isolated from C57BL/6 mice were plated at a concentration of 3.5 × 106 cells/well in quadruplicates in sterile 24-well tissue culture plates. Cells were treated with the isolated compounds 1−3. Supernatants were collected after 72 h of incubation at 37 °C and analyzed for the production of IL-6 and IL-10 by ELISA (Biolegend Inc.).
Quantification of Nitric Oxide
Nitric oxide content in the culture supernatants from macrophages cultured and treated for 72 h was analyzed by the Griess assay.41 Results obtained were extrapolated from a standard curve prepared with NaNO2 at different concentrations (0 to 400 μM).
Statistical Analysis
The results are represented as the mean and standard deviation of replicate samples from at least two independent assays. The IC50 values were calculated using sigmoidal dose−response curves using GraphPad Prism 5.0 software. The 95% confidence interval is included in parentheses with the analyses. The t test was used for significance testing (p < 0.05).
Supplementary Material
Acknowledgments
The authors thank São Paulo Research Foundation (FAPESP) [projects 2012/18756-1, 2013/50318-7, and 2014/19762-0], TACS’s scholarship 2013/07275-5, and Conselho Nacional de Desenvolvimento Cientifico e Tecnológico (CNPq) [project 470853/2012-3]. We also thank CAPES and UFABC for financial support. The authors are grateful for the CNPq Scientific Research Award given to A.G.T. and J.H.G.L., grant NIH RO1 AI29646, and grant W81XWH-14-2-0168 from the U.S. Army Medical Research Acquisition Activity.
Footnotes
Supporting Information
Spectroscopic data of metabolites 1−3 are available free of charge via the Internet at http://pubs.acs.org.
Notes
The authors declare no competing financial interest.
References
- 1.Den Boer M, Argaw D, Jannin J, Alvar J. Clin Microbiol Infect. 2011;17:1471–1477. doi: 10.1111/j.1469-0691.2011.03635.x. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Control of the Leishmaniases. WHO; Geneve: 2010. (WHO Technical Report Series). [PubMed] [Google Scholar]
- 3.Frézard F, Demicheli C, Ribeiro RR. Molecules. 2009;14:2317–2336. doi: 10.3390/molecules14072317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Espuelas S, Plano D, Nguewa P, Font M, Palop JA, Irache JM, Sanmartín C. Curr Med Chem. 2012;19:4259–4288. doi: 10.2174/092986712802884222. [DOI] [PubMed] [Google Scholar]
- 5.Sundar S, More DK, Singh MK, Singh VP, Sharma S, Makharia A, Kumar PC, Murray HW. Clin Infect Dis. 2000;31:1104–1107. doi: 10.1086/318121. [DOI] [PubMed] [Google Scholar]
- 6.Sundar S, Makharia A, More DK, Agrawal G, Voss A, Fischer C, Bachmann P, Murray HW. Clin Infect Dis. 2000;31:1110–1113. doi: 10.1086/318122. [DOI] [PubMed] [Google Scholar]
- 7.Rijal S, Ostyn B, Uranw S, Rai K, Bhattarai NR, Dorlo TP, Beijnen JH, Vanaerschot M, Decuypere S, Dhakal SS, Das ML, Karki P, Singh R, Boelaert M, Dujardin JC. Clin Infect Dis. 2013;56:1530–1538. doi: 10.1093/cid/cit102. [DOI] [PubMed] [Google Scholar]
- 8.Singh OP, Sundar S. Front Immunol. 2014;5:296. doi: 10.3389/fimmu.2014.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newman DJ, Cragg GM. J Nat Prod. 2012;75:311–335. doi: 10.1021/np200906s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Plant List. Lauraceae. http://www.theplantlist.org/1.1/browse/A/Lauraceae/ (accessed July 14, 2014)
- 11.Gottlieb OR. Phytochemistry. 1972;11:1537–1570. [Google Scholar]
- 12.Lordello ALL, Cavalheiro AJ, Yoshida M, Gottlieb OR. Rev Latinoam Quim. 2000;28:35–39. [Google Scholar]
- 13.Garcez FR, Garcez WS, Hamerski L, Miguita CH. Quim Nova. 2009;32:407–411. [Google Scholar]
- 14.Da Silva Filho AA, Costa ES, Cunha WR, Silva ML, Nanayakkara NP, Bastos JK. Phytother Res. 2008;22:1307–1310. doi: 10.1002/ptr.2486. [DOI] [PubMed] [Google Scholar]
- 15.Cabral MM, Barbosa-Filho JM, Maia GL, Chaves MC, Braga MV, De Souza W, Soares RO. Exp Parasitol. 2010;124:319–324. doi: 10.1016/j.exppara.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 16.Diaz AMP, Gottlieb HE, Gottlieb OR. Phytochemistry. 1980;19:681–682. [Google Scholar]
- 17.Reetz MT, Kühling KM, Hinrichs H, Deege A. Chirality. 2000;12:479–482. doi: 10.1002/(SICI)1520-636X(2000)12:5/6<479::AID-CHIR32>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 18.Tada H, Shiho O, Kuroshima K, Koyama M, Tsukamoto KJ. Immunol Methods. 1986;93:157–165. doi: 10.1016/0022-1759(86)90183-3. [DOI] [PubMed] [Google Scholar]
- 19.Lezama-Dávila CM, Isaac-Márquez AP, Kapadia G, Owens K, Oghumu S, Beverley S, Satoskar AR. Biol Pharm Bull. 2012;35:1761–1764. doi: 10.1248/bpb.b12-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sairafianpour M, Kayser O, Christensen J, Asfa M, Witt M, Staerk D, Jaroszewski JW. J Nat Prod. 2002;65:1754–1758. doi: 10.1021/np020244s. [DOI] [PubMed] [Google Scholar]
- 21.Bastos JK, Albuquerque S, Silva ML. Planta Med. 1999;65:541–544. doi: 10.1055/s-1999-14012. [DOI] [PubMed] [Google Scholar]
- 22.Taleb-Contini SH, Salvador MJ, Balanco JM, Albuquerque S, De Oliveira DC. Phytother Res. 2004;18:250–254. doi: 10.1002/ptr.1431. [DOI] [PubMed] [Google Scholar]
- 23.De Souza VA, Da Silva R, Pereira AC, Royo V, De A, Saraiva J, Montanheiro M, De Souza GH, Da Silva Filho AA, Grando MD, Donate PM, Bastos JK, Albuquerque S, E Silva ML. Bioorg Med Chem Lett. 2005;17(15):303–307. doi: 10.1016/j.bmcl.2004.10.079. [DOI] [PubMed] [Google Scholar]
- 24.Saraiva J, Vega C, Rolon M, Da Silva R, E Silva ML, Donate PM, Bastos JK, Gomez-Barrio A, Albuquerque S. Parasitol Res. 2007;100:791–795. doi: 10.1007/s00436-006-0327-4. [DOI] [PubMed] [Google Scholar]
- 25.Felippe LG, Baldoqui DC, Kato MJ, Bolzani VdS, Guimarães EF, Cicarelli RM, Furlan M. Phytochemistry. 2008;69:445–450. doi: 10.1016/j.phytochem.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 26.Da Silva Filho AA, Pires Bueno PC, Gregório LE, Andrade e Silva ML, Albuquerque S, Bastos JK. J Pharm Pharmacol. 2004;56:1195–1199. doi: 10.1211/0022357044067. [DOI] [PubMed] [Google Scholar]
- 27.Grecco SS, Felix MJP, Lago JHG, Pinto EG, Tempone AG, Romoff P, Ferreira MJP, Sartorelli P. Nat Prod Commun. 2014;9:171–173. [PubMed] [Google Scholar]
- 28.Dos Santos RA, Batista J, Jr, Rosa SI, Torquato HF, Bassi CL, Ribeiro TA, De Sousa PT, Jr, Bessera AM, Fontes CJ, Da Silva LE, Piuvezam MR. Parasitology. 2011;138:1224–1233. doi: 10.1017/S0031182011001168. [DOI] [PubMed] [Google Scholar]
- 29.Sharma M, Chauhan K, Shivahare R, Vishwakarma P, Suthar MK, Sharma A, Gupta S, Saxena JK, Lal J, Chandra P, Kumar B, Chauhan PM. J Med Chem. 2013;13(56):4374–4392. doi: 10.1021/jm400053v. [DOI] [PubMed] [Google Scholar]
- 30.Di Giorgio C, Lamidi M, Delmas F, Balansard G, Ollivier E. Planta Med. 2006;72:1396–1402. doi: 10.1055/s-2006-951726. [DOI] [PubMed] [Google Scholar]
- 31.Lee JY, Woo ER, Kang KW. J Ethnopharmacol. 2005;97:561–566. doi: 10.1016/j.jep.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 32.Hong SS, Oh JS. Arch Pharm Res. 2012;35:315–320. doi: 10.1007/s12272-012-0211-y. [DOI] [PubMed] [Google Scholar]
- 33.Mukbel RM, Patten C, Jr, Gibson K, Ghosh M, Petersen C, Jones DE. Am J Trop Med Hyg. 2007;76:669–675. [PubMed] [Google Scholar]
- 34.Costa DL, Rocha RL, Carvalho RM, Lima-Neto AS, Harhay MO, Costa CH, Barral-Neto M, Barral AP. Pathog Glob Health. 2013;107:78–87. doi: 10.1179/2047773213Y.0000000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murray HW. Infect Immun. 2008;76:4088–4091. doi: 10.1128/IAI.00490-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ansari NA, Saluja S, Salotra P. Clin Immunol. 2006;119:339–345. doi: 10.1016/j.clim.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 37.Verma S, Kumar R, Katara GK, Singh LC, Negi NS, Ramesh V, Salotra P. PLoS One. 2010;5:e10107. doi: 10.1371/journal.pone.0010107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lage RS, Oliveira GC, Busek SU, Guerra LL, Giunchetti RC, Corrêa-Oliveira R, Reis AB. Vet Immunol Immunopathol. 2007;115:135–145. doi: 10.1016/j.vetimm.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 39.Houghton P, Fang R, Techatanawat I, Steventon G, Hylands PJ, Lee CC. Methods. 2007;42:377–387. doi: 10.1016/j.ymeth.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 40.Ng LG, Hsu A, Mandell MA, Roediger B, Hoeller C, Mrass P, Iparraguirre A, Cavanagh LL, Triccas JA, Beverley SM, Scott P, Weninger W. PLoS Pathog. 2008;4:e1000222. doi: 10.1371/journal.ppat.1000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lezama-Dávila CM, Isaac-Márquez AP, Barbi J, Cummings HE, Lu B, Satoskar AR. Immunol Cell Biol. 2008;86:539–543. doi: 10.1038/icb.2008.39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


