Abstract
Objective:
To assess the use of epilepsy surgery in patients with medically intractable epilepsy in a publicly funded universal health care system.
Methods:
We performed a population-based retrospective cohort study using linked health care databases for Ontario, Canada, between 2001 and 2010. We identified all patients with medically intractable epilepsy, defined as those with seizures that did not respond to at least 2 adequate trials of seizure medications. We assessed the proportion of patients who had epilepsy surgery within the following 2 years. We further identified the characteristics associated with epilepsy surgery.
Results:
A total of 10,661 patients were identified with medically intractable epilepsy (mean age 47 years, 51% male); most (74%) did not have other comorbidities. Within 2 years of being defined as medically intractable, only 124 patients (1.2%) underwent epilepsy surgery. Death occurred in 12% of those with medically intractable epilepsy. Those who underwent the procedure were younger and had fewer comorbidities compared to those who did not.
Conclusion:
In our setting of publicly funded universal health care, more than 10% of patients died within 2 years of developing medically intractable epilepsy. Epilepsy surgery may be an effective treatment for some patients; however, fewer than 2% of patients who may have benefited from epilepsy surgery received it.
In Canada, 1 in every 200 people has epilepsy.1 Seizure drugs prevent ongoing seizures in most (70%) patients with epilepsy.2,3 Medically intractable epilepsy is a term coined by the International League Against Epilepsy (ILAE) to define a group of patients who do not respond to treatment with seizure drugs for a reasonable period of time.4 Epilepsy surgery should be considered in such patients.5
Since the 1950s, epilepsy surgery has been the treatment of choice for patients not responding to treatment with seizure drugs. In 2001, a team of Canadians performed the first randomized controlled trial of surgery for temporal lobe epilepsy, the most common type of medically intractable epilepsy. In this trial, the benefit of epilepsy surgery was found to be significantly better than the continuation of seizure drugs, not only with regards to seizure control, but also in terms of quality of life.6 A subsequent trial in the United States confirmed these findings,7 prompting the American Academy of Neurology to publish a practice parameter recommending epilepsy surgery in patients with focal epilepsy who do not respond to seizure drugs.8
In spite of the increasing evidence and introduction of a new practice parameter, candidate patients continue to wait years to see a specialist and particularly to be assessed in an epilepsy surgery program.5 Even with the publication of a Canadian tool to determine the appropriateness for a referral to an epilepsy surgery program,9 there is uncertainty as to whether referral patterns have changed. Furthermore, the ILAE through a special task force found that epilepsy surgery is underutilized in North America, despite the existence of many comprehensive epilepsy surgery programs in Canada and the United States.10
To better understand the current practices in Canada, we assessed the rate of epilepsy surgery in patients with medically intractable epilepsy using large population-based databases in Ontario. To further determine possible inequalities in access, we additionally identified patient predictors associated with no surgery.
METHODS
Study design.
Ontario is the most populous province in Canada, with approximately 13 million residents (2012 population estimate: 13,505,900). All residents have universal access to hospital care and physician services, while eligible residents (including those aged 65 years or older, on social assistance, receiving home care, in long-term care, or eligible for the special drugs program11) have additional universal prescription drug coverage of more than 3,800 medications when purchasing within the province.12 These health care encounters are recorded in population-based, linkable databases that are held at the Institute for Clinical and Evaluative Sciences (ICES). We conducted a retrospective, population-based cohort study of patients with medically intractable epilepsy from January 1, 2001, to December 31, 2010, using these linked health care databases in Ontario, Canada.
Standard protocol approvals, registrations, and patient consents.
The reporting of this study followed guidelines for observational studies.13 The study was approved by the Sunnybrook Health Science Centre Research Ethics Board in Toronto, Ontario, Canada.
Data sources.
We identified our cohort of patients, their characteristics, and outcomes using 6 data sources: the Ontario Health Insurance Plan (OHIP), which includes information for inpatient and outpatient fee-for-service physician claims; the Registered Persons Database (RPDB), which contains vital statistics on all permanent residents of Ontario; the National Ambulatory Care Reporting System (NARCS) and the Canadian Institute for Health Information Discharge Abstract Database (CIHI-DAD), which provide diagnostic and procedural information on all hospitalizations and emergency room visits using the ICD-9 (prior to April 2002) and ICD-10 (after April 2002) coding systems; and the Ontario Drug Benefits (ODB) database, which provides information on prescription drug use for eligible patients of all ages. This latter data source contains highly accurate records, including the name of the drug, daily doses, and dates of all outpatient prescriptions dispensed to eligible patients. These databases have been used extensively to research health outcomes and health services.14–20 These databases were held securely in a linked, de-identified form at ICES and analyzed at the ICES Western site.
We used a combination of CIHI-DAD, NACRS, and ODB to identify patients who met the definition of medically intractable epilepsy and CIHI-DAD, OHIP, NACRS, and RPDB to define patient characteristics and baseline comorbidities and report patient outcomes. To define baseline comorbidities, we reviewed all health care records (inpatient and outpatient) in the 5 years prior to the diagnosis of medically intractable epilepsy. In some cases the look-back period included a time frame prior to the transition from ICD-9 to ICD-10 coding (prior to April 1, 2002). Therefore, whenever possible we used database codes that had been validated with chart review or established coding algorithms included in previous administrative database studies.
Identification of patients with medically intractable epilepsy.
Identification of patients with medically intractable epilepsy is detailed in figure e-1 on the Neurology® Web site at Neurology.org. The ILAE defines medically intractable epilepsy as a continuation of seizures despite the use of 2 adequate trials of seizure drugs. In this study, we accrued patients 18 years of age and older meeting the definition of medically intractable epilepsy over a 10-year period as follows. We first identified all patients with a documented seizure episode between January 1, 2001, and December 31, 2010. Seizures were identified through emergency room and hospitalization records using validated ICD-9 and ICD-10 codes.21,22 We then excluded records with invalid or inaccurate information and all patients younger than 18 years at the time of the seizure. We further excluded patients with a diagnosis of a brain tumor in the previous 5 years as occasionally patients with brain tumors undergo surgery because of focal neurologic deficits, the tumor's nature (e.g., malignancy), and not because their seizures are refractory to medical treatment. We also excluded patients who had a previous epilepsy surgery dating back to the earliest available health care records in Ontario (July 1, 1991). This was done to eliminate potential preclusion of surgery as subsequent treatment. Since the definition of medically intractable epilepsy requires the knowledge of prior seizure drug use, we further restricted this group to patients who were eligible for prescription drug coverage in the previous 2 years by ensuring that patients had filled at least one prescription with the ODB in each of the 2 years prior to the index seizure. Finally, we excluded patients who did not fill at least 2 different seizure drugs, each with a cumulative day supply of at least 6 months in the 2 years prior to the index seizure (as these patients did not meet the definition of medically intractable epilepsy). The final study cohort was established by restricting to the first seizure episode per patient; this date served as the index date and the start time for follow-up. Patients who turned 18 during the study period were eligible for entry in the study as long as they had a seizure event after age 18 years.
Outcomes.
Our primary outcome included the assessment for epilepsy surgery, or procedure for epilepsy surgery in the 2 years following the index date, identified using billing codes. In addition to the epilepsy surgery procedure, we also considered the placement of intracranial electrodes as this indicated that the patient was assessed for epilepsy surgery, but did not receive it because he or she was not a candidate for the procedure. Secondary outcomes investigated during the same 2-year follow-up window were any neurologic consults by a neurologist, subsequent emergency visits for seizures, and all-cause mortality.
Statistical analysis.
Using t tests for continuous variables and χ2 tests for categorical variables, we compared baseline characteristics of the patients with medically intractable epilepsy who later underwent epilepsy surgery to baseline characteristics of those who did not have surgery. We used multivariable log-binomial regression to present relative risk estimates of possible predictors for epilepsy surgery. Predictors included the patient characteristics of age; sex; location of residence (urban or rural); the Ontario marginalization index,23 based on Canadian census dissemination areas (49,153 in total) for residential instability, deprivation, dependency, and ethnic concentration23; and the Charlson Comorbidity Index, a measure of comorbidity.24 To compare the mortality rate between medically intractable patients and the general population, we matched each patient to four community controls on age, sex, location (rural/urban), and neighborhood income quintile. We presented survival differences using Kaplan-Meier estimates and used conditional logistic regression to estimate the odds ratio. All analyses were conducted using 2-sided tests with p value cutoffs of 0.05. Analyses were conducted using SAS statistical software version 9.3 (Cary, NC, USA).
RESULTS
Patient characteristics.
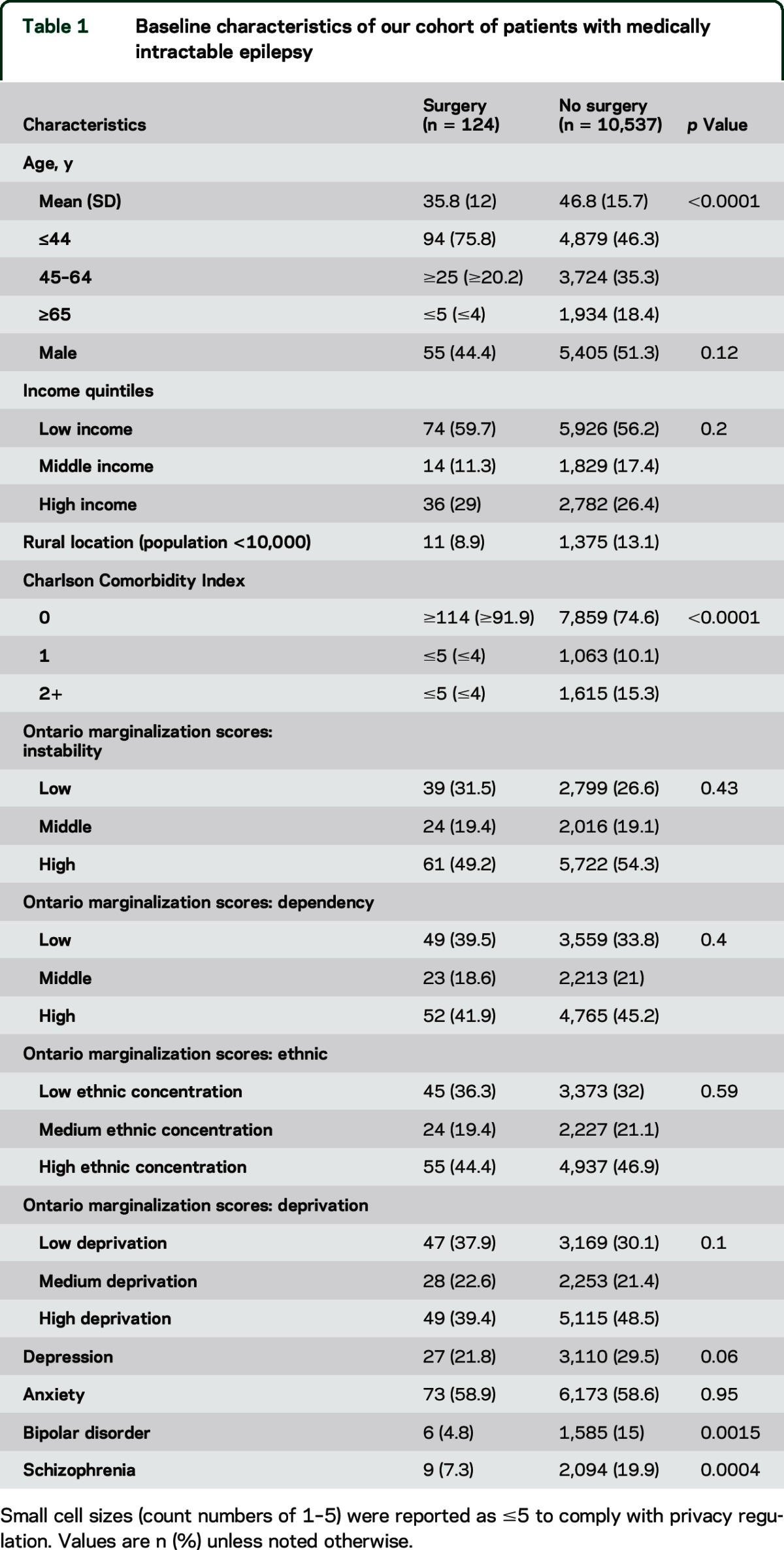
A total of 10,661 medically intractable epilepsy patients were identified between 2001 and 2010 (table 1). The mean age was 47 years and 51% were male. Most patients lived in urban regions (86.9%) and had few additional medical comorbidities.24 Of note, 29.5% of patients had a history of depression, while 58.6% had a documented diagnosis of anxiety, 15% bipolar disorder, and 19.9% schizophrenia.
Table 1.
Baseline characteristics of our cohort of patients with medically intractable epilepsy
Primary results.
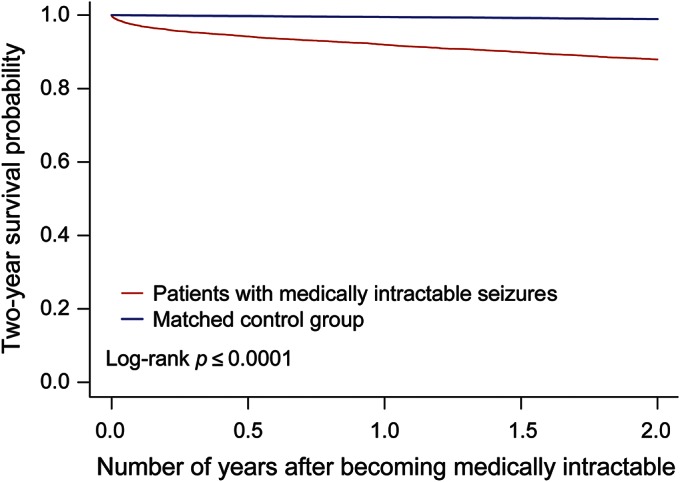
A total of 234 out of 10,661 (2.2%) patients with medically intractable epilepsy underwent prolonged video-EEG, and 124 (1.2%) underwent epilepsy surgery or were assessed with intracranial electrodes within 2 years of their index date (table 2). During the same follow-up period, 4,404 (41.3%) patients had at least one emergency room visit for a seizure, and 6,314 (59.2%) were seen by a neurologist. Death occurred in 1,280 (12%) patients. When compared to community controls matched on a 1:4 ratio, we found the proportion of deaths among those with medically intractable epilepsy to be substantially higher (12% vs 1.1%; odds ratio 14.6; 95% confidence interval [CI] 12.9–16.4) than controls (figure 1).
Table 2.
Patients with medically intractable epilepsy in Ontario from 2001 to 2010 who underwent epilepsy surgery, visited an emergency department for seizures, died, or visited a neurologist within 2 years of their index date
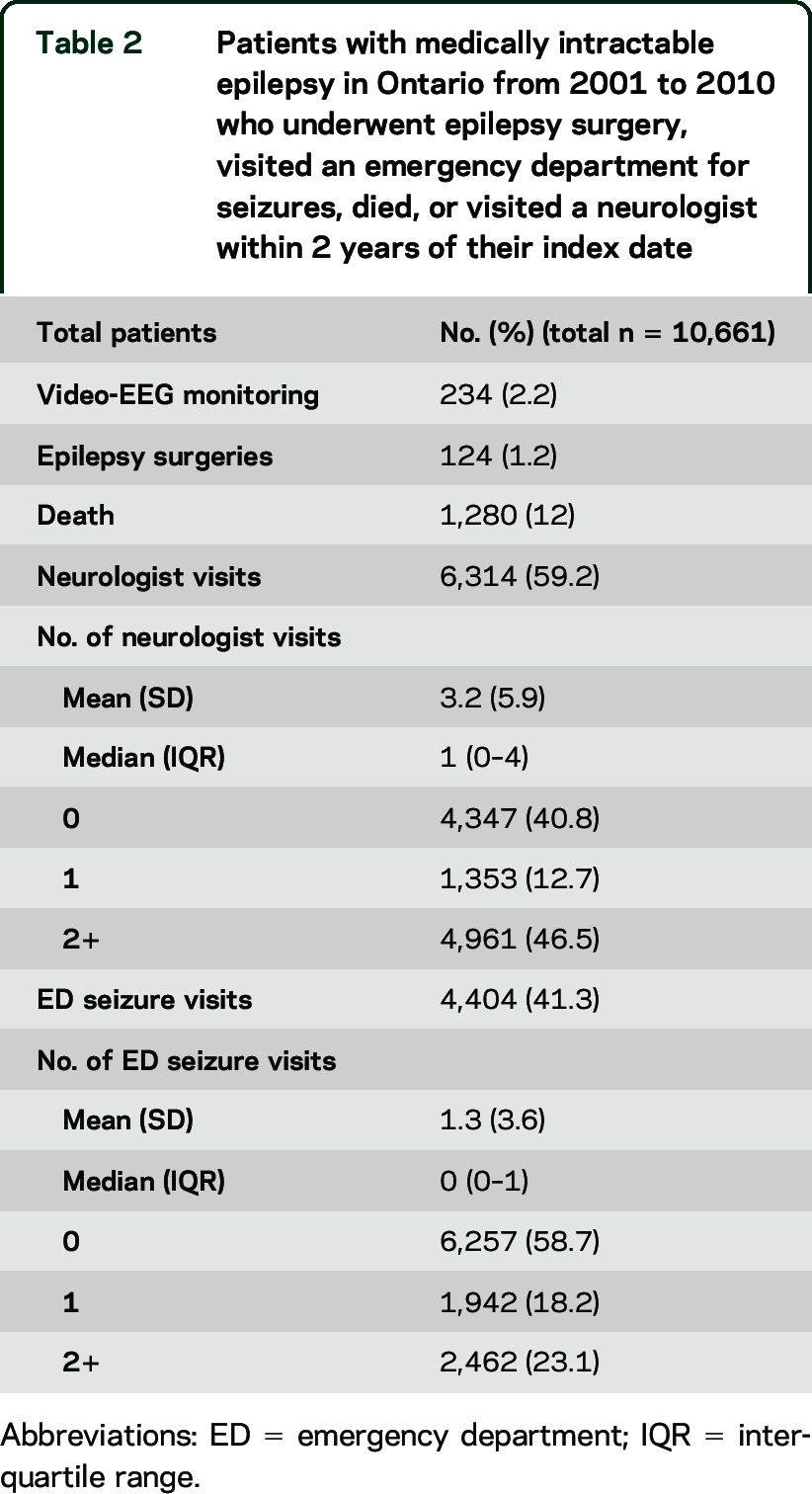
Figure 1. Two-year survival probability of patients with medically intractable seizures vs matched control group.
Predictors of epilepsy surgery.
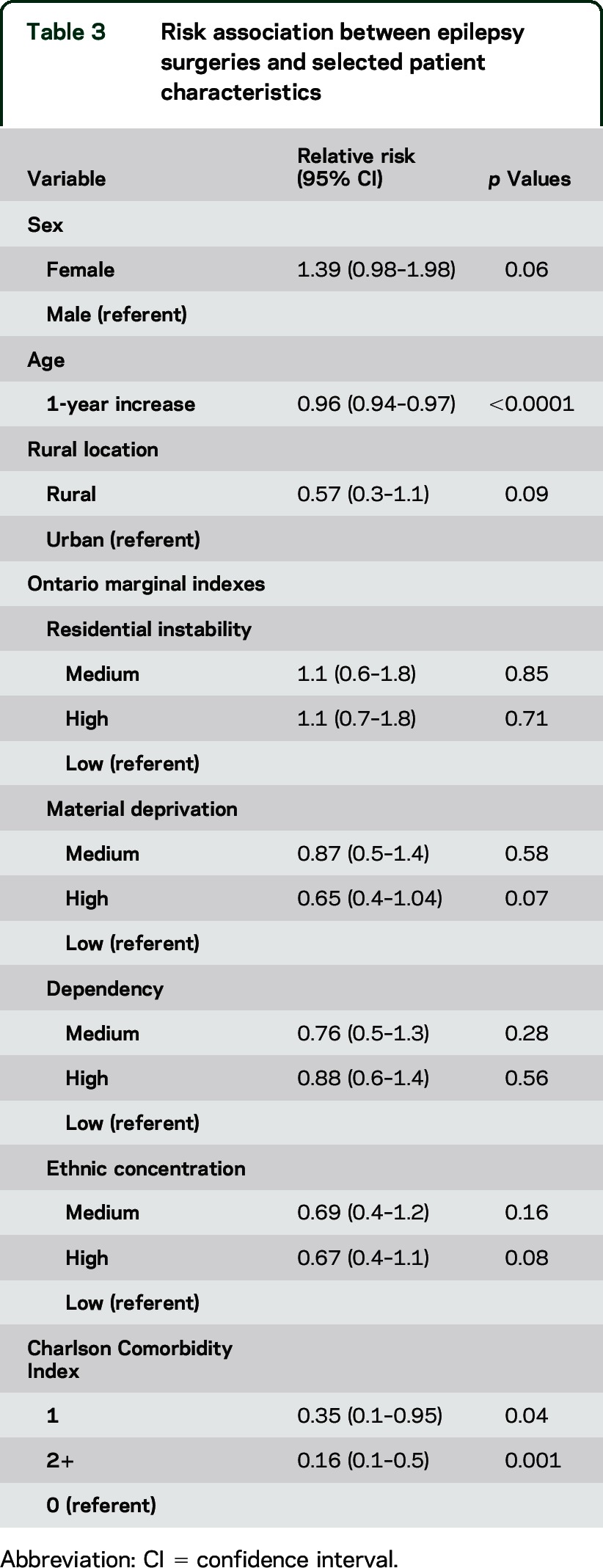
Patients who underwent epilepsy surgery were younger than those who did not (mean age 35.8 vs 46.8 years, p < 0.0001). No significant differences were observed in sex, income level, location or residence, or marginalization scores (table 1). When combined in a multivariable model, older age (relative risk [RR] 0.96, 95% CI 0.94–0.97) and high comorbidity index (RR 0.16, 95% CI 0.05–0.51) were associated with lower risk of undergoing surgery (table 3).
Table 3.
Risk association between epilepsy surgeries and selected patient characteristics
DISCUSSION
In this study, we identified that a small percentage of patients with medically intractable epilepsy received epilepsy surgery treatment. Even though consideration for epilepsy surgery is the recommended standard of care for patients with medically intractable epilepsy, that treatment is not being adequately utilized.
These findings are intriguing given the strong evidence in the literature favoring this treatment.6,8 A possible explanation includes lack of awareness among general practitioners or neurologists, which has not been explored. Most likely there is a combination of lack of knowledge, misconceptions about the risks vs benefits of the procedure, as well as lack of education in medical schools and residency programs. Furthermore, patients and families may also lack awareness of the effectiveness and low risk of morbidity of epilepsy surgery. Another explanation may relate to the small number of epilepsy programs with the capability to perform a comprehensive investigation in order to determine if the patient is a surgical candidate and subsequently perform the surgical procedure. In Ontario, by the time this study was finished, there were only 2 programs with infrastructure and personnel to perform epilepsy surgery in adults and 2 in children, with a total 18 beds with video-EEG capability. They are located in the cities of London and Toronto, in the southwestern portion of the province. Other major cities in the province like Ottawa do not have video-EEG monitoring beds or epilepsy surgery programs. However, isolated reports, letters, and commentaries in medical journals indicate that lack of infrastructure does not appear to be the cause for the low number of epilepsy surgeries.5,25
In the United States, trends of epilepsy surgery have also been published and the situation is similar.26 We thought the situation might be different in a society with a universal health system like Ontario, but our findings do not support that.
The main limitations of the study reside in its retrospective nature as well as the limited access we had to identify all patients with medically intractable epilepsy in Ontario. Information obtained from the drug dispensing database only represented a portion of the overall Ontario population. The ODB provides government-sponsored drug coverage to all patients older than 65 years, as well as those under 65 years who have high drug costs relative to their income, or receive social assistance due to unemployment or a medical disability. Even though not all patients with epilepsy receive ODB coverage we suspect that a large proportion do. This is likely because epilepsy affects individuals' performance at work; additionally, ongoing seizures would render them ineligible to drive or perform risky jobs. While developing our cohort, we identified that 55% adult seizure patients were not covered under ODB; however, not all these patients would have met the clinical definition of epilepsy or required seizure medications. This is thus an overestimate of the proportion of medically intractable epilepsy patients who were not captured in this study.
The use of administrative databases in research allows the inclusion of population-based samples, increasing statistical power as well as maximizing generalizability of findings. It also allows the recording of health services use in a contemporary manner, avoiding the problems associated with imperfect recall, nonresponse, or reporting bias. These represent the major strengths of their use; however, limitations related to their use are important to note. These databases rely on coding to identify diagnoses and procedures; coding is often completed by trained coders based on information entered on the patient’s chart. Diagnostic coding is thus often underrepresented as apparent diagnoses may not be noted by clinicians on patient charts. This may impact the magnitude of reported comorbidities. Furthermore, since these databases were created for administrative and financial purposes, they may lack details on important clinical factors such as height, weight, blood pressure readings, and smoking status.27,28
The time window of this study included the transition from ICD-9 to ICD-10 in Canada. Validation studies for both ICD-9 and ICD-10 versions of seizure codes report similar operating characteristics.22 Furthermore, we observed that the annual number of patients with medically intractable epilepsy was consistent throughout the study period, suggesting no obvious difference in seizure case definitions due to the changes in coding practices.
We found that only 2.2% of those with medically intractable epilepsy underwent prolonged video-EEG, and half of them underwent epilepsy surgery. Unfortunately, we could not determine why some of those who did have a presurgical evaluation with video-EEG did not have surgery. Reasons could have been multifocal or generalized epilepsy, nonepileptic events, or patient's own preference.
Another issue is the fact that we did not include patients who had any type of neurostimulator implanted for the management of epilepsy, particularly the vagus nerve stimulator (VNS). A review of the physicians’ billing database revealed that only 14 patients received a peripheral nerve stimulation device (which is how VNS is coded in OHIP). That may have included other types of stimulators not used for epilepsy (like a spinal cord stimulator for pain management). Furthermore, the provincial budget for neurostimulators for epilepsy was almost nonexistent before 2011, and thalamic or hippocampal stimulators were approved for clinical use only after 2011.
Another interesting observation of the study is the high percentage of patients going to the emergency room because of seizures within the first 2 years after they were identified as medically intractable. This group of patients produces a high cost to the health system.29 Furthermore, there is a high percentage of death among middle-aged patients with medically intractable epilepsy; in this study, we could not reliably determine the cause of death. But the proportion of deaths among those with medically intractable epilepsy was substantially higher than in matched controls from the community.
Medically intractable epilepsy is a condition that impairs patient health and quality of life. Most patients with epilepsy are young, and cannot join the workforce because of frequent seizures. Furthermore, medically intractable epilepsy is associated with increased mortality and high societal costs. Epilepsy surgery may be an effective treatment for some patients, but is currently underutilized even in a health system with universal access.
Supplementary Material
ACKNOWLEDGMENT
Parts of this material are based on data and information compiled and provided by the Canadian Institutes for Health Information (CIHI). The analyses, conclusions, opinions, and statements expressed herein are those of the authors, and not necessarily those of CIHI.
GLOSSARY
- CI
confidence interval
- CIHI-DAD
Canadian Institute for Health Information Discharge Abstract Database
- ICD
International Classification of Diseases
- ICES
Institute for Clinical and Evaluative Sciences
- ILAE
International League Against Epilepsy
- NARCS
National Ambulatory Care Reporting System
- ODB
Ontario Drug Benefits
- OHIP
Ontario Health Insurance Plan
- RPDB
Registered Persons Database
- RR
relative risk
- VNS
vagus nerve stimulator
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Jorge G. Burneo: design and conceptualization of the study, interpretation of data, drafting and revising the manuscript for intellectual content. Salimah Z. Shariff: analysis and interpretation of data, revising the manuscript for intellectual content. Kuan Liu: analysis and interpretation of data, revising the manuscript for intellectual content. Sean Leonard: revision of the manuscript for intellectual content. Gustavo Saposnik: revision of the manuscript for intellectual content. Amit X. Garg: interpretation of data, revision of the manuscript for intellectual content.
STUDY FUNDING
This study was supported by the Institute for Clinical Evaluative Sciences (ICES) Western site. ICES is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). Core funding for ICES Western is provided by the Academic Medical Organization of Southwestern Ontario (AMOSO), the Schulich School of Medicine and Dentistry (SSMD), Western University, and the Lawson Health Research Institute (LHRI). The opinions, results, and conclusions are those of the authors and are independent from the funding sources. No endorsement by ICES, AMOSO, SSMD, LHRI, or the MOHLTC is intended or should be inferred.
DISCLOSURE
J. Burneo has received funding for research from UCB Canada and The Ontario Brain Institute; has served on the advisory boards of Sunovion and UCB Canada; and has been part of the Speaker's Bureau for UCB Canada and Eisai. Dr. Burneo is an ICES Scholar and is on the editorial boards of The Canadian Journal of Neurological Sciences, Epilepsy & Behavior, Clinical Neurology and Neurosurgery, Revista de Neuropsiquiatria, and Frontiers in Epilepsy. S. Shariff, K. Liu, and S. Leonard report no disclosures relevant to the manuscript. G. Saposnik is supported by the Heart & Stroke Foundation of Canada, Distinguished Clinician Scientist Award, following an open peer-reviewed competition. A. Garg reports no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Tellez-Zenteno JF, Pondal-Sordo M, Matijevic S, Wiebe S. National and regional prevalence of self-reported epilepsy in Canada. Epilepsia 2004;45:1623–1629. [DOI] [PubMed] [Google Scholar]
- 2.Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med 2000;342:314–319. [DOI] [PubMed] [Google Scholar]
- 3.Brodie MJ, Barry SJ, Bamagous GA, Norrie JD, Kwan P. Patterns of treatment response in newly diagnosed epilepsy. Neurology 2012;78:1548–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwan P, Arzimanoglou A, Berg AT, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010;51:1069–1077. [DOI] [PubMed] [Google Scholar]
- 5.Burneo JG, McLachlan RS. When should surgery be considered for the treatment of epilepsy? CMAJ 2005;172:1175–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiebe S, Blume WT, Girvin JP, Eliasziw M; Effectiveness, Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 2001;345:311–318. [DOI] [PubMed] [Google Scholar]
- 7.Engel J, Jr, McDermott MP, Wiebe S, et al. Early surgical therapy for drug-resistant temporal lobe epilepsy: a randomized trial. JAMA 2012;307:922–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engel J, Jr, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy: report of the Quality Standards Subcommittee of the American Academy of Neurology, in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology 2003;60:538–547. [DOI] [PubMed] [Google Scholar]
- 9.Jette N, Quan H, Tellez-Zenteno JF, et al. Development of an online tool to determine appropriateness for an epilepsy surgery evaluation. Neurology 2012;79:1084–1093. [DOI] [PubMed] [Google Scholar]
- 10.Burneo JG, Jette N, Theodore W, et al. Disparities in epilepsy: report of a systematic review by the North American Commission of the International League against Epilepsy. Epilepsia 2009;50:2285–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levy AR, O'Brien BJ, Sellors C, Grootendorst P, Willison D. Coding accuracy of administrative drug claims in the Ontario Drug Benefit database. Can J Clin Pharmacol 2003;10:67–71. [PubMed] [Google Scholar]
- 12.The Ontario Drug Benefit Program. Available at: http://www.health.gov.on.ca/en/public/programs/drugs/programs/odb/odb.aspx. Accessed January 26, 2015.
- 13.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology 2007;18:800–804. [DOI] [PubMed] [Google Scholar]
- 14.Austin PC, Mamdani MM, Tu K, Jaakkimainen L. Prescriptions for estrogen replacement therapy in Ontario before and after publication of the Women's Health Initiative Study. JAMA 2003;289:3241–3242. [DOI] [PubMed] [Google Scholar]
- 15.Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med 1999;341:1359–1367. [DOI] [PubMed] [Google Scholar]
- 16.Mamdani M, Juurlink DN, Lee DS, et al. Cyclo-oxygenase-2 inhibitors versus non-selective non-steroidal anti-inflammatory drugs and congestive heart failure outcomes in elderly patients: a population-based cohort study. Lancet 2004;363:1751–1756. [DOI] [PubMed] [Google Scholar]
- 17.Juurlink DN, Mamdani MM, Lee DS, et al. Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N Engl J Med 2004;351:543–551. [DOI] [PubMed] [Google Scholar]
- 18.Gandhi S, Fleet JL, Bailey DG, et al. Calcium-channel blocker-clarithromycin drug interactions and acute kidney injury. JAMA 2013;310:2544–2553. [DOI] [PubMed] [Google Scholar]
- 19.Hwang YJ, Dixon SN, Reiss JP, et al. Atypical antipsychotic drugs and the risk for acute kidney injury and other adverse outcomes in older adults: a population-based cohort study. Ann Internal Med 2014;161:242–248. [DOI] [PubMed] [Google Scholar]
- 20.Garg AX, Nevis IF, McArthur E, et al. Gestational hypertension and preeclampsia in living kidney donors. N Engl J Med 2015;372:124–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jette N, Reid AY, Quan H, Hill MD, Wiebe S. How accurate is ICD coding for epilepsy? Epilepsia 2010;51:62–69. [DOI] [PubMed] [Google Scholar]
- 22.Reid AY, St Germaine-Smith C, Liu M, et al. Development and validation of a case definition for epilepsy for use with administrative health data. Epilepsy Res 2012;102:173–179. [DOI] [PubMed] [Google Scholar]
- 23.The Ontario Marginalization Index. Toronto: Center for Research on Inner City Health; 2012. Available at: http://crunch.mcmaster.ca/documents/ON-Marg_user_guide_1.0_FINAL_MAY2012.pdf. Accessed January 26, 2015. [Google Scholar]
- 24.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 25.Ibrahim GM, Rutka JT, Snead OC., III Epilepsy surgery in childhood: no longer the treatment of last resort. CMAJ 2014;186:973–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Englot DJ, Ouyang D, Garcia PA, Barbaro NM, Chang EF. Epilepsy surgery trends in the United States, 1990-2008. Neurology 2012;78:1200–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grimes DA. Epidemiologic research using administrative databases: garbage in, garbage out. Obstet Gynecol 2010;116:1018–1019. [DOI] [PubMed] [Google Scholar]
- 28.Suissa S, Garbe E. Primer: administrative health databases in observational studies of drug effects: advantages and disadvantages. Nat Clin Pract Rheumatol 2007;3:725–732. [DOI] [PubMed] [Google Scholar]
- 29.Wiebe S, Bellhouse DR, Fallahay C, Eliasziw M. Burden of epilepsy: the Ontario Health Survey. Can J Neurol Sci 1999;26:263–270. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


