Abstract
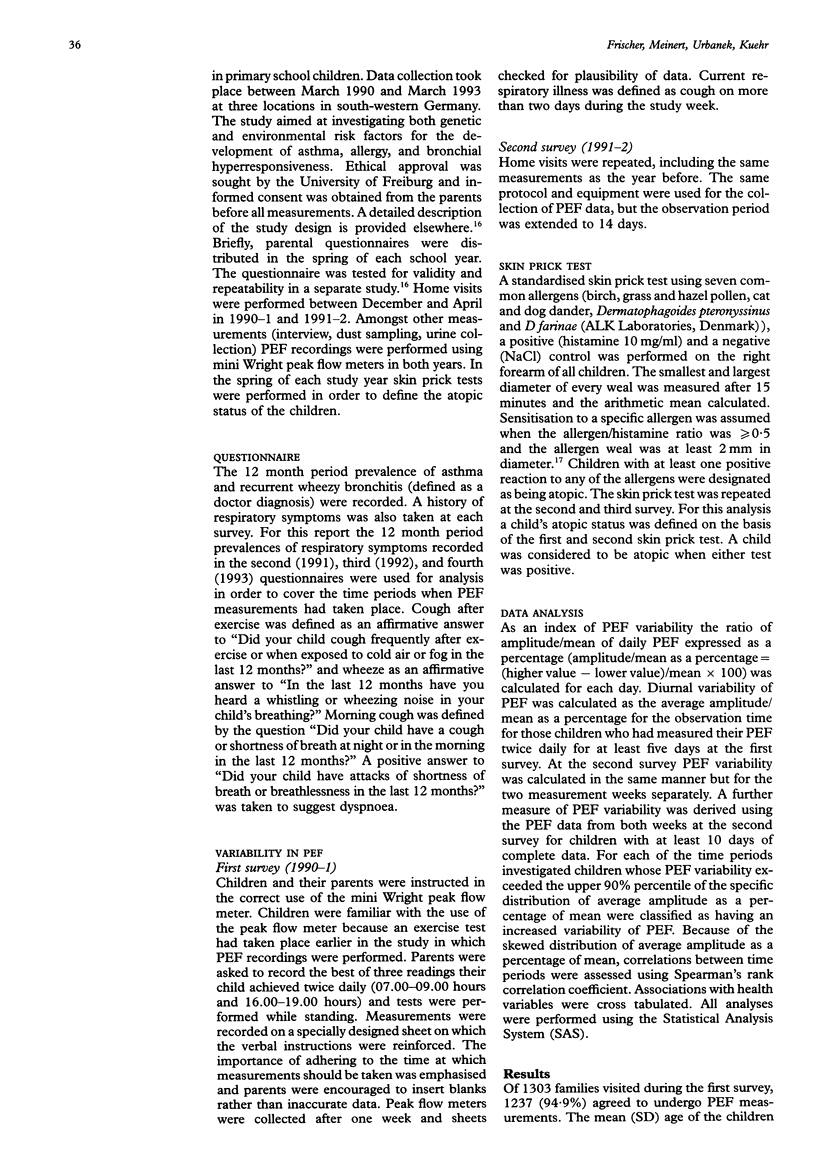
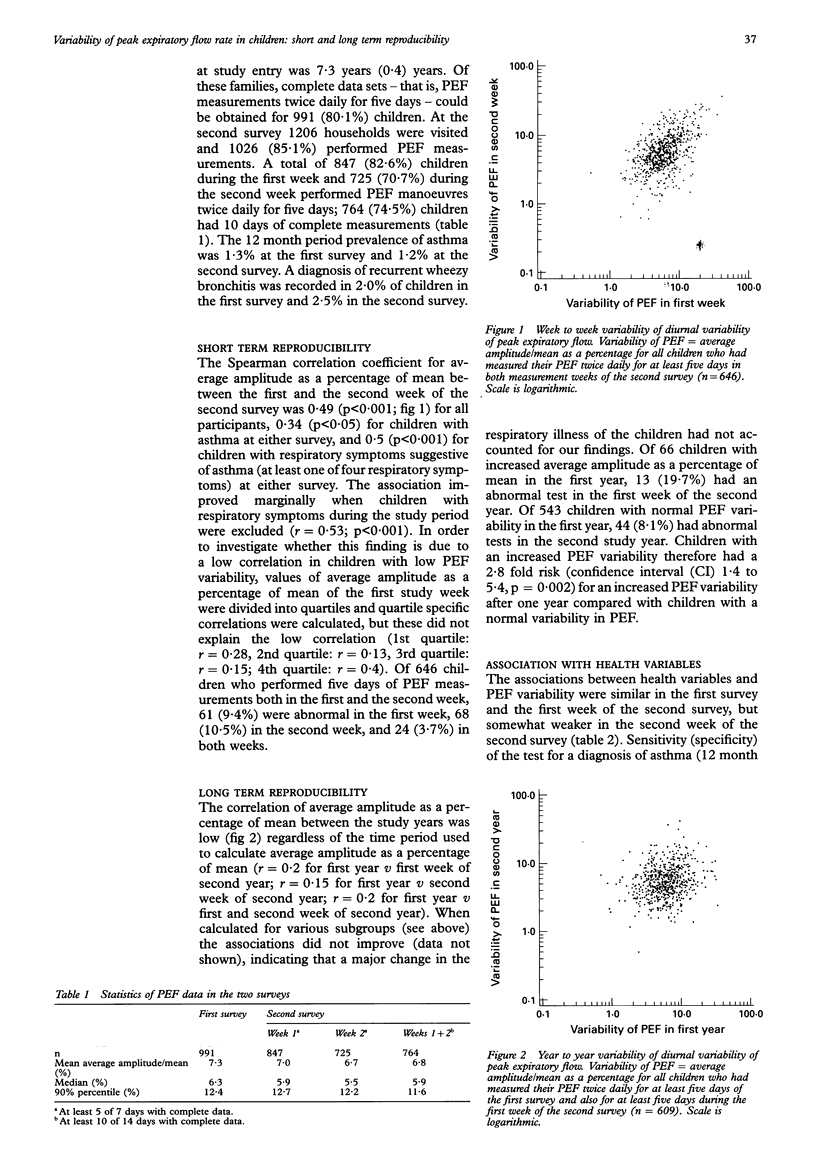
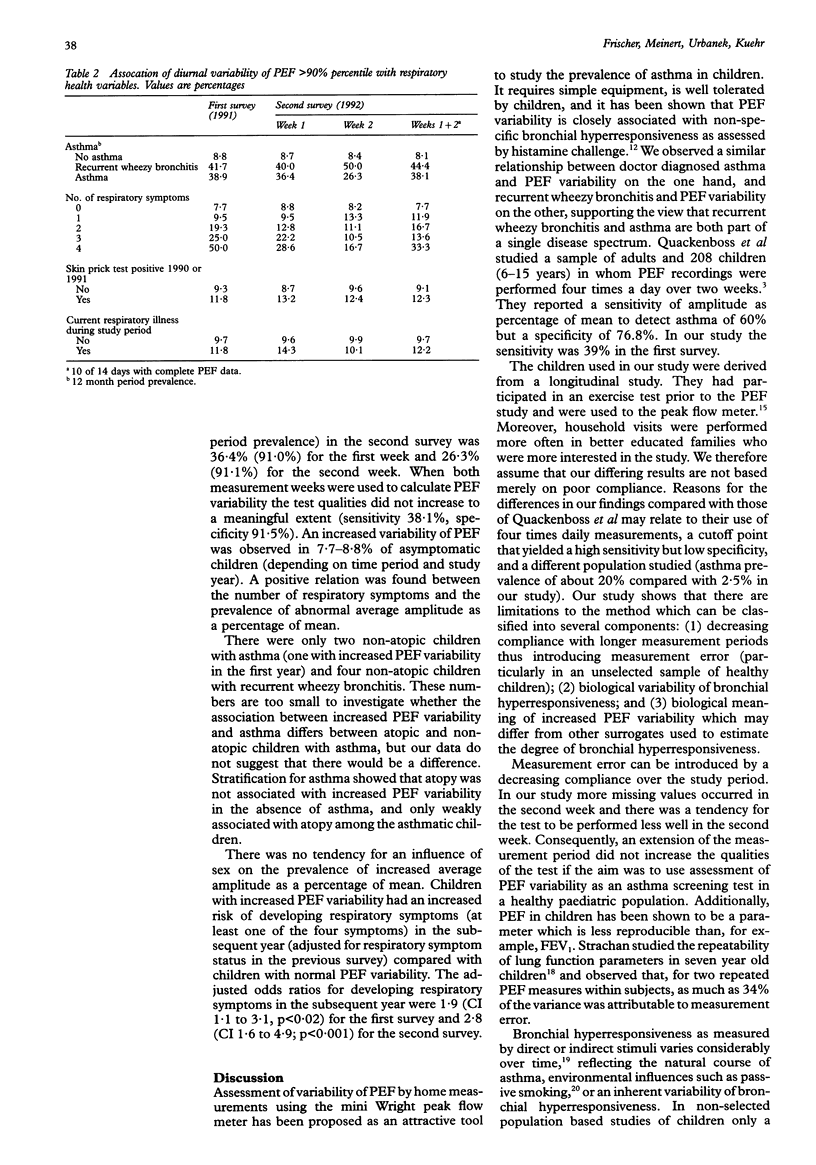
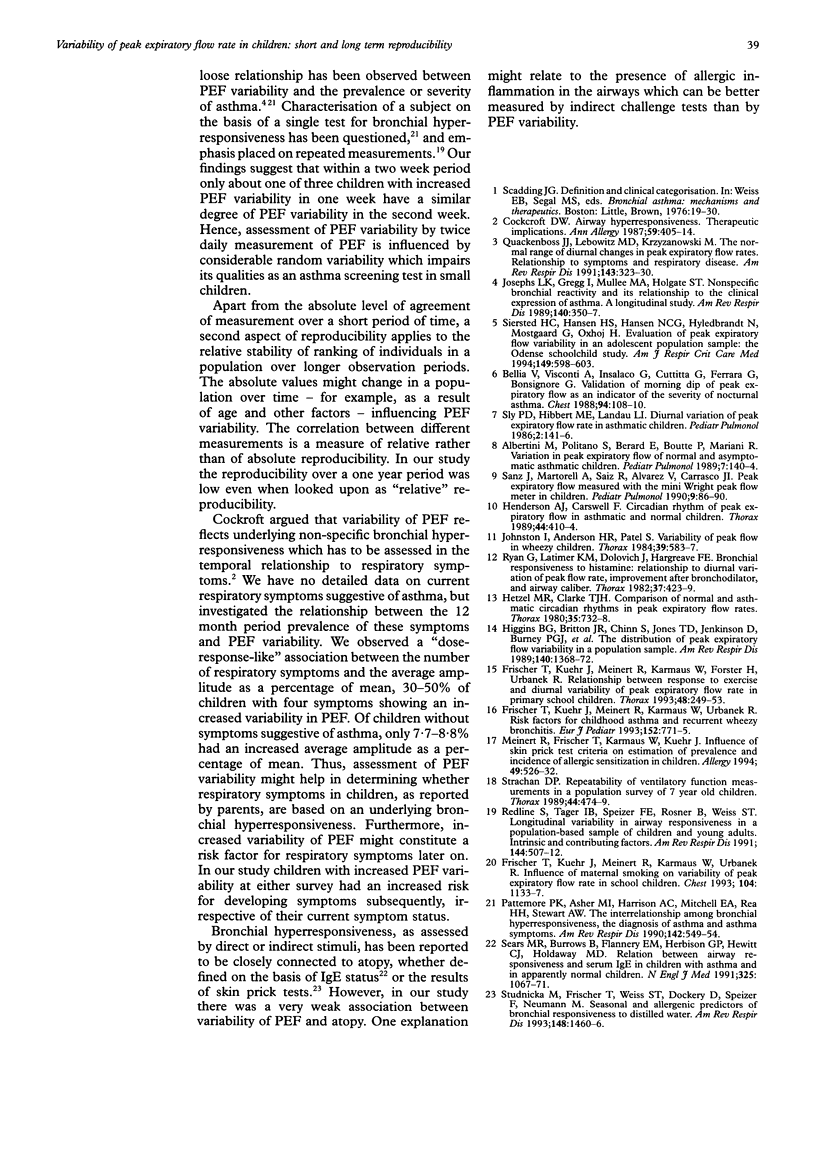
BACKGROUND--Variability of peak expiratory flow (PEF) has been proposed as a surrogate for bronchial hyperresponsiveness. The normal range of variability of PEF for children has been reported and the test has been used to screen for asthma in population based studies. However, there is little information on the reproducibility of the method in epidemiological settings. METHODS--In a cohort study of primary school children the variability in PEF was recorded in two consecutive years for one week (first survey) and two weeks (second survey) using mini Wright peak flow meters. PEF was recorded twice daily (morning and evening) and average amplitude as a percentage of mean was calculated as a standard measure of PEF variability for each single week of PEF measurement. Children with PEF variability exceeding the 90% percentile of the distribution for the specific time period were regarded as having increased variability of PEF. RESULTS--Of 66 children with increased PEF variability in the first year, 13 (19.7%) had an abnormal test in the first week of the second year. Of 543 children with normal PEF variability in the first year, 44 (8.1%) had an abnormal test in the second study year (odds ratio 2.8, confidence interval (CI) 1.4 to 5.4). Of 646 children in the second survey 61 (9.4%) were abnormal during the first week and 68 (10.5%) had an increased PEF variability during the second week, but only 24 (3.7%) children had an increased PEF variability in both weeks. The sensitivity (specificity) for doctor-diagnosed asthma (12 month period prevalence) was 36.4% (91.0%) in the first week of the second survey. When measurements of both weeks of the second survey were used to calculate PEF variability there was little improvement in the sensitivity (38.1%) and specificity (91.5%), mainly because of decreased compliance in the second measurement week. CONCLUSIONS--In young children assessment of PEF variability in order to screen for asthma is of limited value because of the low reproducibility of the method.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Albertini M., Politano S., Berard E., Boutte P., Mariani R. Variation in peak expiratory flow of normal and asymptomatic asthmatic children. Pediatr Pulmonol. 1989;7(3):140–144. doi: 10.1002/ppul.1950070305. [DOI] [PubMed] [Google Scholar]
- Bellia V., Visconti A., Insalaco G., Cuttitta G., Ferrara G., Bonsignore G. Validation of morning dip of peak expiratory flow as an indicator of the severity of nocturnal asthma. Chest. 1988 Jul;94(1):108–110. doi: 10.1378/chest.94.1.108. [DOI] [PubMed] [Google Scholar]
- Cockcroft D. W. Airway hyperresponsiveness: therapeutic implications. Ann Allergy. 1987 Dec;59(6):405–414. [PubMed] [Google Scholar]
- Frischer T., Kuehr J., Meinert R., Karmaus W., Urbanek R. Risk factors for childhood asthma and recurrent wheezy bronchitis. Eur J Pediatr. 1993 Sep;152(9):771–775. doi: 10.1007/BF01954000. [DOI] [PubMed] [Google Scholar]
- Frischer T., Kühr J., Meinert R., Karmaus W., Forster J., Urbanek R. Relation between response to exercise and diurnal variability of peak expiratory flow in primary school children. Thorax. 1993 Mar;48(3):249–253. doi: 10.1136/thx.48.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frischer T., Kühr J., Meinert R., Karmaus W., Urbanek R. Influence of maternal smoking on variability of peak expiratory flow rate in school children. Chest. 1993 Oct;104(4):1133–1137. doi: 10.1378/chest.104.4.1133. [DOI] [PubMed] [Google Scholar]
- Henderson A. J., Carswell F. Circadian rhythm of peak expiratory flow in asthmatic and normal children. Thorax. 1989 May;44(5):410–414. doi: 10.1136/thx.44.5.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetzel M. R., Clark T. J. Comparison of normal and asthmatic circadian rhythms in peak expiratory flow rate. Thorax. 1980 Oct;35(10):732–738. doi: 10.1136/thx.35.10.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins B. G., Britton J. R., Chinn S., Jones T. D., Jenkinson D., Burney P. G., Tattersfield A. E. The distribution of peak expiratory flow variability in a population sample. Am Rev Respir Dis. 1989 Nov;140(5):1368–1372. doi: 10.1164/ajrccm/140.5.1368. [DOI] [PubMed] [Google Scholar]
- Johnston I., Anderson H. R., Patel S. Variability of peak flow in wheezy children. Thorax. 1984 Aug;39(8):583–587. doi: 10.1136/thx.39.8.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josephs L. K., Gregg I., Mullee M. A., Holgate S. T. Nonspecific bronchial reactivity and its relationship to the clinical expression of asthma. A longitudinal study. Am Rev Respir Dis. 1989 Aug;140(2):350–357. doi: 10.1164/ajrccm/140.2.350. [DOI] [PubMed] [Google Scholar]
- Meinert R., Frischer T., Karmaus W., Kuehr J. Influence of skin prick test criteria on estimation of prevalence and incidence of allergic sensitization in children. Allergy. 1994 Aug;49(7):526–532. doi: 10.1111/j.1398-9995.1994.tb01124.x. [DOI] [PubMed] [Google Scholar]
- Pattemore P. K., Asher M. I., Harrison A. C., Mitchell E. A., Rea H. H., Stewart A. W. The interrelationship among bronchial hyperresponsiveness, the diagnosis of asthma, and asthma symptoms. Am Rev Respir Dis. 1990 Sep;142(3):549–554. doi: 10.1164/ajrccm/142.3.549. [DOI] [PubMed] [Google Scholar]
- Regnis J. A., Alison J. A., Henke K. G., Donnelly P. M., Bye P. T. Changes in end-expiratory lung volume during exercise in cystic fibrosis relate to severity of lung disease. Am Rev Respir Dis. 1991 Sep;144(3 Pt 1):507–512. doi: 10.1164/ajrccm/144.3_Pt_1.507. [DOI] [PubMed] [Google Scholar]
- Ryan G., Latimer K. M., Dolovich J., Hargreave F. E. Bronchial responsiveness to histamine: relationship to diurnal variation of peak flow rate, improvement after bronchodilator, and airway calibre. Thorax. 1982 Jun;37(6):423–429. doi: 10.1136/thx.37.6.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanz J., Martorell A., Saiz R., Alvarez V., Carrasco J. I. Peak expiratory flow measured with the Mini Wright Peak Flow Meter in children. Pediatr Pulmonol. 1990;9(2):86–90. doi: 10.1002/ppul.1950090205. [DOI] [PubMed] [Google Scholar]
- Sears M. R., Burrows B., Flannery E. M., Herbison G. P., Hewitt C. J., Holdaway M. D. Relation between airway responsiveness and serum IgE in children with asthma and in apparently normal children. N Engl J Med. 1991 Oct 10;325(15):1067–1071. doi: 10.1056/NEJM199110103251504. [DOI] [PubMed] [Google Scholar]
- Siersted H. C., Hansen H. S., Hansen N. C., Hyldebrandt N., Mostgaard G., Oxhøj H. Evaluation of peak expiratory flow variability in an adolescent population sample. The Odense Schoolchild Study. Am J Respir Crit Care Med. 1994 Mar;149(3 Pt 1):598–603. doi: 10.1164/ajrccm.149.3.8118624. [DOI] [PubMed] [Google Scholar]
- Sly P. D., Hibbert M. E., Landau L. I. Diurnal variation of peak expiratory flow rate in asthmatic children. Pediatr Pulmonol. 1986 May-Jun;2(3):141–146. doi: 10.1002/ppul.1950020305. [DOI] [PubMed] [Google Scholar]
- Strachan D. P. Repeatability of ventilatory function measurements in a population survey of 7 year old children. Thorax. 1989 Jun;44(6):474–479. doi: 10.1136/thx.44.6.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studnicka M. J., Frischer T., Weiss S. T., Dockery D. W., Speizer F. E., Neumann M. G. Seasonal and allergenic predictors of bronchial responsiveness to distilled water. Am Rev Respir Dis. 1993 Dec;148(6 Pt 1):1460–1466. doi: 10.1164/ajrccm/148.6_Pt_1.1460. [DOI] [PubMed] [Google Scholar]


