Abstract
Loss of motion of the fifth tarsometatarsal joint can be a cause of lateral foot pain after Lisfranc fracture-dislocation or fracture of the fifth metatarsal tubercle. Arthroscopic lysis of the joint can be an effective surgical treatment with the advantage of minimal soft-tissue trauma and early vigorous mobilization of the joint. The lysis can be extended to the fourth tarsometatarsal joint and the adjacent tendons if indicated.
The Lisfranc joint is the combination of the intertarsal, proximal intermetatarsal, and tarsometatarsal (TMT) joints,1 which are flat joints supported by strong ligaments. The medial 3 TMT joints are relatively immobile, with the second and third TMT joints being dominant in contact loading and the medial 3 TMT joints being dominant in force transmission. The fourth and fifth TMT joints are mobile and function as a unit about an independent axis of motion.1 Each of the fourth and fifth TMT joints has an arc of motion approximating 10° in both the flexion-extension and supination-pronation planes.2
Lisfranc fracture-dislocation or fracture of the tubercle of the fifth metatarsal can result in arthrofibrosis of the fifth TMT joint, especially after open reduction, internal fixation, and cast immobilization. The resultant stiffness of the joint can cause lateral foot pain. We describe the technique of endoscopic lysis of the joint, which has minimal soft-tissue trauma and allows early vigorous mobilization of the joint. We believe that this can maximize the functional recovery and minimize the risk of recurrence of symptoms.
Technique
The patient is supine, and a tourniquet is applied to the ipsilateral thigh to provide a bloodless surgical field. Arthroscopy of the fifth TMT is performed through the P45 and lateral TMT portals. The P45 portal is located at the junction point between the fourth and fifth TMT joints, and the lateral portal is just dorsal to the insertion of the peroneus brevis tendon at the tip of the fifth metatarsal tubercle.3 The portals are located with needles and checked under fluoroscopy before skin incisions are made. A 2.7-mm 30° arthroscope (Henke-Sass Wolf, Tuttlingen, Germany) is used. The P45 and lateral portals can be switched as the visualization and instrumentation portals. Entry to the dorsal gutter of the fifth TMT joint can be difficult because the dorsal capsule is contracted and the dorsal gutter is filled with fibrous tissue. The contracted dorsal capsule can be stripped from the joint with a small periosteal elevator before insertion of the arthroscope and shaver. The fibrous tissue of the dorsal gutter of the fifth TMT joint is resected with an arthroscopic shaver (Smith & Nephew Endoscopy, Andover, MA) (Fig 1). In the second step, the scar tissue at the lateral gutter (just proximal to the nonarticular part of the base of the fifth metatarsal) is resected with an arthroscopic shaver through the lateral portal (Fig 2). The scar tissue is usually dense and needs to be mobilized with an arthroscopic probe before resection with an arthroscopic shaver. The third step is release of the fibrous tissue from the fifth metatarsal. The distal attachment of the dorsal capsule of the fifth TMT joint is stripped together with the scar tissue from the base of the fifth metatarsal joint with a shaver and small periosteal elevator (Fig 3). The fourth step is release of the fibrous tissue from the cuboid. The proximal attachment of the dorsal capsule of the fifth TMT joint is stripped together with the scar tissue from the cuboid (Fig 4). The extent of proximal and distal stripping depends on the extent of fibrosis. This depends on the approach and instrumentation during the previous fixation of the fracture. The adhesiolysis should extend beyond the previous operative site. Open reduction and tension-band wiring or plating of the fracture usually require a more distal incision and dissection of the proximal part of the fifth metatarsal. This will induce fibrosis at the metatarsal and require more extensive distal adhesiolysis. Closed reduction and intramedullary screw fixation of the fracture, on the other hand, require a more proximal incision and dissection. This will induce fibrosis at the cuboid region and require more extensive proximal adhesiolysis. After adequate clearance of the scar tissue and adhesiolysis, the normal joint motion is restored and the joint can be opened for examination of the articular cartilage (Video 1). Postoperatively, full weight bearing is allowed, and the patient is instructed to perform passive mobilization of the joint (Table 1).
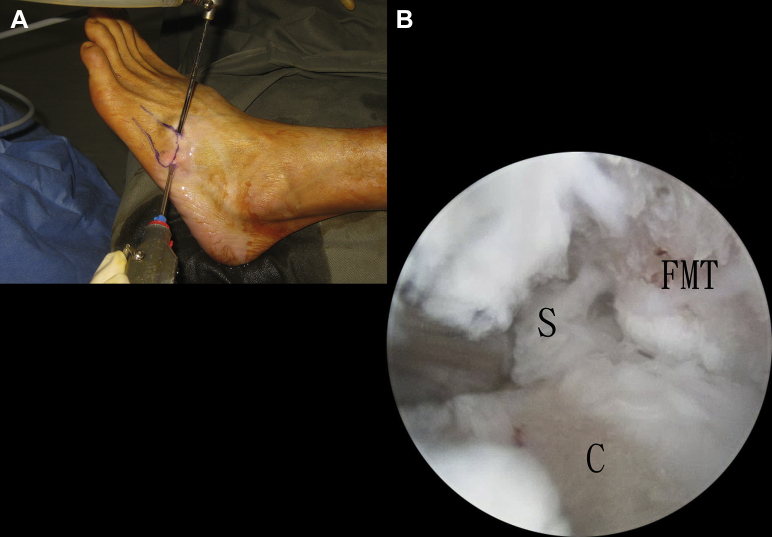
Fig 1.
(A) Lateral Lisfranc arthroscopy of the left foot is performed through the portals at the fifth metatarsal tubercle (lateral portal) and at the junction between the fourth and fifth tarsometatarsal joints (P45 portal). (B) The scar tissue at the dorsal gutter of the fifth metatarsal is resected with an arthroscopic shaver, and the articulation between the fifth metatarsal (FMT) and cuboid (C) is exposed.
Fig 2.
The scar tissue (S) at the lateral gutter of the fifth tarsometatarsal joint is resected with an arthroscopic shaver through the lateral portal. It may be helpful to lessen the amount of deep scar tissue with an arthroscopic probe before resection. (C, cuboid; FMT, fifth metatarsal.)
Fig 3.
The dorsal capsule of the fifth tarsometatarsal joint is stripped from the metatarsal together with the scar tissue at the dorsum of the base of the fifth metatarsal (FMT).
Fig 4.
The dorsal capsule of the fifth tarsometatarsal joint is stripped from the cuboid together with the scar tissue at the dorsum of the cuboid (C).
Table 1.
Pearls of Arthroscopic Lysis of Fifth Tarsometatarsal Joint
| The contracted dorsal capsule can be stripped from the joint with a small periosteal elevator before insertion of the arthroscope and shaver. |
| Keeping the shaver opening toward the bone can minimize the risk of tendon injury. |
| The adhesiolysis should extend beyond the previous operative site. |
| Vigorous mobilization of the fifth tarsometatarsal joint should be started immediately after the operation. |
Discussion
Whereas the medial 3 TMT joints are relatively immobile, the more mobile lateral fourth and fifth TMT joints provide balance and accommodation on uneven ground.4 The mobility of the fourth and fifth TMT joints is important for normal function of the foot.2, 5
Post-traumatic degeneration is the primary cause of arthritis of the Lisfranc joint, although primary degeneration and inflammatory conditions can also affect this area. Surgical intervention is indicated if nonoperative measures fail to relieve the symptoms. It typically involves arthrodesis of the medial TMT joints.4 Involvement of the more mobile fourth and fifth TMT joints presents a difficult clinical situation.6 The best surgical treatment is a subject of debate,4 although maintaining mobility of the fourth and fifth TMT joints has been reported to be important in arthrodesis of the midfoot.5, 6, 7 A lateral TMT resection arthroplasty with tendon interposition has been proposed for symptomatic fourth and fifth TMT arthritis to relieve pain while maintaining joint mobility.6 Ceramic interpositional arthroplasty is another surgical option with maintenance of joint motion.7 Arthrodesis of the fourth and fifth TMT joints may lead to the development of chronic pain from overloading the usually mobile lateral column, resulting in an increased nonunion and stress fracture rate, as well as the development of a rigid prominence on the lateral side of the midfoot.5 Other concerns with arthrodesis include foot stiffness, metatarsalgia, and arthrosis in the adjacent joints, particularly the calcaneocuboid joint.1 It may be a last resort for patients with lateral column collapse, rocker bottom deformity, and debilitating symptoms.1, 5
Besides post-traumatic arthritis, loss of motion of the lateral TMT joints can lead to an unfavorable outcome after Lisfranc fracture-dislocation.8 A similar problem has been observed after fracture of the tubercle of the fifth metatarsal.9
Arthroscopic lysis of the fifth TMT joint is indicated in patients with symptomatic stiffness of the joint without arthritic changes. In the case of arthritis of the joint, arthroscopic tendon interposition arthroplasty should be performed instead.3, 10 The fourth and fifth TMT joints have support from the interosseous ligaments, the dorsal and plantar cubometatarsal ligaments, and a slip from the long plantar ligament. The fourth metatarsal base is also supported by a slip from the tibialis posterior tendon and the adductor obliquus hallucis. The plantar capsular and ligamentous structures provide the most soft-tissue support to the fourth and fifth TMT joints.6 These structures are preserved during the arthroscopic lysis. The potential sites of fibrosis (lateral and dorsal gutters of the joint and dorsal surface of the fifth metatarsal and cuboid) are released during the procedure. If the fourth TMT joint is also involved, both the fourth and fifth TMT joints can be released through the P34 portal (junction between the third and fourth TMT joints) and lateral portal because the joints share a common capsular compartment.3, 6 Finally, if there is concomitant adhesion of the adjacent tendons (e.g., peroneus tertius and extensor tendon to fifth toe), endoscopic tenolysis can be performed through the same portals.
The sural nerve, intermedial dorsal cutaneous nerve of the superficial peroneal nerve, peroneus tertius tendon, peroneus brevis tendon, and extensor tendon to the little toe are potentially at risk during the procedure. This technique is technically demanding and should be performed by arthroscopists familiar with small joint arthroscopy of the foot and ankle.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Arthroscopic lysis of the fifth tarsometatarsal joint of the left foot. The patient is in the supine position. In step 1, lateral Lisfranc arthroscopy is performed with the portals at the fifth metatarsal tubercle (lateral portal) and at the junction between the fourth and fifth tarsometatarsal joints (P45 portal). The scar tissue at the dorsal gutter of the fifth metatarsal is resected with an arthroscopic shaver. After resection of the scar tissue, the articular cartilage of the tarsometatarsal joint can be seen. In step 2, the scar tissue at the lateral gutter of the fifth tarsometatarsal joint is resected with an arthroscopic shaver through the lateral portal. It may be helpful to lessen the amount of deep scar tissue with an arthroscopic probe before resection. In step 3, the dorsal capsule of the fifth tarsometatarsal joint is stripped from the metatarsal together with the scar tissue at the dorsum of the base of the fifth metatarsal. In step 4, the dorsal capsule of the fifth tarsometatarsal joint is stripped from the cuboid together with the scar tissue at the dorsum of the cuboid. Finally, after adequate lysis, the normal gliding motion of the joint can be observed.
References
- 1.Russell D.F., Ferdinand R.D. Review of the evidence: Surgical management of 4th and 5th tarsometatarsal joint osteoarthritis. Foot Ankle Surg. 2013;19:207–211. doi: 10.1016/j.fas.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Ouzounian T.J., Shereff M.J. In vitro determination of midfoot motion. Foot Ankle. 1989;10:140–146. doi: 10.1177/107110078901000305. [DOI] [PubMed] [Google Scholar]
- 3.Lui T.H. Arthroscopic tarsometatarsal (Lisfranc) arthrodesis. Knee Surg Sports Traumatol Arthrosc. 2007;15:671–675. doi: 10.1007/s00167-006-0142-6. [DOI] [PubMed] [Google Scholar]
- 4.Patel A., Rao S., Nawoczenski D., Flemister A.S., DiGiovanni B., Baumhauer J.F. Midfoot arthritis. J Am Acad Orthop Surg. 2010;18:417–425. doi: 10.5435/00124635-201007000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Raikin S.M., Schon L.C. Arthrodesis of the fourth and fifth tarsometatarsal joints of the midfoot. Foot Ankle Int. 2003;24:584–590. doi: 10.1177/107110070302400803. [DOI] [PubMed] [Google Scholar]
- 6.Berlet G.C., Hodges Davis W., Anderson R.B. Tendon arthroplasty for basal fourth and fifth metatarsal arthritis. Foot Ankle Int. 2002;23:440–446. doi: 10.1177/107110070202300512. [DOI] [PubMed] [Google Scholar]
- 7.Viens N.A., Adams S.B., Jr., Nunley J.A., II Ceramic interpositional arthroplasty for fourth and fifth tarsometatarsal joint arthritis. J Surg Orthop Adv. 2012;21:126–131. doi: 10.3113/jsoa.2012.0126. [DOI] [PubMed] [Google Scholar]
- 8.Teng A.L., Pinzur M.S., Lomasney L., Mahoney L., Havey R. Functional outcome following anatomic restoration of tarsal-metatarsal fracture dislocation. Foot Ankle Int. 2002;23:922–926. doi: 10.1177/107110070202301006. [DOI] [PubMed] [Google Scholar]
- 9.Lui T.H. Lateral foot pain following open reduction and internal fixation of the fracture of the fifth metatarsal tubercle: Treated by arthroscopic arthrolysis and endoscopic tenolysis. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-204116. bcr2014204116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lui T.H. Arthroscopy and endoscopy of the foot and ankle: Indications for new techniques. Arthroscopy. 2007;23:889–902. doi: 10.1016/j.arthro.2007.03.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic lysis of the fifth tarsometatarsal joint of the left foot. The patient is in the supine position. In step 1, lateral Lisfranc arthroscopy is performed with the portals at the fifth metatarsal tubercle (lateral portal) and at the junction between the fourth and fifth tarsometatarsal joints (P45 portal). The scar tissue at the dorsal gutter of the fifth metatarsal is resected with an arthroscopic shaver. After resection of the scar tissue, the articular cartilage of the tarsometatarsal joint can be seen. In step 2, the scar tissue at the lateral gutter of the fifth tarsometatarsal joint is resected with an arthroscopic shaver through the lateral portal. It may be helpful to lessen the amount of deep scar tissue with an arthroscopic probe before resection. In step 3, the dorsal capsule of the fifth tarsometatarsal joint is stripped from the metatarsal together with the scar tissue at the dorsum of the base of the fifth metatarsal. In step 4, the dorsal capsule of the fifth tarsometatarsal joint is stripped from the cuboid together with the scar tissue at the dorsum of the cuboid. Finally, after adequate lysis, the normal gliding motion of the joint can be observed.