Abstract
Background
Although survival benefits have been shown at the population level, it remains unclear what drives the outcome benefits for helicopter emergency medical services (HEMS) in trauma. While speed is often cited as the vital factor of HEMS, we hypothesized a survival benefit would exist in the absence of a time-savings over ground emergency medical services (GEMS). The objective was to examine the association of survival with HEMS compared to GEMS transport across similar prehospital transport times (PHTT).
Methods
Retrospective cohort of scene HEMS and GEMS transports in the NTDB (2007–2012). Propensity score matching was used to match HEMS and GEMS subjects on the likelihood of HEMS transport. Subjects were stratified by PHTT in 5min increments. Conditional logistic regression determined the association of HEMS with survival across PHTT strata controlling for confounders. Transport distance was estimated from PHTT and average HEMS/GEMS transport speeds.
Results
There were 155,691 HEMS/GEMS pairs matched. HEMS had a survival benefit over GEMS for PHTT between 6 and 30min. This benefit ranged from a 46% increase in odds of survival between 26–30min (AOR 1.46; 95%CI 1.11—1.93, p<0.01) to an 80% increase in odds of survival between 16–20min (AOR 1.80; 95%CI 1.52—2.03, p<0.01). This PHTT window corresponds to estimated transport distance between 14.3–71.3mi for HEMS and 3.3–16.6mi for GEMS.
Conclusions
When stratified by PHTT, HEMS had a survival benefit concentrated in a window between 6–30min. Since there was no time-savings advantage for HEMS, these findings may reflect care delivered by HEMS providers.
INTRODUCTION
Helicopter emergency medical services (HEMS) have become an integral component of modern trauma systems in the United States. Although significant survival benefits for HEMS compared to ground emergency medical services (GEMS) have been shown at the population level,1–5 it remains unclear what elements of this intervention are driving these outcomes. Factors that have been suggested as determinants of improved outcomes for HEMS transport in trauma include speed, availability of advanced interventions, and trauma center access.6 It is likely some combination of these elements; however these issues have been difficult to evaluate in prior work.
The most obvious advantage of HEMS over GEMS transport is speed. This is highly dependent on a number of factors, including distance from the scene of injury to the helicopter base and trauma center, traffic, weather, HEMS activation timing, and geographic distribution of HEMS bases.7, 8 Recent guidelines recommend HEMS transport only if a significant time savings is present over GEMS transport; however no definition of a significant time savings was suggested.9
While trauma remains a time-sensitive disease, and delay to definitive care is a well-documented cause of adverse outcomes,10 HEMS may confer benefits other than simply being faster. HEMS providers often have advanced capabilities beyond those available from GEMS providers. Particularly for airway interventions, others have shown high rates of procedural success and improved outcomes for air medical providers.11–13 Our group recently demonstrated prehospital blood transfusion by HEMS providers significantly improves early outcomes for air medical trauma patients in shock.14 Additionally, HEMS providers have greater experience with severely injured patients. As a result, HEMS providers are more familiar with managing these patients, and may confer outcome benefits similar to the volume-outcome relationship seen for trauma centers. Thus HEMS providers may act as a form of “regionalized” prehospital trauma care.
Finally, HEMS transport may impart benefit from providing access directly to a trauma center rather than transport to a non-trauma center for initial evaluation. Nirula and colleagues demonstrated transfer compared to direct transport to a trauma center worsened outcomes,15 and this may underlie some of the benefit of HEMS by reducing time to definitive care rather than simply reducing out of hospital time.
It is possible then that injured patients undergoing HEMS transport may have a survival benefit when no time-saving advantage is present. Others have shown a survival benefit for HEMS transport independent of total prehospital time in patients with physiologic instability.16 Thus, it was the objective of this study to examine the association of survival with HEMS compared to GEMS transport across similar prehospital transport times. We hypothesized that factors other than speed play a role in outcome, and that a survival benefit would exist for HEMS transport even in the absence of a time-saving advantage over GEMS transport.
METHODS
Study Population
Patients aged ≥16 years undergoing either HEMS or GEMS transport from the scene of injury in the National Trauma Databank (NTDB) between 2007 and 2012 were eligible for inclusion. The NTDB represents a national database containing over 3 million injured patients from more than 900 hospitals in the US.17 Subjects transferred from another hospital, that were dead on arrival, or had unknown United States geographic census region were excluded. Subjects with missing prehospital transport time were also excluded. Demographics, injury severity, vital signs, prehospital response time, prehospital scene time, prehospital transport time, International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes, intensive care unit (ICU) admission, mechanical ventilation, emergency department (ED) disposition, hospital disposition, and hospital characteristics were collected for each subject. Subjects were then stratified by prehospital transport time in 5 minute increments between 0 minutes and 60 minutes to remove any significant time-saving advantage for HEMS transport. Subjects with a prehospital transport time >60 minutes were grouped together.
Missing Data
Multiple imputation was performed for analysis variables missing between 1% and 25% of observations. Imputed variables included insurance status, mechanism of injury, prehospital systolic blood pressure (SBP), prehospital heart rate (HR), prehospital respiratory rate (RR), and prehospital Glasgow Coma Scale (GCS). Multiple imputation using an iterative Markov chain Monte Carlo fully conditional specification model based on available demographics, vital signs, and injury characteristics was performed using five imputation steps to develop five imputed datasets. Outcome models were performed using multiple imputation estimation techniques that combine model coefficients and standard errors from each imputed dataset while adjusting for the variability between imputed datasets.18 Missing data for imputed variables ranged from 3% (mechanism of injury) to 14% (insurance status). The analysis was repeated using complete cases only to assess the multiple imputation procedures, and no significant differences were seen between the imputed and complete case results.
Propensity Score Matching
As transport mode was not randomly assigned, HEMS subjects were more likely to be severely injured and represents treatment selection bias. To mitigate this, propensity score matching was performed. Propensity score matching has been shown to produce more accurate treatment effect estimates when comparing HEMS and GEMS patients, and reduces potential bias by matching treated and control subjects based on their likelihood of being exposed to the treatment taking into account known variables in the dataset that would be expected to influence treatment assignment.2, 19 The propensity score model was developed to predict the likelihood of undergoing HEMS transport based on prehospital information that prehospital providers would reasonably use to guide the decision to assign a patient to either HEMS or GEMS transport at the scene of injury. Covariates in the propensity score model included age, gender, prehospital SBP, prehospital HR, prehospital RR, prehospital GCS, prehospital response time, prehospital scene time, and the presence of any one of the eight anatomic triage criteria from the most recent version of the Centers for Disease Control national field triage guidelines.20 Prehospital response and scene times were included to ensure no time-saving advantage would be present for HEMS transport outside of transport time. Propensity scores were estimated using a probit model. Propensity score model performance was assessed using the C-statistic. HEMS subjects were considered treatment subjects while GEMS subjects were considered control subjects.
As geographic region can significantly influence outcomes for HEMS,21 matching was performed separately within each geographic United States census region to ensure matched pairs being compared came from similar geographic regions.22 Matched pairs from each of the US census regions were then combined to give the final study population. Matching was performed using a 1:1 ratio nearest neighbor algorithm without replacement or caliper. Standardized differences were used to assess the balance of covariates used in propensity score estimation after matching. An absolute value for the standardized difference >0.2 for a given variable was considered to indicate significant residual imbalance between treatment groups.23
Statistical Analysis
In-hospital survival was the primary outcome. Conditional logistic regression models were used to determine the association of survival with HEMS compared to GEMS transport across prehospital transport time strata. Model covariates were selected a priori for known prognostic significance in survival after injury which were not accounted for in the propensity score matching procedure. Covariates included race, insurance status, injury severity score (ISS), Trauma Mortality Prediction Model (TMPM) predicted mortality,24 ICU admission, need for urgent operation, need for mechanical ventilation, and trauma center level. These covariates were then confirmed to be associated with survival in univariate analysis or change the model coefficient for transport mode by ≥10%. Collinearity was assessed using variance inflation factors and any covariate with a value >10 was removed from final models. Model standard errors were calculated using a sandwich estimator that allowed for intragroup correlation to account for clustering at the center level. For each of the thirteen prehospital transport time strata, the adjusted odds ratio (AOR) and 95% confidence interval (95%CI) of in-hospital survival for HEMS compared to GEMS transport was determined.
To account for multiple model comparisons across prehospital transport time strata, false discovery rate correction was used. False discovery rate correction is a powerful method to ensure the probability of a type I error remains at the pre-specified level across all hypotheses tested and reports q-values which are false discovery rate adjusted p values.25 These q-values can be interpreted similarly to standard p values, and for this study a q-value ≤0.05 was considered statistically significant with two-sided tests.
For univariate comparisons of baseline subject-level characteristics, standardized differences were used with an absolute value for the standardized difference >0.2 again considered to indicate significant residual imbalance between treatment groups. Standardized differences have been proposed as a superior method of comparing baseline characteristics in matched samples.26 Further, standardized differences are not influenced by large samples sizes as standard t-tests or Chi-square tests are, which can result in statistically significantly differences when no clinically meaningful difference exists. Data analysis was conducted using Stata version 13 (College Station, TX).
Transport Distance
Due to the relative difference in transport speed between helicopter and ground ambulances, similar prehospital transport times represent different transport distances, depending on a number of factors including traffic, weather, and geography. To evaluate these potential differences, transport distance was estimated using prehospital transport time and transport speed. Transport speeds were obtained from a meta-analysis of prehospital trauma care times, which reported national average transport speeds for helicopter and ground ambulances.27 Helicopter transport was estimated at an average speed of 142.6mph. Ground ambulance transport was estimated at an average speed of 20.1mph in urban areas, 47.5mph in suburban areas, and 56.4mph in rural areas. These speeds were used to estimate the average transport distance for prehospital transport time intervals where survival was significantly difference between HEMS and GEMS transport. For ground ambulance transport, the three transport speeds for different population densities were combined into a single weighted average. The proportion of urban, suburban, and rural land area in the United States was obtained from census data and used to calculate a weighted average ground ambulance speed within each US census region.22, 28 The proportion of each US census region among GEMS transports in the matched cohort was then used to calculate a weighted average of ground ambulance transport speed across the US, which was then used to estimate transport distances from prehospital transport time.
To evaluate the geographic coverage represented by prehospital transport time across specific geographic regions, a geographic information systems (GIS) network analysis was performed. Geographic locations of level I and II trauma centers in the United States were geocoded and mapped.29 Network service area analysis was performed using prehospital transport times as driving times to each trauma center to represent the ground ambulance geographic coverage for prehospital transport time intervals that had significantly different survival between HEMS and GEMS transport. Buffer analysis was also performed to represent the geographic coverage of straight line helicopter transport to each trauma center for the same prehospital transport time intervals. All GIS analysis was performed using ArcGIS software (ESRI, Redlands, CA).
Sensitivity Analyses
Given the differences in GEMS and HEMS logistics for transport, four sensitivity analyses were undertaken to ensure substantial differences in outcomes were not seen under a variety of conditions. Since HEMS transport is sometimes initiated after arrival and assessment by a GEMS unit, a time lag may occur prior to activation of the HEMS unit for transport. Further, this may introduce potential survival bias if severely injured patients assessed by GEMS units did not survive long enough for HEMS activation. Although patients dead on arrival were initially excluded from the main study population to mitigate the potential for this type survival bias, we further excluded all patients who died in the ED in the first sensitivity analysis to evaluate outcomes without early deaths.
The NTDB allows documentation of other types of prehospital transport and treatment in addition to the primary transport mode to the hospital. All patients who underwent HEMS transport and had a GEMS unit documented as providing care during the prehospital period were identified. For the next sensitivity analysis, the median GEMS response time (6min) and scene time (15min) among all GEMS patients prior to matching was added to the response time for HEMS patients that had involvement of a GEMS unit prior to transport by helicopter to account for the time lag that may occur prior to HEMS activation. A third more conservative sensitivity analysis was also conducted in which the 21 minute lag time was added to the response time for all HEMS transport patients. Finally, the last sensitivity analysis excluded all HEMS patients that had involvement of a GEMS unit prior to transport.
For all sensitivity analyses, exclusions or time additions were made to the original study population of subjects available for matching. Subsequently, propensity score matching and the outcome models were then reapplied to the new set of subjects available for matching in each sensitivity analysis.
RESULTS
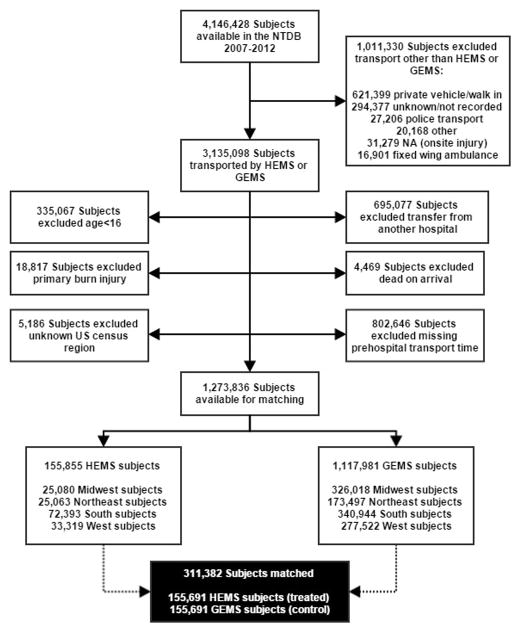
Of the 1,273,836 subjects available for matching, 155,691 pairs were matched giving a final study population of 311,382 subjects for analysis (Fig. 1). After matching in each region, no variable included in the estimation of the propensity score remained unbalanced with an absolute value of the standardized difference >0.2 (Table 1), and standardized difference was reduced for each propensity score variable within each region (Fig 2). The propensity score model C-statistic ranged from 0.87 in the West to 0.94 in the Midwest, indicating excellent discrimination across all US census regions to predict treatment assignment.
Figure 1.
Study participant selection of helicopter emergency medical service (HEMS) and ground emergency medical service (GEMS) subjects from the National Trauma Databank 2007—2012.
Table 1.
Characteristics of matched subjects transported by HEMS or GEMS
| HEMS n = 155,691 |
GEMS n = 155,691 |
Standardized difference* | |
|---|---|---|---|
| Age [years, med (IQR)] | 39 (25, 54) | 39 (24, 57) | −0.083 |
| Sex [n (%) male] | 110,565 (71) | 106,941 (69) | 0.045 |
| Race [n (%)] | −0.219 | ||
| Caucasian | 128,029 (82) | 114,262 (73) | |
| Non-Caucasian | 27,662 (18) | 41,429 (27) | |
| Insurance Status [n (%)] | 0.131 | ||
| Commercial | 80,959 (52) | 70,527 (45) | |
| Subsidized/None | 74,732 (48) | 85,164 (52) | |
| Mechanism [penetrating, n (%)] | 13,115 (8) | 17,958 (12) | −0.107 |
| Prehospital response time [mins, med (IQR)] | 19 (13, 25) | 20 (13, 27) | −0.057 |
| Prehospital scene time [mins, med (IQR)] | 14 (10, 21) | 15 (10, 21) | 0.001 |
| Prehospital transport time [mins, med (IQR)] | 21 (16, 30) | 24 (15, 36) | −0.203 |
| Prehospital SBP [mmHg, med (IQR)] | 131 (115, 147) | 132 (118, 148) | −0.018 |
| Prehospital HR [beats/min, med (IQR)] | 93 (80, 108) | 91 (80, 106) | 0.056 |
| Prehospital RR [breaths/min, med (IQR)] | 18 (16, 20) | 18 (16, 20) | −0.049 |
| Prehospital GCS [med (IQR)] | 15 (13, 15) | 15 (14, 15) | −0.123 |
| Anatomic triage criteria [n (%)] | 41,081 (26) | 36,750 (24) | 0.064 |
| ISS [med (IQR)] | 13 (6, 22) | 9 (4, 14) | 0.404 |
| TMPM predicted mortality [%, med(IQR)] | 2.7 (1.1, 10.7) | 1.7 (0.8, 4.7) | 0.214 |
| ICU admission [n (%)] | 75,499 (49) | 43,717 (28) | 0.423 |
| Urgent operation [n (%)] | 29,775 (19) | 20,353 (13) | 0.161 |
| Mechanical ventilation [n (%)] | 43,955 (28) | 23,535 (15) | 0.317 |
| Trauma center level | 0.455 | ||
| Level I/II | 150,159 (96) | 128,783 (83) | |
| Non-Level I/II | 5,532 (4) | 26,908 (17) | |
| In-hospital Survival [n (%)] | 142,968 (92) | 144,559 (93) | −0.039 |
Represents the standardized difference between groups after matching for variables used in propensity score estimation. Absolute values for the standardized difference >0.2 are considered to indicate imbalance between groups after matching.
HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; med, median; IQR, interquartile range; SBP, systolic blood pressure; HR, heart rate; RR, respiratory rate; GCS, Glasgow Coma Scale; ISS, injury severity score; TMPM, trauma mortality prediction model; ICU, intensive care unit
Figure 2.
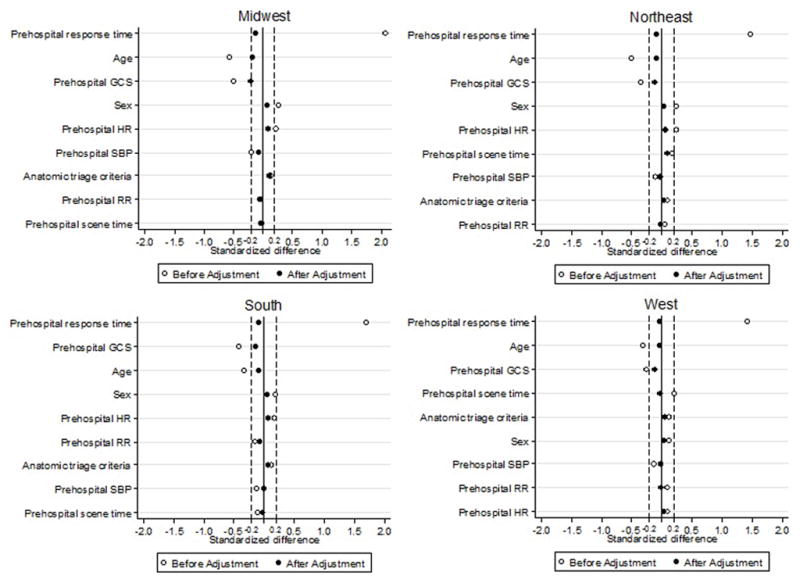
Standardized differences for variables included in the propensity score estimation before and after the matching procedure in each geographic United States census region.
Table 1 summarizes and compares characteristics of matched HEMS and GEMS subjects. After matching, HEMS and GEMS groups had similar prehospital response (19min vs. 20min), scene (14min vs 15min), and transport (21min vs 24min) times, as well as prehospital vital signs. HEMS subjects were more likely Caucasian, had a higher ISS, TMPM predicted mortality, rate of ICU admission and mechanical ventilation, and more often brought to a level I or II trauma center.
The distribution of prehospital transport time strata are shown in Table 2. When stratified by prehospital transport time, HEMS transport was associated with an increased odds of in-hospital survival for prehospital transport times between 6 and 30 minutes (Fig. 3). The significant benefit of HEMS transport began at transport times between 6 and 10 minutes (AOR 1.69; 95%CI 1.21—2.35, q=0.006), increased between 11 and 15 minutes (AOR 1.71; 95%CI 1.45—2.03, q=0.004), peaked between 16 to 20 minutes with an 80% increase in odds of survival (AOR 1.80; 95%CI 1.51—2.14, q=0.004), and declined through 21 to 25 minutes (AOR 1.53; 95%CI 1.24—1.88, q=0.004) and 26 to 30 minutes (AOR 1.46; 95%CI 1.11—1.93, q=0.018. There was no difference in the odds of survival between HEMS and GEMS groups for very early prehospital transport times (0–5 minutes) or transport times longer than 30 minutes (q>0.05).
Table 2.
Distribution of prehospital transport time by transport mode
| Prehospital transport time strata [n (%)] | HEMS n = 155,691 |
GEMS n = 155,691 |
|---|---|---|
| 0 – 5 minutes | 1,840 (1.2) | 5,776 (3.7) |
| 6 – 10 minutes | 8,818 (5.7) | 14,386 (9.2) |
| 11 – 15 minutes | 26,214 (16.7) | 21,595 (13.9) |
| 16 – 20 minutes | 34,669 (22.3) | 22,549 (14.5) |
| 21 – 25 minutes | 28,478 (18.3) | 20,732 (13.3) |
| 26 – 30 minutes | 19,656 (12.6) | 17,319 (11.1) |
| 31 – 35 minutes | 12,891 (8.3) | 13,797 (8.9) |
| 36 – 40 minutes | 8,419 (5.4) | 10,687 (6.9) |
| 41 – 45 minutes | 5,412 (3.5) | 8,027 (5.2) |
| 46 – 50 minutes | 3,411 (2.2) | 5,738 (3.7) |
| 51 – 55 minutes | 2,094 (1.3) | 4,250 (2.7) |
| 56 – 60 minutes | 1,217 (0.8) | 3,318 (2.1) |
| >60 minutes | 2,572 (1.7) | 7,517 (4.8) |
HEMS, helicopter emergency medical services; GEMS, ground emergency medical services
Figure 3.
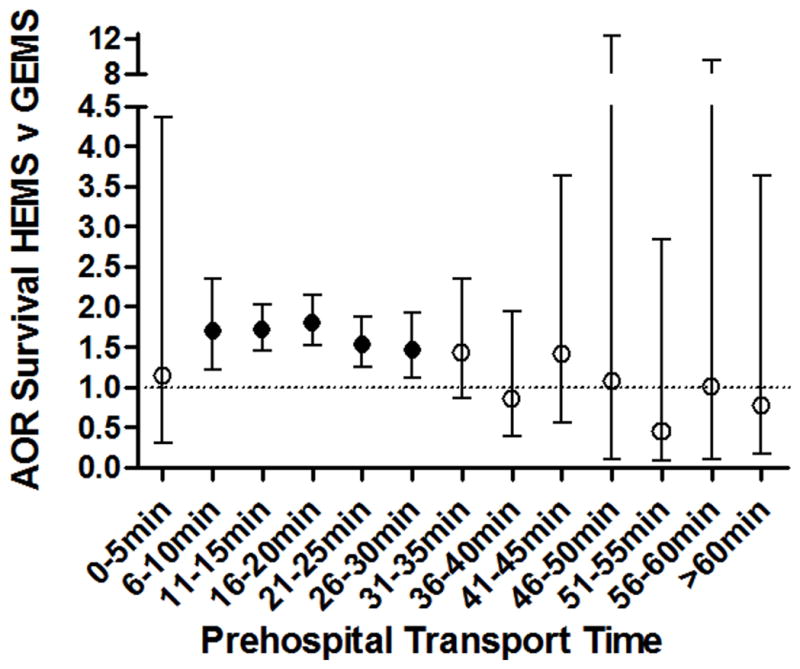
Adjusted odds ratio (AOR) of in-hospital survival for helicopter emergency medical services (HEMS) compared to ground emergency medical services (GEMS) across prehospital transport strata. Error bars represent the 95% confidence interval for the AOR. Error bars that cross the dotted line at 1.0 represent no significant difference in odds of survival between HEMS and GEMS subjects.
For HEMS transport, this 6 to 30 minute transport time window of survival benefit corresponds to an estimated average transport distance of 14.3 to 71.3 miles. For GEMS transport, the final weighted average ground ambulance transport speed was calculated at 33.3mph. The 6 to 30 minute transport window for GEMS transport corresponds to an estimated average transport distance of 3.3 to 16.6 miles.
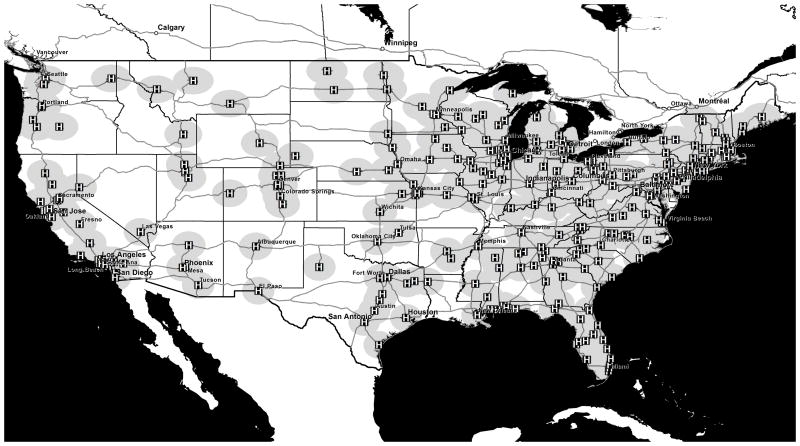
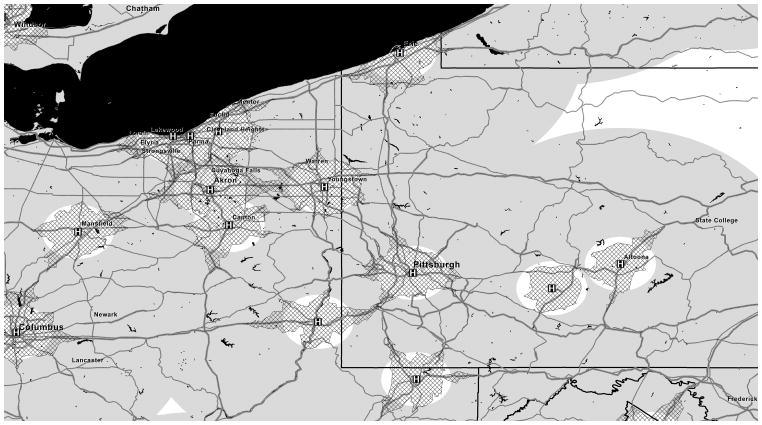
GIS analysis in Figure 4 demonstrates the geographic coverage for HEMS transport to a level I or level II trauma center in the United States with a transport time between 6 and 30 minutes. A closer view of western Pennsylvania and eastern Ohio as an example in Figure 5 again demonstrates the geographic coverage for helicopter transport, now with ground ambulance geographic coverage corresponding to transport times between 6 and 30 minutes. Depending on regional features, there may or may not be geographic overlap between helicopter and ground ambulance coverage within this transport time window.
Figure 4.
Geographic coverage for straight line helicopter transport to a level I or level II trauma center in the United States with a transport time between 6 and 30 minutes at an average speed of 142.6mph. The “H” hospital symbols represent level I or level II trauma centers; gray shading areas represent helicopter coverage.
Figure 5.
Geographic coverage for helicopter and ground ambulance transport to level I or level II trauma centers in western Pennsylvania and eastern Ohio with a transport time between 6 and 30 minutes. The “H” hospital symbols represent level I or level II trauma centers; gray shading areas represents helicopter coverage; cross-hatch shading areas represent ground ambulance coverage.
Sensitivity analyses revealed similar results to the main findings. When all deaths in the ED were excluded, 152,766 pairs were matched. HEMS transport again showed a significant increase in the odds of survival between 6 and 30 minutes. The benefit ranged from 36% increase in odds of survival (AOR 1.36; 95%CI 1.01—1.84, q=0.042) to a nearly 2.5 fold increase in odds of survival (AOR 2.47; 95%CI 1.27—4.84, q=0.008).
Overall, 31% of HEMS transports had a documented GEMS unit involved prior to transport. After adding a time lag to these patients, 147,227 pairs were matched. HEMS transport also showed a significant increase in the odds of survival between 6 and 30 minutes. The benefit ranged from 51% increase in odds of survival (AOR 1.51; 95%CI 1.06—2.16, q=0.023) to a 2 fold increase in odds of survival (AOR 2.00; 95%CI 1.48—2.70, q=0.004). When adding the time lag to all HEMS transports, 114,419 pairs were matched. The HEMS survival advantage persisted between 6 and 30 minutes, with the benefit ranging from 40% increase in odds of survival (AOR 1.40; 95%CI 1.02—1.94, q=0.037) to a more than 2 fold increase in odds of survival (AOR 2.27; 95%CI 1.17—4.39, q=0.015). When all HEMS patients with prior GEMS unit care were excluded, 107,301 patients were matched. The 6 to 30 minute benefit window remained for HEMS transport, ranging from 46% increase in odds of survival (AOR 1.46; 95%CI 1.14—1.88, q=0.008) to a nearly 2.5 fold increase in odds of survival (AOR 2.42; 95%CI 1.84—3.18, q=0.004). Thus, all sensitivity analyses demonstrated the same 6 to 30 minute window for benefit of HEMS transport while all other prehospital transport time strata were non-significant (q>0.05). The size of treatment effects are also similar to the main results with slightly widened confidence intervals likely due to the lower number of pairs in each sensitivity analysis.
DISCUSSION
The current results demonstrate HEMS transport has a significant survival benefit over GEMS transport for prehospital transport times between 6 and 30 minutes after propensity score matching and stratification by transport time. Thus, HEMS does demonstrate a survival benefit in the absence of a time savings over GEMS transport. This benefit peaked at a transport time between 16 and 20 minutes with a nearly two-fold increase in the odds of in-hospital survival. Survival in very short transport times and those longer than 30 minutes was not impacted by transport mode. This transport time window of benefit corresponds to an estimated helicopter transport distance between 14 and 71 miles and estimated ground ambulance transport distance between 3 and 17 miles. GIS analysis demonstrates that the geographic overlap for helicopter and ground ambulance transport to a level I or II trauma center within this transport time window appears to be dependent on regional highway and traffic networks. This will be further influenced by weather and time of day variations in traffic congestion.
Our approach of matching on prehospital response and scene times while stratifying by prehospital transport time meant there was no time-saving advantage for HEMS transport over GEMS transport. The matching of scene times also ensures that both HEMS and GEMS providers had the same length of time to provide on-scene care to the patients. Thus, patients in each transport mode group compared for survival were exposed to their prehospital providers for the same length of time. These findings then may reflect the care that is delivered to the patient by the respective prehospital providers during transport. Further, this benefit was not uniform across all transport times, and a transport time window for a survival benefit emerged. The pattern of this time widow would make sense if the effects seen are at least partially driven by care delivered by prehospital providers. For very early transport times between 0 and 5 minutes, it is unlikely that there is enough time for prehospital providers to administer any interventions to substantially impact survival. At longer transport times, it may be that if patients survived a prolonged transport time, they are likely to survive regardless of prehospital care delivered. Alternatively, it may be that longer transport times represent a delay to definitive care that negate any beneficial effect of the HEMS care and interventions. It is also possible that beyond 30 minutes of transport time, speed is the driving factor in improved outcomes which would not be seen in this matched analysis.
Several large studies utilizing the NTDB have demonstrated a survival benefit of HEMS over GEMS scene transport of injured patients.1, 2, 4, 5 These studies generally evaluated all comers who were transported to a level I or II trauma center. The magnitude of benefit ranged from a 16% increase in odds of survival in a propensity matched cohort to a 64% increase in odds of survival. However, each of these studies noted that it was unclear why HEMS conferred a survival advantage and further study was needed to elucidate the mechanisms of benefit. Thus, this study attempts to address this gap in knowledge and is the first to examine outcome between HEMS and GEMS transport while removing any time-saving advantage.
In Europe, HEMS agencies are frequently staffed by physicians and the helicopter’s role is primarily to bring advanced providers and capabilities to the injured patient. Several European studies report more advanced interventions in the prehospital environment with a HEMS physician led team.30–32 However, in the US the concept of HEMS has developed primarily to transport patients rapidly to a trauma center, most often without direct physician involvement. This has been reinforced by early studies demonstrating HEMS is not useful in US urban environments with proximity to trauma centers.33–35
Few studies in a US setting have examined the potential for HEMS transport to improve survival based on care provided. An early trial by Baxt demonstrated a physician staffed HEMS service had a lower actual-to-predicted mortality than a paramedic staffed HEMS service; however critics point out the modern prehospital care likely makes these results non-applicable to current trauma systems in the US.36 A study of patients with severe traumatic brain injury demonstrated airway interventions by HEMS providers resulted in improved outcomes.13 Our group recently evaluated a propensity score matched cohort of HEMS trauma patients receiving prehospital blood transfusion.14 Blood transfusion by HEMS providers was associated with a more than six-fold increase in the odds of 24hour survival and a strong trend towards in-hospital survival compared to matched controls not receiving transfusion. Thus, this advanced capability improves survival even within HEMS patients, and may be responsible in part for some of the survival benefit seen for HEMS transport of injured patients.
Ryb et al examined the effect of HEMS transport on outcomes in the NTDB while accounting for total prehospital time.16 The authors dichotomized patients by revised trauma score (RTS) and total prehospital time, demonstrating only patients with RTS <6 and total prehospital time <60 minutes transported by HEMS had an outcome benefit, with a more than two-fold increase in the odds of survival. Although limited by examining only total prehospital time with only two levels of stratification, the results do point towards the potential benefit of HEMS due to care delivered to patients. Only patients with physiological instability benefited from HEMS, and this group of patients is most likely to benefit from the advanced capabilities and experience of HEMS providers. The current study results are also similar to those of Ryb and colleagues, demonstrating shorter prehospital times are association with improved survival for HEMS, while patients with longer times are likely to survival regardless of transport mode and care delivered during transport.
Despite this, the current study cannot delineate the specific aspects of HEMS care that is responsible for the benefits seen. Although advanced capabilities may provide some benefit, some systems have similar capabilities between HEMS and GEMS providers. It may then be the experience of HEMS providers caring for severely injured patients, demonstrating a volume-outcome relationship among severely injured patients requiring life-saving interventions. Future studies should aim to evaluate the potential contributions of advanced capabilities and provider experience to improved outcomes in HEMS transport for trauma.
These findings also have potential important implications for HEMS triage of trauma patients. The issue of HEMS triage has been understudied; however the American College of Surgeons Committee on Trauma has raised it as a priority for future research.37, 38 Recently, multiple stakeholder agencies developed guidelines for air medical transport of trauma patients using Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology.9 This effort was hampered by very low quality evidence, but recommended HEMS transport in patients meeting any physiologic or anatomic triage criteria from the National Field Triage Guidelines only when a significant time savings is present over GEMS transport.9, 20 However, it is unclear from these guidelines what length of time would constitute a significant time savings. Further, our group has shown that only a subset of the physiologic and anatomic triage criteria are useful for HEMS triage, based on improved survival for HEMS transport.39 Finally, the current findings exhibit a survival benefit for HEMS when no time-saving advantage exists over GEMS transport. Undoubtedly there are patients that have time-sensitive injuries, and the time savings of HEMS transport will be critical to their outcomes. The next step, however, is to identify criteria that can be used at the scene of injury to distinguish patients most likely to benefit from the care delivered by HEMS providers irrespective of time savings over GEMS transport.
The current data also highlight the logistical considerations of HEMS transport within individual trauma systems. Stratifying by prehospital transport time resulted in comparing patients coming from different distances from the trauma center, with HEMS patients coming from further away due to the differences in transport speed. The goal of this analysis was to eliminate any time-saving advantage for HEMS transport and compared care for patients exposed to prehospital providers for the same length of time. Nevertheless, GIS network analysis did demonstrate some overlap of helicopter and ground ambulance coverage within the 6 to 30 minute transport time window for individual regions, and strong consideration should be given to HEMS transport for patients in these areas. This overlap may be significantly altered depending on regional highway structure, urbanicity, time of day, and weather. GIS analysis has been used in the past to examine appropriate HEMS transport and will be a powerful tool going forward to help optimize the role of HEMS within individual trauma systems.40, 41
This study has several limitations. First are those inherent to a retrospective design. Second are those outlined by American College of Surgeons Committee on Trauma for use of the NTDB.17 Although the NTDB data quality has improved substantially, high levels of missing data persist, particularly in prehospital variables. Multiple imputation was used to mitigate this, with less than 15% of any variable missing. This technique has been validated in the NTDB previously.42, 43 No significant differences were seen for outcomes in analysis using complete cases only. Subjects missing prehospital transport time were excluded, which represented 25% of the original population. We felt imputation of this variable would lead to significant bias, given the important role of transport time in the study; however this remains a limitation. The NTDB is not a population-based dataset and skewed towards large trauma centers.44 Further, the NTDB does not contain information regarding time from injury to emergency medical services activation. Patients declared dead in the field and not transported would also not be included. As noted, there is a potential time lag prior to HEMS activation that may also introduce a survival bias for patients that die in the field prior to HEMS activation. We excluded patients who were dead on arrival to mitigate this. Further, subsequent sensitivity analyses that excluded early deaths, as well as accounted for this time lag in HEMS activation demonstrated similar results, engendering confidence in the findings. Other outcomes such as health related quality of life are not available, but remain important to evaluate in severely injured trauma patients. Although we postulate that the survival benefit seen here is at least in part due to care delivered during transport, the NTDB does not specify the level of care available or actually delivered during prehospital transport. Further, other factors such as primary access to a trauma center may be in part responsible for the survival benefit rather than prehospital care alone. Thus, we cannot evaluate the underlying mechanism of the survival benefit seen for HEMS in the absence of a time-saving advantage over GEMS. Given the current findings, further study is necessary and warranted to delineate the mechanisms responsible for the observed survival advantage seen here. This would allow tailoring of prehospital trauma systems to match specific elements of prehospital care to patients most likely to benefit from them.
This study used propensity score matching to reduce the inevitable selection bias for allocation of transport mode. Despite this, only observed confounders can be utilized in the propensity score and unmeasured confounding may remain. Although the groups were well matched for prehospital characteristics in the propensity score, the HEMS group had a higher injury severity and was intubated and admitted to the ICU more often. This may represent a selection bias, with a lower threshold of intubation prior to transport for HEMS given the difficulties of airway management in the air. Additionally air medical patients may have been perceived more injured due to their mode of transport and admitted to the ICU. We adjusted for these factors in outcome models, and this would actually favor the GEMS group. Despite this, the HEMS group demonstrated improved outcomes with a defined transport time window.
The transport distances reported are crude estimates, dependent on a number of assumptions and averages. Although time and distance are correlated, the exact nature of the relationship is affected by many factors. The GIS analysis assumes straight line flight for HEMS to the trauma center from the scene of injury which may not occur in all cases. More sophisticated GIS analysis at the individual trauma system level is merited to explore the transport time and distance relationships. Finally, the dataset represents a heterogeneous population and requires careful application of the results to any individual trauma system.
CONCLUSION
When stratified by prehospital transport time, the survival benefit of HEMS transport in trauma is not uniform and is concentrated in a transport time window between 6 and 30 minutes. This survival benefit is present even in the absence of a time-saving advantage of HEMS over GEMS. This is the first study to evaluate transport mode across equal prehospital times, and these novel findings likely reflect the care delivered during HEMS transport, demonstrating a critical time window in which HEMS care and interventions have the ability to affect outcome. Further study is warranted of the interplay between time, distance, and HEMS provider resources to better understand which elements of HEMS care drive this benefit. Finally, work is needed to identify injured patients most likely to benefit from HEMS transport even in the absence of a time-saving advantage over GEMS.
Acknowledgments
Funding/Support: No funding or support was directly received to perform the current study. Dr. Brown receives support from an institutional T32 Ruth L. Kischstein National Research Service Award training grant (5T32GM008516-20) & L30GM112034 from the National Institutes of Health. Dr. Sperry receives support from a career development award (K23GM093032) from the National Institute of General Medical Sciences.
Committee on Trauma, American College of Surgeons. NTDB 2007–2012, Chicago, IL. The content reproduced from the NTDB remains the full and exclusive copyrighted property of the American College of Surgeons. The American College of Surgeons is not responsible for any claims arising from works based on the original data, text, tables, or figures.
ABBREVIATIONS
- HEMS
helicopter emergency medical services
- GEMS
ground emergency medical services
- PHTT
prehospital transport time
- NTDB
National Trauma Databank
- ED
emergency department
- SBP
systolic blood pressure
- HR
heart rate
- RR
respiratory rate
- GCS
Glasgow Coma Scale
- ISS
injury severity score
- TMPM
Trauma Mortality Prediction Model
- GIS
geographic information systems
- AOR
adjusted odds ratio
- 95%CI
95% confidence interval
- RTS
revised trauma score
Footnotes
Meeting Presentation: Data from this paper was presented at the 10th annual Academic Surgical Congress in Las Vegas, Nevada, February 2015.
Contributor Information
Joshua B. Brown, Email: brownjb@upmc.edu.
Mark L. Gestring, Email: mark_gestring@urmc.rochester.edu.
Francis X. Guyette, Email: guyefx@upmc.edu.
Matthew R. Rosengart, Email: rosengartmr@upmc.edu.
Nicole A. Stassen, Email: nicole_stassen@urmc.rochester.edu.
Raquel M. Forsythe, Email: forsytherm@upmc.edu.
Timothy R. Billiar, Email: billiartr@upmc.edu.
Andrew B. Peitzman, Email: peitzmanab@upmc.edu.
Jason L. Sperry, Email: sperryjl@upmc.edu.
References
- 1.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. The Journal of trauma. 2010;69:1030–4. doi: 10.1097/TA.0b013e3181f6f450. discussion 4–6. [DOI] [PubMed] [Google Scholar]
- 2.Galvagno SM, Jr, Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ, Jr, et al. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA : the journal of the American Medical Association. 2012;307:1602–10. doi: 10.1001/jama.2012.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart KE, Cowan LD, Thompson DM, Sacra JC, Albrecht R. Association of direct helicopter versus ground transport and in-hospital mortality in trauma patients: a propensity score analysis. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2011;18:1208–16. doi: 10.1111/j.1553-2712.2011.01207.x. [DOI] [PubMed] [Google Scholar]
- 4.Sullivent EE, Faul M, Wald MM. Reduced mortality in injured adults transported by helicopter emergency medical services. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2011;15:295–302. doi: 10.3109/10903127.2011.569849. [DOI] [PubMed] [Google Scholar]
- 5.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters improve survival in seriously injured patients requiring interfacility transfer for definitive care. The Journal of trauma. 2011;70:310–4. doi: 10.1097/TA.0b013e3182032b4f. [DOI] [PubMed] [Google Scholar]
- 6.Galvagno SM., Jr Comparative effectiveness of helicopter emergency medical services compared to ground emergency medical services. Critical care (London, England) 2013;17:169. doi: 10.1186/cc12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diaz MA, Hendey GW, Bivins HG. When Is the Helicopter Faster? A Comparison of Helicopter and Ground Ambulance Transport Times. The Journal of Trauma: Injury, Infection, and Critical Care. 2005;58:148–53. doi: 10.1097/01.ta.0000124264.43941.41. [DOI] [PubMed] [Google Scholar]
- 8.Rhinehart ZJ, Guyette FX, Sperry JL, Forsythe RM, Murdock A, Alarcon LH, et al. The association between air ambulance distribution and trauma mortality. Annals of surgery. 2013;257:1147–53. doi: 10.1097/SLA.0b013e31827ee6b0. [DOI] [PubMed] [Google Scholar]
- 9.Thomas SH, Brown KM, Oliver ZJ, Spaite DW, Lawner BJ, Sahni R, et al. An Evidence-based Guideline for the air medical transportation of prehospital trauma patients. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2014;18(Suppl 1):35–44. doi: 10.3109/10903127.2013.844872. [DOI] [PubMed] [Google Scholar]
- 10.Sampalis JS, Denis R, Lavoie A, Frechette P, Boukas S, Nikolis A, et al. Trauma Care Regionalization: A Process-Outcome Evaluation. J Trauma Acute Care Surg. 1999;46:565–81. doi: 10.1097/00005373-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Thomas SH, Harrison TH, Buras WR, Ahmed W, Cheema F, Wedel SK. Helicopter transport and blunt trauma mortality: a multicenter trial. The Journal of trauma. 2002;52:136–45. doi: 10.1097/00005373-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Annals of emergency medicine. 2004;44:439–50. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Davis DP, Peay J, Serrano JA, Buono C, Vilke GM, Sise MJ, et al. The impact of aeromedical response to patients with moderate to severe traumatic brain injury. Annals of emergency medicine. 2005;46:115–22. doi: 10.1016/j.annemergmed.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 14.Brown JB, Sperry JL, Fombona A, Billiar T, Peitzman AB, Guyette FX. Pre-Trauma Center Red Blood Cell Transfusion is Associated with Improved Early Outcomes in Air Medical Trauma Patients. Journal of the American College of Surgeons. 2015;220:797–808. doi: 10.1016/j.jamcollsurg.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nirula R, Maier R, Moore E, Sperry J, Gentilello L. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer’s effect on mortality. The Journal of trauma. 2010;69:595–9. doi: 10.1097/TA.0b013e3181ee6e32. discussion 9–601. [DOI] [PubMed] [Google Scholar]
- 16.Ryb GE, Dischinger P, Cooper C, Kufera JA. Does helicopter transport improve outcomes independently of emergency medical system time? J Trauma Acute Care Surg. 2013;74:149–54. doi: 10.1097/TA.0b013e31827890cc. discussion 54–6. [DOI] [PubMed] [Google Scholar]
- 17.American College of Surgeons. National Trauma Databank Research Data Set Admission Year 2012. Chicago, IL: American College of Surgeons; 2012. [Google Scholar]
- 18.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons; 1987. [Google Scholar]
- 19.Rubin DB. Estimating causal effects from large data sets using propensity scores. Annals of internal medicine. 1997;127:757–63. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 20.Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, et al. Guidelines for Field Triage of Injured Patients. MMWR. 2012;61:1–20. [PubMed] [Google Scholar]
- 21.Brown JB, Gestring ML, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, et al. Geographic Variation in Outcome Benefits of Helicopter Transport for Trauma in the United States. Annals of surgery. 2015 doi: 10.1097/SLA.0000000000001047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.United States Census Bureau. Census Regions and Divisions of the United States. 2010. [Google Scholar]
- 23.Yang D, JED . A unified approach to measuring the effect size between two groups using SAS®. 2012. [Google Scholar]
- 24.Glance LG, Osler TM, Mukamel DB, Meredith W, Wagner J, Dick AW. TMPM-ICD9: a trauma mortality prediction model based on ICD-9-CM codes. Annals of surgery. 2009;249:1032–9. doi: 10.1097/SLA.0b013e3181a38f28. [DOI] [PubMed] [Google Scholar]
- 25.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Statist Soc B. 1995;57:289–300. [Google Scholar]
- 26.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Statistics in medicine. 2009;28:3083–107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carr BG, Caplan JM, Pryor JP, Branas CC. A meta-analysis of prehospital care times for trauma. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2006;10:198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 28.United States Census Bureau. 2010 Census Urban and Rural Classification and Urban Area Criteria. 2010. [Google Scholar]
- 29.Carr B, Branas C TraumaMaps.org Trauma Center Maps. Copyright © 2006 Trustees of the University of Pennsylvania. 2006. University of Pennsylvania Cartographic Modeling Laboratory. [Google Scholar]
- 30.Andruszkow H, Lefering R, Frink M, Mommsen P, Zeckey C, Rahe K, et al. Survival benefit of helicopter emergency medical services compared to ground emergency medical services in traumatized patients. Critical care (London, England) 2013;17:R124. doi: 10.1186/cc12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Butler DP, Anwar I, Willett K. Is it the H or the EMS in HEMS that has an impact on trauma patient mortality? A systematic review of the evidence. Emergency medicine journal : EMJ. 2010;27:692–701. doi: 10.1136/emj.2009.087486. [DOI] [PubMed] [Google Scholar]
- 32.Roberts K, Blethyn K, Foreman M, Bleetman A. Influence of air ambulance doctors on on-scene times, clinical interventions, decision-making and independent paramedic practice. Emergency medicine journal : EMJ. 2009;26:128–34. doi: 10.1136/emj.2008.059899. [DOI] [PubMed] [Google Scholar]
- 33.Cocanour CS, Fischer RP, Ursic CM. Are scene flights for penetrating trauma justified? The Journal of trauma. 1997;43:83–6. doi: 10.1097/00005373-199707000-00019. discussion 6–8. [DOI] [PubMed] [Google Scholar]
- 34.Schiller WR, Knox R, Zinnecker H, Jeevanandam M, Sayre M, Burke J, et al. Effect of helicopter transport of trauma victims on survival in an urban trauma center. The Journal of trauma. 1988;28:1127–34. doi: 10.1097/00005373-198808000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Shatney CH, Homan SJ, Sherck JP, Ho CC. The utility of helicopter transport of trauma patients from the injury scene in an urban trauma system. The Journal of trauma. 2002;53:817–22. doi: 10.1097/00005373-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Baxt W, Moody P. The impact of a physician as part of the aeromedical prehospital team in patients with blunt trauma. JAMA : the journal of the American Medical Association. 1987;257:3246–50. [PubMed] [Google Scholar]
- 37.Doucet J, Bulger E, Sanddal N, Fallat M, Bromberg W, Gestring M, et al. Appropriate use of helicopter emergency medical services for transport of trauma patients: guidelines from the Emergency Medical System Subcommittee, Committee on Trauma, American College of Surgeons. J Trauma Acute Care Surg. 2013;75:734–41. doi: 10.1097/TA.0b013e3182a5389e. [DOI] [PubMed] [Google Scholar]
- 38.Ringburg AN, de Ronde G, Thomas SH, van Lieshout EM, Patka P, Schipper IB. Validity of helicopter emergency medical services dispatch criteria for traumatic injuries: a systematic review. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2009;13:28–36. doi: 10.1080/10903120802472012. [DOI] [PubMed] [Google Scholar]
- 39.Brown JB, Forsythe RM, Stassen NA, Gestring ML. The National Trauma Triage Protocol: can this tool predict which patients with trauma will benefit from helicopter transport? J Trauma Acute Care Surg. 2012;73:319–25. doi: 10.1097/TA.0b013e3182572bee. [DOI] [PubMed] [Google Scholar]
- 40.Lerner EB, Billittier AJ, Sikora J, RMM Use of a geographic information system to determing appropriate means of trauma patient transport. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1999;6:1127–33. doi: 10.1111/j.1553-2712.1999.tb00115.x. [DOI] [PubMed] [Google Scholar]
- 41.Widener MJ, Ginsberg Z, Schleith D, Floccare DJ, Hirshon JM, Galvagno S. Ground and Helicopter Emergency Medical Services Time Tradeoffs Assessed with Geographic Information. Aerosp Med Hum Perform. 2015;86:620–7. doi: 10.3357/AMHP.4173.2015. [DOI] [PubMed] [Google Scholar]
- 42.Haider AH, Saleem T, Leow JJ, Villegas CV, Kisat M, Schneider EB, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? Journal of the American College of Surgeons. 2012;214:756–68. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moore L, Hanley JA, Lavoie A, Turgeon A. Evaluating the validity of multiple imputation for missing physiological data in the national trauma data bank. Journal of emergencies, trauma, and shock. 2009;2:73–9. doi: 10.4103/0974-2700.44774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moore L, Hanley JA, Turgeon AF, Lavoie A, Emond M. A multiple imputation model for imputing missing physiologic data in the national trauma data bank. Journal of the American College of Surgeons. 2009;209:572–9. doi: 10.1016/j.jamcollsurg.2009.07.004. [DOI] [PubMed] [Google Scholar]