Abstract
With rates of obesity and diabetes rising worldwide, effective ways of managing weight are becoming more important. We present the case study of a middle-aged Caucasian-American woman (body mass index (BMI) 27.8, overweight category) who wanted to lose weight. The patient participated in a behaviour modification programme with a physician trained in lifestyle medicine as well as health and wellness coaching. After the 14-week programme, which included 9, 1 h long walking sessions with the clinician, the patient lost 11 Ibs (BMI 24.7, normal category). The programme included a combination of increasing physical activity, eating appropriate quantities of healthy foods, goal setting and a positive attitude. The patient has kept her BMI at or below 24.1 for over 2 years. This case demonstrates a novel approach to weight loss management—walking therapeutic sessions—and also outlines critical components of lifestyle medicine counselling that facilitate the process of sustainable weight loss and lasting change.
Case presentation
Clinical presentation
The patient was a 59-year-old Caucasian-American woman who was 5 feet 3 inches tall. Her primary concern was her recent weight gain of 15 lbs, which had begun when she started a new job, 7 months before treatment. When the patient registered for the intervention, she weighed 157 lbs (body mass index (BMI) 27.8), which classified her in the overweight, preobese category according to WHO standards.1
Fourteen years before treatment, the patient had been diagnosed with uterine fibroid disease. Eight years before treatment, the patient's general practitioner noted that she had dyslipidaemia; her total cholesterol level was 231 mg/dL and her low-density lipoprotein (LDL) level was 162 mg/dL. The patient did not provide her triglyceride level or her high-density lipoprotein (HDL) level. Eleven months before treatment, the patient's cholesterol level was 220 mg/dL and her LDL 151 mg/dL, her triglyceride level was 98 mg/dL and her HDL was 49 mg/dL. She had no other comorbid medical conditions. Her father and grandfather had both died from stroke, at ages 81 and 61 years, respectively, but her mother had no relevant medical conditions. As a family they had lived active lifestyles and eaten well-balanced diets.
As an adult, she biked or walked to her previous jobs. She had weighed 132 lbs (BMI=23.4) when she married, 7 years before treatment. She gained weight for the next few months after her marriage until she reached 152 lbs (BMI=26.9). In the past, she focused only on diet changes to lose weight; she limited her overall food intake and eliminated desserts. Nine months before treatment, she weighed 142 lbs (BMI=25.2). However, she was unable to sustain this weight loss when she started a new job as an accountant.
The patient's lifestyle, particularly her diet and exercise habits, shifted when she started her new job. Instead of walking or biking to work, she drove and remained sedentary during the day. Also, her diet changed as she began eating in the all-you-can-eat cafeteria at work. Her lunch consisted of a hot meal, occasionally with small side salad. Routinely, she ate a couple of freshly baked cookies at lunch and one or two more later in the day. For snacks, the patient consumed plain carbohydrates, such as a box of crackers, or plain protein in the form of large quantities of cheese. The patient's husband cooked dinner and served large portions, including ice cream for dessert. The patient reported difficulty restricting her food intake at meals.
Using the Transtheoretical Model of Change, the clinician assessed that the patient had been in the contemplation stage of change for months prior to the initial contact with the clinician; although the patient was dissatisfied with her current weight, she was not attempting to counteract the weight gain by changing her diet or exercise habits. However, she was eager to try a new approach to lose weight and longed for sustainable change.
The clinician emailed the patient 2 weeks before treatment, inviting her to ponder questions about her current health and goals. The clinician helped the patient craft a vision for the future, label obstacles, and determine which of the patient's character strengths would play a key role in the change process. The patient began to use some of her past diet strategies and, after the email, she moved from the contemplation to preparation stage of change. At the time of the email, the patient's self-reported weight was 152 lbs (BMI=26.9).
Treatment
This case report is the first documentation of a novel lifestyle medicine intervention, PAVING the Path to Wellness, which combines a variety of evidence-based lifestyle medicine principles and health-coaching techniques to help patients lose weight and reach their optimal state of well-being. The clinician (the first author) developed this programme based on her many years of counselling and coaching patients to adopt healthy habits. The programme adheres to the core competencies in lifestyle medicine,2 and provides recommendations based on the latest WHO guidelines for exercise and healthy eating.3 With the PAVING the Path to Wellness programme, the clinician guided the patient through changing the following: P—increasing her level of physical activity; A—shifting her attitude to a growth mindset, which is the belief that skills and abilities can be developed through hard work and perseverance;4 V—increasing the variety in her food choices and activities; I—investigating which changes are effective or ineffective; N—eating nutritious, unprocessed, whole foods; and G—setting SMART goals (specific, measureable, action-oriented, realistic and time-sensitive goals).
The clinician used a collaborative coach approach, in which she and the patient worked together to cocreate enjoyable, individualised treatment.5 This methodology included evidence-based theories and techniques including motivational interviewing,6 appreciative inquiry,7 a growth mindset,4 self-determination theory,8 positive psychology9–12 and goal setting theory.13 In motivational interviewing, the clinician asks open-ended questions, affirms the patient's positive statements and actions, reflects on what the patient has said and makes summary statements after listening to the patient.6 In this way, the clinician guides patients to talk about the benefits of changing behaviour and encourages them to find an intrinsic motivation for achieving their goals. According to the self-determination theory, people are more committed to accomplishing a goal when they have the autonomy to decide how to approach their behaviour change.8
The clinician used appreciative inquiry and positive psychology to build self-efficacy by posing questions that touch on the patient's strengths. Positive psychology examines those strengths of a person that enable them to thrive.9–12 The patient in this case identified several strengths, including being determined, having a sense of humour, having a supportive husband and enjoying using numbers to track progress, which she did by recording her weight and her level of exercise daily. Appreciative inquiry draws from positive psychology; it is a method of asking about the successes and inspiring aspects of life to empower patients to overcome challenges.7 Simply starting a session with an appreciative inquiry strategy such as, “Tell me about what went well this week”, sets the tone for a productive meeting, ripe for brainstorming and tackling difficult issues.
When the clinician wanted to provide the patient with a piece of information to help her achieve her goal, the clinician followed an elicit-provide-elicit pattern, as taught in motivational interviewing.6 14 In this method, the clinician first asked the patient's permission to ensure that the patient was interested in the topic. Once the patient agreed, the clinician shared the guidelines and rationale behind diet or exercise recommendations. Finally, the clinician asked the patient if she had any clarifying questions and then asked her to summarise the information to ensure that the patient grasped the concepts enough to apply them in her own life.
During the walking sessions, the clinician helped the patient to reflect on her previous actions, current thoughts and plans for the week. The patient's overall goal was to restore her sense of a ‘healthy self’ to prevent health problems her friends and family members experienced. Specifically, she aimed to accumulate 10 000 steps each day and lose 25 lbs in 6 months. The clinician and patient also discussed potential obstacles, such as annual service trip, on which the patient had gained 3–5 lbs in past years. They then evaluated potential strategies for continuing healthy habits during challenging periods. Drawing from Rosamund and Ben Zander's work in ‘The art of possibility’, the patient imagined many possibilities for ways forward, which helped her stay optimistic throughout the change process.15
The clinician encouraged the patient to assess her progress and to make adjustments as necessary using a growth mindset. Following Dweck's4 work on mindsets, the clinician stressed the importance of failure and the power of setbacks to help the patient identify a more effective solution. In a fixed mindset, patients believe that because they are overweight and were not able to lose weight during previous dieting attempts, they are destined to be obese. With the growth mindset, patients reflect on their past weight loss attempts, strive to understand what went wrong and recognise the lessons in those mistakes. Slip-ups are opportunities to learn in the growth mindset but are validation of inadequacy in the fixed mindset. Adopting the growth mindset allows patients to persevere with new strategies to lead a healthy life and to learn from each attempt, instead of letting failures define them.
Each session ended with goal setting using the SMART framework. For example, one of the patient's first goals was to walk with her husband after dinner twice that weekend. The second week, she added two more walking sessions during the week and obtained the Mayo Clinic Diet from the local library that weekend.16 These goals were relatively easy for the patient to accomplish, and for the patient and clinician to evaluate. SMART goals set the patient up for success. Most importantly, the patient selected the goals and felt confident in completing them.
The clinician used these methods to create an exercise and nutrition plan that adhered to WHO guidelines on exercise and diet, and that was tailored to the patient's preferences.17 18 Presently, the WHO recommends that people accumulate at least 150 min of moderate intensity aerobic physical activity each week, or equivalent, which is the rate at which people experience the major health benefits from exercise.17 One strategy of accomplishing this is walking 10 000 steps per day because it has been shown that people who do so are more likely to meet these exercise guidelines.19
The clinician guided the patient to consider the quality and quantity of food as well as how quickly she ate. Eating pace was important because it takes 15 to 20 min for a person to feel satiety.20 In addition, if the patient had an hour-long lunch break, eating in 30 min gave her time to briefly exercise, such as by walking with colleagues. The clinician helped the patient create a balanced diet using the evidence-based, nutritional guidelines from ChooseMyPlate.Gov, the Healthy Eating Plate and from the WHO.18 21 22 The WHO recommends that people increase consumption of foods high in vitamins, fibre, phytonutrients and antioxidants, such as fruits and vegetables, legumes, whole grains and nuts, while at the same time limiting energy intake from total fats, shifting away from saturated fats, shifting toward unsaturated fats and eliminating trans fats from the diet, as well as limiting intake of free sugars and salt.3 18 The clinician also emphasised the importance of consuming snacks with complex carbohydrates and protein for longer satiation.23 Following the patient's inquisition regarding specific diets, the clinician provided her with information about the Mediterranean diet,24 plant-based diet25 and the Mayo Clinic Diet.16 Ultimately, the patient and clinician cocreated a healthy diet plan that included healthy food that the patient enjoyed. Regardless of the patient's specific nutrition or exercise choices, the programme utilised the concept of variety. This ensured that the patient did not grow tired of her favourite healthy foods or exercise routines.
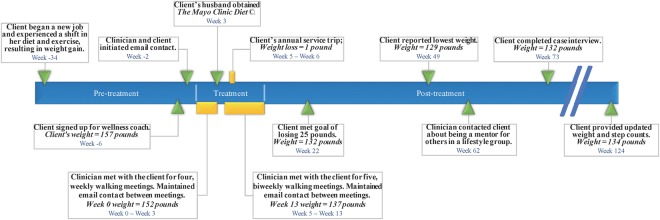
The clinical intervention consisted of nine, 1 h walking meetings over 14 weeks (weeks 0–13; figure 1). The clinician and patient met weekly four times and then bimonthly five times. They walked approximately three miles per meeting. The clinician emailed the patient between sessions once or twice per week to keep the patient accountable for her goals. In these emails, the clinician asked the patient about either a specific goal or sent a news article related to the week's goals. For a year following the 14-week treatment, the clinician continued informal check-ins every 6–8 weeks to share health information and to create an opportunity for guidance or encouragement if the patient desired. They did not have any follow-up lifestyle counselling walking sessions after the lifestyle intervention was over.
Figure 1.
Timeline.
Outcome and follow-up
Physical and clinical changes
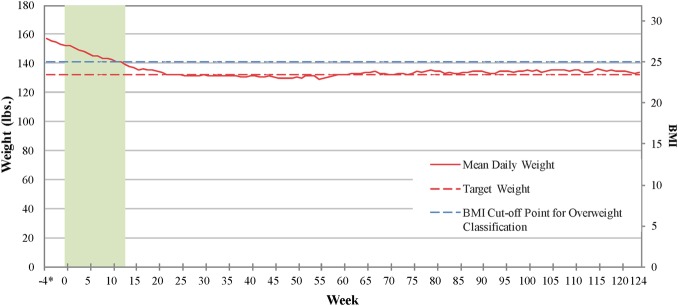
The patient reported losing a total of 28 lbs from the point of initial contact with the patient 6 weeks before treatment to her lowest weight, week 48 (figure 2). She lost 5 lbs in the month between the clinician's first email and the first walking meeting. The patient speculated that enrolling in the treatment and the initial emails from the clinician made her begin to shift towards a healthier mindset. For example, the patient stated that she ate fewer desserts because this was how she successfully lost weight in the past. During the clinical treatment, the patient lost 11 lbs, falling from 152.0 to 140.8 lbs (BMI decreased from 26.9, which is in the overweight range, to 24.9, which is in the normal range).1 Having embraced her new lifestyle, the patient continued to lose weight after the treatment. At week 22, she reached her weight goal of 132 lbs (BMI=23.4) and at week 48, she reached her lowest weight of 129 lbs (BMI=22.8). Since then (from week 49–124), she has maintained her weight, averaging 134 lbs (BMI=23.7).
Figure 2.
Patient self-reported mean daily weight. *The first weight measurement was taken 4 weeks before the start of the intervention. BMI, body mass index.
Although cholesterol was not a focus of the intervention, the patient's cholesterol and LDL levels decreased as she decreased saturated fat intake, increased fruit and vegetable intake, and increased physical activity. The patient provided the clinician with her cholesterol levels, which were measured by her doctor. At week 118, her total cholesterol level was 197 mg/dL, her LDL level was 132 mg/dL, her triglyceride level was 65 mg/dL, and her HDL level was 52 mg/dL. Compared with her cholesterol level 11 months before treatment, her total cholesterol level had decreased by 23, her LDL level decreased by 19, her triglyceride level decreased by 33 and her HDL level had increased by 3.
Behavioural changes
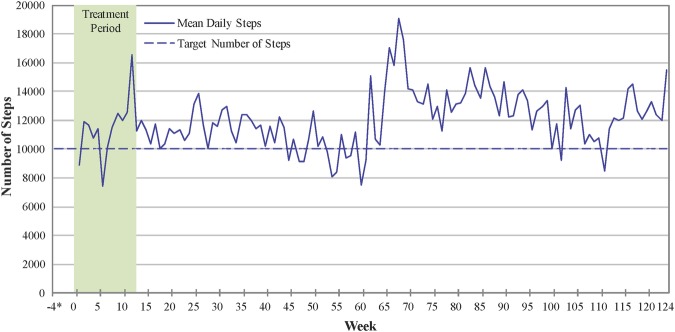
Through PAVING the Path to Wellness, the patient gradually increased her exercise level from being sedentary to accumulating the recommended 2.5 h of moderate intensity physical activity each week. She wore a pedometer and, after the intervention, a Fitbit to monitor her progress. Since the start of treatment, the patient walked an average of 12 061 steps per day, which she estimated was about 5 miles, over 60–80 min (figure 3). She reported that she accumulated about 6000 steps on a long walk and the other 4000 steps throughout the day. The patient stated that given her competitive nature, on days when she did not walk far, she would run or jump in place to increase her step count.
Figure 3.
Patient self-reported mean daily number of steps.
The patient's eating practices shifted to include healthier foods, such as a variety of vegetables and fruits, to monitor and alter snacks, and to decrease the portion size of foods. She found it helpful to share the information from the Mayo Clinic Diet with her husband, who used it to cook dinner. She reported following the clinician's recommendation to eat foods that she loved with high nutritional value, such as grilled fish, vegetables and fruits. Focusing on whole food, a plant-based dietary pattern and avoiding processed foods, the patient decided to avoid processed cheese. Since she loved cheese, she decided to only consume high-quality cheese on rare occasions and refrained from eating pizza on the weekend. Also, she decreased her portion size at dinner by buying smaller bowls and serving herself, instead of allowing her husband to fill her plate. Additionally, she ate fruit for dessert rather than ice cream or cookies. For lunch, she ate salads with chicken or fish as a source of protein.
The patient altered her snacks to include portion-controlled foods with higher nutritional value. For example, she kept a prepackaged, portion-controlled bag of “emergency almonds” in her purse for a quick snack when she felt hungry. She also found carrots and hummus to be a satisfying snack. The patient did not want to forgo foods she loved, so she ate healthier options, such as brown rice crackers with almond butter. Similarly, rather than eliminating chocolate from her diet, the patient eventually kept a dark chocolate bar in her office drawer to replace cookies for when she had a chocolate craving. However, she reported that she resisted chocolate cravings, thinking that she would rather save the chocolate bar for later.
When reflecting on the intervention, the patient was most excited and surprised about her 1 Ib weight loss on her annual service trip. She accomplished this by following the plan she had brainstormed with the clinician: she brought packets of oatmeal with her for breakfast, used bikes for transportation to maintain her physical activity, and ate at predetermined local restaurants with healthy options that fit her current eating plan and pattern. She noted that the specific, easily implementable strategies enabled the weight loss in her challenging vacation situation.
Psychosocial changes
The patient's biggest shift was her attitude; she restored her image as an active, healthy person. She now viewed this lifestyle as something to maintain her whole life in order to feel better, not just as a diet to lose weight for a certain occasion. She no longer saw free food as being free; it was not guilt free. Moreover, she did not view the food as the focus of a party—she hydrated and ate beforehand so she was not tempted by unhealthy foods, and instead ate a small amount of healthier foods. The patient's mindset around taking walks in the middle of her workday also shifted from feeling guilty, as if she were shirking on work responsibilities, to viewing these walks as a tool to help her focus and increase her productivity.
The patient became a change agent for family, friends and colleagues, who began walking with her at lunch and other times. They asked her how they too could implement lifestyle changes because they saw her as someone who exercises and eats healthily. Her perception of herself and the perception that others had of her morphed into one of a healthy person in body and mind. Also, she noted that the attention and affirmation of her successful behaviour change motivated her even more.
Without direct contact with the clinician, the patient's husband also implemented many of the lifestyle changes that the patient had undergone. His weight decreased from 220 to 200 lbs (BMI decreased from 28.2 to 25.7). He also began walking to work, which was a mile away from their house. Soon the couple also became known within their neighbourhood as ‘the walkers’. This exemplifies the importance of social connection, and the influence of friends and family for patients to sustain lifestyle changes.
Follow-up
During the case interview, the patient noted that the clinician's follow-up emails post-treatment served as a reminder to maintain her new lifestyle. The patient reported that she had been slipping back into old habits of a more sedentary life in weeks 57–61. She averaged only 7000 steps per day, some days with only 3000 steps. Coincidentally, in week 62, the clinician emailed her about the possibility of the patient acting as a mentor for a wellness group of four colleagues. Although the patient was unable to be a mentor for the group, she stated that this email reminded her to reinstate her active lifestyle.
The clinician did not have any subsequent contact with the patient, other than to gather information for this case study. The patient has maintained her lifestyle changes for 2.5 years, which she attributes to the fact that the changes were small but important and they became a part of her regular routine.
Global health problem list
Sedentary occupations and motor-vehicle transportation decrease routine and incidental opportunities to exercise and burn calories. This is compounded by reduced physical activity for recreation.
People living in industrialised countries have an increased likelihood of working at sedentary occupations and using modes of transportation rather than walking.
An unhealthy diet, high in energy-dense, nutrition-poor foods (high fat, sugar and salt) and low in whole grains, fibre, and fruits and vegetables, contributes to weight gain.
Family lifestyle can increase obesity due to social pressure. The patient's husband cooked unhealthy food and served her large portions.
Obesogenic environments, such as having readily available high caloric food within a workplace, promote weight gain.
Metabolic factors, including dyslipidaemia, increase the risk of cardiovascular disease.
As people age, hormonal changes and decreased muscle mass decrease metabolism, increasing the importance of controlling food intake and being physically active.
Global health problem analysis
Modifiable lifestyle factors account for the leading causes of death worldwide.26 The four most prevalent non-communicable diseases—cardiovascular diseases, cancers, chronic respiratory diseases and diabetes—share four common risk factors: use of tobacco, unhealthy diet and physical inactivity.27 Dietary risk factors and physical inactivity account for 10% of global burden of disease, and physical inactivity alone increases risk of all-causes of mortality by 20–30%.17 28 Patients can decrease their risk of cardiovascular and other diseases by practicing four healthy habits: refraining from smoking, exercising regularly, eating five or more fruits and vegetables daily, and drinking alcohol in moderation.29 In a longitudinal study on lifestyle habits of Swedish men, researchers found myocardial infarction events could be reduced by 79% if the men followed a healthy diet, consumed only moderate amounts of alcohol, did not smoke, were physically active and did not have abdominal adiposity.30 Nonetheless, in 2010, 23% of adults globally were insufficiently physically active, with women and the elderly having higher rates of physical inactivity relative to men and younger people.31 According to the Centers for Disease Control and Prevention, in the USA, 38% of adults reported eating fruit less than once a day and 28% of adults reported eating vegetables less than once a day.32 From 1980 to 2008, the global prevalence of obesity has nearly doubled.33
Helping patients lose weight and maintain the weight loss is a critical goal for healthcare providers of the 21st century. Weight loss can be affected by factors including genetics, endocrine function (eg, thyroid function), metabolic rate, muscle mass, sleep, non-exercise activity thermogenesis (how much a person naturally fidgets or moves around), stress levels, the presence of comorbid disease such as obstructive sleep apnoea, amount and type of food, and amount of exercise.34 Weight regulation differs from person to person, even in those with a similar genetic profile.35
It is important to note that the patient in this case had no endocrine issues and no comorbidities that could have complicated the weight loss process. In addition, she readily responded to the lifestyle changes. Despite research suggesting that eating out for lunch can cause weight gain in postmenopausal women,36 the patient was able to lose weight while eating lunch in the cafeteria by modifying what she ate. Other people may require a more extensive work-up for the weight loss, may need medication or may even be candidates for a weight loss procedure. Conversely, some people are able to alter their diet and exercise habits without a lifestyle specialist, by using books and online resources for portion control and dietary information. Thus, it is important to apply an individualised approach to weight regulation to accommodate individual variability.
Policymakers play a key role in decreasing the obesity epidemic by creating programmes and regulations that aim to reverse obesogenic environments. An obesogenic environment is one that encourages sedentary behaviour and the intake of high-calorie, low-nutrient foods.37 A systems approach that addresses the physical environments is needed.38 This involves a number of initiatives including food labelling, city urban planning and employer policies. To decrease sedentary time at work, it is recommended that employees spend at least 2 h standing or performing light activity for 2 h in the workday with the goal of increasing this to 4 h over time.39 This is especially important in high-income countries, which have more than double the prevalence of physical inactivity compared with low-income countries.40
To date, there is no exemplar public health policy to combat obesity and for this reason effective individual approaches are needed.41 42 According to a WHO report, it is important to adopt programmes appropriate to the local context and culture, to use existing social structures to reduce barriers to implementation, to involve local participants in both, the planning and implementation stages, and to evaluate the sustainability of the programme.43 Health promotion advice and efforts are important, but ultimately the individual must make the choice to select the healthy food option and to be more physically active.44 Patients need to have the knowledge about healthy habits, as well as skills, tools and positive attitudes to be able to successfully adopt health-promoting behaviours.
There is a need for behaviour change counselling to prevent and treat lifestyle-related health problems such as heart disease, diabetes, hypertension, stroke and obesity. A review of health and wellness coaching concluded that this form of collaborative counselling can be an effective way to manage weight.45 Other randomised controlled studies in health coaching examining health outcomes have demonstrated that this approach is effective and shows great promise for lowering cholesterol,46 decreasing glycated haemoglobin,47 controlling cancer pain48 and even reducing hospital readmission in paediatric patients with asthma.49 This method of counselling is patient-centred, as the clinician and patient are cocreators of the plans and goals for lifestyle change. In 2002, a landmark study by the Diabetes Prevention Program published in the New England Journal of Medicine found that, in a prediabetic population, a lifestyle intervention was more effective at reducing the incidence of diabetes than a drug for glucose control.50
Similar to this landmark study, the lifestyle medicine clinician focused on nutrition, physical activity and behaviour change techniques to empower the patient to adopt healthy habits that last. Unlike many lifestyle interventions, the clinician in this case study conducted the counselling sessions during walking meetings. The merit of walking meetings is supported by a recent study by Oppezzo and Schwartz. They found that walking increased participants’ creativity in exploring potential solutions.51 In addition, there are several studies that report on the fact that a physician's personal exercise habits affect the recommendations they give to their patients.52 Thus, these walking meetings were excellent opportunities to brainstorm creative solutions around obstacles, as well as to demonstrate the positive effects of physical activity. Making physical activity part of a daily routine is a critical part of a healthy lifestyle.38
The main limitation of this case report is that it used a retrospective, observational design. The clinician did not take direct measurements of the patient's heart rate, blood pressure, or waist circumference to track the patient's progress. These physiological measurements would have increased the rigour of the clinical data. Future research is needed to determine the efficacy of these types of lifestyle intervention with walking meetings in a randomised control design.
Additionally, the case study design was not sensitive enough to determine the role of self-monitoring technology, such as the pedometer, in producing lifestyle changes. Self-monitoring behaviours and changes, such as daily steps and weight, as well as keeping food journals, have been shown to be effective behaviour change strategies.36 53 54 This patient gravitated to monitoring her daily steps and weight, but not food intake. Although the clinician did not regularly recommend routine weigh-ins to her patients (there were mixed reports and mixed feelings among researchers and clinicians about this practise), this particular patient chose this strategy herself and was happy with it. A review on factors associated with weight loss maintenance describes that, although self-monitoring behaviours can play a key role in maintaining weight loss, a person's attitudes and motivations are equally as important.55 This suggests that only self-monitoring her weight and steps would not have been enough to produce sustained lifestyle changes. Recording the difference between her motivation, attitudes and beliefs, before and after the intervention, would have added to the value of this case study and should be included in future research. Future studies should examine the use of wearable health technologies in similar behaviour change programmes.
Finally, the patient did not have financial constraints to limit purchasing healthier foods and her job allowed her to take exercise breaks throughout the day—two factors that, if not present, can decrease the success of weight loss interventions.56 However, walking is free and can be added into a person's daily routine with a few minor changes, such as taking a short walk during lunch. In addition, frozen vegetables are available throughout the year in supermarkets in low-socioeconomic areas and are a healthy economical choice. Making meals at home on a budget can be less-expensive than eating out, but this routine takes careful planning and preparation. However, the time and energy is worth it, if the outcome is a healthy weight and reduced risk for disease. This case study reinforces the findings that lifestyle changes, including walking regularly and maintaining a portion-controlled, low-calorie diet, are an effective way to maintain long-term weight loss.57
The PAVING the Path to Wellness lifestyle intervention offers recommendations tailored to a patient's goals and circumstances. Although this programme was designed to create enduring weight loss, some patients may desire more rapid weight loss without a long-term focus. For these patients, the clinician can tailor their recommendations to include both a more rigorous exercise routine and an increased focus on decreasing food portions, and avoiding eating processed, hyperpalatable foods. Additionally, the programme can be delivered by any healthcare professional (nurse, nurse practitioner, physician's assistant) with the appropriate lifestyle counselling training. If a physician does not have the time to offer this lifestyle medicine programme or to train in the motivational interviewing or health coaching techniques, then someone can be hired to fill this role. For example, health coaches can be used to help patients adopt healthy lifestyles.58
In this case, the patient continued to lose weight after the end of the treatment period and maintained the weight loss for >2 years after the treatment ended. These sustained improvements strengthen the literature on wellness coaching and lifestyle medicine interventions because few prior studies included such a long follow-up measurement.45 This case study demonstrates the benefits of a lifestyle intervention using walking meetings and coaching techniques to increase a patient's engagement in her own behaviour change, and ultimately to increase her level of exercise and healthy nutritional intake leading to lasting weight loss.
Patient's perspective.
The walking meeting was a revelation and served as a (good) slap upside the head. I have had discussions both trivial and profound while walking or bicycling with friends, but had never had (or even heard proposed) a walking meeting or appointment. It's a brilliant idea that created time out of thin air by combining the appointment to which I had already committed with the exercise I wanted but didn't think I had time for. It demonstrated the clinician's commitment to exercise, allowed her to directly observe my ability to undertake an exercise programme of moderate intensity, provided me with a sense of routes I could walk, close to work, and, most importantly, gave me ‘permission’ to take the time during the workday to walk, clear my head and raise my energy levels. I am more than a bit of an intellectual snob, so was immediately drawn to the fact that my ‘lifestyle coach’ was also a physician, not a self-promoter peddling the latest diet fad. It was critical that early on in the process, she debunked the widespread belief that you simply can't lose significant weight in your 50s or 60s, validating my desire to get back to ‘wedding weight’—a 25 lbs drop—as a reasonable goal. I learned from the clinician's website that her personal motivation sprang from a family history of stroke, which spoke to my own history and anxieties. And I particularly liked her focus on wellness and feeling good, rather than simply on weight loss (which, while critical to health, I tend to think of as more a matter of ‘looking good’ and therefore more vanity than priority).
I am also highly competitive and a numbers person. Measurable goals, for weight loss as well as for daily steps, gave me a variety of success points to reach for. I might not always eat (or not eat) what I should, but I could still hit that 10 000 step mark—even if it meant jogging in place while brushing my teeth—to end the day with a sense of accomplishment. As I look back on the experience, I realise that, while I think of myself as a content, data-driven person, the success of this programme was all in the ‘packaging’, the coach and the method. I already knew I needed to exercise more, eat less and make better food selections. This approach gave me the tools, the time and the confidence to make it stick. Feeling better is profoundly more motivating than a fleeting desire to fit into those old jeans, and my “new” lifestyle is much more in sync with my self-image than the sedentary, frumpy overweight person I had become. Friends and acquaintances now refer to my husband and me as the ‘walkers’, and colleagues (as well as my inner voice) repeat my clinician's words, ‘No, no, no, no, no’, when I am tempted by those fabulous chocolate chip cookies.
Learning points.
Walking meetings allow for patient and healthcare provider to enjoy physical activity as well as foster an environment for increased creativity.
Collaborating and negotiating with a patient rather than dictating to the patient what he or she ‘must’ do is an effective form of behaviour change counselling, and is more enjoyable for patient and provider.
Eating nutritious food daily and engaging in regular exercise are important behaviours to adopt for health and for weight loss.
Changes in diet and exercise are more sustainable when combined with a growth mindset and a strengths-based approach.
Individual approaches to weight loss complement public health and global health initiatives, to encourage individuals to shift their diet and exercise habits.
Footnotes
Twitter: Follow Margaret Crane at @margaret_crane1
Contributors: EPF saw the patient, outlined the manuscript and wrote a rough draft. MEC interviewed the patient, performed the literature search, created figures and graphs, and contributed original writing to the original rough draft. Both the authors proofed the final manuscript and agreed it was ready for submission.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.World Health Organization. Obesity: preventing and managing the global epidemic. 2000. http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ [PubMed]
- 2.Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA 2010;304:202–3. 10.1001/jama.2010.903 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Global strategy on diet, physical activity and health. 2004. http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf
- 4.Dweck CS. Mindset: the new psychology of success. New York: Random House, 2006. [Google Scholar]
- 5.Frates EP, Moore MA, Lopez CN et al. Coaching for behavior change in physiatry. Am J Phys Med Rehabil 2011;90:1074–82. 10.1097/PHM.0b013e31822dea9a [DOI] [PubMed] [Google Scholar]
- 6.Miller WR, Rollnick S. Motivational interviewing. New York: Guilford Press, 2012. [Google Scholar]
- 7.Watkins JM, Cooperrider D. Appreciative inquiry: a transformative paradigm. OD Practitioner 2000;32:6–12. [Google Scholar]
- 8.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68–78. 10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- 9.Duckworth AL, Steen TA, Seligman MEP. Positive psychology in clinical practice. Annu Rev Clin Psychol 2005;1:629–51. 10.1146/annurev.clinpsy.1.102803.144154 [DOI] [PubMed] [Google Scholar]
- 10.Seligman MEP. Authentic happiness. New York: Free Press, 2002. [Google Scholar]
- 11.Frederickson BL. Love 2.0. New York: Plume, 2013. [Google Scholar]
- 12.Csikszentmihalyi M. Flow. New York: Harper Perennial, 1990. [Google Scholar]
- 13.Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation: a 35-year odyssey. Am Psychol 2002;57:705–17. 10.1037/0003-066X.57.9.705 [DOI] [PubMed] [Google Scholar]
- 14.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: conceptual issues and evidence review. J Am Diet Assoc 2006;106:2024–33. 10.1016/j.jada.2006.09.015 [DOI] [PubMed] [Google Scholar]
- 15.Zander R, Zander B. The art of possibility. New York: Penguin Press, 2000. [Google Scholar]
- 16.The Mayo Clinic Staff. The Mayo Clinic Diet: eat well. Enjoy life. Lose weight. Intercourse: Good Books, 2013. [Google Scholar]
- 17.World Health Organization. Global recommendations on physical activity for health. 2010. http://apps.who.int/iris/bitstream/10665/44399/1/9789241599979_eng.pdf [PubMed]
- 18.World Health Organization, Food and Agriculture Organization. Diet, nutrition and the prevention of chronic diseases 2003; Report No. 916.
- 19.Kurti AN, Dallery J. Internet-based contingency management increases walking in sedentary adults. J Appl Behav Anal 2013;46:568–81. 10.1002/jaba.58 [DOI] [PubMed] [Google Scholar]
- 20.Rolls ET, Rolls BJ, Rowe EA. Sensory-specific and motivation-specific satiety for the sight and taste of food and water in man. Physiol Behav 1983;30:185–92. 10.1016/0031-9384(83)90003-3 [DOI] [PubMed] [Google Scholar]
- 21.United States Department of Agriculture. Choose MyPlate 2014. http://www.choosemyplate.gov/ (accessed 9 Sep 2015).
- 22.The Healthy Eating Plate. The Harvard School of Public Health. http://www.hsph.harvard.edu/nutritionsource/pyramid-full-story/(accessed 19 Sep 2015).
- 23.Rolls BJ, Hetherington M, Burley VJ. The specificity of satiety: the influence of foods of different macronutrient content on the development of satiety. Physiol Behav 1988;43:145–53. 10.1016/0031-9384(88)90230-2 [DOI] [PubMed] [Google Scholar]
- 24.Willett WC, Sacks F, Trichopoulou A et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 1995;61(Suppl):1402S–6S. [DOI] [PubMed] [Google Scholar]
- 25.Fotsis T, Pepper M, Adlercreutz H et al. Genistein, a dietary ingested isoflavonoid, inhibits cell proliferation and in vitro angiogenesis. J Nutr 1995;125:790S–7S. [DOI] [PubMed] [Google Scholar]
- 26.Forouzanfar MH, Alexander L, Anderson HR et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287–323. 10.1016/S0140-6736(15)00128-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013–2020 2013. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf
- 28.Lim SS, Vos T, Flaxman AD et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matheson EM, King DE, Everett CJ. Healthy lifestyle habits and mortality in overweight and obese individuals. J Am Board Fam Med 2012;25:9–15. 10.3122/jabfm.2012.01.110164 [DOI] [PubMed] [Google Scholar]
- 30.Åkesson A, Larsson SC, Discacciati A et al. Low-risk diet and lifestyle habits in the primary prevention of myocardial infarction in men: a population-based prospective cohort study. J Am Coll Cardiol 2014;64:1299–306. 10.1016/j.jacc.2014.06.1190 [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization. Global status report on noncommunicable diseases 2014. 2014. http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf
- 32.Centers for Disease Control and Prevention. State indicator report on fruits and vegetables. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, 2013. [Google Scholar]
- 33.Ng M, Fleming T, Robinson M et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ 1997;315:477–80. 10.1136/bmj.315.7106.477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greenway FL. Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes 2015;39:1188–96. 10.1038/ijo.2015.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kong A, Beresford SAA, Alfano CM et al. Self-monitoring and eating-related behaviors are associated with 12-month weight loss in postmenopausal overweight-to-obese women. J Acad Nutr Diet 2012;112:1428–35. 10.1016/j.jand.2012.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lake A, Townshend T. Obesogenic environments: exploring the built and food environments. J R Soc Promot Health 2006;126:262–7. 10.1177/1466424006070487 [DOI] [PubMed] [Google Scholar]
- 38.Kohl HW, Craig CL, Lambert EV et al. The pandemic of physical inactivity: global action for public health. Lancet 2012;380:294–305. 10.1016/S0140-6736(12)60898-8 [DOI] [PubMed] [Google Scholar]
- 39.Buckley JP, Hedge A, Yates T et al. The sedentary office: an expert statement on the growing case for change towards better health and productivity. Br J Sports Med 2015;49:1357–62. 10.1136/bjsports-2015-094618 [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization. Global status report on noncommunicable diseases 2010. 2010. http://www.who.int/nmh/publications/ncd_report_full_en.pdf
- 41.Swinburn BA, Sacks G, Hall KD et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet 2011;378:804–14. 10.1016/S0140-6736(11)60813-1 [DOI] [PubMed] [Google Scholar]
- 42.Nestle M, Jacobson MF. Halting the obesity epidemic: a public health policy approach. Public Health Rep 2000;115:12–24. 10.1093/phr/115.1.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.World Health Organization. Interventions on diet and physical activity: what works: summary report. 2009. http://www.who.int/dietphysicalactivity/methods-09.pdf [PubMed]
- 44.Chan RS, Woo J. Prevention of overweight and obesity: how effective is the current public health approach. Int J Environ Res Public Health 2010;7:765–83. 10.3390/ijerph7030765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Olsen JM, Nesbitt BJ. Health coaching to improve healthy lifestyle behaviors: an integrative review. Am J Health Promot 2010;25:e1–12. 10.4278/ajhp.090313-LIT-101 [DOI] [PubMed] [Google Scholar]
- 46.Vale MJ, Jelinek MV, Best JD et al. Coaching patients On Achieving Cardiovascular Health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med 2003;163:2775–83. 10.1001/archinte.163.22.2775 [DOI] [PubMed] [Google Scholar]
- 47.Wolever RQ, Simmons LA, Sforzo GA et al. A systematic review of the literature on health and wellness coaching: defining a key behavioral intervention in healthcare. Global Adv Health Med 2013;2:38–57. 10.7453/gahmj.2013.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oliver JW, Kravitz RL, Kaplan SH et al. Individualized patient education and coaching to improve pain control among cancer outpatients. J Clin Oncol 2001;19:2206–12. [DOI] [PubMed] [Google Scholar]
- 49.Fisher EB, Strunk RC, Highstein GR et al. A randomized controlled evaluation of the effect of community health workers on hospitalization for asthma: the asthma coach. Arch Pediatr Adolesc Med 2009;163:225–32. 10.1001/archpediatrics.2008.577 [DOI] [PubMed] [Google Scholar]
- 50.Knowler WC, Barrett-Connor E, Fowler SE et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403. 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oppezzo M, Schwartz DL. Give your ideas some legs: the positive effect of walking on creative thinking. J Exp Psychol Learn Mem Cogn 2014;40:1142–52. 10.1037/a0036577 [DOI] [PubMed] [Google Scholar]
- 52.Abramson S, Stein J, Schaufele M et al. Personal exercise habits and counseling practices of primary care physicians: a national survey. Clin J Sport Med 2000;10:40–8. [DOI] [PubMed] [Google Scholar]
- 53.Michie S, Richardson M, Johnston M et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 54.Zheng Y, Klem ML, Sereika SM et al. Self-weighing in weight management: a systematic literature review. Obesity 2015;23:256–65. 10.1002/oby.20946 [DOI] [PubMed] [Google Scholar]
- 55.Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 2005;6:67–85. 10.1111/j.1467-789X.2005.00170.x [DOI] [PubMed] [Google Scholar]
- 56.Kruger J, Blanck HM, Gillespie C. Dietary and physical activity behaviors among adults successful at weight loss maintenance. Int J Behav Nutr Phys Act 2006;3(1):17 10.1186/1479-5868-3-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res 2004;12(S12):151S–62S. 10.1038/oby.2004.282 [DOI] [PubMed] [Google Scholar]
- 58.Tugwell P, O'Connor A, Andersson N et al. Reduction of inequalities in health: assessing evidence-based tools. Int J Equity Health 2006;5:11 10.1186/1475-9276-5-11 [DOI] [PMC free article] [PubMed] [Google Scholar]