Abstract
This is an updated guideline for the diagnosis and management of asthma, developed by the Saudi Initiative for Asthma (SINA) group, a subsidiary of the Saudi Thoracic Society. The main objective of SINA is to have guidelines that are up to date, simple to understand and easy to use by nonasthma specialists, including primary care and general practice physicians. SINA approach is mainly based on symptom control and assessment of risk as it is the ultimate goal of treatment. The new SINA guidelines include updates of acute and chronic asthma management, with more emphasis on the use of asthma control in the management of asthma in adults and children, inclusion of a new medication appendix, and keeping consistency on the management at different age groups. The section on asthma in children is rewritten and expanded where the approach is stratified based on the age. The guidelines are constructed based on the available evidence, local literature, and the current situation in Saudi Arabia. There is also an emphasis on patient–doctor partnership in the management that also includes a self-management plan.
Key words: Asthma, Asthma control test, guidelines, Saudi Arabia
Asthma is a common heterogeneous chronic disorder of the airways, characterized by variable usually reversible and recurring symptoms related to one or more of airflow obstruction, bronchial hyper-responsiveness, and underlying inflammation. It is one of the most common chronic diseases in Saudi Arabia, affecting more than 2 million Saudis.[1] Its impact is manifested in patients, their families, and the community as a whole in terms of lost work and school days, poor quality of life, frequent emergency department (ED) visits, hospitalizations, and deaths.[2,3,4] As part of the commitment of the Saudi Thoracic Society (STS) toward a long-term enhancement plan for promoting the best practice in the field of respiratory diseases,[5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23] the Saudi Initiative for Asthma (SINA) was developed in 2009 with special attention to nonasthma specialists, including primary care and general practice physicians.[24,25] Sections related to asthma in children represent the views of a panel from the Saudi Pediatric Pulmonology Association, another subsidiary of the STS. SINA guidelines previously updated in 2012 with an emphasis on new evidence including a new section on difficult to treat asthma (DTA), easy to use charts, and more information related to asthma in children.[25] SINA panel is a group of Saudi experts with well-respected academic backgrounds and experience in the field of asthma. Since SINA aims to have updated guidelines, which are simple to understand and easy to use, SINA expert panel realized the need to update the current guidelines with the available new evidence, new medications, new indications for existing medications, and changes in current practices. To streamline recommendations, SINA expert panel has stratified the guidelines based on the following age groups: Adults age above 18 years, adolescents age 12–18 years, and children who were stratified into two groups such as 5–11 years and below 5 years.
Methods
SINA guidelines were initially based on two existing international guidelines, the Global Initiative for Asthma (GINA) and the National Asthma Education and Prevention Program.[26,27,28,29,30,31] These were customized based on reviewing the available local literature and the current setting in Saudi Arabia. The same approach was continued in 2012 and 2016 update.[32] Consensus among the SINA panel was followed whenever there was lack of evidence in the form of nonrandomized controlled trials or nonrandomized studies.[33] The following criteria are used to grade the evidence:
Evidence category A: Randomized controlled trials with rich body of data
Evidence category B: Randomized controlled trials with limited body of data
Evidence category C: Nonrandomized trials and observational studies
Evidence category D: SINA panel consensus judgment. This category is only used in cases where the provision of some guidance was deemed valuable, but the clinical literature addressing the subject was insufficient to justify placement in one of the other categories.
For this update, the same approach has been continued where each section was internally reviewed by at least two other members. SINA panel conducted round-table discussions frequently and jointly reviewed it. A panel of international experts reviewed the guidelines, and their recommendations were thoughtfully considered. The expected outcome will lead to a safe and high-quality patient care.
Epidemiology
Asthma is one of the most common chronic illnesses in Saudi Arabia, and local reports suggest that the prevalence of asthma is increasing.[34,35,36] Poor knowledge, fear of the use of new drugs, and the lack of awareness of the importance of disease control are common among primary care physicians who care for asthma patients in Saudi Arabia. In addition to these important factors, there are other attributes to the magnitude of disease burdens such as socioeconomic status, number of siblings, knowledge of caregivers, and income.[37,38,39,40,41,42] Consequently, many asthma patients continue to be underdiagnosed, undertreated, and at risk of acute exacerbations resulting in missed work or school, increased use of expensive acute healthcare services, and reduced quality of life.[43,44,45] A study by Al-Kabbaa et al. found that only 39% of primary care physicians met the standards of the national guidelines in management of asthma.[46] In addition, the overall level of awareness among physicians was low (52%). Their proficiency in general knowledge, diagnosis, classification of severity, and management was also low. An asthma control survey of patients showed that only 5% of the patients were controlled, 31% were partially controlled, and 64% were uncontrolled.[47]
The prevalence of asthma in two population of school children aged between 8 and 16 years was studied using an internationally designed protocol in 1986 and 1995.[48] Comparison of the data from Riyadh versus Hail (inland desert areas with dry environment) and Jeddah versus Jazan (coastal humid environment) revealed that the prevalence of asthma in similar population increased significantly from 8% in 1986 to 23% in 1995.[49] The study also revealed that there was increased exposure to environmental factors such as tobacco smoke and indoor animals in Saudi houses, which may have contributed. Bener et al. compared the prevalence of physician-diagnosed asthma among Saudi school boys in the industrial city of Yanbu to two nonindustrial villages in a cross-sectional study.[50] The prevalences in industrial and nonindustrial areas were 13.9% and 8%, respectively. Hijazi et al. conducted a study of 1020 urban and 424 rural children aged 12 years. They attempted to compare the prevalence of allergic symptoms among those living in urban and rural areas of the Saudi Arabia and investigate factors associated with any differences found.[51] The prevalence of allergic symptoms was found to be significantly greater among urban children than the rural ones and was more among Saudi than non-Saudi children.[52] Males were more susceptible to have certain respiratory symptoms and females had more eye and skin symptoms. The educational level and occupation of the father did not influence the likelihood of having symptoms.
Most of the studies investigating the prevalence of asthma in various countries have focused on children below the age of 15 years or adults above the age of 18 years. There is limited knowledge concerning the prevalence of asthma in 16–18 years old adolescents. A study conducted by STS investigated the prevalence of asthma and associated symptoms in 16–18 years old adolescents attending high schools in the city of Riyadh. This study utilized the International Study of Asthma and Allergies in Children (ISAAC) questionnaire tool. Of 3073 students (1504 boys and 1569 girls), the prevalence of lifetime wheeze, wheeze during the past 12 months, and physician-diagnosed asthma were 25.3%, 18.5%, and 19.6%, respectively. The prevalence of exercise-induced wheezing and night coughing in the previous 12 months were 20.2% and 25.7%, respectively. The prevalence of rhinitis symptoms in students with lifetime wheeze, physician-diagnosed asthma, and exercise-induced wheeze were 61.1%, 59.9%, and 57.4%, respectively. Rhinitis symptoms were significantly associated with lifetime wheeze (odds ratio [OR] = 2.5, P < 0.001), physician-diagnosed asthma (OR = 2.2, P < 0.001), and exercise-induced wheeze (OR = 1.9, P < 0.001).[53] By utilizing the ISAAC questionnaire method, a recent study by Nahhas et al. conducted among 5188 primary school children in Madinah showed that the prevalence of asthma was 23.6%, where 41.7% had symptoms suggestive of at least one allergic disorder.[54]
Although the prevalence of asthma in Saudi Arabian adults is unknown, the overall prevalence of asthma in children from Saudi Arabia has been reported to range from 8% to 25% based on studies conducted over the past three decades. The highest prevalence of physician-diagnosed asthma in Saudi Arabia was reported to be 25% in 2004.[55] The increasing prevalence of asthma in the past three decades may be attributed to rapid lifestyle changes related to the modernization of Saudi society, changes in dietary habits, and exposure to environmental factors such as indoor allergens, dust, sand storms, and tobacco. In addition, this high prevalence of asthma could be attributed to an increase in asthma awareness in the general population and among healthcare workers, allowing more individuals to be diagnosed. Other explanations have attributed the increased prevalence to the hygiene hypothesis, which proposes that there is a lack of sufficient microbial exposure early in life due to pharmacological manipulations and vaccines.[56]
Diagnosis of asthma in adults and adolescent
The diagnosis of asthma is based on clinical assessment as there is no gold standard diagnostic test for asthma. This includes a detailed history and physical examination supplemented by spirometry with reversibility testing to support the diagnosis.
History
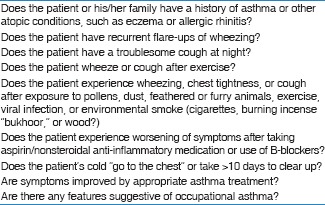
The symptoms of wheezing, cough, shortness of breath, and chest tightness are not specific for asthma and can be seen with other pulmonary diseases. However, the combination of these symptoms increases the probability of asthma. The pattern of symptoms is usually variable over time, and the patient may be entirely asymptomatic between exacerbations.[57,58] Symptoms are usually worse at night, particularly in children, and can be provoked by exercise or other triggering factors such as viral infections and/or smoke. Box 1 lists the relevant questions that are commonly considered when taking a history. Asthma control may be worsened by coexisting symptomatic gastroesophageal reflux disease (GERD), rhinosinusitis, obesity, sleep disorders, or the use of some medications such as beta blockers and nonsteroidal anti-inflammatory drugs (NSAIDs) including aspirin (ASA).[59] Asthma and rhinosinusitis commonly coexist.[60,61]
Box 1.
Relevant questions in the diagnosis of asthma
Physical examination
It is important to note that the examination of the chest maybe normal but the presence of bilateral expiratory wheezing is suggestive of a diagnosis of asthma. Examination of the upper airways is important to look for evidence of allergic rhinitises such as mucosal swelling, nasal polyps, and postnasal dripping. Other allergic manifestations, such as atopic dermatitis and/or eczema, also support the diagnosis of allergic asthma.[57,62] The presence of a localized wheeze, crackles, stridor, clubbing, or heart murmurs should suggest alternative diagnoses.[63,64] Therefore, there should be a careful consideration of any possible alternative diagnosis before commencing asthma treatment by a physician.
Essential investigations
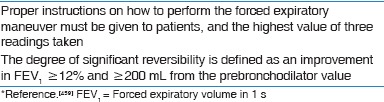
Spirometry is necessary to confirm airflow obstruction, assess severity and demonstrates significant reversibility [Box 2]. It may help identify other diagnoses, for example, upper airway obstruction. However, normal spirometry, including a failure to show reversibility, does not rule out the diagnosis of asthma as it can be normal with the patient still being symptomatic.[65] Serial peak expiratory flow rate (PEFR) measurements may be helpful in the diagnosis of asthma by showing the characteristic variability and for follow-up after starting treatment. Bronchoprovocation testing is another tool to rule out asthma when the result is negative. A diagnostic, therapeutic trial with an inhaled steroids and a bronchodilator may be useful in confirming a diagnosis when it shows a favorable response.[66]
Box 2.
Acceptable spirometry and significant bronchodilator response*
Chest X-ray is not routinely recommended unless the diagnosis is in doubt, when symptoms are not typical, or suggest other diagnoses. Peripheral eosinophilia and elevated immunoglobulin E (IgE) level are supportive of the diagnosis but are not routinely recommended. Skin testing and radioallergosorbent test (RAST) may be helpful in identifying allergens to which the patient has been sensitized and in developing a strategy for avoiding allergen exposure.[67]
Clinical assessment in adults and adolescents
Principles of asthma assessment
The principles of optimal asthma management should consist initially of an assessment of asthma control.[68] Before commencing a patient on treatment, SINA expert panel recommends to ensure the following:
Assessment of asthma control [Box 3]
Physiological measurement with tools such as spirometry or peak flow meter
Documentation of current treatment and any related issues such as side effects, adherence, and inhaler technique
Provision of a written asthma action plan
Assessment of comorbidities such as rhinosinusitis, GERD, obesity, obstructive sleep apnea, and anxiety
Close monitoring for patients with severe asthma and history of asthma exacerbations.[69]
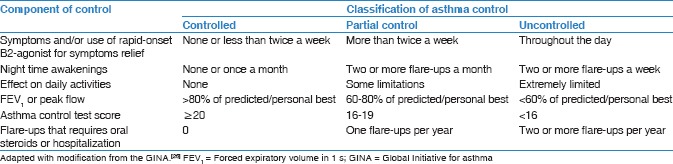
Box 3.
Assessing asthma control in adults
Asthma control test
Asthma severity was historically used as the entry point to determine the management strategy. This trend has been replaced by the concept of asthma control.[70] Asthma control is a reflection of the adequacy of management by describing the clinical status of a patient as controlled, partially controlled, or uncontrolled. The control status may vary markedly over short period and is recommended to entail short-term assessment of current asthma status, asthma burden, and medical management.[71] Focusing on asthma control may improve patient perceptions and expectations that improve symptoms reporting and subsequently treatment decisions by clinicians.[71] In addition to assessing the control status, future risk of adverse outcomes should be assessed. This is achieved by assessing future risk of exacerbations, fixed airflow obstruction, and adverse effect of medications.
SINA expert panel recommends the utilization of asthma control test (ACT) to initiate asthma treatment in adults and adjust it at follow-up.[72,73,74] ACT is a commonly used tool to assess asthma control. It is a short, validated, self-administered questionnaire to assess asthma control [Box 4]. It consists of five items including limitation of activity, shortness of breath, frequency of night symptoms, use of rescue medication, and rating of overall control of the disease over the past 4 weeks.[75] The score of ACT is the sum of the five questions where each is scored from 1 (worst) to 5 (best), leading to a maximum best score of 25. The clinically important change in ACT score is considered ≥3 units.[76] The level of asthma control is categorized into:[74,75,77]
Box 4.
Asthma control test*
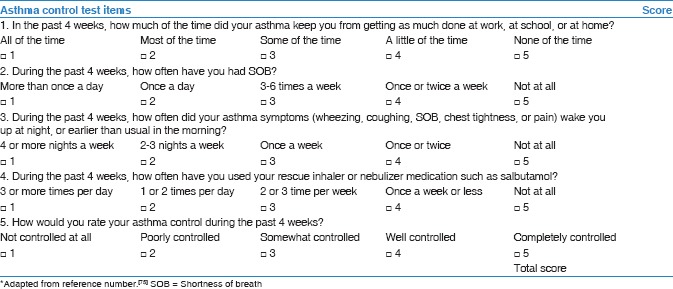
Controlled: An ACT score of ≥20
Partially controlled: An ACT score of 16–19
Uncontrolled: An ACT score of <16.
Assessment when control is not achieved
If asthma control is not achieved at any step during therapy, SINA expert panel recommends assessing the following:
Medications and doses currently used
Patient's adherence and correct technique in using devices
Selection of the appropriate device and appropriate prescription of spacer with metered dose inhaler (MDI) device
Problems and difficulties faced by the patient taking the medications (e.g., cost, time, and lack of perceived need)
Patient's concerns about asthma medications.
Assessment of risk factors for asthma exacerbations
SINA expert panel recommends assessment of risk factors for poor asthma outcomes, especially those patients experiencing exacerbations.[31] The presence of one or more of the following risk factors increases the risk of exacerbation despite controlled asthma status:
High usage of relievers medication[78]
Inadequate inhaled corticosteroid (ICS) use[79]
Low forced expiratory volume in 1 s (FEV1)[80]
Previous Intensive Care Unit (ICU) admission[81]
A severe asthma exacerbation in the previous 12 months[82]
Major psychological disorders or reduced socioeconomic status[83]
Continuous exposure to allergens[84]
Presence of comorbidities
Sputum or blood eosinophils[85]
Pregnancy.[86]
Asthma severity assessment in clinical practice
There is a trend in clinical practice to retrospectively assess asthma severity based on the step of treatment required to control symptoms and exacerbations.[31,87,88,89] Before classifying asthma severity, “it is essential to ensure that control is achieved on the minimal level of medications over a few months.” Such asthma severity level could change over years or months. Therefore, asthma level of severity can be as follows:
Mild asthma: Controlled asthma at step 1 or 2 (as needed reliever treatment, monotherapy of low-dose ICS, or leukotriene receptor antagonist [LTRA])
Moderate asthma: Controlled asthma at step 3 (on combination of ICS/long-acting beta 2 agonist [LABA] or other alternative options at steps 3)
Severe asthma: Asthma that requires treatment step 4 or 5 (on combination of high-dose ICS/LABA with or without add-on treatment).
Nonpharmacological management
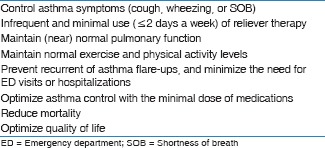
The long-term goal of asthma therapy is to achieve and maintain asthma control by utilizing pharmacological and nonpharmacological measures [Box 5]. Appropriate implementation of nonpharmacological measures is expected to lead to utilization of the least possible dose of medications to minimize the risk of their side effects if any.
Box 5.
Long-term goals of asthma management
Developing partnership with the patient
The development of partnership between patients and healthcare professionals leads to enhancement of knowledge, skills, and attitude toward understanding asthma and its management. Based upon agreed goals of management, a written self-management action plan should be offered to the patient. A wide variety of plans are available which vary from patient-based to physician-based plans. This is expected to be reflected positively on patient adherence, which is a major issue in the management. Factors leading to nonadherence may be related to poor inhaler technique, a regimen with multiple drugs, concern regarding side effects from the drugs, or the cost of medications.[90,91,92] Other factors include lack of knowledge about asthma, lack of partnership in its management, inappropriate expectations, underestimation of asthma symptoms, use of unconventional therapy, and cultural issues.[93,94]
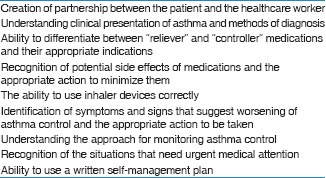
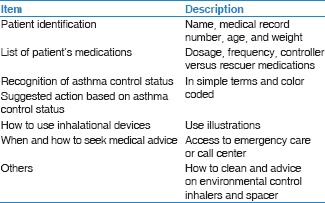
Asthma education
The goal of asthma education is to provide a patient with asthma (or the parents of a child with asthma) – adequate training to enhance their knowledge and skills to be able to adjust treatment according to guided self-management.[69,95,96,97,98,99] To enhance the level of knowledge and skills among asthma patients, education is recommended to include knowledge about asthma and skills related to inhaler devices prescribed, as there maybe misperceptions about the use of inhalers and the safety of ICS.[100,101,102,103] Asthma education should be conducted by a well-trained healthcare worker, who has good communication skills and can create an interactive dialog in a friendly environment. With the availability of appropriate information, patients will be encouraged to continue on the management plan and reassured about the control of their asthma.[104] It is essential to get the feedback from the patient to maintain a bidirectional rapport and an optimum environment. It has been documented that a well-structured asthma education program improves quality of life, reduces cost, and decreases the utilization of healthcare resources.[105,106,107,108] Asthma should be structured based on the available resources [Box 6].
Box 6.
Outcomes of asthma education program
Written action plan for asthma
It is considered an integral part of asthma management for patients and doctors. It helps recognize the loss of control of asthma and gives clear instructions for early intervention to prevent asthma exacerbations. The asthma action plan may be based on symptoms or PEFR measurements [Box 7].[109] Regular review of the asthma action plan is important as a person's level of asthma control may change over time. If a patient has an asthma exacerbation, the patient should be assessed to see if he/she has effectively used their action plan.
Box 7.
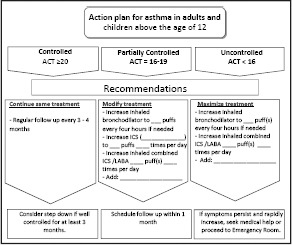
Action plan for Asthma for adults and adolescent
Identify and reduce exposure to risk factors
Measures to prevent or reduce exposures to risk factors should be implemented wherever possible. There are different triggers leading to acute asthma exacerbations, which may include allergens, viral infections, pollutants, drugs, and occupational agents. These factors can be classified as indoor or outdoor allergens and occupational sensitizers.
Indoor allergens and air pollutants
There is a wide spectrum of indoor allergens that includes domestic mites, furred animals, cockroaches, and fungi.[110,111] The most important indoor air pollutant is related to tobacco exposure.[112] Measures to avoid tobacco exposure will lead to better asthma control and avoidance of long-term lung function impairment.
Outdoor allergens
Outdoor allergens such as pollens and molds are impossible to avoid completely; exposure may be reduced by closing windows and doors, remaining indoors during dust storms, and initial rainy seasons, and using air conditioning if possible. It is recommended to avoid outdoor strenuous physical activities in cold weather, low humidity, or high air pollution.[113]
Occupational exposures
Whenever an occupational sensitizer is identified, it is advisable to keep the affected person away from that environment. The earlier the removal of this sensitizer takes place the higher the chance of complete recovery from occupational asthma.
Food and drugs
Food and food additives are uncommon triggers of asthma. Avoidance cannot be recommended until it is documented by a specialist. However, certain drugs whenever identified should be avoided (e.g., beta blockers).
Influenza vaccination
Annual influenza vaccination is advised for individuals with asthma, especially those with severe asthma.[114,115]
Pharmacological management in adults and adolescent
SINA expert panel recommends asthma treatment to be based on following phases:
Initiation of treatment
Adjustment of treatment
Maintenance of treatment.
At each phase, the patient is recommended to have clinical assessment that includes symptoms assessment by ACT, physiological measurement with PEFR or spirometry, review of current medications and patients’ adherence and inhaler technique, risk for exacerbations, and response to treatment. Based on clinical and physiological assessment, the patient is placed on the appropriate step of treatment [Box 8]. Appendix 1 contains more information about medications used in asthma treatment. In general, SINA expert panel recommends the following strategies for treating patient with asthma:
Box 8.
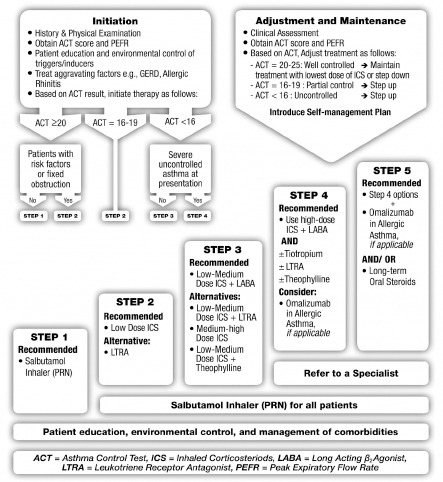
Initiation, adjustment and maintenance of outpatient asthma treatment in adults and adolescent patients
A daily controller medication is needed. ICS is considered the most effective controller especially for mild to moderate disease (Evidence A)[116,117]
Relievers or rescue medications must be available to patients at all steps. Short-acting bronchodilators (SABAs) are recommended to be taken on “as needed bases” to relieve symptoms. Increasing the use of reliever treatment is usually an early sign of worsening of asthma control (Evidence A)[118]
Regular assessment of adequate doses of treatment, proper technique, and adherence
Management of comorbidities with special attention to concomitant rhinosinusitis. As this condition affects asthma control, its treatment is expected to improve asthma (Evidence A).[119,120,121,122,123,124] The treatment includes nasal steroids, LTRA, and antihistamines. Coexisting rhinosinusitis is recommended to be treated appropriately as well.
Initiation of treatment
Patients with asthma often underestimate the presence of asthma symptoms and also tend to assume their asthma is controlled when this is not the case.[125] Therefore, the consensus among SINA expert panel is to simplify the approach and supplement the initiation of asthma therapy by utilizing an objective measurement with the ACT [Box 4]. The following initial steps are recommended based on ACT score:
-
ACT score ≥20:
- Step 1: For patients with mild and infrequent symptoms (Evidence B)[74]
- Step 2: For patients with risk factors for exacerbation or fixed obstruction (Evidence B).[116,126] It is also recommended for patients with seasonal asthma who are symptomatic during the season, otherwise, it is recommended to be treated at step 1 for the rest of the year if their score is ≥20 (Evidence D).
-
ACT score 16-19:
- Step 2: For patients with an ACT score of 16–19 who also qualified for partially controlled asthma status (Evidence B).[74] This includes those with a history of asthma exacerbation in the past year.
-
ACT score <16:
- Step 3: For most patients with an ACT score of <16 (Evidence B).[74] However, for patients with early signs of exacerbation at presentation, a short course of oral steroids may be required
- Step 4: For patients who have severely uncontrolled asthma at presentation, initiation of asthma treatment at a higher step with a combination of high-dose ICS and/LABA may be required (Evidence D).
Adjustment of treatment
After initiation of asthma treatment, it is recommended to assess the patient in 1–3 months (Evidence D). SINA expert panel recommends the utilization of stepwise approach to therapy to achieve asthma control. The stepwise approach consists of 5 steps as shown in Box 8. Upon follow-up, it is recommended to either maintain treatment until patients have achieved control, to step up for those did not achieve control (assuming adherence and appropriate inhaler technique have been confirmed), or step down for those who have maintained control for an extended period. It is important to determine the minimal amount of medications required to maintain control to reduce the risk of side effects. The following paragraphs will describe each step in detail.
Treatment at step 1
Recommended option: SABA on “as-needed bases.” Symptoms are usually mild and infrequent with an ACT score of ≥20 (Evidence A)[118,127]
Some patients may be recommended for a higher step if they are controlled during the time of assessment (an ACT score of ≥20), but have risk factors for exacerbations or fixed airway obstruction (see below).
Treatment at step 2
Recommended option: A daily low-dose ICS (<500 mcg of beclomethasone or equivalent/day) with SABA on “as needed bases” (Evidence A)[116,128]
An alternative treatment is LTRA (montelukast), especially in those patients reluctant to use ICS, resisting its use or continue to have voice hoarseness despite preventive measures (Evidence A).[129] It should be noted LTRA is less-effective than ICS in achieving asthma control and also less-effective in reducing the risk of exacerbations
Patients with mild and infrequent symptoms and an ACT score of ≥20 with risk factors for exacerbation or fixed obstruction are recommended for at least step 2 between asthma exacerbations (Evidence B)[116,126]
Patients with seasonal asthma who are symptomatic during the season are recommended to be treated at step 2 during the season, otherwise, it is recommended to be maintained at step 1 for the rest of the year; i.e., using SABA on “as needed bases” (Evidence D).
Treatment at step 3
Recommended option: Adding a LABA to a low-medium dose ICS in a combination device improves asthma control for patients whose asthma is not controlled at step 2 (Evidence A).[126,130,131] The patient is recommended to continue on reliever treatment on “as needed bases” (Evidence A)
ICSs in the form of beclomethasone propionate, budesonide, momethasone furoate, or fluticasone propionate are currently combined with either salmeterol or formoterol. These are normally prescribed twice daily [refer to Appendix 2]
If a combination inhaler containing formoterol is selected, patient may be advised to use it for both maintenance and rescue using extra puffs from the same inhaler (Evidence A).[132] When combination of budesonide and formoterol is used (Symbicort Turbohaler - 160/4.5), the recommended dose is 1–2 puffs twice daily plus extra puffs that should not exceed 12 puffs/day. Those patients who require such high-doses for 2–3 days should seek medical advice to step up therapy as they may require the use of a short course of oral prednisolone (Evidence A)
If a twice a day combination of fluticasone propionate/salmeterol (Seretide) is selected, an escalation of the regular daily doses was found to achieve well-controlled asthma status in 85% of patients and totally controlled asthma status in 30% (Evidence A)[133]
The new once a day combination of ICS/ultra LABA can be prescribed based on availability. The approved product in Saudi market is fluticasone furoate/vilanterol (Relvar) that can be prescribed for adults and children above 12 years at a dose of 100/25 mcg dose (Evidence A).[134,135] The ultra LABA (Vilanterol) has the advantage of onset of action within 15 min and a long half-life; therefore, the patient should be advised to only use it once a day on a regular basis
There has been a warning about the use of inhaled LABAs alone in asthma management.[136] Asthma patients taking inhaled LABAs without inhaled ICS are at an increased risk of asthma exacerbations, hospitalizations, and death.[137] Based on this evidence, the Saudi Food and Drug Administration withdrew all LABA monotherapy medications from the Saudi market by the end of 2010.[138] Therefore, the SINA panel has limited the use of relievers to SABA or formoterol containing combination when SMART approach is used
Alternative and generally less-effective strategies include the continuation of ICS as a monotherapy by increasing the dose to the medium-high dose range (Evidence A),[137,139] and the addition of LTRA to a low-medium dose ICS (Evidence A),[140,141] especially in patients with concomitant rhinitis.[142] The addition of sustained release theophylline to a low-medium dose ICS is a possible but not favorable choice (Evidence B)[143]
Tiotropium is a long-acting anticholinergic agent approved for the treatment of chronic obstructive pulmonary disease (COPD).[144,145,146] Recent evidence has shown that when tiotropium when added to an ICS, improves symptoms, reduce risk of exacerbation, and improve lung function in patients with inadequately controlled asthma. Its effect appears to be at least equivalent to LABA (Evidence A).[147,148,149] This evidence supports that tiotropium can be used as an alternative to LABA when added to ICS
Consultation with a specialist is recommended for patients whenever there is a difficulty in achieving control at step 3 (Evidence D).
Treatment at step 4
Recommended option: Escalation of treatment by combining high-dose ICS with LABA (Evidence A)[104,139,140,150]
In addition to the currently available combinations of ICS/LABA mentioned in step three section, the new once a day combination of fluticasone furoate/vilanterol (Relvar) can be prescribed for adults and children above 12 years at a dose of 200/25 mcg dose[134,135]
If symptom control is not achieved, adding tiotropium to the combination of ICS and LABA is a recommended option as it significantly improves lung function in uncontrolled cases and reduce exacerbations (Evidence A)[144,151,152]
Adding LTRA to the combination of high-dose ICS and LABA is also recommended but the evidence for this is less robust (Evidence B)[153,154]
Adding theophylline to the combination of high-dose ICS and LABA is another less favorable alternative (Evidence B)[154,155]
Omalizumab may be considered for those patients uncontrolled on maximum treatment at this step with modification of any triggers and who have allergic asthma as determined by an IgE level in the appropriate therapeutic range, the result of skin test or RAST study (Evidence A), or a strong history of atopy (Evidence D).[139,140,150] Special knowledge about the drug and its side effects should be available before administering omalizumab by any physician. Therefore, referral to an asthma specialist is mandatory[156]
Consultation with a specialist is recommended for patients who require this step of therapy (Evidence D).[157]
Treatment at step 5
Consultation with an asthma specialist is strongly recommended for patients having difficulty in achieving asthma control at step 4 and requires step-up to step 5 (Evidence D)
In patients who continue to be symptomatic despite step 4 level of care, omalizumab is recommended for patients who have allergic asthma and persistent symptoms despite the maximum therapy mentioned above (Evidence A)[139,140,150]
If the patient does not have allergic asthma or omalizumab is not available or not adequately controlling the disease, the alternative approach is to use the lowest possible dose of long-term oral corticosteroids (Evidence D). However, there are many new monoclonal antibodies in the horizon for management of asthma that are not yet available in the local market[89]
-
For patients who require long-term systemic corticosteroids, the following are recommended to be considered:
- Use the lowest possible dose to maintain control
- Closely monitor the development of corticosteroid-related side effects
- When asthma control is achieved, continue attempts to reduce the dose of systemic corticosteroids, preferably to every other day frequency. Maintaining high-dose of ICS therapy may help to reduce the dose of systemic steroid
- Adjustment of steroid dose at the time of stress (e.g. infection, asthma exacerbations, and surgery) is essential
- Strongly consider concurrent treatments with calcium supplements, Vitamin D, and bone-sparing medications (e.g., bisphosphonates) in patients who have risk factors for osteoporosis or low bone mineral density (Evidence C).
Maintaining asthma control
Regular follow-up by a healthcare worker is essential. Depending on the level of asthma control, it is recommended to have a follow-up at 1–3 month intervals (Evidence D).[104,158] Follow-up should include monitoring and reviewing the patient's written asthma action plan, medication adherence and inhaler technique, patient's behaviors, and possible side effects of medications. Once asthma is well controlled and the control is maintained for at least 3 months, a step down in pharmacologic therapy is recommended to at the minimum therapy level that can maintain good control and minimize side effects (Evidence D). The following are recommended:
Reduction in therapy is recommended to be gradual and closely monitored based on clinical judgment of the individual patient's response to therapy and ACT score (Evidence D)
If the patient is on ICS as monotherapy, the dose of ICS may be reduced by 25% every 3–6 months to the lowest dose possible that is required to maintain control (Evidence B),[97,159,160] and then changed to a single daily dose (Evidence A).[161] It is recommended to be clearly explained to the patient that asthma control may deteriorate if treatment is abruptly discontinued[162]
If patient is on combination of ICS/LABA at step 3 or 4, abrupt discontinuation of LABA may lead to deterioration of control[163]
If the patient is on a combination of ICS, LABA, LTRA, and other controllers, taper ICS to the lowest possible dose (Evidence B).[164,165] If control is achieved, LTRA may be discontinued (Evidence D)[164]
For significant side effects, consider a change in therapy, reduction in the dose or frequency of ICS (if possible), advise vigorous mouth washing after inhalation, use of spacer (concomitant with MDI devices), and/or use of appropriate local antifungal therapy such as mycostatin mouth wash, for severe oral thrush[166]
Patients should be informed that asthma control may deteriorate if treatment is completely discontinued.
Referral to an asthma specialist
Situations that require referral to an asthma specialist for consultation or co-management include:
There is uncertainty regarding the diagnosis
There is difficulty achieving or maintaining control of asthma
Immunotherapy or omalizumab is considered
Difficulty to achieve asthma control at step 3 or higher
The patient has had acute asthma exacerbation requiring hospitalization.
Immunotherapy
Allergen-specific immunotherapy (AIT) is the practice of administering gradually increasing quantities of an allergen product to an individual with IgE-mediated allergic disease to ameliorate the symptoms associated with subsequent exposure to a causative allergen. It is administered either subcutaneously or sublingually.[167,168,169] AIT is the only currently available medical intervention that has the potential to affect the natural course of the disease.[170] There are available data shown that AIT can achieve substantial benefit for patients, improving the allergic individuals’ quality of life, reducing the long-term costs and burden of allergies, and changing the course of the disease. AIT does not only effectively alleviate allergy symptoms, but it has a long-term effect and can prevent the progression of allergic diseases.[171,172] AIT is more effective in seasonal asthma than in perennial asthma, particularly when used against a single allergen. It may be considered if strict environmental avoidance and comprehensive pharmacologic intervention by an asthma specialist have failed to control the disease.[173]
AIT has been a controversial treatment for asthma; however, beneficial clinical effects have been demonstrated in randomized controlled trials including Cochrane Systematic Reviews. Overall, there was a reduction in asthma symptoms, medications, and improvement in bronchial hyper-reactivity following immunotherapy.[174,175] Allergen immunotherapy reduces allergen-specific bronchial hyper-reactivity, with some reduction in nonspecific bronchial hyper-reactivity as well. In addition to concerns regarding safety and cost, there is no consistent effect on lung function.[175,176,177,178]
Management of acute asthma in adults and adolescents
Acute asthma exacerbation is a challenging clinical scenario that requires a systemic approach to rapidly diagnose the condition, evaluate its severity, and initiate therapy. The first step of managing acute asthma is the early recognition to prevent the occurrence of exacerbations. Asthma, in general, has a low mortality rate compared with other lung diseases. Nevertheless, patients do die, especially patients with poorly controlled asthma whose condition deteriorates over a period of days before the final fatal event.[81,179,180,181,182] The most specific marker associated with increased asthma mortality would be a history of repeated hospital admissions, particularly if patients required intensive care treatment or ventilatory assistance.[182,183] A recent study from Saudi Arabia by Al-Dorzi et al. compared 30 patients admitted with near fatal asthma to a control group.[184] They were found to be younger and predominantly males and used less ICS/LABA combination. Near fatal asthma, outcomes included neuromyopathy (23%), mechanical ventilation duration of 6.4 ± 4.7 days, tracheostomy (13%) with no deaths. In addition, it has been shown that a subgroup of patients who present with near-fatal asthma have blunted perception of dyspnea, and have a history of frequent ED visits, hospitalizations, and near fatal asthma events.[185] This section includes assessment of patient with acute asthma, initial management, and follow-up after initial management. More information about medications used in acute asthma is shown in Appendix 2.
Clinical assessment of acute asthma
The initial clinical assessment should rapidly determine whether the patient's presenting symptoms are related to an acute asthma exacerbation or not. Of note, it is necessary to recognize that acute asthma is different from mild to moderate asthma exacerbation secondary to poor asthma control that simply require a step-up in the chronic asthma therapy. Although most acute asthma exacerbations develop over a period of days, patients with brittle asthma may present with a much more dramatic deterioration [Box 9]. It is important to realize that most patients who die from an acute asthma exacerbation had chronically uncontrolled asthma, had received inadequate treatment with ICS, and had inadequate monitoring of their asthma.[186,187,188,189,190] Furthermore, it has been shown that over 80% of such exacerbations developed over more than 48 h, allowing enough time for effective action to reduce the number of exacerbations requiring hospitalization.[191,192,193,194]
Box 9.
Levels of severity of acute asthma in adults
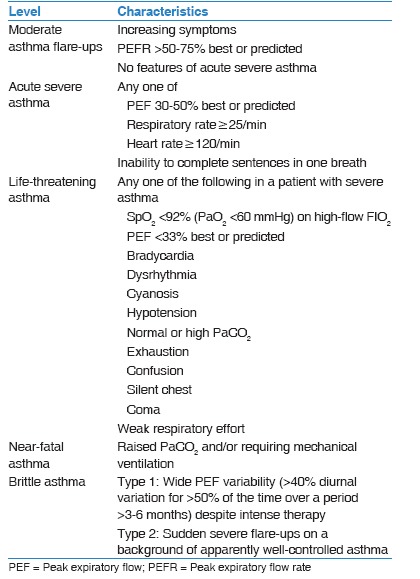
Management of acute asthma in adults is the extreme spectrum of uncontrolled asthma and represents the failure to reach adequate asthma control. The presence of the following features should be sought:
Previous history of near-fatal asthma
Whether the patient is taking three or more medications
Heavy use of SABA
Repeated visits to the ED
Brittle asthma.
Upon presentation, a patient should be carefully assessed to determine the severity of the exacerbations [Box 9] and the type of treatment required.[195,196] PEFR and pulse oximetry measurements are complementary to history taking and physical examination. Treatment of acute asthma exacerbations requires a systematic approach similar to chronic asthma management. Acute asthma management is recommended to follow these steps:
Assess severity of the exacerbation
Initiate treatment to rapidly control the exacerbation
Evaluate continuously the response to treatment.
The following levels of acute asthma severity should be quickly identified, as approach to management and prognosis varies significantly [Box 10].
Box 10.
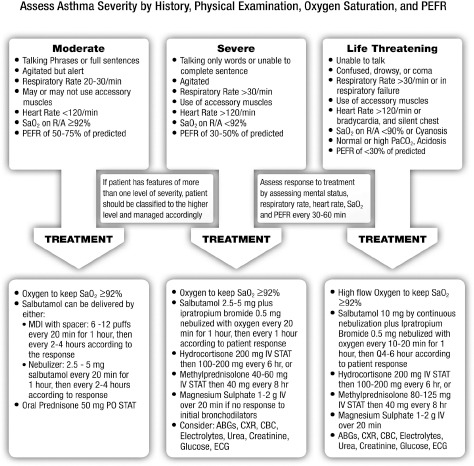
Initial management of acute asthma in adults and adolescents
Assessment of acute asthma severity
Mild acute asthma
Patients presenting with mild asthma exacerbation are usually treated in an outpatient by stepping up in asthma management, including increasing the dose of ICS.[197] However, some cases may require short course of oral steroids.
Moderate acute asthma
Patients with moderate asthma exacerbation are clinically stable. They are usually alert and oriented, but may be agitated. They can communicate and talk in full sentences. They are tachypnoeic and may be using their respiratory accessory muscles. Heart rate is < 120/min and blood pressure is normal. A prolonged expiratory wheeze is usually heard clearly over the lung fields but examination of the chest maybe relatively normal. Oxygen saturation is usually normal secondary to hyperventilation. PEFR is usually in the range of 50–75% of predicted or previously documented best. Measurement of arterial blood gases (ABGs) is not routinely required in this category; however, if done, it shows widened alveolar–arterial oxygen gradient and low PaCO2, secondary to increased ventilation perfusion mismatch and hyperventilation, respectively. Chest X-ray is not usually required for moderate asthma exacerbations unless pneumonia is suspected.
Severe acute asthma
Patients are usually agitated and unable to complete full sentences. Their respiratory rate is usually >30/min and use of accessory muscles is common. Significant tachycardia (pulse rate >120/min) and hypoxia (SaO2 <92% on room air) are usually evident. Chest examination reveals prolonged distant wheeze secondary to severe airflow limitation and hyperinflation; more ominously the chest maybe silent on auscultation. PEFR is usually in the range of 33–50% of predicted. ABGs reveal significant hypoxemia and elevated alveolar–arterial oxygen gradient. PaCO2 may be normal in patients with severe asthma exacerbations. Such finding is an alarming sign, as it indicates fatigue, inadequate ventilation, and pending respiratory failure. Chest radiograph is required if complications are clinically suspected such as pneumothorax or pneumonia.
Life-threatening acute asthma
Patients with life-threatening asthma are severely breathless and unable to talk. They can present in extreme agitation, confusion, drowsiness, or coma. The patient usually breathes at a respiratory rate >30/min and uses their accessory muscles secondary to increased work of breathing. Heart rate is usually >120/min, but at a later stage, patients can be bradycardiac. Patient may have arrhythmia secondary to hypoxia and electrocardiogram (ECG) monitoring is recommended. Oxygen saturation is usually low (<90%) and not easily corrected with oxygen. ABGs are mandatory in this category and usually reveal significant hypoxia and normal or high PaCO2. Respiratory acidosis may be present. PEFR is usually very low (<30% of the predicted). Chest X-ray is mandatory in life-threatening asthma to rule out complications such as pneumothorax or pneumomediastinum. It is important to realize that some patients might have features from more than one level of acute asthma severity. For the patients’ safety, they should be classified at the higher level and managed accordingly.
Initial treatment of acute asthma
After initial assessment of asthma exacerbation, it is recommended to base treatment on severity level [Box 10]. More details of medications are available in Appendix 2.
Moderate asthma exacerbation
Low-flow oxygen is recommended to maintain saturation ≥92%.[198,199] There is evidence that high-flow oxygen may be harmful to some patients.[200] Therefore, it is important to give a controlled dose of oxygen; patients who received 28% oxygen did better than those who received 100% oxygen[200]
Steroid therapy: Oral prednisolone 1 mg/kg to maximum of 50 mg is recommended to be started as soon as possible.[207,208]
Severe asthma exacerbations
Adjusted oxygen flow is recommended to keep saturation ≥92% (avoids excess oxygen)[199,209,210]
Nebulized SABA (2.5–5 mg) are recommended to be repeated every 15–20 min for 1 h, then hourly according to response.[199] Oxygen-driven nebulizers are preferred for nebulizing SABA because of the risk of oxygen desaturation while using air-driven compressors (Evidence A)[207,208,211,212]
Ipratropium bromide is recommended to be added to salbutamol at a dose of 0.5 mg every 20 min for three doses by the nebulized route then every 4–6 h as needed (Evidence B). Alternatively, ipratropium can be administered by MDI at a dose of 4–8 puffs (80–160 mcg) every 20 min, then every 4–6 h as needed[213,214,215,216]
Systemic steroid is recommended to be started as soon as possible (Evidence A). If patient can tolerate orally, oral prednisolone 1 mg/kg to maximum of 50 mg daily is recommended. Alternatively, the following may be prescribed: Intravenous (IV) methylprednisolone 60–80 mg daily in divided doses or IV hydrocortisone 200 mg daily in divided doses[207,217]
If there is no adequate response to previous measures, it is recommended to administer a single dose of IV magnesium sulfate (1–2 g) intravenously over 20 min (Evidence B)[218]
Chest X-ray, electrolytes, glucose, 12-lead ECG, and ABG.
Life-threatening asthma
Patients in this category can progress rapidly to near-fatal asthma, respiratory failure, and death. Hence, an aggressive management approach and continuous monitoring are mandatory.[219] The following steps are recommended for further management:
Consult ICU service. Intubation setting should be readily available
Adequate oxygen flow to keep saturation ≥92%[199]
Deliver nebulized SABA (10 mg) continuously over 1 h (Evidence A).[220,221] Oxygen-driven nebulizers are preferred due to the risk of oxygen desaturation while using air-driven compressors (Evidence A)[211,212]
Ipratropium bromide is recommended to be added to salbutamol at a dose of 0.5 mg every 20 min for three doses by the nebulized route then every 4–6 h as needed (Evidence B). Alternatively, ipratropium can be administered by MDI at a dose of 4–8 puffs (80–160 mcg) every 20 min, then 4–6 h as needed.[213,214,215,216]
Systemic steroid (Evidence A) to be started as soon as possible in one of the following forms: IV methylprednisolone 60–80 mg daily in divided doses or IV hydrocortisone 200 mg daily in divided doses.[207,213,216,217,222,223]
Single dose of IV magnesium sulfate (1–2 g) intravenously over 20 min (Evidence B)[217,223]
Frequent clinical evaluation and CXR, electrolytes, glucose, 12-lead ECG, and ABGs are recommended.
Follow-up after initial treatment
Close evaluation of treatment response is recommended that includes patient's mental and physical status, respiratory rate, heart rate, blood pressure, oxygen saturation, and PEFR. Response to treatment is divided into three categories such as adequate, partial, or poor response [Box 11].
Box 11.
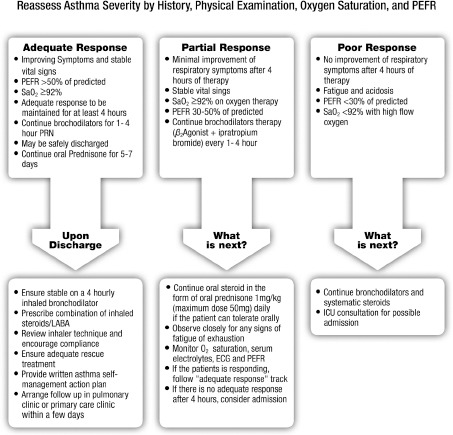
Adjustment of acute asthma treatment in adults and adolescent patients
Adequate response
Adequate response is defined as:
Improvement of respiratory symptoms
Stable vital signs with respiratory rate <25/min and heart rate <120/min
Oxygen saturation ≥92% on room air
PEFR or FEV1 >50% of predicted.
Management: If the above criteria are met and maintained for at least 4 h, the patient can be safely discharged with the following recommendations:
Review and reverse of any treatable cause of the exacerbation
Review of inhaler technique and encourage adherence
Step up of asthma treatment to at least step 3
Prescription of oral steroid for 5–7 days
Adequate SABA on “as needed bases”
A clearly written asthma self-management action plan
A follow-up appointment within 1 week.
Partial response
Partial response is defined as:
Minimal improvement of respiratory symptoms
Stable vital signs with respiratory rate <25/min and heart rate <120/min
Oxygen saturation ≥92% on oxygen therapy
PEFR between 30% and 50% of predicted.
Management: Patients who only achieved partial response after 4 h of the above-described therapy are recommended for the following:
Continue bronchodilator therapy (SABA every 1 h and/or ipratropium bromide), unless limited by side effects (significant arrhythmia or severe hypokalemia)
Continue systemic steroid: IV hydrocortisone 200 mg every 6–8 h, IV methylprednisolone 40 mg every 8 h, or oral prednisolone 1 mg/kg to maximum of 50 mg g daily
Observe closely for any signs of fatigue or exhaustion
Monitor oxygen saturation, serum electrolytes, ECG, and PEFR
Admit to hospital if the patient fails to show adequate response.
Poor response
Poor response is defined as:
No improvement of respiratory symptoms
Altered level of consciousness, drowsiness, or severe agitation
Signs of fatigue or exhaustion
Oxygen saturation <92% with high-flow oxygen
ABGs analysis showing respiratory acidosis and/or rising PaCO2
PEFR of <30%.
Management: Patients showing poor response after 4 h of therapy should have the following recommendations:
Consider ICU admission
Deliver continuous nebulization of SABA, unless limited by side effects
Continue systemic steroid: IV hydrocortisone 200 mg every 6–8 h or IV methylprednisolone 40 mg every 8 h.
Criteria for Intensive Care Unit referral
ICU referral is recommended for patients:
Requiring ventilatory support
Developing acute severe or life-threatening asthma
-
Failing to respond to therapy, evidenced by:
- Deteriorating PEFR
- Persisting or worsening hypoxia
- Hypercapnia
- ABG analysis showing respiratory acidosis
- Exhaustion, shallow respiration
- Drowsiness, confusion, altered conscious state
- Respiratory arrest.
Asthma in special situations
Cough-variant asthma
Patients with cough-variant asthma have chronic cough as their main symptom.[224,225] It is particularly common in children and is often more problematic at night. Other diagnoses considered are drug-induced cough caused by angiotensin-converting enzyme inhibitors, GERD, postnasal drip, eosinophilic bronchitis, and chronic sinusitis. This condition must be also differentiated from eosinophilic bronchitis which is characterized by cough with sputum eosinophilia while spirometry and airway hyper-responsiveness (AH) are normal.[226] Once the diagnosis is established, treatment is recommended with ICS.[227,228]
Rhinitis/sinusitis and nasal polyp
Most asthma patients have coexisting rhinitis or sinusitis and around 40% of patients with rhinitis have asthma.[229] Rhinitis can be classified to allergic or nonallergic. Asking patients about rhinitis symptoms and examination of upper airways is recommended to be part of the routine management of asthma. Treatment with intranasal corticosteroids has been associated with a decrease in asthma hospitalization and ED visits but not asthma control.[230,231]
Exercise-induced bronchoconstriction
Exercise-induced bronchoconstriction (EIB) is common in inadequately controlled asthma patients. However, asthma-like symptoms can sometimes be triggered only by physical activities. Normally, bronchodilation occurs during exercise and lasts for few minutes. In patients with EIB, the initial bronchodilation is followed by bronchoconstriction that generally peaks within 10–15 min after completing the exercise and resolves within 60 min. EIB can be prevented by the use of SABA a few minutes before exercise.[232] A warm-up period before exercise may also reduce EIB symptoms. If this approach does not control the symptoms, the patient is recommended to have maintenance therapy with ICS.[141] Regular use of LTRA may help in this condition especially in children.[141,233]
Aspirin-exacerbated respiratory disease
About 10–20% of adults with asthma suffer from exacerbations in response to ASA or NSAIDs that inhibit cyclooxygenase-1. This condition is more common in patients with severe asthma and poor lung function. The majority of the patients experience first symptoms during their third to fourth decade of life. Once ASA or NSAID hypersensitivity develops, it is present for life. Characteristically, within minutes to 2 h following ingestion of ASA, an acute severe asthma exacerbations develops. It is usually accompanied by rhinorrhea, nasal obstruction, conjunctival irritation, and scarlet flush of the head and neck.[234] A typical history of reaction is considered adequate for diagnosis of ASA-induced asthma. Patients known to have ASA-induced asthma are recommended to avoid all ASA-containing products and NSAIDs. Where an NSAID is strongly indicated, alternative analgesics such as paracetamol are recommended. Prophylactic low-dose ASA is recommended also to be avoided; however, patients for whom ASA is considered essential can be referred to an allergy specialist for ASA desensitization.[235] ASA and NSAID can be used in asthma patients who do not have ASA-induced asthma.[236] Montelukast may be protective against this type of asthma and, therefore, is recommended to be part of the treatment regimen.[237]
Gastroesophageal reflux disease
GERD is more prevalent in patients with asthma compared to the general population. The mechanisms by which GERD worsens asthma include vagal mediated reflex and also reflux secondary to micro-aspiration of gastric contents into the upper and lower airways.[238] All patients with asthma should be questioned about symptoms of GERD. If symptoms are present, a trial of anti-GERD measures (including a proton pump inhibitor) is recommended for 6–8 weeks.[239,240,241] Benefit of proton pump inhibitors is limited to patients with symptomatic GERD and nighttime respiratory symptoms. Of note, patients with asymptomatic GERD do not benefit from GERD therapy (Evidence A).[242]
Pregnancy
The course of asthma during pregnancy is unpredictable; however, one-third of pregnant asthmatics may have a worsening of their asthma control.[243] Maintaining adequate control of asthma during pregnancy is essential for the health and wellbeing of both the mother and her baby. Occurrence of Asthma exacerbations during the first trimester of pregnancy significantly increase the risk of a congenital malformation.[244] Identifying and avoiding triggers are recommended as the first step of therapy for asthma during pregnancy. Treatment is recommended to take the same stepwise approach as in the nonpregnant patient. Salbutamol is the preferred SABA due to its excellent safety profile. ICSs are the preferred treatment for long-term control.[245] ICS, theophylline, antihistamines, B2-agonists, and LTRA are generally safe, and they have not been shown to increase the risk of fetal abnormalities.[246,247] Prolonged use of systemic steroids may be associated with pregnancy-related complications, especially in the first trimester.
Pregnant women are recommended to receive the same drug treatment for acute asthma as nonpregnant patients (Evidence B), including systemic steroids if indicated (Evidence C).[243,248,249,250,251] Fetal monitoring is recommended in severe asthma exacerbation. If anesthesia is required during labor, regional anesthesia is recommended whenever possible (Evidence C).[252] The use of prostaglandin F2α may be associated with severe bronchospasm and should be avoided, if possible (Evidence D). If asthma is well controlled during pregnancy, acute asthma is rare during labor. As asthma treatment is safe in pregnancy, patients are recommended to continue their usual asthma medications during pregnancy and in labor. In the absence of acute severe asthma, reserve cesarean section for the usual obstetric indications. Pregnant asthma patients should be encouraged to breastfeed after delivery and to continue their usual asthma medications during lactation.[253,254,255]
Occupational asthma
All patients with asthma should be asked about their work history and exposures for possible related causal factors. A simple screening test is to ask the patient if their symptoms improve if they are away from work.[256] Once identified, early identification and elimination of occupational sensitizers and removal of patients from further exposure are an essential aspect of management. Patient with suspected or confirmed occupational asthma is recommended for referral to an asthma expert for assessment and advice because of the legal implications of the diagnosis.[257,258]
Difficult to treat asthma
DTA carries several names; each one points to an aspect of the disease.[259] Chronic severe asthma, steroid-dependent asthma, difficult to control asthma, and refractory asthma are some of these terminologies. It is simply defined as persistence of asthma symptoms in patients who require step 4 or step 5 level of therapy. DTA probably accounts for 5–10% of adult asthma, but the health cost is disproportionally high.[260] Morbidity and mortality are also higher compared to regular asthma patients because of increased side effects of treatment and much more frequent exacerbations.[261,262] Before labeling a patient as a case of DTA, the following are recommended:[83,263,264,265,266,267]
Ensure that the patient is adherent to medications with a good inhalation technique
Misdiagnosis where the problem is not bronchial asthma to start with but another respiratory pathology that is not appropriately addressed, for example, bronchiectasis, endobronchial tumors, vocal cord dysfunction, allergic bronchopulmonary aspergillosis, or Churg–Strauss syndrome[265,268]
Comorbidity that worsens bronchial asthma and makes it difficult to manage (e.g. chronic sinusitis, GERD, sleep apnea syndrome, obesity, and congestive heart failure [CHF])[269]
Confounding factors (e.g. presence of allergens at home or work, active or passive smoking, or psychosocial problems).[265]
A significant percentage of patients with DTA do not respond adequately to high-doses of ICS and other controller therapy, thus, they need frequent or continuous oral steroid therapy to achieve a reasonable response.[270] Such control may be lost when oral steroid is discontinued. Patients may differ in the degree of their responsiveness to oral steroids.[271] Some patients may fail to improve their FEV1 by more than 15% following treatment with oral prednisolone (30–40 mg) daily for 2 weeks, a condition called “corticosteroids-resistant asthma.[272,273]
It is strongly recommended to refer DTA patients to an asthma specialist. As it may be difficult to achieve full control in some patients, the aim of the treatment in this situation is to reach the best possible control.[274] After dealing with all comorbidities that could have made asthma difficult to control, maximum therapy is recommended (i.e., step 5), which may include combination therapy of high-dose ICS/LABA, LTRA, and long-acting anti-muscarinic (cholinergic) agent (LAMA).[275] Anti-IgE treatment (omalizumab) is recommended if the patients fulfill the criteria for this treatment.[276,277] If oral steroids are necessary, it is recommended to use the lowest possible dose and to shorten the duration as possible.[278] In this situation, osteoporosis prophylaxis is recommended. New modalities of drug treatment are promising and may help to further control DTA. These modalities need to be considered by a specialized physician in asthma management. Some of these modalities are:
Mepolizumab is a humanized immunoglobulin G (IgG) monoclonal antibody specific to interleukin-5 (IL-5) and preventing it from binding to its receptor on the surface of the eosinophils. It has been shown to reduce asthma exacerbations and improves asthma control in patients with refractory eosinophilic asthma.[279] It is now approved for use in patients above 18 presenting with eosinophilic asthma at a dose of 100 mg via subcutaneous injections or 75 mg intravenously every 4 weeks[280]
Bronchial thermoplasty is a novel treatment modality that utilizes radiofrequency energy to alter the smooth muscles of the airways. However, in selected patients with moderate to severe persistent asthma, it has shown to improve various measures of asthma, including FEV1, quality of life, asthma control, exacerbations, and use of rescue medications.[281,282,283]
Asthma-chronic obstructive pulmonary disease overlap syndrome
In adult patients older than 40 years with a chronic airways disease, COPD becomes more common than asthma. Distinguishing asthma from COPD becomes more difficult as many patients may show features of both diseases. This has been called the asthma-COPD overlap syndrome (ACOS). ACOS is a unique complex syndrome sharing features of both COPD and asthma. At this stage, there is no formal definition of ACOS as there is inadequate data to describe its features, characteristics, and its optimal therapeutic intervention.[31] However, when a patient has features of both asthma and COPD, the diagnosis of ACOS should be considered.
ACOS has been estimated to account for approximately 15–25% of the obstructive airway diseases in adults and patients may experience worse outcomes compared with asthma or COPD alone.[31] Patients with ACOS have the combined risk factors of smoking and atopy. They are generally younger than patients with COPD and have frequent exacerbations, poor quality of life, a more rapid decline in lung function, higher mortality, greater health care utilization and low quality of life; compared to patients with COPD alone.[284,285,286]
Spirometry is required to confirm the diagnosis of chronic airflow limitation. Postbronchodilator FEV1/forced vital capacity of <0.7 is usually present and postbronchodilator increase in FEV1 by >12% and 200 mL from baseline is compatible with diagnosis of ACOS. However, spirometry alone has limited value in distinguishing between asthma, COPD, and ACOS.
If the initial assessment suggests asthma or ACOS or there is uncertainty about the diagnosis of COPD, it is prudent to start treatment for asthma (ICS ± LABA) until further investigation has been performed to confirm or exclude this diagnosis. However, it is important that patients should not be treated with a LABA alone if there are features suggestive of asthma.[287,288,289] Treatment of ACOS is recommended to include advice about other therapeutic strategies including smoking cessation, pulmonary rehabilitation, vaccinations, and treatment of comorbidities.
Management of asthma in children
Asthma represents the commonest chronic illness of childhood.[1,290] It is also considered a leading cause for childhood morbidity as measured by school absences, ED visits, and hospitalizations.[291] From the prospective of both patient and society, the cost of not treating asthma is higher than the cost of asthma treatment.[70,292]
Asthma diagnosis in children
Accurate diagnosis of asthma in children is crucial to prevent inappropriate management and reducing morbidity and mortality due to under-or over-diagnosis.[293,294] Therefore, asthma diagnosis in children should be based on a careful clinical assessment that includes recurrent or chronic symptoms related to airway obstruction, such as wheezing, coughing, night symptoms, activity limitation, and shortness of breath. These symptoms typically result from AH or various stimuli that would be reversible either spontaneously or after receiving a bronchodilator. The diagnosis can be further be supported by the presence of atopy, early sensitization, and a family history of atopy. Whenever possible, spirometry is recommended to be performed to show reversibility of airway obstruction after bronchodilator therapy.[295] In general, spirometry can be performed in children aged ≥5 years. It is preferably planned when the initial diagnosis is made and after 3–6 months of controller therapy initiation with subsequent follow-up assessment. Box 12 presents a summary of symptoms and signs suggestive of the diagnosis of asthma in children.
Box 12.
Diagnosis of asthma in children
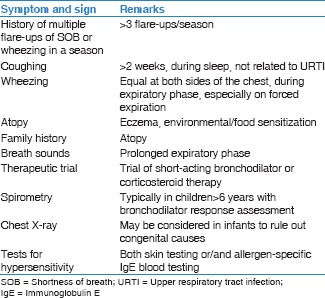
Asthma mimics should be suspected when any of the following is present: Failure to thrive, onset of symptoms during infancy, vomiting associated with respiratory symptoms, continuous wheezing, failure to respond to asthma controller medication, clubbing or focal auscultation signs, and symptoms that are not associated with typical triggers. Clinical suspicion of asthma mimics is an acceptable indication for chest X-ray in a child suspected of having asthma; however, a routine chest X-ray is not recommended to be part of the initial routine work up of asthma in children.[296]
In preschool children, asthma diagnosis and management differs from that of older children and adolescent in many ways. Early childhood wheezing can evolve to different asthma phenotypes that can have variable response to standard therapy.[297] In addition to the diagnosis of asthma, wheezing in preschool children can be due to unique differential diagnoses (e.g., congenital defects, infections especially viral bronchiolitis, bronchopulmonary dysplasia, and cystic fibrosis). In this age group, asthma diagnosis represents a challenging clinical judgment due to the lack of objective assessment (e.g., pulmonary function test or biomarkers). “Reactive airway disease” as a terminology is discouraged as it can restrain full clinical assessment and proper management of asthmatic children in this age group.[295,298,299]
Asthma phenotypes in children
Based on several longitudinal studies, wheezing has been categorized epidemiologically into transient and persistent wheeze phenotype. It is also categorized based on symptoms into episodic/viral induced and multi-trigger wheeze phenotypes.[300,301] Different responses to treatment and variable outcomes have been attributed to phenotype heterogeneity, overlap, and instability over time. On contrary, major factors that may predict persistent symptoms are allergic disease, reduced lung function, viral respiratory infection, and bacterial colonization in infancy. Asthma wheeze phenotype in children has been classified as:[300,302]
Early transient wheezing before the age of 3 years with resolution by the age of 6 years
Persistent wheezing that starts before the age of 3 years and continue after the age of 6 years
Late-onset wheezing between 3 and 6 years of age.
The allocation of children into these categories remains a subject of debate, as their clinical usefulness is still under investigation.[303]
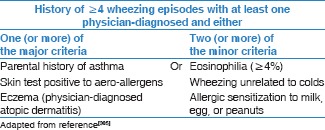
Prediction of asthma in preschool children
For early identification of the risk for persistent asthma among preschool children, SINA expert panel recommends the utilization of the modified asthma predictive index (modified-API). This tool is a clinical scoring instrument that can be used to predict whether a child with intermittent wheezing before the age of 3 years will develop persistent asthma pattern during school-age years [Box 13].[304,305] Children with a history of four or more wheezing exacerbations (at least one is diagnosed by physician) and either one major or two minor criteria at 3 years of age will have 4–10 fold increase in the risk of having asthma during later childhood. On other side, children with negative modified-API will have 95% chance of outgrowing their asthma later on life.[306]
Box 13.
Modified asthma predicative index
Principles of asthma assessment in children
Strategy of asthma management in children
The long-term goals of asthma management in children are not different from those of adults [Box 5].[70] Asthma management requires effective partnership between patients/caregivers and their healthcare providers.[307] Once established and strengthened, this relationship will positively impact asthma control. The asthma management strategy should include:
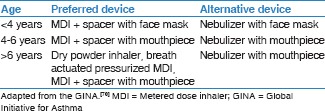
Assessment of asthma control combined with proper treatment: This implies a periodical assessment of asthma control combined with adjustments (if needed) of treatment based on the level of control. It is strongly recommended to use asthma treatment in a stepwise approach with the ultimate goal of achieving “optimal” control with “minimal” amount of medications and dosage.[308] Adherence to the prescribed medications and the proper use of their devices are recommended to be addressed before any modification of the treatment plan. It is extremely important to select the best device for optimal treatment delivery [Box 14]
Patient education:Patient education is recommended to be an integral part of asthma management strategy in children. It is recommended to involve the basic knowledge of the disease pathophysiology, identifying and avoiding triggering factors, environmental controls (especially cigarette smoke exposures), proper use of treatment devices, and recognition of worsening asthma symptoms and the optimal time to seek advice.[309,310] Proper asthma education can lead to a significant reduction in ED visits and hospitalizations, improve self-management of asthma exacerbations, and an overall reduction in the cost of asthma care[311]
Action plan:An action plan that includes medications, doses, and technique should be provided to patients and their caregivers. The action plan is also recommended to include information for patient and caregiver on how to recognize worsening of asthma symptoms and advice of treatment modification in these situations [Box 15]
Prevention:Asthma exacerbations can be triggered by a variety of factors including Allergens, viral infection, pollutants, and drugs. Eliminating these exposures improves the control of asthma and reduces medication needs. Parents/caregivers of children with asthma should be strictly advised not to smoke at home.[70,312] Breastfeeding and Vitamin D supplementation may decrease the chance of developing early wheezing episodes[313] while probiotics benefit is still doubtful in preventing allergic disease.[314,315]
Box 14.
Choosing an inhaler device for children
Box 15.
Components of asthma management action plan
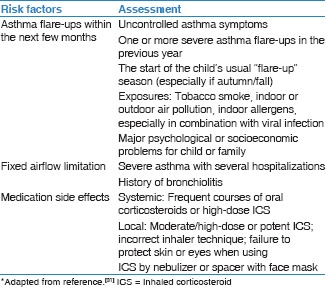
Asthma control level
Asthma control is a reflection of the adequacy of management by describing the clinical status of a child as controlled, partially controlled, or uncontrolled. Focusing on asthma control may improve patient perceptions and expectations that improve symptoms reporting by children and their caregivers and subsequently treatment decisions by clinicians.[71] In children, assessment of asthma control is recommended to cover two domains:[287]
Assessing future risk of adverse outcomes: This achieved by assessing future risk of exacerbations, fixed airflow obstruction, and adverse effect of medications [Box 16]
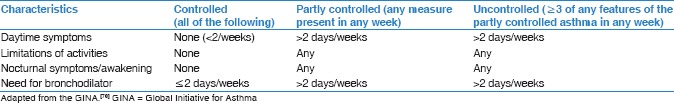
Assessing symptom control: Asthma symptom control has been estimated by physician assessment during clinic visit and/or perception of patients and their caregivers toward asthma control. During each clinic visit, the physician is recommended to utilize GINA criteria for asthma control [Box 17] to assess disease control. Different numerical tools have been developed and validated to objectively assess asthma control utilizing patients and their caregiver perception. However, as these tools have some limitations, they are recommended to be used as a complimentary tool rather than replacing physician assessment.[316]
Box 16.
Assessment of future risk of adverse outcomes of asthma in children*
Box 17.
Levels of asthma control in children
SINA expert panel recommends the following questionnaires to be completed by patients and/or their caregiver before physician evaluation based on the age of the child:
-
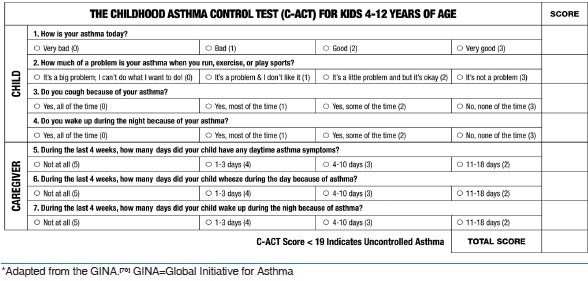
Age group 5–11 years: The childhood-ACT (C-ACT)
The C-ACT is a validated test for 4–12 years old children [Box 18]. C-ACT is a two-part questionnaire with a total of seven questions. The first part is to be answered by the patient and the second part by the caregiver. The final C-ACT score is made up of the sum of the scores of the two parts, ranging from 0 (poorest asthma control) to 27 (optimal asthma control). A score of ≤19 points suggests that a child's asthma is not adequately controlled[317]
-
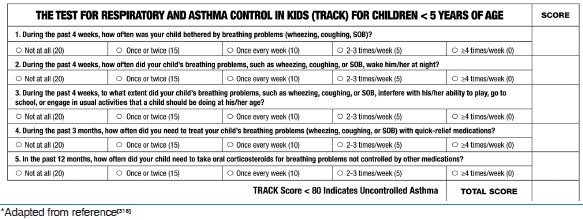
Age group <5 years: The Respiratory and Asthma Control in Kids Questionnaire (TRACK)
The TRACK is a validated test for children <5 years [Box 19]. It is a 5-item standardized questionnaire, with four questions that address the impairment domain and one question that addresses the risk domain of asthma control. Each item is scored from 0 to 20 points on a 5-point Likert-type scale for a total score ranging from 0 to 100. Higher scores would indicate better respiratory and asthma control; a score of <80 points suggests that a child's asthma is not controlled.[318]
Box 18.
The Childhood Asthma Control Test*
Box 19.
The Test for Respiratory and Asthma Control in Kids*
Outpatient treatment of asthma in children
Treatment of asthma should be adjusted continuously based on asthma control. If current treatment has failed to achieve control, then treatment should be stepped up until control is achieved. Whenever control is maintained for at least 3 months, then treatment can be stepped down. This stepwise approach is essential to maintain optimum control with lowest step to maximize safety and minimize cost. Though the stepwise approach is stratified into age categories (<5 years and 5–11 years), there are common concepts in the two age groups that include:
For a child seen in the clinic for the first time while on controller treatment, the managing physician should ensure that the child is receiving the appropriate treatment based on recommendations given in the section on treatment initiation
Assessment of adherence, proper device use, control of environment, and confirmation of the diagnosis, especially if there is a failure to respond to therapy is recommended each time before treatment adjustments
ICS is considered the most effective first-line maintenance monotherapy for childhood asthma (Evidence A)[319,320]
Chronic use of ICS for more than 3 months in prepubertal-aged children can suppress growth velocity; however, this effect is dose dependent. Asthmatic children when treated with low-dose ICS attain normal adult height but at a later age (Evidence A).[321,322] Any potential adverse effects of ICS need to be weighed against the well-established benefit to control persistent asthma. More details of the use of ICS in children is available in Appendix 2
There are insufficient data to recommend short courses of high-dose ICS in children with mild intermittent asthma exacerbations (Evidence B).[323] Safety of this approach has not been established
Children with frequent or severe asthma exacerbations are recommended to receive regular treatment with ICS (Evidence A)[324]
The clinical benefits of intermittent inhaled or systemic steroid for children with intermittent and viral-induced wheezing remain controversial. This practice is recommended to be discouraged until clear evidence-based practices are available on this strategy of asthma management (Evidence C)[325,326]
LTRAs can reduce viral-induced asthma exacerbations in children aged 2–5 years with history of intermittent asthma (Evidence B)[327]
Oral bronchodilators therapy is not recommended due to slower onset of action and higher side effects[328]
LABA should not be used alone as maintenance monotherapy in children (Evidence A)[329]
LABA should be used only in combination with ICS. There are different combinations available in the Saudi market [Appendix 2]
There is no evidence to support the use of LABA in children <5 years
There is no evidence to support the use of LAMA in children <12 years
There is a growing evidence to support the use of anti-IgE in children 6–12 years of age who fulfill the following criteria (Evidence A): Severe persistent allergic asthma with frequent daytime symptoms or night-time awakenings, and who have multiple documented severe asthma exacerbations despite daily high-dose ICS plus LABA.[330,331] However, this line of management is recommended to only be restricted to physicians specialized in asthma (Evidence C)[332,333]
As inhalers are the main method of delivering medications, it is recommended to choose the appropriate device [Box 14]. Use of valved-spacer, with mouthpiece when possible, is recommended when an MDI is prescribed (Evidence B).[334] Breath-actuated devices (e.g., dry powder inhalers) represent an effective and simpler option for maintenance therapy in children ≥5 years of age (Evidence C).[335,336] For more information about medications, refer to Appendix 2
Nebulizers are not superior to MDI delivered by spacer in both acute and chronic asthma management (Evidence A).[337]
In these guidelines, the SINA expert panel ensures consistency in the approach of asthma in adults, adolescents, and children. Therefore, outpatient treatment will be described in three phases such as initiation, adjustment, and maintenance. The recommendations in the following sections are further stratified based on age groups <5 years and 5–11 years.
Initiation of asthma treatment in children
Before initiating asthma treatment in children, it is recommended to document important findings obtained during the initial clinical assessment, such as the status of asthma control and risk factors, obtaining C-CAT score for children aged 5–11 years, and TRACK score for children <5 years. It is also recommended to provide teaching of inhalers technique, action plan and ensure that patient has a follow-up visit. SINA expert panel recommends the following for initiation of treatment based on the common clinical scenarios described below:
-
A child with minimal symptoms and use of SABA (less than twice a week for both) that qualify for a controlled status based on physician assessment and is complemented with a C-ACT score of ≥20 for a child aged 5–11 years or TRACK score of >80 for a child aged <5 years, the following actions are recommended:
- Initiation of treatment with SABA on “as needed bases”[338]
- Initiation of treatment with low-dose ICS for a child with a history of asthma exacerbation in the past year or has ever been admitted to ICU (Evidence D).
-
A child with more symptoms and use of SABA (more than twice a week for both) that qualify to partially controlled status based on physician assessment and is complemented with a C-ACT score of ≤19 for a child aged 5–11 years or TRACK score of ≤80 for a child aged <5 years, the following actions are recommended:
- For a child with early signs of asthma exacerbation at presentation, a short course of oral steroids may be considered in addition to a low-moderate of ICS
-
For a child <5 years of age with:
Adjustment of asthma treatment for children
Adjustment of therapy is recommended after 1–3 months depending on the level of asthma control upon presentation and the C-ACT score for children aged 5–11 years or TRACK score for children aged <5 years. Patient should be clinically assessed regarding medications and doses, compliance to treatment, and accuracy of inhalers technique [Boxes 20 and 21]. Based on clinical assessment and the level of asthma control, the followings are recommended:
Box 20.
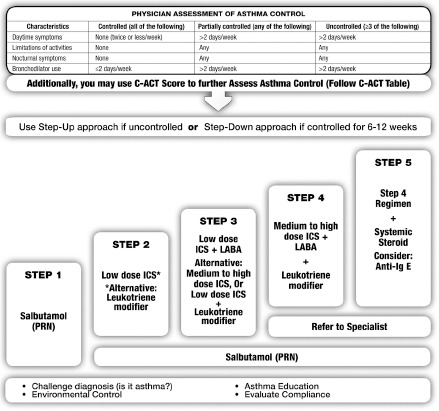
Outpatient management of asthma in children aged 5–11 years
Box 21.
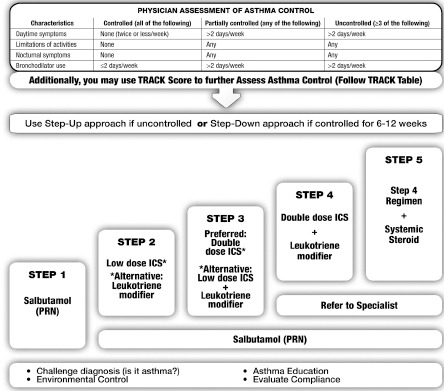
Outpatient management of asthma in children aged <5 years
A child with uncontrolled asthma: Escalation of treatment to at least the next step. Uncontrolled status is determined based on physician assessment complemented by a C-ACT score of ≤19 for a child aged 5–11 years or TRACK score of ≤80 for a child aged <5 years
A child with controlled asthma: Treatment is recommended to be maintained at the same step; however, stepping down may be considered during low seasons for asthma exacerbations. Controlled status is determined based on physician assessment complemented by a C-ACT score of ≥20 for a child aged 5–11 years or TRACK score of >80 for a child aged <5 years.
SINA expert panel recommends the following concepts of treatment adjustment based on age in the following section.
Children aged 5–11 years
A child is not controlled at step 1: The preferred option is to start low-dose ICS (step 2) (Evidence A) [Box 20][319,320]
A child with asthma control is not achieved at step 2: Escalation of treatment to step 3 by adding LABA to low-dose ICS (Evidence A).[126] Alternatively, LTRA can be added to low-dose ICS or the dose of ICS escalated to moderate dose (Evidence A)[350,351,352,353,354,355]
A child is not controlled at step 3: It is recommended to change the combination inhaler to medium dose of ICS/LABA (step 4). LTRA may be added to this combination.
Whenever there is a difficulty to control asthma at step 4, it is strongly recommended to refer patient to a physician specialized in asthma.
Children aged < 5 years [Box 21]
A child is not controlled at step 1: The preferred option is to start low-dose ICS (step 2) (Evidence A)[319,320]
A child with asthma control is not achieved at step 2: It is recommended to escalate treatment to step 3. The recommended option is to double the dose of ICS (Evidence A).[353,356,357] Alternatively, adding LTRA to low-dose ICS is another option although this is considered less-effective[348,349]
A child is not controlled at step 3: It is recommended to escalate treatment to step 4 by the addition of LTRA to moderate dose ICS (Evidence B).[358,359,360]
It is recommended to provide the caregiver an asthma action plan and a follow-up visit in 1–3 months depending on clinical status. Uncontrolled asthma in preschool children can lead to developmental disadvantages due to the negative impact of uncontrolled asthma on their social interaction and sleep. Caregivers of preschool children should be educated that asthma control is an achievable target, and affected children should not be prevented from engagement in age-appropriate activities.
Maintenance of asthma treatment for children
Upon follow-up, it is recommended to perform a full clinical assessment including asthma control status and obtaining C-ACT score for children aged 5–11 years or TRACK score for children aged < 5 years. Based on clinical assessment and asthma control status [Boxes 20 and 21], SINA expert panel recommends the following:
Step up treatment for children who are uncontrolled based on physician assessment and complemented by a C-ACT score of ≤19 for a child aged 5–11 years or TRACK score of ≤80 for a child aged <5 years. It is recommended to rule out any modifiable factors preventing reaching optimal asthma control
Maintain treatment for children who reached controlled status based on physician assessment complemented by a C-ACT score of ≥20 for a child aged 5–11 years or TRACK score of >80 for a child aged <5 years
Consider stepping down treatment for children who are controlled for at least 3 months.
Reduction in therapy should be gradual and closely monitored based on clinical judgment complemented by either C-ACT score or TRACK score. In addition, close monitoring upon treatment stepping down is recommended for patient who has risk of asthma exacerbation especially during seasonal variation or for those with prior acute asthma exacerbation in the past year or history of ICU admission.
SINA expert panel recommends the following concepts for treatment stepping down based on age.
Children aged 5–11 years [Box 20]
If the patient is on ICS as monotherapy, the dose of ICS may be reduced by 25–50% every 3–6 months to the lowest possible dose that is required to maintain control (Evidence B),[159,160,161] It should be clearly explained to the patient and/or caregiver that asthma control may deteriorate if treatment is abruptly discontinued.[162] In such a situation, an action plan that contains instruction on resuming controller therapy if asthma symptoms recurred is recommended to be provided to patients and their caregiver
If the patient is on combination of ICS/LABA at step 3 or 4, abrupt discontinuation of LABA may lead to deterioration of asthma control[163]
If the patient is on a combination of ICS with LABA or LTRA, taper ICS to the lowest possible dose (Evidence B).[164,165] If control is maintained, LABA or LTRA may then be discontinued (Evidence D)[164]
For significant local side effects of ICS, consider a change in therapy, reduction in the dose or frequency of ICS (if possible), advice for a vigorous mouth washing after inhalation, enforce use of MDI with spacer, and/or use of appropriate local antifungal therapy for severe oral thrush[166]
For patients on continuous oral steroids, the dose is recommended to be tapered to the lowest dose and preferably to every other day (Evidence D).
Children aged <5 years [Box 21]
The need for continuation of ICS should be regularly assessed as wheeze remits in a significant portion of children[361]
If the patient is on ICS as monotherapy, the dose of ICS may be reduced by 25–50% every 3–6 months to the lowest possible dose that is required to maintain control (Evidence B),[159,160] It is recommended to be clearly explained to the caregiver that asthma control may deteriorate if treatment is abruptly discontinued.[162] if asthma symptom recurs, an action plan that contains instruction on resuming controller therapy is recommended to be provided to patients and their caregiver
For significant side effects, consider a change in therapy, reduction in the dose or frequency of ICS (if possible), advice for a mouth washing after inhalation if possible, enforce use of MDI with spacer, and/or use of appropriate local antifungal therapy for severe oral thrush[166]
Uncontrolled asthma in preschool children can lead to developmental disadvantages due to the negative impact of uncontrolled asthma on their social interaction and sleep. Caregivers of preschool children are recommended to be educated that asthma control is an achievable target, and affected children should not be prevented from engagement in age-appropriate activities.
Referral to an asthma specialist
Referral to an asthma specialist for consultation or co-management is recommended in the following situations:
There is uncertainty regarding the diagnosis
There is difficulty achieving or maintaining control of asthma
Immunotherapy or omalizumab is being considered
The patient requires step 4 care or higher
The patient has had an asthma exacerbation requiring a hospitalization.
Management of acute asthma in children
Early recognition of acute asthma
Recognition of early signs of acute asthma is essential, especially for those <5 years. Early symptoms of acute asthma include (Evidence D):
An attack of shortness of breath with wheeze or increase of shortness of breath with wheeze
Cough, especially at night
Impairment of daily activity
An increased need for or poor response to SABA
For a child <2 years, the presence of lethargy and poor feeding should raise the suspicion of acute asthma exacerbation.
In a child aged 2–5 years, the combination of the above features can predict approximately 70% of acute asthma exacerbations with low false positive rate.[362] Moreover, upper respiratory tract infection may frequently precede acute asthma exacerbation in children. Clinical assessment is essential in children as the utilization of objective measure such as PFT is problematic, especially in the younger age groups.
Initial management of acute asthma at home
SINA expert panel recommends management of a child with asthma to include an action plan that enable the caregiver to recognize worsening of asthma and the advice for initial treatment (Evidence D). The action plan [Box 15] is recommended to include the features that mandate the need for urgent medical care that includes acute distress of the child, difficulty to complete few words in one breath, and poor response to SABA treatment at home.
In the case of acute exacerbation, initial management at home by the caregiver should be started with salbutamol inhaler 2-4 puffs by a spacer that may be repeated every 20 min for a total of 3 doses. If the child improves, asthma therapy is recommended to be stepped up as per instructions in the action plan (see above under adjustment of asthma treatment for children) and medical advice should be sought as soon as possible. If the child does not adequately improve within or after the initial period, urgent medical care is recommended.
Assessment of asthma severity in the emergency department
Assessment of acute asthma severity in children has an important role in various components of acute asthma management such as Pharmacological interventions, need for hospitalization, and need for ICU admission. The assessment of acute asthma severity in young children is also important for clinical decision-making and evaluation of treatment effectiveness.[71,363,364,365,366,367,368,369,370,371,372,373] This is supported by the fact that PFT measurement is not feasible as more than half of asthma exacerbations in children presented to EDs are of preschool-aged children.[364]
The Pediatric Respiratory Assessment Measure (PRAM) has been found to be feasible, valid, responsive, and reliable tool to determine acute asthma severity in children aged 2–17 years.[364,374] PRAM represents a useful means to record clinical signs in a standardized fashion [Box 22].[71] PRAM score is a 12-point score consisting of oxygen saturation, suprasternal retractions, scalene muscle contraction, air entry, and wheezing.[371] Clinical pathways based on PRAM for inpatient asthma management has been shown to decrease the length of stay and bronchodilator use with no adverse outcomes or increased acute care encounters.[375,376] SINA expert panel recommends measuring PRAM score for asthmatic patients in emergency as it can categorize the risk of hospitalization:
Box 22.
The Pediatric Respiratory Assessment Measure score
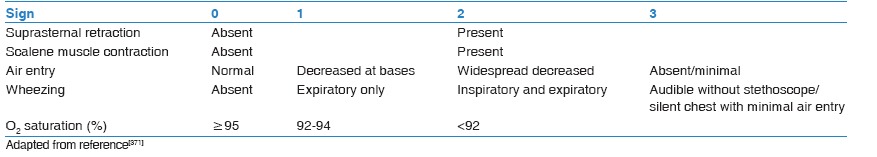
Total score of 1–3: Low risk (<10%) of hospital admission
Total score of 4–7: Moderate risk (10–50%) of hospital admission
Total score of 8–12: High risk (>50%) of hospital admission.
Management of acute asthma in the emergency department
After performing the necessary clinical assessment, SINA expert panel recommends the utilization of PRAM as a tool to assess patients in ED and guide further management. PRAM score should be obtained at the initial assessment and after initiation of treatment as well. In addition, managing physician is recommended to be aware of the following clinical features of severe or life-threatening asthma that require immediate medical attention:
Child is unable to speak or drink
Central cyanosis
Confusion or drowsiness
Significant subcostal or subglottic retraction
Oxygen saturation <92%
Silent chest on auscultation
Tachycardia.
Implementation of clinical pathway that utilizes PRAM score for acute asthma management in children with moderate to severe asthma exacerbations markedly decrease the rate of hospitalization without increasing the rate of return to emergency care (Evidence B) [Box 23].[376,377,378,379] This has been supported by a study showing that PRAM score after 3 h of initial management was associated with a significant improvement in the prediction of admission rate compared to PRAM at triage.[374]
Box 23.
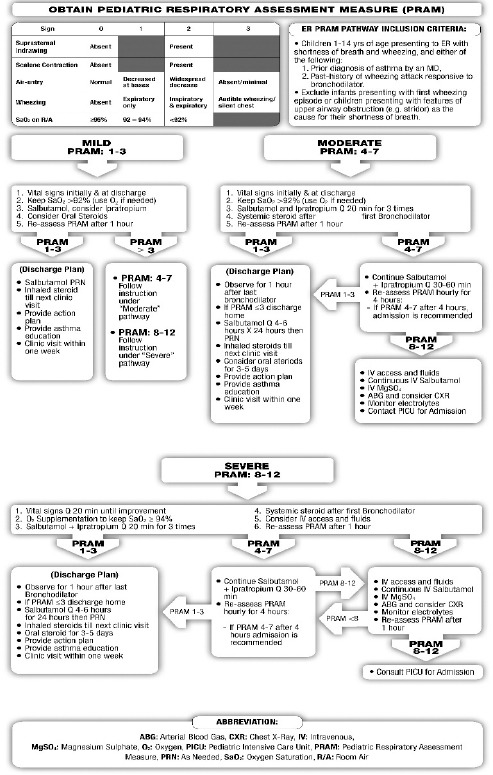
Assessment and treatment of acute asthma in children
Viral infection is the usual cause of asthma exacerbations in children, and thus routine use of antibiotics is strongly discouraged.[380] Antibiotics should only be used when pneumonia or bacterial bronchitis are clinically suspected.[377,378]
SINA expert panel recommends managing asthma based on PRAM score obtained at initial assessment:
Mild - Pediatric Respiratory Assessment Measure score of 1–3
-
Management:
- Obtain vital signs initially and at discharge
- Keep Saturation ≥92% with the appropriate dose of oxygen, if necessary
- Salbutamol (<20 kg: 5 puffs by MDI/spacer or 2.5 mg by nebulizer, ≥20 kg: 10 puffs by MDI/spacer or 5 mg by nebulizer-titrate MDI dose based on response). Physician can consider the addition of ipratropium bromide (4 puffs by MDI/spacer or 250 mcg by nebulizer) every 20 min for the 1st h only.[381] In mild cases, SABA with spacer are not inferior to nebulized SABA[337,382]
- Consider oral steroids (prednisolone 1–2 mg/kg up to a maximum dose as the following: 20 mg for children <2 years, 30 mg for children 2–5 years, and 50 mg for children 5–12 years)[223]
- Re-assess PRAM after 1 h.
-
Management after initial treatment based on PRAM score:
- PRAM score is 1–3: The child may be discharged on salbutamol inhaler with a spacer and ICS if the patient is not already on controller treatment. It is recommended to offer the child an action plan, education on inhalers technique, and a follow-up visit within 1 week to the appropriate clinic
- PRAM is score 4–7: Treat as a moderate asthma exacerbations (see below)
- PRAM is score 8–12: Treat as a severe asthma exacerbations (see below).
Moderate - Pediatric Respiratory Assessment Measure score of 4–7
-
Management:
- Obtain vital signs
- Keep Saturation ≥92% with the appropriate dose of oxygen, if necessary
- Salbutamol (<20 kg: 5 puffs by MDI/spacer or 2.5 mg by nebulizer, ≥20 kg: 10 puffs by MDI/spacer or 5 mg by nebulizer-titrate MDI dose based on response) and ipratropium bromide (2 puffs 80 mcg or 250 mcg by nebulizer every 20 min for the 1st h only).[381,382,383] This combination has been shown to be effective in this situation (Evidence B)[382]
- Reassess PRAM after 1 h
- If PRAM score after 1 h is 1–3, observe for another hour.
-
Management after initial treatment based on PRAM score:
- PRAM score is 1–3: The child may be discharged on salbutamol inhaler with a spacer and ICS if the patient is not already on controller treatment. Oral steroids may be considered (oral prednisolone up to a maximum dose as the following: 20 mg for children <2 years, 30 mg for children 2–5 years, and 50 mg for children 5–12 years).[207,223] It is recommended to offer the child an action plan, education on inhalers technique, and a follow-up visit within 1 week to the appropriate clinic
- PRAM score is 4–7: It is recommended to continue on treatment with salbutamol and ipratropium bromide every 30–60 min. It is also recommended to assess PRAM score hourly. If PRAM score improves to 1–3, the child can be managed as above. If PRAM score does not improve, admission is recommended
- PRAM score is 8–12: Special care and frequent monitoring are needed. IV access is recommended to be established, and appropriate IV fluids started. IV salbutamol (1 mcg/kg/min then titrate based on response for a maximum dose of 10 mcg/kg/min) and IV magnesium sulfate (single dose of 40 mg/kg to the maximum of 2 g by slow IV infusion) might also be considered.[384,385] ABG, CXR, and electrolyte are recommended to be obtained, and the pediatrics critical care or equivalent service must be consulted.
Severe - Pediatric Respiratory Assessment Measure score of 8–12
-
Management:
- Obtain vital signs every 20 min till improvement
- Keep Saturation ≥94% with the appropriate dose of oxygen if necessary
- Salbutamol (<20 kg: 5 puffs by MDI/spacer or 2.5 mg by nebulizer, >20 kg: 10 puffs by MDI/spacer or 5 mg by nebulizer-titrate MDI dose based on response) and ipratropium bromide (2 puffs 80 mcg or 250 mcg by nebulizer every 20 min for the 1st h only).[381,382,383] This combination has been shown to be effective in this situation (Evidence B)[382]
- Re-assess PRAM after 1 h
- Consider IV access and appropriate IV fluids
- If PRAM score after 1 h is 1–3, Observe for another hour.
-
Management after initial treatment based on PRAM score:
- PRAM score is 1–3: The child may be discharged on salbutamol inhaler with a spacer and ICS if the patient is not already on controller treatment. Oral steroids may be considered (oral prednisolone up to a maximum of 20 mg for children <2 years, 30 mg for children 2–5 years, and 50 mg for children 5–12 years).[207,223] It is recommended to offer the child/care giver an action plan, education on inhalers technique, and a follow-up visit within 1 week to the appropriate clinic
- PRAM score is 4–7: It is recommended to continue on treatment with salbutamol and ipratropium bromide every 30–60 min. It is also recommended to assess PRAM score hourly. If PRAM score improves to 1-3, manage as above. If PRAM score does not improve, admission is recommended
- PRAM score 8–12: Deterioration of clinical status despite adequate treatment in the initial period warrants special care and attention. It is recommended to establish IV access and to start on appropriate IV fluids. IV salbutamol (1 mcg/kg/min then titrate based on response to a maximum dose of 10 mcg/kg/min), and IV magnesium sulfate (single dose of 40–50 mg/kg to a maximum of 2 g by slow IV infusion) might be considered.[384,385] ABG, CXR, electrolyte, and consultation for the pediatrics critical care service must be sought.
Appendix 1: Pathophysiology of asthma
Airways inflammation
Asthma is a complex syndrome characterized by AH and is caused by a multicellular inflammatory reaction that leads to airway limitation [Box 24].[386,387] Recruitment and activation of mast cells, macrophages, antigen-presenting dendritic cells, neutrophils, eosinophils, and T lymphocytes result in an inflammatory and cellular infiltration of the airways.[388] Type 2 T-helper cells have a major role in the activation of the immune cascade that leads to the release of many mediators such as ILs IL-3, IL-4, IL-5, IL-13, and granulocyte macrophage colony stimulating factor (GM-CSF).[389,390] Some mediators such as IL-4 and IL-13 activate B lymphocytes to produce IgE while others (e.g., IL-3, IL-5, and GM-CSF) are related to eosinophilic inflammation pathway. Severe asthma may present in various inflammatory phenotypes, such as persistent eosinophilic bronchitis, neutrophilic infiltration of the airway, and a pauci-granulocytopenic type of inflammation.[391,392] Such persistent inflammation results in airway remodeling which includes increased deposition of extracellular proteins, smooth muscle hypertrophy and hyperplasia, and increased goblet cells.[393] The airway epithelium becomes fragile and thin, and the epithelial basement membrane thickens. There is also increased mucus production and endothelial leakage, which leads to mucosal edema. Mediator-induced abnormalities in the parasympathetic and nonadrenergic noncholinergic nervous systems may also lead to increased bronchial hyper-responsiveness. Recent data have shown that all asthmatic patients have inflammation in the upper airways, irrespective of the presence of symptoms of rhinosinusitis. Studies have also shown that stimulation by an irritant instilled in the nose leads to eosinophilic inflammation in the lungs within a few hours. Such co-existence of inflammation in both the upper and lower airways has led to the suggestion of the terminology “united airway disease.” In clinical practice, failure to recognize and treat rhinosinusitis may affect asthma control.[394]
Box 24.
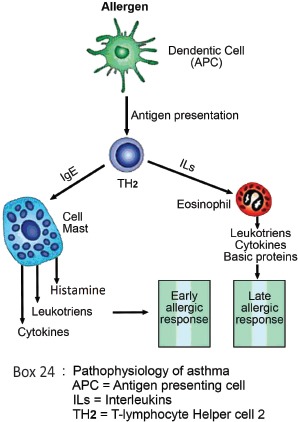
Pathophysiology of asthma
Airways hyper-responsiveness
AH to direct (histamine or methacholine) and indirect (exercise, cold air, mannitol, adenosine monophosphate, or isocapnic hyperventilation) challenges is a characteristic of asthma.[395,396] When asthma symptoms are present, there is a relatively good correlation between the severity of disease and the degree of AH.[397] AH is not a static feature of asthma; it may increase after sensitizing exposures and may decrease after anti-inflammatory treatments or if there is a reduction in relevant environmental exposures. Asthma has a variable component, which is related to airway inflammation, and a more refractory component that is largely attributed to the underlying airway structural changes, which is also known as remodeling.[398]
Early and late responses
Following presentation of the antigen by dendritic cells in a sensitized patient, certain inflammatory cascades become activated leading to the attachment of the IgE antibodies to inflammatory cells such as mast cells.[399] Cross-linking of IgE receptors leads to degranulation of inflammatory cells and liberation of various mediators, which are responsible for the allergic response. The allergen-induced airway response may be immediate (early response) with a fall in expiratory flow within an hour of exposure, or may be delayed (late response) with the fall in expiratory flow being observed within 2–8 h. An increase in AH and the variability of airway obstruction may occur within the following 2–3 days depending on the intensity of the response.[400,401]
Airway remodeling
Structural airway changes may develop even before the disease becomes symptomatic. They can also occur in patients with allergic rhinitis, who are associated with an increased risk of developing asthma. The most prominent changes include epithelial damage, subepithelial fibrosis, increased airway vasculature, increases in extracellular matrix proteins including collagens and proteoglycans, and increased smooth muscle mass. The mucus hypersecretion observed in asthma is related to an increase in the number of secretory glands and cells such as goblet cells. These changes are generally attributed to the underlying inflammatory process, although other mechanisms may play a role.[386] It has been proposed that remodeling may be involved in the development and persistence of asthma, in the accelerated decline of pulmonary function, and in the development of a more “fixed” component of airway obstruction in some asthmatic, particularly in severe cases. Although a relationship has been found between the severity of asthma and some of the components of airway remodeling, researchers have not yet been able to adequately distinguish severe asthma from milder forms on the basis of histological features alone.[402] Prevention of airway remodeling has not been well studied, but it is certain that sustained treatment with anti-inflammatory medications as well as the prevention of asthma exacerbations have a role in preventing or delaying airway remodeling.
Appendix 2: Medications Used for the Treatment of Asthma
The objective of asthma treatment is to achieve and maintain control of the disease. Medications used to treat asthma can be classified as controllers or relievers. Controllers are medications taken daily on a long-term basis to keep asthma under clinical control through their anti-inflammatory effects.[403] Relievers are medications used on an “as-needed bases” that act quickly to reverse bronchoconstriction and relieve symptoms.
Controller medications
Inhaled corticosteroids
ICSs are currently the most effective anti-inflammatory medications for the treatment of asthma.[116,404,405] They reduce symptoms, improve quality of life, improve lung function, decrease AH, control airway inflammation, reduce frequency and severity of asthma exacerbations, and reduce asthma mortality. Early initiation of low-dose ICS in asthma leads to improvement in lung function.[406] When they are discontinued, deterioration of clinical control follows within weeks to months in most patients. ICS differs in its potency and bioavailability. Most of the benefits from ICS are achieved in adults and children at relatively low-doses [Boxes 25 and 26]. Exposure to tobacco smoking, including secondary and tertiary, reduces the responsiveness to ICS. To reach control, add-on therapy with another class of controller is preferred to increasing the dose of ICS.[136,407]
Box 25.
List ICS inhalers available in the Saudi market for adults and adolescents*
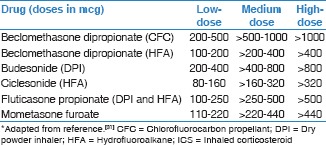
Box 26.
List of ICS inhalers available in the Saudi market for children*
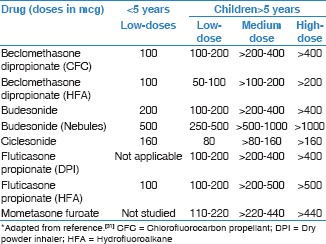
Local adverse effects can occur and include oropharyngeal candidiasis and dysphonia; with MDIs, these effects may be reduced using a spacer device. Mouth washing after inhalation may reduce oral candidiasis. Systemic side effects are occasionally reported with high-doses and long-term treatment. The small risk of adverse events from the use of ICS is well balanced by their efficacy.[408] Though low-medium dose ICS may affect growth in children, this effect is clinically insignificant and may be reversible. Therefore, low-medium dose of ICS is generally safe and well tolerated in children. Formulations with small size particles, such as beclomethasone or ciclesonide, are believed to be more effective and safer as it led to better deposition in the peripheral small airways.[409,410] Some studies have shown that ciclesonide has relatively lower local and systemic side effects, especially in children.[411]
Special considerations for use of inhaled corticosteroid in children
Growth retardation may be seen with all ICSs when a high-dose ICS is chronically used. Based on recent systematic reviews, a mean reduction of 0.48 cm/year in linear height velocity was observed in prepubertal children over 12 months use of low to medium dose of ICS, especially during the 1st year of life.[412] Though this effect was statistically significant, it is not clear if that will be of significant clinical impact. For instance, use of moderate-dose ICS resulted in 1.2 cm reduction in the final adult height after more than 4 years use.[413] Moreover, more studies demonstrated the negative impact of medium to high doses ICS on bone mineralization.[414,415,416] However, it is crucial to remember that long-term use of ICS is safer than frequent bursts of oral corticosteroids on bone mineralization. Adequate nutrition with sufficient intake of calcium and Vitamin D can blunt these effects.[417] In summary, the potential adverse effects of ICS need to be weighed against the well-established benefit to control persistent asthma. Therefore, it is important to target the lowest possible ICS dose that maintains adequate asthma control.
Long-acting inhaled B2-agonists
The commonly used long-acting inhaled B2-agonists, include formoterol and salmeterol, are used twice daily. Novel ultra LABA agents with a 24 h duration of action are available, e.g., indacaterol, vilanterol, and olodaterol.[418,419,420,421,422,423,424] The ultra LABA has a compliance-enhancing advantage. Due to lack of anti-inflammatory effect, this category should not be used alone as monotherapy in asthma as it leads to increased mortality. When used in combination with ICS, there is an improvement in symptoms, decreased nocturnal asthma, improved lung function, decreased use of inhaled B2-agonists, reduced number of asthma exacerbations, and achieving more clinical control of asthma in more patients, more rapidly at a lower dose of ICS. LABA provides longer protection to prevent exercise-induced bronchospasm than short-acting inhaled B2-agonists (SABA).[425] Their side effects are limited to tachycardia, tremor, headaches, muscle cramps, and sometimes hypokalemia. Regular use of LABA combined with ICS may lead to a reduction in these side effects. Furthermore, patients rarely develop a tolerance to LABAs. The effect of LABA products has not been adequately studied in children of 5 years and below.
Fixed combination of inhaled corticosteroid and long-acting beta 2 agonists
Fixed combination of ICS and LABAs is considered more convenient for patients. They increase adherence and ensure that LABA is always accompanied by ICS. Although salmeterol and formoterol provide a similar duration of bronchodilation and protection against bronchoconstriction, formoterol has a more rapid onset of action than salmeterol. Therefore, combination inhalers containing formoterol may be used for both rescue and maintenance of control.[132] Fixed combination inhalers of ICS and LABAs have been available in the form of fluticasone propionate and salmeterol (Seretide) or budesonide and formoterol (Symbicort). New formulations are available in different devices in the Saudi market [Box 27] such as beclomethasone and formoterol (Foster), mometasone and formoterol (Dulera), fluticasone propionate and salmeterol (Rolenium), budesonide and formoterol (Pulmoton), and fluticasone propionate and formoterol (Flutiform).[426,427,428,429]
Box 27.
List of some fixed combinations of inhaled steroid and long-acting beta 2 agonist
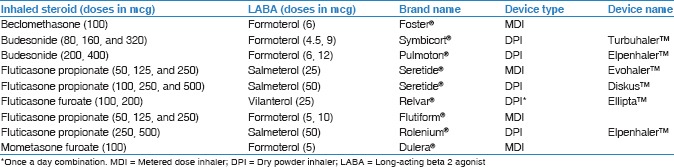
New once a day dry powder combinations of ICS/ultra LABA are expected to be available soon in the Saudi market. One of these, the dry powder combination of fluticasone furoate and vilanterol (Relvar) that comes in two strengths of 100/25 and 200/25 mcg with dispensed equivalent dose of 92/22 and 184/22 mcg, respectively.[134,135] The dose of fluticasone furoate of 100 mcg was found to be equivalent to fluticasone propionate 250 mcg.[430] Such a combination has a potential adherence advantage while maintaining the same safety as the combination of fluticasone propionate and salmeterol.[431]
Leukotriene modifiers
Leukotriene modifier agents reduce airway inflammation and improve asthma symptoms and lung function, but with a less consistent effect on asthma exacerbations, especially when compared to ICS. They may be used as an alternative treatment to ICS for patients with mild asthma, especially in those who have clinical rhinitis. Some patients with ASA-sensitive asthma respond well to the LTRA. However, when used alone as a controller, their effects are generally less than that of low-dose ICS. When added to ICS, LTRA may reduce the dose of ICS required by patients with uncontrolled asthma and may improve asthma control.[432,433] LTRA is generally well tolerated. In children, studies have shown that LTRA may be useful for reducing the number of asthma exacerbations induced by viruses and for reducing bronchial inflammation in atopic children.[433,434,435,436,437] There are no clinical data to support their use under the age of 6 months.
Long-acting anti-muscarinic (cholinergic) agents
LAMAs inhibit the effect of acetylcholine on M3 receptors. Tiotropium was the first agent used in managing patient with COPD. Recently, tiotropium use has been extended to asthma. The more recent LAMA (such as aclidinium bromide, glycopyrronium) has not been studied in asthma yet. The bronchodilatation duration of action of more than 24 h; therefore, it is used once daily.[438,439] The earlier studies for the use of tiotropium were conducted in the HandiHaler. Later studies were conducted in the new Respimat device. Tiotropium is available in the Saudi market with the HandiHaler device where the dose is available in a capsule format that contains 18 mcg. The Respimat device is not yet available in the Saudi market. Tiotropium was first shown to be effective in step-down of treatment when added to a combination of ICS/LABA.[440] More recently, tiotropium was found to be not inferior to salmeterol in the management of asthma not adequately controlled on ICS or combination of ICS/LABA.[145,146,152,441] Anticholinergic drugs are considered safe. The main side effect is dryness of mouth. Although mild prostatic symptoms have been reported, there is no evidence of a direct causal relationship.
Theophylline
Theophylline is a weak bronchodilator with modest anti-inflammatory properties. It may provide benefits as an add-on therapy in patients who do not achieve control with ICS alone but is less-effective than LABA and LTRA. Theophylline is not recommended for use as monotherapy in asthma treatment. Recent data have shown that low-dose theophylline (300 mg/day) may have an important role in improving steroid resistance in patients with severe asthma requiring high-dose ICS.[386,442] Their side effects include gastrointestinal symptoms, cardiac arrhythmias, seizures, and even death. Nausea and vomiting are the early symptoms of toxicity. Liver disease, CHF, quinolones, and some macrolides may increase the risk of toxicity. Use of lower doses may decrease these side effects.
Anti-immunoglobulin E
Anti-IgE is a recombinant humanized IgG1 monoclonal antibody that binds IgE with high affinity and has been developed for the treatment of allergic diseases.[443] Anti-IgE (omalizumab) is indicated for patients of 6 years and above with severe allergic asthma uncontrolled on high-dose ICS and other controllers and who have an IgE level in the appropriate therapeutic range.[444,445,446] As this drug is expensive and requires careful monitoring, it should only be prescribed by a specialist. The side effects include pain and bruising at injection site and very rarely anaphylaxis (0.1%).
Oral B2-agonists
The side effect profile is much higher than that of inhaled B2-agonists. Therefore, their use is highly discouraged. Oral route is not recommended in children.
Cromones
Cromones (sodium cromoglycate and nedocromil sodium) are not recommended for preschool children. They have limited role in the long-term treatment of older children. Evidence showed that low-dose ICS is superior to cromones in the management of asthma.[447]
Systemic corticosteroids
Long-term oral steroid therapy (excluding short courses for acute exacerbations of asthma for 1–2 weeks) may be required to control difficult asthma despite maximum standard therapy. The dose should be reduced to the lowest possible, and other controllers are recommended to be maximized to minimize the side effects from the OCS. Its use is limited by the risk of significant adverse effects. Use of intramuscular long-acting steroids is highly discouraged because of the increased risk of side effects. The side effects include osteoporosis, hypertension, diabetes, adrenal insufficiency, obesity, cataracts, glaucoma, skin thinning, and muscle weakness. Withdrawal can elicit adrenal failure. In patients prescribed long-term systemic corticosteroids, prophylactic treatment for osteoporosis are recommended.
Reliever medications
Relievers are medications used on, an as-needed basis, that act quickly to reverse bronchoconstriction and relieve symptoms.
Rapid onset inhaled B2-agonists
SABA, such as salbutamol, is the medications of choice for relief of symptoms of acute exacerbations of asthma and the pretreatment of EIB. MDI with chamber is as effective as the nebulized route in treatment of acute episodes of wheeze in children.[204] Formoterol is a LABA that has a fast acting component and is not currently available in the Saudi market as a single inhaler; however, it can be used as a rescue medication in formoterol containing combination of ICS/LABA. Regular long-term use of SABA is not recommended.
In acute asthma, inhaled salbutamol is the preferred choice.[201,206] Repeated doses are recommended to be given at 15–20 min intervals. Alternatively, continuous nebulization (salbutamol at 5–10 mg/h) should be used for 1 h if there is an inadequate response to initial treatment. However, a meta-analysis of randomized controlled trials of adults with acute asthma found no significant differences between the continuous or intermittent methods in terms of pulmonary function or hospital admission; nevertheless, patients treated by continuous nebulization had lower side effects.[448] In patients who can use the inhaler devices, 6–12 puffs of MDI with a spacer are equivalent to 5 mg of salbutamol by nebulizer. As the inhaled route has a faster onset of action and fewer adverse effects, the use of IV beta 2 agonists in the initial treatment of patients with acute severe asthma is not generally recommended.[449] IV therapy should not be considered routinely and only cautiously if the response to the inhaled drug is poor or if the patient cannot tolerate the inhaled route.
Anticholinergics
Anticholinergics are less-effective than SABA in asthma. However, when used in combination with SABA in acute asthma, they provide an additional effect.[382] It can also be an alternative bronchodilator for patients who experience adverse effects such as tachycardia, arrhythmia, and tremor from rapid-acting B2-agonists. Their side effects include dryness of the mouth and a bitter taste.
In moderate to severe acute asthma, combining ipratropium bromide with salbutamol has shown to have additional bronchodilation effect and faster improvement in lung function, compared to salbutamol alone.[213,216] A recent systematic review showed the combination therapy has an added benefit in reducing hospitalizations.[215] It has been shown that combining both agents led to reduction in hospital admission rates by 38–57% improvement in lung function, and substantial cost saving.[216,450,451] No evidence of benefit for length of hospital stay and other markers of response when inhaled anticholinergics are added to short-acting β2-agonists in hospitalized asthmatic children with acute exacerbations.[452] The adult dosing of nebulized ipratropium bromide is 500 μg every 20 min for three doses, then as needed. Alternatively, ipratropium can be administered by MDI at a dose of 4–8 puffs (80–160 μg) every 20 min, then as needed for up to 3 h.
Theophylline
There is no evidence supporting the routine use of theophylline in treating acute asthma and its routine use is discouraged. Similarly, routine use of IV aminophylline in acute asthma is strongly discouraged as there is no evidence to show benefit, and the drug has high levels of toxicity and side effects.[453]
Intravenous magnesium sulfate
In a systematic review, magnesium sulfate has shown to reduce hospitalizations in patients with severe or life-threatening asthma exacerbations that fails to respond to initial treatment.[454] A single dose of IV magnesium sulfate (1–2 g) has been shown to be a safe and effective in acute severe asthma.[218]
Aerosol devices used in asthma
Medication aerosol can be delivered using three devices:
Small-volume nebulizer
It is the most popular for patients and clinicians in acute asthma. Small-volume nebulizers are predominately powered by a compressed gas (air or oxygen) to convert one or more drug solutions or suspensions at any concentrations and dose into aerosols. One of its main advantages is that it requires minimal patient cooperation and is therefore suitable for all ages, with normal breathing and no inspiratory pause required. One of its main disadvantages is importability, time to deliver the medication (10–25 min), and potential of contamination. There are high-output aerosol nebulizers that have an output rate of 30–50 ml/h and a flow rate of 10–15 L/min. It provides up to 8 h of continuous nebulization and has a 240 ml reservoir.
Pressurized metered dose inhaler
It is a prepressurized inhaler with medication and a propellant, which when actuated will give one dose of the drug for a single inspiration. MDIs typically require slow inspiratory flow (<30 L/min). One of its main advantages is that it is premixed and the ability to provide multiple doses in a short period. It is also small and portable with limited contamination. Disadvantages include the need of patient training to coordinate inhalation with actuation, and if this not done properly, there is a potential of high deposition of drug in the oropharynx and poor drug delivery. Also, because it does not have dose counter, it is difficult to determine the dose remaining in the canister. Compared to the older chlorofluorocarbon (CFC) propellant formulations, hydrofluroalkane (HFA) formulations provide smaller particle size aerosols with less oral deposition, hence less oral side effects and greater proportion of lung deposition.
Dry powder inhaler
It is not pressurized (no propellant) and, therefore, requires high inspiratory flows (60–90 L/min) to disperse a full dose. In addition to its portability, advantages include that it is breath-actuated, and there is a built-in dose counter. Disadvantages include the need for adequate inspiratory flow to disperse a full dose. If not used properly, high oropharyngeal impaction may occur and exhaled humidity into mouthpiece might affect the function of the device. Therefore, it may not be suitable for very young or very old patients. The commonly available devices in Saudi Arabia are the Turbohaler, Diskus, Handihaler, Easi-Breathe, Ellipta, and Breezhaler devices. HFA formulations provide smaller size particle aerosols with less oral deposition, hence less oral side effects and greater proportion of lung deposition than the older CFC propellant formulations.
Breath-actuated inhalers
These inhalers automatically release a spray of medication when the person begins to inhale. They are easy to use and improve asthma control and compliance to medications.[455,456,457,458]
Acknowledgments
The panel of SINA would like to thank the reviewers of SINA 2016 for their valuable comments: Prof. Mark FitzGerald, University of British Columbia, Vancouver, British Columbia, Canada and Prof. Andrew Bush, Imperial College, National Heart and Lung Institute, London, UK. The panel would like to thank the following consultant reviewers for previous versions on 2009 and 2012 for their valuable reviews: Prof. Mark FitzGerald and Prof. Sheldon Spier from the University of British Columbia, Vancouver, British Columbia, Canada; Prof. Qutayba Hamid and Prof. Ronald Olivenstein from the Meakins-Christie Laboratories, McGill University, Montreal, Quebec, Canada; and Prof. Eric Bateman from the University of Cape Town Lung Institute, Cape Town, South Africa.
References
- 1.Al Frayh AR, Shakoor Z, Gad El Rab MO, Hasnain SM. Increased prevalence of asthma in Saudi Arabia. Ann Allergy Asthma Immunol. 2001;86:292–6. doi: 10.1016/s1081-1206(10)63301-7. [DOI] [PubMed] [Google Scholar]
- 2.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: Results from the American Productivity Audit. J Occup Environ Med. 2003;45:1234–46. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- 3.Al-Mobeireek A. Prescribing for asthmatic children in primary care. Are we following the guidelines? Saudi Med J. 2003;24:1274. [PubMed] [Google Scholar]
- 4.Dashash NA, Mukhtar SH. Prescribing for asthmatic children in primary care. Are we following guidelines? Saudi Med J. 2003;24:507–11. [PubMed] [Google Scholar]
- 5.Khan JH, Lababidi HM, Al-Moamary MS, Zeitouni MO, Al-Jahdali HH, Al-Amoudi OS, et al. The Saudi guidelines for the diagnosis and management of COPD. Ann Thorac Med. 2014;9:55–76. doi: 10.4103/1817-1737.128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tonelli AR, Minai OA. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Perioperative management in patients with pulmonary hypertension. Ann Thorac Med. 2014;9(Suppl 1):S98–107. doi: 10.4103/1817-1737.134048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Minai OA. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Biomarkers in pulmonary arterial hypertension. Ann Thorac Med. 2014;9(Suppl 1):S92–7. doi: 10.4103/1817-1737.134047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Idrees MM, Swiston J, Nizami I, Al Dalaan A, Levy RD. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Medical and surgical management for pulmonary arterial hypertension. Ann Thorac Med. 2014;9(Suppl 1):S79–91. doi: 10.4103/1817-1737.134043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Idrees MM, Swiston J, Levy RD. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: General management for pulmonary hypertension. Ann Thorac Med. 2014;9(Suppl 1):S74–8. doi: 10.4103/1817-1737.134041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saleemi S. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Pulmonary hypertension associated with hemolytic anemia. Ann Thorac Med. 2014;9(Suppl 1):S67–73. doi: 10.4103/1817-1737.134039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayer E, Idrees MM. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Chronic thromboembolic pulmonary hypertension. Ann Thorac Med. 2014;9(Suppl 1):S62–6. doi: 10.4103/1817-1737.134037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sakkijha H, Idrees MM. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Pulmonary hypertension due to lung diseases and/or hypoxia. Ann Thorac Med. 2014;9(Suppl 1):S56–61. doi: 10.4103/1817-1737.134030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alhabeeb W, Idrees MM, Ghio S, Kashour T. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Pulmonary hypertension due to left heart disease. Ann Thorac Med. 2014;9(Suppl 1):S47–55. doi: 10.4103/1817-1737.134026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saleemi S, Idrees MM. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Portopulmonary hypertension. Ann Thorac Med. 2014;9(Suppl 1):S42–6. doi: 10.4103/1817-1737.134021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Butrous G. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Schistosomiasis and pulmonary arterial hypertension. Ann Thorac Med. 2014;9(Suppl 1):S38–41. doi: 10.4103/1817-1737.134019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boueiz A, Hassoun PM. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Pulmonary arterial hypertension associated with connective tissue diseases. Ann Thorac Med. 2014;9(Suppl 1):S26–37. doi: 10.4103/1817-1737.134016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lopes A, Alnajashi K. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Pulmonary arterial hypertension associated with congenital heart disease. Ann Thorac Med. 2014;9(Suppl 1):S21–5. doi: 10.4103/1817-1737.134015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pasha Q. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Genetics of pulmonary hypertension. Ann Thorac Med. 2014;9(Suppl 1):S16–20. doi: 10.4103/1817-1737.134009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhagavatula SK, Idrees MM. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Challenges in managing pulmonary hypertension in the developing countries. Ann Thorac Med. 2014;9(Suppl 1):S127–30. doi: 10.4103/1817-1737.134059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Azem MA, Al-Hazmi MS. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Intensive care management of pulmonary hypertension. Ann Thorac Med. 2014;9(Suppl 1):S121–6. doi: 10.4103/1817-1737.134056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al Dabbagh M, Banjar H, Galal N, Kouatli A, Kandil H, Chehab M. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Pulmonary hypertension in children. Ann Thorac Med. 2014;9(Suppl 1):S113–20. doi: 10.4103/1817-1737.134053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khan J, Idrees MM. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: Pregnancy in pulmonary hypertension. Ann Thorac Med. 2014;9(Suppl 1):S108–12. doi: 10.4103/1817-1737.134050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Idrees MM, Saleemi S, Azem MA, Aldammas S, Alhazmi M, Khan J, et al. Saudi guidelines on the diagnosis and treatment of pulmonary hypertension: 2014 updates. Ann Thorac Med. 2014;9(Suppl 1):S1–15. doi: 10.4103/1817-1737.134006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Moamary MS, Al-Hajjaj MS, Idrees MM, Zeitouni MO, Alanezi MO, Al-Jahdal HH, et al. The Saudi initiative for asthma. Ann Thorac Med. 2009;4:216–33. doi: 10.4103/1817-1737.56001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Moamary MS, Alhaider SA, Al-Hajjaj MS, Al-Ghobain MO, Idrees MM, Zeitouni MO, et al. The Saudi initiative for asthma-2012 update: Guidelines for the diagnosis and management of asthma in adults and children. Ann Thorac Med. 2012;7:175–204. doi: 10.4103/1817-1737.102166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prevention GsfAma. Global Initiative for Asthma (GINA); 2009. [Last accessed on 2012 Jun 02]. Available from: http://www.ginAsthma.org .
- 27.Prevention GsfAma. Global Initiative for Asthma in Children 5 Years and Younger. 2009. [Last accessed on 2012 Jun 02]. Available from: http://www.ginAsthma.org .
- 28.Bousquet J, Clark TJ, Hurd S, Khaltaev N, Lenfant C, O’byrne P, et al. GINA guidelines on asthma and beyond. Allergy. 2007;62:102–12. doi: 10.1111/j.1398-9995.2006.01305.x. [DOI] [PubMed] [Google Scholar]
- 29.National Asthma Education and Prevention Program. National asthma education and prevention program.expert panel report: Guidelines for the Diagnosis and management of asthma update on selected topics-2002. J Allergy Clin Immunol. 2002;110(5 Suppl):S141–219. [PubMed] [Google Scholar]
- 30.Boulet LP, FitzGerald JM, Reddel HK. The revised 2014 GINA strategy report: Opportunities for change. Curr Opin Pulm Med. 2015;21:1–7. doi: 10.1097/MCP.0000000000000125. [DOI] [PubMed] [Google Scholar]
- 31.GINA. Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma (GINA) 2015. [Last accessed on 2015 Aug. 14]. Available at: http://www.ginasthma.org/documents/4 .
- 32.Wechsler ME. Managing asthma in primary care: Putting new guideline recommendations into context. Mayo Clin Proc. 2009;84:707–17. doi: 10.4065/84.8.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jadad AR, Moher M, Browman GP, Booker L, Sigouin C, Fuentes M, et al. Systematic reviews and meta-analyses on treatment of asthma: Critical evaluation. BMJ. 2000;320:537–40. doi: 10.1136/bmj.320.7234.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Ghamdi BR, Mahfouz AA, Abdelmoneim I, Khan MY, Daffallah AA. Altitude and bronchial asthma in South-Western Saudi Arabia. East Mediterr Health J. 2008;14:17–23. [PubMed] [Google Scholar]
- 35.Rabe KF, Adachi M, Lai CK, Soriano JB, Vermeire PA, Weiss KB, et al. Worldwide severity and control of asthma in children and adults: The global asthma insights and reality surveys. J Allergy Clin Immunol. 2004;114:40–7. doi: 10.1016/j.jaci.2004.04.042. [DOI] [PubMed] [Google Scholar]
- 36.Abudahish A, Bella H. Primary care physicians perceptions and practices on asthma care in Aseer region, Saudi Arabia. Saudi Med J. 2006;27:333–7. [PubMed] [Google Scholar]
- 37.Alamoudi O. Prevalence of respiratory diseases in hospitalized patients in Saudi Arabia: A 5 years study 1996-2000. Ann Thorac Med. 2006;1:76–80. [Google Scholar]
- 38.BinSaeed AA. Caregiver knowledge and its relationship to asthma control among children in Saudi Arabia. J Asthma. 2014;51:870–5. doi: 10.3109/02770903.2014.906608. [DOI] [PubMed] [Google Scholar]
- 39.BinSaeed AA, Torchyan AA, Alsadhan AA, Almidani GM, Alsubaie AA, Aldakhail AA, et al. Determinants of asthma control among children in Saudi Arabia. J Asthma. 2014;51:435–9. doi: 10.3109/02770903.2013.876649. [DOI] [PubMed] [Google Scholar]
- 40.Al Zahrani SS, El Morsy E, Laila S, Dorgham L. The impact of bronchial asthma on quality of life among affected children and adolescents in Taif city, Saudi Arabia. Life Sci J. 2014;11:283–91. [Google Scholar]
- 41.Ahmed AE, Al-Jahdali H, Al-Harbi A, Khan M, Ali Y, Al Shimemeri A, et al. Factors associated with poor asthma control among asthmatic patient visiting emergency department. Clin Respir J. 2014;8:431–6. doi: 10.1111/crj.12090. [DOI] [PubMed] [Google Scholar]
- 42.Al-Jahdali H, Anwar A, Al-Harbi A, Baharoon S, Halwani R, Al Shimemeri A, et al. Factors associated with patient visits to the emergency department for asthma therapy. BMC Pulm Med. 2012;12:80. doi: 10.1186/1471-2466-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Colver AF. Underdiagnosis and undertreatment of asthma in childhood. Br Med J (Clin Res Ed) 1983;286:1511–2. doi: 10.1136/bmj.286.6376.1511-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Speight AN, Lee DA, Hey EN. Underdiagnosis and undertreatment of asthma in childhood. Br Med J (Clin Res Ed) 1983;286:1253–6. doi: 10.1136/bmj.286.6373.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Al-Zahrani JM, Ahmad A, Al-Harbi A, Khan AM, Al-Bader B, Baharoon S, et al. Factors associated with poor asthma control in the outpatient clinic setting. Ann Thorac Med. 2015;10:100–4. doi: 10.4103/1817-1737.152450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al-Kabbaa AF, Al-Shamrani KM, Salih MA. Does the management of bronchial asthma by family physicians meet standards of the national protocol? J Family Community Med. 2002;9:21–5. [PMC free article] [PubMed] [Google Scholar]
- 47.Al-Jahdali HH, Al-Hajjaj MS, Alanezi MO, Zeitoni MO, Al-Tasan TH. Asthma control assessment using asthma control test among patients attending 5 tertiary care hospitals in Saudi Arabia. Saudi Med J. 2008;29:714–7. [PubMed] [Google Scholar]
- 48.al Frayh AR. Asthma patterns in Saudi Arabian children. J R Soc Health. 1990;110:98–100. doi: 10.1177/146642409011000309. [DOI] [PubMed] [Google Scholar]
- 49.al Frayh AR, al Nahdi M, Bener AR, Jawadi TQ. Epidemiology of asthma and allergic rhinitis in two coastal regions of Saudi Arabia. Allerg Immunol (Paris) 1989;21:389–93. [PubMed] [Google Scholar]
- 50.Bener A, al-Jawadi TQ, Ozkaragoz F, Anderson JA. Prevalence of asthma and wheeze in two different climatic areas of Saudi Arabia. Indian J Chest Dis Allied Sci. 1993;35:9–15. [PubMed] [Google Scholar]
- 51.Hijazi N, Abalkhail B, Seaton A. Asthma and respiratory symptoms in urban and rural Saudi Arabia. Eur Respir J. 1998;12:41–4. doi: 10.1183/09031936.98.12010041. [DOI] [PubMed] [Google Scholar]
- 52.Alshehri MA, Abolfotouh MA, Sadeg A, Al Najjar YM, Asindi AA, Al Harthi AM, et al. Screening for asthma and associated risk factors among urban school boys in Abha city. Saudi Med J. 2000;21:1048–53. [PubMed] [Google Scholar]
- 53.Al Ghobain MO, Al-Hajjaj MS, Al Moamary MS. Asthma prevalence among 16- to 18-year-old adolescents in Saudi Arabia using the ISAAC questionnaire. BMC Public Health. 2012;12:239. doi: 10.1186/1471-2458-12-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nahhas M, Bhopal R, Anandan C, Elton R, Sheikh A. Prevalence of allergic disorders among primary school-aged children in Madinah, Saudi Arabia: Two-stage cross-sectional survey. PLoS One. 2012;7:e36848. doi: 10.1371/journal.pone.0036848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sobki SH, Zakzouk SM. Point prevalence of allergic rhinitis among Saudi children. Rhinology. 2004;42:137–40. [PubMed] [Google Scholar]
- 56.Duran-Tauleria E, Rona RJ. Geographical and socioeconomic variation in the prevalence of asthma symptoms in English and Scottish children. Thorax. 1999;54:476–81. doi: 10.1136/thx.54.6.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stempel DA, McLaughin TP, Stanford RH, Fuhlbrigge AL. Patterns of asthma control: A 3-year analysis of patient claims. J Allergy Clin Immunol. 2005;115:935–9. doi: 10.1016/j.jaci.2005.01.054. [DOI] [PubMed] [Google Scholar]
- 58.Horne R, Price D, Cleland J, Costa R, Covey D, Gruffydd-Jones K, et al. Can asthma control be improved by understanding the patient's perspective? BMC Pulm Med. 2007;7:8. doi: 10.1186/1471-2466-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alharbi M, Almutairi A, Alotaibi D, Alotaibi A, Shaikh S, Bahammam AS. The prevalence of asthma in patients with obstructive sleep apnoea. Prim Care Respir J. 2009;18:328–30. doi: 10.4104/pcrj.2009.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Berlow BA. Eight key questions to ask when your patient with asthma doesn’t get better. Am Fam Physician. 1997;55:183. [PubMed] [Google Scholar]
- 61.Price D. Asthma and allergic rhinitis: Linked in treatment and outcomes. Ann Thorac Med. 2010;5:63–4. doi: 10.4103/1817-1737.62467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fireman P. Rhinitis and asthma connection: Management of coexisting upper airway allergic diseases and asthma. Allergy Asthma Proc. 2000;21:45–54. doi: 10.2500/108854100778248935. [DOI] [PubMed] [Google Scholar]
- 63.Al-Mobeireek AF, Al-Sarhani A, Al-Amri S, Bamgboye E, Ahmed SS. Chronic cough at a non-teaching hospital: Are extrapulmonary causes overlooked? Respirology. 2002;7:141–6. doi: 10.1046/j.1440-1843.2002.00378.x. [DOI] [PubMed] [Google Scholar]
- 64.Al-Otair H, Bahammam AS. Unusual cause of respiratory distress misdiagnosed as refractory asthma. Ann Thorac Med. 2006;1:28–30. [Google Scholar]
- 65.Cowie RL, Underwood MF, Field SK. Asthma symptoms do not predict spirometry. Can Respir J. 2007;14:339–42. doi: 10.1155/2007/816132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tashkin DP, Altose MD, Connett JE, Kanner RE, Lee WW, Wise RA. Methacholine reactivity predicts changes in lung function over time in smokers with early chronic obstructive pulmonary disease. The Lung Health Study Research Group. Am J Respir Crit Care Med. 1996;153(6 Pt 1):1802–11. doi: 10.1164/ajrccm.153.6.8665038. [DOI] [PubMed] [Google Scholar]
- 67.Witteman AM, Stapel SO, Perdok GJ, Sjamsoedin DH, Jansen HM, Aalberse RC, et al. The relationship between RAST and skin test results in patients with asthma or rhinitis: A quantitative study with purified major allergens. J Allergy Clin Immunol. 1996;97(1 Pt 1):16–25. doi: 10.1016/s0091-6749(96)70278-6. [DOI] [PubMed] [Google Scholar]
- 68.Humbert M, Holgate S, Boulet LP, Bousquet J. Asthma control or severity: That is the question. Allergy. 2007;62:95–101. doi: 10.1111/j.1398-9995.2006.01308.x. [DOI] [PubMed] [Google Scholar]
- 69.Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma Control study. Am J Respir Crit Care Med. 2004;170:836–44. doi: 10.1164/rccm.200401-033OC. [DOI] [PubMed] [Google Scholar]
- 70.Pedersen SE, Hurd SS, Lemanske RF, Jr, Becker A, Zar HJ, Sly PD, et al. Global strategy for the diagnosis and management of asthma in children 5 years and younger. Pediatr Pulmonol. 2011;46:1–17. doi: 10.1002/ppul.21321. [DOI] [PubMed] [Google Scholar]
- 71.Cope SF, Ungar WJ, Glazier RH. International differences in asthma guidelines for children. Int Arch Allergy Immunol. 2009;148:265–78. doi: 10.1159/000170380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lababidi H, Hijaoui A, Zarzour M. Validation of the Arabic version of the asthma control test. Ann Thorac Med. 2008;3:44–7. doi: 10.4103/1817-1737.39635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Alanezi M, Al-Jahdali HH, Al-Hajjaj MS, Zeitoni MO, Al-Tasan TH. Levels of acceptance of Asthma Control Test questionnaire among Saudi patients attending 5 tertiary care hospitals in Saudi Arabia. Saudi Med J. 2009;30:546–9. [PubMed] [Google Scholar]
- 74.Al Moamary MS, Al-Kordi AG, Al Ghobain MO, Tamim HM. Utilization and responsiveness of the asthma control test (ACT) at the initiation of therapy for patients with asthma: A randomized controlled trial. BMC Pulm Med. 2012;12:14. doi: 10.1186/1471-2466-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: A survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 76.Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P. The minimally important difference of the Asthma Control Test. J Allergy Clin Immunol. 2009;124:719–23.e1. doi: 10.1016/j.jaci.2009.06.053. [DOI] [PubMed] [Google Scholar]
- 77.Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: Reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117:549–56. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 78.Patel M, Pilcher J, Reddel HK, Pritchard A, Corin A, Helm C, et al. Metrics of salbutamol use as predictors of future adverse outcomes in asthma. Clin Exp Allergy. 2013;43:1144–51. doi: 10.1111/cea.12166. [DOI] [PubMed] [Google Scholar]
- 79.Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105:930–8. doi: 10.1016/j.rmed.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 80.Fuhlbrigge AL, Kitch BT, Paltiel AD, Kuntz KM, Neumann PJ, Dockery DW, et al. FEV (1) is associated with risk of asthma attacks in a pediatric population. J Allergy Clin Immunol. 2001;107:61–7. doi: 10.1067/mai.2001.111590. [DOI] [PubMed] [Google Scholar]
- 81.Turner MO, Noertjojo K, Vedal S, Bai T, Crump S, Fitzgerald JM. Risk factors for near-fatal asthma. A case-control study in hospitalized patients with asthma. Am J Respir Crit Care Med. 1998;157(6 Pt 1):1804–9. doi: 10.1164/ajrccm.157.6.9708092. [DOI] [PubMed] [Google Scholar]
- 82.Miller MK, Lee JH, Miller DP, Wenzel SE TENOR Study Group. Recent asthma exacerbations: A key predictor of future exacerbations. Respir Med. 2007;101:481–9. doi: 10.1016/j.rmed.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 83.Sturdy PM, Victor CR, Anderson HR, Bland JM, Butland BK, Harrison BD, et al. Psychological, social and health behaviour risk factors for deaths certified as asthma: A national case-control study. Thorax. 2002;57:1034–9. doi: 10.1136/thorax.57.12.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Osborne ML, Pedula KL, O’Hollaren M, Ettinger KM, Stibolt T, Buist AS, et al. Assessing future need for acute care in adult asthmatics: The Profile of Asthma Risk Study: A prospective health maintenance organization-based study. Chest. 2007;132:1151–61. doi: 10.1378/chest.05-3084. [DOI] [PubMed] [Google Scholar]
- 85.Belda J, Giner J, Casan P, Sanchis J. Mild exacerbations and eosinophilic inflammation in patients with stable, well-controlled asthma after 1 year of follow-up. Chest. 2001;119:1011–7. doi: 10.1378/chest.119.4.1011. [DOI] [PubMed] [Google Scholar]
- 86.Murphy VE, Clifton VL, Gibson PG. Asthma exacerbations during pregnancy: Incidence and association with adverse pregnancy outcomes. Thorax. 2006;61:169–76. doi: 10.1136/thx.2005.049718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: Asthma control and exacerbations: Standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180:59–99. doi: 10.1164/rccm.200801-060ST. [DOI] [PubMed] [Google Scholar]
- 88.Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB, et al. Anew perspective on concepts of asthma severity and control. Eur Respir J. 2008;32:545–54. doi: 10.1183/09031936.00155307. [DOI] [PubMed] [Google Scholar]
- 89.Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43:343–73. doi: 10.1183/09031936.00202013. [DOI] [PubMed] [Google Scholar]
- 90.Al-Jahdali HH, Al-Zahrani AI, Al-Otaibi ST, Hassan IS, Al-Moamary MS, Al-Duhaim AS, et al. Perception of the role of inhaled corticosteroids and factors affecting compliance among asthmatic adult patients. Saudi Med J. 2007;28:569–73. [PubMed] [Google Scholar]
- 91.Alsheri MA. Comparative study of different inhaler devices in asthmatic children. Ann Saudi Med. 2003;23:349–53. doi: 10.5144/0256-4947.2003.349. [DOI] [PubMed] [Google Scholar]
- 92.Al-Wasil MA, Al-Mohaimeed A. Assessment of inhalation technique in primary care asthmatic patients using metered-dose inhalers with or without a spacer. Ann Saudi Med. 2003;23:264–9. doi: 10.5144/0256-4947.2003.264. [DOI] [PubMed] [Google Scholar]
- 93.Al-Haddad N, Nour A, Koshak E. Asthma care: Structural foundations at primary health care at Al-Qassim region, Saudi Arabia. Ann Thorac Med. 2006;1:8–11. [Google Scholar]
- 94.Al Moamary MS. Unconventional therapy use among asthma patients in a tertiary care center in Riyadh, Saudi Arabia. Ann Thorac Med. 2008;3:48–51. doi: 10.4103/1817-1737.39636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Al-Haddad N, Al-Ansari SS, Al-Shari AT. Impact of asthma education program on asthma knowledge of general practitioners. Ann Saudi Med. 1997;17:550–2. doi: 10.5144/0256-4947.1997.550. [DOI] [PubMed] [Google Scholar]
- 96.Barnes NC. Can guideline-defined asthma control be achieved. The Gaining Optimal Asthma Control study? Am J Respir Crit Care Med. 2004;170:830–1. doi: 10.1164/rccm.2408006. [DOI] [PubMed] [Google Scholar]
- 97.Gibson PG, Powell H. Written action plans for asthma: An evidence-based review of the key components. Thorax. 2004;59:94–9. doi: 10.1136/thorax.2003.011858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gibson PG, Powell H, Coughlan J, Wilson AJ, Hensley MJ, Abramson M, et al. Limited (information only) patient education programs for adults with asthma. Cochrane Database Syst Rev. 2002 doi: 10.1002/14651858.CD001005. CD001005. [DOI] [PubMed] [Google Scholar]
- 99.Guevara JP, Wolf FM, Grum CM, Clark NM. Effects of educational interventions for self management of asthma in children and adolescents: Systematic review and meta-analysis. BMJ. 2003;326:1308–9. doi: 10.1136/bmj.326.7402.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zaraket R, Al-Tannir MA, Bin Abdulhak AA, Shatila A, Lababidi H. Parental perceptions and beliefs about childhood asthma: A cross-sectional study. Croat Med J. 2011;52:637–43. doi: 10.3325/cmj.2011.52.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Al-Binali AM, Mahfouz AA, Al-Fifi S, Naser SM, Al-Gelban KS. Asthma knowledge and behaviours among mothers of asthmatic children in Aseer, South-West Saudi Arabia. East Mediterr Health J. 2010;16:1153–8. [PubMed] [Google Scholar]
- 102.Al-Yami SM, Mohajer KA, Al-Jeraisy MI, Batarfi AM, Abolfotouh MA. Recurrent visits and admissions of children with asthma in central Saudi Arabia. Saudi Med J. 2010;31:921–4. [PubMed] [Google Scholar]
- 103.Basyouni MH, BinDhim NF, Saini B, Williams KA. Online health information needs for patients with asthma in Saudi Arabia. J Consum Health Internet. 2015;19:13–24. [Google Scholar]
- 104.Al-Shimemeri A, Al-Ghadeer H, Giridhar H, Al-Jahdali M, Al-Moamary M, Khan J. Impact of an extensive Asthma education campaign for physicians on their drug prescription practices. Ann Thorac Med. 2006;20:1–5. [Google Scholar]
- 105.Al-Mobeireek A. The efficacy of a management protocol in reducing emergency visits and hospitalizations in chronic asthmatics. Saudi Med J. 2003;24:694. [PubMed] [Google Scholar]
- 106.Alamoudi OS. The efficacy of a management protocol in reducing emergency visits and hospitalizations in chronic asthmatics. Saudi Med J. 2002;23:1373–9. [PubMed] [Google Scholar]
- 107.Al-Jahdali HH, Al-Omar AM, Al-Moamary MS, Al-Duhaim AS, Al-Hodeib AS, Hassan IS, et al. Implementation of the national asthma management guidelines in the emergency department. Saudi Med J. 2004;25:1208–11. [PubMed] [Google Scholar]
- 108.Alotaibi G. Status of respiratory care profession in Saudi Arabia: A national survey. Ann Thorac Med. 2015;10:55–60. doi: 10.4103/1817-1737.146878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Buist AS, Vollmer WM, Wilson SR, Frazier EA, Hayward AD. A randomized clinical trial of peak flow versus symptom monitoring in older adults with asthma. Am J Respir Crit Care Med. 2006;174:1077–87. doi: 10.1164/rccm.200510-1606OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Al-Frayh AS, Hasnain SM, Gad-El-Rab MO, Schwartz B, Al-Mobairek K, Al-Sedairy ST. House dust mite allergens in Saudi Arabia: Regional variations and immune response. Ann Saudi Med. 1997;17:156–60. doi: 10.5144/0256-4947.1997.156. [DOI] [PubMed] [Google Scholar]
- 111.Hasnain SM, Fatima K, Al-Frayh A. Prevalence of airborne allergenic Amaranthus viridis pollen in seven different regions of Saudi Arabia. Ann Saudi Med. 2007;27:259–63. doi: 10.5144/0256-4947.2007.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tunnicliffe WS, Fletcher TJ, Hammond K, Roberts K, Custovic A, Simpson A, et al. Sensitivity and exposure to indoor allergens in adults with differing asthma severity. Eur Respir J. 1999;13:654–9. doi: 10.1183/09031936.99.13365499. [DOI] [PubMed] [Google Scholar]
- 113.Troisi RJ, Speizer FE, Rosner B, Trichopoulos D, Willett WC. Cigarette smoking and incidence of chronic bronchitis and asthma in women. Chest. 1995;108:1557–61. doi: 10.1378/chest.108.6.1557. [DOI] [PubMed] [Google Scholar]
- 114.Nicholson KG, Nguyen-Van-Tam JS, Ahmed AH, Wiselka MJ, Leese J, Ayres J, et al. Randomised placebo-controlled crossover trial on effect of inactivated influenza vaccine on pulmonary function in asthma. Lancet. 1998;351:326–31. doi: 10.1016/S0140-6736(97)07468-0. [DOI] [PubMed] [Google Scholar]
- 115.Bueving HJ, van der Wouden JC, Raat H, Bernsen RM, de Jongste JC, van Suijlekom-Smit LW, et al. Influenza vaccination in asthmatic children: Effects on quality of life and symptoms. Eur Respir J. 2004;24:925–31. doi: 10.1183/09031936.04.00060504. [DOI] [PubMed] [Google Scholar]
- 116.Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen YZ, Ohlsson SV, et al. Early intervention with budesonide in mild persistent asthma: A randomised, double-blind trial. Lancet. 2003;361:1071–6. doi: 10.1016/S0140-6736(03)12891-7. [DOI] [PubMed] [Google Scholar]
- 117.Barnes PJ, Pedersen S. Efficacy and safety of inhaled corticosteroids in asthma. Report of a workshop held in Eze, France, October 1992. Am Rev Respir Dis. 1993;148(4 Pt 2):S1–26. doi: 10.1164/ajrccm/148.4_Pt_2.S1. [DOI] [PubMed] [Google Scholar]
- 118.Berger WE. Levalbuterol: Pharmacologic properties and use in the treatment of pediatric and adult asthma. Ann Allergy Asthma Immunol. 2003;90:583–91. doi: 10.1016/S1081-1206(10)61859-5. [DOI] [PubMed] [Google Scholar]
- 119.Leynaert B, Bousquet J, Neukirch C, Liard R, Neukirch F. Perennial rhinitis: An independent risk factor for asthma in nonatopic subjects: Results from the European Community Respiratory Health Survey. J Allergy Clin Immunol. 1999;104(2 Pt 1):301–4. doi: 10.1016/s0091-6749(99)70370-2. [DOI] [PubMed] [Google Scholar]
- 120.Taramarcaz P, Gibson PG. Intranasal corticosteroids for asthma control in people with coexisting asthma and rhinitis. Cochrane Database Syst Rev 2003 Cochrane Database Syst Rev. 2003;4:CD003570. doi: 10.1002/14651858.CD003570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Dahl R, Nielsen LP, Kips J, Foresi A, Cauwenberge P, Tudoric N, et al. Intranasal and inhaled fluticasone propionate for pollen-induced rhinitis and asthma. Allergy. 2005;60:875–81. doi: 10.1111/j.1398-9995.2005.00819.x. [DOI] [PubMed] [Google Scholar]
- 122.Philip G, Nayak AS, Berger WE, Leynadier F, Vrijens F, Dass SB, et al. The effect of montelukast on rhinitis symptoms in patients with asthma and seasonal allergic rhinitis. Curr Med Res Opin. 2004;20:1549–58. doi: 10.1185/030079904x3348. [DOI] [PubMed] [Google Scholar]
- 123.Vignola AM, Humbert M, Bousquet J, Boulet LP, Hedgecock S, Blogg M, et al. Efficacy and tolerability of anti-immunoglobulin E therapy with omalizumab in patients with concomitant allergic asthma and persistent allergic rhinitis: SOLAR. Allergy. 2004;59:709–17. doi: 10.1111/j.1398-9995.2004.00550.x. [DOI] [PubMed] [Google Scholar]
- 124.Wilson AM, Dempsey OJ, Sims EJ, Lipworth BJ. A comparison of topical budesonide and oral montelukast in seasonal allergic rhinitis and asthma. Clin Exp Allergy. 2001;31:616–24. doi: 10.1046/j.1365-2222.2001.01088.x. [DOI] [PubMed] [Google Scholar]
- 125.Koshak EA. Classification of asthma according to revised 2006 GINA: Evolution from severity to control. Ann Thorac Med. 2007;2:45–6. doi: 10.4103/1817-1737.32228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: The OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164(8 Pt 1):1392–7. doi: 10.1164/ajrccm.164.8.2104102. [DOI] [PubMed] [Google Scholar]
- 127.Shah L, Wilson AJ, Gibson PG, Coughlan J. Long acting beta-agonists versus theophylline for maintenance treatment of asthma. Cochrane Database Syst Rev. 2003;3:CD001281. doi: 10.1002/14651858.CD001281. [DOI] [PubMed] [Google Scholar]
- 128.Powell H, Gibson PG. Initial starting dose of inhaled corticosteroids in adults with asthma: A systematic review. Thorax. 2004;59:1041–5. doi: 10.1136/thx.2004.023754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Drazen JM, Israel E, O’Byrne PM. Treatment of asthma with drugs modifying the leukotriene pathway. N Engl J Med. 1999;340:197–206. doi: 10.1056/NEJM199901213400306. [DOI] [PubMed] [Google Scholar]
- 130.Godard P, Greillier P, Pigearias B, Nachbaur G, Desfougeres JL, Attali V. Maintaining asthma control in persistent asthma: Comparison of three strategies in a 6-month double-blind randomised study. Respir Med. 2008;102:1124–31. doi: 10.1016/j.rmed.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 131.Kankaanranta H, Lahdensuo A, Moilanen E, Barnes PJ. Add-on therapy options in asthma not adequately controlled by inhaled corticosteroids: A comprehensive review. Respir Res. 2004;5:17. doi: 10.1186/1465-9921-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.O’Byrne PM, Bisgaard H, Godard PP, Pistolesi M, Palmqvist M, Zhu Y, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med. 2005;171:129–36. doi: 10.1164/rccm.200407-884OC. [DOI] [PubMed] [Google Scholar]
- 133.Bateman ED, Bousquet J, Keech ML, Busse WW, Clark TJ, Pedersen SE. The correlation between asthma control and health status: The GOAL study. Eur Respir J. 2007;29:56–62. doi: 10.1183/09031936.00128505. [DOI] [PubMed] [Google Scholar]
- 134.O’Byrne PM, Bleecker ER, Bateman ED, Busse WW, Woodcock A, Forth R, et al. Once-daily fluticasone furoate alone or combined with vilanterol in persistent asthma. Eur Respir J. 2014;43:773–82. doi: 10.1183/09031936.00064513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Woodcock A, Bleecker ER, Lötvall J, O’Byrne PM, Bateman ED, Medley H, et al. Efficacy and safety of fluticasone furoate/vilanterol compared with fluticasone propionate/salmeterol combination in adult and adolescent patients with persistent asthma: A randomized trial. Chest. 2013;144:1222–9. doi: 10.1378/chest.13-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chowdhury BA, Dal Pan G. The FDA and safe use of long-acting beta-agonists in the treatment of asthma. N Engl J Med. 2010;362:1169–71. doi: 10.1056/NEJMp1002074. [DOI] [PubMed] [Google Scholar]
- 137.Szefler SJ, Martin RJ, King TS, Boushey HA, Cherniack RM, Chinchilli VM, et al. Significant variability in response to inhaled corticosteroids for persistent asthma. J Allergy Clin Immunol. 2002;109:410–8. doi: 10.1067/mai.2002.122635. [DOI] [PubMed] [Google Scholar]
- 138.Koshak EA. New FDA safety warnings for LABAs: A call for asthma guidelines revisit for solo beta agonist. Ann Thorac Med. 2010;5:65–6. doi: 10.4103/1817-1737.62468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Powell H, Gibson PG. Inhaled corticosteroid doses in asthma: An evidence-based approach. Med J Aust. 2003;178:223–5. doi: 10.5694/j.1326-5377.2003.tb05167.x. [DOI] [PubMed] [Google Scholar]
- 140.Vaquerizo MJ, Casan P, Castillo J, Perpiña M, Sanchis J, Sobradillo V, et al. Effect of montelukast added to inhaled budesonide on control of mild to moderate asthma. Thorax. 2003;58:204–10. doi: 10.1136/thorax.58.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Joos S, Miksch A, Szecsenyi J, Wieseler B, Grouven U, Kaiser T, et al. Montelukast as add-on therapy to inhaled corticosteroids in the treatment of mild to moderate asthma: A systematic review. Thorax. 2008;63:453–62. doi: 10.1136/thx.2007.081596. [DOI] [PubMed] [Google Scholar]
- 142.Zeiger RS, Szefler SJ, Phillips BR, Schatz M, Martinez FD, Chinchilli VM, et al. Response profiles to fluticasone and montelukast in mild-to-moderate persistent childhood asthma. J Allergy Clin Immunol. 2006;117:45–52. doi: 10.1016/j.jaci.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 143.Evans DJ, Taylor DA, Zetterstrom O, Chung KF, O’Connor BJ, Barnes PJ. A comparison of low-dose inhaled budesonide plus theophylline and high-dose inhaled budesonide for moderate asthma. N Engl J Med. 1997;337:1412–8. doi: 10.1056/NEJM199711133372002. [DOI] [PubMed] [Google Scholar]
- 144.Kerstjens HA, van den Berge M. Regular treatment for moderate asthma: Guidelines hold true. Lancet Respir Med. 2015;3:88–9. doi: 10.1016/S2213-2600(14)70297-8. [DOI] [PubMed] [Google Scholar]
- 145.Beeh KM, Moroni-Zentgraf P, Ablinger O, Hollaenderova Z, Unseld A, Engel M, et al. Tiotropium Respimat® in asthma: A double-blind, randomised, dose-ranging study in adult patients with moderate asthma. Respir Res. 2014;15:61. doi: 10.1186/1465-9921-15-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Tian JW, Chen JW, Chen R, Chen X. Tiotropium versus placebo for inadequately controlled asthma: A meta-analysis. Respir Care. 2014;59:654–66. doi: 10.4187/respcare.02703. [DOI] [PubMed] [Google Scholar]
- 147.Peters SP, Kunselman SJ, Icitovic N, Moore WC, Pascual R, Ameredes BT, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med. 2010;363:1715–26. doi: 10.1056/NEJMoa1008770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bateman ED, Kornmann O, Schmidt P, Pivovarova A, Engel M, Fabbri LM. Tiotropium is noninferior to salmeterol in maintaining improved lung function in B16-Arg/Arg patients with asthma. J Allergy Clin Immunol. 2011;128:315–22. doi: 10.1016/j.jaci.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 149.Smith LJ. Anticholinergics for patients with asthma? N Engl J Med. 2010;363:1764–5. doi: 10.1056/NEJMe1009429. [DOI] [PubMed] [Google Scholar]
- 150.Pauwels RA, Löfdahl CG, Postma DS, Tattersfield AE, O’Byrne P, Barnes PJ, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. N Engl J Med. 1997;337:1405–11. doi: 10.1056/NEJM199711133372001. [DOI] [PubMed] [Google Scholar]
- 151.Kerstjens HA, Disse B, Schröder-Babo W, Bantje TA, Gahlemann M, Sigmund R, et al. Tiotropium improves lung function in patients with severe uncontrolled asthma: A randomized controlled trial. J Allergy Clin Immunol. 2011;128:308–14. doi: 10.1016/j.jaci.2011.04.039. [DOI] [PubMed] [Google Scholar]
- 152.Kerstjens HA, Engel M, Dahl R, Paggiaro P, Beck E, Vandewalker M, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med. 2012;367:1198–207. doi: 10.1056/NEJMoa1208606. [DOI] [PubMed] [Google Scholar]
- 153.Virchow JC, Jr, Prasse A, Naya I, Summerton L, Harris A. Zafirlukast improves asthma control in patients receiving high-dose inhaled corticosteroids. Am J Respir Crit Care Med. 2000;162(2 Pt 1):578–85. doi: 10.1164/ajrccm.162.2.9905041. [DOI] [PubMed] [Google Scholar]
- 154.American Lung Association Asthma Clinical Research Centers. Clinical trial of low-dose theophylline and montelukast in patients with poorly controlled asthma. Am J Respir Crit Care Med. 2007;175:235–42. doi: 10.1164/rccm.200603-416OC. [DOI] [PubMed] [Google Scholar]
- 155.Rivington RN, Boulet LP, Côté J, Kreisman H, Small DI, Alexander M, et al. Efficacy of Uniphyl, salbutamol, and their combination in asthmatic patients on high-dose inhaled steroids. Am J Respir Crit Care Med. 1995;151(2 Pt 1):325–32. doi: 10.1164/ajrccm.151.2.7842186. [DOI] [PubMed] [Google Scholar]
- 156.Poon AH, Hamid Q. Personalized medicine for asthma: Are we there yet? Ann Thorac Med. 2012;7:55–6. doi: 10.4103/1817-1737.94519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Al-Hajjaj MS. Difficult-to-treat asthma, is it really difficult? Ann Thorac Med. 2011;6:1–2. doi: 10.4103/1817-1737.74268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ignacio-Garcia JM, Gonzalez-Santos P. Asthma self-management education program by home monitoring of peak expiratory flow. Am J Respir Crit Care Med. 1995;151(2 Pt 1):353–9. doi: 10.1164/ajrccm.151.2.7842191. [DOI] [PubMed] [Google Scholar]
- 159.Hawkins G, McMahon AD, Twaddle S, Wood SF, Ford I, Thomson NC. Stepping down inhaled corticosteroids in asthma: Randomised controlled trial. BMJ. 2003;326:1115. doi: 10.1136/bmj.326.7399.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Powell H, Gibson PG. High dose versus low dose inhaled corticosteroid as initial starting dose for asthma in adults and children. Cochrane Database Syst Rev. 2004;2:CD004109. doi: 10.1002/14651858.CD004109.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Boulet LP, Drollmann A, Magyar P, Timar M, Knight A, Engelstätter R, et al. Comparative efficacy of once-daily ciclesonide and budesonide in the treatment of persistent asthma. Respir Med. 2006;100:785–94. doi: 10.1016/j.rmed.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 162.Rank MA, Hagan JB, Park MA, Podjasek JC, Samant SA, Volcheck GW, et al. The risk of asthma exacerbation after stopping low-dose inhaled corticosteroids: A systematic review and meta-analysis of randomized controlled trials. J Allergy Clin Immunol. 2013;131:724–9. doi: 10.1016/j.jaci.2012.11.038. [DOI] [PubMed] [Google Scholar]
- 163.Brozek JL, Kraft M, Krishnan JA, Cloutier MM, Lazarus SC, Li JT, et al. Long-acting ß2-agonist step-off in patients with controlled asthma. Arch Intern Med. 2012;172:1365–75. doi: 10.1001/archinternmed.2012.3250. [DOI] [PubMed] [Google Scholar]
- 164.Masoli M, Weatherall M, Holt S, Beasley R. Budesonide once versus twice-daily administration: Meta-analysis. Respirology. 2004;9:528–34. doi: 10.1111/j.1440-1843.2004.00635.x. [DOI] [PubMed] [Google Scholar]
- 165.Bateman ED, Fairall L, Lombardi DM, English R. Budesonide/formoterol and formoterol provide similar rapid relief in patients with acute asthma showing refractoriness to salbutamol. Respir Res. 2006;7:13. doi: 10.1186/1465-9921-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Randell TL, Donaghue KC, Ambler GR, Cowell CT, Fitzgerald DA, van Asperen PP. Safety of the newer inhaled corticosteroids in childhood asthma. Paediatr Drugs. 2003;5:481–504. doi: 10.2165/00128072-200305070-00005. [DOI] [PubMed] [Google Scholar]
- 167.Cox L, Nelson H, Lockey R, Calabria C, Chacko T, Finegold I, et al. Allergen immunotherapy: A practice parameter third update. J Allergy Clin Immunol. 2011;127(1 Suppl):S1–55. doi: 10.1016/j.jaci.2010.09.034. [DOI] [PubMed] [Google Scholar]
- 168.Madsen F. EAACI ‘Standards for practical allergen-specific immunotherapy’. Allergy. 2007;62:332. doi: 10.1111/j.1398-9995.2007.01302.x. [DOI] [PubMed] [Google Scholar]
- 169.Alvarez-Cuesta E, Bousquet J, Canonica GW, Durham SR, Malling HJ, Valovirta E; EAACI, et al. Standards for practical allergen-specific immunotherapy. Allergy. 2006;61(Suppl 82):1–20. doi: 10.1111/j.1398-9995.2006.01219_1.x. [DOI] [PubMed] [Google Scholar]
- 170.Akdis C, Papadopoulos N, Cardona V. Fighting allergies beyond symptoms: The European declaration on immunotherapy. Eur J Immunol. 2011;41:2802–4. doi: 10.1002/eji.201190061. [DOI] [PubMed] [Google Scholar]
- 171.Calderon MA, Demoly P, Gerth van Wijk R, Bousquet J, Sheikh A, Frew A, et al. EAACI: A European declaration on immunotherapy. Designing the future of allergen specific immunotherapy. Clin Transl Allergy. 2012;2:20. doi: 10.1186/2045-7022-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Moote W, Kim H. Allergen-specific immunotherapy. Allergy Asthma Clin Immunol. 2011;7(Suppl 1):S5. doi: 10.1186/1710-1492-7-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Allergen immunotherapy: A practice parameter second update. J Allergy Clin Immunol. 2007;120(3 Suppl):S25–85. doi: 10.1016/j.jaci.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 174.Jacobsen L. Preventive aspects of immunotherapy: Prevention for children at risk of developing asthma. Ann Allergy Asthma Immunol. 2001;87(1 Suppl 1):43–6. doi: 10.1016/s1081-1206(10)62194-1. [DOI] [PubMed] [Google Scholar]
- 175.Abramson MJ, Puy RM, Weiner JM. Injection allergen immunotherapy for asthma. Cochrane Database Syst Rev. 2010 Aug 4;8:CD001186. doi: 10.1002/14651858.CD001186.pub2. [DOI] [PubMed] [Google Scholar]
- 176.Kopp MV. Role of immunmodulators in allergen-specific immunotherapy. Allergy. 2011;66:792–7. doi: 10.1111/j.1398-9995.2011.02553.x. [DOI] [PubMed] [Google Scholar]
- 177.Sandström T. Omalizumab in the management of patients with allergic (IgE-mediated) asthma. J Asthma Allergy. 2009;2:49–62. doi: 10.2147/jaa.s3116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Stock P, Rolinck-Werninghaus C, Wahn U, Hamelmann E. The role of anti-IgE therapy in combination with allergen specific immunotherapy for seasonal allergic rhinitis. BioDrugs. 2007;21:403–10. doi: 10.2165/00063030-200721060-00007. [DOI] [PubMed] [Google Scholar]
- 179.Abramson MJ, Bailey MJ, Couper FJ, Driver JS, Drummer OH, Forbes AB, et al. Are asthma medications and management related to deaths from asthma? Am J Respir Crit Care Med. 2001;163:12–8. doi: 10.1164/ajrccm.163.1.9910042. [DOI] [PubMed] [Google Scholar]
- 180.Omachi TA, Iribarren C, Sarkar U, Tolstykh I, Yelin EH, Katz PP, et al. Risk factors for death in adults with severe asthma. Ann Allergy Asthma Immunol. 2008;101:130–6. doi: 10.1016/S1081-1206(10)60200-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Hessel PA, Mitchell I, Tough S, Green FH, Cockcroft D, Kepron W, et al. Risk factors for death from asthma. Prairie Provinces Asthma Study Group. Ann Allergy Asthma Immunol. 1999;83:362–8. doi: 10.1016/s1081-1206(10)62832-3. [DOI] [PubMed] [Google Scholar]
- 182.Plaza V, Serrano J, Picado C, Sanchis J High Risk Asthma Research Group. Frequency and clinical characteristics of rapid-onset fatal and near-fatal asthma. Eur Respir J. 2002;19:846–52. doi: 10.1183/09031936.02.00241502. [DOI] [PubMed] [Google Scholar]
- 183.Mitchell I, Tough SC, Semple LK, Green FH, Hessel PA. Near-fatal asthma: A population-based study of risk factors. Chest. 2002;121:1407–13. doi: 10.1378/chest.121.5.1407. [DOI] [PubMed] [Google Scholar]
- 184.Al-Dorzi HM, Al-Shammary HA, Al-Shareef SY, Tamim HM, Shammout K, Al Dawood A, et al. Risk factors, management and outcomes of patients admitted with near fatal asthma to a tertiary care hospital in Riyadh. Ann Thorac Med. 2014;9:33–8. doi: 10.4103/1817-1737.124441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Magadle R, Berar-Yanay N, Weiner P. The risk of hospitalization and near-fatal and fatal asthma in relation to the perception of dyspnea. Chest. 2002;121:329–33. doi: 10.1378/chest.121.2.329. [DOI] [PubMed] [Google Scholar]
- 186.Reddel H, Ware S, Marks G, Salome C, Jenkins C, Woolcock A. Differences between asthma exacerbations and poor asthma control. Lancet. 1999;353:364–9. doi: 10.1016/S0140-6736(98)06128-5. [DOI] [PubMed] [Google Scholar]
- 187.Badminton MN, Campbell AK, Rembold CM. Differential regulation of nuclear and cytosolic Ca2+in HeLa cells. J Biol Chem. 1996;271:31210–4. doi: 10.1074/jbc.271.49.31210. [DOI] [PubMed] [Google Scholar]
- 188.Harrison DE, Slack R, Berrill WT, Wright SC. Results of a national confidential enquiry into asthma deaths. Asthma J. 2000;5:180–6. [Google Scholar]
- 189.Spitzer WO, Suissa S, Ernst P, Horwitz RI, Habbick B, Cockcroft D, et al. The use of beta-agonists and the risk of death and near death from asthma. N Engl J Med. 1992;326:501–6. doi: 10.1056/NEJM199202203260801. [DOI] [PubMed] [Google Scholar]
- 190.Suissa S, Blais L, Ernst P. Patterns of increasing beta-agonist use and the risk of fatal or near-fatal asthma. Eur Respir J. 1994;7:1602–9. doi: 10.1183/09031936.94.07091602. [DOI] [PubMed] [Google Scholar]
- 191.Ramnath VR, Clark S, Camargo CA., Jr Multicenter study of clinical features of sudden-onset versus slower-onset asthma exacerbations requiring hospitalization. Respir Care. 2007;52:1013–20. [PubMed] [Google Scholar]
- 192.Barr RG, Woodruff PG, Clark S, Camargo CA., Jr Sudden-onset asthma exacerbations: Clinical features, response to therapy, and 2-week follow-up. Multicenter Airway Research Collaboration (MARC) investigators. Eur Respir J. 2000;15:266–73. doi: 10.1034/j.1399-3003.2000.15b08.x. [DOI] [PubMed] [Google Scholar]
- 193.Kolbe J, Fergusson W, Garrett J. Rapid onset asthma: A severe but uncommon manifestation. Thorax. 1998;53:241–7. doi: 10.1136/thx.53.4.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Kolbe J, Fergusson W, Vamos M, Garrett J. Case-control study of severe life threatening asthma (SLTA) in adults: Psychological factors. Thorax. 2002;57:317–22. doi: 10.1136/thorax.57.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Al-Dawood KM. Pattern and risk factors associated with hospital emergency visits among schoolboys with bronchial asthma in Al-Khobar. Ann Saudi Med. 2002;22:29–33. doi: 10.5144/0256-4947.2002.29. [DOI] [PubMed] [Google Scholar]
- 196.Courtney AU, McCarter DF, Pollart SM. Childhood asthma: Treatment update. Am Fam Physician. 2005;71:1959–68. [PubMed] [Google Scholar]
- 197.Rowe BH, Keller JL, Oxman AD. Effectiveness of steroid therapy in acute exacerbations of asthma: A meta-analysis. Am J Emerg Med. 1992;10:301–10. doi: 10.1016/0735-6757(92)90007-k. [DOI] [PubMed] [Google Scholar]
- 198.O’Driscoll BR, Howard LS, Davison AG British Thoracic Society. BTS guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Suppl 6):vi1–68. doi: 10.1136/thx.2008.102947. [DOI] [PubMed] [Google Scholar]
- 199.Chien JW, Ciufo R, Novak R, Skowronski M, Nelson J, Coreno A, et al. Uncontrolled oxygen administration and respiratory failure in acute asthma. Chest. 2000;117:728–33. doi: 10.1378/chest.117.3.728. [DOI] [PubMed] [Google Scholar]
- 200.Rodrigo GJ, Rodriquez Verde M, Peregalli V, Rodrigo C. Effects of short-term 28% and 100% oxygen on PaCO2 and peak expiratory flow rate in acute asthma: A randomized trial. Chest. 2003;124:1312–7. doi: 10.1378/chest.124.4.1312. [DOI] [PubMed] [Google Scholar]
- 201.McFadden ER., Jr Critical appraisal of the therapy of asthma – An idea whose time has come. Am Rev Respir Dis. 1986;133:723–4. doi: 10.1164/arrd.1986.133.5.723. [DOI] [PubMed] [Google Scholar]
- 202.Kerem E, Levison H, Schuh S, O’Brodovich H, Reisman J, Bentur L, et al. Efficacy of albuterol administered by nebulizer versus spacer device in children with acute asthma. J Pediatr. 1993;123:313–7. doi: 10.1016/s0022-3476(05)81710-x. [DOI] [PubMed] [Google Scholar]
- 203.Rodrigo C, Rodrigo G. Salbutamol treatment of acute severe asthma in the ED: MDI versus hand-held nebulizer. Am J Emerg Med. 1998;16:637–42. doi: 10.1016/s0735-6757(98)90164-4. [DOI] [PubMed] [Google Scholar]
- 204.Cates CJ, Crilly JA, Rowe BH. Holding chambers (spacers) versus nebulisers for beta-agonist treatment of acute asthma. Cochrane Database Syst Rev 2006; Cochrane Database Syst Rev. 2006 Apr 19;2:CD000052. doi: 10.1002/14651858.CD000052.pub2. [DOI] [PubMed] [Google Scholar]
- 205.Cates CC, Bara A, Crilly JA, Rowe BH. Holding chambers versus nebulisers for beta-agonist treatment of acute asthma. Cochrane Database Syst Rev. 2003;3:CD000052. doi: 10.1002/14651858.CD000052. [DOI] [PubMed] [Google Scholar]
- 206.Rossing TH, Fanta CH, Goldstein DH, Snapper JR, McFadden ER., Jr Emergency therapy of asthma: Comparison of the acute effects of parenteral and inhaled sympathomimetics and infused aminophylline. Am Rev Respir Dis. 1980;122:365–71. doi: 10.1164/arrd.1980.122.3.365. [DOI] [PubMed] [Google Scholar]
- 207.Rowe BH, Spooner C, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 2001;1:CD002178. doi: 10.1002/14651858.CD002178. [DOI] [PubMed] [Google Scholar]
- 208.Rowe BH, Spooner C, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev 2000; Cochrane Database Syst Rev. 2001;1:CD002178. doi: 10.1002/14651858.CD002178. [DOI] [PubMed] [Google Scholar]
- 209.Tokuda Y, Miyagi S. Oxygen treatment for acute severe asthma. Home oxygenation would be more effective. BMJ. 2001;323:1069. [PMC free article] [PubMed] [Google Scholar]
- 210.Inwald D, Roland M, Kuitert L, McKenzie SA, Petros A. Oxygen treatment for acute severe asthma. BMJ. 2001;323:98–100. doi: 10.1136/bmj.323.7304.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Gleeson JG, Green S, Price JF. Air or oxygen as driving gas for nebulised salbutamol. Arch Dis Child. 1988;63:900–4. doi: 10.1136/adc.63.8.900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Douglas JG, Rafferty P, Fergusson RJ, Prescott RJ, Crompton GK, Grant IW. Nebulised salbutamol without oxygen in severe acute asthma: How effective and how safe? Thorax. 1985;40:180–3. doi: 10.1136/thx.40.3.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Lanes SF, Garrett JE, Wentworth CE rd, Fitzgerald JM, Karpel JP. The effect of adding ipratropium bromide to salbutamol in the treatment of acute asthma: A pooled analysis of three trials. Chest. 1998;114:365–72. doi: 10.1378/chest.114.2.365. [DOI] [PubMed] [Google Scholar]
- 214.Chassany O, Fullerton S. Meta-analysis of the effects of ipratropium bromide in adults with acute asthma. Am J Med. 2000;108:596–7. doi: 10.1016/s0002-9343(00)00298-9. [DOI] [PubMed] [Google Scholar]
- 215.Rodrigo G, Rodrigo C, Burschtin O. A meta-analysis of the effects of ipratropium bromide in adults with acute asthma. Am J Med. 1999;107:363–70. doi: 10.1016/s0002-9343(99)00243-0. [DOI] [PubMed] [Google Scholar]
- 216.Stoodley RG, Aaron SD, Dales RE. The role of ipratropium bromide in the emergency management of acute asthma exacerbation: A metaanalysis of randomized clinical trials. Ann Emerg Med. 1999;34:8–18. doi: 10.1016/s0196-0644(99)70266-0. [DOI] [PubMed] [Google Scholar]
- 217.Rowe BH, Spooner CH, Ducharme FM, Bretzlaff JA, Bota GW. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst Rev. 2001;1:CD000195. doi: 10.1002/14651858.CD000195. [DOI] [PubMed] [Google Scholar]
- 218.Rowe BH, Bretzlaff JA, Bourdon C, Bota GW, Camargo CA., Jr Magnesium sulfate for treating exacerbations of acute asthma in the emergency department. Cochrane Database Syst Rev 2000; Cochrane Database Syst Rev. 2000;2:CD001490. doi: 10.1002/14651858.CD001490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Alzeer AH, Al Otair HA, Khurshid SM, Badrawy SE, Bakir BM. A case of near fatal asthma: The role of ECMO as rescue therapy. Ann Thorac Med. 2015;10:143–5. doi: 10.4103/1817-1737.152461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Shrestha M, Bidadi K, Gourlay S, Hayes J. Continuous vs intermittent albuterol, at high and low doses, in the treatment of severe acute asthma in adults. Chest. 1996;110:42–7. doi: 10.1378/chest.110.1.42. [DOI] [PubMed] [Google Scholar]
- 221.Lin RY, Sauter D, Newman T, Sirleaf J, Walters J, Tavakol M. Continuous versus intermittent albuterol nebulization in the treatment of acute asthma. Ann Emerg Med. 1993;22:1847–53. doi: 10.1016/s0196-0644(05)80412-3. [DOI] [PubMed] [Google Scholar]
- 222.Fitzgerald JM, Baynham R, Powles AC. Use of oxygen therapy for adult patients outside the critical care areas of a university hospital. Lancet. 1988;1:981–3. doi: 10.1016/s0140-6736(88)91791-6. [DOI] [PubMed] [Google Scholar]
- 223.Rowe BH, Spooner CH, Ducharme FM, Bretzlaff JA, Bota GW. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst Rev. 2001;1:CD000195. doi: 10.1002/14651858.CD000195. [DOI] [PubMed] [Google Scholar]
- 224.Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):169S–73S. doi: 10.1378/chest.129.1_suppl.169S. [DOI] [PubMed] [Google Scholar]
- 225.Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):75S–9S. doi: 10.1378/chest.129.1_suppl.75S. [DOI] [PubMed] [Google Scholar]
- 226.Desai D, Brightling C. Cough due to asthma, cough-variant asthma and non-asthmatic eosinophilic bronchitis. Otolaryngol Clin North Am. 2010;43:123–30. doi: 10.1016/j.otc.2009.11.006. x. [DOI] [PubMed] [Google Scholar]
- 227.Morice AH, McGarvey L, Pavord I British Thoracic Society Cough Guideline Group. Recommendations for the management of cough in adults. Thorax. 2006;61(Suppl 1):i1–24. doi: 10.1136/thx.2006.065144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Spector SL, Tan RA. Effectiveness of montelukast in the treatment of cough variant asthma. Ann Allergy Asthma Immunol. 2004;93:232–6. doi: 10.1016/S1081-1206(10)61493-7. [DOI] [PubMed] [Google Scholar]
- 229.Cruz AA, Popov T, Pawankar R, Annesi-Maesano I, Fokkens W, Kemp J, et al. Common characteristics of upper and lower airways in rhinitis and asthma: ARIA update, in collaboration with GA (2) LEN. Allergy. 2007;62(Suppl 84):1–41. doi: 10.1111/j.1398-9995.2007.01551.x. [DOI] [PubMed] [Google Scholar]
- 230.Cheng L, Zhang L. Introduction to allergic rhinitis and its impact on asthma (ARIA) guidelines 2010 revision. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2011;46:437–9. [PubMed] [Google Scholar]
- 231.Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126:466–76. doi: 10.1016/j.jaci.2010.06.047. [DOI] [PubMed] [Google Scholar]
- 232.Sears MR, Lötvall J. Past, present and future – Beta2-adrenoceptor agonists in asthma management. Respir Med. 2005;99:152–70. doi: 10.1016/j.rmed.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 233.de Benedictis FM, del Giudice MM, Forenza N, Decimo F, de Benedictis D, Capristo A. Lack of tolerance to the protective effect of montelukast in exercise-induced bronchoconstriction in children. Eur Respir J. 2006;28:291–5. doi: 10.1183/09031936.06.00020606. [DOI] [PubMed] [Google Scholar]
- 234.Szczeklik A, Stevenson DD. Aspirin-induced asthma: Advances in pathogenesis, diagnosis, and management. J Allergy Clin Immunol. 2003;111:913–21. doi: 10.1067/mai.2003.1487. [DOI] [PubMed] [Google Scholar]
- 235.Berges-Gimeno MP, Simon RA, Stevenson DD. Long-term treatment with aspirin desensitization in asthmatic patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2003;111:180–6. doi: 10.1067/mai.2003.7. [DOI] [PubMed] [Google Scholar]
- 236.Stevenson DD. Diagnosis, prevention, and treatment of adverse reactions to aspirin and nonsteroidal anti-inflammatory drugs. J Allergy Clin Immunol. 1984;74(4 Pt 2):617–22. doi: 10.1016/0091-6749(84)90115-5. [DOI] [PubMed] [Google Scholar]
- 237.Park JS, Jang AS, Park SW, Lee YM, Uh ST, Kim YH, et al. Protection of leukotriene receptor antagonist against aspirin-induced bronchospasm in asthmatics. Allergy Asthma Immunol Res. 2010;2:48–54. doi: 10.4168/aair.2010.2.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Al-Asoom LI, Al-Rubaish A, Al-Quorain AA, Qutub H, El-Munshid HA. The association of gastroesophageal reflux with bronchial asthma. Can asthma also trigger reflux? Hepatogastroenterology. 2006;53:64–72. [PubMed] [Google Scholar]
- 239.Bresci G, Sacco R. Pulmonary or otolaryngologic extraesophageal manifestations in patients with gastroesophageal reflux disease. World J Gastrointest Endosc. 2010;2:47–9. doi: 10.4253/wjge.v2.i2.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Gaude GS. Pulmonary manifestations of gastroesophageal reflux disease. Ann Thorac Med. 2009;4:115–23. doi: 10.4103/1817-1737.53347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Champion GL, Richter JE. Atypical presentation of gastroesophageal reflux disease: Chest pain, pulmonary, and ear, nose, throat manifestations. Gastroenterologist. 1993;1:18–33. [PubMed] [Google Scholar]
- 242.Asano K, Suzuki H. Silent acid reflux and asthma control. N Engl J Med. 2009;360:1551–3. doi: 10.1056/NEJMe0900117. [DOI] [PubMed] [Google Scholar]
- 243.Schatz M, Harden K, Forsythe A, Chilingar L, Hoffman C, Sperling W, et al. The course of asthma during pregnancy, post partum, and with successive pregnancies: A prospective analysis. J Allergy Clin Immunol. 1988;81:509–17. [PubMed] [Google Scholar]
- 244.Blais L, Kettani FZ, Forget A, Beauchesne MF, Lemière C. Asthma exacerbations during the first trimester of pregnancy and congenital malformations: Revisiting the association in a large representative cohort. Thorax. 2015;70:647–52. doi: 10.1136/thoraxjnl-2014-206634. [DOI] [PubMed] [Google Scholar]
- 245.Murphy VE, Gibson PG, Smith R, Clifton VL. Asthma during pregnancy: Mechanisms and treatment implications. Eur Respir J. 2005;25:731–50. doi: 10.1183/09031936.05.00085704. [DOI] [PubMed] [Google Scholar]
- 246.Holland SM, Thomson KD. Acute severe asthma presenting in late pregnancy. Int J Obstet Anesth. 2006;15:75–8. doi: 10.1016/j.ijoa.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 247.Hanania NA, Belfort MA. Acute asthma in pregnancy. Crit Care Med. 2005;33(10 Suppl):S319–24. doi: 10.1097/01.ccm.0000182789.14710.a1. [DOI] [PubMed] [Google Scholar]
- 248.Smy L, Chan AC, Bozzo P, Koren G. Is it safe to use inhaled corticosteroids in pregnancy? Can Fam Physician. 2014;60:809. [PMC free article] [PubMed] [Google Scholar]
- 249.Rahimi R, Nikfar S, Abdollahi M. Meta-analysis finds use of inhaled corticosteroids during pregnancy safe: A systematic meta-analysis review. Hum Exp Toxicol. 2006;25:447–52. doi: 10.1191/0960327106het647oa. [DOI] [PubMed] [Google Scholar]
- 250.Gluck JC, Gluck PA. The effect of pregnancy on the course of asthma. Immunol Allergy Clin North Am. 2006;26:63–80. doi: 10.1016/j.iac.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 251.Wendel PJ, Ramin SM, Barnett-Hamm C, Rowe TF, Cunningham FG. Asthma treatment in pregnancy: A randomized controlled study. Am J Obstet Gynecol. 1996;175:150–4. doi: 10.1016/s0002-9378(96)70265-x. [DOI] [PubMed] [Google Scholar]
- 252.Lao TT, Huengsburg M. Labour and delivery in mothers with asthma. Eur J Obstet Gynecol Reprod Biol. 1990;35:183–90. doi: 10.1016/0028-2243(90)90160-3. [DOI] [PubMed] [Google Scholar]
- 253.Arora N, Mahajan K, Jana N, Maiti TK, Mandal D, Pandey R. Successful pregnancy outcome among women with end-stage renal disease requiring haemodialysis. J Indian Med Assoc. 2009;107:237–8. [PubMed] [Google Scholar]
- 254.Fitzsimons R, Greenberger PA, Patterson R. Outcome of pregnancy in women requiring corticosteroids for severe asthma. J Allergy Clin Immunol. 1986;78:349–53. doi: 10.1016/s0091-6749(86)80088-4. [DOI] [PubMed] [Google Scholar]
- 255.Perlow JH, Montgomery D, Morgan MA, Towers CV, Porto M. Severity of asthma and perinatal outcome. Am J Obstet Gynecol. 1992;167(4 Pt 1):963–7. doi: 10.1016/s0002-9378(12)80020-2. [DOI] [PubMed] [Google Scholar]
- 256.Levy ML, Nicholson PJ. Occupational asthma case finding: A role for primary care. Br J Gen Pract. 2004;54:731–3. [PMC free article] [PubMed] [Google Scholar]
- 257.Baur X, Aasen TB, Burge PS, Heederik D, Henneberger PK, Maestrelli P, et al. The management of work-related asthma guidelines: A broader perspective. Eur Respir Rev. 2012;21:125–39. doi: 10.1183/09059180.00004711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Legiest B, Nemery B. Management of work-related asthma: Guidelines and challenges. Eur Respir Rev. 2012;21:79–81. doi: 10.1183/09059180.00002912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Currie GP, Douglas JG, Heaney LG. Difficult to treat asthma in adults. BMJ. 2009;338:b494. doi: 10.1136/bmj.b494. [DOI] [PubMed] [Google Scholar]
- 260.Sullivan SD, Rasouliyan L, Russo PA, Kamath T, Chipps BE TENOR Study Group. Extent, patterns, and burden of uncontrolled disease in severe or difficult-to-treat asthma. Allergy. 2007;62:126–33. doi: 10.1111/j.1398-9995.2006.01254.x. [DOI] [PubMed] [Google Scholar]
- 261.Serra-Batlles J, Plaza V, Morejón E, Comella A, Brugués J. Costs of asthma according to the degree of severity. Eur Respir J. 1998;12:1322–6. doi: 10.1183/09031936.98.12061322. [DOI] [PubMed] [Google Scholar]
- 262.Chen H, Blanc PD, Hayden ML, Bleecker ER, Chawla A, Lee JH TENOR Study Group. Assessing productivity loss and activity impairment in severe or difficult-to-treat asthma. Value Health. 2008;11:231–9. doi: 10.1111/j.1524-4733.2007.00229.x. [DOI] [PubMed] [Google Scholar]
- 263.Lee JH, Haselkorn T, Borish L, Rasouliyan L, Chipps BE, Wenzel SE. Risk factors associated with persistent airflow limitation in severe or difficult-to-treat asthma: Insights from the TENOR study. Chest. 2007;132:1882–9. doi: 10.1378/chest.07-0713. [DOI] [PubMed] [Google Scholar]
- 264.Butler C, Heaney LG. Risk factors of frequent exacerbations in difficult-to-treat asthma. Eur Respir J. 2006;27:1324–5. doi: 10.1183/09031936.06.00022606. [DOI] [PubMed] [Google Scholar]
- 265.Gaga M, Papageorgiou N, Yiourgioti G, Karydi P, Liapikou A, Bitsakou H, et al. Risk factors and characteristics associated with severe and difficult to treat asthma phenotype: An analysis of the ENFUMOSA group of patients based on the ECRHS questionnaire. Clin Exp Allergy. 2005;35:954–9. doi: 10.1111/j.1365-2222.2005.02281.x. [DOI] [PubMed] [Google Scholar]
- 266.Sullivan SD, Wenzel SE, Bresnahan BW, Zheng B, Lee JH, Pritchard M, et al. Association of control and risk of severe asthma-related events in severe or difficult-to-treat asthma patients. Allergy. 2007;62:655–60. doi: 10.1111/j.1398-9995.2007.01383.x. [DOI] [PubMed] [Google Scholar]
- 267.Robinson DS, Campbell DA, Durham SR, Pfeffer J, Barnes PJ, Chung KF, et al. Systematic assessment of difficult-to-treat asthma. Eur Respir J. 2003;22:478–83. doi: 10.1183/09031936.03.00017003. [DOI] [PubMed] [Google Scholar]
- 268.Natarajan S, Subramanian P. Allergic bronchopulmonary aspergillosis: A clinical review of 24 patients: Are we right in frequent serologic monitoring? Ann Thorac Med. 2014;9:216–20. doi: 10.4103/1817-1737.140130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Jani AL, Hamilos DL. Current thinking on the relationship between rhinosinusitis and asthma. J Asthma. 2005;42:1–7. doi: 10.1081/jas-200044744. [DOI] [PubMed] [Google Scholar]
- 270.Heaney LG, Brightling CE, Menzies-Gow A, Stevenson M, Niven RM British Thoracic Society Difficult Asthma Network. Refractory asthma in the UK: Cross-sectional findings from a UK multicentre registry. Thorax. 2010;65:787–94. doi: 10.1136/thx.2010.137414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Adcock IM, Lane SJ, Brown CR, Peters MJ, Lee TH, Barnes PJ. Differences in binding of glucocorticoid receptor to DNA in steroid-resistant asthma. J Immunol. 1995;154:3500–5. [PubMed] [Google Scholar]
- 272.Barnes PJ. Corticosteroid resistance in airway disease. Proc Am Thorac Soc. 2004;1:264–8. doi: 10.1513/pats.200402-014MS. [DOI] [PubMed] [Google Scholar]
- 273.Ayres JG. Pseudo-steroid resistant asthma. Thorax. 1999;54:956. doi: 10.1136/thx.54.10.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Roberts NJ, Robinson DS, Partridge MR. How is difficult asthma managed? Eur Respir J. 2006;28:968–73. doi: 10.1183/09031936.06.00003706. [DOI] [PubMed] [Google Scholar]
- 275.Smits W, Letz K. Managing difficult-to-treat asthma: Lessons from a center of excellence in allergy and asthma care. J Med Pract Manage. 2007;22:350–8. [PubMed] [Google Scholar]
- 276.Saji J, Arai M, Yamamoto T, Mineshita M, Miyazawa T. Efficacy of omalizumab in patients with severe asthma using the asthma health questionnaire and asthma control test. Arerugi. 2014;63:1338–47. [PubMed] [Google Scholar]
- 277.Storms W, Bowdish MS, Farrar JR. Omalizumab and asthma control in patients with moderate-to-severe allergic asthma: A 6-year pragmatic data review. Allergy Asthma Proc. 2012;33:172–7. doi: 10.2500/aap.2012.33.3527. [DOI] [PubMed] [Google Scholar]
- 278.Campbell JD, Blough DK, Sullivan SD. Comparison of guideline-based control definitions and associations with outcomes in severe or difficult-to-treat asthma. Ann Allergy Asthma Immunol. 2008;101:474–81. doi: 10.1016/S1081-1206(10)60285-2. [DOI] [PubMed] [Google Scholar]
- 279.Haldar P, Brightling CE, Hargadon B, Gupta S, Monteiro W, Sousa A, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med. 2009;360:973–84. doi: 10.1056/NEJMoa0808991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.FDA NUCALA® (Mepolizumab) for Treatment of Patients with Severe Asthma with Eosinophilic Inflammation-BLA125526. 2015. [accessed on 2015 Jul 12]. Available at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Pulmonary-AllergyDrugsAdvisoryCommittee/UCM450248.pdf .
- 281.Iyer VN, Lim KG. Bronchial thermoplasty: Where there is smoke, there is fire. Allergy Asthma Proc. 2015;36:251–5. doi: 10.2500/aap.2015.36.3857. [DOI] [PubMed] [Google Scholar]
- 282.Michaud G, Ernst A. Counterpoint: Efficacy of bronchial thermoplasty for patients with severe asthma. Is there sufficient evidence? Not yet Chest. 2011;140:576–7. doi: 10.1378/chest.11-1390. [DOI] [PubMed] [Google Scholar]
- 283.Wu Q, Xing Y, Zhou X, Wang D. Meta-analysis of the efficacy and safety of bronchial thermoplasty in patients with moderate-to-severe persistent asthma. J Int Med Res. 2011;39:10–22. doi: 10.1177/147323001103900102. [DOI] [PubMed] [Google Scholar]
- 284.Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: What are its features and how important is it? Thorax. 2009;64:728–35. doi: 10.1136/thx.2008.108027. [DOI] [PubMed] [Google Scholar]
- 285.Kauppi P, Kupiainen H, Lindqvist A, Tammilehto L, Kilpeläinen M, Kinnula VL, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011;48:279–85. doi: 10.3109/02770903.2011.555576. [DOI] [PubMed] [Google Scholar]
- 286.Hardin M, Silverman EK, Barr RG, Hansel NN, Schroeder JD, Make BJ, et al. The clinical features of the overlap between COPD and asthma. Respir Res. 2011;12:127. doi: 10.1186/1465-9921-12-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Asthma GIF; 2015. [Last accessed on 2015 Aug. 14]. Asthma GIF. The Global Strategy for Asthma Management and Prevention. Available at: http://www.ginasthma.org/documents/4 . [Google Scholar]
- 288.Louie S, Zeki AA, Schivo M, Chan AL, Yoneda KY, Avdalovic M, et al. The asthma-chronic obstructive pulmonary disease overlap syndrome: Pharmacotherapeutic considerations. Expert Rev Clin Pharmacol. 2013;6:197–219. doi: 10.1586/ecp.13.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Al-Kassimi FA, Alhamad EH, Al-Hajjaj MS, Abba AA, Raddaoui E, Shaikh SA. Abrupt withdrawal of inhaled corticosteroids does not result in spirometric deterioration in chronic obstructive pulmonary disease: Effect of phenotyping? Ann Thorac Med. 2012;7:238–42. doi: 10.4103/1817-1737.102185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma (GINA) Program. The global burden of asthma: Executive summary of the GINA Dissemination Committee report. Allergy. 2004;59:469–78. doi: 10.1111/j.1398-9995.2004.00526.x. [DOI] [PubMed] [Google Scholar]
- 291.Edmonds ML, Camargo CA, Jr, Pollack CV, Jr, Rowe BH. Early use of inhaled corticosteroids in the emergency department treatment of acute asthma. Cochrane Database Syst Rev. 2003;3:CD002308. doi: 10.1002/14651858.CD002308. [DOI] [PubMed] [Google Scholar]
- 292.Denlinger LC, Sorkness CA, Chinchilli VM, Lemanske RF., Jr Guideline-defining asthma clinical trials of the National Heart, Lung, and Blood Institute's Asthma Clinical Research Network and Childhood Asthma Research and Education Network. J Allergy Clin Immunol. 2007;119:3–11. doi: 10.1016/j.jaci.2006.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Glauber JH, Fuhlbrigge AL, Finkelstein JA, Homer CJ, Weiss ST. Relationship between asthma medication and antibiotic use. Chest. 2001;120:1485–92. doi: 10.1378/chest.120.5.1485. [DOI] [PubMed] [Google Scholar]
- 294.Seear M, Wensley D, West N. How accurate is the diagnosis of exercise induced asthma among Vancouver schoolchildren? Arch Dis Child. 2005;90:898–902. doi: 10.1136/adc.2004.063974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Weinberger M. Pediatric asthma and related allergic and nonallergic diseases: Patient-oriented evidence-based essentials that matter. Pediatr Health. 2008;2:631–50. [Google Scholar]
- 296.Hederos CA, Janson S, Andersson H, Hedlin G. Chest X-ray investigation in newly discovered asthma. Pediatr Allergy Immunol. 2004;15:163–5. doi: 10.1046/j.1399-3038.2003.00098.x. [DOI] [PubMed] [Google Scholar]
- 297.Chipps BE, Bacharier LB, Harder JM. Phenotypic expressions of childhood wheezing and asthma: Implications for therapy. J Pediatr. 2011;158:878–84.e1. doi: 10.1016/j.jpeds.2011.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Fahy JV, O’Byrne PM. “Reactive airways disease”. A lazy term of uncertain meaning that should be abandoned. Am J Respir Crit Care Med. 2001;163:822–3. doi: 10.1164/ajrccm.163.4.2005049. [DOI] [PubMed] [Google Scholar]
- 299.Weinberger MI, Sirey JA, Bruce ML, Heo M, Papademetriou E, Meyers BS. Predictors of major depression six months after admission for outpatient treatment. Psychiatr Serv. 2008;59:1211–5. doi: 10.1176/appi.ps.59.10.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 1995;332:133–8. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 301.Bubshait DK, Albuali WH, Yousef AA, Obeid OE, Alkharsah KR, Hassan MI, et al. Clinical description of human bocavirus viremia in children with LRTI, Eastern Province, Saudi Arabia. Ann Thorac Med. 2015;10:146–9. doi: 10.4103/1817-1737.151437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Just J, Gouvis-Echraghi R, Couderc R, Guillemot-Lambert N, Saint-Pierre P. Novel severe wheezy young children phenotypes: Boys atopic multiple-trigger and girls nonatopic uncontrolled wheeze. J Allergy Clin Immunol. 2012;130:103–10.e8. doi: 10.1016/j.jaci.2012.02.041. [DOI] [PubMed] [Google Scholar]
- 303.Savenije OE, Kerkhof M, Koppelman GH, Postma DS. Predicting who will have asthma at school age among preschool children. J Allergy Clin Immunol. 2012;130:325–31. doi: 10.1016/j.jaci.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 304.Guilbert TW, Morgan WJ, Zeiger RS, Bacharier LB, Boehmer SJ, Krawiec M, et al. Atopic characteristics of children with recurrent wheezing at high risk for the development of childhood asthma. J Allergy Clin Immunol. 2004;114:1282–7. doi: 10.1016/j.jaci.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 305.Castro-Rodriguez JA. The Asthma Predictive Index: A very useful tool for predicting asthma in young children. J Allergy Clin Immunol. 2010;126:212–6. doi: 10.1016/j.jaci.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 306.Chang TS, Lemanske RF, Jr, Guilbert TW, Gern JE, Coen MH, Evans MD, et al. Evaluation of the modified asthma predictive index in high-risk preschool children. J Allergy Clin Immunol Pract. 2013;1:152–6. doi: 10.1016/j.jaip.2012.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Yousef AA, Al-Shamrani AS, Al-Haider SA, Said YS, Al Harbi S, Al-Harbi AS. Pediatric pulmonary services in Saudi Arabia. Ann Thorac Med. 2013;8:224–8. doi: 10.4103/1817-1737.118502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Yawn BP, Brenneman SK, Allen-Ramey FC, Cabana MD, Markson LE. Assessment of asthma severity and asthma control in children. Pediatrics. 2006;118:322–9. doi: 10.1542/peds.2005-2576. [DOI] [PubMed] [Google Scholar]
- 309.Welsh EJ, Hasan M, Li P. Home-based educational interventions for children with asthma. Cochrane Database Syst Rev. 2011 Oct 5;10:CD008469. doi: 10.1002/14651858.CD008469.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Wolf FM, Guevara JP, Grum CM, Clark NM, Cates CJ. Educational interventions for asthma in children. Cochrane Database Syst Rev. 2003;1:CD000326. doi: 10.1002/14651858.CD000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Wood MR, Bolyard D. Making education count: The nurse's role in asthma education using a medical home model of care. J Pediatr Nurs. 2011;26:552–8. doi: 10.1016/j.pedn.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 312.Becker A, Lemière C, Bérubé D, Boulet LP, Ducharme FM, FitzGerald M, et al. Summary of recommendations from the Canadian Asthma Consensus guidelines, 2003. CMAJ. 2005;173(6 Suppl):S3–11. [PMC free article] [PubMed] [Google Scholar]
- 313.Nurmatov U, Devereux G, Sheikh A. Nutrients and foods for the primary prevention of asthma and allergy: Systematic review and meta-analysis. J Allergy Clin Immunol. 2011;127:724–33.e1-30. doi: 10.1016/j.jaci.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 314.Pelucchi C, Chatenoud L, Turati F, Galeone C, Moja L, Bach JF, et al. Probiotics supplementation during pregnancy or infancy for the prevention of atopic dermatitis: A meta-analysis. Epidemiology. 2012;23:402–14. doi: 10.1097/EDE.0b013e31824d5da2. [DOI] [PubMed] [Google Scholar]
- 315.Kozyrskyj AL, Pawlowski AN. Maternal distress and childhood wheeze: Mechanisms and context. Am J Respir Crit Care Med. 2013;187:1160–2. doi: 10.1164/rccm.201304-0649ED. [DOI] [PubMed] [Google Scholar]
- 316.Liu AH, Zeiger R, Sorkness C, Mahr T, Ostrom N, Burgess S, et al. Development and cross-sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol. 2007;119:817–25. doi: 10.1016/j.jaci.2006.12.662. [DOI] [PubMed] [Google Scholar]
- 317.Liu AH, Zeiger RS, Sorkness CA, Ostrom NK, Chipps BE, Rosa K, et al. The Childhood Asthma Control Test: Retrospective determination and clinical validation of a cut point to identify children with very poorly controlled asthma. J Allergy Clin Immunol. 2010;126:267–73. doi: 10.1016/j.jaci.2010.05.031. 273.e1. [DOI] [PubMed] [Google Scholar]
- 318.Zeiger RS, Mellon M, Chipps B, Murphy KR, Schatz M, Kosinski M, et al. Test for Respiratory and Asthma Control in Kids (TRACK): Clinically meaningful changes in score. J Allergy Clin Immunol. 2011;128:983–8. doi: 10.1016/j.jaci.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 319.Bisgaard H, Allen D, Milanowski J, Kalev I, Willits L, Davies P. Twelve-month safety and efficacy of inhaled fluticasone propionate in children aged 1 to 3 years with recurrent wheezing. Pediatrics. 2004;113:e87–94. doi: 10.1542/peds.113.2.e87. [DOI] [PubMed] [Google Scholar]
- 320.Leflein JG, Szefler SJ, Murphy KR, Fitzpatrick S, Cruz-Rivera M, Miller CJ, et al. Nebulized budesonide inhalation suspension compared with cromolyn sodium nebulizer solution for asthma in young children: Results of a randomized outcomes trial. Pediatrics. 2002;109:866–72. doi: 10.1542/peds.109.5.866. [DOI] [PubMed] [Google Scholar]
- 321.Zhang L, Pruteanu AI, Prietsch SO, Chauhan BF, Ducharme FM. Cochrane in context: Inhaled corticosteroids in children with persistent asthma: Effects on growth and dose-response effects on growth. Evid Based Child Health. 2014;9:1047–51. doi: 10.1002/ebch.1984. [DOI] [PubMed] [Google Scholar]
- 322.Pruteanu AI, Chauhan BF, Zhang L, Prietsch SO, Ducharme FM. Inhaled corticosteroids in children with persistent asthma: Dose-response effects on growth. Evid Based Child Health. 2014;9:931–1046. doi: 10.1002/ebch.1989. [DOI] [PubMed] [Google Scholar]
- 323.Dufour V, Millon L, Faucher JF, Bard E, Robinet E, Piarroux R, et al. Effects of a short-course of amoxicillin/clavulanic acid on systemic and mucosal immunity in healthy adult humans. Int Immunopharmacol. 2005;5:917–28. doi: 10.1016/j.intimp.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 324.Adams NP, Bestall JB, Jones PW. Inhaled beclomethasone versus placebo for chronic asthma. Cochrane Database Syst Rev. 2000;4:CD002738. doi: 10.1002/14651858.CD002738. [DOI] [PubMed] [Google Scholar]
- 325.Bacharier LB, Phillips BR, Zeiger RS, Szefler SJ, Martinez FD, Lemanske RF, Jr, et al. Episodic use of an inhaled corticosteroid or leukotriene receptor antagonist in preschool children with moderate-to-severe intermittent wheezing. J Allergy Clin Immunol. 2008;122:1127–35.e8. doi: 10.1016/j.jaci.2008.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Reddel HK, Foster JM. Inconclusive evidence about the efficacy of diverse strategies for intermittent versus daily inhaled corticosteroids for persistent asthma in adults and children. Evid Based Med. 2014;19:e2. doi: 10.1136/eb-2013-101249. [DOI] [PubMed] [Google Scholar]
- 327.Hakim F, Vilozni D, Adler A, Livnat G, Tal A, Bentur L. The effect of montelukast on bronchial hyperreactivity in preschool children. Chest. 2007;131:180–6. doi: 10.1378/chest.06-1402. [DOI] [PubMed] [Google Scholar]
- 328.Kemp JP, Meltzer EO. Beta 2 adrenergic agonists – Oral or aerosol for the treatment of asthma? J Asthma. 1990;27:149–57. doi: 10.3109/02770909009073315. [DOI] [PubMed] [Google Scholar]
- 329.Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF, Jr, Sorkness CA, et al. Long-acting beta2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: A randomized controlled trial. JAMA. 2001;285:2583–93. doi: 10.1001/jama.285.20.2583. [DOI] [PubMed] [Google Scholar]
- 330.Kulus M, Hébert J, Garcia E, Fowler Taylor A, Fernandez Vidaurre C, Blogg M. Omalizumab in children with inadequately controlled severe allergic (IgE-mediated) asthma. Curr Med Res Opin. 2010;26:1285–93. doi: 10.1185/03007991003771338. [DOI] [PubMed] [Google Scholar]
- 331.Lanier B, Bridges T, Kulus M, Taylor AF, Berhane I, Vidaurre CF. Omalizumab for the treatment of exacerbations in children with inadequately controlled allergic (IgE-mediated) asthma. J Allergy Clin Immunol. 2009;124:1210–6. doi: 10.1016/j.jaci.2009.09.021. [DOI] [PubMed] [Google Scholar]
- 332.Deschildre A, Marguet C, Langlois C, Pin I, Rittié JL, Derelle J, et al. Real-life long-term omalizumab therapy in children with severe allergic asthma. Eur Respir J. 2015;46:856–9. doi: 10.1183/09031936.00008115. [DOI] [PubMed] [Google Scholar]
- 333.Licari A, Marseglia A, Caimmi S, Castagnoli R, Foiadelli T, Barberi S, et al. Omalizumab in children. Paediatr Drugs. 2014;16:491–502. doi: 10.1007/s40272-014-0107-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Deerojanawong J, Manuyakorn W, Prapphal N, Harnruthakorn C, Sritippayawan S, Samransamruajkit R. Randomized controlled trial of salbutamol aerosol therapy via metered dose inhaler-spacer vs.jet nebulizer in young children with wheezing. Pediatr Pulmonol. 2005;39:466–72. doi: 10.1002/ppul.20204. [DOI] [PubMed] [Google Scholar]
- 335.Agertoft L, Pedersen S. Importance of training for correct Turbuhaler use in preschool children. Acta Paediatr. 1998;87:842–7. doi: 10.1080/080352598750013608. [DOI] [PubMed] [Google Scholar]
- 336.Drblik S, Lapierre G, Thivierge R, Turgeon J, Gaudreault P, Cummins-McManus B, et al. Comparative efficacy of terbutaline sulphate delivered by Turbuhaler dry powder inhaler or pressurised metered dose inhaler with Nebuhaler spacer in children during an acute asthmatic episode. Arch Dis Child. 2003;88:319–23. doi: 10.1136/adc.88.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Castro-Rodriguez JA, Rodrigo GJ. beta-agonists through metered-dose inhaler with valved holding chamber versus nebulizer for acute exacerbation of wheezing or asthma in children under 5 years of age: A systematic review with meta-analysis. J Pediatr. 2004;145:172–7. doi: 10.1016/j.jpeds.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 338.Pearlman DS, Chervinsky P, LaForce C, Seltzer JM, Southern DL, Kemp JP, et al. A comparison of salmeterol with albuterol in the treatment of mild-to-moderate asthma. N Engl J Med. 1992;327:1420–5. doi: 10.1056/NEJM199211123272004. [DOI] [PubMed] [Google Scholar]
- 339.Ducharme FM, Lemire C, Noya FJ, Davis GM, Alos N, Leblond H, et al. Preemptive use of high-dose fluticasone for virus-induced wheezing in young children. N Engl J Med. 2009;360:339–53. doi: 10.1056/NEJMoa0808907. [DOI] [PubMed] [Google Scholar]
- 340.Bisgaard H, Hermansen MN, Loland L, Halkjaer LB, Buchvald F. Intermittent inhaled corticosteroids in infants with episodic wheezing. N Engl J Med. 2006;354:1998–2005. doi: 10.1056/NEJMoa054692. [DOI] [PubMed] [Google Scholar]
- 341.Papi A, Nicolini G, Baraldi E, Boner AL, Cutrera R, Rossi GA, et al. Regular vs prn nebulized treatment in wheeze preschool children. Allergy. 2009;64:1463–71. doi: 10.1111/j.1398-9995.2009.02134.x. [DOI] [PubMed] [Google Scholar]
- 342.Guilbert TW, Morgan WJ, Zeiger RS, Mauger DT, Boehmer SJ, Szefler SJ, et al. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med. 2006;354:1985–97. doi: 10.1056/NEJMoa051378. [DOI] [PubMed] [Google Scholar]
- 343.Nielsen KG, Bisgaard H. The effect of inhaled budesonide on symptoms, lung function, and cold air and methacholine responsiveness in 2- to 5-year-old asthmatic children. Am J Respir Crit Care Med. 2000;162(4 Pt 1):1500–6. doi: 10.1164/ajrccm.162.4.2002019. [DOI] [PubMed] [Google Scholar]
- 344.Szefler SJ, Baker JW, Uryniak T, Goldman M, Silkoff PE. Comparative study of budesonide inhalation suspension and montelukast in young children with mild persistent asthma. J Allergy Clin Immunol. 2007;120:1043–50. doi: 10.1016/j.jaci.2007.08.063. [DOI] [PubMed] [Google Scholar]
- 345.Knorr B, Franchi LM, Bisgaard H, Vermeulen JH, LeSouef P, Santanello N, et al. Montelukast, a leukotriene receptor antagonist, for the treatment of persistent asthma in children aged 2 to 5 years. Pediatrics. 2001;108:E48. doi: 10.1542/peds.108.3.e48. [DOI] [PubMed] [Google Scholar]
- 346.Bisgaard H. Leukotriene modifiers in pediatric asthma management. Pediatrics. 2001;107:381–90. doi: 10.1542/peds.107.2.381. [DOI] [PubMed] [Google Scholar]
- 347.Ducharme FM, Hicks GC. Anti-leukotriene agents compared to inhaled corticosteroids in the management of recurrent and/or chronic asthma in adults and children. Cochrane Database Syst Rev. 2002;3:CD002314. doi: 10.1002/14651858.CD002314. [DOI] [PubMed] [Google Scholar]
- 348.Chauhan BF, Ducharme FM. Addition to inhaled corticosteroids of long-acting beta2-agonists versus anti-leukotrienes for chronic asthma. Cochrane Database Syst Rev. 2014;1:CD003137. doi: 10.1002/14651858.CD003137.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Chong JK, Chauhan BF. Addition of antileukotriene agents to inhaled corticosteroids in children with persistent asthma. Paediatr Child Health. 2014;19:473–4. doi: 10.1093/pch/19.9.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Shrewsbury S, Pyke S, Britton M. Meta-analysis of increased dose of inhaled steroid or addition of salmeterol in symptomatic asthma (MIASMA) BMJ. 2000;320:1368–73. doi: 10.1136/bmj.320.7246.1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Matz J, Emmett A, Rickard K, Kalberg C. Addition of salmeterol to low-dose fluticasone versus higher-dose fluticasone: An analysis of asthma exacerbations. J Allergy Clin Immunol. 2001;107:783–9. doi: 10.1067/mai.2001.114709. [DOI] [PubMed] [Google Scholar]
- 352.Vaessen-Verberne AA, van den Berg NJ, van Nierop JC, Brackel HJ, Gerrits GP, Hop WC, et al. Combination therapy salmeterol/fluticasone versus doubling dose of fluticasone in children with asthma. Am J Respir Crit Care Med. 2010;182:1221–7. doi: 10.1164/rccm.201002-0193OC. [DOI] [PubMed] [Google Scholar]
- 353.Verberne AA, Frost C, Duiverman EJ, Grol MH, Kerrebijn KF. Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. The Dutch Asthma Study Group. Am J Respir Crit Care Med. 1998;158:213–9. doi: 10.1164/ajrccm.158.1.9706048. [DOI] [PubMed] [Google Scholar]
- 354.Ducharme FM, Ni Chroinin M, Greenstone I, Lasserson TJ. Addition of long-acting beta2-agonists to inhaled corticosteroids versus same dose inhaled corticosteroids for chronic asthma in adults and children. Cochrane Database Syst Rev. 2010 May 12;5:CD005535. doi: 10.1002/14651858.CD005535.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Ducharme FM, Ni Chroinin M, Greenstone I, Lasserson TJ. Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma. Cochrane Database Syst Rev. 2010 Apr 14;4:CD005533. doi: 10.1002/14651858.CD005533.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Ni Chroinin M, Greenstone I, Lasserson TJ, Ducharme FM. Addition of inhaled long-acting beta2-agonists to inhaled steroids as first line therapy for persistent asthma in steroid-naive adults and children. Cochrane Database Syst Rev. 2009 Oct 7;4:CD005307. doi: 10.1002/14651858.CD005307.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Ni Chroinin M, Lasserson TJ, Greenstone I, Ducharme FM. Addition of long-acting beta-agonists to inhaled corticosteroids for chronic asthma in children. Cochrane Database Syst Rev 2009; Cochrane Database Syst Rev. 2003;4:CD003570:CD007949. doi: 10.1002/14651858.CD007949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Ducharme FM. Anti-leukotrienes as add-on therapy to inhaled glucocorticoids in patients with asthma: Systematic review of current evidence. BMJ. 2002;324:1545. doi: 10.1136/bmj.324.7353.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Phipatanakul W, Cronin B, Wood RA, Eggleston PA, Shih MC, Song L, et al. Effect of environmental intervention on mouse allergen levels in homes of inner-city Boston children with asthma. Ann Allergy Asthma Immunol. 2004;92:420–5. doi: 10.1016/S1081-1206(10)61777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Simons FE, Villa JR, Lee BW, Teper AM, Lyttle B, Aristizabal G, et al. Montelukast added to budesonide in children with persistent asthma: A randomized, double-blind, crossover study. J Pediatr. 2001;138:694–8. doi: 10.1067/mpd.2001.112899. [DOI] [PubMed] [Google Scholar]
- 361.Goksör E, Amark M, Alm B, Gustafsson PM, Wennergren G. Asthma symptoms in early childhood – What happens then? Acta Paediatr. 2006;95:471–8. doi: 10.1080/08035250500499440. [DOI] [PubMed] [Google Scholar]
- 362.Swern AS, Tozzi CA, Knorr B, Bisgaard H. Predicting an asthma exacerbation in children 2 to 5 years of age. Ann Allergy Asthma Immunol. 2008;101:626–30. doi: 10.1016/S1081-1206(10)60226-8. [DOI] [PubMed] [Google Scholar]
- 363.Ducharme FM, Chalut D, Plotnick L, Savdie C, Kudirka D, Zhang X, et al. The pediatric respiratory assessment measure: A valid clinical score for assessing acute asthma severity from toddlers to teenagers. J Pediatr. 2008;152:476–80. doi: 10.1016/j.jpeds.2007.08.034. 480.e1. [DOI] [PubMed] [Google Scholar]
- 364.Birken CS, Parkin PC, Macarthur C. Asthma severity scores for preschoolers displayed weaknesses in reliability, validity, and responsiveness. J Clin Epidemiol. 2004;57:1177–81. doi: 10.1016/j.jclinepi.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 365.Parkin PC, Macarthur C, Saunders NR, Diamond SA, Winders PM. Development of a clinical asthma score for use in hospitalized children between 1 and 5 years of age. J Clin Epidemiol. 1996;49:821–5. doi: 10.1016/0895-4356(96)00027-3. [DOI] [PubMed] [Google Scholar]
- 366.Bentur L, Kerem E, Canny G, Reisman J, Schuh S, Stein R, et al. Response of acute asthma to a beta 2 agonist in children less than two years of age. Ann Allergy. 1990;65:122–6. [PubMed] [Google Scholar]
- 367.Wennergren G, Engström I, Bjure J. Transcutaneous oxygen and carbon dioxide levels and a clinical symptom scale for monitoring the acute asthmatic state in infants and young children. Acta Paediatr Scand. 1986;75:465–9. doi: 10.1111/j.1651-2227.1986.tb10231.x. [DOI] [PubMed] [Google Scholar]
- 368.Tal A, Bavilski C, Yohai D, Bearman JE, Gorodischer R, Moses SW. Dexamethasone and salbutamol in the treatment of acute wheezing in infants. Pediatrics. 1983;71:13–8. [PubMed] [Google Scholar]
- 369.Bentur L, Canny GJ, Shields MD, Kerem E, Schuh S, Reisman JJ, et al. Controlled trial of nebulized albuterol in children younger than 2 years of age with acute asthma. Pediatrics. 1992;89:133–7. [PubMed] [Google Scholar]
- 370.Tal A, Levy N, Bearman JE. Methylprednisolone therapy for acute asthma in infants and toddlers: A controlled clinical trial. Pediatrics. 1990;86:350–6. [PubMed] [Google Scholar]
- 371.Chalut DS, Ducharme FM, Davis GM. The Preschool Respiratory Assessment Measure (PRAM): A responsive index of acute asthma severity. J Pediatr. 2000;137:762–8. doi: 10.1067/mpd.2000.110121. [DOI] [PubMed] [Google Scholar]
- 372.Alangari AA, Riaz M, Mahjoub MO, Malhis N, Al-Tamimi S, Al-Modaihsh A. The effect of sand storms on acute asthma in Riyadh, Saudi Arabia. Ann Thorac Med. 2015 Mar;10:29–33. doi: 10.4103/1817-1737.146857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Al-Muhsen S, Horanieh N, Dulgom S, Aseri ZA, Vazquez-Tello A, Halwani R, et al. Poor asthma education and medication compliance are associated with increased emergency department visits by asthmatic children. Ann Thorac Med. 2015;10:123–31. doi: 10.4103/1817-1737.150735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Alnaji F, Zemek R, Barrowman N, Plint A. PRAM score as predictor of pediatric asthma hospitalization. Acad Emerg Med. 2014;21:872–8. doi: 10.1111/acem.12422. [DOI] [PubMed] [Google Scholar]
- 375.Jarvis SW, Kovacs C, Badriyah T, Briggs J, Mohammed MA, Meredith P, et al. Development and validation of a decision tree early warning score based on routine laboratory test results for the discrimination of hospital mortality in emergency medical admissions. Resuscitation. 2013;84:1494–9. doi: 10.1016/j.resuscitation.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 376.Johnson KB, Blaisdell CJ, Walker A, Eggleston P. Effectiveness of a clinical pathway for inpatient asthma management. Pediatrics. 2000;106:1006–12. [PubMed] [Google Scholar]
- 377.Norton SP, Pusic MV, Taha F, Heathcote S, Carleton BC. Effect of a clinical pathway on the hospitalisation rates of children with asthma: A prospective study. Arch Dis Child. 2007;92:60–6. doi: 10.1136/adc.2006.097287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Lougheed MD, Olajos-Clow JG. Asthma care pathways in the emergency department. Curr Opin Allergy Clin Immunol. 2010;10:181–7. doi: 10.1097/ACI.0b013e328339731d. [DOI] [PubMed] [Google Scholar]
- 379.Browne GJ, Giles H, McCaskill ME, Fasher BJ, Lam LT. The benefits of using clinical pathways for managing acute paediatric illness in an emergency department. J Qual Clin Pract. 2001;21:50–5. doi: 10.1046/j.1440-1762.2001.00405.x. [DOI] [PubMed] [Google Scholar]
- 380.Graham VA, Milton AF, Knowles GK, Davies RJ. Routine antibiotics in hospital management of acute asthma. Lancet. 1982;1:418–20. doi: 10.1016/s0140-6736(82)91619-1. [DOI] [PubMed] [Google Scholar]
- 381.Griffiths B, Ducharme FM. Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children. Cochrane Database Syst Rev. 2013;8:CD000060. doi: 10.1002/14651858.CD000060.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Everard ML, Bara A, Kurian M, Elliott TM, Ducharme F, Mayowe V. Anticholinergic drugs for wheeze in children under the age of two years. Cochrane Database Syst Rev. 2005 Jul 20;3:CD001279. doi: 10.1002/14651858.CD001279.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Griffiths B, Ducharme FM. Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children. Paediatr Respir Rev. 2013;14:234–5. doi: 10.1016/j.prrv.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 384.Powell CV, Kolamunnage-Dona R, Lowe J, Boland A, Petrou S, Doull I, et al. MAGNEsium Trial In Children (MAGNETIC): A randomised, placebo-controlled trial and economic evaluation of nebulised magnesium sulphate in acute severe asthma in children. (1-216).Health Technol Assess. 2013;17:v–vi. doi: 10.3310/hta17450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Powell C, Kolamunnage-Dona R, Lowe J, Boland A, Petrou S, Doull I, et al. Magnesium sulphate in acute severe asthma in children (MAGNETIC): A randomised, placebo-controlled trial. Lancet Respir Med. 2013;1:301–8. doi: 10.1016/S2213-2600(13)70037-7. [DOI] [PubMed] [Google Scholar]
- 386.Hamid Q, Tulic MK. New insights into the pathophysiology of the small airways in asthma. Ann Thorac Med. 2007;2:28–33. doi: 10.4103/1817-1737.30361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Al-Muhsen S, Vazquez-Tello A, Alzaabi A, Al-Hajjaj MS, Al-Jahdali HH, Halwani R. IL-4 receptor alpha single-nucleotide polymorphisms rs1805010 and rs1801275 are associated with increased risk of asthma in a Saudi Arabian population. Ann Thorac Med. 2014;9:81–6. doi: 10.4103/1817-1737.128849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Cohn L, Homer RJ, Marinov A, Rankin J, Bottomly K. Induction of airway mucus production By T helper 2 (Th2) cells: A critical role for interleukin 4 in cell recruitment but not mucus production. J Exp Med. 1997;186:1737–47. doi: 10.1084/jem.186.10.1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Akbari O, Stock P, Meyer E, Kronenberg M, Sidobre S, Nakayama T, et al. Essential role of NKT cells producing IL-4 and IL-13 in the development of allergen-induced airway hyperreactivity. Nat Med. 2003;9:582–8. doi: 10.1038/nm851. [DOI] [PubMed] [Google Scholar]
- 390.Alzoghaibi MA, Bahammam AS. Circulating LTB4 and Eotaxin-1 in stable asthmatics on inhaled corticosteroids and long-acting β 2-agonists. Ann Thorac Med. 2006;1:67–70. [Google Scholar]
- 391.Humbert M, Corrigan CJ, Kimmitt P, Till SJ, Kay AB, Durham SR. Relationship between IL-4 and IL-5 mRNA expression and disease severity in atopic asthma. Am J Respir Crit Care Med. 1997;156(3 Pt 1):704–8. doi: 10.1164/ajrccm.156.3.9610033. [DOI] [PubMed] [Google Scholar]
- 392.Ahmad A, Shameem M, Husain Q. Relation of oxidant-antioxidant imbalance with disease progression in patients with asthma. Ann Thorac Med. 2012;7:226–32. doi: 10.4103/1817-1737.102182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Holgate ST, Peters-Golden M, Panettieri RA, Henderson WR., Jr Roles of cysteinyl leukotrienes in airway inflammation, smooth muscle function, and remodeling. J Allergy Clin Immunol. 2003;111(1 Suppl):S18–34. doi: 10.1067/mai.2003.25. [DOI] [PubMed] [Google Scholar]
- 394.Tobin MJ. Asthma, airway biology, and nasal disorders in AJRCCM 2003. Am J Respir Crit Care Med. 2004;169:265–76. doi: 10.1164/rccm.2312011. [DOI] [PubMed] [Google Scholar]
- 395.Linzer J. Review of asthma: Pathophysiology and current treatment options. Clin Pediatr Emerg Med. 2007;8:87–95. [Google Scholar]
- 396.Sposato B, Scalese M, Pammolli A, Scala R, Naldi M. Seasons can influence the results of the methacholine challenge test. Ann Thorac Med. 2012;7:61–8. doi: 10.4103/1817-1737.94521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Kendrick AH, Higgs CM, Whitfield MJ, Laszlo G. Accuracy of perception of severity of asthma: Patients treated in general practice. BMJ. 1993;307:422–4. doi: 10.1136/bmj.307.6901.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.An SS, Bai TR, Bates JH, Black JL, Brown RH, Brusasco V, et al. Airway smooth muscle dynamics: A common pathway of airway obstruction in asthma. Eur Respir J. 2007;29:834–60. doi: 10.1183/09031936.00112606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Kinet JP. The high-affinity IgE receptor (Fc epsilon RI): From physiology to pathology. Annu Rev Immunol. 1999;17:931–72. doi: 10.1146/annurev.immunol.17.1.931. [DOI] [PubMed] [Google Scholar]
- 400.King GG, Paré PD, Seow CY. The mechanics of exaggerated airway narrowing in asthma: The role of smooth muscle. Respir Physiol. 1999;118:1–13. doi: 10.1016/s0034-5687(99)00076-6. [DOI] [PubMed] [Google Scholar]
- 401.James AL, Paré PD, Hogg JC. The mechanics of airway narrowing in asthma. Am Rev Respir Dis. 1989;139:242–6. doi: 10.1164/ajrccm/139.1.242. [DOI] [PubMed] [Google Scholar]
- 402.Niimi A, Matsumoto H, Takemura M, Ueda T, Chin K, Mishima M. Relationship of airway wall thickness to airway sensitivity and airway reactivity in asthma. Am J Respir Crit Care Med. 2003;168:983–8. doi: 10.1164/rccm.200211-1268OC. [DOI] [PubMed] [Google Scholar]
- 403.Creticos PS. Treatment options for initial maintenance therapy of persistent asthma: A review of inhaled corticosteroids and leukotriene receptor antagonists. Drugs. 2003;63(Suppl 2):1–20. doi: 10.2165/00003495-200363002-00002. [DOI] [PubMed] [Google Scholar]
- 404.Lemanske RF, Jr, Sorkness CA, Mauger EA, Lazarus SC, Boushey HA, Fahy JV, et al. Inhaled corticosteroid reduction and elimination in patients with persistent asthma receiving salmeterol: A randomized controlled trial. JAMA. 2001;285:2594–603. doi: 10.1001/jama.285.20.2594. [DOI] [PubMed] [Google Scholar]
- 405.Alangari AA. Corticosteroids in the treatment of acute asthma. Ann Thorac Med. 2014;9:187–92. doi: 10.4103/1817-1737.140120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Selroos O. Effect of disease duration on dose-response of inhaled budesonide in asthma. Respir Med. 2008;102:1065–72. doi: 10.1016/j.rmed.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 407.Masoli M, Weatherall M, Holt S, Beasley R. Moderate dose inhaled corticosteroids plus salmeterol versus higher doses of inhaled corticosteroids in symptomatic asthma. Thorax. 2005;60:730–4. doi: 10.1136/thx.2004.039180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Fouda MA, Al-Kassimi FA. Budesonide and fluticasone and adrenal suppression. Ann Thorac Med. 2012;7:253. doi: 10.4103/1817-1737.102188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Leach C, Colice GL, Luskin A. Particle size of inhaled corticosteroids: Does it matter? J Allergy Clin Immunol. 2009;124(6 Suppl):S88–93. doi: 10.1016/j.jaci.2009.09.050. [DOI] [PubMed] [Google Scholar]
- 410.Menzies D, Nair A, Hopkinson P, McFarlane L, Lipworth BJ. Differential anti-inflammatory effects of large and small particle size inhaled corticosteroids in asthma. Allergy. 2007;62:661–7. doi: 10.1111/j.1398-9995.2007.01376.x. [DOI] [PubMed] [Google Scholar]
- 411.Kramer S, Rottier BL, Scholten RJ, Boluyt N. Ciclesonide versus other inhaled corticosteroids for chronic asthma in children. Cochrane Libr 2013. Cochrane Database Syst Rev. 2013 Feb 28;2:CD010352. doi: 10.1002/14651858.CD010352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Pruteanu AI, Chauhan BF, Zhang L, Prietsch SO, Ducharme FM. Inhaled corticosteroids in children with persistent asthma: Dose-response effects on growth. Cochrane Database Syst Rev. 2014;7:CD009878. doi: 10.1002/14651858.CD009878.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Hoover RM, Erramouspe J, Bell EA, Cleveland KW. Effect of inhaled corticosteroids on long-term growth in pediatric patients with asthma and allergic rhinitis. Ann Pharmacother. 2013;47:1175–81. doi: 10.1177/1060028013503125. [DOI] [PubMed] [Google Scholar]
- 414.Kelly HW, Van Natta ML, Covar RA, Tonascia J, Green RP, Strunk RC CAMP Research Group. Effect of long-term corticosteroid use on bone mineral density in children: A prospective longitudinal assessment in the childhood Asthma Management Program (CAMP) study. Pediatrics. 2008;122:e53–61. doi: 10.1542/peds.2007-3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Sidoroff VH, Ylinen MK, Kröger LM, Kröger HP, Korppi MO. Inhaled corticosteroids and bone mineral density at school age: A follow-up study after early childhood wheezing. Pediatr Pulmonol. 2015;50:1–7. doi: 10.1002/ppul.22968. [DOI] [PubMed] [Google Scholar]
- 416.Stelmach I, Olszowiec-Chlebna M, Jerzynska J, Grzelewski T, Stelmach W, Majak P. Inhaled corticosteroids may have a beneficial effect on bone metabolism in newly diagnosed asthmatic children. Pulm Pharmacol Ther. 2011;24:414–20. doi: 10.1016/j.pupt.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 417.Altintas DU, Karakoc GB, Can S, Yilmaz M, Kendirli SG. The effects of long term use of inhaled corticosteroids on linear growth, adrenal function and bone mineral density in children. Allergol Immunopathol (Madr) 2005;33:204–9. doi: 10.1157/13077744. [DOI] [PubMed] [Google Scholar]
- 418.Lötvall J, Bateman ED, Bleecker ER, Busse WW, Woodcock A, Follows R, et al. 24-h duration of the novel LABA vilanterol trifenatate in asthma patients treated with inhaled corticosteroids. Eur Respir J. 2012;40:570–9. doi: 10.1183/09031936.00121411. [DOI] [PubMed] [Google Scholar]
- 419.Casarosa P, Kollak I, Kiechle T, Ostermann A, Schnapp A, Kiesling R, et al. Functional and biochemical rationales for the 24-hour-long duration of action of olodaterol. J Pharmacol Exp Ther. 2011;337:600–9. doi: 10.1124/jpet.111.179259. [DOI] [PubMed] [Google Scholar]
- 420.Pearlman DS, Greos L, LaForce C, Orevillo CJ, Owen R, Higgins M. Bronchodilator efficacy of indacaterol, a novel once-daily beta2-agonist, in patients with persistent asthma. Ann Allergy Asthma Immunol. 2008;101:90–5. doi: 10.1016/S1081-1206(10)60840-X. [DOI] [PubMed] [Google Scholar]
- 421.Sugihara N, Kanada S, Haida M, Ichinose M, Adachi M, Hosoe M, et al. 24-h bronchodilator efficacy of single doses of indacaterol in Japanese patients with asthma: A comparison with placebo and salmeterol. Respir Med. 2010;104:1629–37. doi: 10.1016/j.rmed.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 422.Cazzola M, Segreti A, Matera MG. Novel bronchodilators in asthma. Curr Opin Pulm Med. 2010;16:6–12. doi: 10.1097/MCP.0b013e32833303d2. [DOI] [PubMed] [Google Scholar]
- 423.Cazzola M, Matera MG. Novel long-acting bronchodilators for COPD and asthma. Br J Pharmacol. 2008;155:291–9. doi: 10.1038/bjp.2008.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.LaForce C, Korenblat P, Osborne P, Dong F, Higgins M. 24-hour bronchodilator efficacy of single doses of indacaterol in patients with persistent asthma: Comparison with placebo and formoterol. Curr Med Res Opin. 2009;25:2353–9. doi: 10.1185/03007990903143143. [DOI] [PubMed] [Google Scholar]
- 425.Cates CJ, Jaeschke R, Schmidt S, Ferrer M. Regular treatment with formoterol and inhaled steroids for chronic asthma: Serious adverse events. Cochrane Database Syst Rev. 2013;6:CD006924. doi: 10.1002/14651858.CD006924.pub3. [DOI] [PubMed] [Google Scholar]
- 426.Huchon G, Magnussen H, Chuchalin A, Dymek L, Gonod FB, Bousquet J. Lung function and asthma control with beclomethasone and formoterol in a single inhaler. Respir Med. 2009;103:41–9. doi: 10.1016/j.rmed.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 427.Nolte H, Pavord I, Backer V, Spector S, Shekar T, Gates D, et al. Dose-dependent anti-inflammatory effect of inhaled mometasone furoate/formoterol in subjects with asthma. Respir Med. 2013;107:656–64. doi: 10.1016/j.rmed.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 428.Grekas N, Athanassiou K, Papataxiarchou K, Rizea Savu S, Silvestro L. Pharmacokinetic study for the establishment of bioequivalence of two inhalation treatments containing budesonide plus formoterol. J Pharm Pharmacol. 2014;66:1677–85. doi: 10.1111/jphp.12303. [DOI] [PubMed] [Google Scholar]
- 429.Bodzenta-Lukaszyk A, Pulka G, Dymek A, Bumbacea D, McIver T, Schwab B, et al. Efficacy and safety of fluticasone and formoterol in a single pressurized metered dose inhaler. Respir Med. 2011;105:674–82. doi: 10.1016/j.rmed.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 430.Bateman ED, O’Byrne PM, Busse WW, Lötvall J, Bleecker ER, Andersen L, et al. Once-daily fluticasone furoate (FF)/vilanterol reduces risk of severe exacerbations in asthma versus FF alone. Thorax. 2014;69:312–9. doi: 10.1136/thoraxjnl-2013-203600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Busse WW, O’Byrne PM, Bleecker ER, Lötvall J, Woodcock A, Andersen L, et al. Safety and tolerability of the novel inhaled corticosteroid fluticasone furoate in combination with the ß2 agonist vilanterol administered once daily for 52 weeks in patients >=12 years old with asthma: A randomised trial. Thorax. 2013;68:513–20. doi: 10.1136/thoraxjnl-2012-202606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Bjermer L, Diamant Z. The use of leukotriene receptor antagonists (LTRAs) as complementary therapy in asthma. Monaldi Arch Chest Dis. 2002;57:76–83. [PubMed] [Google Scholar]
- 433.Idrees MM, Al Moamary MS. Blocking leukotrienes optimize asthma control: The BLOC survey. Ann Thorac Med. 2007;2:99–102. doi: 10.4103/1817-1737.33696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Bisgaard H Study Group on Montelukast and Respiratory Syncytial Virus. A randomized trial of montelukast in respiratory syncytial virus postbronchiolitis. Am J Respir Crit Care Med. 2003;167:379–83. doi: 10.1164/rccm.200207-747OC. [DOI] [PubMed] [Google Scholar]
- 435.Straub DA, Minocchieri S, Moeller A, Hamacher J, Wildhaber JH. The effect of montelukast on exhaled nitric oxide and lung function in asthmatic children 2 to 5 years old. Chest. 2005;127:509–14. doi: 10.1378/chest.127.2.509. [DOI] [PubMed] [Google Scholar]
- 436.Straub DA, Moeller A, Minocchieri S, Hamacher J, Sennhauser FH, Hall GL, et al. The effect of montelukast on lung function and exhaled nitric oxide in infants with early childhood asthma. Eur Respir J. 2005;25:289–94. doi: 10.1183/09031936.05.00031904. [DOI] [PubMed] [Google Scholar]
- 437.Bisgaard H, Zielen S, Garcia-Garcia ML, Johnston SL, Gilles L, Menten J, et al. Montelukast reduces asthma exacerbations in 2- to 5-year-old children with intermittent asthma. Am J Respir Crit Care Med. 2005;171:315–22. doi: 10.1164/rccm.200407-894OC. [DOI] [PubMed] [Google Scholar]
- 438.van Noord JA, Bantje TA, Eland ME, Korducki L, Cornelissen PJ. A randomised controlled comparison of tiotropium nd ipratropium in the treatment of chronic obstructive pulmonary disease. The Dutch Tiotropium Study Group. Thorax. 2000;55:289–94. doi: 10.1136/thorax.55.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Maesen FP, Smeets JJ, Sledsens TJ, Wald FD, Cornelissen PJ. Tiotropium bromide, a new long-acting antimuscarinic bronchodilator: A pharmacodynamic study in patients with chronic obstructive pulmonary disease (COPD). Dutch Study Group. Eur Respir J. 1995;8:1506–13. [PubMed] [Google Scholar]
- 440.Fardon T, Haggart K, Lee DK, Lipworth BJ. A proof of concept study to evaluate stepping down the dose of fluticasone in combination with salmeterol and tiotropium in severe persistent asthma. Respir Med. 2007;101:1218–28. doi: 10.1016/j.rmed.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 441.Rodrigo GJ, Castro-Rodríguez JA. What is the role of tiotropium in asthma? a systematic review with meta-analysis. Chest. 2015;147:388–96. doi: 10.1378/chest.14-1698. [DOI] [PubMed] [Google Scholar]
- 442.Elias JA, Lee CG, Zheng T, Ma B, Homer RJ, Zhu Z. New insights into the pathogenesis of asthma. J Clin Invest. 2003;111:291–7. doi: 10.1172/JCI17748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Buhl R. Anti-IgE antibodies for the treatment of asthma. Curr Opin Pulm Med. 2005;11:27–34. doi: 10.1097/01.mcp.0000147860.83639.30. [DOI] [PubMed] [Google Scholar]
- 444.D’Amato G, Bucchioni E, Oldani V, Canonica W. Treating Moderate-to-Severe Allergic Asthma with a Recombinant Humanized Anti-IgE Monoclonal Antibody (Omalizumab) Treat Respir Med. 2006;5:393–8. doi: 10.2165/00151829-200605060-00004. [DOI] [PubMed] [Google Scholar]
- 445.Busse W, Corren J, Lanier BQ, McAlary M, Fowler-Taylor A, Cioppa GD, et al. Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. J Allergy Clin Immunol. 2001;108:184–90. doi: 10.1067/mai.2001.117880. [DOI] [PubMed] [Google Scholar]
- 446.Busse WW, Morgan WJ, Gergen PJ, Mitchell HE, Gern JE, Liu AH, et al. Randomized trial of omalizumab (anti-IgE) for asthma in inner-city children. N Engl J Med. 2011;364:1005–15. doi: 10.1056/NEJMoa1009705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Sridhar AV, McKean M. Nedocromil sodium for chronic asthma in children. Cochrane Database Syst Rev. 2006 Jul 19;3:CD004108. doi: 10.1002/14651858.CD004108.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.Rodrigo GJ, Rodrigo C. Continuous vs intermittent beta-agonists in the treatment of acute adult asthma: A systematic review with meta-analysis. Chest. 2002;122:160–5. doi: 10.1378/chest.122.1.160. [DOI] [PubMed] [Google Scholar]
- 449.Travers AH, Rowe BH, Barker S, Jones A, Camargo CA., Jr The effectiveness of IV beta-agonists in treating patients with acute asthma in the emergency department: A meta-analysis. Chest. 2002;122:1200–7. doi: 10.1378/chest.122.4.1200. [DOI] [PubMed] [Google Scholar]
- 450.Rodrigo GJ, Rodrigo C. First-line therapy for adult patients with acute asthma receiving a multiple-dose protocol of ipratropium bromide plus albuterol in the emergency department. Am J Respir Crit Care Med. 2000;161:1862–8. doi: 10.1164/ajrccm.161.6.9908115. [DOI] [PubMed] [Google Scholar]
- 451.Rodrigo GJ, Rodrigo C. The role of anticholinergics in acute asthma treatment: An evidence-based evaluation. Chest. 2002;121:1977–87. doi: 10.1378/chest.121.6.1977. [DOI] [PubMed] [Google Scholar]
- 452.Vézina K, Chauhan BF, Ducharme FM. Inhaled anticholinergics and short-acting beta (2)-agonists versus short-acting beta2-agonists alone for children with acute asthma in hospital. Cochrane Database Syst Rev. 2014;7:CD010283. doi: 10.1002/14651858.CD010283.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.Parameswaran K, Belda J, Rowe BH. Addition of intravenous aminophylline to beta2-agonists in adults with acute asthma. Cochrane Database Syst Rev. 2000;4:CD002742. doi: 10.1002/14651858.CD002742. [DOI] [PubMed] [Google Scholar]
- 454.Silverman RA, Osborn H, Runge J, Gallagher EJ, Chiang W, Feldman J, et al. IV magnesium sulfate in the treatment of acute severe asthma: A multicenter randomized controlled trial. Chest. 2002;122:489–97. doi: 10.1378/chest.122.2.489. [DOI] [PubMed] [Google Scholar]
- 455.Nair A, Menzies D, Barnes M, Burns P, McFarlane L, Lipworth BJ. Respirable dose delivery of fluticasone propionate from a small valved holding chamber, a compact breath actuated integrated vortex device and a metered dose inhaler. Br J Clin Pharmacol. 2008;66:20–6. doi: 10.1111/j.1365-2125.2008.03153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Giraud V, Allaert FA, Roche N. Inhaler technique and asthma: Feasibility and acceptability of training by pharmacists. Respir Med. 2011;105:1815–22. doi: 10.1016/j.rmed.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 457.Giraud V, Allaert FA. Improved asthma control with breath-actuated pressurized metered dose inhaler (pMDI): The SYSTER survey. Eur Rev Med Pharmacol Sci. 2009;13:323–30. [PubMed] [Google Scholar]
- 458.Donnell D. Inhaled corticosteroid delivery systems: Clinical role of a breath-actuated device. Eur Rev Med Pharmacol Sci. 2001;5:7–16. [PubMed] [Google Scholar]
- 459.Standardization of spirometry, 1994 update. American thoracic society. Am J Respir Crit Care Med. 1995;152:1107–36. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]


