Summary
Background
Patients with liver cirrhosis have an increased risk of developing hepatocellular carcinoma (HCC). Implantation metastasis following diagnostic biopsy is a well-known complication. Therefore, primary resection of a hypervascularised tumour suspicious for HCC is often performed with curative intent.
Case Report
An exophytically growing mass was diagnosed between liver segments III and IVb by means of ultrasound in a 53-year old male patient with decompensated liver cirrhosis. Computed tomography confirmed a 3.5 cm large hypervascularised tumour with given resectability. Intraoperatively, the tumour appeared like a HCC. Thus, an atypical resection was performed. Histopathology revealed ectopic spleen tissue without any signs of malignancy. As enquiries revealed, the patient had undergone splenectomy after a blunt abdominal trauma 9 years prior to admission.
Conclusion
In the present patient, hepatic splenosis in a cirrhotic liver was misinterpreted as HCC. In patients with a history of traumatic rupture of the spleen or splenectomy, splenosis has to be considered as a potential differential diagnosis of a hypervascularised tumour. Specific diagnostics should be performed to rule out splenosis.
Keywords: Liver tumour, Hypervascularised tumour, Liver resection, Splenosis
Introduction
Hepatocellular carcinoma (HCC) is one of the most common carcinomas worldwide and is associated with a significant cancer-related mortality [1]. In patients with liver cirrhosis the risk of developing HCC is markedly increased. Therefore, in these patients HCC screening is recommended by means of ultrasound (US) examination or measurement of alpha-fetoprotein [2,3].
Tumours suspicious for HCC are further diagnosed by computed tomography (CT) or magnetic resonance imaging (MRI) to gain information about their localization and to evaluate given resectability. In order to assure the diagnosis, percutaneous liver biopsy might be considered. Thus, a HCC can be histologically differentiated from metastasis or other tumour entities [4]. Transcutaneous biopsies are often avoided due to the risk of bleeding and metastatic spread, which occurs in 0.0095-5% [5]. Therefore, primary liver resection is often performed in patients with an increased risk for bleeding complications and assumed HCC.
Case Report
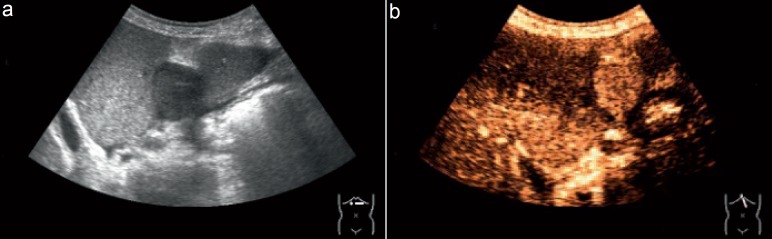
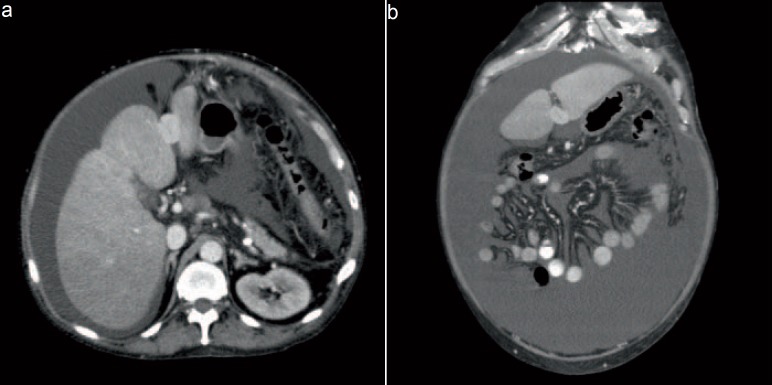
A 53-year-old male patient was initially admitted to the Department of Gastroenterology, University of Rostock, Germany, due to decompensated Child-Pugh class B liver cirrhosis based on a history of severe alcohol abuse. The patient suffered from therapy-refractory ascites, multiple gastric ulcers, duodenitis, sigma diverticulosis, and a condition after hepatorenal syndrome. Regarding the past medical history, the patient reported of a splenectomy after an industrial accident with traumatic rupture of the spleen and left-sided hematothorax 9 years ago. Routine US revealed a space-occupying mass of approximately 3.5 cm size in the central part of the liver (fig. 1). As a second, independent imaging modality CT revealed a contrast enhancement typical for HCC within the tumour (fig. 2). The plasmatic level of alfa-fetoprotein was within normal range.
Fig. 1.
a Native and b contrast-enhanced US scan showing a hypervascularized hepatic tumour.
Fig. 2.
a Axial and b coronal contrast-enhanced CT scan showing a hypervascularized mass between liver segments III and IVb.
After presentation of the case and synopsis of the actual findings in the interdisciplinary tumour board, primary resection of the tumour was recommended. The patient was transferred to our department and underwent explorative laparotomy. Intraoperatively, moderate adhesions between organs and peritoneum were found. The liver showed a fine nodular sclerosis with the exophytically growing tumour between the liver segments III and IVb close to the rotund and falciform ligaments. No further hepatic lesions were seen macroscopically or by US. Thus, an atypical liver resection and a cholecystectomy were performed. Postoperatively, the patient was transferred to the intensive care unit before being shifted to a regular hospital ward. The postoperative course was uneventful.
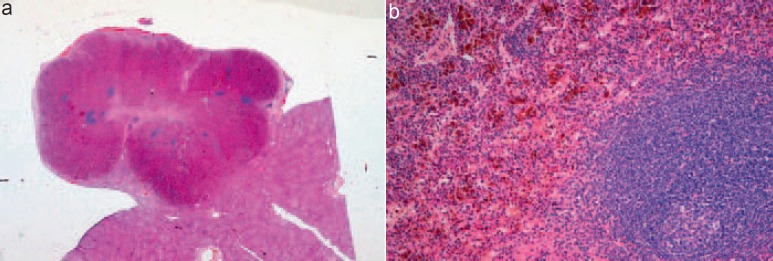
However, histopathology of the resected tumour revealed ectopic spleen tissue in the fringe cupule of the complete micronodular reconstructed cirrhotic liver tissue without any evidence of malignancy (fig. 3).
Fig. 3.
a Low-power view of an exophytic mass adherent to the liver (H&E; original magnification ×5); b high-power view of the mass demonstrating splenic tissue with hemosiderosis (H&E; original magnification ×100).
Discussion
Splenosis is a condition of ectopic spleen tissue caused by autotransplantation after traumatic rupture of the spleen or splenectomy and occurs both inside and outside of the peritoneal cavity (i.e. thorax, abdomen, pelvis, or subcutaneously). It was first reported in 1939 [6] and can be found in 16-67% after trauma of the spleen [7]. Splenic implants should be distinguished from accessory spleens due to their different localization and vascular supply.
Splenosis is usually asymptomatic and an incidental finding during routine US, CT, MRI, or even during surgery. These splenic implants can be partially or even fully functioning and thus be beneficial for the immune system of the patient, reducing the risk of infection and maintaining normal immunological function. Management of asymptomatic splenosis is therefore conservative. In rare cases, complications due to splenosis might occur, such as abdominal pain, gastrointestinal bleeding, or obstruction, depending on the size and localization of the ectopic spleen tissue, and indicate the need for resection of the ectopic spleen tissue.
In the present case, the clinical presentation of the patient with liver cirrhosis and a hypervascularised hepatic mass raised our suspicion of a HCC, not considering the differential diagnosis of a splenosis with the background of splenectomy due to traumatic rupture of the spleen. In addition to our case, other rare case reports show that splenosis is still often misdiagnosed as a malignant tumour [8,9,10], leading to unnecessary major surgery. Splenosis should be considered as a rare but important differential diagnosis of hypervascularised tumours, especially in patients with a past medical history of a traumatic rupture of the spleen or splenectomy [11,12].
In order to rule out splenosis from the differential diagnosis preoperatively, histopathological examination based on tissue gained by needle aspiration prior to operation [13] or scintigraphy with (99m)Tc-labelled head-denatured erythrocytes, a technique with the greatest specificity in the demonstration of splenic tissue, should be performed [14]. However, the risk of tumour dissemination following needle biopsy has to be considered [5]. A further diagnostic option is MRI with gadoxetic acid. Due to this liver-specific contrast agent both sensitivity and specificity for detecting and characterising liver lesions by means of MRI are markedly increased [15]. However, similarly to the surgeon, the radiologist has to be aware of a possible splenosis during assessment of the images. Finally, rapid pathological examination might be required intraoperatively if a splenosis is potentially reasonable due to the patient's past medical history of a traumatic rupture of the spleen or a splenectomy.
Conclusion
Knowledge of the possibility and consideration of a splenosis is crucial to avoid unnecessary surgery in patients with hypervascularised tumours of unknown aetiology and a past medical history of traumatic rupture of the spleen. This equally counts for patients after splenectomy due to other reasons. Even though another diagnosis seems to be more likely, it is quite important to perform further diagnostics, such as scintigraphy or contrast-enhanced MRI, prior to resection or ablation especially in patients with hypervascularised tumours of the liver close to the surface with a high risk for bleeding complications during diagnostic biopsy.
Disclosure Statement
The authors report no declarations of interest.
References
- 1.Bosch FX, Ribes J, Díaz M, Cléries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology. 2004;127:S5–S16. doi: 10.1053/j.gastro.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Sherman M. The radiological diagnosis of hepatocellular carcinoma. Am J Gastroenterol. 2010;105:610–612. doi: 10.1038/ajg.2009.663. [DOI] [PubMed] [Google Scholar]
- 3.Singal A, Volk ML, Waljee A, Salgia R, Higgins P, Rogers MA, Marrero JA. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30:37–47. doi: 10.1111/j.1365-2036.2009.04014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tannapfel A, Dienes HP, Lohse AW. The indications for liver biopsy. Dtsch Aerztebl Int. 2012;109:477–483. doi: 10.3238/arztebl.2012.0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silva MA, Hegab B, Hyde C, Guo B, Buckels JA, Mirza DF. Needle track seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: a systematic review and meta-analysis. Gut. 2008;57:1592–1596. doi: 10.1136/gut.2008.149062. [DOI] [PubMed] [Google Scholar]
- 6.Buchbinder JH, Lipkoff CJ. Splenosis: multiple peritoneal splenic implant following abdominal injury. Surgery. 1939;6:927–934. [Google Scholar]
- 7.Fleming CR, Dickson ER, Harrison EG. Splenosis: autotransplantation of splenic tissue. Am J Med. 1976;61:414–419. doi: 10.1016/0002-9343(76)90380-6. [DOI] [PubMed] [Google Scholar]
- 8.Kang KC, Cho GS, Chung GA, Kang GH, Kim YJ, Lee MS, Kim HK, Park SJ. Intrahepatic splenosis mimicking liver metastasis in a patient with gastric cancer. J Gastric Cancer. 2011;11:64–68. doi: 10.5230/jgc.2011.11.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu Y, Ji B, Wang G, Wang Y. Abdominal multiple splenosis mimicking liver and colon tumors: a case report and review of the literature. Int J Med Sci. 2012;9:174–177. doi: 10.7150/ijms.3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kandil TS, El Sorogy M, Naiem Y, Elkashef WF. Post-splenectomy splenosis presenting as hepatocellular carcinoma in the left lateral section of the liver: a case report. Int J Surg Case Rep. 2014;5:877–878. doi: 10.1016/j.ijscr.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yeh CJ, Chuang WY, Kuo TT. Unusual subcutaneous splenosis occurring in a gunshot wound scar: pathology and immunohistochemical identification. Pathol Int. 2006;56:336–339. doi: 10.1111/j.1440-1827.2006.01968.x. [DOI] [PubMed] [Google Scholar]
- 12.Khan AM, Manzoor K, Gordon D, Berman A. Thoracic splenosis: a diagnosis by history and imaging. Respirology. 2008;13:481–483. doi: 10.1111/j.1440-1843.2008.01272.x. [DOI] [PubMed] [Google Scholar]
- 13.Renne G, Coci A, Biraghi T, Schmid C. Fine needle aspiration of thoracic splenosis. A case report. Acta Cytol. 1999;43:492–494. doi: 10.1159/000331107. [DOI] [PubMed] [Google Scholar]
- 14.Menth M, Herrmann K, Haug A, Raziorrouh B, Zachoval R, Jung CM, Otto C. Intra-hepatic splenosis as an unexpected cause of a focal liver lesion in a patient with hepatitis C and liver cirrhosis: a case report. Cases J. 2009;2:8335. doi: 10.4076/1757-1626-2-8335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jhaveri K, Cleary S, Audet P, Balaa F, Bhayana D, Burak K, Chang S, Dixon E, Haider M, Molinari M, Reinhold C, Sherman M. Consensus statements from a multidisciplinary expert panel on the utilization and application of a liver-specific MRI contrast agent (gadoxetic acid) AJR Am J Roentgenol. 2015;204:498–509. doi: 10.2214/AJR.13.12399. [DOI] [PubMed] [Google Scholar]