Abstract
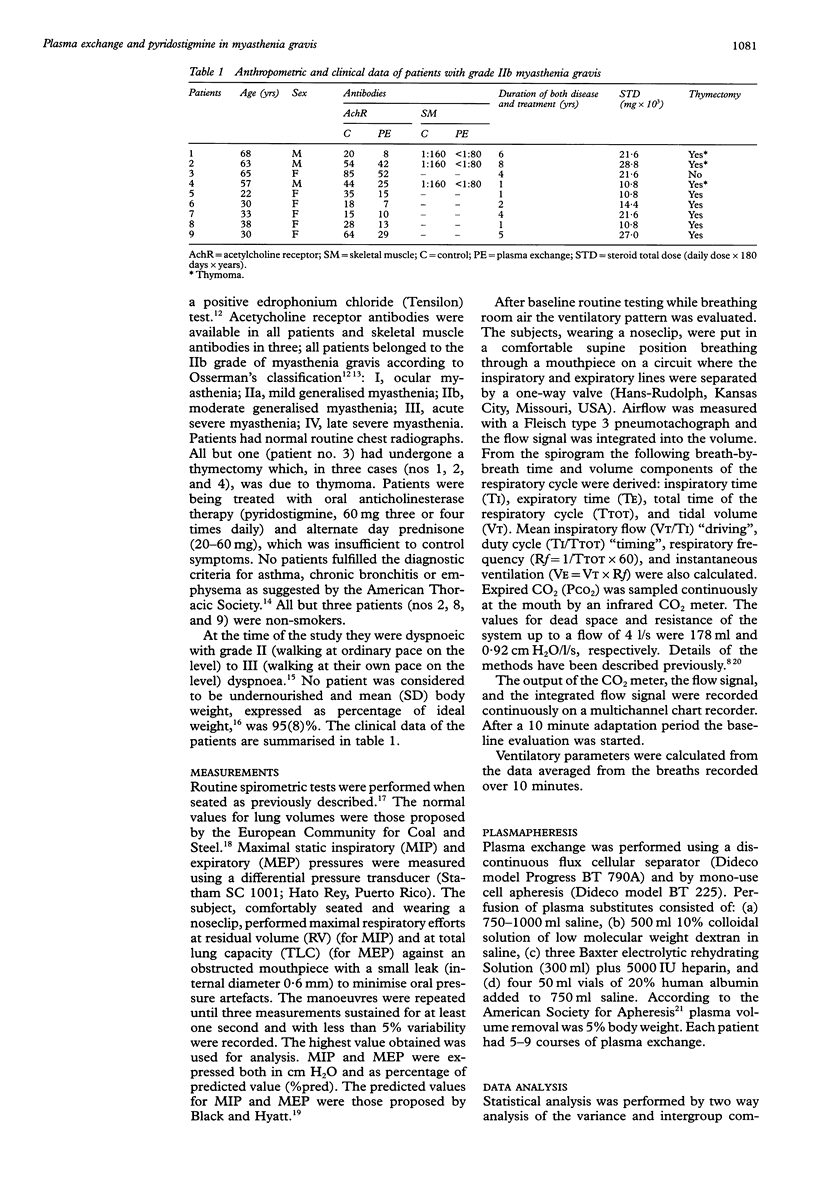
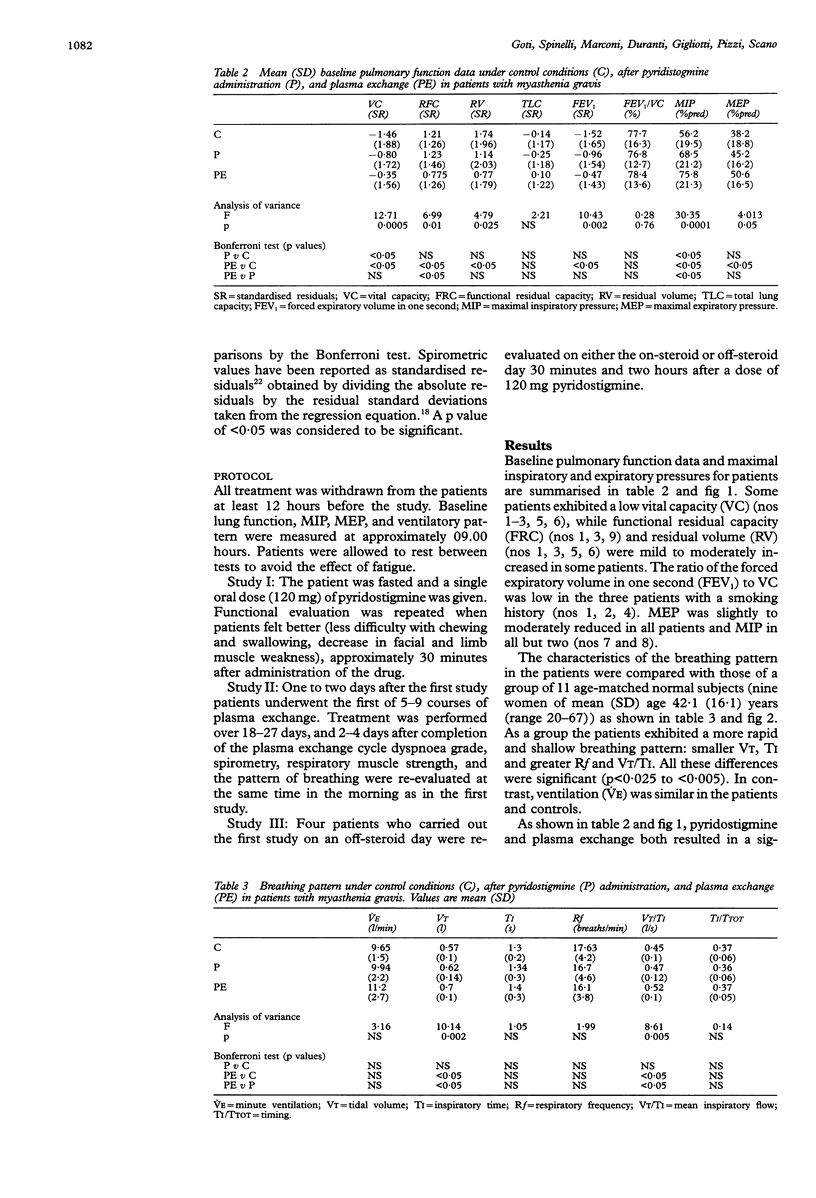
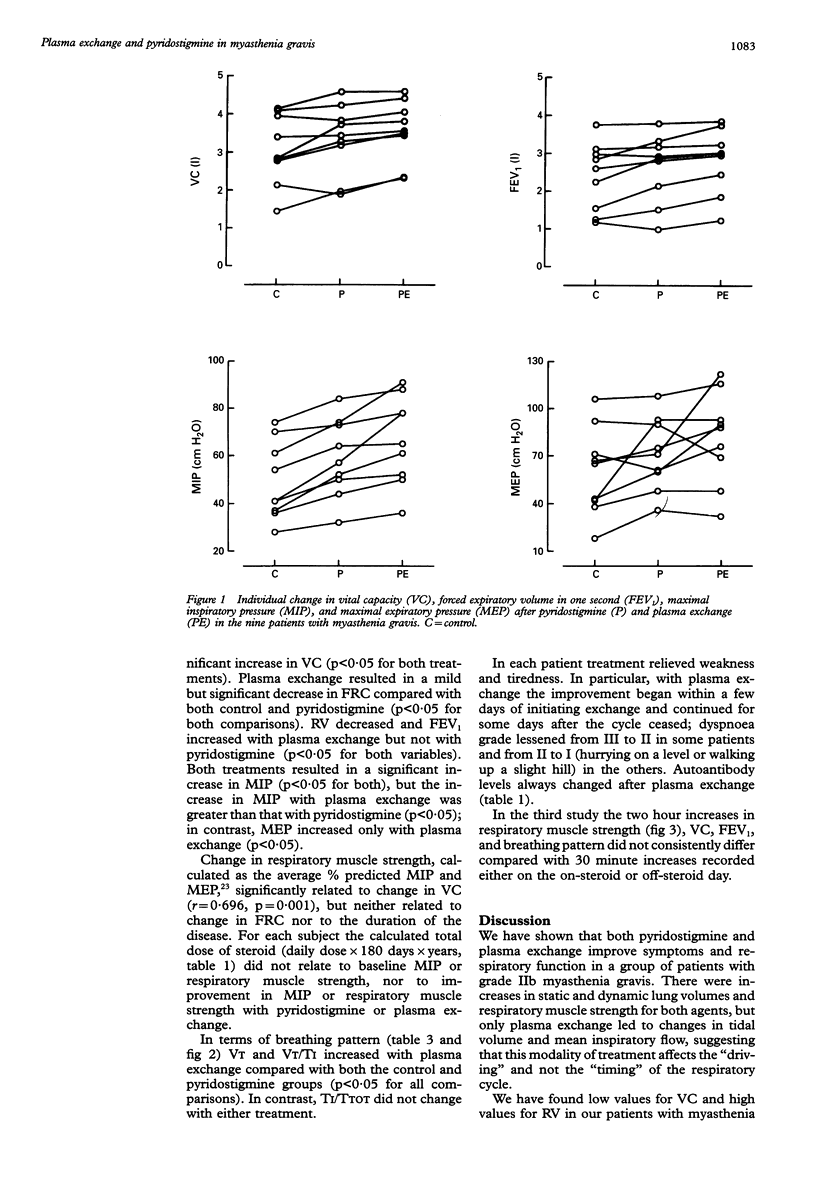
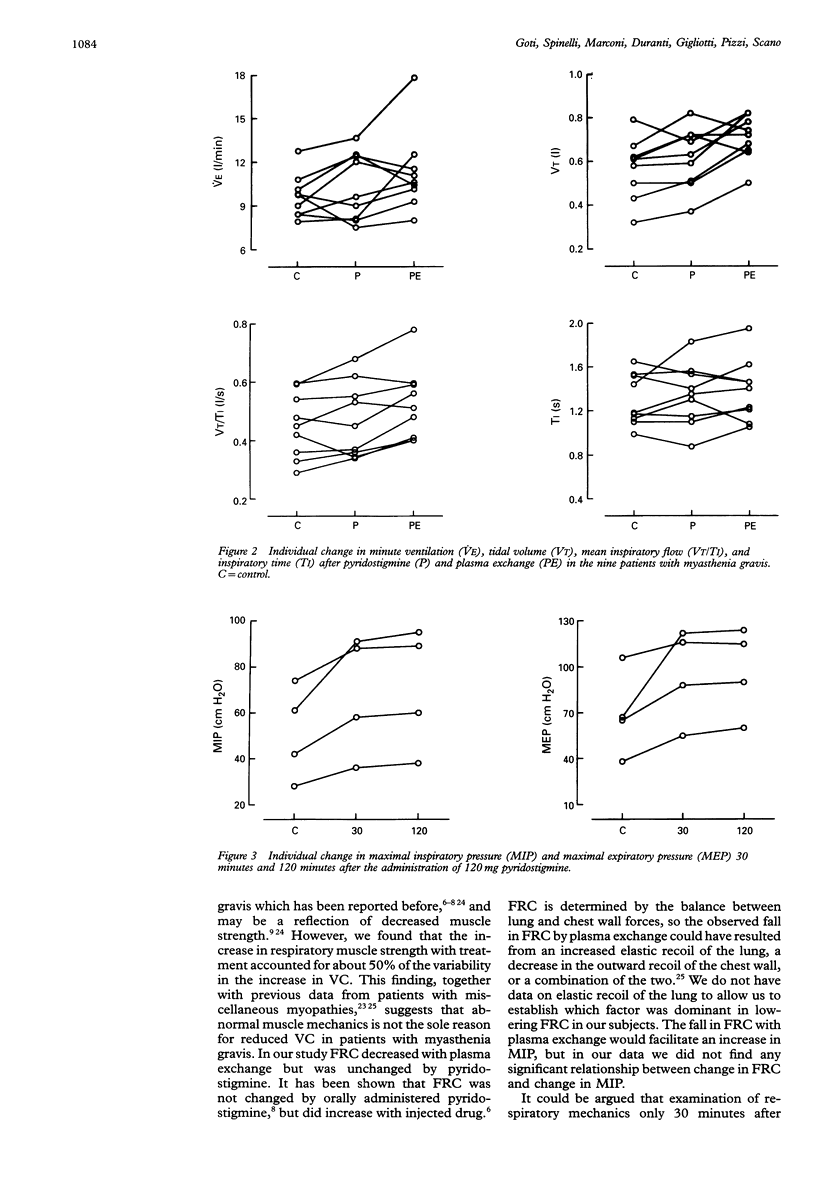
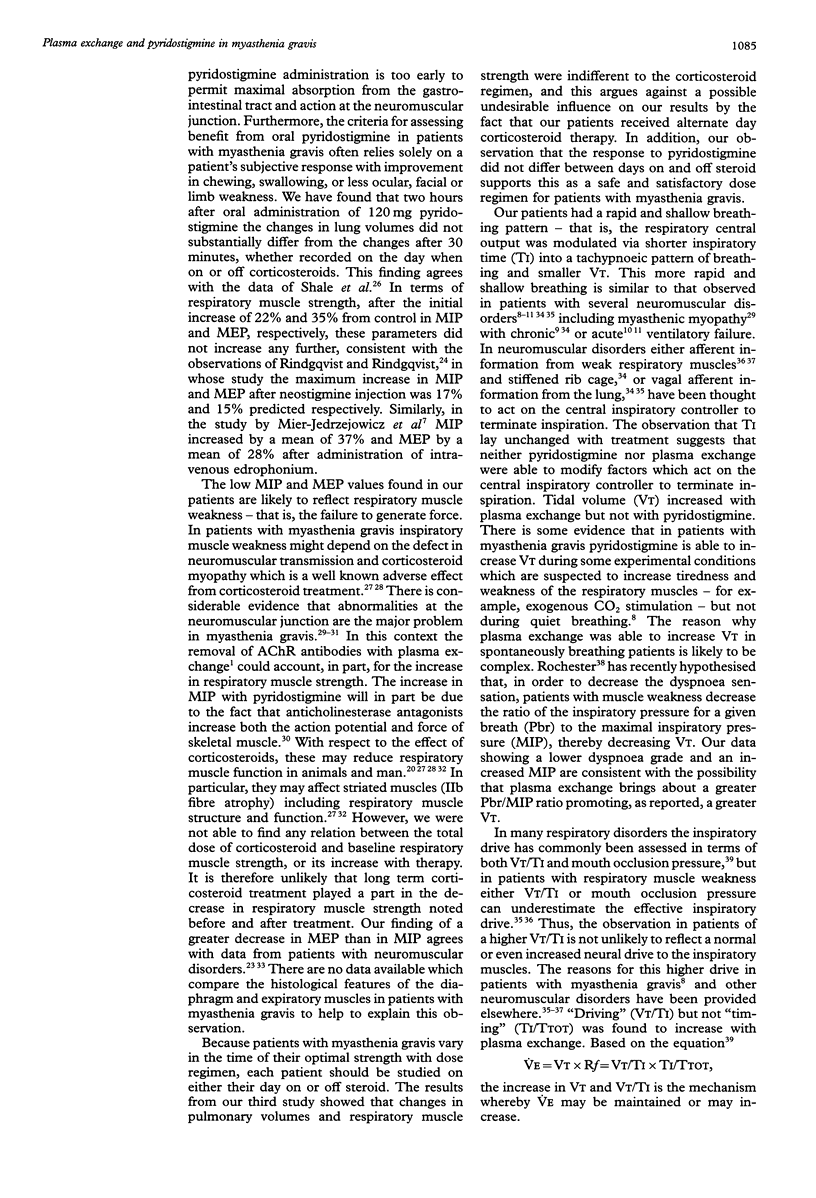
BACKGROUND--Pyridostigmine, an acetylcholinesterase antagonist, is useful in improving respiratory function in patients with myasthenia gravis. More recently, plasma exchange has been employed in myasthenia gravis because it acts presumably by removal of circulating antibodies against acetylcholine receptors. Surprisingly, comparative data on the effects of pyridostigmine and plasma exchange on lung volumes, respiratory muscle strength, and ventilatory control system in patients with myasthenia gravis are lacking. METHODS--Nine consecutive patients with grade IIb myasthenia gravis were studied under control conditions and after a therapeutic dose of pyridostigmine. In a second study the patients were re-evaluated a few days after a cycle of plasma exchange, before taking pyridostigmine. In each subject pulmonary volumes, inspiratory (MIP) and expiratory (MEP) muscle force, and respiratory muscle strength, calculated as average MIP and MEP as percentages of their predicted values, were measured. The ventilatory control system was evaluated in terms of volume (tidal volume, VT) and time (inspiratory time, TI, and total time, TTOT) components of the respiratory cycle. Mean inspiratory flow (VT/TI)--that is, the "driving"--and TI/TTOT--that is, the "timing"--components of ventilation were also measured. RESULTS--In each patient treatment relieved weakness and tiredness, and dyspnoea grade was reduced with plasma exchange. Following treatment, vital capacity (VC) increased on average by 9.7% with pyridostigmine and by 14% with plasma exchange, and MIP increased by 18% and 26%, respectively. In addition, with plasma exchange but not with pyridostigmine forced expiratory volume in one second (FEV1) increased by 16% and MEP increased by 24.5%, while functional residual capacity (FRC) decreased a little (6.8%). The change in respiratory muscle strength was related to change in VC (r2 = 0.48). With plasma exchange, VT increased by 18.6% and VT/TI increased by 13.5%, while neither TI nor TI/TTOT changed. CONCLUSIONS--Plasma exchange can be used in patients with myasthenia gravis when symptoms are not adequately controlled by anticholinesterase agents. Plasma exchange increases respiratory muscle force and tidal volume due to changes in "driving" but not "timing" of the respiratory cycle.
Full text
PDF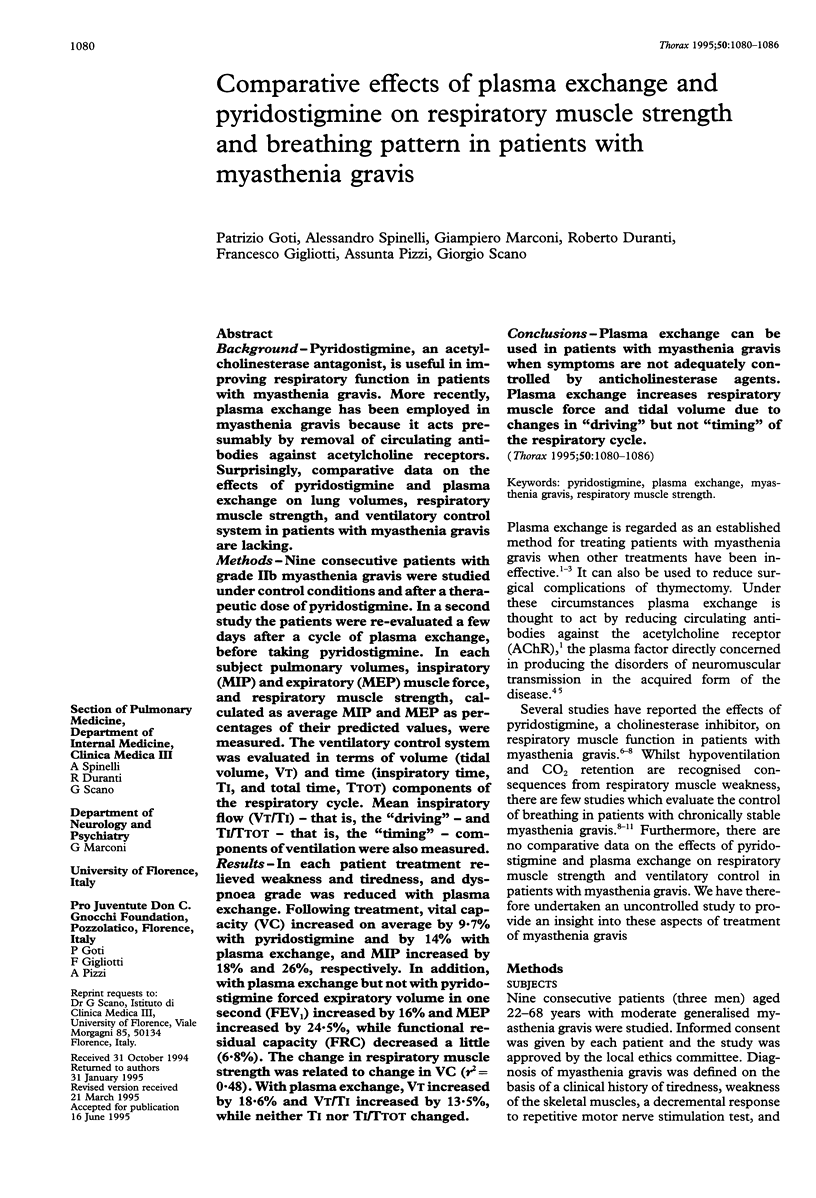
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Almon R. R., Andrew C. G., Appel S. H. Serum globulin in myasthenia gravis: inhibition of alpha-bungarotoxin binding to acetylcholine receptors. Science. 1974 Oct 4;186(4158):55–57. doi: 10.1126/science.186.4158.55. [DOI] [PubMed] [Google Scholar]
- Black L. F., Hyatt R. E. Maximal static respiratory pressures in generalized neuromuscular disease. Am Rev Respir Dis. 1971 May;103(5):641–650. doi: 10.1164/arrd.1971.103.5.641. [DOI] [PubMed] [Google Scholar]
- Borel C. O., Tilford C., Nichols D. G., Hanley D. F., Traystman R. J. Diaphragmatic performance during recovery from acute ventilatory failure in Guillain-Barré syndrome and myasthenia gravis. Chest. 1991 Feb;99(2):444–451. doi: 10.1378/chest.99.2.444. [DOI] [PubMed] [Google Scholar]
- Braun N. M., Arora N. S., Rochester D. F. Respiratory muscle and pulmonary function in polymyositis and other proximal myopathies. Thorax. 1983 Aug;38(8):616–623. doi: 10.1136/thx.38.8.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DESMEDT J. E. The physio-pathology of neuromuscular transmission and the trophic influence of motor innervation. Am J Phys Med. 1959 Dec;38:248–261. [PubMed] [Google Scholar]
- Dau P. C., Lindstrom J. M., Cassel C. K., Denys E. H., Shev E. E., Spitler L. E. Plasmapheresis and immunosuppressive drug therapy in myasthenia gravis. N Engl J Med. 1977 Nov 24;297(21):1134–1140. doi: 10.1056/NEJM197711242972102. [DOI] [PubMed] [Google Scholar]
- Davis J., Goldman M., Loh L., Casson M. Diaphragm function and alveolar hypoventilation. Q J Med. 1976 Jan;45(177):87–100. [PubMed] [Google Scholar]
- De Troyer A., Borenstein S. Acute changes in respiratory mechanics after pyridostigmine injection in patients with myasthenia gravis. Am Rev Respir Dis. 1980 Apr;121(4):629–638. doi: 10.1164/arrd.1980.121.4.629. [DOI] [PubMed] [Google Scholar]
- De Troyer A., Borenstein S., Cordier R. Analysis of lung volume restriction in patients with respiratory muscle weakness. Thorax. 1980 Aug;35(8):603–610. doi: 10.1136/thx.35.8.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Troyer A., Borenstein S., Cordier R. Analysis of lung volume restriction in patients with respiratory muscle weakness. Thorax. 1980 Aug;35(8):603–610. doi: 10.1136/thx.35.8.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decramer M., Stas K. J. Corticosteroid-induced myopathy involving respiratory muscles in patients with chronic obstructive pulmonary disease or asthma. Am Rev Respir Dis. 1992 Sep;146(3):800–802. doi: 10.1164/ajrccm/146.3.800. [DOI] [PubMed] [Google Scholar]
- Dekhuijzen P. N., Decramer M. Steroid-induced myopathy and its significance to respiratory disease: a known disease rediscovered. Eur Respir J. 1992 Sep;5(8):997–1003. [PubMed] [Google Scholar]
- Demedts M., Beckers J., Rochette F., Bulcke J. Pulmonary function in moderate neuromuscular disease without respiratory complaints. Eur J Respir Dis. 1982 Jan;63(1):62–67. [PubMed] [Google Scholar]
- Ellis E. F. Steroid myopathy. J Allergy Clin Immunol. 1985 Sep;76(3):431–432. doi: 10.1016/0091-6749(85)90722-5. [DOI] [PubMed] [Google Scholar]
- Fishman A. P., Ledlie J. F. Dyspnea. Bull Eur Physiopathol Respir. 1979 Sep-Oct;15(5):789–804. [PubMed] [Google Scholar]
- Gibson G. J., Pride N. B., Davis J. N., Loh L. C. Pulmonary mechanics in patients with respiratory muscle weakness. Am Rev Respir Dis. 1977 Mar;115(3):389–395. doi: 10.1164/arrd.1977.115.3.389. [DOI] [PubMed] [Google Scholar]
- Gorini M., Ginanni R., Spinelli A., Duranti R., Andreotti L., Scano G. Inspiratory muscle strength and respiratory drive in patients with rheumatoid arthritis. Am Rev Respir Dis. 1990 Aug;142(2):289–294. doi: 10.1164/ajrccm/142.2.289. [DOI] [PubMed] [Google Scholar]
- Gracey D. R., Howard F. M., Jr, Divertie M. B. Plasmapheresis in the treatment of ventilator-dependent myasthenia gravis patients. Report of four cases. Chest. 1984 Jun;85(6):739–743. doi: 10.1378/chest.85.6.739. [DOI] [PubMed] [Google Scholar]
- Grinman S., Whitelaw W. A. Pattern of breathing in a case of generalized respiratory muscle weakness. Chest. 1983 Dec;84(6):770–772. doi: 10.1378/chest.84.6.770. [DOI] [PubMed] [Google Scholar]
- Miller M. R., Pincock A. C. Predicted values: how should we use them? Thorax. 1988 Apr;43(4):265–267. doi: 10.1136/thx.43.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NEW height-weight tables. Importance of new criteria. JAMA. 1960 Aug 6;173:1576–1576. [PubMed] [Google Scholar]
- Pinching A. J., Peters D. K. Remission of myasthenia gravis following plasma-exchange. Lancet. 1976 Dec 25;2(8000):1373–1376. doi: 10.1016/s0140-6736(76)91917-6. [DOI] [PubMed] [Google Scholar]
- Rochester D. F. Respiratory muscle weakness, pattern of breathing, and CO2 retention in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1991 May;143(5 Pt 1):901–903. doi: 10.1164/ajrccm/143.5_Pt_1.901. [DOI] [PubMed] [Google Scholar]
- Scano G., Garcia-Herreros P., Stendardi D., Degre S., De Coster A., Sergysels R. Cardiopulmonary adaptation to exercise in coal miners. Arch Environ Health. 1980 Nov-Dec;35(6):360–366. doi: 10.1080/00039896.1980.10667520. [DOI] [PubMed] [Google Scholar]
- Shale D. J., Lane D. J., Davis C. J. Air-flow limitation in myasthenia gravis. The effect of acetylcholinesterase inhibitor therapy on air-flow limitation. Am Rev Respir Dis. 1983 Oct;128(4):618–621. doi: 10.1164/arrd.1983.128.4.618. [DOI] [PubMed] [Google Scholar]
- Smith P. E., Calverley P. M., Edwards R. H., Evans G. A., Campbell E. J. Practical problems in the respiratory care of patients with muscular dystrophy. N Engl J Med. 1987 May 7;316(19):1197–1205. doi: 10.1056/NEJM198705073161906. [DOI] [PubMed] [Google Scholar]
- Spinelli A., Marconi G., Gorini M., Pizzi A., Scano G. Control of breathing in patients with myasthenia gravis. Am Rev Respir Dis. 1992 Jun;145(6):1359–1366. doi: 10.1164/ajrccm/145.6.1359. [DOI] [PubMed] [Google Scholar]
- Tarrab-Hazdai R., Aharonov A., Silman I., Fuchs S., Abramsky O. Experimental autoimmune myasthenia induced in monkeys by purified acetylcholine receptor. Nature. 1975 Jul 10;256(5513):128–130. doi: 10.1038/256128a0. [DOI] [PubMed] [Google Scholar]


