Abstract
In epidemiological and twin populations, prior interview studies have identified an externalizing spectrum of disorders. Could this be detected utilizing objective registry data? In 20,603 twin pairs from the Swedish Twin Registry, we obtained information from national medical, criminal and pharmacy records on drug abuse (DA), criminal behavior (CB) and alcohol use disorders (AUD). Multivariate twin modeling was performed with the OpenMx package. A common pathway model with quantitative but not qualitative sex effects fit best with twin resemblance for the latent liability to externalizing syndromes due to both genetic and shared environmental factors. Heritability of the liability was higher in females (76 vs. 62 %) while shared environmental influences were considerably stronger in males (23 vs. 3 %). In both sexes, this latent liability was most strongly indexed by DA and least by CB. All three syndromes had specific genetic influences (especially CB and AUD in males, and CB in females) and specific shared environmental effects (especially DA and CB in males, and AUD in females). For DA, CB and AUD in men, and DA and AUD in women, at least 75 % of the genetic risk arose through the common factor. The best fit model assumed that genetic and environmental influences on these externalizing syndromes in males and females were the same. We identified, in registry data, a highly heritable externalizing spectrum. DA, CB and AUD share substantial genetic and modest to moderate shared environmental influences. The nature of the externalizing spectrum differed meaningfully between the sexes.
Keywords: Drug abuse, Crime, Alcohol use disorders, Externalizing disorders, Twins
Introduction
In population-based samples, externalizing disorders assessed at personal interview—most typically conduct, antisocial personality, and drug and alcohol use disorders—have high rates of comorbidity and form, in multivariate analyses, a discrete psychopathologic dimension (Krueger et al. 1998, 1999, 2001). Twin studies from Virginia (Kendler et al. 2003), Minnesota (Hicks et al. 2004) and Norway (Kendler et al. 2011) have all suggested that these disorders share a common genetic liability that is largely responsible for their tendency to cluster together in human populations.
These studies have all utilized interview-based assessment that depend for their validity on subject cooperation, and accurate recall and reporting of behavior that is typically socially sanctioned and sometimes illegal. Prior surveys have suggested that externalizing behaviors are associated both with lowered rates of cooperation and greater attrition in longitudinal studies (Cox et al. 1977; Eaton et al. 1992; Heath et al. 1998; Karp et al. 1993; Robins 1966).
In this report, we explore, in a Swedish national twin sample, the degree to which three classic externalizing syndromes—drug abuse (DA), alcohol use disorders (AUD) and criminal behavior (CB)—share genetic and environmental risk factors. These disorders are assessed using medical, criminal and pharmacy registries available on all members of the population so that subject cooperation and accurate recall are not required.
Females have substantially lower rates of all externalizing psychopathology compared to males (Compton et al. 2007; Hasin et al. 2007; Kessler et al. 1994). Because of our large sample size, we have an opportunity to explore sex effects in genetic influences of externalizing disorders in more detail than has been possible in prior genetically informative studies (Hicks et al. 2004; Kendler et al. 2003, 2011).
Methods
Sample
We linked nationwide Swedish registers via the unique 10-digit identification number assigned at birth or immigration to all Swedish residents. The identification number was replaced by a serial number to ensure anonymity. From the Swedish Twin Registry, we selected all twin pairs with birth years from 1958 to 1991 with known zygosity (n = 20,603). Over these years, the registry contained both same- and opposite-sex twin pairs.
Zygosity was, of course, known a priori in the opposite sex-pairs. As detailed elsewhere (Lichtenstein et al. 2002), zygosity in the same-sex pairs registry was assigned using standard self-report items obtained from mailed questionnaires which, when validated against biological markers, were 95–99 % accurate. As seen in Table 1, the prevalence of DA, CB and AUD are slightly lower in both males and females in monozygotic (MZ) and same sex dizygotic (DZ) pairs versus opposite sex twin pairs. This is almost surely because the former but not the latter were screened for level of cooperation. That is at least one member of the pair had to return a questionnaire to the twin registry to be able to assign a zygosity, and cooperation was lower in subjects with DA, CB and AUD.
Table 1.
Descriptive statistics on the twin sample
| Pair type | Number of complete pairs |
Mean age (SD) |
Prevalence |
||
|---|---|---|---|---|---|
| Drug abuse (%) |
Criminal behavior (%) |
Alcohol use disorders (%) |
|||
| Monozygotic twins male–male | 2,798 | 38.3 (8.1) | 3.0 | 14.8 | 3.4 |
| Dizygotic twins male–male | 2,585 | 40.7 (8.4) | 2.2 | 15.7 | 4.2 |
| Monozygotic twins female– female |
3,403 | 38.2 (8.2) | 1.6 | 5.3 | 1.8 |
| Dizygotic twins female–female | 2,853 | 40.4 (8.5) | 1.4 | 5.6 | 1.8 |
| Dizygotic twins male–female | 8,964 | 37.4 (10.1) | M: 4.2 F:2.1 | M: 16.8 F: 6.4 | M: 4.9 F:2.2 |
Measures
Information was matched to the individual twins from our data base using their unique serial number. The following sources were used to create our database: the Total Population Register, containing data on birth year and gender; the Multi-Generation Register, providing information on family relations; the Swedish Hospital Discharge Register, containing all hospitalizations for all Swedish inhabitants from 1964 to 2010; the Swedish Prescribed Drug Register, containing all prescriptions in Sweden picked up by patients from 2005 to 2009; the Outpatient Care Register, containing information from all outpatient clinics from 2001 to 2010; the Primary Health Care Register, containing outpatient primary care data on diagnoses and time for diagnoses 2001–2007 for 1 million patients from Stockholm and middle Sweden; the Swedish Crime Register that included national complete data on all convictions in lower court from 1973 to 2011; the Swedish Suspicion Register that included national complete data on all individuals strongly suspected of crime from 1998 to 2011; the Swedish Mortality Register, containing causes of death.
To ascertain DA, we utilized information about medical treatment for DA, criminal behavior directly related to DA and prescription DA as detected from pharmacy records. Specifically, DA was identified in the Swedish medical registries by ICD codes [ICD8: Drug dependence (304); ICD9: Drug psychoses (292) and Drug dependence (304); ICD10: Mental and behavioral disorders due to psychoactive substance use (F10–F19), except those due to alcohol (F10) or tobacco (F17)]; in the Suspicion Register by codes 3070, 5010, 5011, and 5012, which reflect crimes related to DA; and in the Crime Register by references to laws covering narcotics (law 1968:64, paragraph 1, point 6) and drug-related driving offences (law 1951:649, paragraph 4, subsection 2 and paragraph 4A, subsection 2). DA was identified in individuals (excluding those suffering from cancer) in the Prescribed Drug Register who had retrieved (in average) more than four defined daily doses a day for 12 months from either of Hypnotics and Sedatives (Anatomical Therapeutic Chemical (ATC) Classification System N05C and N05BA) or Opioids (ATC: N02A).
Criminal behavior (CB) was defined from the Swedish Crime Register based on the following convictions, law and chapter in parentheses: (aggravated) assault (3:5, 3:6); illegal threat (4:5); threats and violence against an officer (17:1, 17:2); intimidation (4:7); (Gross) violation of a person’s/woman’s integrity (4:4a); kidnapping (4:1); illegal confinement or restraint (4:2); (aggravated) robbery (8:5, 8:6); illegal coercion (4:4); (aggravated) Arson (13:1, 13:2); murder, manslaughter or filicide (3:1, 3:2, 3:3); sexual crimes (excluding prostitution and the buying of sexual services but including child pornography) (6:1–6:10, 6:12, 16:10A); theft of a vehicle (8:1–2, 8:4, 8:7–8); theft (including burglary) (8:1–2, 8:4); vandalism (12:1–4); vandalism causing danger to the public, sabotage, hijacking (13:3–10 (5a–b)); unlawful entering of a person’s home, trespassing (4:6); fraud (9:1–10); embezzlement (10:1–8 (5a–e)); dishonesty/crime towards a creditor (includes forged book-keeping in companies) (11:1–5); and forgery (14:1–10); and thereby excluding convictions for minor crimes like traffic infractions.
To ascertain Alcohol use disorder (AUD), we utilized information about medical treatment for AUD, medical disorder directly attributable to AUD, criminal behavior directly related to AUD, and pharmacologic treatment for AUD as detected from pharmacy records. More specifically, AUD was defined by ICD codes for main and secondary diagnoses from Swedish medical registries for the following diagnoses: ICD9: alcohol-related psychiatric disorders (291), alcohol dependence (303), alcohol abuse (305A), alcohol-related polyneuropathy (357F), alcohol-related cardiomyopathy (425F), alcohol-related gastritis (535D), alcoholic fatty liver, alcohol hepatitis, alcoholic cirrhosis, unspecified liver damage caused by alcohol (571A–D), toxic effects of alcohol (980), alcoholism (V79B); ICD10: alcohol related psychiatric and behavioral disorders (F10, excluding acute alcohol intoxication: F10.0), rehabilitation of a person with alcohol abuse (Z50.2), guidance and medical advice to a person with alcohol abuse (Z71.4), alcohol-related pseudo-Cushing syndrome (E24.4), alcohol-related degeneration of the nervous system and brain (G31.2), alcohol-related polyneuropathy (G62.1), alcohol-related myopathy (G72.1), alcohol-related cardiomyopathy (I42.6), alcohol-related gastritis (K29.2), liver diseases caused by alcohol (K70.0–K70.9), acute pancreatitis caused by alcohol (K85.2), chronic pancreatitis caused by alcohol (K86.0), treatment of pregnant alcoholic woman (O35.4), toxic effects of alcohol (T51.0–T51.9); and based on Anatomical Therapeutic Chemical (ATC) codes in the Prescribed Drug Register: disulfiram (N07BB01), acamprosate (N07BB03), or naltrexone (N07BB04). Additionally, we identified individuals with at least two convictions of drunk driving (law 1951:649) or drunk in charge of maritime vessel (law 1994:1009) in the Crime register. We used the Cause of Death Register to obtain data on alcohol-associated death and used the same codes as above.
Statistical methods
We utilized a classical twin model assuming three sources of liability: additive genetic (A), shared environment (C), and unique environment (E). The model assumes that MZ twins share all their genes while DZ twins share on average half of their genes identical by descent, and that the shared environment, reflecting family and community experiences, is the same within each twin pair. Unique environment includes random developmental effects, environmental experiences not shared by siblings, and random error. We examine the relative fits of two trivariate models applied to the three externalizing syndromes of DA, CB and AUDs: an independent pathway and a common pathway model. In both of these models, each of the three variance components (A, C and E) are decomposed into two parts: one that is common to all three phenotypes (denoted Ac, Cc, and Ec) and one that is specific to each one of them (As, Cs, and Es). In the independent pathway model, the paths from Ac, Cc, and Ec go directly to the observed phenotypes. In the common pathway model, the paths from Ac, Cc, and Ec to the phenotypes are mediated through a latent liability to externalizing disorders. The simpler common pathway model is nested within the independent pathway model.
Although our sample size of twins is considerable, the models include relatively rare phenotypes (i.e., DA and AUD in females) and therefore have limited statistical power. As the objective is to quantify the magnitude of the variation in the population coming from various sources, we chose to present the full model with A, C and E components rather than try to obtain the best fitting submodel (i.e. an AE model only). This is in line with recommendations based on simulations which show that in such situations, parameter estimates from the full model are typically more accurate than those from submodels even if the latter provide a better model fit (Sullivan and Eaves 2002). We present the log likelihood and AIC values to facilitate comparisons between models. Models were fit in the OpenMx software (Boker et al. 2011).
Although we have limited power, because of its substantial theoretical interest, we explore qualitative sex effects in our models—that is are the same genetic and environmental factors influencing risk of CB in both sexes? Qualitative sex effects are captured by the parameters rg and rc that reflect, respectively, the degree to which the genetic or shared environmental risk factors are correlated in the two sexes. In our models, we examine separate estimates for rg in Ac and As and rc in Cc and Cs, termed, respectively: rac, ras, rcc, and rcs. (Note that three values of ras and rcs have to be estimated, one for each phenotype.) We also examine quantitative sex effects—that is whether the genetic and environmental parameter estimates in the model can be constrained to equality or significantly differ between the sexes.
Results
Descriptive findings
The number of the available twin pairs and the prevalence rates for DA, CB and AUD by sex and zygosity group are seen in Table 1. CB was the most common of the syndromes, followed by AUD and then DA. Prevalence rates were higher for all three syndromes in males than in females and in opposite sex versus same-sex pairs.
Twin correlations in the five sex-zygosity groups are seen in Tables 2, 3 and 4. In the same-sex pairs, the twin correlations for DA, CB and AUD were substantially higher in MZ than in DZ twins and modestly higher in same-sex than in opposite sex DZ pairs. In all twin pairs, the within-syndrome cross-twin correlations were moderately higher than the cross-syndrome cross-twin correlations. For example, in MZ females the correlations for DA, CB and AUD ranged from +.64 to +0.71 with a mean of +0.68. The cross-disorder cross twin correlations ranged from +0.38 to +0.59, with a mean of +0.47.
Table 2.
Twin tetrachoric correlations and standard errors in male–male twin pairs: MZ twins above and DZ twins below the diagonal
| DA 1 | CB 1 | AUD 1 | DA 2 | CB 2 | AUD 2 | |
|---|---|---|---|---|---|---|
| DA 1 | 1 (0) | 0.547 (0.049) | 0.745 (0.043) | 0.823 (0.034) | 0.468 (0.053) | 0.497 (0.067) |
| CB 1 | 0.544 (0.053) | 1 (0) | 0.456 (0.052) | 0.535 (0.05) | 0.728 (0.024) | 0.484 (0.05) |
| AUD 1 | 0.606 (0.06) | 0.55 (0.047) | 1 (0) | 0.633 (0.055) | 0.422 (0.053) | 0.664 (0.05) |
| DA 2 | 0.586 (0.074) | 0.299 (0.074) | 0.323 (0.097) | 1 (0) | 0.581 (0.047) | 0.684 (0.049) |
| CB 2 | 0.318 (0.064) | 0.507 (0.034) | 0.318 (0.058) | 0.605 (0.056) | 1 (0) | 0.592 (0.044) |
| AUD 2 | 0.317 (0.082) | 0.314 (0.055) | 0.332 (0.074) | 0.68 (0.056) | 0.534 (0.045) | 1 (0) |
Within-syndrome cross twin correlations are bolded
Table 3.
Twin tetrachoric correlations and standard errors in female–female twin pairs: MZ twins above and DZ twins below the diagonal
| DA 1 | CB 1 | AUD 1 | DA 2 | CB 2 | AUD 2 | |
|---|---|---|---|---|---|---|
| DA 1 | 1 (0) | 0.564 (0.058) | 0.739 (0.049) | 0.708 (0.059) | 0.477 (0.065) | 0.384 (0.098) |
| CB 1 | 0.56 (0.07) | 1 (0) | 0.565 (0.056) | 0.518 (0.068) | 0.639 (0.039) | 0.452 (0.07) |
| AUD 1 | 0.635 (0.078) | 0.476 (0.073) | 1 (0) | 0.588 (0.073) | 0.397 (0.069) | 0.684 (0.058) |
| DA 2 | 0.401 (0.117) | 0.308 (0.092) | 0.36 (0.116) | 1 (0) | 0.577 (0.062) | 0.666 (0.067) |
| CB 2 | 0.064 (0.118) | 0.413 (0.056) | 0.182 (0.098) | 0.548 (0.069) | 1 (0) | 0.382 (0.076) |
| AUD 2 | 0.453 (0.101) | 0.358 (0.08) | 0.527 (0.085) | 0.718 (0.061) | 0.522 (0.065) | 1 (0) |
Within-syndrome cross twin correlations are bolded
Table 4.
Twin tetrachoric correlations and standard errors in male–female DZ twin pairs
| CB 1 | AUD 1 | DA 2 | CB 2 | AUD 2 | |
|---|---|---|---|---|---|
| DA 1 | 0.637 (0.022) | 0.647 (0.025) | 0.380 (0.045) | 0.257 (0.038) | 0.273 (0.05) |
| CB 1 | 0.61 (0.021) | 0.29 (0.038) | 0.282 (0.027) | 0.21 (0.039) | |
| AUD 1 | 0.306 (0.047) | 0.242 (0.037) | 0.323 (0.046) | ||
| DA 2 | 0.526 (0.035) | 0.729 (0.03) | |||
| CB 2 | 0.445 (0.038) |
Within-syndrome cross twin correlations are bolded
Model-fitting
We began our model fitting demonstrating that the fit of a full common pathway model (which permitted different parameter estimates across the sexes) as indicated by the AIC value (−2LogL = 42,781.93, df = 123,584, AIC = −204386.1) was better than a full independent pathway model (−2logL = 42,771.54, df = 123,576, AIC = −204380.5). Then, we found that this common pathway model fitted considerably better than a similar model that constrained to equality all parameter estimates in males and females (−2logL = 42842.83, df = 123,595, AIC = −204347.2). Therefore, in our subsequent analyses, we focused on common-pathway models with quantitative sex effects and turned to examining the presence and/or nature of qualitative sex effects.
Our model had four major genetic or shared environmental correlations between the sexes that could be estimated (rac, ras, rcc, and rcs) where correlations related to the specific syndromes (ras and rcs) could be the same or differ between DA, CB and AUD. However, a model with separate estimates of all correlations was not identified and therefore, of the very large number of possible of models, we chose on a priori grounds to examine four. As seen in Table 5, our first and simplest common pathway model constrained to unity all four relevant sex correlations: rac =ras = rcc = rcs = 1. The second model gave us optimal power to distinguish the genetic and environmental correlations for the externalizing disorders in males and females. We set all the genetic correlations to equality and allowed them to differ from all the shared environmental correlations that were also constrained to equality. The genetic correlations were estimated at +0.78 and the shared environmental correlations at +0.80. However, this model did not fit quite as well as the first model. Our third model constrained to equality the common factor genetic and environmental sex correlations (rac = rcc), and the specific genetic and environmental sex correlations (ras = rcs). The two common and syndrome-specific factor correlations were estimated at +0.79 and +0.80, respectively. But again this model fit modestly worse than model 1. Our fourth model constrained the common factor genetic and environmental correlations to unity (rac = rcc = 1), and constrained the specific genetic and environmental correlations to equality separately for DA, CB and AUD. The model estimated the between sex genetic and environmental correlations for DA and AUD to be high (+.92 and +0.98, respectively) but the estimated correlation for CB was lower (+0.37). However, this model also fitted worse than model 1.
Table 5.
Exploration of qualitative sex effect models
| Model | Description | rg and rc estimates | Number of parametersestimated |
−2logL | df | AIC | |
|---|---|---|---|---|---|---|---|
| 1 | rac = ras = rcc = rcs = 1 | 34 | 42781.93 | 123584 | −204386.7 | ||
| 2 | rac =ras and rcc =rcs | rac = ras = 0.78, rcc = rcs = 0.80 |
36 | 42778.78 | 123582 | −204385.2 | |
| 3 | rac =rcc and ras =rcs | rac = rcc = 0.79, rcs = rcs = 0.80 |
36 | 42779.00 | 123582 | −204385.0 | |
| 4 | rac = rcc = 1; ras = rcs separately for DA, CB, and AUD |
|
37 | 42778.82 | 123581 | −204383.2 |
Parameter estimates
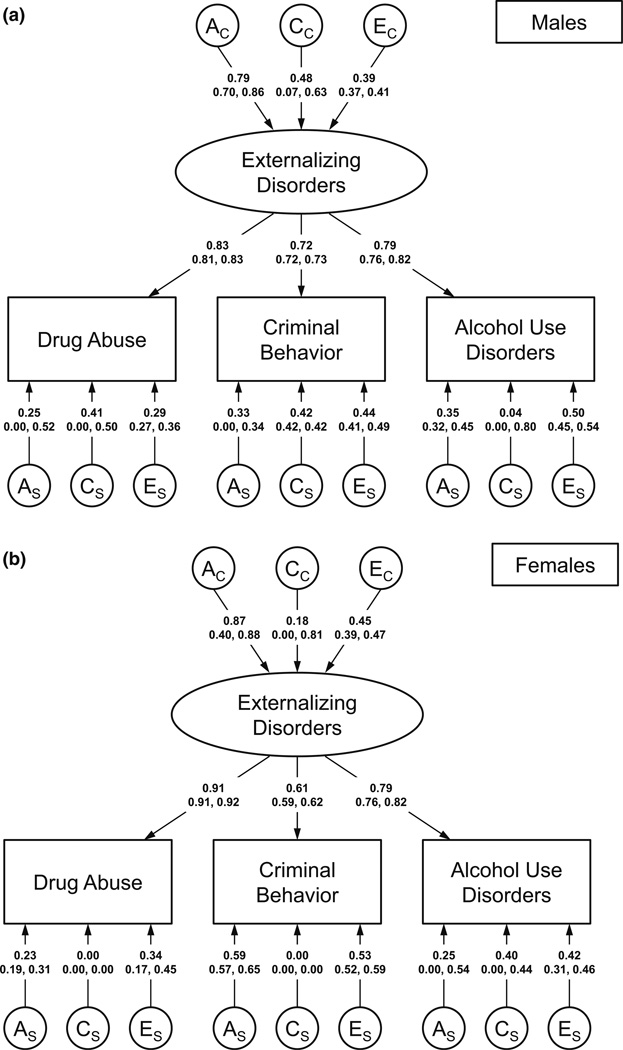
We present path estimates and 95 % CIs for the best-fitting model 1 in Fig. 1a (males) and Fig. 1b (females), variance components with 95 % CIs in Table 6, and the decomposed genetic and environmental influences on the three disorders in both males and females in Table 7. Six results are noteworthy. First, the latent construct of externalizing disorders was highly heritable in males (a2 = 0.62) and especially in females (a2 = 0.76). Second, shared environmental influences on the latent trait of externalizing disorders was considerably stronger in males (c2 = 0.23) than in females (c2 = 0.03). Third, in both sexes, loadings on the externalizing disorder common factor were strongest for DA and weakest for CB. This difference was substantially greater in females than males. Fourth, for all three externalizing syndromes in males, and DA and AUD in females, the large majority (75–92 %) of genetic risk factors were shared with the other externalizing disorders (Table 7). The exception was CB in females where over half of the total heritability derived from syndrome-specific genetic risk factors. Fifth, the pattern was quite different for shared environmental risk factors. For DA and CB in males, roughly half of the shared environmental influences were shared with the latent construct of externalizing disorders and half were specific to these syndromes. However, for AUD in males, and DA and CB in females, nearly all of the shared environmental influences were shared with other externalizing disorders. Finally, for AUD in females, nearly 90 % of the shared environmental effects were unique to that syndrome. Finally, a higher proportion of the unique environmental effects for DA in both males and females were shared in common with the other disorders than was seen for CB and AUD.
Fig. 1.
a Parameter estimates and 95 % confidence intervals for males from best fit common pathway model 1 (Table 5). The model contains additive genetic (A), shared environmental (C) and individual-specific (E) paths to the latent common externalizing disorder factor (subscript “c”) as well as A, C and E paths specific to the three externalizing syndromes (subscript “s”). Paths are standardized partial regression coefficients. b Parameter estimates and 95 % confidence intervals for females from best fit common pathway model 1 (Table 5). The model contains additive genetic (A), shared environmental (C) and individual-specific (E) paths to the latent common Externalizing Disorder factor (subscript “c”) as well as A, C and E paths specific to the three externalizing syndromes (subscript “s”). Paths are standardized partial regression coefficients.
Table 6.
Estimates of the variance components from the best-fitting model
|
|
|
|
|
|
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drug abuse—males | 42.4 % (29.9, 62.4) |
15.9 % (13.9, 26.7) |
10.2 % (9.3, 10.9) |
6.4 % (2.7, 24.7) | 16.6 % (0, 24.8) | 8.4 % (7.5, 13.4) | ||||||
| Criminal behavior—males | 32.2 % (21.7, 47.6) |
12.1 % (10.5, 21.4) |
7.7 % (7.0, 8.4) | 10.6 % (0.0, 12.9) |
17.8 % (16.8, 25.8) |
19.5 % (16.6, 23.1) |
||||||
| Alcohol use disorder— males |
38.4 % (26.8, 56.6) |
14.4 % (12.5, 24.4) |
9.2 % (8.7, 11.8) | 12.5 % (1.2, 16.2) |
0.2 % (0, 0.5) | 25.2 % (17.5, 27.4) |
||||||
| Drug abuse females | 63.1 % (6.0, 74.2) |
2.8 % (1.8, 3.8) | 16.8 % (15.6, 25.8) |
5.5 % (2.0, 7.1) | 0 % (0, 0) | 11.8 % (10.5, 13.2) |
||||||
| Criminal behavior— females |
28.1 % (21.4, 29.5) |
1.2 % (1.0, 1.5) | 7.5 % (6.2, 8.3) | 34.8 % (30.0, 42.7) |
0 % (0, 0) | 28.4 % (27.1, 29.4) |
||||||
| Alcohol use disorder— females |
45.8 % (9.1, 47.6) |
2.0 % (1.4, 2.5) | 12.2 % (11.3, 12.9) |
6.4 % (0, 29.6) | 15.9 % (13.3, 20.6) |
17.6 % (12.0, 24.2) |
A additive genetic effects, C shared environmental effects, E individual specific environmental effects; subscript “c” indicates effects common to all the externalizing disorders; subscript “s” indicates effects specific to individual externalizing disorders
Table 7.
The proportion of variance in liability to drug abuse, criminal behavior and alcohol use disorders in males and females due to additive genetic and shared and unique environmental effects and the proportion of these effects that are in common with the other syndromes versus unique
| Additive Genetic Effects |
Shared Environmental Effects |
Unique Environmental Effects |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Syndrome/sex | Total (95 % CIs) | % Common | % Syndrome Specific |
Total (95 % CIs) | % Common | % Syndrome Specific |
Total (95 % CIs) | % Common | % Syndrome Specific |
| Drug abuse males | 48.9 % (32.3, 72.2) | 86.3 | 13.2 | 32.5 % (8.2, 35.9) | 48.9 | 51.1 | 18.6 % (17.7, 24.3) | 54.8 | 45.2 |
| Criminal behavior males | 42.9 % (32.9, 51.9) | 75.3 | 24.8 | 29.9 % (28.8, 35.6) | 40.5 | 59.5 | 27.3 % (26.4, 29.5) | 28.4 | 71.6 |
| Alcohol use disorder males | 50.9 % (48.8, 50.9) | 75.4 | 24.6 | 14.6 % (12.5, 17.2) | 98.7 | 1.3 | 34.5 % (26.5, 36.6) | 26.8 | 73.2 |
| Drug abuse females | 68.6 % (59.9, 77.7) | 92.1 | 8.0 | 2.8 % (0.2, 16.6) | 100 | 0 | 28.6 % (27.2, 32.3) | 58.8 | 41.2 |
| Criminal behavior females | 62.9 % (50.9, 64.6) | 44.6 | 55.4 | 1.3 % (1.0, 1.5) | 100 | 0 | 35.9 % (31.5,37.3) | 20.8 | 79.2 |
| Alcohol use disorder females | 52.2 % (18.2, 53.6) | 87.8 | 12.2 | 17.9 % (2.3, 20.5) | 11.4 | 88.6 | 29.9 % (26.7, 39.0) | 40.9 | 59.1 |
Discussion
The goal of this report was to clarify the inter-relationship of the genetic and environmental influences on externalizing disorders in a national Swedish population where cases were ascertained via medical, legal and pharmacy registries. We would emphasize six major findings which we review in turn.
First, consistent with prior studies based on personal interviews (Hicks et al. 2004; Kendler et al. 2003, 2011), we found substantial sharing of both genetic and environmental risk factors across the three externalizing syndromes of DA, CB and AUD. Because the syndromes in our sample were ascertained from registries, our results rule out the possibility that prior evidence for an externalizing spectrum is an artifact of measurement due, for example, to rater or reporter bias.
A common pathway model fitted better than an independent pathway model providing strong theoretical support for a latent dimension of liability to externalizing disorders. We are aware of only one prior test of whether externalizing disorders were best explained by a common pathway model. Consistently with our results, Hicks et al. found that the parent–offspring transmission for externalizing disorders were all mediated through a latent common pathway (Hicks et al. 2004). While our estimates of the heritability of the latent liability to ED were substantial (62 % in males and 76 % in females), they were lower than that reported in both sexes (80 %) in the Hicks et al. study that utilized adolescent twins and their parents (Hicks et al. 2004).
Second, contrary to prior studies of this question (Hicks et al. 2004; Kendler et al. 2003, 2011), we found shared environmental influences on the externalizing disorders. Furthermore, these effects were considerably stronger in males than in females. We would hypothesize that this results from a greater impact of peer influences on externalizing behaviors in males than females. This hypothesis is consistent with several lines of evidence. We previously showed that cohabitation effects in childhood and adolescence are stronger on risk for DA in males than in females (Kendler et al. 2013). In comparison to females, males are more motivated to use psychoactive substances to conform to subgroup values, more influenced by peers in their intake of drugs and later delinquency is better predicted by deviant peer groups (Borsari and Carey 2001; Graziano et al. 2012; Piquero et al. 2005). In a particularly relevant Swedish survey of high-school students, Svensson (Svensson 2003) found males to have consistently higher levels of exposure to deviant peers than females and found that this arose because parents of girls monitored their offspring’s social network more closely than did parents of boys. He also found that the probability of substance use was more strongly predicted by exposure to peer deviance in males than in females (Svensson 2003). Both more frequent exposure to peer deviance and a greater impact of that exposure on externalizing behaviors in males versus females would likely translate into stronger peer influences in young Swedish men than Swedish women.
Third, we found substantial quantitative differences in the genetic and environmental parameter estimates of our externalizing spectrum in males and females. Of three prior broadly comparable studies, one (Kendler et al. 2011) did not explore quantitative sex effects while one study (Kendler and Myers 2013) found and the other did not find (Hicks et al. 2004) evidence for such an effect. Our large sample probably gave us substantial power to detect some interesting differences in the structure of the externalizing syndrome in males and females.
Fourth, in both males and females, DA was the strongest index of liability to externalizing disorders and CB was the weakest. This difference was considerably more pronounced in females than in males. These results were partially confirmed by a prior study based on personal interviews in the Virginia Adult Twin Study of Psychiatric and Substance Use Disorders, which found that the genetic risk to externalizing disorders was best indexed in males by (in order) antisocial personality disorder (ASPD), DA, AUD, and conduct disorder (CD) and in females by DA, AUD, nicotine dependence, and ASPD (Kendler and Myers 2013). However, our results are inconsistent with those found by Hicks et al. in their interview-based study where the common factor for externalizing disorders loaded most strongly on, in order, ASPD, AUD and DA (Hicks et al. 2004).
Fifth, the three externalizing syndromes shared genetic risk factors more strongly than shared environmental risk factors. For DA, CD and AUD in men, and DA and AUD in women, at least 75 % of the genetic risk came from the common factor. Only CB in women stood out from this pattern with more than 50 % of the genetic risk unique to that syndrome. By contrast, only for AUD in men, and DA and CB in women did a large majority of the shared environmental effects originate with the common factor. For DA and CB in males, and AUD in females a majority of the shared environmental influences were syndrome specific. These results suggest that the tendency for an individual with a high genetic liability to externalizing disorders to develop DA versus CD or AUD might be substantially influenced by shared environmental exposures. These results have implications for molecular genetic studies and would predict that many of the risk alleles found for individual externalizing disorders would be shared with a range of similar syndromes.
Sixth, prior twin studies of externalizing disorders did not test for qualitative sex effects—that is the degree to which the genetic and shared environmental influences on these syndromes were the same in men and women. We examined this question and were surprised to find that the best fit model constrained these correlations to equality both for the externalizing common factor and for the syndrome specific influences. Consistent with the one relevant power analysis (Prescott and Gottesman 1993), further analyses suggested, that despite our large sample size, we actually had rather limited power to discriminate different models. Other models that fit slightly less well suggested that the correlation between sexes might be slightly less than unity but to be high and similar for genetic and for shared environmental influences. They also suggested that the sharing of genetic influences might be modestly lower for CB than for DA or AUD. But we should regard these findings as only suggestive and worthy of follow-up.
Limitations
These results should be interpreted in the context of three potential methodological limitations. First, while ascertaining cases of DA, CB and AUD from registry data has important advantage, especially independence from subject cooperation and accurate recall and reporting, it also has significant limitations. In Sweden as in most other countries, a majority of most crimes are not officially reported or do not result in a conviction so we are sampling from the more severe end of the spectrum of criminal activities (Swedish National Council for Crime Prevention 2008). For DA and AUD, there are surely false negatives for individuals who abuse substances but avoid medical or police attention. The validity of our detection of these syndromes is supported by evidence for strong co-registration across our registries. The mean OR for case detection of DA across our 5 relevant registries was 52 (Kendler et al. 2012) and for AUD across 4 registries was 33 (Kendler et al. 2014).
Second, we were not able to simultaneously estimate all the possible genetic correlations within our model. This could result in a bias in our parameter estimates, if qualitative effects were present. Such a bias would likely effect parameter estimates more seriously in females as they are less precisely known than in males due to the sex-related prevalence differences in externalizing syndromes. We were able to explore in a limited and tentative fashion the large parameter space and gain some insight into the possible presence of qualitative sex effects.
Third, we were only able to include same-sex twins whose zygosity was known as a result of at least one member responding to a mailed questionnaire but this does not apply to opposite-sex pairs. As expected, individuals with externalizing syndromes had a reduced probability of returning questionnaires so the rate of DA, CB and AUD were lower in both males and females from same-sex than from opposite sex pairs. This is a form of “concordance-dependent” ascertainment where the probability of known zygosity will be lowest in pairs concordant for an externalizing syndrome, intermediate in those discordant and highest in those where neither twin has an externalizing syndrome. Simulations suggest that with the moderate level of differential ascertainment expected in our data given the observed prevalence differences, biases in parameter estimates are likely to be modest and result in slight under-estimations of a2 and c2 and overestimation of e2 (Kendler and Eaves 1989).
Acknowledgments
This project was supported by the Grants RO1DA030005 and R01AA023534 from the National Institute of Health Abuse, the Ellison Medical Foundation, the Swedish Research Council to Kristina Sundquist (K2012-70X-15428-08-3), the Swedish Research Council for Health, Working Life and Welfare (In Swedish: Forte; Reg.nr: 2013-1836) to Kristina Sundquist, the Swedish Research Council to Jan Sundquist (2012-2378) as well as ALF funding from Region Skaåne awarded to Jan Sundquist and Kristina Sundquist.
Footnotes
Compliance with Ethical Standards
Conflict of Interest Kenneth S. Kendler, Sara Larsson Lönn, Her-mine H. Maes, Paul Lichtenstein, Jan Sundquist and Kristina Sundquist declare that they have no conflicts of interest to report.
Human and Animal Rights and Informed Consent This study was approved by the Ethics Committee of Lund University in Malmö, Sweden.
References
- Boker S, Neale M, Maes H, Wilde M, Spiegel M, Brick T, Spies J, Estabrook R, Kenny S, Bates T, Mehta P, Fox J. openmx: an open source extended structural equation modeling framework. Psychometrika. 2011;76(2):306–317. doi: 10.1007/s11336-010-9200-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Peer influences on college drinking: a review of the research. J Subst Abuse. 2001;13(4):391–424. doi: 10.1016/s0899-3289(01)00098-0. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64(5):566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cox A, Rutter M, Yule B, Quinton D. Bias resulting from missing information: some epidemiological findings. Br J Prev Soc Med. 1977;31(2):131–136. doi: 10.1136/jech.31.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Anthony JC, Tepper S, Dryman A. Psychopathology and attrition in the epidemiologic catchment area surveys. Am J Epidemiol. 1992;135(9):1051–1059. doi: 10.1093/oxfordjournals.aje.a116399. [DOI] [PubMed] [Google Scholar]
- Graziano F, Bina M, Giannotta F, Ciairano S. Drinking motives and alcoholic beverage preferences among Italian adolescents. J Adolesc. 2012;35(4):823–831. doi: 10.1016/j.adolescence.2011.11.010. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Heath AC, Madden PA, Martin NG. Assessing the effects of cooperation bias and attrition in behavioral genetic research using data-weighting. Behav Genet. 1998;28(6):415–427. doi: 10.1023/a:1021633127604. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders: a twin-family study. Arch Gen Psychiatry. 2004;61(9):922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- Karp JF, Frank E, Anderson B, George CJ, Reynolds CF, III, Mazumdar S, Kupfer DJ. Time to remission in late-life depression: analysis of effects of demographic, treatment, and life-events measures. Depression. 1993;1:250–256. [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GP, Roysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common dsm-iv axis I and all axis II disorders. AJP. 2011;168(1):29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Eaves LJ. The estimation of probandwise concordance in twins: the effect of unequal ascertainment. Acta Genet Med et Gemellol. 1989;38(3–4):253–270. doi: 10.1017/s000156600000266x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Ji J, Edwards AC, Ohlsson H, Sundquist J, Sundquist K. An extended swedish national adoption study of alcohol use disorders. JAMA Psychiatry. 2014;72:211–218. doi: 10.1001/jamapsychiatry.2014.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Maes HH, Sundquist K, Ohlsson H, Sundquist J. Genetic and family and community environmental effects on drug abuse in adolescence: a Swedish National Twin and Sibling Study. AJP. 2013;171(2):209–217. doi: 10.1176/appi.ajp.2013.12101300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Myers J. The boundaries of the internalizing and externalizing genetic spectra in men and women. Psychol Med. 2013;44(3):647–655. doi: 10.1017/S0033291713000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Sundquist K, Ohlsson H, Palmer K, Maes H, Winkleby MA, Sundquist J. Genetic and familial environmental influences on the risk for drug abuse: a national Swedish adoption study. Arch Gen Psychiatry. 2012;69(7):690–697. doi: 10.1001/archgenpsychiatry.2011.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56(10):921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. J Abnorm Psych. 1998;107(2):216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: internalization, externalization, and their connections to personality. Person Individ Differ. 2001;30(7):1245–1259. [Google Scholar]
- Lichtenstein P, de Faire U, Floderus B, Svartengren M, Svedberg P, Pedersen NL. The Swedish Twin Registry: a unique resource for clinical, epidemiological and genetic studies. J Intern Med. 2002;252(3):184–205. doi: 10.1046/j.1365-2796.2002.01032.x. [DOI] [PubMed] [Google Scholar]
- Piquero NL, Gover AR, MacDonald JM, Piquero AR. the influence of delinquent peers on delinquency: does gender matter? Youth Soc. 2005;36:251–275. [Google Scholar]
- Prescott CA, Gottesman I. power limitations in detecting heterogeneity of genetic effects: the case of sex differences in alcoholism. Presented at the annual meeting of the Society for Research on Psychopathology; Oct 1993; Chicago. [Google Scholar]
- Robins LN. Deviant children grown up. Baltimore: Williams & Wilkins; 1966. [Google Scholar]
- Sullivan PF, Eaves LJ. Evaluation of analyses of univariate discrete twin data. Behav Genet. 2002;32(3):221–227. doi: 10.1023/a:1016025229858. [DOI] [PubMed] [Google Scholar]
- Svensson R. Gender differences in adolescent drug use—the impact of parental monitoring and peer deviance. Youth Soc. 2003;34(3):300–329. [Google Scholar]
- Swedish National Council for Crime Prevention. Victims’ tendency to report crime, report 2008:12. Stockholm: Brottsforebyggande radet; 2008. [Google Scholar]