Abstract
Extracellular matrix is composed by a complex array of molecules that together provide structural and functional support to cells. These properties are mainly mediated by the activity of collagenous and elastic fibers, proteoglycans, and proteins such as fibronectin and laminin. ECM composition is tissue-specific and could include matricellular proteins whose primary role is to modulate cell-matrix interactions. In adults, matricellular proteins are primarily expressed during injury, inflammation and disease. Particularly, they are closely associated with the progression and prognosis of cardiovascular and fibrotic diseases, and cancer. This review aims to provide an overview of the potential use of matricellular proteins in drug delivery including the generation of therapeutic agents based on the properties and structures of these proteins as well as their utility as biomarkers for specific diseases.
Keywords: Extracellular matrix, matricellular, cell-matrix interactions, angiogenesis, fibrosis
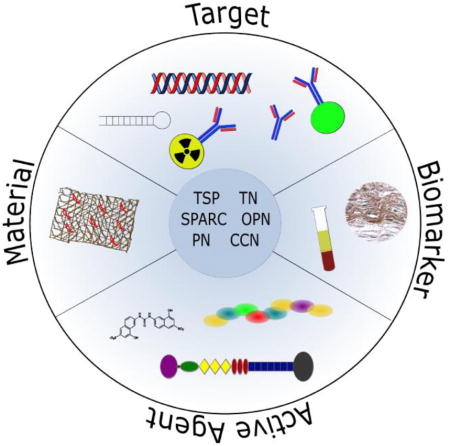
Graphical abstract
1. Introduction
Matricellular proteins constitute a class of molecules linked by their ability to function as modulators of cell-matrix interactions without serving primary roles as structural components (1). Originally, this genetically unrelated group consisted of several thrombospondin (TSP) family members, osteopontin (OPN), tenascin-C (TN-C), and secreted protein acidic and rich in cysteines (SPARC). More recently, the group has expanded to include additional proteins such as periostin, autotaxin, PEDF, fibulin-5 and other tenascins that contribute to its functional complexity. In fact, for some matricellular proteins there is now an appreciation for significant intracellular functions (2–7). Because of their ability to interact with both matricellular proteins and cell surface receptors, these proteins have been shown to influence ECM assembly (collagen secretion, fibrillogenesis) as well as numerous cell functions (adhesion, proliferation, migration). Despite the ability of the matricellular proteins to influence these significant processes, mice lacking one or more matricellular genes are, in most cases, viable and fertile and do not display remarkable phenotypes (8). These observations suggested that the matricellular proteins are dispensable during development. However, some matricellular proteins, including autotaxin and members of the CCN family, are necessary for development, and deletion is embryonic lethal (9, 10). In addition, their expression in adult tissues is usually low but is highly induced in various pathologies or injuries (11–14). Therefore, investigators have sought to establish functions in various disease and injury models. Such studies have expanded our understanding of the matricellular proteins and have suggested that they can be exploited in the context of developing therapeutic strategies, and many of those strategies have advanced to the clinic (Table 1) (15). Specifically, because they have diverse functions in many tissues, they can they can be used in multiple ways to enable effective drug delivery. Based on their expression and contribution to various pathologies, matricellular proteins could serve as either targets for inhibition or as a basis for the development of therapeutic agents (15–19). In addition, their ability to interact with both cells and matrix makes them suitable for localized drug delivery. Finally, the presence of certain matricellular proteins, both in diseased tissue or in circulation, can indicate the state and progression of the disease and thus could be useful biomarkers for assessing clinical outcomes (Table 2). Therefore, several matricellular proteins have been suggested as diagnostic or predictive biomarkers for various diseases ranging from cardiovascular pathologies to cancer (20, 21).
Table 1.
Registered clinical trials of matricellular protein-based therapeutic agents
| Family | Agent | Trial Design | Population | Study Phase | Enrollment (actual or estimated) | Trial Number |
|---|---|---|---|---|---|---|
| Thrombospondins | ABT-510 | TSP-1 mimetic to treat advanced renal cell carcinoma | Patients with locally recurrent or metastatic renal cell carcinoma that is not amendable to curative resection | Phase II | 103 | NCT00073125 |
| ABT-510 | TSP-1 mimetic to treat advanced or metastatic soft tissue carcinoma | Patients with locally advanced or metastatic soft tissue sarcoma not amenable to surgery, radiotherapy or combined modality therapy with curative intent | Phase II | 88 | NCT00061659 | |
| ABT-510 | TSP-1 mimetic plus combination chemotherapy in subjects with non-small cell lung cancer | Patients with Stage IIIB with pleural effusion or Stage IV NSCLC | Phase II | 25 | NCT00061646 | |
| ABT-510 | TSP-1 mimetic to treat patients with advanced head and neck cancer | Patients with squamous cell carcinoma of the head and neck that is not amenable to curative therapy, including radiation or surgery | Phase I, II | 6 | NCT00113334 | |
| ABT-510 | TSP-1 mimetic to treat subjects with refractory lymphoma | Patients with non-Hodgkin's Lymphoma (NHL) (excluding Burkitt's, Burkitt's type or HIV associated lymphoma) or Hodgkin's Lymphoma (HL) that is refractory to or has relapsed after standard therapy or for which there is no known effective treatment | Phase II | 67 | NCT00061672 | |
| CVX-045 | A Thrombospondin-1 Mimetic, Anti-Angiogenic Agent, In Patients With Advanced Solid Tumors | Patients with advanced solid tumors unresponsive to currently available therapies, or for which there is no standard therapy | Phase I | 40 | NCT00879554 | |
|
| ||||||
| Osteopontin | Osteopontin | Osteopontin addition to formula to increase infant growth, health, and immune function | Healthy infants 37–42 weeks of age. | 320 | NCT00970398 | |
|
| ||||||
| Tenascins | Neuradiab® | Combination therapy with Bevacizumab and Neuradiab (131I-labled anti tenascin mab) | Recurrent glioblastoma | Phase II | 60 | NCT00906516 |
| 211At labled 81C6 (mab) | Astatine 211 labled anti-tenascin mab (At 211 Mab 81C6) delivered into the resection cavity | Recurrent primary and metastatic brain tumors | Phase I, II | 12–24 | NCT00003461 | |
| I 131 Mab 81C6 | Iodine 131 labled anti-tenascin mab infused into the resection cavity and followed by carmustine and irinotecan chemotherapy | Primary brain tumors after external beam radiation | Phase I, II | 21 | NCT00003484 | |
| I 131 Mab 81C6 | Iodine 131 labled anti-tenascin mab infused into the resection cavity | Primary or metastatic brain tumors, with or without previous radiotherapy | Phase I, II | NCT00002752 | ||
| I 131 Mab 81C6 | Comparison of bolus injection and microinfusion of radiolabled anti-tenascin mab | Malignant primary brain tumors | Phase I, II | 10 | NCT00003478 | |
| I 131 Mab 81C6 | Intracystic delivery of radiolabled anti-tenascin mab | Recurrent cycstic glioma | Phase I | 6 | NCT00002753 | |
| Neuradiab® | Randomized evaluation of radiolabled anti-tenascin mab in combination with radiation therapy (XRT) and temozolomide | Newly diagnosed glioblastoma multiforme | Phase III | 9 | NCT00615186 | |
|
| ||||||
| CCNs | FG-3019 | Monoclonal antibody targeting CTGF for treatment of liver fibrosis | Chronic hepatitis B infection and liver fibrosis | Phase II | 228 | NCT01217632 |
| FG-3019 | Monoclonal antibody targeting CTGF for treatment of advanced or metastatic pancreatic cancer | Stage III or IV adenocarcinoma of the pancreas | Phase I | 50 | NCT01181245 | |
| FG-3019 | Monoclonal antibody targeting CTGF for treatment of focal segmental glomerulosclerosis | Focal segmental glomerulosclerosis | Phase I | 12 | NCT00782561 | |
| FG-3019 | Monoclonal antibody targeting CTGF for treatment of diabetic nephropathy | Diabetic nephropathy and proteinuria (with ACE inhibitor or angiotensin II receptor antagonist therapy) | Phase I | 36 | NCT00754143 | |
| Phase II | 34 | NCT00913393 | ||||
| FG-3019 | Monoclonal antibody targeting CTGF for treatment of idiopathic pulmonary fibrosis | Idiopathic pulmonary fibrosis | Phase II | 136 | NCT01890265 | |
| Phase II | 42 | NCT01262001 | ||||
| Phase I | 27 | NCT00074698 | ||||
| FG-3019 | Monoclonal antibody targeting CTGF as neoadjuvant chemotherapy for advanced pancreatic cancer | Pancreatic ductal adenocarcinoma | Phase II | 40 | NCT02210559 | |
| FG-3019 | Monoclonal antibody targeting CTGF for treatment of incipient nephropathy | Type 1 or type 2 diabetes and incipient nephropathy | Phase I | 20 | NCT00102297 | |
| Pravastatin | Small molecule targeting Rho/ROCK/CTGF pathway for treatment of radio-induced fibrosis | Cutaneous and subcutaneous radio-induced fibrosis | Phase II | 55 | NCT01268202 | |
| Sparc | Nab-paclitaxel | Albumin bound nanoparticles proposed to target elevated SPARC in tumor microenvironment | SPARC positive patients with resectable/resectable borderline pancreatic cancer | Pilot | 15 | NCT01442974 |
|
| ||||||
| PEDF | AdGVPEDF.11D | Adenoviral vector containg the gene to encode PEDF | Neovascular age-related macular degeneration (AMD) | Phase I | NCT00109499 | |
Selected clinical trials from the U.S. National Institutes of Health database, ClinicalTrials.gov
Table 2.
Registered clinical trials based on matricellular proteins as biomarkers
| Family | Model | Trial Design | Status | Trial Number |
|---|---|---|---|---|
| Thrombospondins (TSPs) | Intracerebral Hemorrhage | Determine the predictive effect of TSP1 levels (plasma) in patients with acute intracerebral hemorrhage | Completed | NCT02465671 |
| Diabetes | Expression of TSP1 (blood and vitreous) in diabetes | Completed | NCT01809093 | |
|
| ||||
| Osteopontin | Coronary Artery Disease (CAD) | OPN and other proteins as biomarkers (plasma) for CAD severity | Completed | NCT02159235 |
|
| ||||
| (OPN) | Osteoarthritis | Expression of OPN and other proteins (synovial fluid) in osteoarthritis and correlation to inflammatory markers | Recruiting | NCT01993342 |
| Head, Neck, Lung Cancers | OPN and other proteins as biomarkers (serum, tumor) for head, neck, and lung cancers | Recruiting | NCT00568490 | |
| Mesothelioma | OPN and other proteins as biomarkers (serum) for malignant pleural mesothelioma | Completed | NCT02029105 | |
|
| ||||
| CCN | Transitional Cell Carcinoma | Expression of CCN1/CYR61 in urinary tract transitional cell carcinomas | Pending | NCT01189838 |
| Non-small Cell Lung Cancer | CCN1/CYR61 as a transcript biomarker (salivary) for non-small cell lung cancer detection | Recruiting | NCT02294578 | |
| Proliferative Retinopathy | CCN1/CYR61 as a biomarker (vitreous) for different stages of proliferative diabetic retinopathy | Completed | NCT01920984 | |
| Atrial Fibrillation | CTGF as a biomarker (plasma) for recurrence of atrial fibrillation after surgical maze procedure | Completed | NCT00542659 | |
| Kidney Disease | CTGF as a biomarker (urinary and serum) for chronic allograft nephropathy | Completed | NCT00056784 | |
|
| ||||
| SPARC | Triple Negative Metastatic Breast Cancer | SPARC expression in breast tumors as a prediction for progression-free survival post chemotherapy | Completed | NCT00479674 |
| Non-Small Cell Lung Cancer | SPARC expression and correlation with overall survival post chemotherapy | Completed | NCT00540514 | |
| Periostin | Chronic Kidney Disease | Periostin as a biomarker (urinary) for renal pathology and chronic kidney disease | Completed | NCT02493101 |
| Bone Fragility | Periostin as a biomarker (serum) for cortical porosity in hyperparathyroidism patients | Recruiting | NCT02524041 | |
| Asthma | Periostin as a biomarker (serum) for “allergic” vs. “non-allergic” asthma | Completed | NCT01618318 | |
| Periodontal Disease | Periostin as a biomarker (gingival crevicular fluid (GCF), saliva, serum) for susceptibility and/or progression of periodontal disease | Completed | NCT01180920 | |
|
| ||||
| Autotaxin | Intrahepatic cholestasis of pregnancy | Determine the diagnostic accuracy of autotaxin as a biomarker for cholestasis and differentiate ICP from of liver disorders | Recruiting | NCT02480478 |
|
| ||||
| PEDF | Diabetes mellitus | Measure levels and isoforms of PEDF and TSP-1 to determine correlation with diabetic retinopathy severity | Completed | NCT01809093 |
Selected clinical trials from the U.S. National Institutes of Health database, ClinicalTrials.gov
2.1 Thrombospondins and drug delivery
Thrombospondins (TSP) are a family of secreted multifunctional ECM proteins with five members (TSP 1-5) (8). TSP-1 and -2 are synthesized as homotrimers with a molecular weight of 450,000. TSP-3, -4 and -5 are synthesized as homopentamers with molecular weights of each monomer ranging from 105,000 to160,000. TSP-1 and TSP-2 share a high degree of homology and display potent anti-angiogenic activity (22). However, they display distinct spatiotemporal expression patterns and functional diversity due to differences in their promoter regions (23). For example, both are implicated in wound healing but TSP-1, which is primarily released by platelets and secreted by monocytes/macrophages, plays a significant role in the early inflammatory phase. In contrast, TSP-2 is mainly secreted by fibroblasts and influences matrix remodeling. In addition to angiogenesis, TSPs have been implicated in many other processes including ECM synthesis and assembly, synaptogenesis, and inflammation (24–26). Despite the differences in structure and expression patterns, TSPs have been implicated in a variety of diseases including cancers, glaucoma, pulmonary and cardiovascular diseases, and kidney diseases (14, 27–30). Because of their significant roles in these conditions, both the overexpression and inhibitory targeting of TSPs have been pursued as therapeutic treatments (31–34).
The primary biological functions of TSP-1 are platelet aggregation, modulation of the inflammatory response, and the regulation of angiogenesis (35). Of these roles, the antiangiogenic effect is the most studied (36). In cancer, many oncogenic mutations result in the downregulation of TSP-1, which enable a proangiogenic phenotype (37). The restoration or induction of TSP-1 signaling in the tumor environment has the potential to restrict tumor growth by decreasing the tumor vasculature. This effect was observed in human skin carcinoma cells that were engineered to express TSP-1, the resulting tumors had greatly reduced vascularity and exhibited restricted growth (38). The effect was reversed with antisense inhibition of TSP-1. The inhibition of angiogenesis and restriction of tumor growth was also observed in cutaneous squamous cell carcinomas, breast carcinomas, and in human gliomas transfected to overexpress TSP-1 (39–41).
The initial attempt to create a therapy out of TSP-1’s antiangiogenic properties was with the isolation of antiangiogenic peptides from the larger TSP-1 protein (42). A recombinant protein composed of 3 type 1 repeats (TSR) from the antiangiogenic region of TSP-1was designed to avoid using the full length protein. 3TSR treatment was initially proven effective at inhibiting lung and pancreatic tumor growth (43, 44). Antiangiogenic treatment with 3TSR has also been used in combination with traditional cytotoxic chemotherapy. In an advanced ovarian cancer model, treatment with 3TSR normalized the tumor vasculature and increased the efficacy of carboplatin delivered by either a maximum tolerated dose or metronomic dosing regimens (45). Similary, lexatumumab, a humanized antibody against TRAIL receptor DR5, was used in combination with 3TSR to attack tumor endothelial cells. The combination therapy was shown to be more effective than either drug as a monotherapy in treating a colon cancer model in mice (46). This synergy results from 3TSRs ability to upregulate DR5, and prime the tumor cells for treatment with the antibody (47).
In addition to 3TSR, individual peptides from TSP-1 were created and utilized for antiangiogenic chemotherapy (48). The two peptide mimetics, named ABT-510 and ABT-526, were shown to be effective at inhibiting angiogenesis and tumor growth in both mouse cancer models and naturally occurring cancers in dogs (48–50). An initial phase 1 study of ABT-510 in humans showed linear pharmokinetics across all doses, but continuous infusions resulted in pain at the injection site, which was minimized by bolus dosing (51). Further clinical trials investigated ABT-510 as a monotherapy for patients with advanced soft tissue sarcoma, renal cell carcinoma, and metastatic melanoma (52–54). In each case ABT-510 exhibit a good safety profile, but failed to produce clinical responses. ABT-510 was used in additional Phase 1 clinical trials in combination with 5-fluoruracil and leucovorin, or gemcitabine and cisplatin, for solid tumors, and with temozolomide and radiation as a treatment for glioblastoma (55–57). Each study noted a strong safety profile for ABT-510 as part of a combination therapy. Additional combination therapies are being examined in preclinical models to build on ABT-510s antiangiogenic capability (58, 59).
Like TSP-1, TSP-2 is antiangiogenic and a potent inhibitor of tumor growth (60). Cell-based techniques have been developed to provide local delivery of TSP-2, and could prove useful for cancer treatment, macular degeneration, or other diseases of aberrant angiogenesis (61). However, TSP-2 also plays a role in ECM assembly, wound healing, and the foreign body response (62–64). Wounds in TSP-2 null mice appear to heal faster, produce less scarring, and produce an irregular, highly vascularized, granulation tissue. Injection of polymer-based delivery vehicles loaded with antisense TSP-2 cDNA was able to reproduce the increased angiogenesis and irregular matrix remodeling observed in the null mice (65).
Implants in TSP-2 null mice induce an altered foreign body response that results in more vascularized capsules, when compared to WT controls. A gene-activated matrix that delivered anti-sense TSP-2 cDNA was able to induce local transfection and yield a vascularized capsule similar to TSP-2 null mice (66). Looser, more vascularized capsules could enable the use of implantable devices, like glucose sensors for diabetics. A reduced FBR would also be advantageous for vascular grafts, where adverse remodeling after implantation can lead to neointimal hyperplasia and restenosis. One potential solution, a vascular graft coated in gene delivery vehicles for TSP-2 siRNA, showed the ability to transfect adhered aortic smooth muscle cells and knockdown TSP-2 (67).
2.2 Osteopontin and drug delivery
OPN, also known as bone sialoprotein I (BSP-1 or BNSP) is a highly negatively charged, extracellular matrix protein that is heavily glycosylated and phosphorylated (68–70). Both the extensive presence of acidic amino acids and many phosphate groups contribute to its negative charge. In addition to phosphorylation, OPN undergoes glycosylation and sulphation (71). Moreover, full length OPN can be modified via enzymatic digestions by thrombin and carboxypeptidase C that expose cryptic sequences and remove the C-terminal amino acids, respectively. Splice variants of OPN have also been described with expression patterns that appear to be cancer-specific (72). Coupled with the ability of OPN to interact with multiple receptors, the existence of multiple OPN isoforms contribute to its functional complexity. Even though OPN was first identified as a major constituent of bone with prominent roles in bone formation and calcification, it is now appreciated that it is a multifunctional molecule with critical roles in physiology and pathology that are primarily dependent on its spatiotemporal expression. Consistent with its extensive associations with numerous processes, OPN has been shown to be expressed in multiple cell types including fibroblasts, various bone cells, chondrocytes, immune and inflammatory cells, and vascular cells and it is associated with cell attachment via integrins, chemotaxis, and survival/apoptosis (68). In terms of physiological processes, OPN functions in bone mineralization and remodeling, angiogenesis, and immune and cardiovascular functions (68, 69, 73). OPN has also been linked to many pathological conditions such as skeletal disorders, cancer, rheumatoid arthritis, multiple sclerosis, atherosclerosis and heart disease (68, 73–80).
OPN has been shown to play a role in the epithelial to mesenchymal transition (EMT), a process where epithelial cells lose polarity and gain motility (18). In cancer, EMT generally precedes growth and metastasis, which makes OPN a likely biomarker for disease progression. In colon, prostate, pancreatic, head and neck, and metastatic breast cancers, expression of OPN is correlated with disease progression and decreased survival (81–86). Osteopontin is also strongly associated with metastasis, particularly with bone metastasis, which makes it a good biomarker for disease progression in many types of cancers (87, 88).
The role of OPN in the growth and metastasis of multiple cancers is well-known, and there have been multiple studies examining OPN as a therapeutic target (74, 89). The anticancer effects of dietary genistein (an isoflavone found in soy bean), resveratrol, curcumin, and thalidomide in animal cancer models was partially attributed to each compounds ability to decrease OPN (90–93). Posttrascriptional gene silencing using siRNA or shRNA has also been used to silence OPN expression in animal models of cancer. The technique has been used extensively in models of liver and gastric cancers, with knockdown of OPN resulting in decreased growth, invasion, and angiogenesis (21). Similar results were seen in vitro and in vivo with breast, oral, and endometrial cancer cell lines (94–96). As with other matricellular proteins, aptamers, small molecule inhibitors, and antibodies can also be used therapeutically (74, 97).
An alternate approach to treating cancer, via the inhibition of OPN, is by attempting to prevent metastasis. To examine this approach Yu et. al. used an orthotopic mouse breast cancer model that metastasized to the lungs (98). Two weeks after tumor inoculation, shRNA against OPN was delivered as an aerosol into the lungs of the mice. The shRNA decreased the levels of OPN in the lung tissue and prevented metastasis up to two months after application.
Outside of cancer, OPN has been associated with a variety of other diseases. A recent study of OPN as a biomarker for sepsis, determined that plasma OPN could serve as a prognostic biomarker for a variety of critically ill patients (99). This increase in plasma OPN was attributed to increased levels TNF-α and IL-1, which are increased in inflammation and stimulate the expression of OPN. Plasma OPN also correlated with disease severity in both alcoholic liver cirrhosis and hepatic fibrosis from hepatitis C virus infection (100, 101). Moreover, hydrodynamic intravenous injection of OPN siRNA reduced liver tissue injury in a murine model of concanavalin A (ConA)-induced fulminant hepatitis (102).
Osteopontin has also been shown to be upregulated during oxidative stress, making it a biomarker for vascular diseases (103–105). In a mouse stroke model, OPN increased after injury, reaching peak levels 5 days post-occlusion (106). In humans, OPN increased after stroke, and greater levels in plasma correlated with disability and decreased functional outcome (104, 107).
The use of OPN as a target or treatment for cardiac disease is complicated by the need to balance inflammation, angiogenesis, and fibrosis (19). However, in the CNS, OPN is neuroprotective when administered after an ischemic event (108). The neuroprotective effect is mediated via RGD motif and signaling via Akt and MAPK. As a therapy, both OPN peptide mimics and OPN containing gelatin nanoparticles were neuroprotective in a mouse MCAO stroke model after intranasal administration (109–111).
Outside of OPNs use as an active agent or therapeutic target, the adhesive capability of OPN, mediated by a variety of binding motifs, makes it a good candidate for integrative biomaterial coatings and implants (112). For example, surface treatment of positively charged polymer (p(HEMA-co-AEMA) with oriented OPN reduced the foreign body response in a mouse implant model (113). Mixtures of OPN and gelatin have shown improved integration in both tooth and bone repair (114, 115). The adhesive capacity can also be used to direct the cellular coating of biomaterial implants. Endothelial progenitor cells were shown to increase adhesion and spreading on a surface coated with OPN (116). Similarly, mesenchymal stem cells showed attachment, spreading, and motility on OPN coated hydroxyapatite and gold surfaces, which could be potentially useful as orthopedic implants (117). Finally, in a murine dorsal air sac assay the OPN-derived peptide SVVYGLR induced an angiogenic response similar to vascular endothelial growth factor (VEGF) (118).
2.3 Tenascins and drug delivery
Four molecules, TN-C, TN-R, TN-W, and TN-X make up the TN family. These large oligomeric proteins are homologous in structure and are made as homotrimers or hexamers that contain tandem epidermal growth factor and fibronectin type III repeats and a fibrinogen homology domain (119, 120). As a family, the tenascins have been shown to play roles in cancer, fibrosis, and the function of the central nervous system (CNS) (120, 121). However, more specialized roles in physiological and pathological conditions have been described for each member. TN-C is a hexameric protein with a molecular weight of 220,00 and is the most widely studied member of the family (122, 123). It has anti-adhesive properties that are mediated by its ability to interact with fibronectin. In addition, isoforms of TN-C generated via alternative splicing have shown functional heterogeneity that includes effects on cell proliferation and migration. Thus far, TN-C has been implicated in various diseases including cancers and sarcomas, fibrosis, and cardiovascular disease (124–127). TN-R, TN-W, and TN-X exist in multiple isoforms and are less well studied with limited reports linking them to vascular calcification, Ehlers-Danlos syndrome, and CNS diseases (128–131).
In cancer, TN-C is produced by both the tumor and stromal cells in the primary tumor and as a part of the metastatic niche (119). TN-C supports the growth and metastasis of neoplasms by promoting proliferation, migration, angiogenesis, metastasis, and aiding in the EMT (132–134). In breast cancer, TN-C expression is correlated with disease progression and relapse by metastasis to the lung and is a potential biomarker for the disease (135, 136). Similarly, TN-C has also been noted as a biomarker for pancreatic, bladder, colorectal cancers, and glioma (137–141). Therapeutic inhibition of TN-C is a possible treatment strategy in these models as well, which was illustrated in a mouse breast cancer model when cells treated with shRNA against TN-C produced fewer metastases (135).
A great amount of research has been conducted on the relationship between TN-C and glioma. Expression of TN-C in glioma is associated with increased invasion, recurrence, and poor prognosis (142). Encouragingly, initial research using glioma cell lines showed that inhibition of TN-C using antibodies resulting in decreased proliferation and migration (143). As a result, one of the first studies of RNAi in humans was a study that injected dsRNA targeting TN-C into the brains of patients with recurrent gliomas (144). After positive results in the initial, 8 person, study, a larger 46 person trial was conducted (145). The results showed an improvement in survival and disease score, but the observed benefits were not definitively linked to therapeutic gene silencing. However, the study was a promising first step towards a new therapy for glioma, and there have been numerous advances in RNAi technology since the completion of the study.
Another way the overexpression of TN-C can be used to treat brain tumors is by using targeting ligands to localize toxins or radiotherapeutics. Using this strategy, an aptamer against TN-C was able to localize imaging agents to intracranial tumors, indicating potential as a therapeutic (146). An alternative to aptamers, antibodies against TN-C have been developed, tagged with radiolabels, and are able to specifically target intracranial tumors from i.v. administration (147, 148). One therapeutic modality, referred to as an avidin-biotin pretargeting system, used systemic administration of a biotinylated anti-tenascin antibody, followed by avidin administration and then subsequent administration of a biotinylated radioligand to provide radiotherapy (149).
Anti-TN-C antibodies were also used in intracranially delivered radiotherapy. Phase one safety studies showed good tolerability with few instances of hematologic toxicity of TN-C targeted radioligands administered into the resection cavity of patients with recurrent or newly diagnosed glioma (150, 151). Follow up studies evaluated new antibodies, radioligands, patient populations, and dosing methods, all with promising results for the intracranially delivered therapeutic (150, 152–155). The progression free survival achieved with the local administration of the targeted radiotherapy compared favorably with Gliadel, a locally delivered chemotherapeutic (156). The ability of TN-C antibodies to target radiotherapies could conceivably be extended to larger drug delivery vehicles delivered intracranially (157, 158).
TN-C also plays a role in cardiovascular disease. After myocardial infarction, TN-C is transiently expressed at the border of the injury and is not expressed in the mature scar (14). Experiments in TN-C null mice have demonstrated that it promotes cell migration in the early phase, but may contribute to fibrosis at later stages (159, 160). This highlights the multifunctional role of TN-C in cardiac remodeling, which involves the recruitment of myofibroblasts, collagen fiber formation, and angiogenesis that promote repair, as well as the creation of a de-adhesive state, upregulation of MMPs, and enhancement of inflammation that contribute to fibrosis (19). As such, TN-C is a reported biomarker for a number of cardiovascular diseases, including: dilated cardiomyopathy, coronary plaque rupture, heart failure, and acute myocardial infarction (161–166). For cardiovascular imaging, a labeled TN-C antibody has been used to noninvasively detect remodeling in rats after infarction, and could potentially be used to look for left ventricular remodeling, which can lead to heart failure in humans (167).
In vascular disease, TN-C has been shown to accelerate neointimal formation (168, 169). The formation was reduced in TN-C-null mice, identifying a possible therapeutic target. Towards this end, PLGA microparticles have been fabricated to deliver an antisense oligonucleotide against TN-C and are able to reduce smooth muscle cell proliferation and migration (170). Tenascin-C is also found in atherosclerotic plaques, and a labeled TN-C antibody was able to successfully image them in rats (171). The characteristics that make TN-C deleterious for vascular grafts could make it advantageous for aneurysm treatment. This was evident in a study that implanted TN-C coated platinum coils into a rat aneurysm model and observed accelerated organization and decreased aneurysm volume (172).
Tenascin-C can also serve as a biomarker and potential therapeutic for inflammatory conditions. TN-C is expressed at sites of damage and inflammation in rheumatoid joints, and is required to maintain inflammation (173). A preclinical investigation of a TN-C targeting antibody conjugated to IL10 (F8-IL10), successfully inhibited the progression of arthritis in a mouse model and showed a good safety profile in monkeys (174). An update on the Phase 1b study of F8-IL10 noted early beneficial effects and no dose-limiting toxicities (175).
Early promising results have also been observed in the connection between Alzheimer’s disease and TN-C (176). TN-C was noticed to be upregulated in cultured microglial cells challenged with amyloid β peptide and in the brains of mouse that overexpress a mutated amyloid β. Crossbreeding the amyloid β overexpressing mouse into a TN-C null mouse resulted in a reduced amyloid β load and improved disease pathogenesis, indicating an exciting new possible therapy.
While TN-C is the most studied member of the tenascin family, TN-W also plays a role in the progression of cancer (134). TN-W is present in many solid tumors, including colon and breast cancers, and functions in the same manner as TN-C, but its presence in healthy tissues is more restricted (177). Further studies have shown that TN-W could be an effective biomarker for glioma, melanomas, pancreas, kidney, and lung carcinomas, and warrants further study alongside TN-C as a biomarker and therapeutic target (20).
2.4 CCNs and drug delivery
CCN intercellular signaling proteins consist of six members that make the CCN family of extracellular matrix (ECM)-associated signaling proteins (178–182). Based on the first three members of this family (CYR61, CTGF, and NOV; now known as CCN1, CCN2, and CCN3, respectively) the acronym CCN was selected (183). WISP1, WISP2, and WISP3 were also added to the family as CCN4, CCN5, and CCN6. All the CCNs are characterized by having four conserved cysteine-rich domains. These include an insulin-like growth factor binding protein (IGFBP) domain (domain I), a Von Willebrand factor domain (domain II), a thrombospondin-homology domain (domain III), and a cysteine knot, heparin-binding domain (domain IV). Despite early studies suggesting that CCNs had growth factor-like activities, it is now well accepted that they are matricellular proteins with diverse functions. Importantly, consistent with the matricellular concept, CCN proteins are involved in the integration of signals between the extracellular matrix and the cell surface. Recent studies have also indicated that they play significant roles in several diseases and are considered valid candidates for either therapeutic targeting or development of therapeutics (184, 185). These include diseases related to chronic inflammation such as rheumatoid arthritis, atherosclerosis, diabetes-related pathologies, as well as hematological malignancies, and many cancers.
Expression of the CCN family of matricellular proteins is often correlated with increased vascular density, growth, and metastasis (179, 185). In fact, the increased presence of one or multiple members of the CCN family is associated with poor prognosis in breast, prostate, pancreatic, renal, bone, head and neck, and brain cancers (186–190). More specifically, CCN4 is upregulated in early stages of prostate cancer and correlated with higher circulating levels of the protein (191). CCN5 has been correlated with decreased progression free survival and overall survival in patients with astrocytomas (192). Additionally, CCN1 can be used as a biomarker to predict poor prognosis in patients with esophageal squamous cell carcinoma (193).
The overexpression of the CCN family during the growth and metastasis of cancer presents an opportunity for therapeutic intervention (184). Pancreatic, ovarian, and prostate cancer xenografts showed less growth and metastatic ability in vivo after transfection with RNA inhibitors against CCN1 or CCN2 (187, 194–196). siRNA against CCN1 was also effective at slowing the growth of an orthotopic glioma model when injected intratumorally (197). In addition to CCN1 and CCN2, CCN4 inhibition using antibodies was able to slow the growth and metastasis of a prostate cancer xenograft in vivo (191). In contract, the addition of CCN3, 5, and 6 can negatively affect proliferation of cancer xenografts (198–202).
Outside of cancer, CCN2 plays a prominent role in, and can be used as a biomarker for, many fibrotic diseases (184, 203). In scleroderma, CCN2 is correlated with severity of the disease in both plasma and tissue samples (204). Similarly, CCN2 in plasma also correlates with risk and mortality for patients with diabetic retinopathy (205, 206).
A strong relationship between CCN2 and multiple types of fibrotic disease has inspired the development of multiple therapeutic inhibitors (207, 208). Therapeutic gene silencing using siRNA has been shown to reduce the expression of CCN2 in vitro and in rodent models, and that the reduction in expression correlates with reduced fibrosis (209–211). Antisense oligonucleotides have also been used in rodent models with similar effects (212, 213).
Therapeutic antibodies against CCN2 have also been developed, and one, FibroGens’s FG-3019, is currently undergoing clinical trials for the treatment of fibrotic diseases in humans (184, 208, 214). A phase 1 study of FG-3019 in patients with diabetic nephropathy showed good tolerability and a reduction in albuminuria (215, 216). In the Duchenne muscular dystrophy mouse model, FG-3019 was able to improve muscular strength and reduce impairment and fibrosis (217). An aptamer is also being developed to inhibit CCN2 signaling (218).
CCN proteins themselves, because of their effects on adhesion, angiogenesis and inflammation, can also serve as therapeutics. CCN1 in particular has a potent ability to modulate inflammation (219). Vascular graft remodeling, a process driven by inflammation, was improved in a sheep model with a decellularized graft coated with CCN1 that showed enhanced endothelialization (220, 221). CCN1 also reduced immune infiltration and disease score in a mouse model of myocarditis (222).
2.5 SPARC and drug delivery
SPARC, also known as osteonectin, has a molecular weight of 40,000 and is composed of four domains that include a calcium-binding region at the amino terminus, a cysteine-rich domain, a hydrophilic domain, and a helix-loop-helix structural motif (EF hand) at the carboxy terminus (223, 224). In addition to binding calcium and promoting mineral crystal formation, SPARC interacts with collagen and participates in the activation of latent TGF-β (223). It is made by multiple cell types including fibroblasts, endothelial cells, osteoblasts and macrophages and has been shown to influence cell adhesion and morphology as well as proliferation. In addition, SPARC plays important roles in tissue remodeling, wound healing, and fibrosis. Various studies have also linked SPARC expression to different types of cancer, diabetes, glaucoma, and fibrotic disorders (225–231).
The role of SPARC in the pathophysiology of cancer is complicated by its many functions. SPARC can abrogate focal adhesions and lead to migration and metastasis (232). However, it can also bind and interact with growth factors to promote cell cycle arrest and reduce angiogenesis (233). This dichotomy is borne out in the literature, summarized nicely by Podhajcer et.al., where SPARC is noted to be highly expressed in a wide range of very aggressive human tumors, but is also noted to be antitumorigenic in many other models (234). Using glioblastoma as an example, SPARC expression has been correlated with increased migration and poor prognosis in humans (235, 236). However, when SPARC expression was inhibited using shRNA, a human cell line showed increased growth and tumorigenic potential (237). The multiple roles played by SPARC in the tumoral environment complicate its use as a biomarker and as a target for therapeutic inhibition.
The high expression of SPARC in the tumor environment, regardless of its function, could be used to localize other therapeutic molecules. The high levels of tumoral SPARC was proposed as one mechanism for the efficacy of nanoparticulate albumin bound paclitaxel (nab-paclitaxel), owing to the capacity of SPARC to bind albumin, and in a Phase III trial of nab-paclitaxel in metastatic pancreatic, SPARC had positive association with efficacy (238, 239). However, in a mouse pancreatic cancer model, this binding effect was found to be saturable at low doses and not responsible for efficacy of the nab-paclitaxel (240). The effect of SPARC expression on nab-paclitaxel efficacy in vivo is likely muted by the abundance of albumin in serum, and the pharmacokinetics of the nab-paclitaxel. More specific targeting of SPARC, using a high affinity antibody linked to a nanoparticle, was able to increase the detection of tumor and metastases using CT and fluorescent imaging in mice. SPARC can also be used as a target antigen to direct immunotherapy, providing therapeutic localization while avoiding inhibition (241).
Outside of cancer, SPARC is highly involved in fibrosis, mediated by its role in the organization of collagen and ECM assembly as well as TGF-β activity (1). In humans, SPARC expression is increased in pulmonary, renal, hepatic, and dermal fibrosis (230). Experiments in SPARC-null mice illustrated that in the absence of SPARC, fibrosis was decreased (230, 242). In wild type mice, SPARC gene silencing using siRNA has been examined as a method to reduce fibrosis. For example, the injection or instillation of siRNA against SPARC reduced the expression of SPARC in situ and reduced the extent of fibrosis in both skin a lung fibrosis models (243). A nanoparticle system based on hydroxyapatite was developed to deliver SPARC siRNA more efficiently to fibroblasts that drive fibrosis (244).
In a biomaterial based approach, SPARC-derived components susceptible to enzymatic cleavage have been incorporated into hydrogels to enhance their degradation in response to plasmin, matrix metalloproteinase 1 (MMP-1), and MMP-2 (245). Incorporation of such degradation sensitive sites allows for the tuned response of the hydrogel system, and enables tissue specific delivery.
2.6 Periostin and drug delivery
Periostin, also known as osteoblast-specific factor-2, has a molecular weight of 90,000 and contains a fasciclin domain (FAS1 domain), which is involved in cell adhesion (246, 247). It shares structural homology with FAS1, which is an axon guidance protein, and transforming growth factor (TGF)-β-induced protein, βig-h3. Consistent with the presence of a fasciclin domain, periostin promotes adhesion as well as spreading of various cell types (248). Isoforms of periostin also exist due to alternative splicing and have been linked to cancers (249). In addition, periostin has been associated with numerous pathological conditions including asthma, skin disorders, polycystic kidney disease, and cardiovascular disease (247, 250–254).
Periostin, like many of the other matricellular proteins, is expressed at low levels in healthy tissue but is upregulated in pathology and during tissue repair, and neoplasia (14). One pathological condition where periostin is significantly upregulated is asthma, as a result of fibrosis in the lungs (246). Specifically, periostin is associated with eosinophilic, TH2 driven asthma, which responds well to corticosteroid treatment (255). Serum levels of periostin can serve as a biomarker for this subtype of asthma and, when confirmed, patients can be given the appropriate therapy (256). Via a similar mechanism, periostin is a biomarker for idiopathic interstitial pneumonias with fibrosis (257).
The expression of periostin is increased in many cancers, including neuroblastoma, ovarian, breast, colon, pancreas, NSCLC, and head and neck cancers (258). In each of these cancers, the presence of periostin is associated with metastasis, progression, and poor survival. The therapeutic inhibition of periostin has been proposed as a method to reduce tumor growth and metastasis, and improve survival, particularly in gastric cancer and glioma (259, 260). This strategy was used successfully in an orthotopic breast cancer xenograft (261). After tumor inoculation, systemic injection of an inhibitory DNA aptamer, PNDA-3, reduced tumor growth and metastasis. Inhibition of tumor growth was also observed in an ovarian cancer model when periostin was inhibited by specific siRNA delivered using chitosan nanoparticles (262).
In development, periostin is responsible for ECM maturation in the heart (254). Similarly, in failing hearts, increased levels of periostin are associated with myocardial fibrosis (263). However, after a myocardial infarction, there is damaged tissue in the heart that needs to be repaired for proper function, and periostin, because of its ability to regulate fibrosis, angiogenesis, and proliferation, could promote the cardiac healing process (264). This hypothesis was tested in a rat myocardial infarct model, where delivery of periostin via injection or in a gelfoam matrix improved cardiac remodeling and reduced the infarct area after (265). The gelfoam matrix delivery system was evaluated again in a swine model of myocardial infarction (266). In this large animal model, delivery of periostin again resulted in increased cardiomyocyte cell cycle activity and increased angiogenesis at the infarct border. However, a similar study using gelfoam to deliver a periostin peptide described an increase in cardiac fibrosis in addition to improved cardiac function (267). The potentially limiting fibrosis observed in the swine model highlights the complexity encountered when delivering a multifunctional active agent with a complex signaling pathway. Clinical translation will rely on careful dosing and control over the pharmacokinetics to ensure improved healing without fibrosis.
2.7 Other Matricellular proteins and drug delivery
As mentioned in the introduction, the matricellular family of proteins has recently expanded with the addition of autotaxin, R-Spondin, PEDF, and fibulin-5. This diverse group of proteins has pleiotropic functions that include modulation of cell-matrix interactions and cell adhesion. Similar to the prototypical members of the matricellular family, studies have implicated these proteins in the pathophysiology of several diseases. In this section, we briefly describe these proteins, their functions, and their associations with specific diseases.
Autotaxin is an ecto-lysophospholipase involved in the generation of lysophosphatic acid and has been implicated in the regulation of proliferation, invasion, migration and angiogenesis (268). In addition, studies have implicated this protein in several diseases including idiopathic pulmonary fibrosis, liver cirrhosis, and several cancers (269–278). Because its structure has been elucidated and the active sites are defined, autotaxin has been utilized in the development of small molecular weight drugs (270, 279). R-spondins are predominantly involved in Wnt signaling and play roles in gonadal and skeletal development (280, 281). They are considered matricellular because they contain type 1 TSP repeats and can interact with both ECM components and cell surface receptors. PEDF is a secreted protein with anti-angiogenic and neurotrophic activities (282). It has been implicated in a diverse set of diseases including Alzheimers, acute coronary syndrome, bone diseases, and tumors (283–286). From a therapeutic perspective, PEDF has been successful employed in the treatment of age-related macular degeneration (282). In addition, its ability to treat tumors due to its anti-angiogenic activity and its role in other angiogenic diseases has received attention (287, 288). Finally, fibulin-5 is a secreted protein that is intimately involved in the process of elastogenesis and plays a prominent role in development (289). Similar to other matricellular protein it has anti-angiogenic activity and has been suggested as a possible treatment in tumors (290).
3 Conclusion
The ability of matricellular proteins to regulate cell-cell and cell-matrix interactions during the progression of multiple disease states makes them targets for potential therapies, most notably in cardiovascular diseases and cancer. Many matricellular proteins, including TSP-1and 2, SPARC, OPN, and TN-C, are involved in the structure and remodeling of the myocardium following injury (14, 19). They are typically expressed at low levels, if at all, in healthy tissue, but are highly expressed after injury and during remodeling. Their role in the regulation of vascular growth factors, and the creation of a de-adhesive state, can lead to improper remodeling and tissue dysfunction. However, in the correct context, certain matricellular proteins can actually improve healing after injury. This dichotomy complicates their use as therapeutics and therapeutic targets in cardiovascular disease.
In addition to cardiovascular disease, matricellular proteins have a demonstrated role in the progression of cancer. The hallmarks of cancer, and the progression of healthy cells towards malignancy, arise as a result of the loss of homeostasis governing growth, proliferation, and death (291). In addition, the growth and metastasis of the resulting neoplasm requires the induction of angiogenesis, increased motility, and avoidance of immune detection. The extracellular matrix and matricellular proteins are potent modulators of each of those hallmarks, and their expression can be used to drive or suppress cancer progression (292). Their integral role in the tumoral microenvironment makes matricellular proteins useful as biomarkers, therapeutic targets, and active agents.
However, the multifunctional role of matricellular proteins within the environment complicates their use in the design of novel therapies. Each of the matricellular proteins has multiple functional regions that interact with many cell surface and ECM molecules to modulate cell-cell and cell-matrix interactions. In many cases, the exact nature of these interactions is unclear, and can result in a complicated network of signaling events. For example, TSP1 has known antiangiogenic properties, but is also highly expressed in certain high grade tumors (293, 294). This suggests that in certain cancers the ability of TSP-1 to promote motility, proliferation, and adhesion, outweigh the effects on angiogenesis (295).
The complicated roles of matricellular proteins present significant difficulties in designing therapies to inhibit or mimic their activities. Fortunately, TSP-1 also provides a positive example of isolating a single matrix protein property for the development of a therapeutic agent. By identifying the specific peptide regions responsible for TSP1’s antiangiogenic activity, therapeutic peptides and small molecules can be designed to reduce angiogenesis in the clinic (34, 51). Similarly, elucidation of sites in these proteins that mediate their interactions with cells and matrix could lead to the development of small molecular weight inhibitors with highly specific activities. In addition to TSP1, the rest of the matricellular proteins discussed in this review highlight multiple opportunities for effective drug delivery, especially in cardiovascular disease and cancer. However, the continued development of therapies derived from matricellular proteins, will require more research to precisely define their mode of action, and allow for the identification and creation of powerful targets, agonists, and drug carriers.
Acknowledgments
The authors acknowledge funding support from the National Institute of Health (GM072194, HL 107205 and T32HL007950-12). We also thank Aaron Morris, Nicole Calabro, Nina Kristofik and Britta Kunkemoeller for helpful discussions and assistance with preparation of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Murphy-Ullrich JE, Sage EH. Revisiting the matricellular concept. Matrix Biol. 2014;37:1–14. doi: 10.1016/j.matbio.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lynch JM, Maillet M, Vanhoutte D, Schloemer A, Sargent MA, Blair NS, et al. A thrombospondin-dependent pathway for a protective ER stress response. Cell. 2012;149(6):1257–68. doi: 10.1016/j.cell.2012.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inoue M, Shinohara ML. Intracellular osteopontin (iOPN) and immunity. Immunol Res. 2011;49(1–3):160–72. doi: 10.1007/s12026-010-8179-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gooden MD, Vernon RB, Bassuk JA, Sage EH. Cell cycle-dependent nuclear location of the matricellular protein SPARC: association with the nuclear matrix. J Cell Biochem. 1999;74(2):152–67. [PubMed] [Google Scholar]
- 5.Yan Q, Weaver M, Perdue N, Sage EH. Matricellular protein SPARC is translocated to the nuclei of immortalized murine lens epithelial cells. J Cell Physiol. 2005;203(1):286–94. doi: 10.1002/jcp.20226. [DOI] [PubMed] [Google Scholar]
- 6.Wahab NA, Brinkman H, Mason RM. Uptake and intracellular transport of the connective tissue growth factor: a potential mode of action. Biochem J. 2001;359(Pt 1):89–97. doi: 10.1042/0264-6021:3590089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubota S, Hattori T, Shimo T, Nakanishi T, Takigawa M. Novel intracellular effects of human connective tissue growth factor expressed in Cos-7 cells. FEBS letters. 2000;474(1):58–62. doi: 10.1016/s0014-5793(00)01573-8. [DOI] [PubMed] [Google Scholar]
- 8.Murphy-Ullrich JE, Iozzo RV. Thrombospondins in physiology and disease: new tricks for old dogs. Matrix Biol. 2012;31(3):152–4. doi: 10.1016/j.matbio.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferry G, Giganti A, Coge F, Bertaux F, Thiam K, Boutin JA. Functional invalidation of the autotaxin gene by a single amino acid mutation in mouse is lethal. FEBS Lett. 2007;581(18):3572–8. doi: 10.1016/j.febslet.2007.06.064. [DOI] [PubMed] [Google Scholar]
- 10.Canalis E, Zanotti S, Beamer WG, Economides AN, Smerdel-Ramoya A. Connective tissue growth factor is required for skeletal development and postnatal skeletal homeostasis in male mice. Endocrinology. 2010;151(8):3490–501. doi: 10.1210/en.2010-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsui Y, Morimoto J, Uede T. Role of matricellular proteins in cardiac tissue remodeling after myocardial infarction. World J Biol Chem. 2010;1(5):69–80. doi: 10.4331/wjbc.v1.i5.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morris AH, Kyriakides TR. Matricellular proteins and biomaterials. Matrix Biol. 2014;37:183–91. doi: 10.1016/j.matbio.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong GS, Rustgi AK. Matricellular proteins: priming the tumour microenvironment for cancer development and metastasis. Br J Cancer. 2013;108(4):755–61. doi: 10.1038/bjc.2012.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frangogiannis NG. Matricellular proteins in cardiac adaptation and disease. Physiological Reviews. 2012;92(2):635–88. doi: 10.1152/physrev.00008.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bornstein P. Matricellular proteins: an overview. J Cell Commun Signal. 2009;3(3–4):163–5. doi: 10.1007/s12079-009-0069-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murphy-Ullrich JE. The de-adhesive activity of matricellular proteins: is intermediate cell adhesion an adaptive state? J Clin Invest. 2001;107(7):785–90. doi: 10.1172/JCI12609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bornstein P, Sage EH. Matricellular proteins: extracellular modulators of cell function. Curr Opin Cell Biol. 2002;14(5):608–16. doi: 10.1016/s0955-0674(02)00361-7. [DOI] [PubMed] [Google Scholar]
- 18.Chong HC, Tan CK, Huang RL, Tan NS. Matricellular proteins: a sticky affair with cancers. Journal of Oncology. 2012;2012:351089. doi: 10.1155/2012/351089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okamoto H, Imanaka-Yoshida K. Matricellular proteins: new molecular targets to prevent heart failure. Cardiovasc Therapeutics. 2012;30(4):e198–209. doi: 10.1111/j.1755-5922.2011.00276.x. [DOI] [PubMed] [Google Scholar]
- 20.Brellier F, Martina E, Degen M, Heuze-Vourc'h N, Petit A, Kryza T, et al. Tenascin-W is a better cancer biomarker than tenascin-C for most human solid tumors. BMC Clin Pathol. 2012;12:14. doi: 10.1186/1472-6890-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cao DX, Li ZJ, Jiang XO, Lum YL, Khin E, Lee NP, et al. Osteopontin as potential biomarker and therapeutic target in gastric and liver cancers. World J Gastroenterol. 2012;18(30):3923–30. doi: 10.3748/wjg.v18.i30.3923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawler PR, Lawler J. Molecular basis for the regulation of angiogenesis by thrombospondin-1 and -2. Cold Spring Harb Perspect Med. 2012;2(5):a006627. doi: 10.1101/cshperspect.a006627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stenina-Adognravi O. Invoking the power of thrombospondins: regulation of thrombospondins expression. Matrix Biol. 2014;37:69–82. doi: 10.1016/j.matbio.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calabro NE, Kristofik NJ, Kyriakides TR. Thrombospondin-2 and extracellular matrix assembly. Biochim Biophys Acta. 2014;1840(8):2396–402. doi: 10.1016/j.bbagen.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Risher WC, Eroglu C. Thrombospondins as key regulators of synaptogenesis in the central nervous system. Matrix Biol. 2012;31(3):170–7. doi: 10.1016/j.matbio.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lopez-Dee Z, Pidcock K, Gutierrez LS. Thrombospondin-1: multiple paths to inflammation. Mediators Inflamm. 2011;2011:296069. doi: 10.1155/2011/296069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Resovi A, Pinessi D, Chiorino G, Taraboletti G. Current understanding of the thrombospondin-1 interactome. Matrix Biol. 2014;37:83–91. doi: 10.1016/j.matbio.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 28.Esemuede N, Lee T, Pierre-Paul D, Sumpio BE, Gahtan V. The role of thrombospondin-1 in human disease. J Surg Res. 2004;122(1):135–42. doi: 10.1016/j.jss.2004.05.015. [DOI] [PubMed] [Google Scholar]
- 29.Ghoneim C, Soula-Rothhut M, Rothhut B. Thrombospondin-1 in differentiated thyroid cancer: Dr. Jekyll and Mr. Hyde. Connect Tissue Res. 2008;49(3):257–60. doi: 10.1080/03008200802147795. [DOI] [PubMed] [Google Scholar]
- 30.Kazerounian S, Yee KO, Lawler J. Thrombospondins in cancer. Cell Mol Life Sci. 2008;65(5):700–12. doi: 10.1007/s00018-007-7486-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henkin J, Volpert OV. Therapies using anti-angiogenic peptide mimetics of thrombospondin-1. Expert Opin Ther Targets. 2011;15(12):1369–86. doi: 10.1517/14728222.2011.640319. [DOI] [PubMed] [Google Scholar]
- 32.Sid B, Sartelet H, Bellon G, El Btaouri H, Rath G, Delorme N, et al. Thrombospondin 1: a multifunctional protein implicated in the regulation of tumor growth. Crit Rev Oncol Hematol. 2004;49(3):245–58. doi: 10.1016/j.critrevonc.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 33.Mustonen E, Ruskoaho H, Rysa J. Thrombospondins, potential drug targets for cardiovascular diseases. Basic Clin Pharmacol Toxicol. 2013;112(1):4–12. doi: 10.1111/bcpt.12026. [DOI] [PubMed] [Google Scholar]
- 34.Taraboletti G, Rusnati M, Ragona L, Colombo G. Targeting tumor angiogenesis with TSP-1-based compounds: rational design of antiangiogenic mimetics of endogenous inhibitors. Oncotarget. 2010;1(7):662–73. doi: 10.18632/oncotarget.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adams JC, Lawler J. The thrombospondins. Int J Biochem Cell Biol. 2004;36(6):961–8. doi: 10.1016/j.biocel.2004.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Good DJ, Polverini PJ, Rastinejad F, Le Beau MM, Lemons RS, Frazier WA, et al. A tumor suppressor-dependent inhibitor of angiogenesis is immunologically and functionally indistinguishable from a fragment of thrombospondin. Proc Natl Acad Sci U S A. 1990;87(17):6624–8. doi: 10.1073/pnas.87.17.6624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lawler J, Detmar M. Tumor progression: the effects of thrombospondin-1 and -2. Int J Biochem Cell Biol. 2004;36(6):1038–45. doi: 10.1016/j.biocel.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Bleuel K, Popp S, Fusenig NE, Stanbridge EJ, Boukamp P. Tumor suppression in human skin carcinoma cells by chromosome 15 transfer or thrombospondin-1 overexpression through halted tumor vascularization. Proc Natl Acad Sci U S A. 1999;96(5):2065–70. doi: 10.1073/pnas.96.5.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Streit M, Velasco P, Brown LF, Skobe M, Richard L, Riccardi L, et al. Overexpression of thrombospondin-1 decreases angiogenesis and inhibits the growth of human cutaneous squamous cell carcinomas. Am J Pathol. 1999;155(2):441–52. doi: 10.1016/S0002-9440(10)65140-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hsu SC, Volpert OV, Steck PA, Mikkelsen T, Polverini PJ, Rao S, et al. Inhibition of angiogenesis in human glioblastomas by chromosome 10 induction of thrombospondin-1. Cancer Res. 1996;56(24):5684–91. [PubMed] [Google Scholar]
- 41.Weinstat-Saslow DL, Zabrenetzky VS, VanHoutte K, Frazier WA, Roberts DD, Steeg PS. Transfection of thrombospondin 1 complementary DNA into a human breast carcinoma cell line reduces primary tumor growth, metastatic potential, and angiogenesis. Cancer Res. 1994;54(24):6504–11. [PubMed] [Google Scholar]
- 42.Tolsma SS, Volpert OV, Good DJ, Frazier WA, Polverini PJ, Bouck N. Peptides derived from two separate domains of the matrix protein thrombospondin-1 have anti-angiogenic activity. J Cell Biol. 1993;122(2):497–511. doi: 10.1083/jcb.122.2.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miao WM, Seng WL, Duquette M, Lawler P, Laus C, Lawler J. Thrombospondin-1 type 1 repeat recombinant proteins inhibit tumor growth through transforming growth factor-beta-dependent and -independent mechanisms. Cancer Res. 2001;61(21):7830–9. [PubMed] [Google Scholar]
- 44.Zhang X, Connolly C, Duquette M, Lawler J, Parangi S. Continuous administration of the three thrombospondin-1 type 1 repeats recombinant protein improves the potency of therapy in an orthotopic human pancreatic cancer model. Cancer Lett. 2007;247(1):143–9. doi: 10.1016/j.canlet.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Russell S, Duquette M, Liu J, Drapkin R, Lawler J, Petrik J. Combined therapy with thrombospondin-1 type I repeats (3TSR) and chemotherapy induces regression and significantly improves survival in a preclinical model of advanced stage epithelial ovarian cancer. FASEB J. 2015;29(2):576–88. doi: 10.1096/fj.14-261636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ren B, Song K, Parangi S, Jin T, Ye M, Humphreys R, et al. A double hit to kill tumor and endothelial cells by TRAIL and antiangiogenic 3TSR. Cancer Res. 2009;69(9):3856–65. doi: 10.1158/0008-5472.CAN-08-2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Choi SH, Tamura K, Khajuria RK, Bhere D, Nesterenko I, Lawler J, et al. Antiangiogenic variant of TSP-1 targets tumor cells in glioblastomas. Mol Ther. 2015;23(2):235–43. doi: 10.1038/mt.2014.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reiher FK, Volpert OV, Jimenez B, Crawford SE, Dinney CP, Henkin J, et al. Inhibition of tumor growth by systemic treatment with thrombospondin-1 peptide mimetics. Int J Cancer. 2002;98(5):682–9. doi: 10.1002/ijc.10247. [DOI] [PubMed] [Google Scholar]
- 49.Rusk A, McKeegan E, Haviv F, Majest S, Henkin J, Khanna C. Preclinical evaluation of antiangiogenic thrombospondin-1 peptide mimetics, ABT-526 and ABT-510, in companion dogs with naturally occurring cancers. Clin Cancer Res. 2006;12(24):7444–55. doi: 10.1158/1078-0432.CCR-06-0109. [DOI] [PubMed] [Google Scholar]
- 50.Haviv F, Bradley MF, Kalvin DM, Schneider AJ, Davidson DJ, Majest SM, et al. Thrombospondin-1 mimetic peptide inhibitors of angiogenesis and tumor growth: design, synthesis, and optimization of pharmacokinetics and biological activities. J Med Chem. 2005;48(8):2838–46. doi: 10.1021/jm0401560. [DOI] [PubMed] [Google Scholar]
- 51.Hoekstra R, de Vos FY, Eskens FA, Gietema JA, van der Gaast A, Groen HJ, et al. Phase I safety, pharmacokinetic, and pharmacodynamic study of the thrombospondin-1-mimetic angiogenesis inhibitor ABT-510 in patients with advanced cancer. J Clin Oncol. 2005;23(22):5188–97. doi: 10.1200/JCO.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 52.Markovic SN, Suman VJ, Rao RA, Ingle JN, Kaur JS, Erickson LA, et al. A phase II study of ABT-510 (thrombospondin-1 analog) for the treatment of metastatic melanoma. Am J Clin Oncol. 2007;30(3):303–9. doi: 10.1097/01.coc.0000256104.80089.35. [DOI] [PubMed] [Google Scholar]
- 53.Ebbinghaus S, Hussain M, Tannir N, Gordon M, Desai AA, Knight RA, et al. Phase 2 study of ABT-510 in patients with previously untreated advanced renal cell carcinoma. Clin Cancer Res. 2007;13(22 Pt 1):6689–95. doi: 10.1158/1078-0432.CCR-07-1477. [DOI] [PubMed] [Google Scholar]
- 54.Baker LH, Rowinsky EK, Mendelson D, Humerickhouse RA, Knight RA, Qian J, et al. Randomized, phase II study of the thrombospondin-1-mimetic angiogenesis inhibitor ABT-510 in patients with advanced soft tissue sarcoma. J Clin Oncol. 2008;26(34):5583–8. doi: 10.1200/JCO.2008.17.4706. [DOI] [PubMed] [Google Scholar]
- 55.Nabors LB, Fiveash JB, Markert JM, Kekan MS, Gillespie GY, Huang Z, et al. A phase 1 trial of ABT-510 concurrent with standard chemoradiation for patients with newly diagnosed glioblastoma. Arch Neurol. 2010;67(3):313–9. doi: 10.1001/archneurol.2010.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gietema JA, Hoekstra R, de Vos FY, Uges DR, van der Gaast A, Groen HJ, et al. A phase I study assessing the safety and pharmacokinetics of the thrombospondin-1-mimetic angiogenesis inhibitor ABT-510 with gemcitabine and cisplatin in patients with solid tumors. Ann Oncol. 2006;17(8):1320–7. doi: 10.1093/annonc/mdl102. [DOI] [PubMed] [Google Scholar]
- 57.Hoekstra R, de Vos FY, Eskens FA, de Vries EG, Uges DR, Knight R, et al. Phase I study of the thrombospondin-1-mimetic angiogenesis inhibitor ABT-510 with 5-fluorouracil and leucovorin: a safe combination. Eur J Cancer. 2006;42(4):467–72. doi: 10.1016/j.ejca.2005.08.040. [DOI] [PubMed] [Google Scholar]
- 58.Campbell NE, Greenaway J, Henkin J, Moorehead RA, Petrik J. The thrombospondin-1 mimetic ABT-510 increases the uptake and effectiveness of cisplatin and paclitaxel in a mouse model of epithelial ovarian cancer. Neoplasia. 2010;12(3):275–83. doi: 10.1593/neo.91880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang Q, Tian Y, Liu S, Zeine R, Chlenski A, Salwen HR, et al. Thrombospondin-1 peptide ABT-510 combined with valproic acid is an effective antiangiogenesis strategy in neuroblastoma. Cancer Res. 2007;67(4):1716–24. doi: 10.1158/0008-5472.CAN-06-2595. [DOI] [PubMed] [Google Scholar]
- 60.Streit M, Riccardi L, Velasco P, Brown LF, Hawighorst T, Bornstein P, et al. Thrombospondin-2: a potent endogenous inhibitor of tumor growth and angiogenesis. Proc Natl Acad Sci U S A. 1999;96(26):14888–93. doi: 10.1073/pnas.96.26.14888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Streit M, Stephen AE, Hawighorst T, Matsuda K, Lange-Asschenfeldt B, Brown LF, et al. Systemic inhibition of tumor growth and angiogenesis by thrombospondin-2 using cell-based antiangiogenic gene therapy. Cancer Res. 2002;62(7):2004–12. [PubMed] [Google Scholar]
- 62.Bornstein P, Armstrong LC, Hankenson KD, Kyriakides TR, Yang Z. Thrombospondin 2, a matricellular protein with diverse functions. Matrix Biol. 2000;19(7):557–68. doi: 10.1016/s0945-053x(00)00104-9. [DOI] [PubMed] [Google Scholar]
- 63.Kyriakides TR, Tam JW, Bornstein P. Accelerated wound healing in mice with a disruption of the thrombospondin 2 gene. J Invest Dermatol. 1999;113(5):782–7. doi: 10.1046/j.1523-1747.1999.00755.x. [DOI] [PubMed] [Google Scholar]
- 64.Kyriakides TR, Leach KJ, Hoffman AS, Ratner BD, Bornstein P. Mice that lack the angiogenesis inhibitor, thrombospondin 2, mount an altered foreign body reaction characterized by increased vascularity. Proc Natl Acad Sci U S A. 1999;96(8):4449–54. doi: 10.1073/pnas.96.8.4449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kyriakides TR, Cheung CY, Murthy N, Bornstein P, Stayton PS, Hoffman AS. pH-sensitive polymers that enhance intracellular drug delivery in vivo. J Control Release. 2002;78(1–3):295–303. doi: 10.1016/s0168-3659(01)00504-1. [DOI] [PubMed] [Google Scholar]
- 66.Kyriakides TR, Hartzel T, Huynh G, Bornstein P. Regulation of angiogenesis and matrix remodeling by localized, matrix-mediated antisense gene delivery. Mol Ther. 2001;3(6):842–9. doi: 10.1006/mthe.2001.0336. [DOI] [PubMed] [Google Scholar]
- 67.Nabzdyk CS, Chun MC, Oliver-Allen HS, Pathan SG, Phaneuf MD, You JO, et al. Gene silencing in human aortic smooth muscle cells induced by PEI-siRNA complexes released from dip-coated electrospun poly(ethylene terephthalate) grafts. Biomaterials. 2014;35(9):3071–9. doi: 10.1016/j.biomaterials.2013.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Subraman V, Thiyagarajan M, Malathi N, Rajan ST. OPN -Revisited. J Clin Diagn Res. 2015;9(6):ZE10–3. doi: 10.7860/JCDR/2015/12872.6111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pagel CN, Wasgewatte Wijesinghe DK, Taghavi Esfandouni N, Mackie EJ. Osteopontin, inflammation and myogenesis: influencing regeneration, fibrosis and size of skeletal muscle. J Cell Commun Signal. 2014;8(2):95–103. doi: 10.1007/s12079-013-0217-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rangaswami H, Bulbule A, Kundu GC. Osteopontin: role in cell signaling and cancer progression. Trends Cell Biol. 2006;16(2):79–87. doi: 10.1016/j.tcb.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 71.Anborgh PH, Mutrie JC, Tuck AB, Chambers AF. Pre- and post-translational regulation of osteopontin in cancer. J Cell Commun Signal. 2011;5(2):111–22. doi: 10.1007/s12079-011-0130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gimba ER, Tilli TM. Human osteopontin splicing isoforms: known roles, potential clinical applications and activated signaling pathways. Cancer Lett. 2013;331(1):11–7. doi: 10.1016/j.canlet.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 73.Ramchandani D, Weber GF. Interactions between osteopontin and vascular endothelial growth factor: Implications for skeletal disorders. Bone. 2015;81:7–15. doi: 10.1016/j.bone.2015.05.047. [DOI] [PubMed] [Google Scholar]
- 74.Ahmed M, Behera R, Chakraborty G, Jain S, Kumar V, Sharma P, et al. Osteopontin: a potentially important therapeutic target in cancer. Expert Opin Ther Targets. 2011;15(9):1113–26. doi: 10.1517/14728222.2011.594438. [DOI] [PubMed] [Google Scholar]
- 75.Bandopadhyay M, Bulbule A, Butti R, Chakraborty G, Ghorpade P, Ghosh P, et al. Osteopontin as a therapeutic target for cancer. Expert Opin Ther Targets. 2014;18(8):883–95. doi: 10.1517/14728222.2014.925447. [DOI] [PubMed] [Google Scholar]
- 76.Zhang F, Luo W, Li Y, Gao S, Lei G. Role of osteopontin in rheumatoid arthritis. Rheumatol Int. 2015;35(4):589–95. doi: 10.1007/s00296-014-3122-z. [DOI] [PubMed] [Google Scholar]
- 77.Housley WJ, Pitt D, Hafler DA. Biomarkers in multiple sclerosis. Clin Immunol. 2015 doi: 10.1016/j.clim.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 78.Braitch M, Constantinescu CS. The role of osteopontin in experimental autoimmune encephalomyelitis (EAE) and multiple sclerosis (MS) Inflamm Allergy Drug Targets. 2010;9(4):249–56. doi: 10.2174/187152810793358778. [DOI] [PubMed] [Google Scholar]
- 79.Wolak T. Osteopontin - a multi-modal marker and mediator in atherosclerotic vascular disease. Atherosclerosis. 2014;236(2):327–37. doi: 10.1016/j.atherosclerosis.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 80.Waller AH, Sanchez-Ross M, Kaluski E, Klapholz M. Osteopontin in cardiovascular disease: a potential therapeutic target. Cardiol Rev. 2010;18(3):125–31. doi: 10.1097/CRD.0b013e3181cfb646. [DOI] [PubMed] [Google Scholar]
- 81.Singhal H, Bautista DS, Tonkin KS, O'Malley FP, Tuck AB, Chambers AF, et al. Elevated plasma osteopontin in metastatic breast cancer associated with increased tumor burden and decreased survival. Clin Cancer Res. 1997;3(4):605–11. [PubMed] [Google Scholar]
- 82.Agrawal D, Chen T, Irby R, Quackenbush J, Chambers AF, Szabo M, et al. Osteopontin identified as lead marker of colon cancer progression, using pooled sample expression profiling. J Natl Cancer Inst. 2002;94(7):513–21. doi: 10.1093/jnci/94.7.513. [DOI] [PubMed] [Google Scholar]
- 83.Thalmann GN, Sikes RA, Devoll RE, Kiefer JA, Markwalder R, Klima I, et al. Osteopontin: possible role in prostate cancer progression. Clin Cancer Res. 1999;5(8):2271–7. [PubMed] [Google Scholar]
- 84.Mutrie JC, Chambers AF, Tuck AB. Osteopontin increases breast cancer cell sensitivity to specific signaling pathway inhibitors in preclinical models. Cancer Biol Ther. 2011;12(8):680–90. doi: 10.4161/cbt.12.8.16440. [DOI] [PubMed] [Google Scholar]
- 85.Hill RP. Targeted treatment: insights from studies of osteopontin and hypoxia. Lancet Oncol. 2005;6(10):733–4. doi: 10.1016/S1470-2045(05)70363-6. [DOI] [PubMed] [Google Scholar]
- 86.Nolen BM, Brand RE, Prosser D, Velikokhatnaya L, Allen PJ, Zeh HJ, et al. Prediagnostic serum biomarkers as early detection tools for pancreatic cancer in a large prospective cohort study. PLoS One. 2014;9(4):e94928. doi: 10.1371/journal.pone.0094928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Weber GF. The metastasis gene osteopontin: a candidate target for cancer therapy. Biochim Biophys Acta. 2001;1552(2):61–85. doi: 10.1016/s0304-419x(01)00037-3. [DOI] [PubMed] [Google Scholar]
- 88.Wai PY, Kuo PC. Osteopontin: regulation in tumor metastasis. Cancer Metastasis Rev. 2008;27(1):103–18. doi: 10.1007/s10555-007-9104-9. [DOI] [PubMed] [Google Scholar]
- 89.Shevde LA, Samant RS. Role of osteopontin in the pathophysiology of cancer. Matrix Biol. 2014;37:131–41. doi: 10.1016/j.matbio.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chakraborty G, Jain S, Kale S, Raja R, Kumar S, Mishra R, et al. Curcumin suppresses breast tumor angiogenesis by abrogating osteopontin-induced VEGF expression. Mol Med Rep. 2008;1(5):641–6. doi: 10.3892/mmr_00000005. [DOI] [PubMed] [Google Scholar]
- 91.Lin F, Cao J, Huang Z, Pei Z, Gu W, Fan S, et al. Effect of thalidomide on the proliferation of hepatoma cells assessed by osteopontin levels in nude mice. Exp Ther Med. 2013;5(5):1403–7. doi: 10.3892/etm.2013.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mentor-Marcel R, Lamartiniere CA, Eltoum IA, Greenberg NM, Elgavish A. Dietary genistein improves survival and reduces expression of osteopontin in the prostate of transgenic mice with prostatic adenocarcinoma (TRAMP) J Nutr. 2005;135(5):989–95. doi: 10.1093/jn/135.5.989. [DOI] [PubMed] [Google Scholar]
- 93.Boissy P, Andersen TL, Abdallah BM, Kassem M, Plesner T, Delaisse JM. Resveratrol inhibits myeloma cell growth, prevents osteoclast formation, and promotes osteoblast differentiation. Cancer Res. 2005;65(21):9943–52. doi: 10.1158/0008-5472.CAN-05-0651. [DOI] [PubMed] [Google Scholar]
- 94.Muramatsu T, Shima K, Ohta K, Kizaki H, Ro Y, Kohno Y, et al. Inhibition of osteopontin expression and function in oral cancer cell lines by antisense oligonucleotides. Cancer Lett. 2005;217(1):87–95. doi: 10.1016/j.canlet.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 95.Du XL, Jiang T, Sheng XG, Gao R, Li QS. Inhibition of osteopontin suppresses in vitro and in vivo angiogenesis in endometrial cancer. Gynecol Oncol. 2009;115(3):371–6. doi: 10.1016/j.ygyno.2009.08.029. [DOI] [PubMed] [Google Scholar]
- 96.Zhang H, Guo M, Chen JH, Wang Z, Du XF, Liu PX, et al. Osteopontin knockdown inhibits alphav,beta3 integrin-induced cell migration and invasion and promotes apoptosis of breast cancer cells by inducing autophagy and inactivating the PI3K/Akt/mTOR pathway. Cell Physiol Biochem. 2014;33(4):991–1002. doi: 10.1159/000358670. [DOI] [PubMed] [Google Scholar]
- 97.Mason CK, McFarlane S, Johnston PG, Crowe P, Erwin PJ, Domostoj MM, et al. Agelastatin A: a novel inhibitor of osteopontin-mediated adhesion, invasion, and colony formation. Mol Cancer Ther. 2008;7(3):548–58. doi: 10.1158/1535-7163.MCT-07-2251. [DOI] [PubMed] [Google Scholar]
- 98.Yu KN, Minai-Tehrani A, Chang SH, Hwang SK, Hong SH, Kim JE, et al. Aerosol delivery of small hairpin osteopontin blocks pulmonary metastasis of breast cancer in mice. PLoS One. 2010;5(12):e15623. doi: 10.1371/journal.pone.0015623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Roderburg C, Benz F, Cardenas DV, Lutz M, Hippe HJ, Luedde T, et al. Persistently elevated osteopontin serum levels predict mortality in critically ill patients. Crit Care. 2015;19:271. doi: 10.1186/s13054-015-0988-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Simao A, Madaleno J, Silva N, Rodrigues F, Caseiro P, Costa JN, et al. Plasma osteopontin is a biomarker for the severity of alcoholic liver cirrhosis, not for hepatocellular carcinoma screening. BMC Gastroenterol. 2015;15(1):73. doi: 10.1186/s12876-015-0307-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Matsue Y, Tsutsumi M, Hayashi N, Saito T, Tsuchishima M, Toshikuni N, et al. Serum osteopontin predicts degree of hepatic fibrosis and serves as a biomarker in patients with hepatitis C virus infection. PLoS One. 2015;10(3):e0118744. doi: 10.1371/journal.pone.0118744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Saito Y, Kon S, Fujiwara Y, Nakayama Y, Kurotaki D, Fukuda N, et al. Osteopontin small interfering RNA protects mice from fulminant hepatitis. Human gene therapy. 2007;18(12):1205–14. doi: 10.1089/hum.2007.069. [DOI] [PubMed] [Google Scholar]
- 103.Maziere C, Gomila C, Maziere JC. Oxidized low-density lipoprotein increases osteopontin expression by generation of oxidative stress. Free Radic Biol Med. 2010;48(10):1382–7. doi: 10.1016/j.freeradbiomed.2010.02.022. [DOI] [PubMed] [Google Scholar]
- 104.Carbone F, Vuilleumier N, Burger F, Roversi G, Tamborino C, Casetta I, et al. Serum osteopontin levels are upregulated and predict disability after an ischaemic stroke. Eur J Clin Invest. 2015;45(6):579–86. doi: 10.1111/eci.12446. [DOI] [PubMed] [Google Scholar]
- 105.Jimenez-Corona AE, Damian-Zamacona S, Perez-Torres A, Moreno A, Mas-Oliva J. Osteopontin upregulation in atherogenesis is associated with cellular oxidative stress triggered by the activation of scavenger receptors. Arch Med Res. 2012;43(2):102–11. doi: 10.1016/j.arcmed.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 106.Wang X, Louden C, Yue TL, Ellison JA, Barone FC, Solleveld HA, et al. Delayed expression of osteopontin after focal stroke in the rat. J Neurosci. 1998;18(6):2075–83. doi: 10.1523/JNEUROSCI.18-06-02075.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mendioroz M, Fernandez-Cadenas I, Rosell A, Delgado P, Domingues-Montanari S, Ribo M, et al. Osteopontin predicts long-term functional outcome among ischemic stroke patients. J Neurol. 2011;258(3):486–93. doi: 10.1007/s00415-010-5785-z. [DOI] [PubMed] [Google Scholar]
- 108.Meller R, Stevens SL, Minami M, Cameron JA, King S, Rosenzweig H, et al. Neuroprotection by osteopontin in stroke. J Cereb Blood Flow Metab. 2005;25(2):217–25. doi: 10.1038/sj.jcbfm.9600022. [DOI] [PubMed] [Google Scholar]
- 109.Doyle KP, Yang T, Lessov NS, Ciesielski TM, Stevens SL, Simon RP, et al. Nasal administration of osteopontin peptide mimetics confers neuroprotection in stroke. J Cereb Blood Flow Metab. 2008;28(6):1235–48. doi: 10.1038/jcbfm.2008.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Joachim E, Kim ID, Jin Y, Kim KK, Lee JK, Choi H. Gelatin nanoparticles enhance the neuroprotective effects of intranasally administered osteopontin in rat ischemic stroke model. Drug delivery and translational research. 2014;4(5–6):395–9. doi: 10.1007/s13346-014-0208-9. [DOI] [PubMed] [Google Scholar]
- 111.Jin Y, Kim IY, Kim ID, Lee HK, Park JY, Han PL, et al. Biodegradable gelatin microspheres enhance the neuroprotective potency of osteopontin via quick and sustained release in the post-ischemic brain. Acta Biomater. 2014;10(7):3126–35. doi: 10.1016/j.actbio.2014.02.045. [DOI] [PubMed] [Google Scholar]
- 112.Giachelli CM, Steitz S. Osteopontin: a versatile regulator of inflammation and biomineralization. Matrix Biol. 2000;19(7):615–22. doi: 10.1016/s0945-053x(00)00108-6. [DOI] [PubMed] [Google Scholar]
- 113.Liu L, Chen G, Chao T, Ratner BD, Sage EH, Jiang S. Reduced foreign body reaction to implanted biomaterials by surface treatment with oriented osteopontin. J Biomater Sci Polym Ed. 2008;19(6):821–35. doi: 10.1163/156856208784522083. [DOI] [PubMed] [Google Scholar]
- 114.Decup F, Six N, Palmier B, Buch D, Lasfargues JJ, Salih E, et al. Bone sialoprotein-induced reparative dentinogenesis in the pulp of rat's molar. Clin Oral Investig. 2000;4(2):110–9. doi: 10.1007/s007840050126. [DOI] [PubMed] [Google Scholar]
- 115.Xu L, Anderson AL, Lu Q, Wang J. Role of fibrillar structure of collagenous carrier in bone sialoprotein-mediated matrix mineralization and osteoblast differentiation. Biomaterials. 2007;28(4):750–61. doi: 10.1016/j.biomaterials.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 116.Yuan Y, Altalhi WA, Ng JJ, Courtman DW. Derivation of human peripheral blood derived endothelial progenitor cells and the role of osteopontin surface modification and eNOS transfection. Biomaterials. 2013;34(30):7292–301. doi: 10.1016/j.biomaterials.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 117.Jensen T, Dolatshahi-Pirouz A, Foss M, Baas J, Lovmand J, Duch M, et al. Interaction of human mesenchymal stem cells with osteopontin coated hydroxyapatite surfaces. Colloids Surf B Biointerfaces. 2010;75(1):186–93. doi: 10.1016/j.colsurfb.2009.08.029. [DOI] [PubMed] [Google Scholar]
- 118.Hamada Y, Yuki K, Okazaki M, Fujitani W, Matsumoto T, Hashida MK, et al. Osteopontin-derived peptide SVVYGLR induces angiogenesis in vivo. Dental materials journal. 2004;23(4):650–5. doi: 10.4012/dmj.23.650. [DOI] [PubMed] [Google Scholar]
- 119.Chiquet-Ehrismann R, Orend G, Chiquet M, Tucker RP, Midwood KS. Tenascins in stem cell niches. Matrix Biol. 2014;37:112–23. doi: 10.1016/j.matbio.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 120.Kasprzycka M, Hammarstrom C, Haraldsen G. Tenascins in fibrotic disorders-from bench to bedside. Cell Adh Migr. 2015;9(1–2):83–9. doi: 10.4161/19336918.2014.994901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jakovcevski I, Miljkovic D, Schachner M, Andjus PR. Tenascins and inflammation in disorders of the nervous system. Amino acids. 2013;44(4):1115–27. doi: 10.1007/s00726-012-1446-0. [DOI] [PubMed] [Google Scholar]
- 122.Tucker RP, Chiquet-Ehrismann R. Tenascin-C: Its functions as an integrin ligand. Int J Biochem Cell Biol. 2015;65:165–8. doi: 10.1016/j.biocel.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 123.Udalova IA, Ruhmann M, Thomson SJ, Midwood KS. Expression and immune function of tenascin-C. Crit Rev Immunol. 2011;31(2):115–45. doi: 10.1615/critrevimmunol.v31.i2.30. [DOI] [PubMed] [Google Scholar]
- 124.Berndt A, Richter P, Kosmehl H, Franz M. Tenascin-C and carcinoma cell invasion in oral and urinary bladder cancer. Cell Adh Migr. 2015;9(1–2):105–11. doi: 10.1080/19336918.2015.1005463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Imanaka-Yoshida K. Tenascin-C in cardiovascular tissue remodeling: from development to inflammation and repair. Circ J. 2012;76(11):2513–20. doi: 10.1253/circj.cj-12-1033. [DOI] [PubMed] [Google Scholar]
- 126.Kong X, Ma W, Li Y, Wang Y, Guan J, Gao J, et al. Does Tenascin have Clinical Implications in Pathological Grade of Glioma Patients?: A Systematic Meta-Analysis. Medicine. 2015;94(32):e1330. doi: 10.1097/MD.0000000000001330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Iyoda T, Fukai F. Modulation of Tumor Cell Survival, Proliferation, and Differentiation by the Peptide Derived from Tenascin-C: Implication of beta1-Integrin Activation. Int J Cell Biol. 2012;2012:647594. doi: 10.1155/2012/647594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Matsumoto K. Vascular Calcification - Pathological Mechanism and Clinical Application - . Extracellular matrix tenascin-X in calcific aortic valves. Clin Calcium. 2015;25(5):701–10. [PubMed] [Google Scholar]
- 129.Anlar B, Gunel-Ozcan A. Tenascin-R: role in the central nervous system. Int J Biochem Cell Biol. 2012;44(9):1385–9. doi: 10.1016/j.biocel.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 130.O'Connell M, Burrows NP, van Vlijmen-Willems MJ, Clark SM, Schalkwijk J. Tenascin-X deficiency and Ehlers-Danlos syndrome: a case report and review of the literature. Br J Dermatol. 2010;163(6):1340–5. doi: 10.1111/j.1365-2133.2010.09949.x. [DOI] [PubMed] [Google Scholar]
- 131.Martina E, Chiquet-Ehrismann R, Brellier F. Tenascin-W: an extracellular matrix protein associated with osteogenesis and cancer. Int J Biochem Cell Biol. 2010;42(9):1412–5. doi: 10.1016/j.biocel.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 132.Midwood KS, Orend G. The role of tenascin-C in tissue injury and tumorigenesis. J Cell Commun Signal. 2009;3(3–4):287–310. doi: 10.1007/s12079-009-0075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Orend G. Potential oncogenic action of tenascin-C in tumorigenesis. Int J Biochem Cell Biol. 2005;37(5):1066–83. doi: 10.1016/j.biocel.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 134.Brellier F, Chiquet-Ehrismann R. How do tenascins influence the birth and life of a malignant cell? J Cell Mol Med. 2012;16(1):32–40. doi: 10.1111/j.1582-4934.2011.01360.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Oskarsson T, Acharyya S, Zhang XH, Vanharanta S, Tavazoie SF, Morris PG, et al. Breast cancer cells produce tenascin C as a metastatic niche component to colonize the lungs. Nat Med. 2011;17(7):867–74. doi: 10.1038/nm.2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Coradini D, Daidone MG. Biomolecular prognostic factors in breast cancer. Curr Opin Obstet Gynecol. 2004;16(1):49–55. doi: 10.1097/00001703-200402000-00010. [DOI] [PubMed] [Google Scholar]
- 137.Takeda A, Otani Y, Iseki H, Takeuchi H, Aikawa K, Tabuchi S, et al. Clinical significance of large tenascin-C spliced variant as a potential biomarker for colorectal cancer. World J Surg. 2007;31(2):388–94. doi: 10.1007/s00268-006-0328-6. [DOI] [PubMed] [Google Scholar]
- 138.Kalinina J, Peng J, Ritchie JC, Van Meir EG. Proteomics of gliomas: initial biomarker discovery and evolution of technology. Neuro Oncol. 2011;13(9):926–42. doi: 10.1093/neuonc/nor078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Iskaros BF, Tanaka KE, Hu X, Kadish AS, Steinberg JJ. Morphologic pattern of tenascin as a diagnostic biomarker in colon cancer. J Surg Oncol. 1997;64(2):98–101. doi: 10.1002/(sici)1096-9098(199702)64:2<98::aid-jso2>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 140.Guan Z, Zeng J, Wang Z, Xie H, Lv C, Ma Z, et al. Urine tenascinC is an independent risk factor for bladder cancer patients. Mol Med Rep. 2014;9(3):961–6. doi: 10.3892/mmr.2013.1873. [DOI] [PubMed] [Google Scholar]
- 141.Balasenthil S, Chen N, Lott ST, Chen J, Carter J, Grizzle WE, et al. A migration signature and plasma biomarker panel for pancreatic adenocarcinoma. Cancer Prev Res (Phila) 2011;4(1):137–49. doi: 10.1158/1940-6207.CAPR-10-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Midwood KS, Hussenet T, Langlois B, Orend G. Advances in tenascin-C biology. Cell Mol Life Sci. 2011;68(19):3175–99. doi: 10.1007/s00018-011-0783-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Herold-Mende C, Mueller MM, Bonsanto MM, Schmitt HP, Kunze S, Steiner HH. Clinical impact and functional aspects of tenascin-C expression during glioma progression. Int J Cancer. 2002;98(3):362–9. doi: 10.1002/ijc.10233. [DOI] [PubMed] [Google Scholar]
- 144.Zukiel R, Nowak S, Wyszko E, Rolle K, Gawronska I, Barciszewska MZ, et al. Suppression of human brain tumor with interference RNA specific for tenascin-C. Cancer Biol Ther. 2006;5(8):1002–7. doi: 10.4161/cbt.5.8.2886. [DOI] [PubMed] [Google Scholar]
- 145.Wyszko E, Rolle K, Nowak S, Zukiel R, Nowak M, Piestrzeniewicz R, et al. A multivariate analysis of patients with brain tumors treated with ATN-RNA. Acta Pol Pharm. 2008;65(6):677–84. [PubMed] [Google Scholar]
- 146.Hicke BJ, Stephens AW, Gould T, Chang YF, Lynott CK, Heil J, et al. Tumor targeting by an aptamer. J Nucl Med. 2006;47(4):668–78. [PubMed] [Google Scholar]
- 147.He X, Archer GE, Wikstrand CJ, Morrison SL, Zalutsky MR, Bigner DD, et al. Generation and characterization of a mouse/human chimeric antibody directed against extracellular matrix protein tenascin. J Neuroimmunol. 1994;52(2):127–37. doi: 10.1016/0165-5728(94)90106-6. [DOI] [PubMed] [Google Scholar]
- 148.Zalutsky MR, Moseley RP, Coakham HB, Coleman RE, Bigner DD. Pharmacokinetics and tumor localization of 131I-labeled anti-tenascin monoclonal antibody 81C6 in patients with gliomas and other intracranial malignancies. Cancer Res. 1989;49(10):2807–13. [PubMed] [Google Scholar]
- 149.Grana CM, Chinol M, De Cicco C, Batolomei M, Cremonesi M, Bodei L, et al. Eleven-year experience with the avidin-biotin pretargeting system in glioblastoma: toxicity, efficacy, and survival. The Open Nuclear Medicine Journal. 2012;4:14–20. [Google Scholar]
- 150.Bigner DD, Brown MT, Friedman AH, Coleman RE, Akabani G, Friedman HS, et al. Iodine-131-labeled antitenascin monoclonal antibody 81C6 treatment of patients with recurrent malignant gliomas: phase I trial results. J Clin Oncol. 1998;16(6):2202–12. doi: 10.1200/JCO.1998.16.6.2202. [DOI] [PubMed] [Google Scholar]
- 151.Cokgor I, Akabani G, Kuan CT, Friedman HS, Friedman AH, Coleman RE, et al. Phase I trial results of iodine-131-labeled antitenascin monoclonal antibody 81C6 treatment of patients with newly diagnosed malignant gliomas. J Clin Oncol. 2000;18(22):3862–72. doi: 10.1200/JCO.2000.18.22.3862. [DOI] [PubMed] [Google Scholar]
- 152.Reardon DA, Quinn JA, Akabani G, Coleman RE, Friedman AH, Friedman HS, et al. Novel human IgG2b/murine chimeric antitenascin monoclonal antibody construct radiolabeled with 131I and administered into the surgically created resection cavity of patients with malignant glioma: phase I trial results. J Nucl Med. 2006;47(6):912–8. [PubMed] [Google Scholar]
- 153.Reardon DA, Akabani G, Coleman RE, Friedman AH, Friedman HS, Herndon JE, 2nd, et al. Salvage radioimmunotherapy with murine iodine-131-labeled antitenascin monoclonal antibody 81C6 for patients with recurrent primary and metastatic malignant brain tumors: phase II study results. J Clin Oncol. 2006;24(1):115–22. doi: 10.1200/JCO.2005.03.4082. [DOI] [PubMed] [Google Scholar]
- 154.Reardon DA, Akabani G, Coleman RE, Friedman AH, Friedman HS, Herndon JE, 2nd, et al. Phase II trial of murine (131)I-labeled antitenascin monoclonal antibody 81C6 administered into surgically created resection cavities of patients with newly diagnosed malignant gliomas. J Clin Oncol. 2002;20(5):1389–97. doi: 10.1200/JCO.2002.20.5.1389. [DOI] [PubMed] [Google Scholar]
- 155.Zalutsky MR, Reardon DA, Akabani G, Coleman RE, Friedman AH, Friedman HS, et al. Clinical experience with alpha-particle emitting 211At: treatment of recurrent brain tumor patients with 211At-labeled chimeric antitenascin monoclonal antibody 81C6. J Nucl Med. 2008;49(1):30–8. doi: 10.2967/jnumed.107.046938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Reardon DA, Zalutsky MR, Bigner DD. Antitenascin-C monoclonal antibody radioimmunotherapy for malignant glioma patients. Expert Rev Anticancer Ther. 2007;7(5):675–87. doi: 10.1586/14737140.7.5.675. [DOI] [PubMed] [Google Scholar]
- 157.Sawyer AJ, Piepmeier JM, Saltzman WM. New methods for direct delivery of chemotherapy for treating brain tumors. The Yale journal of biology and medicine. 2006;79(3–4):141–52. [PMC free article] [PubMed] [Google Scholar]
- 158.Sawyer AJ, Saucier-Sawyer JK, Booth CJ, Liu J, Patel T, Piepmeier JM, et al. Convection-enhanced delivery of camptothecin-loaded polymer nanoparticles for treatment of intracranial tumors. Drug delivery and translational research. 2011;1(1):34–42. doi: 10.1007/s13346-010-0001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tamaoki M, Imanaka-Yoshida K, Yokoyama K, Nishioka T, Inada H, Hiroe M, et al. Tenascin-C regulates recruitment of myofibroblasts during tissue repair after myocardial injury. Am J Pathol. 2005;167(1):71–80. doi: 10.1016/S0002-9440(10)62954-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Nishioka T, Onishi K, Shimojo N, Nagano Y, Matsusaka H, Ikeuchi M, et al. Tenascin-C may aggravate left ventricular remodeling and function after myocardial infarction in mice. Am J Physiol Heart Circ Physiol. 2010;298(3):H1072–8. doi: 10.1152/ajpheart.00255.2009. [DOI] [PubMed] [Google Scholar]
- 161.Aso N, Tamura A, Nasu M. Circulating tenascin-C levels in patients with idiopathic dilated cardiomyopathy. Am J Cardiol. 2004;94(11):1468–70. doi: 10.1016/j.amjcard.2004.07.156. [DOI] [PubMed] [Google Scholar]
- 162.Sato A, Hiroe M, Akiyama D, Hikita H, Nozato T, Hoshi T, et al. Prognostic value of serum tenascin-C levels on long-term outcome after acute myocardial infarction. J Card Fail. 2012;18(6):480–6. doi: 10.1016/j.cardfail.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 163.Kitaoka H, Kubo T, Baba Y, Yamasaki N, Matsumura Y, Furuno T, et al. Serum tenascin-C levels as a prognostic biomarker of heart failure events in patients with hypertrophic cardiomyopathy. J Cardiol. 2012;59(2):209–14. doi: 10.1016/j.jjcc.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 164.Terasaki F, Okamoto H, Onishi K, Sato A, Shimomura H, Tsukada B, et al. Higher serum tenascin-C levels reflect the severity of heart failure, left ventricular dysfunction and remodeling in patients with dilated cardiomyopathy. Circ J. 2007;71(3):327–30. doi: 10.1253/circj.71.327. [DOI] [PubMed] [Google Scholar]
- 165.Sakamoto N, Hoshino Y, Misaka T, Mizukami H, Suzuki S, Sugimoto K, et al. Serum tenascin-C level is associated with coronary plaque rupture in patients with acute coronary syndrome. Heart Vessels. 2014;29(2):165–70. doi: 10.1007/s00380-013-0341-2. [DOI] [PubMed] [Google Scholar]
- 166.Franz M, Berndt A, Neri D, Galler K, Grun K, Porrmann C, et al. Matrix metalloproteinase-9, tissue inhibitor of metalloproteinase-1, B(+) tenascin-C and ED-A(+) fibronectin in dilated cardiomyopathy: potential impact on disease progression and patients' prognosis. Int J Cardiol. 2013;168(6):5344–51. doi: 10.1016/j.ijcard.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 167.Odaka K, Uehara T, Arano Y, Adachi S, Tadokoro H, Yoshida K, et al. Noninvasive detection of cardiac repair after acute myocardial infarction in rats by 111 In Fab fragment of monoclonal antibody specific for tenascin-C. Int Heart J. 2008;49(4):481–92. doi: 10.1536/ihj.49.481. [DOI] [PubMed] [Google Scholar]
- 168.Yamamoto K, Onoda K, Sawada Y, Fujinaga K, Imanaka-Yoshida K, Shimpo H, et al. Tenascin-C is an essential factor for neointimal hyperplasia after aortotomy in mice. Cardiovasc Res. 2005;65(3):737–42. doi: 10.1016/j.cardiores.2004.10.034. [DOI] [PubMed] [Google Scholar]
- 169.Sawada Y, Onoda K, Imanaka-Yoshida K, Maruyama J, Yamamoto K, Yoshida T, et al. Tenascin-C synthesized in both donor grafts and recipients accelerates artery graft stenosis. Cardiovasc Res. 2007;74(3):366–76. doi: 10.1016/j.cardiores.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 170.Cleek RL, Rege AA, Denner LA, Eskin SG, Mikos AG. Inhibition of smooth muscle cell growth in vitro by an antisense oligodeoxynucleotide released from poly(DL-lactic-co-glycolic acid) microparticles. J Biomed Mater Res. 1997;35(4):525–30. doi: 10.1002/(sici)1097-4636(19970615)35:4<525::aid-jbm12>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 171.von Lukowicz T, Silacci M, Wyss MT, Trachsel E, Lohmann C, Buck A, et al. Human antibody against C domain of tenascin-C visualizes murine atherosclerotic plaques ex vivo. J Nucl Med. 2007;48(4):582–7. doi: 10.2967/jnumed.106.036046. [DOI] [PubMed] [Google Scholar]
- 172.Toma N, Imanaka-Yoshida K, Takeuchi T, Matsushima S, Iwata H, Yoshida T, et al. Tenascin-C-coated platinum coils for acceleration of organization of cavities and reduction of lumen size in a rat aneurysm model. J Neurosurg. 2005;103(4):681–6. doi: 10.3171/jns.2005.103.4.0681. [DOI] [PubMed] [Google Scholar]
- 173.Midwood K, Sacre S, Piccinini AM, Inglis J, Trebaul A, Chan E, et al. Tenascin-C is an endogenous activator of Toll-like receptor 4 that is essential for maintaining inflammation in arthritic joint disease. Nat Med. 2009;15(7):774–80. doi: 10.1038/nm.1987. [DOI] [PubMed] [Google Scholar]
- 174.Schwager K, Kaspar M, Bootz F, Marcolongo R, Paresce E, Neri D, et al. Preclinical characterization of DEKAVIL (F8-IL10), a novel clinical-stage immunocytokine which inhibits the progression of collagen-induced arthritis. Arthritis Res Ther. 2009;11(5):R142. doi: 10.1186/ar2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Galeazzi M, Bazzichi L, Sebastiani GD, Neri D, Garcia E, Ravenni N, et al. A phase IB clinical trial with Dekavil (F8-IL10), an immunoregulatory 'armed antibody' for the treatment of rheumatoid arthritis, used in combination wiIh methotrexate. Isr Med Assoc J. 2014;16(10):666. [PubMed] [Google Scholar]
- 176.Xie K, Liu Y, Hao W, Walter S, Penke B, Hartmann T, et al. Tenascin-C deficiency ameliorates Alzheimer's disease-related pathology in mice. Neurobiol Aging. 2013;34(10):2389–98. doi: 10.1016/j.neurobiolaging.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 177.Degen M, Brellier F, Schenk S, Driscoll R, Zaman K, Stupp R, et al. Tenascin-W, a new marker of cancer stroma, is elevated in sera of colon and breast cancer patients. Int J Cancer. 2008;122(11):2454–61. doi: 10.1002/ijc.23417. [DOI] [PubMed] [Google Scholar]
- 178.Leask A, Abraham DJ. All in the CCN family: essential matricellular signaling modulators emerge from the bunker. J Cell Sci. 2006;119(Pt 23):4803–10. doi: 10.1242/jcs.03270. [DOI] [PubMed] [Google Scholar]
- 179.Chen CC, Lau LF. Functions and mechanisms of action of CCN matricellular proteins. Int J Biochem Cell Biol. 2009;41(4):771–83. doi: 10.1016/j.biocel.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Holbourn KP, Acharya KR, Perbal B. The CCN family of proteins: structure-function relationships. Trends Biochem Sci. 2008;33(10):461–73. doi: 10.1016/j.tibs.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Kubota S, Takigawa M. The CCN family acting throughout the body: recent research developments. Biomol Concepts. 2013;4(5):477–94. doi: 10.1515/bmc-2013-0018. [DOI] [PubMed] [Google Scholar]
- 182.Perbal B. CCN proteins: A centralized communication network. J Cell Commun Signal. 2013;7(3):169–77. doi: 10.1007/s12079-013-0193-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Brigstock DR, Goldschmeding R, Katsube KI, Lam SC, Lau LF, Lyons K, et al. Proposal for a unified CCN nomenclature. Mol Pathol. 2003;56(2):127–8. doi: 10.1136/mp.56.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Yeger H, Perbal B. The CCN family of genes: a perspective on CCN biology and therapeutic potential. J Cell Commun Signal. 2007;1(3–4):159–64. doi: 10.1007/s12079-008-0022-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Jun JI, Lau LF. Taking aim at the extracellular matrix: CCN proteins as emerging therapeutic targets. Nat Rev Drug Discov. 2011;10(12):945–63. doi: 10.1038/nrd3599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Bleau AM, Planque N, Perbal B. CCN proteins and cancer: two to tango. Front Biosci. 2005;10:998–1009. doi: 10.2741/1594. [DOI] [PubMed] [Google Scholar]
- 187.Haque I, Mehta S, Majumder M, Dhar K, De A, McGregor D, et al. Cyr61/CCN1 signaling is critical for epithelial-mesenchymal transition and stemness and promotes pancreatic carcinogenesis. Mol Cancer. 2011;10:8. doi: 10.1186/1476-4598-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Menendez JA, Mehmi I, Griggs DW, Lupu R. The angiogenic factor CYR61 in breast cancer: molecular pathology and therapeutic perspectives. Endocr Relat Cancer. 2003;10(2):141–52. doi: 10.1677/erc.0.0100141. [DOI] [PubMed] [Google Scholar]
- 189.Menendez JA, Vellon L, Mehmi I, Teng PK, Griggs DW, Lupu R. A novel CYR61-triggered 'CYR61-alphavbeta3 integrin loop' regulates breast cancer cell survival and chemosensitivity through activation of ERK1/ERK2 MAPK signaling pathway. Oncogene. 2005;24(5):761–79. doi: 10.1038/sj.onc.1208238. [DOI] [PubMed] [Google Scholar]
- 190.Kok SH, Chang HH, Tsai JY, Hung HC, Lin CY, Chiang CP, et al. Expression of Cyr61 (CCN1) in human oral squamous cell carcinoma: An independent marker for poor prognosis. Head Neck. 2010;32(12):1665–73. doi: 10.1002/hed.21381. [DOI] [PubMed] [Google Scholar]
- 191.Ono M, Inkson CA, Sonn R, Kilts TM, de Castro LF, Maeda A, et al. WISP1/CCN4: a potential target for inhibiting prostate cancer growth and spread to bone. PLoS One. 2013;8(8):e71709. doi: 10.1371/journal.pone.0071709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Xiao G, Tang Z, Yuan X, Yuan J, Zhao J, Zhang Z, et al. The expression of Wnt-1 inducible signaling pathway protein-2 in astrocytoma: Correlation between pathological grade and clinical outcome. Oncol Lett. 2015;9(1):235–40. doi: 10.3892/ol.2014.2663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Xie JJ, Xu LY, Wu ZY, Li LY, Xu XE, Wu JY, et al. Expression of cysteine-rich 61 is correlated with poor prognosis in patients with esophageal squamous cell carcinoma. Eur J Surg Oncol. 2011;37(8):669–74. doi: 10.1016/j.ejso.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 194.Bennewith KL, Huang X, Ham CM, Graves EE, Erler JT, Kambham N, et al. The role of tumor cell-derived connective tissue growth factor (CTGF/CCN2) in pancreatic tumor growth. Cancer Res. 2009;69(3):775–84. doi: 10.1158/0008-5472.CAN-08-0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Gery S, Xie D, Yin D, Gabra H, Miller C, Wang H, et al. Ovarian carcinomas: CCN genes are aberrantly expressed and CCN1 promotes proliferation of these cells. Clin Cancer Res. 2005;11(20):7243–54. doi: 10.1158/1078-0432.CCR-05-0231. [DOI] [PubMed] [Google Scholar]
- 196.Sun ZJ, Wang Y, Cai Z, Chen PP, Tong XJ, Xie D. Involvement of Cyr61 in growth, migration, and metastasis of prostate cancer cells. Br J Cancer. 2008;99(10):1656–67. doi: 10.1038/sj.bjc.6604712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Goodwin CR, Lal B, Zhou X, Ho S, Xia S, Taeger A, et al. Cyr61 mediates hepatocyte growth factor-dependent tumor cell growth, migration, and Akt activation. Cancer Res. 2010;70(7):2932–41. doi: 10.1158/0008-5472.CAN-09-3570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Bleau AM, Planque N, Lazar N, Zambelli D, Ori A, Quan T, et al. Antiproliferative activity of CCN3: involvement of the C-terminal module and post-translational regulation. J Cell Biochem. 2007;101(6):1475–91. doi: 10.1002/jcb.21262. [DOI] [PubMed] [Google Scholar]
- 199.Gupta N, Wang H, McLeod TL, Naus CC, Kyurkchiev S, Advani S, et al. Inhibition of glioma cell growth and tumorigenic potential by CCN3 (NOV) Mol Pathol. 2001;54(5):293–9. doi: 10.1136/mp.54.5.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Haque I, Banerjee S, De A, Maity G, Sarkar S, Majumdar M, et al. CCN5/WISP-2 promotes growth arrest of triple-negative breast cancer cells through accumulation and trafficking of p27(Kip1) via Skp2 and FOXO3a regulation. Oncogene. 2015;34(24):3152–63. doi: 10.1038/onc.2014.250. [DOI] [PubMed] [Google Scholar]
- 201.Russo JW, Castellot JJ. CCN5: biology and pathophysiology. J Cell Commun Signal. 2010;4(3):119–30. doi: 10.1007/s12079-010-0098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Kleer CG, Zhang Y, Pan Q, van Golen KL, Wu ZF, Livant D, et al. WISP3 is a novel tumor suppressor gene of inflammatory breast cancer. Oncogene. 2002;21(20):3172–80. doi: 10.1038/sj.onc.1205462. [DOI] [PubMed] [Google Scholar]
- 203.Leask A, Parapuram SK, Shi-Wen X, Abraham DJ. Connective tissue growth factor (CTGF, CCN2) gene regulation: a potent clinical bio-marker of fibroproliferative disease? J Cell Commun Signal. 2009;3(2):89–94. doi: 10.1007/s12079-009-0037-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Dziadzio M, Usinger W, Leask A, Abraham D, Black CM, Denton C, et al. N-terminal connective tissue growth factor is a marker of the fibrotic phenotype in scleroderma. QJM. 2005;98(7):485–92. doi: 10.1093/qjmed/hci078. [DOI] [PubMed] [Google Scholar]
- 205.Jaffa AA, Usinger WR, McHenry MB, Jaffa MA, Lipstiz SR, Lackland D, et al. Connective tissue growth factor and susceptibility to renal and vascular disease risk in type 1 diabetes. J Clin Endocrinol Metab. 2008;93(5):1893–900. doi: 10.1210/jc.2007-2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Nguyen TQ, Tarnow L, Jorsal A, Oliver N, Roestenberg P, Ito Y, et al. Plasma connective tissue growth factor is an independent predictor of end-stage renal disease and mortality in type 1 diabetic nephropathy. Diabetes Care. 2008;31(6):1177–82. doi: 10.2337/dc07-2469. [DOI] [PubMed] [Google Scholar]
- 207.Leask A. CCN2: a bona fide target for anti-fibrotic drug intervention. J Cell Commun Signal. 2011;5(2):131–3. doi: 10.1007/s12079-011-0125-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Brigstock DR. Strategies for blocking the fibrogenic actions of connective tissue growth factor (CCN2): From pharmacological inhibition in vitro to targeted siRNA therapy in vivo. J Cell Commun Signal. 2009;3(1):5–18. doi: 10.1007/s12079-009-0043-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Lang C, Sauter M, Szalay G, Racchi G, Grassi G, Rainaldi G, et al. Connective tissue growth factor: a crucial cytokine-mediating cardiac fibrosis in ongoing enterovirus myocarditis. J Mol Med (Berl) 2008;86(1):49–60. doi: 10.1007/s00109-007-0249-3. [DOI] [PubMed] [Google Scholar]
- 210.Okada H, Kikuta T, Kobayashi T, Inoue T, Kanno Y, Takigawa M, et al. Connective tissue growth factor expressed in tubular epithelium plays a pivotal role in renal fibrogenesis. J Am Soc Nephrol. 2005;16(1):133–43. doi: 10.1681/ASN.2004040339. [DOI] [PubMed] [Google Scholar]
- 211.Luo GH, Lu YP, Song J, Yang L, Shi YJ, Li YP. Inhibition of connective tissue growth factor by small interfering RNA prevents renal fibrosis in rats undergoing chronic allograft nephropathy. Transplant Proc. 2008;40(7):2365–9. doi: 10.1016/j.transproceed.2008.07.100. [DOI] [PubMed] [Google Scholar]
- 212.Yokoi H, Mukoyama M, Nagae T, Mori K, Suganami T, Sawai K, et al. Reduction in connective tissue growth factor by antisense treatment ameliorates renal tubulointerstitial fibrosis. J Am Soc Nephrol. 2004;15(6):1430–40. doi: 10.1097/01.asn.0000130565.69170.85. [DOI] [PubMed] [Google Scholar]
- 213.Guha M, Xu ZG, Tung D, Lanting L, Natarajan R. Specific down-regulation of connective tissue growth factor attenuates progression of nephropathy in mouse models of type 1 and type 2 diabetes. FASEB J. 2007;21(12):3355–68. doi: 10.1096/fj.06-6713com. [DOI] [PubMed] [Google Scholar]
- 214.Phanish MK, Winn SK, Dockrell ME. Connective tissue growth factor-(CTGF, CCN2)--a marker, mediator and therapeutic target for renal fibrosis. Nephron Exp Nephrol. 2010;114(3):e83–92. doi: 10.1159/000262316. [DOI] [PubMed] [Google Scholar]
- 215.Twigg SM. Mastering a mediator: blockade of CCN-2 shows early promise in human diabetic kidney disease. J Cell Commun Signal. 2010;4(4):189–96. doi: 10.1007/s12079-010-0102-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Adler SG, Schwartz S, Williams ME, Arauz-Pacheco C, Bolton WK, Lee T, et al. Phase 1 study of anti-CTGF monoclonal antibody in patients with diabetes and microalbuminuria. Clin J Am Soc Nephrol. 2010;5(8):1420–8. doi: 10.2215/CJN.09321209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Morales MG, Gutierrez J, Cabello-Verrugio C, Cabrera D, Lipson KE, Goldschmeding R, et al. Reducing CTGF/CCN2 slows down mdx muscle dystrophy and improves cell therapy. Hum Mol Genet. 2013;22(24):4938–51. doi: 10.1093/hmg/ddt352. [DOI] [PubMed] [Google Scholar]
- 218.Li S, Huo Y, Tian H, Zhang Q, Lv Y, Hao Z. In vitro selection and characterization of deoxyribonucleic acid aptamers against connective tissue growth factor. Biochem Biophys Res Commun. 2015;457(4):640–6. doi: 10.1016/j.bbrc.2015.01.041. [DOI] [PubMed] [Google Scholar]
- 219.Poller W, Rother M, Skurk C, Scheibenbogen C. Endogenous migration modulators as parent compounds for the development of novel cardiovascular and anti-inflammatory drugs. Br J Pharmacol. 2012;165(7):2044–58. doi: 10.1111/j.1476-5381.2011.01762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Boer U, Spengler C, Jonigk D, Klingenberg M, Schrimpf C, Lutzner S, et al. Coating decellularized equine carotid arteries with CCN1 improves cellular repopulation, local biocompatibility, and immune response in sheep. Tissue Eng Part A. 2013;19(15–16):1829–42. doi: 10.1089/ten.TEA.2012.0558. [DOI] [PubMed] [Google Scholar]
- 221.Roh JD, Sawh-Martinez R, Brennan MP, Jay SM, Devine L, Rao DA, et al. Tissue-engineered vascular grafts transform into mature blood vessels via an inflammation-mediated process of vascular remodeling. Proc Natl Acad Sci U S A. 2010;107(10):4669–74. doi: 10.1073/pnas.0911465107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Rother M, Krohn S, Kania G, Vanhoutte D, Eisenreich A, Wang X, et al. Matricellular signaling molecule CCN1 attenuates experimental autoimmune myocarditis by acting as a novel immune cell migration modulator. Circulation. 2010;122(25):2688–98. doi: 10.1161/CIRCULATIONAHA.110.945261. [DOI] [PubMed] [Google Scholar]
- 223.Bradshaw AD. Diverse biological functions of the SPARC family of proteins. Int J Biochem Cell Biol. 2012;44(3):480–8. doi: 10.1016/j.biocel.2011.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Rivera LB, Bradshaw AD, Brekken RA. The regulatory function of SPARC in vascular biology. Cell Mol Life Sci. 2011;68(19):3165–73. doi: 10.1007/s00018-011-0781-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Wang Z, Hao B, Yang Y, Wang R, Li Y, Wu Q. Prognostic role of SPARC expression in gastric cancer: a meta-analysis. Arch Med Sci. 2014;10(5):863–9. doi: 10.5114/aoms.2014.46207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Neuzillet C, Tijeras-Raballand A, Cros J, Faivre S, Hammel P, Raymond E. Stromal expression of SPARC in pancreatic adenocarcinoma. Cancer Metastasis Rev. 2013;32(3–4):585–602. doi: 10.1007/s10555-013-9439-3. [DOI] [PubMed] [Google Scholar]
- 227.Kaleagasioglu F, Berger MR. SIBLINGs and SPARC families: their emerging roles in pancreatic cancer. World J Gastroenterol. 2014;20(40):14747–59. doi: 10.3748/wjg.v20.i40.14747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Tang L, Feng J. SPARC in Tumor Pathophysiology and as a Potential Therapeutic Target. Curr Pharm Des. 2014 doi: 10.2174/1381612820666140619123255. [DOI] [PubMed] [Google Scholar]
- 229.Wallace DM, Murphy-Ullrich JE, Downs JC, O'Brien CJ. The role of matricellular proteins in glaucoma. Matrix Biol. 2014;37:174–82. doi: 10.1016/j.matbio.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 230.Trombetta-Esilva J, Bradshaw AD. The Function of SPARC as a Mediator of Fibrosis. Open Rheumatol J. 2012;6:146–55. doi: 10.2174/1874312901206010146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Kos K, Wilding JP. SPARC: a key player in the pathologies associated with obesity and diabetes. Nat Rev Endocrinol. 2010;6(4):225–35. doi: 10.1038/nrendo.2010.18. [DOI] [PubMed] [Google Scholar]
- 232.Brekken RA, Sage EH. SPARC, a matricellular protein: at the crossroads of cell-matrix communication. Matrix Biol. 2001;19(8):816–27. doi: 10.1016/s0945-053x(00)00133-5. [DOI] [PubMed] [Google Scholar]
- 233.Rusnati M, Urbinati C, Bonifacio S, Presta M, Taraboletti G. Thrombospondin-1 as a paradigm for the development of antiangiogenic agents endowed with multiple mechanisms of action. Pharmaceuticals. 2010;3:1241–78. doi: 10.3390/ph3041241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Podhajcer OL, Benedetti L, Girotti MR, Prada F, Salvatierra E, Llera AS. The role of the matricellular protein SPARC in the dynamic interaction between the tumor and the host. Cancer Metastasis Rev. 2008;27(3):523–37. doi: 10.1007/s10555-008-9135-x. [DOI] [PubMed] [Google Scholar]
- 235.Vajkoczy P, Menger MD, Goldbrunner R, Ge S, Fong TA, Vollmar B, et al. Targeting angiogenesis inhibits tumor infiltration and expression of the pro-invasive protein SPARC. Int J Cancer. 2000;87(2):261–8. doi: 10.1002/1097-0215(20000715)87:2<261::aid-ijc18>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 236.Rich JN, Hans C, Jones B, Iversen ES, McLendon RE, Rasheed BK, et al. Gene expression profiling and genetic markers in glioblastoma survival. Cancer Res. 2005;65(10):4051–8. doi: 10.1158/0008-5472.CAN-04-3936. [DOI] [PubMed] [Google Scholar]
- 237.Liu H, Xu Y, Chen Y, Zhang H, Fan S, Feng S, et al. RNA interference against SPARC promotes the growth of U-87MG human malignant glioma cells. Oncol Lett. 2011;2(5):985–90. doi: 10.3892/ol.2011.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Hidalgo M, Plaza C, Musteanu M, Illei P, Brachmann CB, Heise C, et al. SPARC Expression Did Not Predict Efficacy of nab-Paclitaxel Plus Gemcitabine or Gemcitabine Alone for Metastatic Pancreatic Cancer in an Exploratory Analysis of the Phase III MPACT Trial. Clin Cancer Res. 2015 doi: 10.1158/1078-0432.CCR-14-3222. [DOI] [PubMed]
- 239.Tai IT, Tang MJ. SPARC in cancer biology: its role in cancer progression and potential for therapy. Drug Resist Updat. 2008;11(6):231–46. doi: 10.1016/j.drup.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 240.Neesse A, Frese KK, Chan DS, Bapiro TE, Howat WJ, Richards FM, et al. SPARC independent drug delivery and antitumour effects of nab-paclitaxel in genetically engineered mice. Gut. 2014;63(6):974–83. doi: 10.1136/gutjnl-2013-305559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Inoue M, Senju S, Hirata S, Ikuta Y, Hayashida Y, Irie A, et al. Identification of SPARC as a candidate target antigen for immunotherapy of various cancers. Int J Cancer. 2010;127(6):1393–403. doi: 10.1002/ijc.25160. [DOI] [PubMed] [Google Scholar]
- 242.Atorrasagasti C, Peixoto E, Aquino JB, Kippes N, Malvicini M, Alaniz L, et al. Lack of the matricellular protein SPARC (secreted protein, acidic and rich in cysteine) attenuates liver fibrogenesis in mice. PLoS One. 2013;8(2):e54962. doi: 10.1371/journal.pone.0054962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Wang JC, Lai S, Guo X, Zhang X, de Crombrugghe B, Sonnylal S, et al. Attenuation of fibrosis in vitro and in vivo with SPARC siRNA. Arthritis Res Ther. 2010;12(2):R60. doi: 10.1186/ar2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Tan YF, Mundargi RC, Chen MH, Lessig J, Neu B, Venkatraman SS, et al. Layer-by-layer nanoparticles as an efficient siRNA delivery vehicle for SPARC silencing. Small. 2014;10(9):1790–8. doi: 10.1002/smll.201303201. [DOI] [PubMed] [Google Scholar]
- 245.Patterson J, Hubbell JA. SPARC-derived protease substrates to enhance the plasmin sensitivity of molecularly engineered PEG hydrogels. Biomaterials. 2011;32(5):1301–10. doi: 10.1016/j.biomaterials.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 246.Liu AY, Zheng H, Ouyang G. Periostin, a multifunctional matricellular protein in inflammatory and tumor microenvironments. Matrix Biol. 2014;37:150–6. doi: 10.1016/j.matbio.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 247.Conway SJ, Izuhara K, Kudo Y, Litvin J, Markwald R, Ouyang G, et al. The role of periostin in tissue remodeling across health and disease. Cell Mol Life Sci. 2014;71(7):1279–88. doi: 10.1007/s00018-013-1494-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Kudo A. Periostin in fibrillogenesis for tissue regeneration: periostin actions inside and outside the cell. Cell Mol Life Sci. 2011;68(19):3201–7. doi: 10.1007/s00018-011-0784-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Hoersch S, Andrade-Navarro MA. Periostin shows increased evolutionary plasticity in its alternatively spliced region. BMC Evol Biol. 2010;10:30. doi: 10.1186/1471-2148-10-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Li W, Gao P, Zhi Y, Xu W, Wu Y, Yin J, et al. Periostin: its role in asthma and its potential as a diagnostic or therapeutic target. Respir Res. 2015;16:57. doi: 10.1186/s12931-015-0218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Boulet LP, Chanez P. Clinically relevant outcome measures for new therapies of asthma using pharmaceutical and biologic agents. Curr Opin Allergy Clin Immunol. 2015;15(3):213–9. doi: 10.1097/ACI.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 252.Yamaguchi Y. Periostin in skin tissue and skin-related diseases. Allergol Int. 2014;63(2):161–70. doi: 10.2332/allergolint.13-RAI-0685. [DOI] [PubMed] [Google Scholar]
- 253.Bible E. Polycystic kidney disease: Periostin is involved in cell proliferation and interstitial fibrosis in polycystic kidney disease. Nat Rev Nephrol. 2014;10(2):66. doi: 10.1038/nrneph.2013.270. [DOI] [PubMed] [Google Scholar]
- 254.Norris RA, Moreno-Rodriguez R, Hoffman S, Markwald RR. The many facets of the matricelluar protein periostin during cardiac development, remodeling, and pathophysiology. J Cell Commun Signal. 2009;3(3–4):275–86. doi: 10.1007/s12079-009-0063-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Jia G, Erickson RW, Choy DF, Mosesova S, Wu LC, Solberg OD, et al. Periostin is a systemic biomarker of eosinophilic airway inflammation in asthmatic patients. J Allergy Clin Immunol. 2012;130(3):647–54. e10. doi: 10.1016/j.jaci.2012.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Parulekar AD, Atik MA, Hanania NA. Periostin, a novel biomarker of TH2-driven asthma. Curr Opin Pulm Med. 2014;20(1):60–5. doi: 10.1097/MCP.0000000000000005. [DOI] [PubMed] [Google Scholar]
- 257.Okamoto M, Hoshino T, Kitasato Y, Sakazaki Y, Kawayama T, Fujimoto K, et al. Periostin, a matrix protein, is a novel biomarker for idiopathic interstitial pneumonias. Eur Respir J. 2011;37(5):1119–27. doi: 10.1183/09031936.00059810. [DOI] [PubMed] [Google Scholar]
- 258.Kudo Y, Siriwardena BS, Hatano H, Ogawa I, Takata T. Periostin: novel diagnostic and therapeutic target for cancer. Histol Histopathol. 2007;22(10):1167–74. doi: 10.14670/HH-22.1167. [DOI] [PubMed] [Google Scholar]
- 259.Liu GX, Xi HQ, Sun XY, Wei B. Role of periostin and its antagonist PNDA-3 in gastric cancer metastasis. World J Gastroenterol. 2015;21(9):2605–13. doi: 10.3748/wjg.v21.i9.2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Mikheev AM, Mikheeva SA, Trister AD, Tokita MJ, Emerson SN, Parada CA, et al. Periostin is a novel therapeutic target that predicts and regulates glioma malignancy. Neuro Oncol. 2015;17(3):372–82. doi: 10.1093/neuonc/nou161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Lee YJ, Kim IS, Park SA, Kim Y, Lee JE, Noh DY, et al. Periostin-binding DNA aptamer inhibits breast cancer growth and metastasis. Mol Ther. 2013;21(5):1004–13. doi: 10.1038/mt.2013.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Han HD, Mangala LS, Lee JW, Shahzad MM, Kim HS, Shen D, et al. Targeted gene silencing using RGD-labeled chitosan nanoparticles. Clin Cancer Res. 2010;16(15):3910–22. doi: 10.1158/1078-0432.CCR-10-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Zhao S, Wu H, Xia W, Chen X, Zhu S, Zhang S, et al. Periostin expression is upregulated and associated with myocardial fibrosis in human failing hearts. J Cardiol. 2014;63(5):373–8. doi: 10.1016/j.jjcc.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 264.Dorn GW., 2nd Periostin and myocardial repair, regeneration, and recovery. N Engl J Med. 2007;357(15):1552–4. doi: 10.1056/NEJMcibr074816. [DOI] [PubMed] [Google Scholar]
- 265.Kuhn B, del Monte F, Hajjar RJ, Chang YS, Lebeche D, Arab S, et al. Periostin induces proliferation of differentiated cardiomyocytes and promotes cardiac repair. Nat Med. 2007;13(8):962–9. doi: 10.1038/nm1619. [DOI] [PubMed] [Google Scholar]
- 266.Polizzotti BD, Arab S, Kuhn B. Intrapericardial delivery of gelfoam enables the targeted delivery of Periostin peptide after myocardial infarction by inducing fibrin clot formation. PLoS One. 2012;7(5):e36788. doi: 10.1371/journal.pone.0036788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Ladage D, Yaniz-Galende E, Rapti K, Ishikawa K, Tilemann L, Shapiro S, et al. Stimulating myocardial regeneration with periostin Peptide in large mammals improves function post-myocardial infarction but increases myocardial fibrosis. PLoS One. 2013;8(5):e59656. doi: 10.1371/journal.pone.0059656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Yuelling LM, Fuss B. Autotaxin (ATX): a multi-functional and multi-modular protein possessing enzymatic lysoPLD activity and matricellular properties. Biochimica et biophysica acta. 2008;1781(9):525–30. doi: 10.1016/j.bbalip.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Tang X, Benesch MG, Brindley DN. Lipid phosphate phosphatases and their roles in mammalian physiology and pathology. J Lipid Res. 2015 doi: 10.1194/jlr.R058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Barbayianni E, Kaffe E, Aidinis V, Kokotos G. Autotaxin, a secreted lysophospholipase D, as a promising therapeutic target in chronic inflammation and cancer. Prog Lipid Res. 2015;58:76–96. doi: 10.1016/j.plipres.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 271.Federico L, Jeong KJ, Vellano CP, Mills GB. Autotaxin, a lysophospholipase D with pleomorphic effects in oncogenesis and cancer progression. J Lipid Res. 2015 doi: 10.1194/jlr.R060020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Benesch MG, Ko YM, McMullen TP, Brindley DN. Autotaxin in the crosshairs: taking aim at cancer and other inflammatory conditions. FEBS Lett. 2014;588(16):2712–27. doi: 10.1016/j.febslet.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 273.Leblanc R, Peyruchaud O. New insights into the autotaxin/LPA axis in cancer development and metastasis. Exp Cell Res. 2015;333(2):183–9. doi: 10.1016/j.yexcr.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 274.Teo K, Brunton VG. The role and therapeutic potential of the autotaxin-lysophosphatidate signalling axis in breast cancer. Biochem J. 2014;463(1):157–65. doi: 10.1042/BJ20140680. [DOI] [PubMed] [Google Scholar]
- 275.Ikeda H, Yatomi Y. Autotaxin in liver fibrosis. Clin Chim Acta. 2012;413(23–24):1817–21. doi: 10.1016/j.cca.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 276.Oikonomou N, Mouratis MA, Tzouvelekis A, Kaffe E, Valavanis C, Vilaras G, et al. Pulmonary autotaxin expression contributes to the pathogenesis of pulmonary fibrosis. Am J Respir Cell Mol Biol. 2012;47(5):566–74. doi: 10.1165/rcmb.2012-0004OC. [DOI] [PubMed] [Google Scholar]
- 277.Pleli T, Martin D, Kronenberger B, Brunner F, Koberle V, Grammatikos G, et al. Serum autotaxin is a parameter for the severity of liver cirrhosis and overall survival in patients with liver cirrhosis--a prospective cohort study. PLoS One. 2014;9(7):e103532. doi: 10.1371/journal.pone.0103532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Tager AM. Autotaxin emerges as a therapeutic target for idiopathic pulmonary fibrosis: limiting fibrosis by limiting lysophosphatidic acid synthesis. Am J Respir Cell Mol Biol. 2012;47(5):563–5. doi: 10.1165/rcmb.2012-0235ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Katsamakas S, Bermperoglou E, Hadjipavlou-Litina D. Considering autotaxin inhibitors in terms of 2D-QSAR and 3D-mapping- review and evaluation. Curr Med Chem. 2015;22(12):1428–61. doi: 10.2174/0929867322666150227154253. [DOI] [PubMed] [Google Scholar]
- 280.de Lau WB, Snel B, Clevers HC. The R-spondin protein family. Genome Biol. 2012;13(3):242. doi: 10.1186/gb-2012-13-3-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Knight MN, Hankenson KD. R-spondins: novel matricellular regulators of the skeleton. Matrix Biol. 2014;37:157–61. doi: 10.1016/j.matbio.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 282.Craword SE, Fitchev P, Veliceasa D, Volpert OV. The many facets of PEDF in drug discovery and disease: a diamond in the rough or split personality disorder? Expert Opin Drug Discov. 2013;8(7):769–92. doi: 10.1517/17460441.2013.794781. [DOI] [PubMed] [Google Scholar]
- 283.Cutler P, Akuffo EL, Bodnar WM, Briggs DM, Davis JB, Debouck CM, et al. Proteomic identification and early validation of complement 1 inhibitor and pigment epithelium-derived factor: Two novel biomarkers of Alzheimer's disease in human plasma. Proteomics Clin Appl. 2008;2(4):467–77. doi: 10.1002/prca.200780101. [DOI] [PubMed] [Google Scholar]
- 284.Thadani U, Latif F. Pigment epithelial-derived factor and acute coronary syndrome: a novel protective biomarker but not for routine clinical use at present. Cardiology. 2014;127(1):28–30. doi: 10.1159/000355453. [DOI] [PubMed] [Google Scholar]
- 285.Broadhead ML, Akiyama T, Choong PF, Dass CR. The pathophysiological role of PEDF in bone diseases. Curr Mol Med. 2010;10(3):296–301. doi: 10.2174/156652410791065345. [DOI] [PubMed] [Google Scholar]
- 286.Manalo KB, Choong PF, Dass CR. Pigment epithelium-derived factor as an impending therapeutic agent against vascular epithelial growth factor-driven tumor-angiogenesis. Mol Carcinog. 2011;50(2):67–72. doi: 10.1002/mc.20711. [DOI] [PubMed] [Google Scholar]
- 287.Han J, Guo J. Current Evidence and Potential Mechanisms of Therapeutic Action of PEDF in Cervical Cancer Treatment. Curr Mol Med. 2015;15(5):446–55. doi: 10.2174/1566524015666150630124447. [DOI] [PubMed] [Google Scholar]
- 288.He X, Cheng R, Benyajati S, Ma JX. PEDF and its roles in physiological and pathological conditions: implication in diabetic and hypoxia-induced angiogenic diseases. Clin Sci (Lond) 2015;128(11):805–23. doi: 10.1042/CS20130463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Yanagisawa H, Schluterman MK, Brekken RA. Fibulin-5, an integrin-binding matricellular protein: its function in development and disease. J Cell Commun Signal. 2009;3(3–4):337–47. doi: 10.1007/s12079-009-0065-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Tang JC, Xie AY, Cai XJ. Diverse functions of fibulin-5 in tumors. Mol Biol (Mosk) 2014;48(6):875–80. doi: 10.7868/s0026898414060172. [DOI] [PubMed] [Google Scholar]
- 291.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 292.Pickup MW, Mouw JK, Weaver VM. The extracellular matrix modulates the hallmarks of cancer. EMBO Rep. 2014;15(12):1243–53. doi: 10.15252/embr.201439246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Suh EJ, Kabir MH, Kang UB, Lee JW, Yu J, Noh DY, et al. Comparative profiling of plasma proteome from breast cancer patients reveals thrombospondin-1 and BRWD3 as serological biomarkers. Exp Mol Med. 2012;44(1):36–44. doi: 10.3858/emm.2012.44.1.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Jayachandran A, Anaka M, Prithviraj P, Hudson C, McKeown SJ, Lo PH, et al. Thrombospondin 1 promotes an aggressive phenotype through epithelial-to-mesenchymal transition in human melanoma. Oncotarget. 2014;5(14):5782–97. doi: 10.18632/oncotarget.2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Chong HC, Tan CK, Huang RL, Tan NS. Matricellular proteins: a sticky affair with cancers. J Oncol. 2012;2012:351089. doi: 10.1155/2012/351089. [DOI] [PMC free article] [PubMed] [Google Scholar]


