Abstract
BACKGROUND
Childhood asthma prevalence doubled from 1980 to 1995 and then increased more slowly from 2001 to 2010. During this second period, racial disparities increased. More recent trends remain to be described.
METHODS
We analyzed current asthma prevalence using 2001–2013 National Health Interview Survey data for children ages 0 to 17 years. Logistic regression with quadratic terms was used to test for nonlinear patterns in trends. Differences between demographic subgroups were further assessed with multivariate models controlling for gender, age, poverty status, race/ethnicity, urbanicity, and geographic region.
RESULTS
Overall, childhood asthma prevalence increased from 2001 to 2009 followed by a plateau then a decline in 2013. From 2001 to 2013, multivariate logistic regression showed no change in prevalence among non-Hispanic white and Puerto Rican children and those in the Northeast and West; increasing prevalence among 10- to 17-year-olds, poor children, and those living in the South; increasing then plateauing prevalence among 5- to 9-year-olds, near-poor children, and non-Hispanic black children; and increasing then decreasing prevalence among 0- to 4-year-olds, nonpoor, and Mexican children and those in the Midwest. Non-Hispanic black-white disparities stopped increasing, and Puerto Rican children remained with the highest prevalence.
CONCLUSIONS
Current asthma prevalence ceased to increase among children in recent years and the non-Hispanic black-white disparity stopped increasing due mainly to plateauing prevalence among non-Hispanic black children.
Beginning with the recognition of the increase in asthma prevalence from the early 1980s, a pattern often called the “asthma epidemic,” asthma has become a primary public health concern.1 Among children <18 years of age, asthma period prevalence (defined as having asthma in the past 12 months) doubled from 3.6% in 1980 to 7.5% in 1995.2,3 The national survey methodology changed after 1997, and although an overall estimate of asthma prevalence was not available from 1997 to 2000, analyses suggested that asthma prevalence remained level during that period.4 The new measure of current asthma prevalence available beginning in 2001 (defined as having asthma at the time of the health survey) initially showed a plateauing trend from 2001 to 2004.2 However, subsequent analysis showed a continued but slower increase in childhood asthma prevalence from 8.7% in 2001 to 9.3% in 2010.5 Over the entire period, the disparity in asthma prevalence between black and white children increased from no or little disparity in the 1980s to a twofold higher prevalence among black compared with white children by 2010.3,6 That is, whereas racial disparities in adverse asthma outcomes such as hospitalizations and death have been present since the 1980s, racial disparities in prevalence have only more recently emerged.7
These trends are concerning because a higher proportion of the pediatric population is at risk of adverse asthma outcomes, and widening prevalence disparities indicate that minority pediatric populations have a disproportionately high risk. Effective primary prevention strategies have not been widely developed due to the limited understanding of the etiology of asthma.8–10 Development of primary prevention strategies as well as guidance on how to target secondary prevention strategies to prevent adverse outcomes may be enhanced by an improved understanding of the epidemiology of asthma. This study was designed to augment a recent study of childhood asthma trends from 2001 to 2010, which analyzed disparities in asthma prevalence and outcomes between black and white children.6 The current study focuses specifically on recent asthma prevalence trends by using nationally representative data from the National Center for Health Statistics (NCHS) and analyzes subgroup differences in the pediatric population by factors known to be associated with having asthma.
METHODS
Current asthma prevalence estimates were calculated by using National Health Interview Survey (NHIS) data. The NHIS is a face-to-face household survey that uses a multistage, clustered sample to obtain nationally representative estimates for the noninstitutionalized US civilian population.11 In each sampled household, if any children were present, a responsible adult served as a proxy respondent for a randomly chosen sample child. Data from 2001 through 2013, a time period for which there was a consistent survey-based definition of asthma prevalence, were analyzed for the main study. Final response rates for sample children aged 0 to 17 years ranged from 70% to 81% for the included survey years. Records for 152 387 sample children were included in the analysis. Data on current asthma prevalence from 2001 through 2013 were based on affirmative responses to both of the following 2 questions: “Has a doctor or other health professional ever told you that your child had asthma?” and “Does your child still have asthma?” To provide historical perspective, 1982–1996 prevalence estimates were also calculated. However, the prevalence measure from this time period (asthma period prevalence) is not directly comparable to the 2001–2013 measure and was based on a single survey question: “During the past 12 months, did anyone in the family have asthma?” For the analysis of 1982–2013 trends, prevalence was assessed by race only (survey methodology for data on Hispanic origin differed after 1997).12 We used 1982 as the initial year because this was the first year in which race was collected for all household members.12 For overall trends, the average percentage point per year of change was calculated with Joinpoint software (National Cancer Institute, Bethesda, MD) by using unadjusted linear regression.13
We assessed asthma prevalence for each of several demographic characteristics shown in previous studies to be related to asthma status1,14,15 including: gender, age group (0–4, 5–9, and 10–17 years of age), race/ethnic group (6 mutually exclusive categories including non-Hispanic white, non-Hispanic black, other non-Hispanic [including Asian and American Indian/Alaska Native], Mexican American, Puerto Rican, and other Hispanic), family structure (single parent/adult or >1 parent/adult in the household), poverty status (ratio of family income to the federal poverty level [FPL]: family income <100% of the FPL hereafter called “poor,” 100% to <200% of the FPL hereafter called “near poor,” and ≥200% of the FPL hereafter called “nonpoor”), urbanicity (residence in an area characterized as large central, large fringe, medium, small, or micropolitan/rural),16 and geographic region of residence (Northeast, Midwest, South, or West). For simplicity of presentation, estimates for other non-Hispanic and other Hispanic groups are included only in Supplemental Material.
Missing responses for current asthma status ranged from 0.1% to 0.4% from 2001 to 2013; these records were excluded. Missing responses for race/ethnicity (<1%) were imputed by NCHS to one of the Office of Management and Budget race groups by the hot-deck method.11 Family income in the NHIS was missing for 20.5% of the eligible sample. We used NCHS-provided multiply-imputed poverty status values according to the recommended methodology.17
Prevalence Estimates and Overall Trend
We used NHIS survey weights to calculate national prevalence estimates and survey design variables to account for the clustered sample when estimating variance with SUDAAN software (RTI International, Research Triangle Park, NC).18 The difference between annual prevalence estimates was assessed with a 2-sided significance test (z test) at the .05 level. The overall trend from 2001 to 2013 was assessed with a bivariate logistic model with year as the independent variable and asthma status as the dependent variable. To assess nonlinear trends, the model also included a quadratic term for year.
Unadjusted and Adjusted Trends by Subgroup
We used logistic regression to assess overall and subgroup-specific trends. We sequentially tested the interaction between each demographic characteristic and the linear and quadratic terms for time. If the interaction terms were significant based on an F test (P < .05), we concluded that trends in asthma prevalence varied between subgroups of that characteristic. The demographic characteristics with significant interactions with linear and quadratic time terms were included in a final, fully adjusted model controlling for the remaining demographic characteristics. Orthogonal polynomial contrasts were conducted to confirm the presence of significant linear or quadratic trends for each subgroup (P < .05). To show trends in more detail, we used modeled predicted margins to plot adjusted current asthma prevalence. We also estimated the predicted linear slope at each year to more clearly demonstrate when asthma prevalence was significantly increasing or decreasing.
RESULTS
Current asthma prevalence among children aged 0 to 17 years increased from 2001 to 2008, as previously reported.6 Analysis of more recent data shows that after 2008, trends plateaued and then declined significantly in 2013 (Fig 1). The estimated prevalence in 2013 (8.3%; SE: 0.3%) was significantly lower than in 2012 (9.3%; SE: 0.3%) (P < .05). Overall, this pattern suggests that childhood asthma prevalence has recently plateaued. Figure 2 presents a historical perspective of asthma prevalence trends. From 1982 to 1996, asthma period prevalence (the percentage of children who had asthma in the past 12 months) increased from 4.0% to 6.3%, with an average annual increase of 0.2 percentage points per year (P < .05). The increase in current asthma prevalence (the percentage of children who had asthma at the time of the survey) from 2001 (8.7%) to a peak in 2009 (9.7%) was more gradual, with an average increase of 0.1 percentage points per year during that period (P < .05). Racial disparities in asthma prevalence recently emerged, with no or little disparity before 1996 and widening disparities after 2001. These disparities appear to have stopped increasing after 2009.
FIGURE 1.
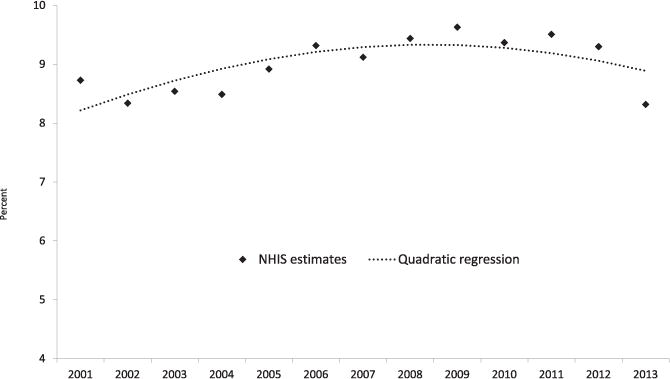
Current asthma prevalence and modeled trend, children aged 0 to 17 years: United States, 2001–2013. The dotted line shows logistic regression with linear and quadratic terms for time with peak modeled prevalence at 2008. Source: CDC/NCHS, NHIS.
FIGURE 2.
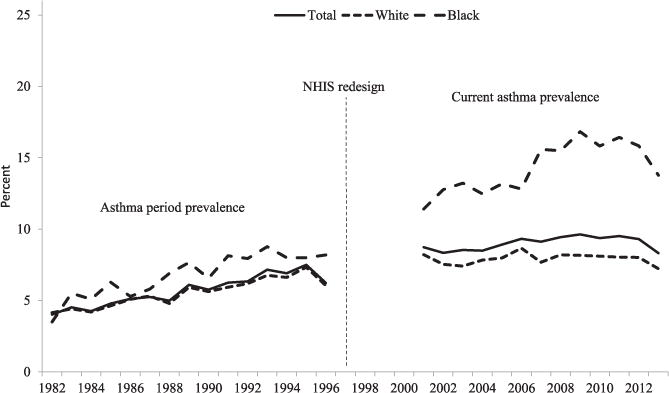
Trend in asthma prevalence by race: United States, 1982–2013. White and black races were analyzed without regard to Hispanic ethnicity to allow greater comparability of estimates across the entire time period. Asthma period prevalence estimates (1982–1996) are not directly comparable to current asthma prevalence estimates (2001–2013) due to different survey questions and methodology. Source: CDC/NCHS, NHIS.
Temporal patterns by additional demographic characteristics were further explored for the more recent period 2001–2013 for which a consistent definition of asthma prevalence is available. Four characteristics had significant interactions with time: age group, poverty status, race/ethnicity, and geographic region. Adjusted and unadjusted results were similar (see Supplemental Figure 4); therefore, adjusted results are presented. By age group (Fig 3A, Supplemental Table 1), adjusted multivariate models showed a significant linear increasing trend for 10- to 17-year-olds and significant quadratic trends for children aged 0 to 4 and 5 to 9 years. Annual linear slopes are shown in Supplemental Table 2 and give greater detail for patterns of trends by age. Children aged 0 to 4 years and 5 to 9 years had increasing asthma prevalence in the beginning of the study period. Although modeled asthma prevalence then decreased significantly at the end of the period among 0- to 4-year-olds, prevalence among 5- to 9-year-olds plateaued after the initial increase. In contrast to these younger age groups, the modeled trend among 10- to 17-year-olds increased during the middle of the period and reached a maximum value at the end of the period. Modeled current asthma prevalence was similar between 5- to 9-year-olds and 10- to 17-year-olds and was lowest in 0- to 4-year-olds.
FIGURE 3.
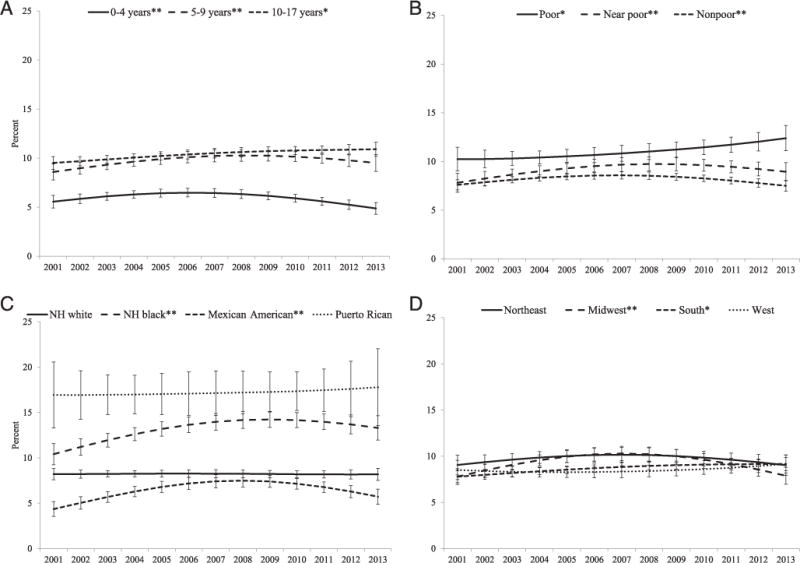
Adjusted predicted margins of current asthma prevalence among 0- to 17-year-olds by age group (A), poverty status (B), race/ethnicity (C), and geographic region (D): United States, 2001–2013. Predicted margins are adjusted for gender, age group, poverty status, race/ethnicity, family structure, urbanicity, geographic region of residence, and 4 interactions (between time [linear and quadratic time in years] and each of 4 groups: age group, poverty status, race/ethnicity, and geographic region). *Significant linear trend by orthogonal polynomial contrast F test, P < .05. **Significant quadratic trend by orthogonal polynomial contrast F test, P < .05. Source: CDC/NCHS, NHIS. NH, non-Hispanic.
By poverty status (Fig 3B, Supplemental Table 1), a significantly increasing linear trend was found for poor children and there was a significant quadratic trend for near-poor and nonpoor children. In particular, annual linear slopes (Supplemental Table 2) show an increasing trend among poor children during the middle of the period. Among children in the near-poor group, current asthma prevalence increased at the beginning of the period but did not change significantly thereafter. Current asthma prevalence also increased among nonpoor children in the beginning of the time period and then declined at the end of the period.
By race/ethnicity (Fig 3C, Supplemental Table 1), there was no significant trend for non-Hispanic white or Puerto Rican children, whereas a significant quadratic trend was observed for non-Hispanic black and Mexican-American children. Annual linear slopes (Supplemental Table 2) show greater detail by year. Current asthma prevalence increased for non-Hispanic black children in first half of the period with no significant change thereafter. Asthma prevalence among Mexican-American children also initially increased but was followed by decreasing prevalence at the end of the period. Prevalence remained highest in Puerto Rican children throughout the period. Non-Hispanic black children had the second highest prevalence, followed by non-Hispanic white and Mexican children. The disparity in asthma prevalence between non-Hispanic black and white children with the use of actual survey estimates (versus modeled estimates) was highest in 2011, with a prevalence ratio of 2.1 (95% confidence interval [CI]: 1.7–2.4); in 2013, the rate ratio was 1.8 (95% CI: 1.5–2.1). The lowest disparity for the period occurred in 2001, with a rate ratio of 1.3 (95% CI: 1.1–1.6).
By geographic region, children residing in the Northeast and West showed no significant trend in asthma prevalence, whereas an increasing linear trend was observed for children living in the South and a quadratic trend was observed for children living in the Midwest (Fig 3D, Supplemental Table 1). Annual linear slopes (Supplemental Table 2) show that in the Midwest, asthma prevalence initially increased and then declined. Prevalence in the South increased significantly during the middle of the period. Compared with differences between subgroups for other demographic characteristics, prevalence levels between geographic areas were similar.
DISCUSSION
Past analyses showed that asthma prevalence increased from 2001 through 20106 after appearing to plateau briefly in the beginning of the decade.2 The results of this study show that these increases did not continue into the next decade. Asthma prevalence reached a maximum in 2009 and subsequent patterns through 2013 are difficult to interpret with certainty. Additional years of data are needed to determine whether asthma prevalence has plateaued or will continue to decline.
Results of this analysis also indicate that differences in asthma prevalence trends exist between sociodemographic subgroups.
There were some groups for whom modeled trends in asthma increased (10- to 17-year-old children, poor children, and those living in the South), others with an increase in prevalence followed by an apparent plateau (5- to 9-year-old children, near-poor children, and non-Hispanic black children), those with increasing then declining prevalence (0- to 4-year-old children, nonpoor children, Mexican children, and those residing in the Midwest), and groups for whom prevalence remained level (non-Hispanic white and Puerto Rican children and those living in the Northeast and West).
The NHIS does not include clinical data or environmental exposure measures. Thus, these cross-sectional data cannot pinpoint underlying factors driving changes in prevalence. Research on the causes of asthma commonly focus on individual risk factors for the development of asthma with smaller clinical studies rather than population-level data.19 However, many theories have been forwarded to explain population-based patterns. Earlier during the “asthma epidemic,” diagnostic transfer from other respiratory conditions was believed to contribute to increasing trends7: improved identification of asthma may have been driven by the recognition of the role of inflammation and more effective preventive treatment.20 Other theories include the hygiene hypothesis (reduced exposure to microbes and parasites early in life leads to increased reactivity to environmental allergens), increased sensitization to indoor allergens (tighter housing with increased time spent indoors), changes in lung-specific protective effects (changing diet and quality of the food supply, changes in micronutrient levels such as vitamin D, decreasing physical activity, increased rate of preterm birth), and changes in immunity-environment interaction (antibiotics and antiseptics alter microbiomes; antiinflammatory medications alter immune responses), among others.21–25 There is general consensus that no single explanation is likely to suffice and that the story of changing asthma prevalence is one of interplay between complex factors.22 The recent plateau of asthma prevalence has not been widely contemplated, but similar plateauing trends have been noted in international studies.21 One speculation could be that a population “reservoir” of asthma susceptibility was exposed through lifestyle and environmental changes over the past several decades, but that it is finite and is now reaching capacity.21 Similarly, other trends that may have driven increasing prevalence (obesity prevalence, diagnostic transfer) may have also recently leveled off.26 This analysis of NHIS data cannot answer the question of why trends change but does provide a comprehensive national picture and some insight into the complexity of asthma prevalence.
One notable pattern is the halt in increasing prevalence among non-Hispanic black children that translated into a halt in the increasing black-white disparity in asthma prevalence. Black children were not always at higher risk of having asthma.6 During the early 1980s to the mid-1990s, asthma prevalence was similar among black and white children. A black-white disparity in asthma prevalence emerged with the new measure of asthma prevalence in 2001, increasing from 40% higher relative disparity in 2001 to 100% in 2010; this increasing disparity was entirely due to increasing prevalence among black children.6 The latest NHIS data suggest that the growth of the racial disparity between non-Hispanic black and non-Hispanic white children in asthma prevalence may have paused.
Plateauing prevalence trends among non-Hispanic black children may have implications for disparities in asthma outcomes. Prevalence disparities are 1 factor that drive “downstream” disparities in adverse asthma outcomes because subgroups with a high prevalence have disproportionate opportunity to suffer asthma exacerbations. A recent change in asthma prevalence trends among non-Hispanic black children may portend future improvements in racial disparities in adverse asthma outcomes. Similarly, rates of some adverse asthma outcomes (emergency department visits and hospitalizations) have also been higher among younger compared with older children.5,7 A changing trend in asthma prevalence among 0- to 4-year-olds and 5- to 9-year-olds may also have a positive impact on the number of children in these age groups who experience asthma-related health care visits and associated costs.
Of note is the diagnostic uncertainty among very young children in whom wheezing is more likely to be associated with lower respiratory tract infection, and to be transient.27 It is unknown if changes in reported prevalence among the 0- to 4-year-old age group are related to greater reluctance to make a diagnosis of asthma among these youngest children and, if so, to what extent the observed trends reflect changes in diagnostic practices versus actual changes in prevalence. The possible influence of factors other than underlying true asthma prevalence, however, has been present throughout the observed trends obtained using NHIS data.
Analyzing trends among different subgroups of children also highlights that socioeconomic status should be disentangled from race/ethnicity when possible. Both unadjusted and adjusted trends showed a change in trend among non-Hispanic black children but not among poor children. Often, the 2 characteristics are treated as synonymous, but they certainly may not be interchangeable markers of risk; this point is relevant to the search for effective primary asthma prevention interventions. Although the data available in NHIS cannot pinpoint why trends differ between subgroups, we could speculate that poverty may be a marker for environmental exposures related to developing asthma.
In addition to the small number of years available to assess a change in trend late in the analyzed period, there are other limitations to this analysis. First, it is possible that survey-related factors have contributed to the observed decline in 2013 estimates. The 2013 NHIS included an asthma supplement with additional questions for participants reporting that their children had current asthma. However, similar supplements were conducted in the 2002, 2003, and 2008 NHIS without observed impact on prevalence estimates. NHIS data are based on proxy report. It is not known how well prevalence estimates correlate with information available in medical records. Finally, there are known etiologic contributors to asthma prevalence that we were not able to assess (eg, prenatal smoking exposure). Differential exposures and other residual confounders may contribute to differential subgroup trends over the study period.
In summary, childhood asthma prevalence has recently stopped increasing. However, additional years of data will be necessary to more definitively discern if increasing trends have ceased or reversed.
Supplementary Material
WHAT’S KNOWN ON THIS SUBJECT
Asthma prevalence among children increased from 1980 to the mid-1990s and then more slowly from 2001 to 2010. Racial disparities in asthma prevalence were small to nonexistent through the 1990s, then increased after 2001.
WHAT THIS STUDY ADDS
Trends in overall childhood asthma prevalence have recently ceased to increase, although trends varied by subgroups. Adjusted prevalence among poor children continued to increase. Racial disparities stopped increasing due to plateauing prevalence among non-Hispanic black children.
Acknowledgments
FUNDING: No external funding.
ABBREVIATIONS
- CI
confidence interval
- FPL
federal poverty level
- NCHS
National Center for Health Statistics
- NHIS
National Health Interview Survey
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006;355(21):2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- 2.Moorman JE, Rudd RA, Johnson CA, et al. Centers for Disease Control and Prevention National surveillance for asthma—United States, 1980–2004. MMWR Surveill Summ. 2007;56(8):1–54. [PubMed] [Google Scholar]
- 3.Division of Health Interview Statistics. National Health Interview Survey. Hyattsville, MD: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 4.Akinbami LJ, Schoendorf KC, Parker J. US childhood asthma prevalence estimates: the impact of the 1997 National Health Interview Survey redesign. Am J Epidemiol. 2003;158(2):99–104. doi: 10.1093/aje/kwg109. [DOI] [PubMed] [Google Scholar]
- 5.Moorman JE, Akinbami LJ, Bailey CM, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat. 2012;3(35):1–67. [PubMed] [Google Scholar]
- 6.Akinbami LJ, Moorman JE, Simon AE, Schoendorf KC. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001–2010. J Allergy Clin Immunol. 2014;134(3):547–553. e545. doi: 10.1016/j.jaci.2014.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics. 2002;110(2 pt 1):315–322. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- 8.President’s Task Force on Environmental Health Risks and Safety Risks to Children Coordinated Federal Action Plan To Reduce Racial and Ethnic Asthma Disparities. Washington, DC: Environmental Protection Agency; 2012. [Google Scholar]
- 9.Bisgaard H, Bonnelykke K. Long-term studies of the natural history of asthma in childhood. J Allergy Clin Immunol. 2010;126(2):187–197. doi: 10.1016/j.jaci.2010.07.011. quiz 198–189. [DOI] [PubMed] [Google Scholar]
- 10.Jackson DJ, Hartert TV, Martinez FD, Weiss ST, Fahy JV. Asthma: NHLBI Workshop on the Primary Prevention of Chronic Lung Diseases. Ann Am Thorac Soc. 2014;11(suppl 3):S139–S145. doi: 10.1513/AnnalsATS.201312-448LD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Division of Health Interview Statistics. 2013 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: National Center for Health Statistics; 2014. [Google Scholar]
- 12.National Center for Health Statistics. NHIS—race and Hispanic origin information: historical context. Published 2010. Updated May 14, 2010. Available at: www.cdc.gov/nchs/nhis/rhoi/rhoi_history.htm. Accessed August 24, 2015.
- 13.National Cancer Institute. Joinpoint Regression Program. Bethesda, MD: National Institutes of Health; 2010. [Google Scholar]
- 14.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117(1):43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 15.Subbarao P, Mandhane PJ, Sears MR. Asthma: epidemiology, etiology and risk factors. CMAJ. 2009;181(9):E181–E190. doi: 10.1503/cmaj.080612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Center for Health Statistics. NCHS Urban-Rural Classification Scheme for Counties. Hyattsville, MD: Centers for Disease Control and Prevention; 2014. Available at: www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed Novermber 16, 2015. [Google Scholar]
- 17.Division of Health Interview Statistics. Multiple Imputation of Family Income and Personal Earnings in the National Health Interview Survey: Methods and Examples. Hyattsville, MD: National Center for Health Statistics; 2014. [Google Scholar]
- 18.SUDAAN Language Manual [computer program] Research Triangle Park, NC: Research Triangle Institute; 2012. Release 11. [Google Scholar]
- 19.Szefler SJ. Advances in pediatric asthma in 2014: moving toward a population health perspective. J Allergy Clin Immunol. 2015;135(3):644–652. doi: 10.1016/j.jaci.2014.12.1921. [DOI] [PubMed] [Google Scholar]
- 20.Szefler SJ. Advancing asthma care: the glass is only half full! J Allergy Clin Immunol. 2011;128(3):485–494. doi: 10.1016/j.jaci.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baïz N, Annesi-Maesano I. Is the asthma epidemic still ascending? Clin Chest Med. 2012;33(3):419–429. doi: 10.1016/j.ccm.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Brooks C, Pearce N, Douwes J. The hygiene hypothesis in allergy and asthma: an update. Curr Opin Allergy Clin Immunol. 2013;13(1):70–77. doi: 10.1097/ACI.0b013e32835ad0d2. [DOI] [PubMed] [Google Scholar]
- 23.Platts-Mills TA. The allergy epidemics: 1870–2010. J Allergy Clin Immunol. 2015;136(1):3–13. doi: 10.1016/j.jaci.2015.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Platts-Mills TA, Erwin E, Heymann P, Woodfolk J. Is the hygiene hypothesis still a viable explanation for the increased prevalence of asthma? Allergy. 2005;60(suppl 79):25–31. doi: 10.1111/j.1398-9995.2005.00854.x. [DOI] [PubMed] [Google Scholar]
- 25.Halken S. Prevention of allergic disease in childhood: clinical and epidemiological aspects of primary and secondary allergy prevention. Pediatr Allergy Immunol. 2004;15(suppl 16, 4–5):9–32. doi: 10.1111/j.1399-3038.2004.0148b.x. [DOI] [PubMed] [Google Scholar]
- 26.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martinez FD. New insights into the natural history of asthma: primary prevention on the horizon. J Allergy Clin Immunol. 2011;128(5):939–945. doi: 10.1016/j.jaci.2011.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


