Abstract
Background
Falls in older adults are a major public health concern due to high prevalence, impact on health outcomes and quality of life, and treatment costs. Physical therapists can play a major role in reducing fall risk for older adults; however, existing clinical practice guidelines (CPGs) related to fall prevention and management are not targeted to physical therapists.
Objective
The purpose of this clinical guidance statement (CGS) is to provide recommendations to physical therapists to help improve outcomes in the identification and management of fall risk in community-dwelling older adults.
Design and Methods
The Subcommittee on Evidence-Based Documents of the Practice Committee of the Academy of Geriatric Physical Therapy developed this CGS. Existing CPGs were identified by systematic search and critically appraised using the Appraisal of Guidelines, Research, and Evaluation in Europe II (AGREE II) tool. Through this process, 3 CPGs were recommended for inclusion in the CGS and were synthesized and summarized.
Results
Screening recommendations include asking all older adults in contact with a health care provider whether they have fallen in the previous year or have concerns about balance or walking. Follow-up should include screening for balance and mobility impairments. Older adults who screen positive should have a targeted multifactorial assessment and targeted intervention. The components of this assessment and intervention are reviewed in this CGS, and barriers and issues related to implementation are discussed.
Limitations
A gap analysis supports the need for the development of a physical therapy–specific CPG to provide more precise recommendations for screening and assessment measures, exercise parameters, and delivery models.
Conclusion
This CGS provides recommendations to assist physical therapists in the identification and management of fall risk in older community-dwelling adults.
According to Sackett et al, “Evidence-based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence-based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research.”1(p71) Tools for implementing evidence-based practice include documents that synthesize available evidence, such as systematic reviews, and documents that guide decision making, such as clinical practice guidelines (CPGs) and clinical guidance statements (CGSs), also known as clinical practice appraisals. According to the Institute of Medicine, “Clinical practice guidelines are statements that include recommendations intended to optimize patient care that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options.”2(p2) Clinical practice guidelines use strong methodology to guide a systematic review of all available literature to develop statements and recommendations for appropriate health care decisions. In contrast, the CGS systematically compares and synthesizes CPGs of similar topic areas. Key elements of each CGS “include a discussion of areas of agreement and difference, the major recommendations and the corresponding strength of evidence and recommendation rating schemes, and a comparison of guideline methodologies.”3
Each year, approximately 30% of adults aged 65 years or older fall, resulting in $30 billion spent annually in direct and indirect medical costs.4 According to 2010 National Health Interview Survey statistics, falls contributed to 13 million medically treated injuries, with 20% of those falls resulting in serious injury that was treated in emergency departments.5 In 2005, emergency department medical costs for treated falls totaled $6.5 billion.6 Death rates from falls have increased substantially over the past decade,7 and the number of falls is projected to increase as the baby boomers age.8 The associated costs of falls and their impact on quality of life have brought fall risk management and prevention to the forefront of clinical and public health initiatives.
There is evidence that falls can be prevented by screening to detect risk factors and by the prescription of tailored interventions, a process within the scope of physical therapist practice.9,10 There is a substantial body of research on risk factors, interventions, and prevention strategies for falls.11–16 This research has provided evidence for the development of best practice recommendations for fall risk screening, including the Centers for Disease Control and Prevention's (CDC's) STEADI (“Stopping Elderly Accidents, Deaths & Injuries”) Tool Kit17 and published recommendations such as those developed by the US Preventive Services Task Force (USPSTF).18 In addition, CPGs for health care practitioners for the assessment and prevention of falls in community-dwelling older adults have been developed by several organizations such as the National Institute for Health and Care Excellence (NICE)19 and the American Geriatrics Society/British Geriatrics Society (AGS/BGS),20 representing a substantial investment of resources and expertise.
A caveat is that these CPGs have been developed within the broad context of medical and public health practice. As such, they do not specifically address a physical therapist's clinical decision making, which may cause ambiguity in interpreting existing evidence and applying that evidence to diverse patient populations and needs. Therefore, the overall aim of this project was to create a CGS to guide physical therapist practice using existing CPGs that address falls in community-dwelling older adults. The specific objectives of this document were: (1) to identify and critically appraise the available CPGs, (2) to synthesize appraisal findings across high-quality CPGs, (3) to provide a clinically useful summary of recommendations of each CPG for the physical therapist, and (4) to report gaps in evidence for CPGs relevant to physical therapist practice. We expect that physical therapists will use this CGS to guide clinical decision making related to the screening and management of patients at risk for falls and ultimately to reduce unwarranted variation in clinical practice and improve health outcomes.
Method
Expert Panel Process
In 2012, the Subcommittee on Evidence-Based Documents was assembled by the Practice Committee of the Academy of Geriatric Physical Therapy. The members of the Subcommittee and one content matter expert formed the core working group, which was charged with developing evidence-based documents (EBDs) for physical therapists for the management of fall risk in older adults. This working group and the coordinator consisted of physical therapists with expertise in rehabilitation science, kinesiology, motor control, geriatrics, measurement, and fall prevention. Multiple panelists had clinical practice experience with community-dwelling older adults. Although the majority of physical therapists' fall-related interactions involve older adults identified as patients, physical therapists also may address fall risk in older adults who are not patients, but rather clients seeking consultation and information. For simplicity, we use the term “patient” in this document, inclusive of both groups.
The identification and critical appraisal of guidelines.
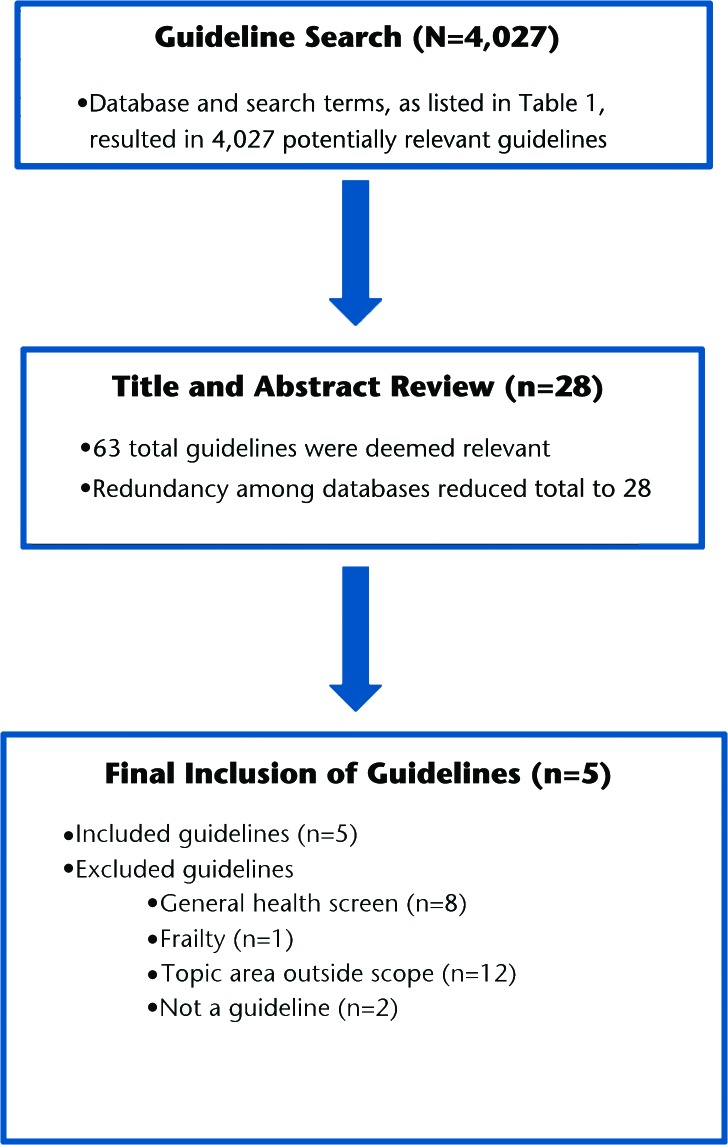
Eleven freely accessible CPG databases were systematically searched for all fall-related content (Tab. 1). Intentionally broad search terms included “falls,” “geriatric,” and “older adults.” Only CPGs were included in this document; all other types of EBDs were excluded. Clinical practice guidelines published between 2000 and 2013 were included if they were written in English and targeted adults over the age of 65 years living in the community or in assisted-living settings. The definition of a fall varies in the literature.21,22 One main difference in definitions is whether falls with loss of consciousness are considered to be falls. We aimed to address the broadest definition of falls; therefore, we did not exclude CPGs based on fall definition. Similarly, there is little consensus on the definition of the term “community-dwelling.” As residents of assisted-living settings have varying levels of independence, CPGs targeting this cohort were included in the search. Due to differences in risk factors and management approaches for fall risk in older adults in acute care, skilled nursing, and long-term care settings, these settings were excluded. Clinical practice guidelines were excluded if they were specific to a neurologic condition (eg, stroke, Parkinson disease, multiple sclerosis) or to fracture management. Figure 1 shows the flow diagram of reviewed CPGs. Of the 4,027 EBDs identified, 5 met the inclusion criteria and were selected for review by the entire core working group.
Table 1.
Search Strategy Used for Retrieval of Clinical Practice Guidelines (CPGs)
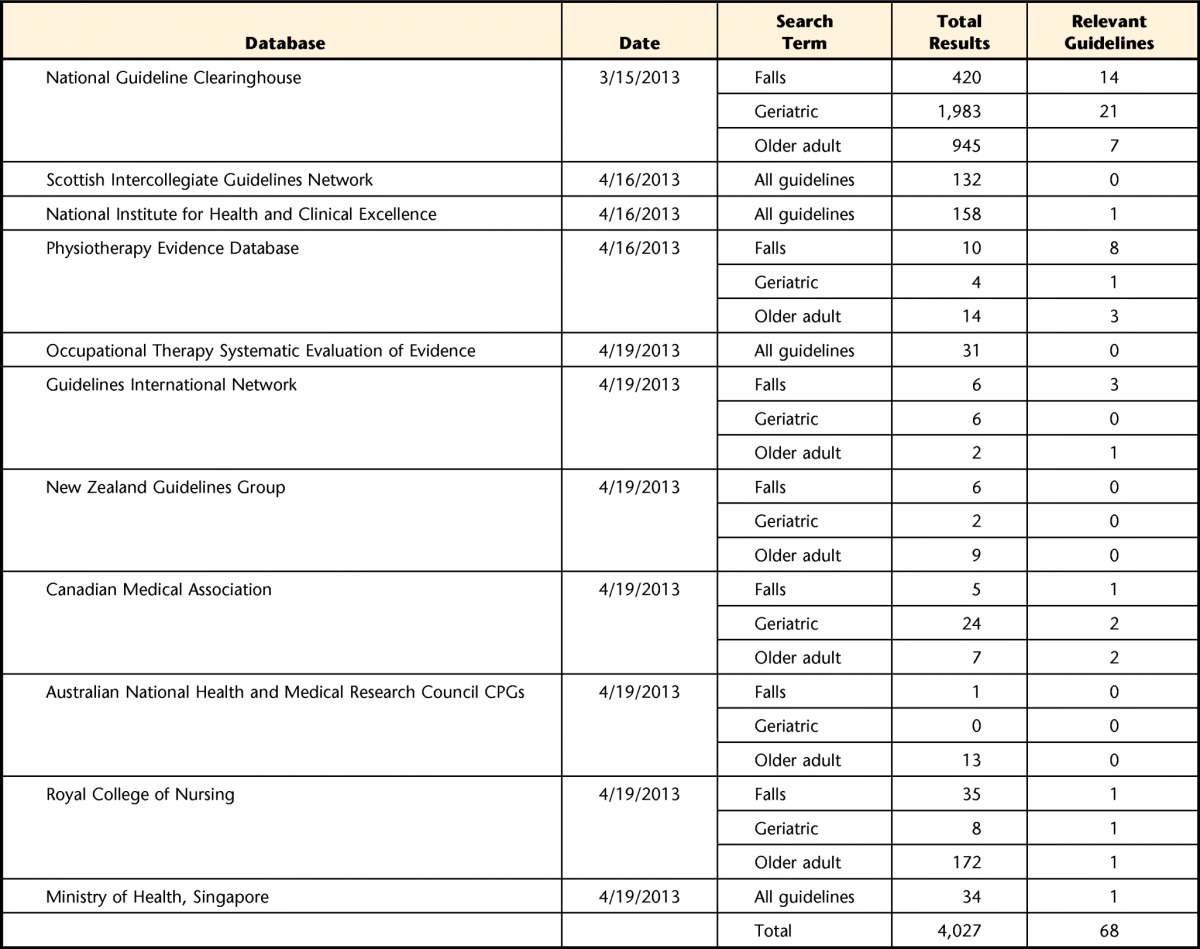
Figure 1.
Flow diagram for clinical practice guidelines.
The 5 CPGs (and associated online content where available) were independently reviewed by the core working group using the Appraisal of Guidelines, Research, and Evaluation in Europe II (AGREE II) tool.23 The AGREE II tool was developed to appraise CPG quality via 23 items addressing 6 key domains: scope and purpose (3 items), stakeholder involvement (3 items), rigor of development (8 items), clarity of presentation (3 items), applicability (4 items), and editorial independence (2 items). Each item was rated using a 7-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). Item values are summed for each of the 6 domains. In addition, reviewers respond to a global quality statement: “I would recommend this guideline for use.” Response options include “yes,” “yes with modifications,” and “no.” Prior to review, all panelists completed online training24 on the AGREE II method. A calibration process was performed for the first 2 reviews (NICE19 and AGS/BGS20 CPGs), in which members independently conducted the AGREE II review, submitted scores, and discussed each scoring item via teleconference. All 5 CPGs were appraised by at least 3 reviewers, and 3 CPGs (NICE,19 AGS/BGS,20 and AGILE25) were reviewed by all members. The core working group discussed each CPG via a series of 4 telephone conference calls and one in-person meeting. Consensus was established for any item for which greater than a 2-point range existed among AGREE II scores.
Stakeholder Input and Review
Stakeholder input was solicited via separate reviews of 2 successive drafts of the CGS. The first review was solicited from the consulting group, which consisted of a physical therapist with expertise in falls in community-dwelling older adults, 2 laypeople who represented the population of interest (ie, community-dwelling older adults), a physician geriatrician, and an exercise physiologist with expertise in falls in community-dwelling older adults. The core working group considered each comment and performed consensus edits to produce a revised second draft.
The second draft was then reviewed by the external review group, which consisted of 2 physical therapists who were board certified in geriatric physical therapy, a physical therapist who was a Certified Exercise Expert for Older Adults and a consultant on legislative affairs and reimbursement, a public health policy maker, a primary care physician, a physician geriatrician, and special reviewers with specific expertise. The core working group considered each comment and performed consensus edits to produce the third draft.
The third draft, in turn, was made available to the public for a 2-week period of review and comment via the website of the Academy of Geriatric Physical Therapy, publicized via 2 blast emails to the membership of the Academy of Geriatric Physical Therapy as well as social media platforms of the Academy of Geriatric Physical Therapy and the American Physical Therapy Association. Resulting comments were reviewed by the authors and discussed via conference call. Actionable comments were then addressed to produce the fourth and final draft.
Results
Description of 3 CPGs Rated as “Recommended for Use”
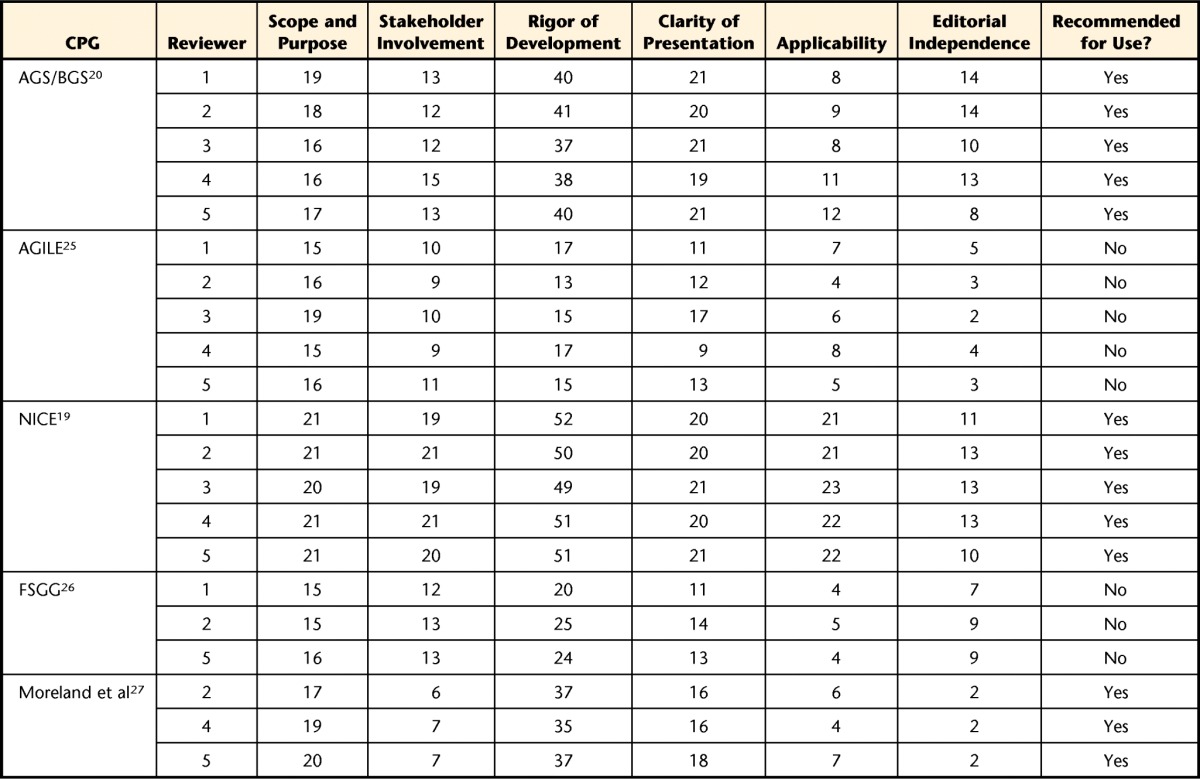
Reviewers obtained highly consistent overall scores and recommendations using the AGREE II instrument (Tab. 219,20,25–27). Three CPGs were rated as “recommended for use,” and 2 were rated as “not recommended for use.” The recommended CPGs are briefly described as follows:
Table 2.
AGREE II Domain Scores and Recommendations for Use for Each Falls CPGa
CPG for assessment and prevention of falls in older people.
Developed by the National Collaborating Centre for Nursing and Supportive Care (NCC-NSC) and funded by NICE, this CPG19 (hereafter referred to as the NICE CPG) was published in 2004, reviewed in 2011, and updated June 2013. This CPG was developed by a multidisciplinary team and incorporated a wide range of stakeholders, including those from a variety of health professions.
Prevention of falls in older people.
Supported by the AGS/BGS, this CPG20 (hereafter referred to as the AGS/BGS CPG) was published in 2001 and revised in 2010. This CPG was developed by a multidisciplinary team and incorporated a wide range of stakeholders, including a Geriatrics Certified Specialist physical therapist.
Evidence-based guidelines for the secondary prevention of falls in older adults.
Developed by Moreland et al27 and funded by the R. Samuel McLaughlin Foundation, this CPG (hereafter referred to as the Moreland CPG) was published in 2003 and has not been updated. In contrast to the other 2 CPGs, it does not address primary prevention of falls, but rather was developed as a tool for clinicians and researchers to address evidence-based assessments and interventions for people who have fallen and are at high risk for future falls. The characteristics of the development group were not described.
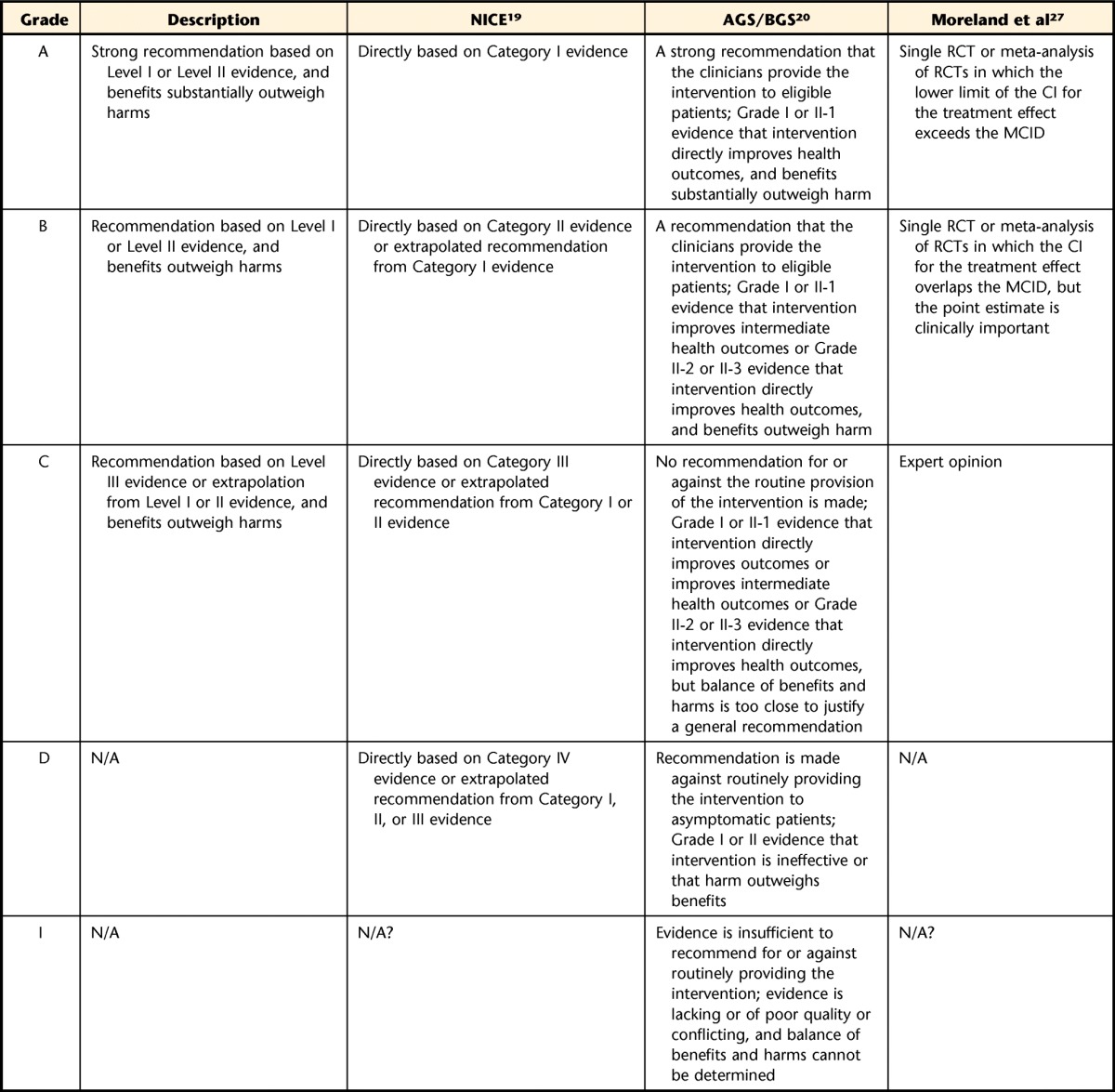
Synthesis of CPG Strength of Evidence and Levels of Recommendation
The included CPGs used different definitions and criteria for their grades of recommendations and levels of evidence (Tabs. 3 and 4). Also, the actions associated with the recommendations put forth were not uniform and required interpretation of the working group. Therefore, our expert opinion comprised synthesizing the specific recommendation or recommendations, strength of the recommendations, and levels of evidence. To determine the strength of recommendation for this CGS, we considered the recommendation strength, grades of levels of evidence, evidence tables, and our interpretation of the balance between benefit and harm. This document refers to the grades of the recommendations from this working group as CGS Grades, and these are described in Table 4.
Table 3.
Level of Evidence Rating Systems Used in the Development of This Clinical Guidance Statementa
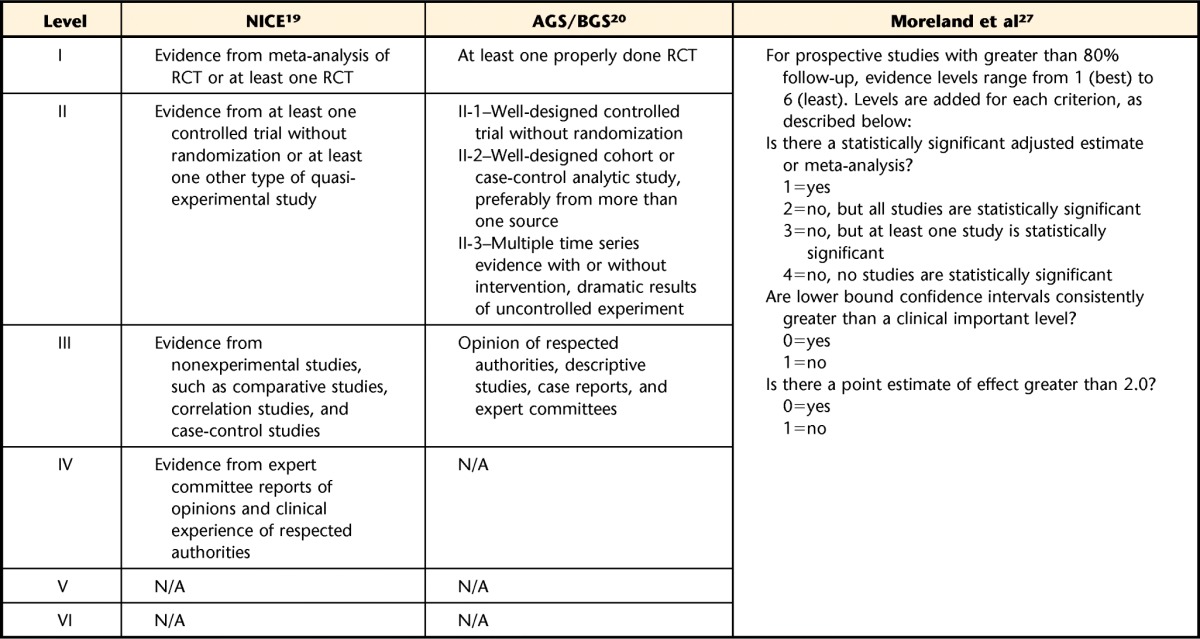
Table 4.
Strength of Recommendation Rating System Used in the Development of This Clinical Guidance Statementa
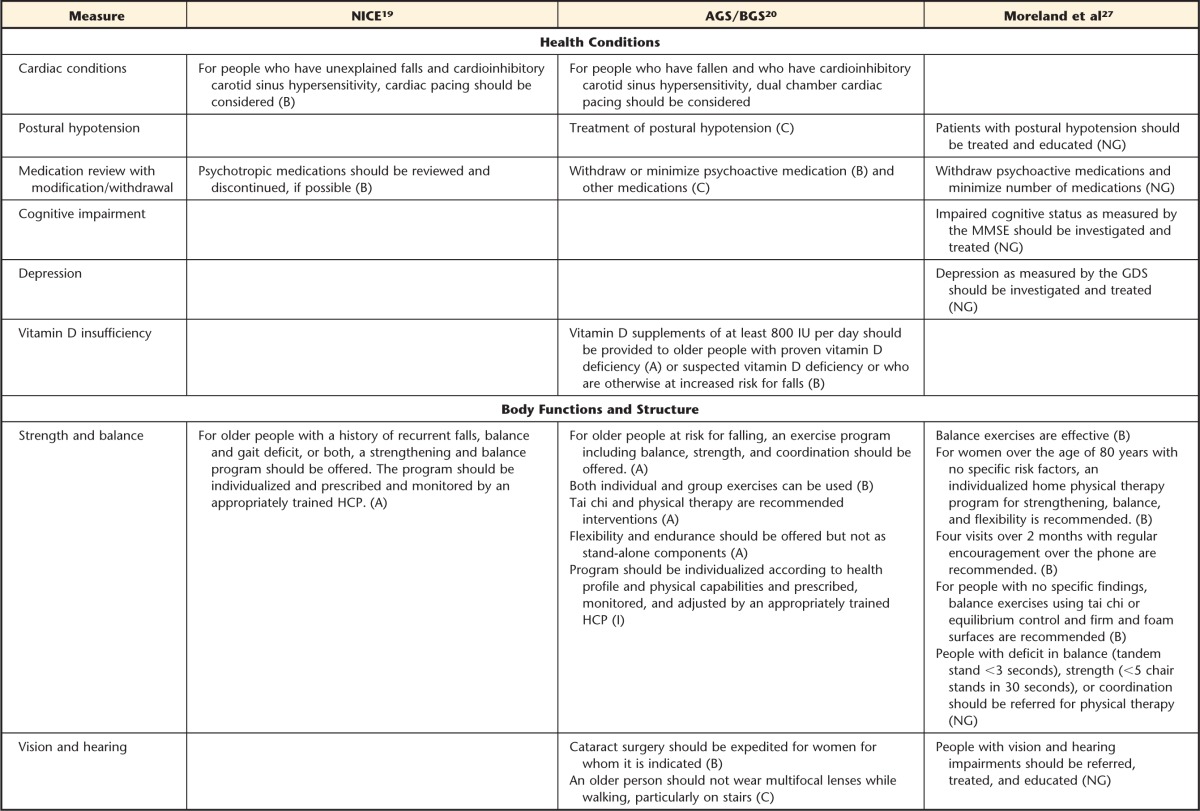
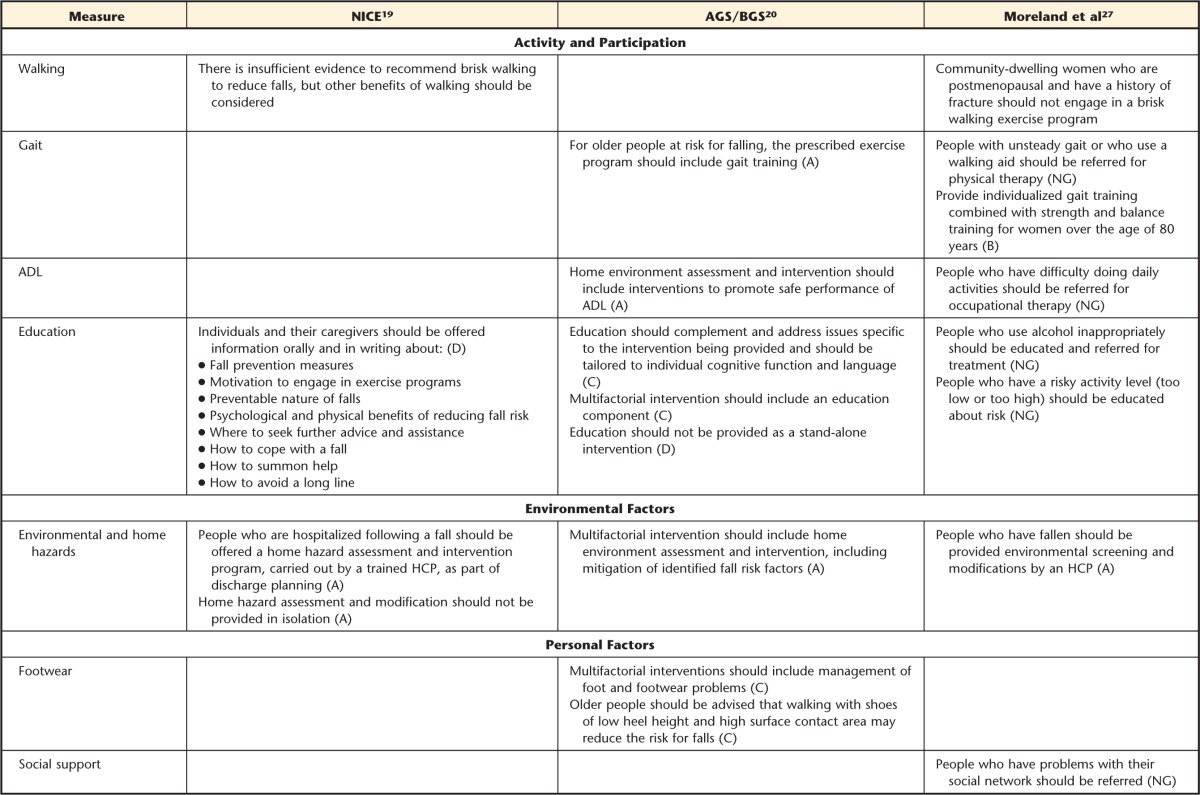
The recommendations from the CPGs are summarized as follows: general recommendations (Tab. 5), the components of a multifactorial assessment for older adults at increased risk (Tab. 6), and the recommendations related to multifactorial interventions (Tab. 7). The recommendations are organized using the World Health Organization International Classification of Functioning, Disability and Health (ICF) framework.28 A summary of action statements is presented in Figure 2.
Table 5.
General Recommendations from 3 High-Quality Clinical Practice Guidelinesa
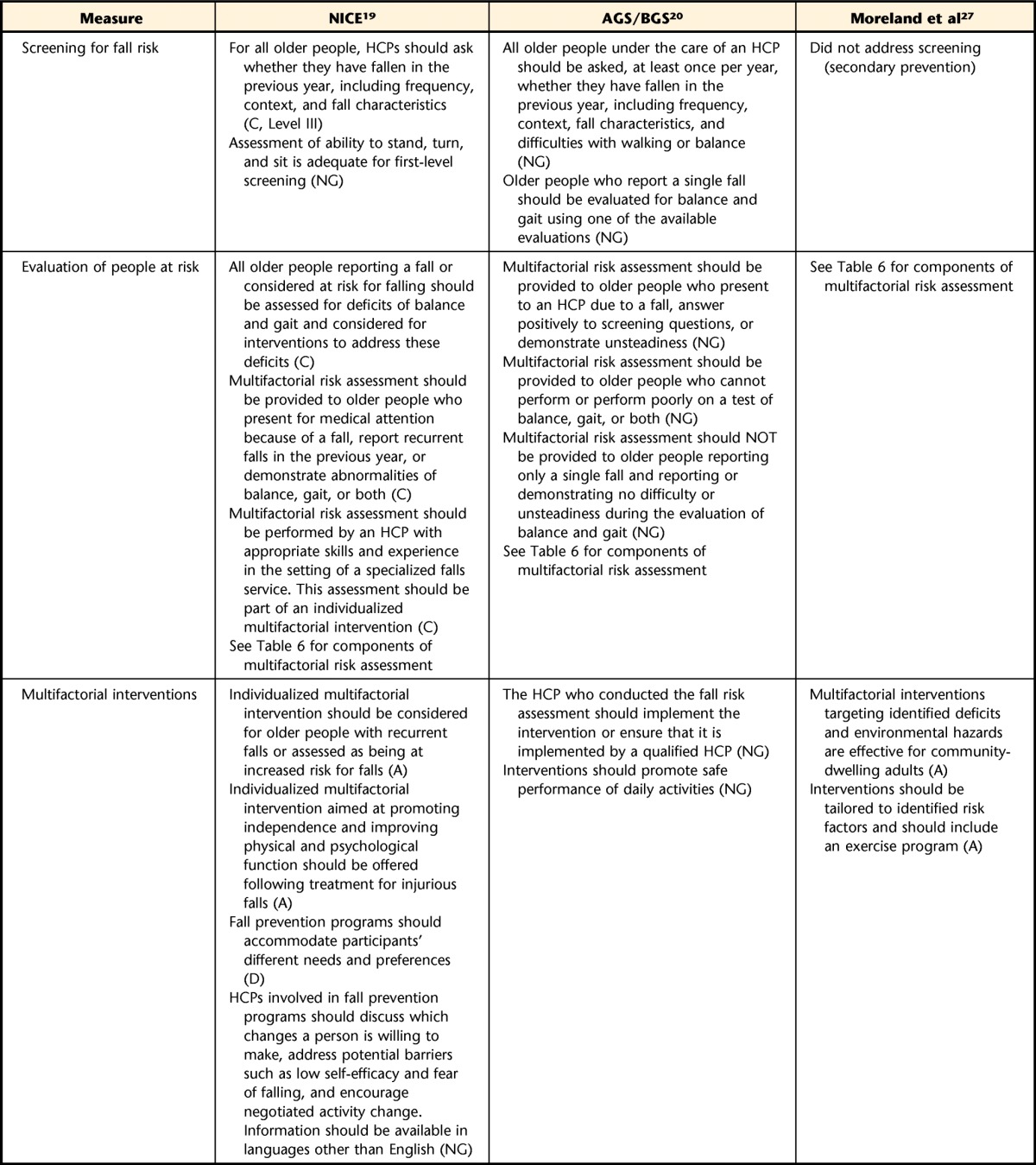
Table 6.
Components of Multifactorial Assessment as Recommended by Reviewed Clinical Practice Guidelinesa
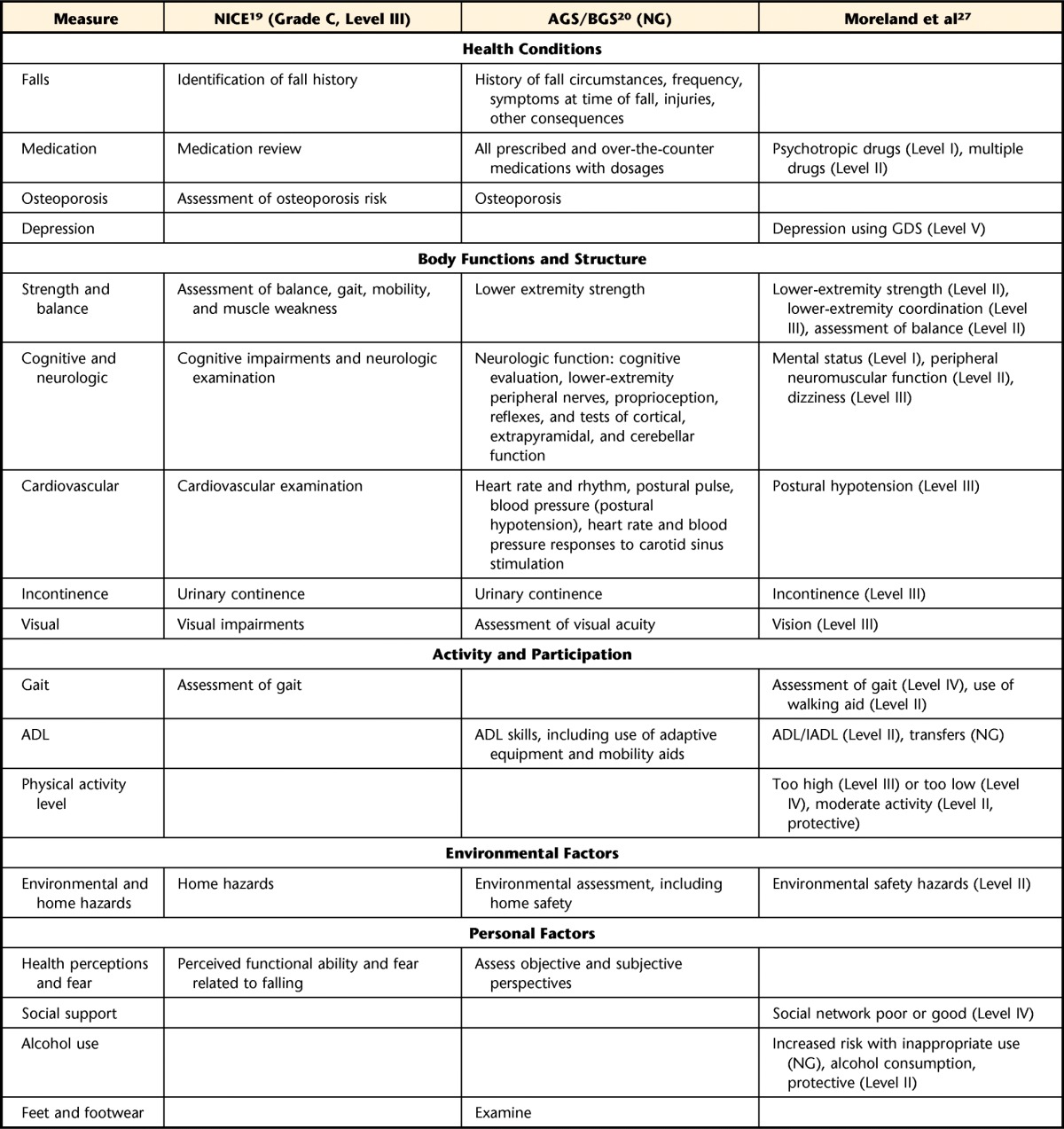
AGS/BGS=American Geriatrics Society/British Geriatrics Society,20 NICE=National Institute for Health and Care Excellence,19 ADL=activities of daily living, IADL=instrumental activities of daily living, GDS=Geriatric Depression Scale, NG=not graded. See Tables 3 and 4 for explanation of evidence levels and recommendation grades.
Table 7.
Summary of Intervention Recommendations for Community-Dwelling Older Adults From Reviewed Clinical Practice Guidelinesa
AGS/BGS=American Geriatrics Society/British Geriatrics Society,20 NICE=National Institute for Health and Care Excellence,19 ADL=activities of daily living, HCP=health care provider, MMSE=Mini-Mental State Examination, GDS=Geriatric Depression Scale, NG=not graded. See Table 4 for definitions of recommendation grades.
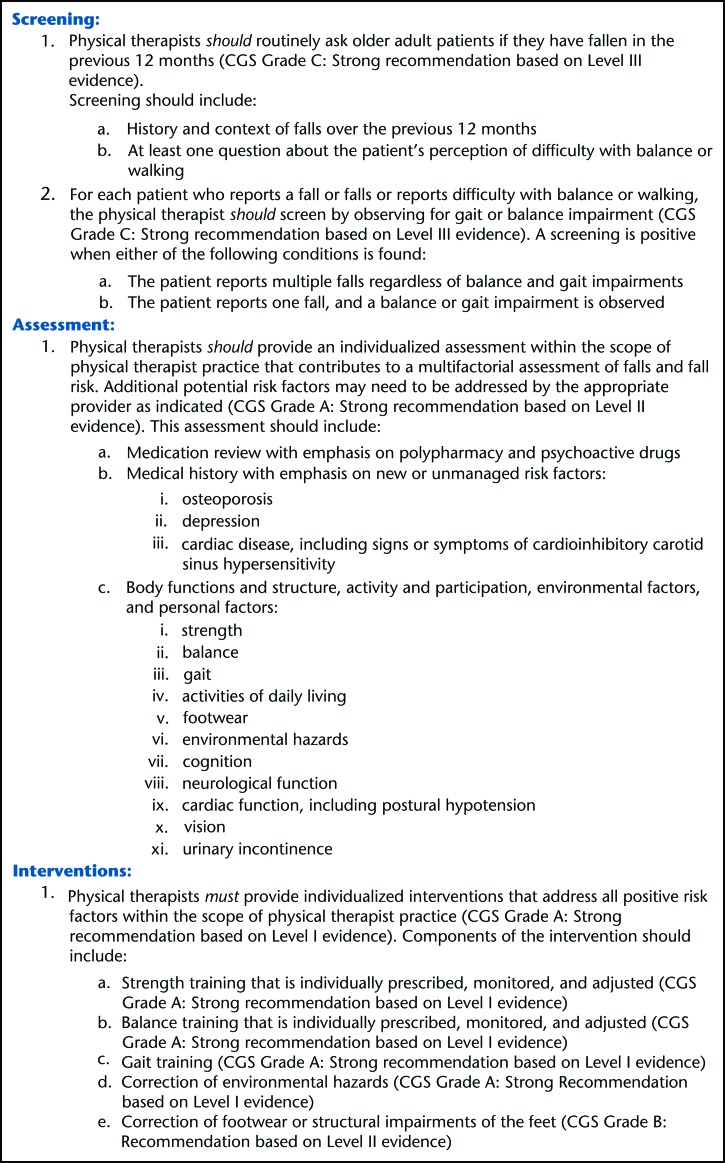
Figure 2.
Summary of action statements.
➢ Screening Recommendations
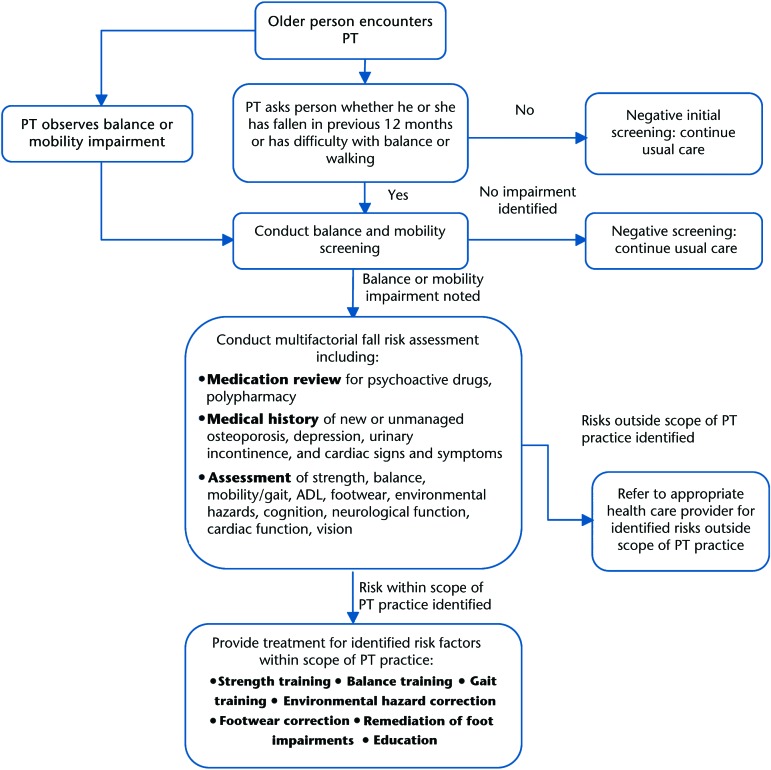
The intention of the screening process is to determine if a multifactorial assessment is necessary. The order in which the screening process should take place is outlined in Figure 3.
Figure 3.
Identification and management of fall risk for community-dwelling older adults. PT=physical therapist, ADL=activities of daily living.
-
Physical therapists should routinely ask older adult patients if they have fallen in the previous 12 months (CGS Grade C: Strong recommendation based on Level III evidence).
Screening should include:- History and context of falls over the previous 12 months
- At least one question about the patient's perception of difficulty with balance or walking
- For each patient who reports a fall or falls or reports difficulty with balance or walking, the physical therapist should screen by observing for gait or balance impairment (CGS Grade C: Strong recommendation based on Level III evidence). A screening is positive when either of the following conditions is found:
- The patient reports multiple falls regardless of balance and gait impairments
- The patient reports one fall, and a balance or gait impairment is observed
Rationale.
Overall, the NICE19 and AGS/BGS20 CPG screening recommendations are similar (Tab. 5); the Moreland27 CPG does not address screening. The NICE and AGS/BGS CPGs recommend screening all older adults by asking them if they have fallen in the previous year. The fall inquiry recommendations include frequency, context, fall characteristics, and, according to the AGS/BGS CPG, self-reported difficulties with balance or walking. The NICE CPG recommends assessing the ability to stand, turn, and sit as being adequate for a first-level screening. The AGS/BGS CPG does not describe an initial screening tool but does suggest including one measure of balance, gait, or both. Examples from the AGS/BGS CPG include the Timed “Up & Go” Test,29 the Berg Balance Scale,30 and the Performance-Oriented Mobility Assessment.31 Although the NICE CPG recommendation is Grade C based on Level III evidence, our recommendation uses stronger language because the benefit of these screening activities far outweighs the associated harms.
The CPGs do not address the situation in which an older adult has obvious balance and gait impairments but does not report having had a fall in the previous 12 months. The AGS/BGS further comments that multifactorial fall risk assessment should not be applied to older adults who (1) report only a single fall and (2) demonstrate no unsteadiness or difficulty with balance or gait.20
➢ Assessment Recommendation
- Physical therapists should provide an individualized assessment within the scope of physical therapist practice that contributes to a multifactorial assessment of falls and fall risk. Additional potential risk factors may need to be addressed by the appropriate provider as indicated (CGS Grade A: Strong recommendation based on Level II evidence). This assessment should include:
- Medication review with emphasis on polypharmacy and psychoactive drugs
- Medical history with emphasis on new or unmanaged risk factors:
- osteoporosis
- depression
- cardiac disease, including signs or symptoms of cardioinhibitory carotid sinus hypersensitivity
- Body functions and structure, activity and participation, environmental factors, and personal factors:
- strength
- balance
- gait
- activities of daily living
- footwear
- environmental hazards
- cognition
- neurological function
- cardiovascular function, including postural hypotension
- vision
- urinary incontinence
Health Conditions
Medication review.
All of the 3 CPGs19,20,27 recommend a medication review as part of the multifactorial assessment. The AGS/BGS20 CPG recommends identification of all medications with dosages. The NICE19 and Moreland et al27 CPGs specifically recommend the identification of psychotropic and cardiac medications, as well as polypharmacy, as risk factors for falls. The Moreland27 CPG identified the following medication classes as psychotropic: benzodiazepines, hypnotics, antidepressants, and major tranquilizers. The term “polypharmacy” is not defined in the CPGs but is often used to represent medication use that is excessive, inappropriate, or both. This term is operationally defined as the use of multiple medications concurrently, excluding preparations that include more than one drug.
Osteoporosis.
The NICE19 and AGS/BGS20 CPGs recommend that osteoporosis risk or diagnosis be assessed as part of the identification of risk factors for falls.
Depression.
The Moreland27 CPG identifies depression as a potentially modifiable risk factor for falls and, therefore, recommended assessment. The Geriatric Depression Scale32 is mentioned as a screening tool for depression in older adults.
Body Functions and Structure
Strength.
All 3 CPGs19,20,27 identify muscular weakness as a risk factor for falls. Accordingly, each CPG includes an assessment of muscle strength as part of a multifactorial assessment. The AGS/BGS20 and Moreland27 CPGs specify inclusion of lower extremity strength.
Balance.
All 3 CPGs19,20,27 recommend balance assessment, but no specific procedures or methods are recommended.
Cognitive and neurologic function.
All 3 CPGs19,20,27 address the assessment of cognitive and neurologic function. The AGS/BGS20 CPG specifies testing lower extremity peripheral nerve function, proprioception, reflexes, and cortical, extrapyramidal, and cerebellar function. The NICE19 CPG recommends assessing for cognitive impairments but does not identify the specific items that should be included. The Moreland27 CPG recommends assessing mental status, peripheral neuromuscular function, and dizziness.
Cardiovascular function.
The NICE19 and AGS/BGS20 CPGs recommend a cardiovascular assessment by a health care professional with specialized skills. The NICE CPG specifically recommends the need to identify anti-arrhythmic medications. The AGS/BGS CPG recommends assessing heart rate and rhythm, postural pulse, blood pressure, and postural hypotension, all of which can be conducted by a physical therapist. However, heart rate and blood pressure responses to carotid sinus stimulation should be performed by a qualified medical professional. The Moreland27 CPG recommends identifying the use of cardiac drugs and presence of postural hypotension.
Vision.
The AGS/BGS20 CPG recommends an assessment of visual acuity. While also recommending an assessment of vision, neither the NICE19 CPG nor the Moreland27 CPG identifies the aspects of vision (eg, acuity, contrast sensitivity, depth perception, peripheral vision, eyewear) that should be addressed.
Urinary function and incontinence.
Assessing for urinary incontinence was recommended by all 3 CPGs,19,20,27 with the NICE19 CPG specifically identifying urge and stress incontinence.
Activity and Participation
Gait.
All 3 CPGs19,20,27 identify gait deficits or abnormalities as a risk factor for falls and recommend a thorough assessment of gait. However, no specific procedures or methods are provided. Moreland et al27 recommended assessing for the use of walking aids. The NICE19 CPG acknowledges that many tests of balance and gait exist and states that the individual provider should identify appropriate measures for each older adult.
Activities of daily living.
The AGS/BGS20 CPG recommends assessment of activities of daily living (ADL), including use of adaptive equipment and mobility aids. The Moreland27 CPG recommends assessment of ADL and instrumental ADL as well as transfers.
Physical activity.
The Moreland27 CPG is the only CPG to recommend an assessment of physical activity. Specifically, it identifies moderate activity levels as having a protective effect and high (not defined) and low (less than once per week) activity levels as risk factors.
Environmental Factors
Environmental assessment.
All 3 CPGs19,20,27 identify home safety and hazards as risk factors for falls and recommend an assessment of the home for hazards. The NICE19 CPG recommends that specific attention be paid to loose rugs and mats and carpet folds or other trip hazards.
Personal Factors
Fear and health perception.
The NICE19 and AGS/BGS20 CPGs recommend an assessment of perceived functional ability and fear of falling.
Social support.
The Moreland27 CPG recommends an assessment of the quality of the older adult's social network.
Alcohol use.
The Moreland27 CPG recommends an assessment of “inappropriate alcohol use”; however, it does not define “inappropriate.”
Feet and footwear.
The AGS/BGS20 CPG recommends the assessment of feet and footwear.
➢ Intervention Recommendations
- Physical therapists must provide individualized interventions that address all positive risk factors within the scope of physical therapist practice (CGS Grade A: Strong recommendation based on Level I evidence). Components of the intervention should include:
- Strength training that is individually prescribed, monitored, and adjusted (CGS Grade A: Strong recommendation based on Level I evidence)
- Balance training that is individually prescribed, monitored, and adjusted (CGS Grade A: Strong recommendation based on Level I evidence)
- Gait training (CGS Grade A: Strong recommendation based on Level I evidence)
- Correction of environmental hazards (CGS Grade A: Strong Recommendation based on Level I evidence)
- Correction of footwear or structural impairments of the feet (CGS Grade B: Recommendation based on Level II evidence)
Rationale.
The recommendations above describe the physical therapy–related components of the multidisciplinary fall risk management interventions represented within the CPGs. Overall, recommendations across the CPGs are similar. There is agreement that an individualized exercise program, including both strength and balance training, should be implemented for those at risk for falls (Grade A). Recommendations for the multidisciplinary interventions are shown in Table 7, and the physical therapy components of the interventions are summarized below.
Body Functions and Structure
Strength and balance training.
Both NICE19 and AGS/BGS20 CPGs recommend that an individualized program be prescribed and monitored by an appropriately trained health professional (Grade A). The NICE CPG recommends a strength and balance training program, whereas the AGS/BGS CPG recommends strength, balance, coordination, and gait training. The AGS/BGS CPG recommends individual and group exercises as well as tai chi and physical therapy. It further recommends offering flexibility and endurance exercises but not as sole interventions. The Moreland27 CPG provides more narrow recommendation of individualized strength and balance training for community-dwelling women over the age of 80 years. It further recommends tai chi or “equilibrium control” exercises using foam and firm surfaces.
Activity and Participation
Walking.
With respect to fall prevention interventions, there is no evidence that unsupervised, brisk walking decreases fall risk. However, it is well documented that walking programs convey other types of health benefits.33 The NICE19 CPG found insufficient evidence to recommend brisk walking to reduce falls but noted that other benefits of brisk walking should be considered. The Moreland27 CPG recommends against brisk walking in community-dwelling women who are postmenopausal and have a history of fracture. The NICE CPG indicates that unsupervised, brisk walking may actually have a detrimental effect in some populations, depending on the patient's impairments and abilities.
Gait training.
The AGS/BGS20 CPG recommends gait training for adults at risk for falls. The Moreland27 CPG specifically recommends individualized gait training combined with strength and balance training for community-dwelling women over the age of 80 years. The Moreland CPG also recommends referral to a physical therapist for those who demonstrate unsteady gait or require a walking aid.
ADL training.
The AGS/BGS20 and Moreland27 CPGs recommend ADL training for those with difficulty performing ADL.
Nonspecific exercise.
The NICE19 found insufficient evidence to recommend low-intensity exercise and generic group exercise programs that do not target impairments known to be related to fall risk.
Education and information giving.
Although not included as recommendations in this CGS because of low strength of evidence, the NICE19 CPG recommends providing information verbally and in writing on fall prevention, effective measures, motivation to engage in exercise, and benefits of engaging in fall risk reduction (Tab. 7) (Grade D). Additional recommendations relevant to the educational intervention include adherence to and motivation to perform exercise programs, where to seek further advice and assistance, how to summon help should a fall occur, and avoidance of use of multifocal lenses while walking (particularly on stairs). The AGS/BGS20 CPG recommends that tailored education be included in a multifactorial intervention but not provided as a sole intervention (Grade D). Moreland et al27 found insufficient evidence to recommend targeted or untargeted educational programs about falls or fear of falling without subsequent follow-up on recommendations, but the Moreland CPG does recommend education related to specific risk factors found during the assessment, including risky activity level and inappropriate alcohol use.
Environmental Factors
Home hazard modification.
All 3 CPGs19,20,27 recommend a home hazard assessment and modification for older people who have fallen and those who are at risk for falls. Both the NICE19 and Moreland27 CPGs specify that home hazard assessment should not be conducted without follow-up and modification. The CPGs do not specify the components of a home hazard assessment or recommend particular home assessment tools.
Personal Factors
Footwear.
The AGS/BGS20 CPG recommends treatment of foot problems identified in a multifactorial assessment and advice to include low heel height and high surface contact area (Grade C). Neither the NICE19 CPG nor the Moreland27 CPG makes recommendations regarding footwear.
Hip protectors.
The NICE19 found insufficient evidence to recommend hip protectors for fall prevention. However, the NICE CPG makes the distinction that hip protectors may not be effective for fall prevention but have been shown to prevent fractures from falling.
Gap Analysis
Existing CPGs19,20,27 are clear that (1) all older adults should be screened for fall risk, (2) multifactorial assessments targeting an individual's risk factors should be conducted on those who screen positive, and (3) tailored interventions should be implemented to address the risk factors that are identified. Physical therapists can address many aspects of fall risk management inherent within these 3 areas of screening, assessment, and intervention; however, knowledge gaps exist across all 3 areas.
Screening
Physical therapists should play a role in questioning older adults about the presence, frequency, and circumstances surrounding falls and in screening for balance impairments and gait limitations. Although taking a fall history seems relatively straightforward, research is limited. It is not clear which are the key questions regarding the specific circumstances or factors linked to the fall history that can be used to guide a physical therapist's clinical decision making. The NICE19 CPG mentions a few balance and gait screening tools. However, not all of the measures have validated cut-points for fall prediction. More research is needed to synthesize evidence and validate cut-points that indicate increased fall risk. There is a need for evidence-based recommendations to describe the predictive performance (eg, sensitivity, specificity, likelihood ratios) and clinical feasibility of fall risk screening tools.
Assessment
A multifactorial assessment is recommended for older adults who screen positive for fall risk (Tab. 5). The NICE19 CPG addresses overarching organizational changes needed to decrease fall risk across the spectrum of care. In that context, it suggests that assessment should occur within a specialized falls service. Research is needed to identify the most effective and efficient delivery model or models for fall risk assessment and management across populations at varying levels of risk. Implementation of these recommendations may vary depending on practice setting.
Existing CPGs recommend components of a multidisciplinary assessment. The information obtained from the assessment tools guides treatment decision making beyond simply identifying risk for falls. However, more research is needed to identify the pertinent characteristics of assessment tools for people who are at risk for falls. For example, objective measures are needed to assess the impact of factors such as ADL limitations and cognitive, lower extremity, and balance impairments and the corresponding implications for the development of optimal interventions.
Interventions
To address recommendations related to cardiac pacing, postural hypotension, medication modification, vitamin D supplementation, and vision referral, physical therapists need to consult with and refer patients to appropriate health care practitioners. In contrast, interventions specific to balance and gait impairments can be directly and effectively managed by a physical therapist. However, current recommendations that guide practice require greater specificity, including (1) optimal mode, intensity, and frequency of balance and strength training; (2) optimal strategies for delivery of exercise programs; (3) optimal strategies for individualization of exercise programs; and (4) characteristics of older adults who may benefit from specific exercise regimens. Further guidance as to mode of information delivery and methods to increase adherence also is needed. Finally, greater specificity is warranted on the prioritization of the components of home hazard modification based on economic and clinical feasibility.
Discussion
The purposes of this CGS are: (1) to identify, critically appraise, and compare published CPGs on fall risk management; (2) to make recommendations for physical therapist practice in screening, assessing, and managing fall risk in community-dwelling older adults; and (3) to analyze gaps in the existing CPGs to guide future research and the development of additional EBDs to facilitate physical therapy and policy decision making.
The recommendations presented in this CGS are the result of a thorough systematic review and critical appraisal process. The 3 CPGs that were identified provided recommendations for fall risk screening, assessment, and intervention. The common recommendations were that (1) all older adults should be screened for fall risk by asking questions about falls and difficulties in gait and balance and briefly observing the presence of difficulties in gait and balance; (2) a positive screening should prompt a comprehensive, multidisciplinary fall risk assessment; and (3) the multifactorial assessment should be followed by an intervention that addresses identified risk factors. The multidisciplinary nature of this assessment lends to some factors requiring a referral to other qualified health care professionals, whereas other factors fall within the scope of physical therapist practice.
The USPSTF34 is an independent expert body that provides evidence-based recommendation statements for preventive services and primary care for clinicians and health systems. Through the Medicare Improvement for Patients and Providers Act of 2008, which governs policy for preventive services, the Department of Health and Human Services is authorized to reimburse preventive services receiving a level A or B rating from the USPSTF. Reimbursement policies that dictate payment and practice are broadly influenced by the largest payer for US health care services, the Medicare program. Therefore, the USPSTF recommendations have a tremendous impact on the implementation of preventive care.35 The USPSTF has developed recommendations related to fall risk screening and management which include a Grade B recommendation for exercise or physical therapy and vitamin D supplementation to prevent falls in community-dwelling adults over 65 years of age.18 The USPSTF can be considered a high-quality EBD relevant to fall risk management in community-dwelling older adults. Compared with the USPSTF, this CGS narrows recommendations to community-dwelling older adults but expands on recommended components of a multifactorial assessment and intervention.
It is not recommended to automatically conduct a multifactorial fall risk assessment for all people aged 65 years or older.18,20 This CGS supports the need for all older adults to be screened for fall risk when they come into contact with a physical therapist. Our recommendations are consistent with the USPSTF statement18 that history of falls or mobility problems and poor performance on the Timed “Up & Go” Test29 be used to identify older people at increased risk for falls. However, more information is needed on the extent to which strength and balance impairments are associated with fall risk and the amount of change that is associated with reduced fall risk. In particular, evidence is needed to guide clinicians in appropriately matching patient characteristics and ability levels to available exercise interventions and evidence-based programs, for example; criteria for or predictors of success in specific home-based, group-based, one-on-one facility-based interventions are lacking.
Consistent with this CGS, the USPSTF18 reports that effective exercise includes group-based classes, home-based physical therapy, or both and specifies that the effective dose of intervention ranges from 9 to 75 hours. This wide range is a major gap that can lead to confusion and practice variation regarding how much exercise would be required to achieve the optimal reduction in fall rate and fall risk. In addition, neither this CGS nor the USPSTF provides recommendations for the most effective types of exercise or components of physical therapy intervention.
Evidence from systematic reviews, some of which have been published since the development of existing CPGs, provides useful information to address this gap and guide the evidence-based implementation of guidelines. Sherrington et al14 summarized evidence related to the mode of delivery and type and intensity of physical activity most effective in reducing the risk for falls in older adults by conducting a meta-analysis of trials in which exercise was the stand-alone intervention. This synthesis provides evidence of the effectiveness of an exercise dose of at least 2 hours per week for at least 6 months, with a total dose of more than 50 hours. Their analysis also supports programs that focus on balance training, defined as exercises conducted in a standing position in which participants aim to stand with their feet close together or on one leg, minimize use of their hands for support, and move the body's center of mass in a controlled manner. Consistent with the CGS, Sherrington and colleagues also found that neither walking nor strength training alone, nor simply encouraging older adults to increase activity, is effective in lowering fall rate or risk, highlighting the need to integrate both strength and balance training into the intervention. Depending on the patient's level of functional ability, the plan of care may include interventions to address impairments or limitations in endurance, coordination, flexibility, mobility, gait, feet and footwear, home safety and environmental hazards, and safe and appropriate use of mobility aids.14
Similarly, a 2012 Cochrane Review and meta-analysis by Gillespie et al16 provides evidence that multifactorial home-based and group-based interventions that include strength and balance training and tai chi reduce both fall rate and fall risk. Programs that focused on only strength training or increasing level of physical activity did not affect rate or risk.
The plan of care should include support for behavior change and optimal adherence.14 Physical therapists should elicit and incorporate patients' values and preferences and partner with them in intervention design. Promoting adherence also may require assessing a patient's self-efficacy and fear of falling as potential barriers and connecting the patient with appropriate resources and community providers of evidence-based programs to help support successful behavior change. Physical therapists must ensure that their patients understand the selected interventions and their responsibility to engage in and adhere to the program to the greatest possible degree. Physical therapists working with patients with high fall risk should emphasize the importance of ongoing physical activity and structured exercise, and patients should be empowered to self-manage their fall risk or transition to community-based exercise programs to maintain the gains made in physical therapy.
Implications for Clinical Practice and Next Steps
This CGS supports that all older adults should be screened for fall risk, and this screening may trigger a multifactorial fall risk assessment. Policies that relate to either screening or assessment of the older adult include the following: (1) fall risk screening is a reimbursable service for physicians when it is included in the introductory “Welcome to Medicare” wellness visit but not in subsequent wellness visits, (2) fall screening is a quality indicator for physicians and practices participating in Meaningful Use and Accountable Care Organization initiatives but is not reimbursed under Medicare, and (3) fall assessment is a reimbursable service as well as a Physician Quality Reporting Initiative (PQRI)36 indicator. From these initiatives, it is clear that attempts are being made to focus on fall risk screening and assessment practices in primary care, but these initiatives do not specifically target physical therapists. Policy makers should understand the important role that physical therapists can play in fall risk screening and management. Physical therapists have education and expertise in choosing and administering assessment instruments for fall risk assessment. They are specifically educated in assessment and management of risk factors such as strength and balance impairment, gait and ADL limitations, and home hazards and feet and footwear.
The CDC has recently released the STEADI Tool Kit,17 based on the AGS/BGS20 CPG. The STEADI provides implementation resources for all stages of fall risk management. Screening resources in the STEADI Tool Kit include the Timed “Up & Go” Test,29 30-second Chair Stand Test,37 and 4-Stage Balance Test.38 These tests were selected based on their performance as fall risk screening measures. The STEADI Tool Kit includes a list of recommended interventions for older adults at increased fall risk. These interventions include evidence-based programs in the community such as tai chi,39 Stepping On,40 and the Otago Exercise Program.41 Tai chi and Stepping On are programs that are available in the community (eg, senior centers, YMCAs), delivered by trained lay leaders, and are most appropriate for older adults who are higher functioning. The Otago Exercise Program is delivered by a physical therapist and is most appropriate for frail, community-dwelling older adults at high risk for falls. The Otago Exercise Program is designed to be delivered in 6 to 9 visits over a 1-year period and has demonstrated a 35% reduction in falls in randomized controlled trials.42 The STEADI Tool Kit is a useful fall risk management implementation tool and is consistent with this CGS. The programs suggested by the STEADI Tool Kit have demonstrated effectiveness in reducing falls and are important options for achieving a dose of 50 or more hours of challenging exercise. However, there remains a paucity of evidence to guide the clinician in matching individual patient impairments, functional level, and fall risk to the appropriate evidence-based exercise program to maximize the benefits of participation and minimize the risk of adverse effects.
Limitations
This CGS has several limitations. First, it is specific to older people without neurologic dysfunction who live in the community and present for care in a clinical setting. This CGS should not be used to guide assessment or interventions for those in acute care hospitals or skilled nursing facilities. Second, it is possible that not all relevant CPGs were identified. However, given the level of redundancy in other databases, we believe that we have minimized this problem to a reasonable degree.
Also, in the process of developing this CGS, several complexities of integrating findings into clinical practice became apparent. The CPGs included in this CGS did not explicitly consider the economic impact of recommendations or the range of delivery models and settings that could be involved in implementation. Therefore, the economic and resource implications of these recommendations are unknown. Evidence to demonstrate the health and economic impact of preventive programs across payment and service delivery models is needed to facilitate policy change related to coverage of fall prevention programs by third-party payers across health care settings.
Conclusions
In summary, existing CPGs are clear that every older adult should be screened for fall risk at least once per year and that consideration of balance impairment and gait and mobility limitations is integral to fall risk screening. Fall risk screening may trigger a multifactorial risk assessment, parts of which would be directly implemented by the physical therapist in consultation with other health care providers. Exercise, including structured physical therapy, is an effective component of a fall prevention program, and the physical therapist also may directly provide home hazard and footwear modification and education about fall risk. Current recommendations lack the specificity required to tailor decision making by the physical therapist, highlighting the need for both additional research and a future CPG that is directed at physical therapists. Nevertheless, this CGS synthesizes current recommendations to provide direction for physical therapists as well as descriptions of evidence-based programs provided in the community that might be useful to facilitate long-term exercise participation following discharge from a physical therapy episode of care.
This CGS highlights the current state of the evidence for managing fall risk and identifies gaps in knowledge. The resulting gap analysis demonstrates that more programs need to be developed and studied for specific subpopulations of older adults, including those with dementia, those with chronic disease, and those in institutional settings. Also, there is a need for additional research and tools specifically for physical therapist assessment and intervention. Finally, more research is needed to optimize components related to exercise interventions, including strength and balance training.
Standards for CPG and CGS development are evolving rapidly according to the Institute of Medicine standards,2 and new databases are being constructed at multiple levels of analysis, such as the Guidelines International Network43 for CPGs, the Rehabilitation Measures Database,44 and APTA's Evaluation Database to Guide Effectiveness (EDGE)45 initiative for outcome measures. To maximize resources, minimize clinician confusion and variation, and improve quality of care, physical therapists should work to integrate standards and guideline development processes of diverse entities and the associated technologies. This process requires careful deliberation and investment by the physical therapy profession. The development of a CPG specific to the physical therapist management of fall risk to complement this CGS is an important initiative and a significant step toward improving the quality of care for and quality of life of community-dwelling older adults.
Footnotes
Dr Avin, Dr Hanke, Dr Kirk-Sanchez, Dr McDonough, and Dr Shubert, Dr Hardage provided concept/idea/research design and writing. Dr Avin, Dr Hanke, Dr Kirk-Sanchez, Dr McDonough, and Dr Shubert provided data collection and analysis. Dr Kirk-Sanchez, Dr McDonough, Dr Hardage, and Dr Hartley provided project management and fund procurement. Dr Kirk-Sanchez, Dr McDonough, and Dr Shubert provided institutional liaisons. Dr Hanke, Dr Kirk-Sanchez, and Dr Hartley provided consultation (including review of manuscript before submission).
The Academy of Geriatric Physical Therapy gratefully acknowledges the members of the consulting group: Holly Jean Coward, MD, CMD (physician geriatrician); Jodi Janczewski, DPT (physical therapist with expertise in falls in community-dwelling older adults); Dixon and Landy Qualls (community-dwelling older adults); and Debbie Rose, PhD (exercise physiologist with expertise in falls in community-dwelling older adults).
The Academy of Geriatric Physical Therapy gratefully acknowledges the members of the external review group: (Bonita) Lynn Beattie, PT, MPT, MHA (public health policymaker); Sandra L. Kaplan, PT, DPT, PhD (special reviewer with expertise in methods); Jon D. Lurie, MD, MS (primary care physician); Michelle M. Lusardi, PT, DPT, PhD (special reviewer with expertise in methods and geriatrics); Mindy Oxman Renfro, PhD, DPT, GCS, CPH (Geriatric Certified Specialist); Cathie Sherrington, PhD, MPH, BAppSc (special reviewer with expertise in falls in community-dwelling older adults); Ellen Strunk, PT, MS, GCS, CEEAA (Certified Exercise Expert for Aging Adults and consultant on legislative affairs and reimbursement); Stephanie A. Studenski, MD, MPH (physician geriatrician); and Vicki Tilley, PT, GCS (Geriatric Certified Specialist).
The Academy of Geriatric Physical Therapy extends its appreciation to those who responded to the call for public review and comment.
This work was supported by a grant from the Department of Practice of the American Physical Therapy Association.
Dr Shubert is part owner of the Evidence in Motion Fall Prevention Application available for the Android and iPhone/iPad platforms.
References
- 1. Sackett DL, Rosenberg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312:71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Institute of Medicine. Clinical Practice Guidelines We Can Trust. Washington, DC: National Academies Press; 2011. Available at: http://www.iom.edu/reports/2011/clinical-practice-guidelines-we-can-trust.aspx Accessed November 30, 2013. [Google Scholar]
- 3. National Guideline Clearinghouse, Agency for Healthcare Research and Quality, US Department of Health & Human Services. Guideline Syntheses. Available at: http://www.guideline.gov/syntheses/index.aspx Accessed November 30, 2013.
- 4. Centers for Disease Control and Prevention. The Cost of Falls Among Older Adults. 2012. Available at: http://www.cdc.gov/HomeandRecreationalSafety/Falls/fallcost.html Accessed December 1, 2012.
- 5. Adams PE, Martinez ME, Vickerie JL, Kirzinger WK. Summary health statistics for the US population: National Health Interview Survey, 2010. Vital Health Stat 10. 2011;251:1–117. [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention. Cost of Fall Injuries in Older Persons in the United States, 2005. Available at: http://www.cdc.gov/homeandrecreationalsafety/Falls/data/cost-estimates-figures1-2.html Accessed September 3, 2013.
- 7. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). Available at: http://www.cdc.gov/injury/wisqars Accessed March 4, 2014.
- 8. When I'm 64: How Boomers Will Change Health Care. Chicago, IL: American Hospital Association; 2007. [Google Scholar]
- 9. Guide to Physical Therapist Practice 3.0. Alexandria, VA: American Physical Therapy Association; 2014. Available at: http://guidetoptpractice.apta.org/. [Google Scholar]
- 10. American Physical Therapy Association. Minimum Required Skills of Physical Therapist Graduates at Entry-Level. BOD P11–05-20-49. Available at: http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/BOD/Education/MinReqSkillsPTGrad.pdf Accessed November 30, 2013.
- 11. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. [DOI] [PubMed] [Google Scholar]
- 12. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(suppl 2):ii37–ii41. [DOI] [PubMed] [Google Scholar]
- 13. Campbell AJ, Robertson MC. Rethinking individual and community fall prevention strategies: a meta-regression comparing single and multifactorial interventions. Age Ageing. 2007;36:656–662. [DOI] [PubMed] [Google Scholar]
- 14. Sherrington C, Whitney JC, Lord SR, et al. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56:2234–2243. [DOI] [PubMed] [Google Scholar]
- 15. Deandrea S, Lucenteforte E, Bravi F, et al. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658–668. [DOI] [PubMed] [Google Scholar]
- 16. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention. STEADI (Stopping Elderly Accidents, Deaths, and Injuries) Tool Kit for Health Care Providers. Available at: http://www.cdc.gov/homeandrecreationalsafety/Falls/steadi/index.html. Updated April 11, 2013 Accessed September 3, 2013.
- 18. Moyer VA; US Preventive Services Task Force. Prevention of falls in community-dwelling older adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:197–204. [DOI] [PubMed] [Google Scholar]
- 19. National Institute for Health and Care Excellence. Falls: assessment and prevention of falls in older people. NICE Clinical Guideline 161. June 2013. Available at: http://www.nice.org.uk/guidance/CG161 Accessed July 9, 2013. [PubMed]
- 20. American Geriatrics Society (AGS) and British Geriatrics Society (BGS) Panel on the Clinical Practice Guideline for the Prevention of Falls in Older Persons. AGS/BGS Clinical Practice Guideline: Prevention of Falls in Older Persons. 2010. Available at: http://www.geriatricscareonline.org/ProductAbstract/updated-american-geriatrics-societybritish-geriatrics-society-clinical-practice-guideline-for-prevention-of-falls-in-older-persons-and-recommendations/CL014 Accessed March 20, 2015.
- 21. Hauer K, Lamb SE, Jorstad EC, et al. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing. 2006;35:5–10. [DOI] [PubMed] [Google Scholar]
- 22. Lamb SE, Jørstad-Stein EC, Hauer K, Becker C; for the Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53:1618–1622. [DOI] [PubMed] [Google Scholar]
- 23. Brouwers M, Kho ME, Browman GP, et al. ; for the AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in healthcare. Can Med Assoc J. 2010;182:E839042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. AGREE. Available at: http://www.agreetrust.org/resource-centre/agree-ii-training-tools/ Accessed February 16, 2015.
- 25. Goodwin V, Briggs L; for the AGILE Falls Guidelines Working Group. Guidelines for the physical therapy management of older people at risk of falling. AGILE: Chartered Physiotherapists Working With Older People. August 2012. Available at: http://agile.csp.org.uk/documents/guidelines-physiotherapy-management-older-people-risk-falling?networkid=338430 Accessed October 13, 2012.
- 26. Beauchet O, Dubost V, Revel-Delhom C, et al. How to manage recurrent falls in clinical practice: Guidelines of the French Society of Geriatrics and Gerontology. J Nutr Health Aging. 2011;15:79–84. [DOI] [PubMed] [Google Scholar]
- 27. Moreland J, Richardson J, Chan DH, et al. Evidence-based guidelines for the secondary prevention of falls in older adults. Gerontology. 2003;49:93–116. [DOI] [PubMed] [Google Scholar]
- 28. International Classification of Functioning, Disability and Health (ICF). Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 29. Podsiadlo D, Richardson S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. [DOI] [PubMed] [Google Scholar]
- 30. Berg K, Wood-Dauphinée S, Williams JI, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–311. [Google Scholar]
- 31. Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–126. [DOI] [PubMed] [Google Scholar]
- 32. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17:37–49. [DOI] [PubMed] [Google Scholar]
- 33. Fritz S, Lusardi M. White paper: “walking speed: the sixth vital sign.” J Geriatr Phys Ther. 2009;32:2–5. [PubMed] [Google Scholar]
- 34. US Preventive Services Task Force. Available at: http://www.uspreventiveservicestaskforce.org Accessed December 1, 2013.
- 35. Lesser LI, Krist AH, Kamerow DB, Bazemore AW. Comparison between US Preventive Services Task Force recommendations and Medicare coverage. Ann Fam Med. 2011;9:44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Centers for Medicare and Medicaid Services. CMS 2012: 2010 Reporting Experience Including Trends (2007-2011): The Physician Quality Reporting System and Electronic Prescribing (eRX) Incentive Program. 2012;3 Available at: http://www.facs.org/∼/media/files/advocacy/pqrs/2013/2010experience%20report.ashx Accessed February 16, 2015.
- 37. Macfarlane DJ, Chou KL, Cheng YH, Chi I. Validity and normative data for thirty-second chair stand test in elderly community-dwelling Hong Kong Chinese. Am J Hum Biol. 2006;18:418–421. [DOI] [PubMed] [Google Scholar]
- 38. Rossiter-Fornoff JE, Wolf SL, Wolfson LI, et al. A cross-sectional validation study of the FICSIT common database static balance measures. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Gerontol A Biol Sci Med Sci. 1995;50:M291–M297. [DOI] [PubMed] [Google Scholar]
- 39. Li F, Harmer P, Fisher KJ, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60:187–194. [DOI] [PubMed] [Google Scholar]
- 40. Clemson L, Cumming RG, Kendig H, et al. The effectiveness of a community-based program for reducing the incidence of falls in the elderly: a randomized trial. J Am Geriatr Soc. 2004;52:1487–1494. [DOI] [PubMed] [Google Scholar]
- 41. Campbell AJ, Robertson MC, Gardner MM, et al. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Thomas S. Does the Otago Exercise Programme reduce mortality and falls in older adults? a systematic review and meta-analysis. Age Ageing. 2010;39:681–687. [DOI] [PubMed] [Google Scholar]
- 43. Guidelines International Network. Available at: http://www.g-i-n.net/ Accessed December 4, 2013.
- 44. Rehabilitation Measures Database. Available at: http://www.rehabmeasures.org/default.aspx Accessed December 4, 2013.
- 45. American Physical Therapy Association. Outcome Measures in Patient Care. Available at: http://www.apta.org/OutcomeMeasures/ Accessed July 13, 2014.