Abstract
Highly pathogenic avian influenza (HPAI) H5N1 epidemics in poultry cause huge economic losses as well as sporadic human morbidity and mortality. Vaccination in poultry has often been reported as being ineffective in preventing transmission and as a potential driving force in the selection of immune escape mutants. We conducted transmission experiments to evaluate the transmission dynamics of HPAI H5N1 strains in chickens vaccinated with high and low doses of immune escape mutants we have previously selected, and analysed the data using mathematical models. Remarkably, we demonstrate that the effect of antigenic distances between the vaccine and challenge strains used in this study is too small to influence the transmission dynamics of the strains used. This is because the effect of a sufficient vaccine dose on antibody levels against the challenge viruses is large enough to compensate for any decrease in antibody titres due to antigenic differences between vaccine and challenge strains. Our results show that at least under experimental conditions, vaccination will remain effective even after antigenic changes as may be caused by the initial selection in vaccinated birds.
Keywords: highly pathogenic avian influenza, H5N1, transmission, antigenic distance, vaccine dose
1. Introduction
Highly pathogenic avian influenza (HPAI) H5N1 virus originally emerged in 1996 in Guangdong province, People's Republic of China (hereafter referred to as China), when it rapidly transmitted within poultry populations and caused sporadic human fatalities [1,2]. Since then it has spread globally and has become endemic in several parts of the world, which is unique for a HPAI strain. The virus transmits efficiently both within and between poultry flocks and infection leads to severe disease resulting in up to 100% mortality.
Controlling HPAI H5N1 infection and transmission by applying strict control measures such as culling of infected poultry and pre-emptive culling, has a devastating effect on the economy, while also carrying an ethical dilemma. On the other hand, control measures against HPAI H5N1 are important not only for the survival of the poultry industry, but also because of its transmission potential to humans. The World Health Organization (WHO) reports 844 confirmed cases of transmission of H5N1 to humans to date (September 2015), 449 of which were fatal, more than ever reported for any other HPAI strain [3]. As a result, HPAI H5N1 is considered one of the most likely candidates for a new pandemic influenza [4]. Controlling the spread of HPAI H5N1 therefore is of paramount importance.
In the case of human influenza, worldwide vaccination of risk groups against seasonal influenza is recommended and variously implemented. In poultry, however, vaccination against avian influenza is not as common. A number of countries (i.e. China, Hong Kong SAR, Vietnam, Indonesia, South Korea, Mexico, Pakistan and Egypt) have used or continue to use vaccination programmes in their fight against H5N1 avian influenza. Nevertheless, in most cases, vaccination programmes appear to be ineffective, since new infections take place constantly and antigenic variants able to escape vaccination-induced immunity appear to arise [4–8]. Studies have shown that these field observations are not necessarily all due to vaccine failure but can also be due to problems concerning the application of vaccination [4–13]. These application issues result in inadequate herd immunity, which in turn leads to insufficient protection against infection and to (further) selection of escape mutants [14–17].
Vaccine efficacy depends on antigenic distance between vaccine and challenge strains, as well as other factors such as antigen content, adjuvant, administration procedure, vaccine coverage, etc. [15,18–20]. These factors determine whether or not vaccination protects against transmission by determining the population distribution of vaccination-induced immunity, usually measured by the haemagglutination inhibition (HI) assays. The antigenic distance between two viruses is the average difference in antibody titre when sera raised against one virus (i.e. the vaccine) are tested against both the same vaccine virus and the (different) circulating field virus. The distribution of HI titres is characterized by their mean and variance, the latter reflecting the differences in an individual's antibody response to the same vaccination. HI titre distribution determines whether or not herd immunity (R < 1) is attained, R being defined as the average number of new cases of an infection caused by one typical infected individual, in a population consisting of ‘susceptible’ (i.e. not infected in the case of vaccinated animals) individuals only [21]. As a consequence, if vaccination is not adequate, it will fail to elicit protective herd immunity, thus giving a false sense of security. Furthermore, it is believed that if the antigenic distance between the vaccine and challenge strains is large, the former may not be able to protect against transmission of the latter. Our hypothesis is that vaccine escape occurs when—because of a large antigenic distance between vaccine and field strain—the herd immunity (R < 1) against the field strain is not attained anymore, whereas at the start of the vaccination, the vaccine did result in herd immunity to the then circulating (parent) virus(es).
The goals of this study therefore are to examine and quantify the effect of different HI titres on virus transmission, where these differences in HI titres are induced by antigenically different vaccine and challenge strains and by two different vaccine doses. To achieve these goals, we have conducted a series of transmission experiments, in which we vaccinated animals with a high and a low dose of vaccines made from the selected escape mutants described in [22,23], the two HPAI H5N1 parent strains (A/turkey/Turkey/1/2005 and A/Cygnus cygnus/Germany/R65/2006) from these two studies [22,23], and an HPAI H5N2 virus (A/Chicken/Pennsylvania/1370/1983, hereafter H5N2) that is known to be very antigenically different from the two HPAI H5N1 parent strains. The high dose used is typical of a single commercial vaccine dose used in the field, whereas the low dose simulates poor vaccination in the field. We then challenged these animals with the parent strains. We used the data from these experiments to characterize the antibody titre distribution with respect to the relevant challenge strain and the effect of titre on the transmission parameters infectivity and susceptibility. As a model for the effects of antibody titre distributions on transmission, we use a threshold model. With this threshold model, the population of vaccinated hosts is sorted in hosts with low (below threshold) titres against the challenge strain and those with high (above threshold) titres against the challenge strain. Thus, the distribution of antibody titres can be characterized by the fraction of the hosts with high titres in a population where all hosts are vaccinated with the same vaccine. The optimal threshold value has to be determined from the transmission experiments and the effect on the susceptibility and/or on the infectivity of hosts having a high titre rather than a low titre have to be estimated.
2. Material and methods
2.1. Experimental studies
2.1.1. Viruses
In the two transmission experiments described in this report, a total of six different strains were used, originating from two separate in vitro selection experiments, performed independently at the CVI [22] and at the Friedrich Löffler Institute (FLI) [23]. Briefly, the CVI mutants were the outcome of 42 rounds of selection under immune pressure from continuously increasing concentrations of homologous polyclonal sera and passaging in 9–11-day-old specific pathogen-free embryonated chicken eggs (SPF ECEs). The CVI viruses included the parent strain used for our mutant-selection experiments (HPAI H5N1 A/turkey/Turkey/1/05, hereafter H5N1 t/T), the last passage CVI mutant t/T-P42, and the antigenically distinct HPAI H5N2 (H5N2). The latter strain was sent to our laboratory from the USDA (Ames, Iowa) in 1984. A detailed description of the CVI mutants and the genetic and antigenic differences between all the strains used in this study can be found in [22]. Briefly, five amino acid mutations were identified in the haemagglutinin (HA) protein of our latest mutant (t/T-P42), and we calculated the antigenic distance between this mutant and the parent strain H5N1 t/T to be 4.5 (22.17) HI units. The strains from FLI included the parent strain HPAI H5N1 A/Cygnus cygnus/Germany/R65/1/2006 (H5N1 R65), and the mutants R65-P18 and R65-P30. Three and eight amino acid mutations were identified in the HA protein of the R65-P18 and R65-P30 mutants, respectively. We have calculated the antigenic distances between the FLI parent strain H5N1 R65 and the R65-P18 and R65-P30 mutants to be 6.23 (22.64) and 9.83 (23.30) HI units, respectively. The HA genes of all the strains used in this study were sequenced and no differences were found with the published sequences. The HA sequence of the t/T-P42 mutant is published in NCBI GenBank (accession number KF042153). The HA sequences of the FLI R65-P18 and R65-P30 mutants are published in EpiFlu (accession numbers EPI287212 and EPI287220, respectively).
2.1.2. Inactivation of strains
All strains were inactivated with 0.02% paraformaldehyde (Merck) for 16 h at 37°C. HA assays were performed on the inactivated viruses to determine the HA titre after inactivation and compare it with the HA titre before inactivation. Complete inactivation was verified by two passages in 9-day-old SPF ECEs lasting 7 days each, followed by HA assays at the end of each passage to check for the presence of virus in the allantoic fluid. The inactivation was considered successful when no virus was detected after the end of each passage.
2.1.3. Transmission experiments
All animals used in the transmission experiments described here were SPF white leghorn chickens, derived from SPF ECEs that were hatched and raised in our HCU facilities. The ECEs were obtained from Charles Rivers Avian Vaccine Services. All animals were housed and handled in accordance to European Union Directive 2010/63/EU on the protection of animals used for scientific purposes, in a way that promoted natural behaviours, including social interaction, foraging and exercise. Water was provided through nipple drinkers or drinking towers and was controlled and changed daily. Appropriate food was provided ad libitum. Bedding (wood shavings) was removed at the end of the experiment. All animals were housed separately according to group (i.e. one group/room). Inside each room, the animals were placed in a cage (0.75 × 0.97 m) on the floor.
2.1.4. Transmission Experiment 1: high vaccine dose
Four groups of animals were used. Each group consisted of 10 three-week-old SPF chickens, of which five would be inoculated (designated I) and five would be contacts (designated S for susceptible).
All 10 animals of each group (except the unvaccinated group) were vaccinated intra-muscularly (i.m.) in the leg muscle at three weeks of age with 0.5 ml of 128 (27) HA units (HAU) of inactivated virus in the presence of a water-in-oil emulsion adjuvant (Stimune, Prionics) at a 4 : 5 (v/v) inactivated virus-to-Stimune ratio. The strains used for vaccination were the parent strain H5N1 R65 and the R65-P18 and R65-P30 mutants. Animals belonging to the unvaccinated group were injected i.m. with 0.5 ml of negative allantoic fluid in the presence of the adjuvant (Stimune, Prionics) at a 4 : 5 (v/v) negative allantoic fluid-to-Stimune ratio. The groups were housed separately and were checked twice a day. Two weeks post-vaccination (p.v.), at five weeks of age, 2 ml of blood were taken from each animal and sera were prepared. The sera were inactivated at 56°C for 50 min and stored at −20°C.
On the same day (i.e. two weeks p.v.), five animals per group were challenged with 105 TCID50/0.2 ml (0.1 ml intra-nasally and 0.1 ml intra-tracheally) of the H5N1 R65 virus. Twenty-four hour post-inoculation (p.i.), the five contact animals/group were added.
Trachea and cloaca swabs were taken at days 1–7, 10 and 14 p.i. On day 1 p.i., swabs were collected only from the inoculated animals and collection took place before the addition of the contact animals.
The animals were checked twice a day (including during the days that sampling was not scheduled) for signs of morbidity and mortality. Animals found dead had a cloaca swab taken before being removed from their group. The experimental protocol made provisions for euthanasia of critically ill animals according to Dutch and European Union Law. Before these animals would be euthanized and removed from their group, trachea and cloaca swabs would be collected.
At the end of the experiment (14 days p.i.), trachea and cloaca swabs as well as 5 ml of blood were collected from all surviving animals. The animals were then euthanized, concluding the experiment.
2.1.5. Transmission Experiment 2: low vaccine dose
Seven groups of animals were used. Each group consisted of 10 three-week-old SPF chicken (five inoculated and five contacts).
For vaccination, the same procedure as described for Transmission Experiment 1 was followed. This time, the vaccine dose was lowered to 4 (22) HAU. The strains used for vaccination were the two parent strains H5N1 R65 and H5N1 t/T, the mutants R65-P30 and t/T-P42 and the antigenically distant H5N2. Animals belonging to the unvaccinated control groups were treated as described for Transmission Experiment 1. The animals were housed in four stables (two groups per stable), separated by a barrier and were checked twice a day. Two weeks p.v. sera were collected as described in Transmission Experiment 1.
Challenge of the animals took place as described in Transmission Experiment 1. Groups 5–8 were challenged with H5N1 R65 and Groups 9–11 with H5N1 t/T. Twenty-four hours p.i., the five contact animals/group were added.
Sampling and euthanasia protocols remained the same as described in Transmission Experiment 1. The experiment was terminated at 14 days p.i.
2.1.6. Haemagglutination inhibition assays
The inactivated sera collected from both transmission experiments were used in HI assays [24,25] in which sera were cross-checked against 8 (23) HAU of the vaccine and challenge strains in order to evaluate the cross-reactivity. The assays took place in duplicate.
2.1.7. RNA isolation from trachea and cloaca swabs
Viral RNA was isolated from the swabs taken throughout the transmission experiment by using the BioRobot 8000 (QIAGEN) for Transmission Experiment 1 and the MagNA Pure 96 system (Roche Applied Sciences) for Transmission Experiment 2. The kits used for RNA isolation were the RNeasy 96 (QIAGEN) for the BioRobot 8000 and the MagNA Pure DNA and Viral RNA Small Volume kit (Roche Applied Sciences) for the MagNA Pure 96 system. Both protocols were used as per the manufacturer's instructions.
2.1.8. Viral RNA quantitation from trachea and cloaca swabs
To quantitate the number of viral RNA copies present in the swabs collected during the duration of the transmission experiments, quantitative real-time reverse transcriptase PCR (qPCR) was used (Mx-3005P, Stratagene). The qPCR protocol and AI probe used were optimized to be specific to the M gene of influenza A viruses, which is highly conserved. In total, 45 cycles of amplification were used. Standard curves comprising of serial dilutions of the challenge strains (ranging from 10−3 to 10−10) were prepared and the quality of the standard curves was checked in the Mx3005P. All standard curves had r2-values of 0.999–1.000. The results from the quantitative PCR were analysed using the MxPro software (Stratagene). All trachea or cloaca samples were considered positive if they were found to have a Cycle Threshold (Ct) value by qPCR.
2.2. Statistical analysis and mathematical models
The following definitions need to be stated before describing the mathematical models and statistical analysis. All contact animals are defined as ‘susceptible’ (S). All inoculated animals and any contact animals that become infected throughout the course of the experiments are defined as ‘infectious' (I) from the first day they are found to be qPCR-positive for influenza, until the last day a positive sample was found. Every time a contact animal becomes infected, this is defined as a ‘case’. After an infected animal stops shedding virus, it is defined as ‘recovered’ (R). ‘Homogeneous mixing’ refers to the fact that due to the experimental set-up, all animals (infectious and susceptible) are in (random) contact with one another.
2.2.1. Model for calculating the effect of antigenic differences on the transmission of H5N1 t/T and H5N1 R65 viruses
The reproduction ratio (R) was used as a measure for the transmission between individuals [21]. We use R rather than R0, as the measure may refer to a population of vaccinated individuals in this study. R was estimated based on the SIR stochastic model, using generalized linear models (GLM) and the statistical software STATA (v. 10). R is the quotient of the infection rate parameter (β) and the recovery rate parameter (α), R = β/α.
Susceptible individuals in a population with susceptible (but possibly vaccinated) animals (S) and infectious animals (I) become infected with a rate of β(I/N). The probability that a susceptible individual becomes infected during a time interval Δt is given by Velthuis et al. [26] as
| 2.1 |
For the GLM analysis, a complementary loglog link function (ln[−ln(1 − p)]) is used with the binomial distribution as the error term. Thereby, equation (2.1) is transformed into a linear relationship with the dependent variable being the number of cases (C) divided by the binomial total, i.e. the number of susceptible (S), and offset ln(IΔt/N).
The GLM analysis estimates ln(β), its confidence intervals and standard error. Thus, by exponentiation, β can be calculated. The average infectious period (T) of all infected animals and corresponding confidence intervals can be directly calculated from the data. Briefly, for the calculation of the infectious period we counted the days that each animal was found to be qPCR-positive for influenza virus. All inoculated animals were considered positive for influenza from day 1 p.i. In the very few isolated instances in which an animal was found to be qPCR-negative for influenza on a day, although it was found qPCR-positive before and after that day, that animal was considered positive on that particular day.
We estimated ln(R) and its confidence bounds, and from that, R and its confidence bounds were calculated. The variance and confidence intervals of the estimator ln(R) can be calculated by the following equations, assuming independence of ln(β) and ln(T) [27]:
| 2.2 |
and
| 2.3 |
where T = 1/α.
2.2.2. Model for calculating the effect of host immunity on the transmission of H5N1
We examined whether the population distribution of HI titres can be used to predict transmission of H5N1 t/T and H5N1 R65, in populations vaccinated with antigenically different virus strains and different vaccine doses. To do this, we used the GLM analysis for a heterogeneous population, by dividing the animals into low and high HI titre groups. Animals were assigned to the low group if sera from these animals had HI titres of <8 (23) HI units (HIU) against the challenge strain and to the high group if the HI titre of their sera was ≥8 (23) HIU against the challenge strain. This threshold of 8 HIU was also evaluated (see Results section). Animals from the unvaccinated groups were included in the low group since we assume that chickens with the same HI titre have the same transmission characteristics. The impact of this assumption was tested with a sensitivity analysis (i.e. by leaving the unvaccinated animals out of the analysis).
We estimated the four possible transmission rate parameters for a population of animals having high or low HI titres against the challenge strain in one model, essentially as described in [28]. This model takes into account the differences in both infectivity and susceptibility of the animals with low and high titres against the challenge strain. The dependent variable is the number of new cases C, the binomial total is the number of all susceptible individuals (either from high or low HI titre groups) and explanatory variables the dummy variable Shigh (value 0 or 1) that is an indicator for the type of susceptible (recipient) animal, and Fhigh as the proportion of infected individuals with high titres against the challenge strain. When Shigh = 1 then the dependent variable is the number of new cases of the susceptible high and binomial total the number of susceptible high and when Shigh = 0 then dependent variable is the number of new cases of susceptible low and binomial total the number of susceptible low.
Therefore, the equation for the model is
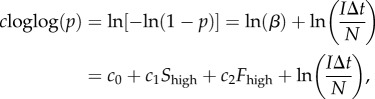 |
2.4 |
where p is the dependent variable, given by the number of cases (C) divided by the number of susceptible (S) (as mentioned above), Fhigh is the fraction of infectious animals with high HI titres against the challenge strain and c0, c1 and c2 are the regression coefficients.
The four βs can then be calculated from the GLM analysis by the estimated regression coefficients, as defined by equation (2.4)
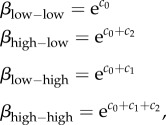 |
where high–low means from high titre infectious animals to low titre recipients and mutatis mutandis for the rest.
The transmission rate parameter can also be written as the product of infectivity (f), susceptibility (g) and with an extra constant c for the overall transmission rate (β = c × f × g). If we take as a reference that the infectivity and susceptibility of animals with low titres equals to 1, then by including the dummy variable Shigh in equation (2.4), we account for the aforementioned assumption and we can calculate the relative infectivity and susceptibility of animals with high titres. This implies that c1 is ln(g) and c2 is ln(f). As there are two types of individuals, there are also two values both for f and g (where the value of low is 1), leading to four combinations. As a consequence, the dynamics are determined by a two-by-two next generation matrix and the R is the dominant eigenvalue of this matrix, for which we assume separable mixing, as explained in detail by Diekmann et al. [21,29]. Therefore, the R is
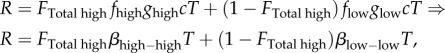 |
2.5 |
where FTotal high is the fraction of the total susceptible population with a high HI titre against the challenge strain.
We evaluated the fit of models (also for different threshold values for the HI titres) by comparing the Akaike information criterion (AIC) values of the models and the predicted values that each model has estimated with the observed values, according to the formula AIC = 2k − 2ln(L), where k is the number of parameters in the statistical model and L is the is the maximized value of the likelihood function for the estimated model [30–32].
2.2.3. Calculation of probability distribution of haemagglutination inhibition titres
We created a model to examine the probability distribution of the HI titres of a single individual, bearing in mind the antigenic distance between vaccine and challenge strain (as calculated in [22]) and the vaccine dose. For this model, we assume a Gaussian distribution. Thus, the model used is as follows:
| 2.6 |
where y is the predicted HI titre, AD is the antigenic distance between vaccine and challenge strain (as calculated in [22]) and is measured in HI units, VD is the vaccine dose (measured in HA units), C0, C1 and C2 are the regression coefficients (C0 is the intercept, C1 is the effect of the AD, and C2 is the effect of VD) and e is the variance (its estimated value depending on the variances and covariances for the estimates of C0, C1 and C2). For the high-dose transmission experiment VD = 1 and for the low-dose transmission experiment VD = 0.
We then calculated the probability distribution that any k number of animals within a group vaccinated against any of the strains used will have a HI titre of ≥8 HIU against the challenge strain (k ranging from 0 to 10 animals). This distribution is binomial with n = 10 and the p is the fraction of the population with a titre <8 (23) HIU, calculated from the Gaussian distribution as shown in equation (2.6) with coefficients (C0, C1, C2) and variance (e), the estimation of which has been described above.
Finally, we calculated the probability that R > 1, which equals to the probability that k > kcritical (kciritical to be determined from the transmission parameters) for each one of the groups in the high and low vaccine dose transmission experiments. Note that the critical fraction needed to bring R > 1 follows from equation (2.5), solving for FTotal high which can be done after having calculated the transmission parameters βhigh–highT and βlow–lowT, which in turn are the R for the high and low HI titre groups, respectively.
3. Results
3.1. Transmission experiments
3.1.1. Transmission Experiment 1: high vaccine dose (128 HAU)
The HI assays performed on sera obtained from all vaccinated animals and checked against the challenge strain H5N1 R65 showed high HI titres (electronic supplementary material, tables S1–S3). HI assays in which the same sera were checked against the homologous vaccine strains, consistently gave slightly higher titres (electronic supplementary material, tables S1–S3). The larger the antigenic distance between vaccine and challenge strains, the larger the difference in HI titres obtained from homologous and heterologous viruses.
After challenge infection, all animals (inoculated and contacts) in the unvaccinated control group (Group 4) died early in the experiment, consistent with the highly pathogenic nature of the H5N1 R65 challenge strain (electronic supplementary material, table S4). In this group, all contact animals became infected and shed virus until the day they died. The Ct values from these animals were low, indicating high virus load (electronic supplementary material, table S15).
By contrast, no animal deaths were observed in the vaccinated groups (Groups 1–3) after challenge infection. From the vaccinated inoculated animals found to be qPCR-positive for influenza virus, most were so only on day 1 p.i. (electronic supplementary material, tables S1–S3). Only two inoculated animals were found to be qPCR-positive for influenza on day 3 p.i. (Groups 1 and 2, one animal each). The Ct values obtained from qPCR-positive vaccinated inoculated animals in the vaccinated Groups 1–3 were high, indicating very low virus load (electronic supplementary material, tables S12–S14).
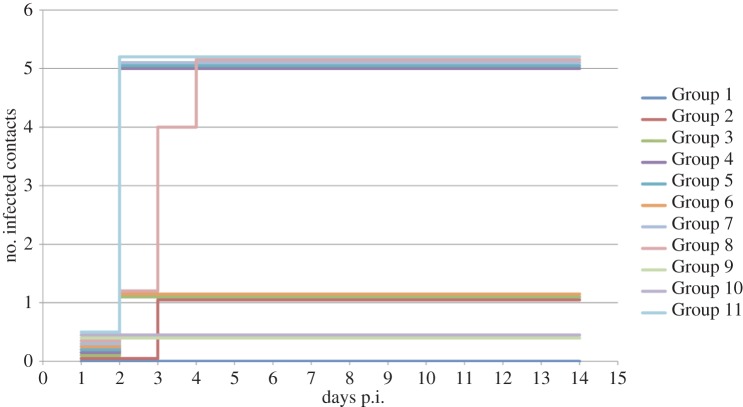
Only two vaccinated contact animals were found to be qPCR-positive for influenza virus (Groups 2 and 3, one animal each). These animals were found to be qPCR-positive for 1 day only (electronic supplementary material, tables S2 and S3). The Ct values of these vaccinated contact animals were high, indicating very low virus load (electronic supplementary material, tables S13 and S14). A graphic representation of the progress of infection in the contact animals for each day p.i. is shown in figure 1.
Figure 1.
Observed progress of contact animal infections. Progress of infection of contact animals (according to qPCR-positive swabs) per group per day. Contact animals were added on day 1 p.i., immediately after sampling (trachea and cloaca swabs) of the inoculated animals took place.
3.1.2. Transmission Experiment 2: low vaccine dose (4 HAU)
The HI assays performed on sera obtained from all vaccinated animals (inoculated and contacts) and cross-checked against the challenge strains showed relatively low HI titres (electronic supplementary material, tables S5–S7 and S9–S10). As in Transmission Experiment 1, HI assays in which the same sera were checked against the homologous vaccine strains, consistently gave higher titres and the larger the antigenic distance between vaccine and challenge strains, the larger the difference in HI titres obtained from homologous and heterologous viruses (electronic supplementary material, tables S5–S7 and S9–S10). Times of death and animals found to be qPCR-positive for the presence of influenza virus in tracheal and cloacal swabs are shown in the electronic supplementary material, tables S5–S11.
In the unvaccinated control Groups 8 and 11 (unvaccinated/H5N1 R65 challenged and unvaccinated/H5N1 t/T challenged, respectively), all contact animals became infected. All animals belonging to these groups died during the experiment, consistent with the highly pathogenic nature of the challenge strains H5N1 R65 and H5N1 t/T, respectively.
In Group 5 (H5N1 R65 vaccinated/H5N1 R65 challenged), all contact animals became infected and shed virus (electronic supplementary material, table S5). In Group 6 (R65-P30 vaccinated/H5N1 R65 challenged), only one contact animal appeared to be positive on day 2 p.i. only (i.e. 24 h after being added to the group; electronic supplementary material, table S6). In Group 7 (H5N2 vaccinated/H5N1 R65 challenged), all contact animals became infected and shed virus (electronic supplementary material, table S7). Finally, in Groups 9 and 10 (t/T-P42 vaccinated/H5N1 t/T challenged and H5N1 t/T vaccinated/H5N1 t/T challenged, respectively), no contact animals were found infected, although the inoculated animals were continuously shedding virus until day 5 p.i. and day 10 p.i., respectively (electronic supplementary material, tables S9–S10 and S20–S21). A graphic representation of the progress of infection in the contact animals for each day p.i. is shown in figure 1.
The Ct values of all positive animals in Groups 5–11 are shown in the electronic supplementary material, tables S16–S22. Ct values of samples obtained from animals that died as a result of the infection were low, indicating a high viral load. Furthermore, relatively low Ct values were obtained from all the positive samples found throughout the experiment (especially when comparing these Ct values to those obtained in Transmission Experiment 1).
3.2. Mathematical analysis of transmission dynamics
3.2.1. Transmission dynamics based on separate groups
For each of the 11 groups in the two transmission experiments, transmission was estimated based on the observed infectious and susceptible animals at the start of each time interval and the number of new cases during that time interval.
The estimates from the GLM analysis for each group are shown in table 1 and the dataset used for this analysis is shown in the electronic supplementary material, table S23. For calculations of the infectious period, it was assumed that since the animals were artificially inoculated for the purposes of the experiment, they were actually shedding virus from day 1 p.i. until the last day they were found to be positive by qPCR.
Table 1.
Transmission dynamics based on separate groups (GLM analysis).
| group no. | vaccine strain | challenge strain | β (day−1) (95% CI) | Var(β) | infectious period (day) (95% CI) | R (95% CI) | Var(R) |
|---|---|---|---|---|---|---|---|
| high vaccine dose | |||||||
| 1 | H5N1 R65 | H5N1 R65 | 0 | n.a. | 1.25 (0.48–3.26) | 0 | n.a. |
| 2 | R65-P18 | H5N1 R65 | 0.27 (0.04–1.90) | 2.72 | 1.2 (0.5–2.89) | 0.32 (0.04–2.74) | 3.32 |
| 3 | R65-P30 | H5N1 R65 | 0.38 (0.05–2.69) | 2.73 | 1 | 0.38 (0.05–2.69) | 2.73 |
| 4 | unvaccinated | H5N1 R65 | ∞a | n.a. | 1.37 (0.60–3.17) | ∞a | n.a. |
| low vaccine dose | |||||||
| 5 | H5N1 R65 | H5N1 R65 | ∞a | n.a. | 3.11 (0.77–12.58) | ∞a | n.a. |
| 6 | R65-P30 | H5N1 R65 | 0.11 (0.02–0.81) | 2.72 | 2.17 (0.38–12.47) | 0.25 (0.02–3.43) | 6.02 |
| 7 | H5N2 | H5N1 R65 | ∞a | n.a. | 2.58 (0.42–15.78) | ∞a | n.a. |
| 8 | unvaccinated | H5N1 R65 | 1.66 (0.68–4.07) | 1.23 | 0.91 (0.11–7.45) | 1.51 (0.15–14.85) | 3.88 |
| 9 | t/T-P42 | H5N1 t/T | 0 | n.a. | 3.73 (2.43–5.72) | 0 | n.a. |
| 10 | H5N1 t/T | H5N1 t/T | 0 | n.a. | 5.49 (2.78–10.88) | 0 | n.a. |
| 11 | unvaccinated | H5N1 t/T | ∞a | n.a. | 2.00 (0.41–9.66) | ∞a | n.a. |
aAll contact animals were infected by day 2 p.i. leading to extreme β and R0 values. n.a.: not applicable.
The overall estimate of β and of the average infectious period in an unvaccinated population were 3.14 (CI: 1.80–5.47) day−1 and 1.47 (CI: 0.444–4.84) day, respectively. The calculated estimate of R0 in an unvaccinated population was 4.60 (CI: 1.39–15.2). There were no significant differences in β between different vaccine groups, only differences between high vaccine dose groups compared with low vaccine dose ones.
3.2.2. Transmission dynamics based on haemagglutination inhibition titres
To model the effect of the HI titres on transmission, all animals were classified in either of two categories, based on their HI titre: susceptible low (Slow) and infected low (Ilow), if the HI titre was <8 against the challenge strain and susceptible high (Shigh) and infected high (Ihigh) if the HI titre was ≥8 against the challenge strain. The dataset used for this model appears in the electronic supplementary material, table S24. The value of 8 (23) HIU was used as the best-fitting threshold value after analysing the data with different threshold values (4, 8 and 16 HIU) and using the AIC values as goodness-of-fit parameters. We performed these model comparisons either with all 11 groups, or by excluding the groups in which either all contact animals were immediately infected (Groups 4, 5, 7 and 11), or no contact animals became infected throughout the experiments (Groups 1, 9 and 10). The rationale for this latter comparison is that when parameters are fitted independently for a group in which either all or no recipients are infected, a perfect match can be obtained by taking the probability of infection to be one or zero, respectively. The threshold value of 8 HI units had the smallest AIC value in this analysis (electronic supplementary material, table S25). The average infectious periods (AIP), β and R and their variances were calculated (table 2).
Table 2.
Transmission dynamics based on HI titres. Animals separated into low (<8 HI units) and high (≥8 HI units) HI titres against the challenge strain.
| HI titre | β (day−1) (95% CI) | Var(β) | infectious period (day) (95% CI) | R (95% CI) | Var(R) |
|---|---|---|---|---|---|
| low | 3.73 (2.37–5.85) | 1.04 | 1.78 (0.30–10.67) | 6.63 (1.06–41.5) | 2.40 |
| high | 0.058 (0.01–0.33) | 1.49 | 2.02 (0.47–8.67) | 0.12 (0.017–0.795) | 2.58 |
In the full model, the susceptibility of animals with either low or high HI titres against the challenge strain does not differ, whereas infectivity is significantly lower for animals with high HI titres (table 3). Therefore, we calculated the model again, considering only the effect of infectivity. The infectivity of animals with high HI titres (β = 0.058 d−1, CI: 0.010–0.330) was again much lower when compared with that of animals with low HI titres (β = 3.73 d−1, CI: 2.37–5.85; tables 2 and 3). Animals with high HI titres were thus approximately 64 times less infectious than animals with low HI titres. The estimated transmission parameters for the high and low HI titre groups imply that 86.5% of the population must have high HI titres (≥8 HI units) in order for the R to be below the threshold value of 1. A sensitivity analysis in which the unvaccinated animals were excluded from the analysis so that they were not included in the group of vaccinated animals with low HI titres showed the same results (i.e. no effect on susceptibility and a similarly large and significant effect on infectivity; electronic supplementary material, table S26).
Table 3.
Effect of infectivity and susceptibility on transmission dynamics. The effect of infectivity and susceptibility of animals with low (<8 HI units) or high (≥8 HI units) HI titres against the challenge strain, on the transmission dynamics of the parent strains.
| regression variables | regression coefficient | 95% CI | p-value |
|---|---|---|---|
| model including susceptibility | |||
| constant | 1.32 | (0.85 to 1.79) | 0.000 |
| Shigh | −0.04 | (−1.30 to 1.22) | 0.950 |
| Fhigh | −4.13 | (−5.74 to −2.52) | 0.000 |
| model excluding susceptibility | |||
| constant | 1.32 | (0.86 to 1.77) | 0.000 |
| Fhigh | −4.16 | (−5.43 to −2.88) | 0.000 |
The AIC values of the model based on separate groups and the model based on HI titres were compared and found to be 60.95 and 68.16, respectively. Still, both models explain the variability between the different groups equally well, because comparing only those groups with intermediate outcomes, the same AIC values were found to be 46.95 and 43.11, suggesting a better fit for the model based on HI titres.
3.2.3. Analysis of haemagglutination inhibition titres as a function of vaccine dose and antigenic distance between vaccine and challenge strains
The results from the model calculating the Gaussian distribution of HI titres against the challenge strain of a single individual (given the vaccine dose and antigenic distance between vaccine and challenge strains) are shown in table 4. These results show that the effect of antigenic distance between vaccine and challenge strains on the distribution of individual HI titres is much smaller compared with the effect of vaccine dose.
Table 4.
Effect of vaccine dose and antigenic distance on HI titre distribution in a vaccinated population.
| regression variables | regression coefficient | 95% CI | p-value |
|---|---|---|---|
| constant | 66.61 | (−102.37 to 235.59) | 0.435 |
| antigenic distance (AD) | −1.99 | (−6.60 to 2.63) | 0.394 |
| vaccine dose (VD) | 964.83 | (720.80 to 1208.87) | 0.000 |
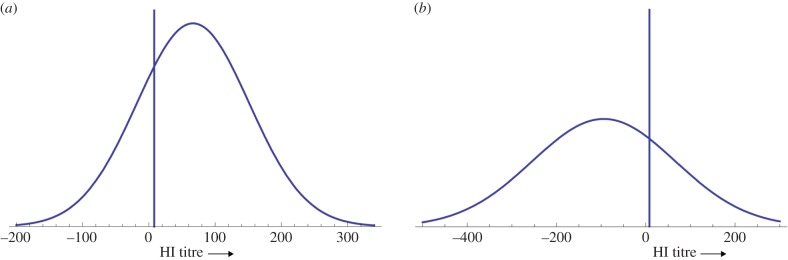
Figure 2a,b shows the Gaussian distribution of HI titres for any individual animal in the low vaccine dose groups exhibiting the smallest (0) and largest (80.88 or 26.34 HIU) antigenic distance, respectively (distances as calculated in [22]). These are the homologous groups 5 (H5N1 R65 vaccinated/H5N1 R65 challenged) and 10 H5N1t/T vaccinated/H5N1 t/T challenged) with an antigenic distance of 0 and Group 7 (H5N2 vaccinated/H5N1 R65 challenged) with an antigenic distance of 80.88 (26.34) HIU.
Figure 2.
Probability density function (PDF) of HI titres of a single individual. Gaussian probability distribution of HI titres against the challenge strain of a single individual in low vaccine dose groups. (a) PDF of the HI titres from a single individual in groups where the vaccine and challenge strain have an antigenic distance of 0 (i.e. homologous groups H5N1 R65 vaccinated/H5N1 R65 challenged and H5N1 t/T vaccinated/H5N1 t/T challenged). (b) PDF of the HI titres from a single individual in a group where the distance between the vaccine and the challenge strain is 80.88 (26.34) HIU (i.e. H5N2 vaccinated/H5N1 R65 challenged). The blue vertical line crosses at HI = 8 units (threshold value calculated by the analysis).
The probability distribution of 0–10 animals of each group having HI ≥ 8 against the challenge strain was calculated (the threshold value of 8 being established from the model based on individual HI titres). From this, we calculated the probability that R > 1. The results from these calculations are shown in the electronic supplementary material, table S27. In summary, we found that for Groups 1–3 (vaccinated groups in the high-dose Transmission Experiment 1), the probability of an individual animal to have HI ≥ 8 is very high (≈1). In the low vaccine dose groups of Transmission Experiment 2, the situation was more diverse. Specifically, in Group 5, the probability of any individual animal having an HI titre ≥ 8 is 0.76, in Group 6, 0.70, in Group 7, 0.26, in Group 9, 0.73 and in Group 10, 0.76 (table 5 and electronic supplementary material, table S27). Regarding the probability that R > 1, this was 0 in Groups 1–3, 0.74 in Group 5, 0.85 in Group 6, ≈1 in Group 7, 0.79 in Group 9 and 0.74 in Group 10.
Table 5.
R calculations based on models with expected/observed fraction and final size.
| group no. | vaccine strain | challenge strain | model with expected fraction |
model with observed fraction |
estimated R |
|||
|---|---|---|---|---|---|---|---|---|
| fraction | R | fraction | R | interval data | final size | |||
| high vaccine dose | ||||||||
| 1 | H5N1 R65 | H5N1 R65 | 1 | 0.12 (0.017–0.795) | 1 | 0.12 (0.017–0.795) | 0 | 0 (<1.64) |
| 2 | R65-P18 | H5N1 R65 | 1 | 0.12 (0.017–0.795) | 1 | 0.12 (0.017–0.795) | 0.32 (0.04–2.74) | 0.38 (0.01–3.22) |
| 3 | R65-P30 | H5N1 R65 | 1 | 0.12 (0.017–0.795) | 1 | 0.12 (0.017–0.795) | 0.38 (0.05–2.69) | 0.38 (0.01–3.22) |
| 4 | unvaccinated | H5N1 R65 | 0 | 6.63 (1.06–41.5) | 0 | 6.63 (1.06–41.47) | ∞ | ∞ (0.84<) |
| low vaccine dose | ||||||||
| 5 | H5N1 R65 | H5N1 R65 | 0.755113 | 1.71 (0.272–10.756) | 0.3 | 4.68 (0.747–29.268) | ∞ | ∞ (0.84<) |
| 6 | R65-P30 | H5N1 R65 | 0.697442 | 2.09 (0.333–13.102) | 0.6 | 2.72 (0.434–17.065) | 0.25 (0.02–3.43) | 0.38 (0.01–3.22) |
| 7 | H5N2 | H5N1 R65 | 0.262287 | 4.92 (0.786–30.801) | 0 | 6.63 (1.06–41.47) | ∞ | ∞ (0.84<) |
| 8 | unvaccinated | H5N1 R65 | 0 | 6.63 (1.06–41.5) | 0 | 6.63 (1.06–41.47) | 1.51 (0.15–14.85) | ∞ (0.84<) |
| 9 | t/T-P42 | H5N1 t/T | 0.732831 | 1.86 (0.296–11.662) | 0.8 | 1.42 (0.226–8.93) | 0 | 0 (<1.64) |
| 10 | H5N1 t/T | H5N1 t/T | 0.755113 | 1.71 (0.272–10.756) | 0.9 | 0.77 (0.121–4.863) | 0 | 0 (<1.64) |
| 11 | unvaccinated | H5N1 t/T | 0 | 6.63 (1.06–41.5) | 0 | 6.63 (1.06–41.47) | ∞ | ∞ (0.84<) |
| group combinations | ||||||||
| 5 and 10 | homologous (low dose) | 0.755113 | 1.71 (0.272–10.756) | — | — | 0.32 (0.13–0.77) | 1.47 (0.30–3.44) | |
| 4,8,11 | unvaccinated | 0 | 6.63 (1.06–41.5) | — | — | 4.60 (1.39–15.2) | ∞ (1.99<) | |
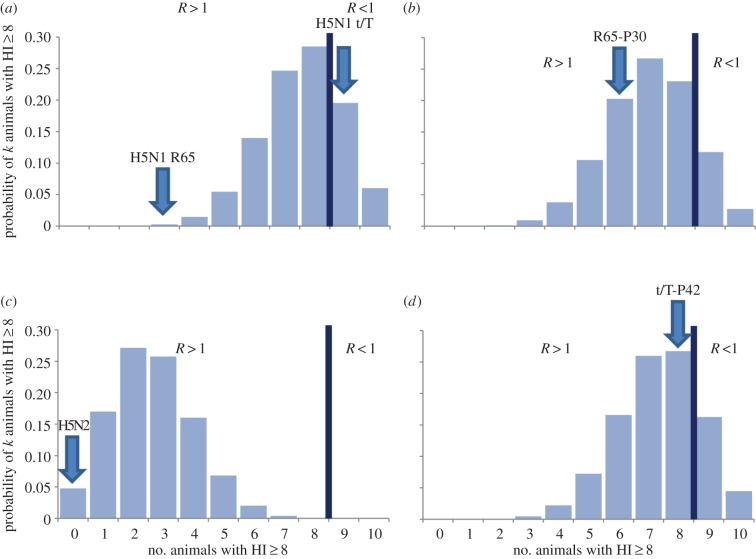
Figure 3a–d shows the graphic representation of the probability distribution for the chance that 0–10 animals in any of the vaccinated groups will have an HI titre ≥ 8 against the challenge strain. Bearing in mind the results from the estimates for the transmission rate parameters from which it was calculated that at least 86.5% of the vaccinated population must have HI titres ≥ 8 in order for R to be less than 1, figure 3a–d incorporates the scenario that nine or more animals will have HI titre ≥ 8.
Figure 3.
Probability distribution of k animals with HI ≥ 8. Probability distribution of 0–10 animals per group with HI ≥ 8. (a) In groups where the vaccine and challenge strains have an antigenic distance of 0 (i.e. homologous groups H5N1 R65 vaccinated/H5N1 R65 challenged and H5N1 t/T vaccinated/H5N1 t/T challenged). (b) In groups where the vaccine and challenge strains have an antigenic distance of 9.83 (23.30) HIU (i.e. R65-P30 vaccinated/H5N1 R65 challenged). (c) In groups where the vaccine and challenge strains have an antigenic distance of 80.88 (26.34) HIU (i.e. H5N2 vaccinated/H5N1 R65 challenged). (d) In groups where the vaccine and challenge strains have an antigenic distance of 4.49 (22.17) HIU (i.e. t/T-P42 vaccinated/H5N1 R65 challenged). The blue vertical line separates the scenarios where R > 1 and R < 1, according to the probability distribution of the number of animals with HI ≥ 8 against the challenge strain. Blue arrows indicate the experimentally observed number of animals with HI ≥ 8 against the challenge strain for each vaccine group.
We calculated the R for each group according to the number of observed animals from each vaccinated group that have HI ≥ 8 against the challenge strain, and consequently the probability for a minor outbreak in each of these groups. The results showed that in the high vaccine dose groups (Groups 1–3) in which all animals had HI titres ≥ 8 against the challenge strain, the R is 0.12 and the probability for a minor outbreak is thus 100%. In the low vaccine dose groups, the results were more diverse due to the different number of animals with HI ≥ 8 against the challenge strain in each group. In detail, in Group 5 (three animals with HI ≥ 8), the R was 4.68 and there was a 21% probability of a minor outbreak in this group. In Group 6 (six animals with HI ≥ 8), the R was 2.72 and the probability of a minor outbreak was 37%. Group 7 (0 animals with HI ≥ 8) had R = 6.63 and a 15% probability of a minor outbreak. Groups 9 and 10 (eight and nine animals with HI ≥ 8, respectively) had the lowest R (1.42 and 0.77, respectively) and consequently the highest probabilities of a minor outbreak (70% and 100%, respectively).
4. Discussion
We have used transmission experiments and mathematical models to study the effect of antigenic distance and vaccination-induced immunity on the transmission dynamics of HPAI H5N1 strains. Furthermore, we examined the combined effect that vaccine dose and antigenic distance have on the distribution of HI titres and how this affects the probability of transmission. To this end, we conducted transmission experiments using two different vaccine doses, a high dose (128 HAU, typical of a single commercial vaccine dose used in the field) and a low dose (4 HAU, to simulate poor vaccination in the field), and with different combinations of vaccine and challenge strains with various antigenic distances between them. In total, we used 11 groups of 10 animals each.
All contact animals became infected and mortality was 100% in the inoculated and contact animals of the unvaccinated control groups, in agreement with the highly pathogenic nature of both challenge viruses and their high transmission rates in unvaccinated individuals [33–35]. The level of protection offered against disease and transmission by the different vaccinations depended mostly on the dose of the vaccine, as it was only in the experiments in which a low vaccine dose was used that the antigenic distance between vaccine and challenge (transmitting) virus seemed to play any role. Our experimental data show that with a low vaccine dose the large antigenic distances that occur between the most extremely different isolates of the same H5 HA type, i.e. H5N1 R65 compared to H5N2 (80.88 or 26.34 HIU as measured in [22]) can play a sufficient role in changing the vaccinated population from not allowing transmission (R < 1) to allowing transmission (R > 1). Our probability distribution studies suggest that the main reason that transmission in such a group occurs is because when a low vaccine dose is used, it is unlikely that ≥86.5% of the vaccinated population will have HI ≥ 8. This however would not be the case if a high vaccine dose were used. Indeed, in our antigenic cartography studies described in [22] in which we vaccinated chickens with 64 (26) HAU of H5N2 vaccine, the immune response was found to be high (1024 or 210 HIU) and when these sera were cross-checked against other strains (including H5N1 R65), no HI titres <8 (23) HIU were obtained. In addition, according to our data, the comparatively smaller differences that occur after several passages in vaccinated animals as mimicked in in vitro selection experiments [22,23], do not lead to sufficient change in the reproduction ratio. This implies that vaccine escape can only occur when transmission of the original virus over a long period of time was already possible due to inadequate vaccination. For example, the Egyptian variant strain discussed in [13,36] is probably much more different than the in vitro selected variants we discuss in this report, as can be seen from the difference in HI titres between the Egyptian parent strain and the variant when checked using the Potsdam/H5N2 sera [13]. It may be speculated that the variant strain was selected after many passages in animals, since field vaccination was applied at the same time that transmission of the viruses continued [37].
In the high vaccine dose groups no transmission was seen, but in the low vaccine dose groups, transmission occurred only in the H5N1 R65 vaccinated/H5N1 R65 challenged and H5N2 vaccinated/H5N1 R65 challenged groups (Groups 5 and 7). Although in theory the former should also be the group with the highest level of protection (since the antigenic distance between vaccine and challenge strain is 0), upon closer inspection, the observed immune responses of the animals in this group were much lower than the ones from other groups, making these animals more infectious. At this point, the chance element needs to be taken into consideration. By chance, a group of animals vaccinated with a low dose may exhibit either low (<8) or high (≥8) HI titres against the challenge strain. Therefore, finding high HI titres in the groups vaccinated with low vaccine doses is not improbable. In addition, if the antigenic distance between vaccine and challenge strain is high, the chance for high HI titres against the challenge strain is lower. This is not the case when a high vaccine dose is used, because the level of HI titres is already sufficiently high for antigenic distances not to play a decisive role.
The immune response of the vaccinated animals (measured in HI titres) is a direct consequence of the vaccine dose used to vaccinate these animals. From both transmission experiments, it became evident that there is strong correlation between high HI titres (≥8 HI units) against the challenge strains and lower infectivity of the inoculated or infected contact animals with such high titres. Since in the high vaccine dose experiment all animals had HI titres ≥8 against the challenge strain, this correlation became more evident in the low vaccine dose experiment, where it was also seen that antigenic distance between vaccine and challenge strains may play a role in transmission, however its effect is small compared with the effect of vaccine dose.
An important finding of this study is that the reduction in R is due to the fact that animals with a high antibody response against the challenge strain (≥8 or 23 HIU) are 64 times less infectious and not because they are less susceptible. Indeed, the susceptibility of the animals was independent of HI titres and the infectious periods did not significantly differ between the two categories of chickens (with high and low HI titres). To come to this conclusion, transmission was estimated between animals with low (<8 HIU) and high antibody response (≥8 HIU) against H5N1 challenge virus. This resulted in four values of the transmission rate parameter. However, the transmission did not depend on the type of the recipient, only on the type of the infectious chickens. Intuitively, if every time for animals in the same group, the two types of animals (high and low HI titre) are infected with the same probability per unit of time, the susceptibility is not different. In addition, if animals in groups that have more low HI titre animals become infected more often than animals in groups with many high HI titre animals, then low HI titre animals are more infectious. Thus, the model based on HI titres is more parsimonious than the model based on separate groups, has less parameters (two instead of 11) and explains the variability between groups more fully, as it attributes it to differences in the levels of immune response between animals.
In the past, it was assumed that the closer the antigenic similarity between vaccine and field strain is, the better the vaccine efficacy is expected to be and the less the chance of selection of novel strains that are antigenically distant from the parent strain and are able to escape vaccination-induced immunity. Indeed, many field studies have attributed the failure of vaccination to prevent infection and transmission of HPAI strains to—among other things—antigenic distances between the vaccine and the circulating field strains, and called for constant vaccine updating, the way it is done for human influenza vaccines [6,7,14,20]. These studies show that use of vaccines that are antigenically distant to the circulating strains led to lack of protection due to low HI titres against the challenge strains. Upon closer examination however, it can be seen (where the data are available) that even HI titres against the vaccine strains were low in these vaccination programmes, thus indicating that the vaccine had failed to induce immunity to begin with [20,37,38]. In addition, reports from the field have emerged in which it is shown that in some cases where vaccination against HPAI is applied nationwide, the population coverage is extremely low, thus allowing transmission to take place in a seemingly vaccinated population [12,14,20]. Therefore, before attributing vaccination failure to antigenic distance, it is important to make certain that the expected level of immunity was actually achieved. Additionally, taking into consideration the previously mentioned evidence of low p.v. titres in some nationwide vaccination programmes, the case against vaccination is challenged further. We believe that although it is important to start a vaccination programme by matching the vaccine strain to the circulating strains as much as possible, if the vaccine raises effective levels of immunity against the challenge strains, it will remain effective even in the face of antigenic distances such as the ones described in our study.
In our study, the antigenic distances between the mutant strains and their parent strains (described in [22]) did not prevent protection of vaccinated animals against infection and did not enable transmission of the parent strain in populations vaccinated against the mutants. Therefore, our results could make vaccination a more attractive measure since the costs associated with constant vaccine updating could be eliminated. It is important to mention that a review of relevant literature shows that the antigenic distances between our laboratory-selected mutants and challenge strains employed in our study are comparable to most antigenic distances observed between vaccine and circulating strains in the field [39–41]. In addition, the most antigenically distant strain used in our study (H5N2) has either been used as a vaccine seed strain or is very similar to other H5N2 strains used in commercial vaccines. Finally, as mentioned in [22] almost all the amino acid mutations found in our laboratory-selected mutants have also been reported in field mutants and most of the mutations are located within known antigenic sites. Therefore, our laboratory-selected mutants are good substitutes for some mutants selected in the field.
Some experimental studies offer indirect evidence that appears to support our hypothesis that a high immune response would protect animals from infection and transmission, even if the antigenic distance between vaccine and challenge strains is high [8,41–48]. Most of these studies, however, involve traditional vaccination/challenge experiments. Although this type of experiment can provide information on whether a vaccine is able to protect animals from morbidity and mortality and allow quantification of virus shedding, it does not offer any information on the vaccine's effectiveness to stop transmission, which is one of the most important aims of vaccination, especially with regard to containing an epidemic. Virus shedding does not necessarily translate to transmission. In other words, these experiments may reflect differences in susceptibility, but do not reflect differences in infectivity. This poses the question of whether vaccination/challenge experiments are useful when the effect of vaccination is expected to be mainly due to differences in infectivity. Therefore, appropriate transmission experiments are needed in order to allow for such differences to be measured and evaluated. To the best of our knowledge, there exist only few experimental studies where transmission was evaluated in birds vaccinated with a strain antigenically distant to the challenge strain [33–35,49,50]. The collective results of these studies show that the high HI titres against the challenge strains obtained in vaccinated animals significantly reduced transmission, even in the face of antigenic distances between vaccine and challenge strains, and thus support our conclusions. It could be that a sufficient level of host immunity achieved by better vaccination can compensate for the antigenic difference between vaccine and field strain [51,52] and prevent the transmission of the latter to animals vaccinated against the former.
Experimental results are corroborated by field studies. Results from countries where vaccination is in place show that if the vaccine coverage and the HI titres of vaccinated animals are high, then vaccination leads to a substantial decrease in transmissibility and infection of animals [17,34,43,53,54]. More studies emerging from the field show that ineffective vaccination has often led to selection of antigenic variants, which spread rapidly because there is in effect no protective immunity [4,5,7,8,14,15,17,55]. We argue that instead of this evidence making a case against vaccination it should provide even more reasons for vaccination to be applied in such a way that high HI titres against the challenge strains can be obtained, since if it is, a sufficient level of herd immunity can be achieved irrespective of the antigenic distance between vaccine and challenge strains that may result from initial selection in vaccinated chickens. More research therefore needs to focus on the quality and application of vaccines in the field. We believe that properly applied vaccination coupled to surveillance and strict biosecurity measures will not only stop transmission, but may also arrest the rate of emergence of antigenic variants.
It is always challenging to extrapolate laboratory results to the field situation. Factors affecting vaccine application and efficiency in a laboratory setting are more effectively controlled than in the field. This is especially so since SPF chickens are used in laboratory experiments, therefore the results are not influenced by issues such as concurrent infections and maternal antibodies, which can affect the level of vaccination-induced immunity. The range of factors that can influence the efficient implementation of a vaccination strategy have already been mentioned in the Introduction. However, socio-economic and political reasons aside, it is important to evaluate which biological factors can substantially influence vaccination in order to prevent transmission of HPAI H5N1 viruses. Our results provide a means of improving vaccination efficiency in stopping transmission of HPAI H5N1, by suggesting evaluation at the start of a vaccination campaign to ascertain whether vaccination is able to stop transmission by estimating both the transmission parameters and the magnitude of HI titres of vaccinated animals to circulating field strains. Furthermore, if vaccination is carried out so that extensive transmission is stopped (R < 1), our results would suggest that the occurrence of new mutants that would be able to transmit in a vaccinated population would be very unlikely.
Supplementary Material
Acknowledgements
The authors would like to acknowledge Dr Riks Maas for his advice, and Rene Heutink, Sandra Venema-Kemper and Diana van Zoelen-Bos for advice in the initial preparation of the transmission experiments.
Ethics
All animal experiments complied fully with Dutch and European Union Law (2010/63/EU) and were reviewed by the Dierexperimenten Commissie (DEC) Animal Sciences Group, Lelystad (animal experiments ethical committee) prior to being carried out. The transmission experiments described in this study were approved by the committee: permit nos. 2010083 and 2011089. Provisions were made in the protocols for appropriate feeding and housing of the animals as well as to ameliorate animal suffering, such as regular monitoring of animal facilities, healthcare of animals and euthanasia of animals by means of cervical dislocation at the end of the experiment (or during the experiment if serious suffering was suspected).
All animal experiments were performed within the High Containment Unit (HCU), in Bio-Safety Level 3+ (BSL3+) facilities at the Central Veterinary Institute (CVI) of Wageningen UR.
Authors' contributions
I.S. performed the experiments. I.S., B.P. and M.C.M.dJ. designed the experiments. I.S. X.R. and M.C.M.dJ. analysed the data, I.S. B.P. and M.C.M.dJ. wrote the manuscript. D.K. and M.B. provided reagents. I.S., X.R., D.K., M.B., B.P. and M.C.M.dJ. read and corrected the manuscript.
Competing interests
We declare we have no competing interests.
Funding
This work was funded by the Economic Structure Enhancement Fund (Fonds Economische Structuurversterking): FES Programme on Avian Influenza.
References
- 1.Peiris JS, de Jong MD, Guan Y. 2007. Avian influenza virus (H5N1): a threat to human health. Clin. Microbiol. Rev. 20, 243–267. ( 10.1128/CMR.00037-06) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu X, Cox NJ, Guo Y. 1999. Genetic characterization of the pathogenic influenza A/Goose/Guangdong/1/96 (H5N1) virus: similarity of its hemagglutinin gene to those of H5N1 viruses from the 1997 outbreaks in Hong Kong. Virology 261, 15–19. ( 10.1006/viro.1999.9820) [DOI] [PubMed] [Google Scholar]
- 3.WHO. 2015. Cumulative number of confirmed human cases for avian influenza A (H5N1) reported to WHO, 2003–2015. [cited 2014 06/07/15]. See http://www.who.int/influenza/human_animal_interface/EN_GIP_20150904cumulativeNumberH5N1cases.pdf?ua=1.
- 4.Smith GJ, et al. 2006. Emergence and predominance of an H5N1 influenza variant in China. Proc. Natl Acad. Sci. USA 103, 16 936–16 941. ( 10.1073/pnas.0608157103) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cattoli G, et al. 2011. Evidence for differing evolutionary dynamics of A/H5N1 viruses among countries applying or not applying avian influenza vaccination in poultry. Vaccine 29, 9368–9375. ( 10.1016/j.vaccine.2011.09.127) [DOI] [PubMed] [Google Scholar]
- 6.Balish AL, et al. 2010. Antigenic and genetic diversity of highly pathogenic avian influenza A (H5N1) viruses isolated in Egypt. Avian Dis. 54(Suppl. 1), 329–334. ( 10.1637/8903-042909-Reg.1) [DOI] [PubMed] [Google Scholar]
- 7.Cattoli G, Milani A, Temperton N, Zecchin B, Buratin A, Molesti E, Aly MM, Arafa A, Capua I. 2011. Antigenic drift in H5N1 avian influenza virus in poultry is driven by mutations in major antigenic sites of the hemagglutinin molecule analogous to those for human influenza virus. J. Virol. 85, 8718–8724. ( 10.1128/JVI.02403-10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee CW, Senne DA, Suarez DL. 2004. Effect of vaccine use in the evolution of Mexican lineage H5N2 avian influenza virus. J. Virol. 78, 8372–8381. ( 10.1128/JVI.78.15.8372-8381.2004) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swayne DE. 2012. Impact of vaccines and vaccination on global control of avian influenza. Avian Dis. 56(Suppl. 4), 818–828. ( 10.1637/10183-041012-Review.1) [DOI] [PubMed] [Google Scholar]
- 10.Swayne DE. 2012. The role of vaccines and vaccination in high pathogenicity avian influenza control and eradication. Exp. Rev. Vaccines 11, 877–880. ( 10.1586/erv.12.60) [DOI] [PubMed] [Google Scholar]
- 11.Pavade G, Awada L, Hamilton K, Swayne DE. 2011. The influence of economic indicators, poultry density and the performance of veterinary services on the control of high-pathogenicity avian influenza in poultry. Revue Sci. Tech. 30, 661–671. [PubMed] [Google Scholar]
- 12.Swayne DE, Pavade G, Hamilton K, Vallat B, Miyagishima K. 2011. Assessment of national strategies for control of high-pathogenicity avian influenza and low-pathogenicity notifiable avian influenza in poultry, with emphasis on vaccines and vaccination. Revue Sci. Tech. 30, 839–870. [DOI] [PubMed] [Google Scholar]
- 13.Grund C, et al. 2011. Highly pathogenic avian influenza virus H5N1 from Egypt escapes vaccine-induced immunity but confers clinical protection against a heterologous clade 2.2.1 Egyptian isolate. Vaccine 29, 5567–5573. ( 10.1016/j.vaccine.2011.01.006) [DOI] [PubMed] [Google Scholar]
- 14.Peyre M, et al. 2009. Avian influenza vaccination in Egypt: limitations of the current strategy. J. Mol. Genet. Med. 3, 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Domenech J, et al. 2009. Experiences with vaccination in countries endemically infected with highly pathogenic avian influenza: the Food and Agriculture Organization perspective. Revue Sci. Tech. 28, 293–305. [DOI] [PubMed] [Google Scholar]
- 16.EMPRES/FAO-GLEWS. 2012. H5N1 HPAI Global overview: January–March 2012. See http://www.fao.org/docrep/015/an388e/an388e.pdf.
- 17.Soares Magalhaes RJ, Pfeiffer DU, Otte J. 2010. Evaluating the control of HPAIV H5N1 in Vietnam: virus transmission within infected flocks reported before and after vaccination. BMC Vet. Res. 6, 31 ( 10.1186/1746-6148-6-31) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kapczynski DR, Swayne DE. 2009. Influenza vaccines for avian species. Curr. Top. Microbiol. Immunol. 333, 133–152. ( 10.1007/978-3-540-92165-3_6) [DOI] [PubMed] [Google Scholar]
- 19.Capua I, Marangon S. 2007. Control and prevention of avian influenza in an evolving scenario. Vaccine 25, 5645–5652. ( 10.1016/j.vaccine.2006.10.053) [DOI] [PubMed] [Google Scholar]
- 20.Capua I, Cattoli G. 2013. Prevention and control of highly pathogenic avian influenza with particular reference to H5N1. Virus Res. 178, 114–120. ( 10.1016/j.virusres.2013.04.002) [DOI] [PubMed] [Google Scholar]
- 21.Diekmann O, Heesterbeek JA, Metz JA. 1990. On the definition and the computation of the basic reproduction ratio R0 in models for infectious diseases in heterogeneous populations. J. Math. Biol. 28, 365–382. ( 10.1007/BF00178324) [DOI] [PubMed] [Google Scholar]
- 22.Sitaras I, Kalthoff D, Beer M, Peeters B, de Jong MC. 2014. Immune escape mutants of highly pathogenic avian influenza H5N1 selected using polyclonal sera: identification of key amino acids in the HA protein. PLoS ONE 9, e84628 ( 10.1371/journal.pone.0084628) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Höper D, Kalthoff D, Hoffmann B, Beer M. 2012. Highly pathogenic avian influenza virus subtype H5N1 escaping neutralization: more than HA variation. J. Virol. 86, 1394–1404. ( 10.1128/JVI.00797-11) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Donald HB, Isaacs A. 1954. Counts of influenza virus particles. J. Gen. Microbiol. 10, 457–464. ( 10.1099/00221287-10-3-457) [DOI] [PubMed] [Google Scholar]
- 25.UN OIE. 2012. Manual of diagnostic tests and vaccines for terrestrial animals (mammals, birds and bees). See http://www.oie.int/manual-of-diagnostic-tests-and-vaccines-for-terrestrial-animals/.
- 26.Velthuis AG, Bouma A, Katsma WE, Nodelijk G, De Jong MC. 2007. Design and analysis of small-scale transmission experiments with animals. Epidemiol. Infect. 135, 202–217. ( 10.1017/S095026880600673X) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klinkenberg D, de Bree J, Laevens H, de Jong MC. 2002. Within- and between-pen transmission of Classical Swine Fever Virus: a new method to estimate the basic reproduction ratio from transmission experiments. Epidemiol. Infect. 128, 293–299. ( 10.1017/S0950268801006537) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Velthuis AG, De Jong MC, Kamp EM, Stockhofe N, Verheijden JH. 2003. Design and analysis of an Actinobacillus pleuropneumoniae transmission experiment. Prev. Vet. Med. 60, 53–68. ( 10.1016/S0167-5877(03)00082-5) [DOI] [PubMed] [Google Scholar]
- 29.Diekmann O, Heesterbeek JA, Roberts MG. 2010. The construction of next-generation matrices for compartmental epidemic models. J. R. Soc. Interface 7, 873–885. ( 10.1098/rsif.2009.0386) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akaike H. 1974. New look at statistical-model identification. IEEE Trans. Automat. Contr. 19, 716–723. ( 10.1109/TAC.1974.1100705) [DOI] [Google Scholar]
- 31.Akaike H. 1980. Likelihood and the Bayes procedure. Trabajos de Estadistica Y de Investigacion Operativa 31, 143–166. ( 10.1007/BF02888350) [DOI] [Google Scholar]
- 32.Burnham KP, Anderson DR. 2004. Multimodel inference: understanding AIC and BIC in model selection. Sociol. Method Res. 33, 261–304. ( 10.1177/0049124104268644) [DOI] [Google Scholar]
- 33.Bouma A, Claassen I, Natih K, Klinkenberg D, Donnelly CA, Koch G, van Boven M. 2009. Estimation of transmission parameters of H5N1 avian influenza virus in chickens. PLoS Pathogens 5, e1000281 ( 10.1371/journal.ppat.1000281) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poetri ON, Bouma A, Murtini S, Claassen I, Koch G, Soejoedono RD, Stegeman JA, van Boven M. 2009. An inactivated H5N2 vaccine reduces transmission of highly pathogenic H5N1 avian influenza virus among native chickens. Vaccine 27, 2864–2869. ( 10.1016/j.vaccine.2009.02.085) [DOI] [PubMed] [Google Scholar]
- 35.van der Goot JA, Koch G, de Jong MC, van Boven M. 2005. Quantification of the effect of vaccination on transmission of avian influenza (H7N7) in chickens. Proc. Natl Acad. Sci. USA. 102, 18 141–18 146. ( 10.1073/pnas.0505098102) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdelwhab EM, Grund C, Aly MM, Beer M, Harder TC, Hafez HM. 2011. Multiple dose vaccination with heterologous H5N2 vaccine: immune response and protection against variant clade 2.2.1 highly pathogenic avian influenza H5N1 in broiler breeder chickens. Vaccine 29, 6219–6225. ( 10.1016/j.vaccine.2011.06.090) [DOI] [PubMed] [Google Scholar]
- 37.Hafez MH, Arafa A, Abdelwhab EM, Selim A, Khoulosy SG, Hassan MK, Aly MM. 2010. Avian influenza H5N1 virus infections in vaccinated commercial and backyard poultry in Egypt. Poultry Sci. 89, 1609–1613. ( 10.3382/ps.2010-00708) [DOI] [PubMed] [Google Scholar]
- 38.Desvaux S, et al. 2013. Evaluation of the vaccination efficacy against H5N1 in domestic poultry in the Red River Delta in Vietnam. Epidemiol. Infect. 141, 776–788. ( 10.1017/S0950268812001628) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koel BF, et al. 2014. Antigenic variation of clade 2.1 H5N1 virus is determined by a few amino acid substitutions immediately adjacent to the receptor binding site. mBio 5, e01070 ( 10.1128/mbio.01070-14) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fouchier RA, Smith DJ. 2010. Use of antigenic cartography in vaccine seed strain selection. Avian Dis. 54(Suppl. 1), 220–223. ( 10.1637/8740-032509-ResNote.1) [DOI] [PubMed] [Google Scholar]
- 41.Abbas MA, et al. 2011. H7 avian influenza virus vaccines protect chickens against challenge with antigenically diverse isolates. Vaccine 29, 7424–7429. ( 10.1016/j.vaccine.2011.07.064) [DOI] [PubMed] [Google Scholar]
- 42.Swayne DE, Lee CW, Spackman E. 2006. Inactivated North American and European H5N2 avian influenza virus vaccines protect chickens from Asian H5N1 high pathogenicity avian influenza virus. Avian Pathol. J. WVPA 35, 141–146. ( 10.1080/03079450600597956) [DOI] [PubMed] [Google Scholar]
- 43.Terregino C, Toffan A, Cilloni F, Monne I, Bertoli E, Castellanos L, Amarin N, Mancin M, Capua I. 2010. Evaluation of the protection induced by avian influenza vaccines containing a 1994 Mexican H5N2 LPAI seed strain against a 2008 Egyptian H5N1 HPAI virus belonging to clade 2.2.1 by means of serological and in vivo tests. Avian Pathol. J. WVPA 39, 215–222. ( 10.1080/03079451003781858) [DOI] [PubMed] [Google Scholar]
- 44.Pfeiffer J, Suarez DL, Sarmento L, To TL, Nguyen T, Pantin-Jackwood MJ. 2010. Efficacy of commercial vaccines in protecting chickens and ducks against H5N1 highly pathogenic avian influenza viruses from Vietnam. Avian Dis. 54(Suppl. 1), 262–271. ( 10.1637/8715-031909-Reg.1) [DOI] [PubMed] [Google Scholar]
- 45.Tian G, et al. 2005. Protective efficacy in chickens, geese and ducks of an H5N1-inactivated vaccine developed by reverse genetics. Virology 341, 153–162. ( 10.1016/j.virol.2005.07.011) [DOI] [PubMed] [Google Scholar]
- 46.Kumar M, Chu HJ, Rodenberg J, Krauss S, Webster RG. 2007. Association of serologic and protective responses of avian influenza vaccines in chickens. Avian Dis. 51(Suppl. 1), 481–483. ( 10.1637/7605-041706R1.1) [DOI] [PubMed] [Google Scholar]
- 47.Swayne DE, Perdue ML, Beck JR, Garcia M, Suarez DL. 2000. Vaccines protect chickens against H5 highly pathogenic avian influenza in the face of genetic changes in field viruses over multiple years. Vet. Microbiol. 74, 165–172. ( 10.1016/S0378-1135(00)00176-0) [DOI] [PubMed] [Google Scholar]
- 48.Swayne DE, et al. 2015. Antibody titer has positive predictive value for vaccine protection against challenge with natural antigenic-drift variants of H5N1 high-pathogenicity avian influenza viruses from Indonesia. J. Virol. 89, 3746–3762. ( 10.1128/JVI.00025-15) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van der Goot JA, van Boven M, Stegeman A, van de Water SG, de Jong MC, Koch G. 2008. Transmission of highly pathogenic avian influenza H5N1 virus in Pekin ducks is significantly reduced by a genetically distant H5N2 vaccine. Virology 382, 91–97. ( 10.1016/j.virol.2008.08.037) [DOI] [PubMed] [Google Scholar]
- 50.Rauw F, et al. 2011. Further evidence of antigenic drift and protective efficacy afforded by a recombinant HVT-H5 vaccine against challenge with two antigenically divergent Egyptian clade 2.2.1 HPAI H5N1 strains. Vaccine 29, 2590–2600. ( 10.1016/j.vaccine.2011.01.048) [DOI] [PubMed] [Google Scholar]
- 51.Park AW, Wood JLN, Daly JM, Newton JR, Glass K, Henley W, Mumford JA, Grenfell BT. 2004. The effects of strain heterology on the epidemiology of equine influenza in a vaccinated population. Proc. R. Soc. B 271, 1547–1555. ( 10.1098/rspb.2004.2766) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Park AW, Daly JM, Lewis NS, Smith DJ, Wood JL, Grenfell BT. 2009. Quantifying the impact of immune escape on transmission dynamics of influenza. Science 326, 726–728. ( 10.1126/science.1175980) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ellis TM, Leung CY, Chow MK, Bissett LA, Wong W, Guan Y, Malik Peiris JS. 2004. Vaccination of chickens against H5N1 avian influenza in the face of an outbreak interrupts virus transmission. Avian Pathol. J. WVPA 33, 405–412. ( 10.1080/03079450410001724012) [DOI] [PubMed] [Google Scholar]
- 54.Walker PG, Cauchemez S, Metras R, Dung do H, Pfeiffer D, Ghani AC. 2010. A Bayesian approach to quantifying the effects of mass poultry vaccination upon the spatial and temporal dynamics of H5N1 in Northern Vietnam. PLoS Comput. Biol. 6, e1000683 ( 10.1371/journal.pcbi.1000683) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Escorcia M, Vazquez L, Mendez ST, Rodriguez-Ropon A, Lucio E, Nava GM. 2008. Avian influenza: genetic evolution under vaccination pressure. Virol. J. 5, 15 ( 10.1186/1743-422X-5-15) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.