Abstract
Falls in older adults are a global public health crisis, but mounting evidence from randomized controlled trials shows that falls can be reduced through exercise. Public health authorities and healthcare professionals endorse the use of evidence‐based, exercise‐focused fall interventions, but there are major obstacles to translating and disseminating research findings into healthcare practice, including lack of evidence of the transferability of efficacy trial results to clinical and community settings, insufficient local expertise to roll out community exercise programs, and inadequate infrastructure to integrate evidence‐based programs into clinical and community practice. The practical solutions highlighted in this article can be used to address these evidence‐to‐practice challenges. Falls and their associated healthcare costs can be reduced by better integrating research on exercise intervention into clinical practice and community programs.
Keywords: falls, older adults, evidence‐based, exercise
Every year, one in three community‐dwelling adults aged 65 and older falls. Many of these falls lead to moderate to severe injuries, resulting in emergency department visits and hospital admissions, and the death rate from falls has risen sharply over the past decade.1 Falls present a considerable financial challenge to the nation's healthcare services. In 2013, the direct medical costs for fall‐related incidents, adjusted for inflation, was $34 billion, mostly covered by Medicare.1, 2 These medical costs will rise as baby boomers age and fall‐related injuries increase.2
Falls are preventable with risk assessment and exercise. Exercise has been shown to reduce the incidence of falls by 13%3 to 40%,4, 5 which has led to a broad consensus among experts that community‐dwelling older adults, especially those at risk of falling, should be offered exercises that incorporate elements of balance, gait, and strength training.6, 7 Organizations including the American Geriatrics Society and British Geriatrics Society,6 Academy of Geriatric Physical Therapy of the American Physical Therapy Assocation,7 National Institute for Health and Care Excellence,8 U.S. Preventive Services Task Force,9 and National Council on Aging have issued guidelines, recommendations, and action plans to assist practitioners working with those at risk for falls.
The Centers for Disease Control and Prevention (CDC) Injury Center has created the CDC Compendium of Effective Fall Interventions: What Works for Community‐Dwelling Older Adults,10 which identifies 14 exercise‐based interventions supported by randomized controlled trials (RCTs). Table 1 provides summary information of these interventions, their outcomes in reducing falls, and on‐line resources.
Table 1.
Summary Information on Exercise‐Focused Evidence‐Based Fall Prevention Interventions Compiled by the Centers for Disease Control and Prevention
| Program | Reduction in Fall Rates or Risk | Setting and Delivery Method | Time Required for Implementation | Online Program Resources | Current Implementation Status | Training Opportunities |
|---|---|---|---|---|---|---|
| Stay Safe, Stay Active11 | 40% | Community setting, delivered by accredited exercise instructors | 1‐hour class session (37 sessions total) once per week over 1‐year period | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| The Otago Exercise Programme12 | 35% | Home setting, delivered by physical therapists or nurses | 30‐minute individual session 3 times per week plus outdoor walk ≥2 times per week |
www.med.unc.edu/aging/cgec/exercise-program
www.acc.co.nz/PRD_EXT_CSMP/groups/external_providers/documents/publications_promotion/prd_ctrb118334.pdf |
www.med.unc.edu/aging/cgec/exercise-program
www.ncoa.org/healthy-aging/falls-prevention/falls-prevention-programs-for-older-adults/ |
www.med.unc.edu/aging/cgec/exercise-program |
| Erlangen Fitness Program13 | 23% | Home setting, delivered by physical therapists or nurses | 1‐hour class session (32 sessions total) twice weekly for 16 weeks plus selected daily home exercises | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| Tai Chi: Moving for Better Balance14, a | 55% risk of multiple falls | Local senior centers and adult activity centers, delivered by a tai chi grand master | 1‐hour class session (48 sessions total) twice weekly for 24 weeks | tjqmbb.org/program.html |
tjqmbb.org www.ncoa.org/healthy‐aging/falls‐prevention/falls‐prevention‐programs‐for‐older‐adults/ |
tjqmbb.org |
| Australian Group Exercise Program15 | 22% for the whole study sample; 31% for a subsample who had fallen in previous year | Residential care community centers and senior centers, delivered by trained exercise instructors | 1‐hour class session (96 sessions total) twice weekly for 12 months | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| Veterans Affairs Group Exercise Program16 | 6 falls per 1,000 hours of activity | Clinical settings, delivered by trained exercise physiology graduate students | 90‐minute class session (36 sessions total) 3 times weekly for 12 weeks | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| Falls Management Exercise Intervention17 | 31% | Community leisure centers and homes, delivered by trained exercise instructors, physical therapists, and occupational therapists | 1‐hour class session (36 sessions total) weekly plus 30‐minute, twice‐weekly home exercise session for 36 weeks | www.laterlifetraining.co.uk/ | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable |
| Central Sydney Tai Chi Trial18 | 35% | General community settings (e.g., town halls, senior centers), delivered by experienced tai chi instructors or instructors experienced in teaching physical activity to older people | 1‐hour class session (16 sessions total) weekly for 16 weeks | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| Simplified Tai Chi19 | 47% risk of multiple falls | Facilities in a residential retirement community, delivered by tai chi grand master | 25‐minute class session (30 sessions total) twice weekly, with an encouragement of 15 minute practice daily, for 15 weeks | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| Lifestyle Approach to Reducing Falls Through Exercise20 | 31% | Home settings, delivered by a physical therapist, occupational therapist, or exercise physiologist | Weekly 40–90 minute sessions for 5 weeks with 2 booster visits |
www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html
ses.library.usyd.edu.au/handle/2123/10627 |
Unavailable | Unavailable |
| Senior Fitness and Prevention21 | 46% | Community gymnasiums, delivered by certified exercise instructors | Twice‐weekly 60‐minute classes plus two 20‐minute home exercise sessions for 18 months | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| Adapted Physical Activity Program22 | 60% | A local community sport center, delivered by a physical therapist and a physical therapy student assistant | 1‐hour class session (48 sessions total) twice weekly for 25 weeks | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| Music‐Based Multitask Exercise Program23 | 54% |
Common areas of residential retirement Communities, delivered by certified Jaques‐Dalcroze instructors |
1‐hour weekly classes (25 sessions total) for 25 weeks | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
| Multitarget Stepping Program24 | 65% | A community health center, delivered by a physical therapist or an exercise trainer | Twice weekly 5‐ to 7‐minute multitask stepping exercises plus 30‐minute physical exercise (including mild strength training, aerobic, balance, flexibility exercises) sessions (48 sessions total) for 24 weeks | www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html | Unavailable | Unavailable |
However, few of these evidence‐based interventions have been adopted in clinical or community practice25, 26 because of a lack of research‐to‐practice data and gaps in the current guidelines regarding how to prescribe appropriate interventions or implement and integrate them into routine clinical and community practice. In this article we highlight current challenges to delivering these CDC‐compiled interventions and offer solutions to enhance their potential to serve clients through community programs and medical practice.
Challenges
Efficacy Versus Effectiveness Research
Most of the CDC Compendium exercise interventions are efficacy (explanatory) trials conducted under controlled “research conditions” (e.g., adhering to stringent eligibility criteria to exclude individuals with comorbidities, poor compliance, medication complications, or limited English language ability) to answer the question “Does this exercise reduce falls?” However, they do not answer the subsequent question “Will this intervention be effective outside of the constraints of the efficacy research model?” Effectiveness trials for fall prevention are rare but necessary to determine whether it makes clinical and financial sense to implement a program in real‐world settings (e.g., outpatient rehabilitation clinics) and community facilities (e.g., senior centers or meal sites) by linking or referring clinical populations at risk for falling per established guidelines6 to primary care settings (i.e., community facilities). Thus, the extent to which these programs are effective in practical settings where healthcare or preventive services are routinely delivered remains to be determined.
Lack of Specific Utilization Directions
Current clinical guidelines6, 7, 8 and recommendations9 do not translate into specific exercise prescriptions for older adults with varying risks of falling, nor are there sufficient resources for making specific referrals to community‐based exercise programs. These deficiencies create obstacles for prescribing fall‐prevention exercise interventions, especially for primary care physicians who are often overburdened with competing healthcare priorities.25
Adoption of Guidelines by Healthcare Providers Is Limited
Adoption of guidelines in clinical practice has been limited and slow.26 Jones and colleagues showed that only 8% of primary care physicians based their fall prevention practices on guidelines from any recognized organization.27 Commonly cited barriers to adoption include the lack of time, training opportunities, financial incentives, and coordination among healthcare providers, and the need for simpler and more easily disseminated materials and referral resources.25, 26, 27 In rehabilitation settings, Peel et al. reported that although home physical therapists were knowledgeable in identifying fall risk factors, they had difficulty linking them to prescribed interventions or identifying available interventions.28
Few Comprehensive Community Programs Are Available
Although community service providers may wish to sponsor fall prevention programs, they often do not have adequate knowledge of best practices in fall prevention29 nor do they have the expertise to support program implementation (e.g., determining the cost and financing for the intervention, training instructors, and monitoring fidelity of intervention delivery). In addition, most CDC‐compiled interventions do not provide an implementation plan with details on program installation, instructor training requirements, class conduct, or program fidelity and adaptation. Consequently, the majority of the interventions are not easily accessible, readily available, or widely disseminated to local communities (Table 1).
Clinicians and Community Providers Do Not Connect
Although it seems obvious that maximizing the impact of any intervention relies primarily on clinicians referring patients to existing community‐based programs, little effort has been made to bridge the communication gap between clinicians and community service providers. Most communities have no coordinated system that allows clinicians to determine what specific interventions are available, which would be the best fit for a particular patient, or whether a patient has enrolled in and completed a program. Similarly, community providers have no standard means to gauge potential demand for specific interventions and generally have offered programs using an “if you build it, they will come” approach rather than responding to a clear need identified by healthcare professionals. These gaps have made implementation of any proven intervention challenging for clinicians and community service providers.
Solutions
Conducting More Translation/Effectiveness Research
Once efficacy has been established, RCTs that have an effectiveness focus need to be implemented in settings where the targeted populations reside and sustainable programs are to be established. Additional research into the optimal training modes (i.e., strength, balance, gait), specificity (duration, intensity, frequency), and delivery methods (e.g., referrals, covered services) in practical settings is necessary. Findings from these studies would improve translation of research into practice and policy.
Studies must include successful public health models, such as RE‐AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance),30 to evaluate translation and dissemination of interventions. For example, when utilizing the RE‐AIM model, Li et al.31 found that a customized Tai Ji Quan program was successfully adopted by healthcare providers (i.e., patients were referred to the program), had excellent reach into the target population (referred patients enrolled in the program), was delivered with high fidelity, and produced significant improvements in physical performance and reductions in falls among participants. This type of data provides critical practice‐based information related to program dissemination and implementation.
Increasing Clinician Awareness and Adoption of Proven Exercise Interventions
To integrate American Geriatrics Society and British Geriatrics Society guidelines into clinical practice, the CDC has developed the toolkit Stopping Elderly Accidents, Deaths, and Injuries,32 which provides clinicians with tools to assess and reduce fall risks among older adults. The materials include recommendations for participation in evidence‐based exercise programs. For example, in the section Integrating Fall Prevention into Practice, providers are encouraged to identify community exercise fall prevention programs for their patients, but as noted previously, clinicians are often unaware of available resources in their community. Links to local community resources that provide details of community fall‐prevention programs must be created so that clinicians can use available resources. Another useful example is the National Council on Aging, which provides excellent resources for professionals, including a checklist for assessing the quality of fall prevention programs, a guide to state coalition building, and a compendium of initiatives from state coalitions.
Professional organizations and the public health sector must actively campaign for, and sponsor, in‐service and continuing education opportunities for healthcare providers to expose them to specific fall prevention interventions and bring available resources (e.g., referral procedures, ready‐to‐use pamphlets, referral pads) directly to their attention. Research shows that offering providers opportunities to undertake training programs as part of their continuing education increases referrals to fall prevention programs.31
Increasing Support for Community Intervention Programs
Two keys to broadening availability of evidence‐based exercise fall prevention programs are enhancing the expertise of community providers and securing financial support. Although interested community providers can improve their understanding of operational challenges associated with fall prevention programs by attending workshops or inviting in experts, substantial progress will require an increase in the availability of turnkey packages derived from translational research that provide specific directions for all aspects of a program (e.g., advertising, recruitment, instructor training, class teaching procedures, program adaption, outcome assessment). To increase the number of these packages, research funding agencies must extend support for research that focuses on the transition of efficacy research findings into effectiveness studies in clinical and community service delivery settings. In the meantime, program developers and physical therapists (who are already directly involved in managing patients with falls and balance deficits)7 might be contracted on an ad hoc basis to assist community implementers in translating efficacy‐based training protocols into practical programs and provide ongoing training and technical support to ensure implementation integrity and intervention fidelity.
Although local community organizations (e.g., Archstone Foundation) fully sponsor a few fall prevention programs, the majority are self‐supported, fee‐based enterprises, which may limit their reach to populations with limited financial resources. Fall prevention exercise programs require financial support through Medicare, Medicaid, and private health insurers to make them truly accessible to all older adults at risk of falls.33 The current model of coverage for screening for fall risk but not for exercise interventions, especially for noninstitutionalized individuals, is shortsighted. This should be a policy priority for national organizations with elder care or public health mandates. Cost‐effectiveness data exist for public policymakers and insurers to underwrite these programs. For example, several of the CDC‐identified programs are shown to deliver excellent returns on investment, with Tai Ji Quan programs returning 509% per dollar invested and the Otago program returning 127% per dollar invested for persons aged 80 and older.34 Funds that support health promotion and disease prevention programs (including falls) sponsored by the Administration on Community Living (ACL),35 in collaboration with National Council on Aging, have helped build a necessary infrastructure that promotes national implementation and dissemination of evidence‐based fall prevention programs through community projects. The ACL effort in conjunction with other public health agencies such as the CDC and community stakeholders is likely to increase participation and assist in the integration and sustainability of these programs.
Improving Communication and Collaboration Between Clinicians and Providers
Given the numerous responsibilities that clinicians already have, it is unlikely they will also be able to remain current on available community fall prevention exercise programs.25 Similarly, community providers often do not know which clinicians have patients requiring their programs. Healthcare systems need to embed intermediaries responsible for connecting clinicians with service providers in their networks to streamline clinical referrals to evidence‐based community interventions.
Integrated Clinical and Community Practice
In the proposed model of clinical and community practice integration (Figure 1), healthcare providers (e.g., physicians, physical therapists) perform a risk assessment according to existing guidelines6, 7, 8 and then simply refer patients to a “health coach,” who is accountable for identifying and facilitating an appropriate fall‐prevention class referral. Community providers are then responsible for enrolling and instructing clients and collecting participation information, which is passed back to the clinician through the health coach to monitor progress. This system requires a collaborative effort and coordination involving multiple providers across different professions in clinical and public health practice but represents an innovative and practical step toward accelerating the transition between clinical practice and community‐based interventions.
Figure 1.
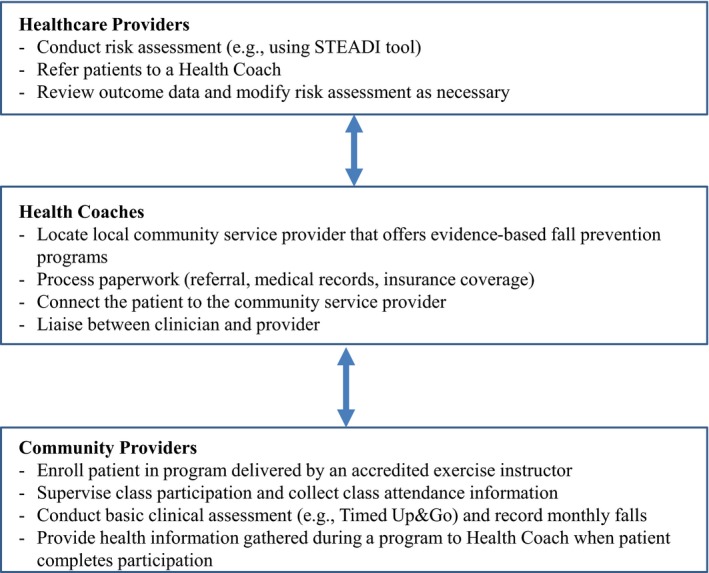
Proposed model to incorporate evidence‐based fall prevention interventions into integrated practice by healthcare professionals and community service providers. STEADI = stopping elderly accidents, deaths, and injuries
Concluding Remarks
The current challenges and possible solutions to disseminating evidence‐based exercise fall prevention interventions have been presented (Table 2). The results of efficacy studies on fall prevention provide a strong foundation on which to build a more‐cohesive and more‐comprehensive approach to this persistent healthcare dilemma. CDC‐compiled interventions provide healthcare practitioners and community‐based organizations with clear directions for linking those at risk of falling to specific evidence‐based programs in the community as part of their care plans, but translational research and uptake of the exercise interventions that the CDC cites have been limited in the community. Unless the challenges to providing exercise‐based options for fall prevention to millions of older adults currently at risk of falling are recognized and overcome, the personal, social, and fiscal costs related to falls will continue to rise. The solutions articulated in this article could bridge evidence‐to‐practice gaps and facilitate clinical and community integration of proven fall‐prevention exercise interventions.
Table 2.
Translation of Efficacy‐Based Fall Prevention Interventions into Clinical and Community Practice: Summary of Challenges and Possible Solutions
| Challenges | Solutions |
|---|---|
| The limited number of exercise‐based fall prevention interventions, which limits broad dissemination to at‐risk older adults | Funding support for effectiveness trials that focus on translating and disseminating evidence‐based interventions, with specific attention to population at risk, mode of intervention, delivery methods, outcome evaluation, and settings where healthcare or preventive services are routinely delivered |
|
Current clinical guidelines and public health recommendations lack: provision of specific exercises appropriate for people at various levels of risk for falling guidance on linking older adults with known fall risk factors to the optimal evidence‐based exercise specific interventions community resources where targeted older adults can be referred and receive an appropriate intervention |
Develop selective preventive interventions that target individuals at higher risk of falling Increase clinical and community awareness of available tools (e.g., Centers for Disease Control and Prevention STEADI) that facilitate adoption of evidence‐based fall prevention interventions; increase access to national and local resources (e.g., National Council on Aging) designed to increase fall prevention efforts Develop streamlined systems that link referrals of at‐risk individuals directly into community‐based interventions delivered by reliable community service providers |
| Limited adoption of guidelines by healthcare providers (lack of time, training opportunities, financial incentives, clinical coordination) |
Increased promotion of STEADI‐type tools that integrate the American Geriatrics Society/British Geriatrics Society guideline and are easy to use in clinical practice Provide fall prevention training opportunities for clinicians Provide resources for implementing evidence‐based interventions available to clinicians Establish a reward system that provides incentives to clinicians to conduct fall risk assessment and link patients to local community‐based interventions |
| Limited number of comprehensive community‐based fall prevention programs currently available |
Provide staff training on fall prevention interventions; encourage integration of evidence‐based programs into fall prevention services Provide sufficient funds to establish community infrastructure to implement evidence‐based interventions Develop turnkey packages for community stakeholders |
|
Lack of communication between healthcare providers and community service providers Lack of integrated fall prevention healthcare systems that link clinical referrals to evidence‐based community interventions |
Engage partnerships and relationships between clinicians, health insurers, and community service providers to fill gaps in converting evidence‐based fall prevention interventions into practice Establish a clinical‐community linkage system (Figure 1) |
STEADI = Stopping Elderly Accidents, Deaths, and Injuries.
Acknowledgments
The authors would like to thank Dorothy Baker and David Fink for their valuable comments on early versions of this manuscript.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper. Fuzhong Li is paid by a National Institutes of Health, National Intistute on Aging Grants AG034956 and AG045094.
Author Contributions: Fuzhong Li conceived the idea for the paper. All authors contributed to the intellectual content of the paper and participated in writing.
Sponsor's Role: There was no sponsor involvement in writing the paper or in the decision to submit it for publication.
J Am Geriatr Soc 64:425–431, 2016.
References
- 1. Centers for Disease Control and Prevention . Falls among older adults: an overview [on‐line]. Available at http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html Accessed April 1, 2015.
- 2. Stevens JA, Corso PS, Finkelstein EA et al. The costs of fatal and nonfatal falls among older adults. Inj Prev 2006;12:290–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Michael YL, Whitlock EP, Lin JS et al. U.S. Preventive Services Task Force. Primary care‐relevant interventions to prevent falling in older adults: A systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 2010;153:815–825. [DOI] [PubMed] [Google Scholar]
- 4. Gillespie LD, Robertson MC, Gillespie WJ et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9:CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sherrington C, Whitney JC, Lord SR et al. Effective exercise for the prevention of falls: A systematic review and meta‐analysis. J Am Geriatr Soc 2008;56:2234–2243. [DOI] [PubMed] [Google Scholar]
- 6. Panel on Prevention of Falls in Older Persons . American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148–157. [DOI] [PubMed] [Google Scholar]
- 7. Avin KG, Hanke TA, Kirk‐Sanchez N et al. Management of falls in community‐dwelling older adults: Clinical Guidance Statement from the Academy of Geriatric Physical Therapy of the American Physical Therapy Association. Phys Ther 2015;95:815–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moyer VA. Prevention of falls in community‐dwelling older adults: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2012;157:197–204. [DOI] [PubMed] [Google Scholar]
- 9. National Institute for Health and Care Excellence . Falls assessment and prevention of falls in older persons. NICE Clinical Guideline 161, June 2013 [on‐line]. Available at http://www.nice.org.uk/CG161 Accessed April 1, 2015.
- 10. Stevens JA. A CDC Compendium of effective fall interventions: What works for community‐dwelling older adults, 3rd Ed. [on‐line]. Available at http://www.cdc.gov/HomeandRecreationalSafety/Falls/compendium.html Accessed June 1, 2015.
- 11. Barnett A, Smith B, Lord S et al. Community‐based group exercise improves balance and reduces falls in at‐risk older people: A randomized controlled trial. Age Ageing 2003;32:407–414. [DOI] [PubMed] [Google Scholar]
- 12. Robertson MC, Campbell AJ, Gardner MM et al. Preventing injuries in older people by preventing falls: A meta‐analysis of individual‐level data. J Am Geriatr Soc 2002;50:905–911. [DOI] [PubMed] [Google Scholar]
- 13. Freiberger E, Menz HB, Abu‐Omar K et al. Preventing falls in physically active community‐dwelling older people: A comparison of two intervention techniques. Gerontology 2007;53:298–305. [DOI] [PubMed] [Google Scholar]
- 14. Li F, Harmer P, Fisher KJ et al. Tai Chi and fall reductions in older adults: A randomized controlled trial. J Gerontol Biol Sci Med Sci 2005;60A:187–194. [DOI] [PubMed] [Google Scholar]
- 15. Lord SR, Castell S, Corcoran J et al. The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: A randomized, controlled trial. J Am Geriatr Soc 2003;51:1685–1692. [DOI] [PubMed] [Google Scholar]
- 16. Rubenstein LZ, Josephson KR, Trueblood PR et al. Effects of a group exercise program on strength, mobility, and falls among fall‐prone elderly men. J Gerontol A Biol Sci Med Sci 2000;55A:M317–M321. [DOI] [PubMed] [Google Scholar]
- 17. Skelton D, Dinan S, Campbell M et al. Tailored group exercise (Falls Management Exercise—FaME) reduces falls in community‐dwelling older frequent fallers (an RCT). Age Ageing 2005;34:636–639. [DOI] [PubMed] [Google Scholar]
- 18. Voukelatos A, Cumming RG, Lord SR et al. A randomized, controlled trial of tai chi for the prevention of falls: The Central Sydney Tai Chi Trial. J Am Geriatr Soc 2007;55:1185–1191. [DOI] [PubMed] [Google Scholar]
- 19. Wolf SL, Barnhart HX, Kutner NG et al. Reducing frailty and falls in older persons: An investigation of tai chi and computerized balance training. J Am Geriatr Soc 1996;44:489–497. [DOI] [PubMed] [Google Scholar]
- 20. Yamada M, Higuchi T, Nishiguchi S et al. Multitarget stepping program in combination with a standardized multicomponent exercise program can prevent falls in community‐dwelling older adults: A randomized, controlled trial. J Am Geriatr Soc 2013;61:1669–1675. [DOI] [PubMed] [Google Scholar]
- 21. Kovács E, Prókai L, Mészáros L et al. Adapted physical activity is beneficial on balance, functional mobility, quality of life and fall risk in community‐dwelling older women: A randomized single‐blinded controlled trial. Eur J Phys Rehabil Med 2013;49:301–310. [PubMed] [Google Scholar]
- 22. Clemson L, Fiatarone Singh MA, Bundy A et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): Randomised parallel trial. BMJ 2012;345:e4547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Trombetti A, Hars M, Herrmann FR et al. Effect of music‐based multitask training on gait, balance, and fall risk in elderly people: A randomized controlled trial. Arch Intern Med 2011;171:525–533. [DOI] [PubMed] [Google Scholar]
- 24. Kemmler W, von Stengel S, Engelke K et al. Exercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women: The randomized controlled senior fitness and prevention (SEFIP) study. Arch Intern Med 2010;25:179–185. [DOI] [PubMed] [Google Scholar]
- 25. Tinetti ME, Gordon C, Sogolow E et al. Fall‐risk evaluation and management: Challenges in adopting geriatric care practices. Gerontologist 2006;46:717–725. [DOI] [PubMed] [Google Scholar]
- 26. Shubert TE, Smith ML, Prizer LP et al. Complexities of fall prevention in clinical settings: A commentary. Gerontologist 2014;54:550–558. [DOI] [PubMed] [Google Scholar]
- 27. Jones TS, Ghosh TS, Horn K et al. Primary care physician perceptions and practices regarding fall prevention in adult's 65 years and over. Acci Anal Prev 2011;43:1605–1609. [DOI] [PubMed] [Google Scholar]
- 28. Peel C, Brown CJ, Lane A et al. A survey of fall prevention knowledge and practice patterns in home health physical therapists. J Geriatr Phys Ther 2008;31:64–70. [DOI] [PubMed] [Google Scholar]
- 29. Laing SS, Silver IF, York S et al. Fall prevention knowledge, attitude, and practices of community stakeholders and older adults. J Aging Res 2011:395357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE‐AIM framework. Am J Public Health 1999;89:1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Li F, Harmer P, Stock R et al. Implementing an evidence‐based fall prevention program in an outpatient clinical setting. J Am Geriatr Soc 2013;61:2142–2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention . Stopping Elderly Accidents, Deaths & Injuries tool kit for health care providers [on‐line]. Available at http://www.cdc.gov/homeandrecreationalsafety/Falls/steadi/index.html#offer Accessed June 1, 2015.
- 33. Tinetti ME, Brach JS. Translating the fall prevention recommendations into a covered service: Can it be done, and who should do it? Ann Intern Med 2012;157:213–214. [DOI] [PubMed] [Google Scholar]
- 34. Carande‐Kulis V, Stevens JA, Florence CS et al. A cost‐benefit analysis of three older adult fall prevention intentions. J Safety Res 2015;52:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Administration for Community Living . ACL funds evidence‐based falls prevention grants [on‐line]. Available at http://acl.gov/NewsRoom/Press_Releases/archive_ACL/2014/2014_09_25a.aspx Accessed April 12, 2015.
- 36. Li F. Transforming traditional tai ji quan techniques into integrative movement therapy—Tai Ji Quan: Moving for Better Balance. J Sport Health Sci 2014;3:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]


