Abstract
Lung adenocarcinomas, like other cancers, develop through the accumulation of epigenetic and genetic alterations. Numerous studies have shown that K-RAS mutation is among the most important early events in carcinogenesis of the lung. However, it is also well established that growth-stimulating signals feed back into growth-suppressing pathways, and any imbalance in these signaling networks will cause the cell to exit the cell cycle, thereby preventing uncontrolled cell growth. How, then, do K-RAS-activated cells evade cellular defense mechanisms? To answer this question, it is necessary to identify the molecular event(s) responsible for the development of early dysplastic lesions that are unable to defend against aberrant oncogene activation. Lineage-determining transcriptional regulators govern differentiation status during normal lung development, as well as in lung adenocarcinoma. Among the genes involved in K-RAS-induced lung tumorigenesis, RUNX3 is unique: inactivation of Runx3 in mouse lung induces lung adenoma and abrogates the ARF–p53 pathway. This observation raises the possibility of intimate cross-talk between the differentiation program and oncogene surveillance. In this review, we summarized evidences suggesting that K-RAS-activated cells do not evade cellular defense mechanisms per se; instead, cells with K-RAS mutations are selected only if they occur in cells in which defense mechanism is abrogated.
Introduction
Lung cancer is one of the most commonly diagnosed malignancies worldwide and the leading cause of cancer-related death.1, 2 Lung cancers comprise four histological types as following: adenocarcinoma, squamous cell carcinoma, large cell carcinoma and small cell carcinoma. Of these four types, adenocarcinoma is the most common and its frequency is increasing rapidly.3, 4
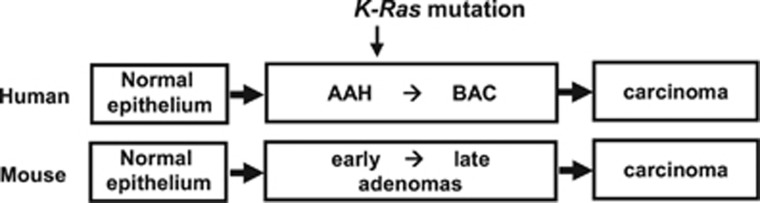
According to the current paradigm, lung adenocarcinoma develops primarily by step-wise progression accompanied by sequential morphologic changes, from atypical adenomatous hyperplasia (AAH) to bronchioloalveolar carcinoma (BAC), and finally to multiple types of invasive tumors, including mucinous and non-mucinous adenocarcinomas.5 AAH/BAC can be divided into two major subtypes, mucinous and non-mucinous;6 K-RAS is predominantly mutated in mucinous AAH/BAC.7 Mouse lung adenoma is considered to be equivalent to human AAH/BAC (Figure 1).
Figure 1.
Current paradigm of lung adenocarcinoma. The majority of lung adenocarcinomas develop through a multi-step tumorigenesis pathway. Tumors develop from atypical adenomatous hyperplasia (AAH) to bronchioalveolar carcinoma (BAC), and ultimately progress to multiple types of invasive tumors. Mouse lung adenoma is equivalent to human AAH and BAC. RUNX3 is inactivated in most early AAH (human) and early adenoma (mouse). K-Ras activation is detected in relatively late AAH or adenoma.21, 48
The progression of lung adenocarcinomas from adenomatous growth to carcinomas proceeds essentially according to the multi-step tumorigenesis pathway established in colon cancer.8, 9 However, the key genetic and epigenetic alterations that are responsible for clonal expansion following each step of tumorigenesis are less well established for lung cancer than for colon cancer. In particular, the critical initial molecular events in the development of lung adenoma remain unclear. Numerous studies have reported that K-RAS mutation, the genetic alteration most frequently detected in lung cancer, is an early event responsible for the development of lung adenoma.10, 11, 12, 13, 14 However, the p14ARF–p53 pathway effectively defends the cell against aberrant oncogene activation.15, 16, 17 Therefore, it is important to determine whether one or more hidden tumor suppressors are inactivated in lung adenomas, or instead the p14ARF–p53 pathway simply provides an incomplete defense against oncogenic K-RAS-induced tumorigenesis. If such hidden tumor suppressors exist, this issue could be resolved by identifying them. Inactivation of key tumor-suppressor genes is often caused by epigenetic process; unfortunately, however, identification of epigenetically silenced tumor suppressors is particularly difficult because gene silencing also occurs over the course of normal differentiation. Therefore, to understand how specific changes in genotype collaborate to create the cancer phenotype, we must actively intervene in the process of tumorigenesis in animal models.
Recent studies aimed at identifying genes involved in the development of lung adenocarcinomas have revealed important roles for lineage-determining transcription factors in K-RAS-induced lung tumorigenesis.18, 19, 20 Inactivation of these genes markedly promotes progression of K-Ras-induced mouse lung adenoma into adenocarcinoma. However, inactivation of most lineage-determining transcription factors does not induce adenoma; the notable exception is Runx3. In mouse lung, inactivation of Runx3 induces adenoma and abrogates oncogene surveillance mechanisms.21 These observations provide an important clue about how adenoma develops and how K-RAS-activated adenoma cells evade cellular defense mechanisms.
Lung epithelial cells
Genetic and epigenetic lesions have major roles in determining tumor phenotypes. However, cancers with distinct phenotypes may also originate from different types of cells within an organ. Therefore, the various distinct types of lung adenocarcinomas can develop either as a result of different molecular events or because they originate from different cell types.22, 23, 24
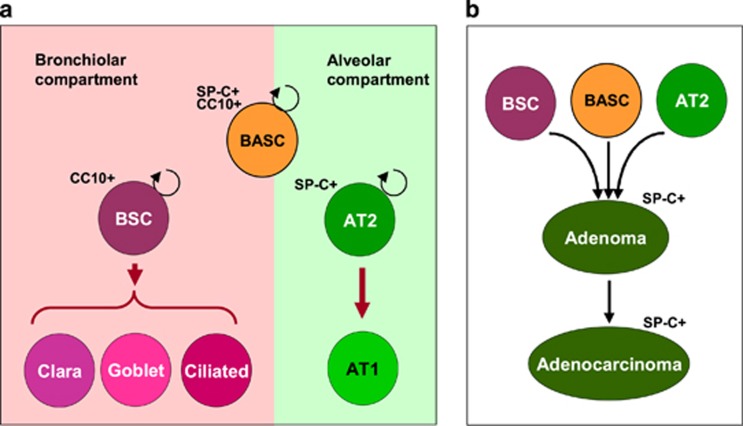
The lung has two distinct cellular compartments, the alveolar and bronchiolar epithelium. The alveolar epithelium includes alveolar epithelial type 1 (AT1) and AT2 cells, which are derived from AT2 cells. The bronchiolar epithelium includes basal cells, ciliated cells, Clara cells, goblet cells and a few pulmonary neuroendocrine cells.25, 26, 27, 28 At least three types of progenitor cells have key roles in maintaining the bronchiolar epithelium of the lung: (1) basal cells, which generate Clara cells and ciliated cells; (2) variant Clara cells (also called bronchiolar stem cells, BSCs), which also generate Clara cells, goblet cells and bronchiolar neuroendocrine cells; and (3) bronchioalveolar stem cells (BASCs) (Figure 2a). BASCs are characterized by their specific location at bronchiolar–alveolar duct junctions and by the expression of both a Clara cell-specific marker (CC10, also known as SCGB1A1 or CCSP) and an AT2 cell-specific marker (SP-C).11 All types of progenitor cells can develop into lung adenocarcinoma in an oncogenic K-Ras-induced mouse lung cancer model24, 29, 30, 31(Figure 2b).
Figure 2.
Lung epithelial cells. (a) Bronchioalveolar stem cells (BASCs) give rise to bronchiolar epithelial cells (BSC or Clara cells) and alveolar epithelial cells (ASC or AT2 cells), which are involved in tissue renewal. BASCs express both BSC-specific markers (CC10) and ASC-specific markers (SP-C). BSCs generate BSCs, Clara cells, goblet cells and ciliated cells, whereas AT2 cells generate AT2 and AT1 cells. (b) BASCs, BSCs and AT2 cells are the known cells of origins of lung adenomas/adenocarcinomas.
K-RAS mutation is critical for the development of lung adenocarcinoma
RAS genes were originally discovered in studies of cancer-causing retroviruses in animals. Two rat sarcoma (RAS)-inducing viruses, Harvey's Ras (H-ras) and Kirsten's Ras (K-ras), were identified in the 1960s.32, 33 Subsequently, transforming genes were isolated from human cancer cell lines in the early 1980s. These genes turned out to be the human homologs of rat H-ras and K-ras.34, 35, 36 A third ras gene (N-ras) was discovered in human cancer cells at 1983.37, 38 RAS family genes encode a membrane-bound GTP-binding protein that transmits extracellular stimuli through receptor tyrosine kinases. Single point mutations, most of which occur at codon 12, 13 or 61 in RAS genes, result in constitutive activation of the encoded proteins.39, 40
K-RAS is one of the most frequently mutated oncogenes in lung adenocarcinoma patients. Approximately 76% of mucinous lung adenocarcinomas have K-RAS mutations, but non-mucinous type adenocarcinomas rarely have the mutation. On the basis of this observation, the role of oncogenic K-RAS in lung cancer initiation has been extensively studied using various knock-in mouse models. Mice of the K-RasLA strain, in which expression of K-RasG12D can be spontaneously activated by random recombination, develop lung adenomas.12 Similarly, in a LoxP-Stop-LoxP-K-Ras conditional mouse strain (K-RasLSL-G12D), expression of oncogenic K-Ras is controlled by a removable transcriptional termination Stop element; when the expression of endogenous level of K-RasG12D was triggered in lung by Adeno-Cre-mediated deletion of the Stop sequence, the mice developed adenomas in a month of stimulation.10, 41
Although these experiments demonstrated the critical role of oncogenic K-RAS in lung tumorigenesis, it remains unclear whether all K-RAS-activated cells are tumorigenic, or instead only some cells are susceptible to K-RAS-induced tumorigenesis. To address this question, Guerra et al. generated K-RasLSL-G12D-IRES-geo mice harboring a K-RasLSL-G12D allele containing IRES-geo, which enables tracing of targeted cells; they then targeted K-RasLSL-G12D-IRES-geo throughout the whole body with tamoxifen-inducible Cre-ERT2 and analyzed the effect on tumor development.42 Notably, systematic tamoxifen treatment induced K-RasLSL-G12D-IRES-geo in 5–15% of cells in most tissues, which include stem cells. However, expression of K-RasG12D throughout the body failed to induce unscheduled proliferation or other growth abnormalities for up to 8 months. Only a subset of K-RasG12D-expressing lung epithelial cells underwent malignant transformation several months after inducer treatment. These results suggested that only a very small number of cells in a specific cellular context are transformed by oncogenic K-Ras.42
In that case, what kinds of cells are susceptible to oncogenic K-Ras-induced tumorigenesis? Kim et al.11 reported that rare BASCs, which express both SP-C and CC10, are the source of oncogenic K-Ras-induced lung adenocarcinomas. Xu et al.43 showed that expression of K-RasG12D in AT2 cells (SP-C-expressing cells) leads to adenocarcinoma formation, suggesting that oncogenic K-Ras-expressing AT2 cells develop into adenocarcinomas. Cho et al.29 reported that constitutive expression of K-RasG12D in Clara cells (that is, CC10-expressing cells) led to adenocarcinoma, suggesting that lung adenocarcinoma could also originate in bronchiolar epithelial cells. These results demonstrate that normal lung epithelial cells, BASCs, Clara cells and AT2 cells can develop into lung adenocarcinomas upon K-Ras activation (Figure 2).
K-RAS mutation alone does not seem to initiate lung tumorigenesis
Notably, Clara and AT2 cells are relatively abundant in lung epithelium, inconsistent with previous observations that only a very limited number of lung epithelial cells are susceptible to oncogenic K-Ras-induced lung tumorigenesis.44 In addition, a simple calculation based on the rate of specific point mutations per cell and the number of cells in the body suggests that several thousand new point-mutated RAS oncogenes are created every day in every human being.7 However, humans do not suffer from cancer as frequently as this calculated rate would predict. Even Costello syndrome patients, who carry H-RASG12A mutant alleles in their germ lines, do not develop tumors at young age. Only 24% of Costello syndrome patients develop malignancy, and then only after several decades of life.45 Therefore, it is likely that normal cells are resistant to transformation by RAS activation alone, and that other genetic or epigenetic alterations are also required. This idea is supported by the observation that K-RAS mutation is a relatively late event in the pathogenesis of human lung adenocarcinoma: K-RAS mutations appear to be involved in the conversion of dysplastic cells to preinvasive cancer cells, rather than initiation of preneoplastic lesions.46
Dysregulation of the differentiation program in lung tumorigenesis
What kind of genetic or epigenetic alterations are involved in the oncogenic K-RAS-induced lung tumorigenesis? It is worth noting that mouse lung adenocarcinomas induced by oncogenic K-Ras alone are all of the non-mucinous type, regardless of the cell type of origin. In humans, however, K-RAS mutation is far more frequent in mucinous than non-mucinous lung adenocarcinomas. Because these subtypes of lung adenocarcinomas are distinguished by the differentiation status of the tumors, we imagine the involvement of differentiation regulators in K-Ras-induced lung tumorigenesis. Development of lung adenocarcinoma is often associated with dysregulation of lung epithelial lineage-determining transcriptional regulators that govern differentiation status.47 For example, Gata6 maintains proper alveolar maturation18 in cooperation with other known lineage-specific transcription factors such as Hopx19 and Nkx2-1.20 Runx3 is required for both bronchiolar and alveolar lineage differentiation.48, 49 Among the differentiation regulators, the roles of Nkx2-1 and Runx3 in oncogenic K-Ras-induced lung tumorigenesis have been most extensively studied.
Nkx2-1 (also called Titf1 or Ttf-1), which is essential for lung epithelial lineage determination, is frequently up- or downregulated in poorly differentiated lung adenocarcinomas.50, 51 Winslow et al.52 noticed that Nkx2-1 is frequently silenced in malignant adenocarcinomas in a KrasLSL-G12D;p53−/− mouse cancer model. Although Nkx2-1+/– mice do not develop spontaneous lung tumors, overexpression of K-RasG12D in Nkx2-1+/– mouse lung results in a larger number of malignant lung tumors (with greater volumes) than in wild-type mice.53 Snyder et al.54 also demonstrated that simultaneous KrasG12D expression and Nkx2-1 deletion in lungs (KrasLSL-G12D;Nkx2-1−/−) results in early onset malignant adenocarcinoma. Notably, simultaneous KrasG12D expression and Nkx2-1 inactivation induces mucinous-type lung adenocarcinomas, whereas KrasG12D expression alone induces only non-mucinous type lung adenoma/adenocarcinomas. To determine whether Nkx2-1 inactivation occurs earlier than K-Ras activation, Snyder et al.54 inactivated Nkx2-1 in established KrasLSL-G12D-induced tumors and showed that non-mucinous-type tumor cells produced mucin upon Nkx2-1 inactivation. However, deletion of Nkx2-1 in adult lung does not induce adenoma.53, 54 Therefore, inactivation of Nkx2-1 appears to be involved not only in tumor initiation but also in the transition from adenoma to mucinous adenocarcinoma, although deletion of Nkx2-1 alone does not result in the development of adenoma.54
RUNX3, a lineage-determining transcription factor expressed in multiple tissues, is frequently downregulated in various tumors.45, 49 During lung development, RUNX3 has an essential role in terminal differentiation of lung epithelial cells: it is required for the generation of bronchiolar lineage cells and for the terminal differentiation of alveolar cells.45 Lee et al.48 found that RUNX3 is inactivated in nearly all human lung AAH and carcinogen-induced early mouse lung adenomas in which K-Ras is not yet mutated. Subsequently, they investigated whether Runx3 inactivation is causally associated with the development of adenomas. Surprisingly, deletion of Runx3 in adult mouse lung results in the early induction of lung adenomas of either the mucinous or non-mucinous type.21 Simultaneous targeting of Runx3f/f and K-RasLSL-G12D/+ led to the progression of the two distinct types of adenomas into the corresponding types of adenocarcinomas. Therefore, Runx3f/f and Runx3f/f;K-RasLSL-G12D/+ mice faithfully recapitulate the development of human lung AAH and adenocarcinoma, respectively.21 Although the specific cells of origin of each type of adenoma remain to be identified, these results clearly demonstrate that inactivation of Runx3 is responsible for the development of multiple types of lung adenomas.
If K-Ras activation alone does not induce lung adenoma, but Runx3 inactivation does, how can lung adenoma develop in a mouse model in which K-Ras is activated alone? Runx3 is expressed in nearly all lung epithelial cells, but silenced in most KrasG12D-induced lung adenocarcinomas,21 implying that KrasG12D can induce adenomas when it is expressed in cells that do not express Runx3 or some other critical gene. These Runx3 non-expressing cells could be rare normal cells or abnormal cells generated by deregulation of gene expression. The former possibility is supported by the observation that BASCs, which express both SP-C and CC10, are the targets of oncogenic K-Ras-induced lung tumorigenesis.11 On the other hand, the latter possibility is supported by the observation that a large proportion of Runx3-inactivated bronchiolar epithelial cells express both SP-C and CC10, and these cells develop into adenomas.21 Although both possibilities are supported by evidence, the latter is more plausible under physiological conditions, because tumor development is considered to be a biological process that resembles Darwinian evolution: random mutations create genetic variability in a cell population, and the force of selection favors the outgrowth of individual mutant cells that happen to be endowed with advantageous traits. On the basis of a combination of Darwinian theory and the concept of multi-step tumor progression, tumorigenesis is now understood as a succession of clonal expansions.8, 9 Selection of cells endowed with advantageous traits requires a large number of cells. However, single-step tumorigenesis by oncogenic K-Ras mutation from rare (but normally existing) cells is not consistent with the Darwinian concept. On the other hand, if Runx3 were inactivated by chance in normal cells, these cells would acquire a proliferative advantage,21 enabling subsequent selection for K-Ras-mutated cells. Undoubtedly, K-Ras-induced lung adenocarcinoma development can proceed via multiple pathways; nonetheless, the high frequency of Runx3 inactivation in K-Ras-induced mouse and human lung adenocarcinoma suggests that a major pathway involves Runx3 inactivation before K-Ras activation.
Critical role of Runx3 in the defense against oncogene activation
Several important differentiation regulators govern lung development. However, deregulation of the differentiation program is not sufficient to induce adenoma: so far, Runx3 is the only gene whose inactivation has been reported to induce lung adenoma. What makes Runx3 is so special in regard to lung tumorigenesis?
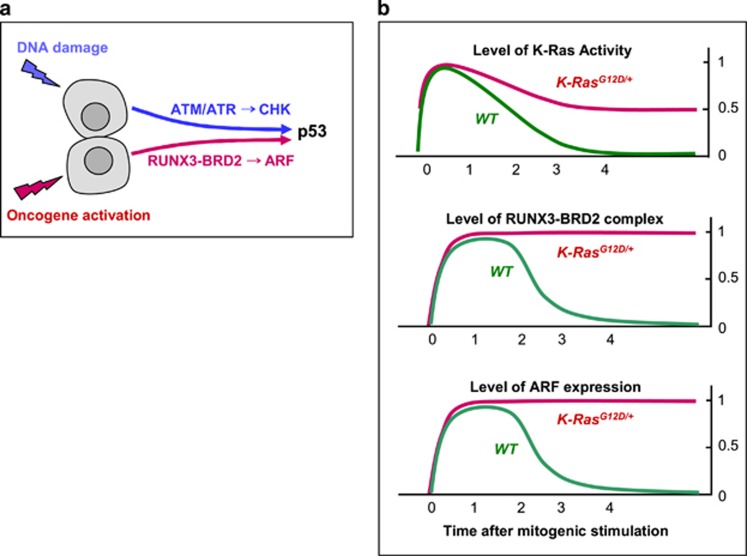
It is well established that cells have evolved effective defense mechanisms against cellular transformation. Ever since it became clear that about 50% of human cancers contain mutations in p53, this gene has been intensively studied as a cellular defense against transformation. The p53 transcriptional program includes the activation of number of pro-apoptotic proteins and cell cycle inhibitors, resulting in apoptosis or irreversible proliferative arrest.55, 56 Two major stresses, DNA damage and oncogene activation, trigger p53 activation through different genetic pathways: DNA damage through the ATM/ATR and CHK1/CHK2 kinases, and oncogenic signaling through p14ARF (in mouse, p19Arf; hereafter, ARF or Arf)57 (Figure 3a). Recent genetic evidence in mice indicates that ARF-dependent activation of p53 is critical for p53-mediated tumor suppression.58
Figure 3.
p53 tumor-suppressor pathways. (a) Two major pathways trigger p53 activation. (1) DNA damage stress is sensed by the ATM/ATR kinases, which activate the CHK1/CHK2 kinases, which in turn stabilize p53. Aberrant oncogene activation is sensed by the RUNX3–BRD2 complex, which induces expression of ARF, which in turn inactivates HDM2 and thereby stabilizes p53. (b) Mechanism for sensing constitutive RAS activation. Normal RAS activity is downregulated to the basal level soon after mitogenic stimulation (top panel, green line). Although RAS is activated, the RUNX3–BRD2 complex is formed (middle panel, green line) and ARF expression is induced (bottom panel, green line). In normal cells, RUNX3–BRD2 complex formation and ARF expression occurs for only a short time (1–3 h after mitogenic stimulation) and disappears when RAS activity is downregulated. However, heterozygous mutation of RAS results in maintenance of 50% of the maximum level of RAS activity. This persistent RAS activity maintains the RUNX3–BRD2 complex and ARF expression until the G1/S check point.
Hence, it is important to determine the role of the ARF–p53 pathway in oncogenic K-RAS-induced lung cancer. Indeed, simultaneous activation of oncogenic K-Ras and inactivation of the p53 tumor suppressor in mouse lung significantly accelerates the malignancy of the resultant adenocarcinoma.41 However, it remained unclear whether inactivation of p53 contributed to the initiation or progression of lung tumorigenesis. To address this issue, Junttila et al. and Feldser et al. induced lung adenocarcinoma by simultaneous inactivation of p53 and K-Ras activation, and then restored p53. Importantly, restoration of p53 activity only resulted in the regression of adenocarcinoma and did not affect adenoma.13, 14 In addition, the Arf–p53 pathway was retained in mouse embryonic fibroblast cells expressing K-RasG12D.42, 59 These results suggested that the p53 pathway is not engaged in the early stage of lung tumorigenesis, even if oncogenic K-Ras is expressed.
Why does the defense mechanism not prevent tumor formation in mice? Palmero et al.60 demonstrated that overexpression of oncogenic K-Ras activates the Arf–p53 pathway in primary cells. On the other hand, Junttila et al.13 and Feldser et al.14 showed that oncogenic K-Ras expressed at the endogenous level does not activate the Arf–p53 pathway in mouse lung. These observations might be explained in two major ways as follows: (1) the p53 pathway has an inherent limit and is not engaged by expression of an activated oncogene at the endogenous level that is sufficient to induce tumors or (2) the p53 pathway fails to be activated not as a result of some inherent limit but instead due to some unknown component(s) that mediates oncogenic activity. Although several lines of evidence support the first possibility,13, 14 several studies have reported that the activation of RAS alone in normal cells is not sufficient to induce transformation.45, 46
Therefore, we must consider the second possibility. ARF, which is induced in response to oncogenic activation, stabilizes p53 by inhibiting HDM2 (in mouse, MDM2).61 Mitogenic signaling activates the GTPase activity of RAS, which decreases to the basal level soon after the signal is transduced to downstream kinase pathways. Oncogenic RAS is a constitutively active form whose activity is not downregulated. Therefore, heterozygous RAS mutation results in maintenance of 50% of the maximum level of Ras activity (Figure 3b). To protect themselves from oncogenic RAS-induced abnormal proliferation, cells should be able to sense the duration of the 50% RAS activity rather than its maximum level of activity. For a long time, however, it was unclear whether cells can indeed recognize aberrant persistence of RAS activity. Lee et al.21 demonstrated that mammals have evolved an effective defense mechanism against the persistent activation of oncogenic RAS. When RAS is activated by normal mitogenic stimulation, RUNX3 forms a complex with p300 and BRD2 (a relative of TAF250) in a MAPK activity-dependent manner; this complex transiently induces ARF, which in turn transiently stabilizes p53. Soon after the mitogenic surge, MAPK activity is reduced. In this situation, the Runx3–BRD2 complex dissociates and ARF expression is repressed. Mitogen-stimulated transient activation of the ARF–p53 pathway does not affect the cell cycle because it occurs only 1–3 h after mitogenic simulation and is then silenced at the G1/S checkpoint. When K-RAS is constitutively activated, the RUNX3–BRD2 complex is maintained, and expression of ARF and p53 continued until the G1/S checkpoint.21 These results show that cells can effectively defend against an endogenous level of RAS activity, and that the RUNX3–BRD2 complex functions as a sensor for abnormal persistence of RAS activity21 (Figure 3b).
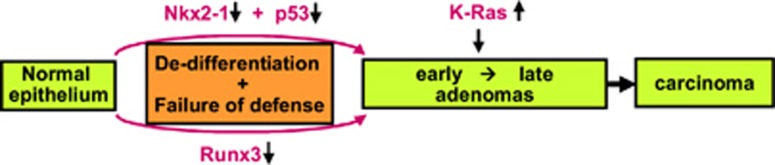
These results demonstrate that RUNX3 has essential roles in oncogene surveillance, as well as regulation of differentiation. To date, RUNX3 is the only gene whose inactivation has been shown to be sufficient to induce adenoma, suggesting that abrogation of both the differentiation program and oncogene surveillance mechanism might be required for adenoma development. Such events could occur either as a result of multiple molecular events (that is, one involved in each pathway) or a single molecular event such as RUNX3 inactivation. Cells acquired K-RAS mutation might be selected when it occurred in cells in which differentiation program and defense mechanism is abrogated (Figure 4). Obviously, the probability of deregulation is much higher for a single gene than for two genes. This might explain why RUNX3 inactivation is so frequently detected in lung AAHs.21
Figure 4.
A model for the step-wise progression of lung adenocarcinoma. Adenoma development may require abrogation of both the differentiation program and oncogene surveillance. These two events could occur independently: for example, the differentiation program could be abrogated by silencing of Nkx2-1, and oncogene surveillance mechanism could be disabled by p53 deletion. Alternatively, the two events could occur simultaneously by inactivation Runx3, allowing adenoma cells to progress to adenocarcinoma upon oncogenic Ras mutation.
Prospects
It is somewhat surprising that a differentiation regulator, RUNX3, has a key role in oncogene surveillance. However, considering the machinery involved in cell cycle decision making, we can imagine the existence of contact points between the differentiation program, cell cycle progression and oncogene surveillance. When stimulated by mitogens, cells decide whether they will remain in G1, retreat from the active cycle into G0 or advance into the remaining phase of the cell cycle.60 This critical decision, which is dependent on cell context, is made 2–3 h after stimulation, at the so-called restriction point (R-point).62, 63 A growing body of evidence indicates that deregulation of the R-point decision-making machinery accompanies the formation of most if not all types of cancer.7 To make an appropriate decision, cells should know their own differentiation status, and RUNX3 might serve to report cellular differentiation status to the R-point ‘committee'. Hence, it would be interesting to investigate whether the tumor-suppressor activity of RUNX3 is associated with R-point commitment.
Although numerous anti-cancer drugs have been developed, most cancers are still ultimately fatal due to the very high rate of recurrence. For example, gefitinib effectively eliminates EGFR-mutated lung adenocarcinomas at the beginning of therapy, but the cancers recur in 90% of patients within 2 years.64 Recurrence of lung cancer occurs mainly due to persistent early lesions that are resistant to the anti-cancer drug. Therefore, to eradicate cancers, it is necessary to eliminate both early and malignant lesions. Because the critical genes involved in the initiation of adenoma development were unknown, to date no anti-cancer drug has been developed that is capable of eliminating early lesions. As noted above, a recent effort to restore p53 in K-Ras-activated mouse tumors failed to eliminate adenoma: p53 restoration killed only malignant adenocarcinomas, leaving adenomas untouched.13, 14 However, the recent findings that RUNX3 is inactivated in most AAHs in human, and that Runx3 inactivation in mice induces lung adenoma, implies that RUNX3-targeted therapies could be a means to eradicate adenomas. It would be exciting indeed if Runx3 restoration in K-Ras-activated tumors is able to eliminate not only adenocarcinomas but also adenomas. If that turns out to be the case, RUNX3 will be a promising target for curative cancer therapy.
Is it possible to reactivate RUNX3 in tumors? It is worth emphasizing that RUNX3 is inactivated in various human tumors, mainly by epigenetic alteration. In theory, epigenetically inactivated genes could be reactivated by DNA methyltransferase inhibitors or histone deacetylase (HDAC) inhibitors. Class III HDACs (as well as class I and II HDACs) inactivate RUNX3, and class III HDACs can be inhibited by physiological concentrations of niacinamide.65, 66 Indeed, inhibition of class III HDACs by niacinamide65, 66 reactivates or protects RUNX3, thereby effectively preventing carcinogen-induced tumorigenesis in the bladder,67 liver68 and lung (our unpublished observation). Because niacinamide is nontoxic, it could be used to prevent tumors. Therefore, identification of RUNX3 as a potential specific target for early-stage lung cancer eradication provides an important theoretical basis for the development of safer and more effective anti-cancer drugs.
Acknowledgments
S-CB is supported by a Creative Research Grant (2014R1A3A2030690) and Y-SL is supported by Basic Science Research Program (2013R1A1A2057659) through the National Research Foundation (NRF) funded by the Ministry of Education of Korea.
The authors declare no conflict of interest.
References
- 1Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics, 1999. CA Cancer J Clin 1999; 49: 8–31. [DOI] [PubMed] [Google Scholar]
- 2Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013; 63: 11–30. [DOI] [PubMed] [Google Scholar]
- 3Minna JD, Roth JA, Gazdar AF. Focus on lung cancer. Cancer Cell 2002; 1: 49–52. [DOI] [PubMed] [Google Scholar]
- 4Travis WD. Pathology of lung cancer. Clin Chest Med 2002; 23: 65–81. [DOI] [PubMed] [Google Scholar]
- 5Wistuba II, Gazdar AF. Lung cancer preneoplasia. Annu Rev Pathol 2006; 1: 331–348. [DOI] [PubMed] [Google Scholar]
- 6Travis WD. World Health Organization. International Agency for Research on Cancer, International Association for the Study of Lung Cancer, International Academy of Pathology. Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. IARC Press Oxford University Press: Lyon Oxford, 2004. [Google Scholar]
- 7Marchetti A, Buttitta F, Pellegrini S, Chella A, Bertacca G, Filardo A et al. Bronchioloalveolar lung carcinomas: K-ras mutations are constant events in the mucinous subtype. J Pathol 1996; 179: 254–259. [DOI] [PubMed] [Google Scholar]
- 8Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M et al. Genetic alterations during colorectal-tumor development. N Engl J Med 1988; 319: 525–532. [DOI] [PubMed] [Google Scholar]
- 9Weinberg RA. The biology of cancer. Garland Science: New York, 2007. [Google Scholar]
- 10Jackson EL, Willis N, Mercer K, Bronson RT, Crowley D, Montoya R et al. Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes Dev 2001; 15: 3243–3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11Kim CF, Jackson EL, Woolfenden AE, Lawrence S, Babar I, Vogel S et al. Identification of bronchioalveolar stem cells in normal lung and lung cancer. Cell 2005; 121: 823–835. [DOI] [PubMed] [Google Scholar]
- 12Johnson L, Mercer K, Greenbaum D, Bronson RT, Crowley D, Tuveson DA et al. Somatic activation of the K-ras oncogene causes early onset lung cancer in mice. Nature 2001; 410: 1111–1116. [DOI] [PubMed] [Google Scholar]
- 13Junttila MR, Karnezis AN, Garcia D, Madriles F, Kortlever RM, Rostker F et al. Selective activation of p53-mediated tumour suppression in high-grade tumours. Nature 2010; 468: 567–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14Feldser DM, Kostova KK, Winslow MM, Taylor SE, Cashman C, Whittaker CA et al. Stage-specific sensitivity to p53 restoration during lung cancer progression. Nature 2010; 468: 572–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15Serrano M, Lin AW, McCurrach ME, Beach D, Lowe SW. Oncogenic ras provokes premature cell senescence associated with accumulation of p53 and p16INK4a. Cell 1997; 88: 593–602. [DOI] [PubMed] [Google Scholar]
- 16Levine AJ. p53, the cellular gatekeeper for growth and division. Cell 1997; 88: 323–331. [DOI] [PubMed] [Google Scholar]
- 17Kruse JP, Gu W. Modes of p53 regulation. Cell 2009; 137: 609–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18Keijzer R, van Tuyl M, Meijers C, Post M, Tibboel D, Grosveld F et al. The transcription factor GATA6 is essential for branching morphogenesis and epithelial cell differentiation during fetal pulmonary development. Development 2001; 128: 503–511. [DOI] [PubMed] [Google Scholar]
- 19Yin Z, Gonzales L, Kolla V, Rath N, Zhang Y, Lu MM et al. Hop functions downstream of Nkx2.1 and GATA6 to mediate HDAC-dependent negative regulation of pulmonary gene expression. Am J Physiol Lung Cell Mol Physiol 2006; 291: L191–L199. [DOI] [PubMed] [Google Scholar]
- 20Zhang Y, Rath N, Hannenhalli S, Wang Z, Cappola T, Kimura S et al. GATA and Nkx factors synergistically regulate tissue-specific gene expression and development in vivo. Development 2007; 134: 189–198. [DOI] [PubMed] [Google Scholar]
- 21Lee YS, Lee JW, Jang JW, Chi XZ, Kim JH, Li YH et al. Runx3 inactivation is a crucial early event in the development of lung adenocarcinoma. Cancer Cell 2013; 24: 603–616. [DOI] [PubMed] [Google Scholar]
- 22Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature 2014; 511: 543–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23Sutherland KD, Berns A. Cell of origin of lung cancer. Mol Oncol 2010; 4: 397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24Blanpain C. Tracing the cellular origin of cancer. Nat Cell Biol 2013; 15: 126–134. [DOI] [PubMed] [Google Scholar]
- 25Bishop AE. Pulmonary epithelial stem cells. Cell Prolif 2004; 37: 89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26Reddy R, Buckley S, Doerken M, Barsky L, Weinberg K, Anderson KD et al. Isolation of a putative progenitor subpopulation of alveolar epithelial type 2 cells. Am J Physiol Lung Cell Mol Physiol 2004; 286: L658–L667. [DOI] [PubMed] [Google Scholar]
- 27Rock JR, Onaitis MW, Rawlins EL, Lu Y, Clark CP, Xue Y et al. Basal cells as stem cells of the mouse trachea and human airway epithelium. Proc Natl Acad Sci USA 2009; 106: 12771–12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28Rock JR, Hogan BL. Epithelial progenitor cells in lung development, maintenance, repair, and disease. Annu Rev Cell Dev Biol 2011; 27: 493–512. [DOI] [PubMed] [Google Scholar]
- 29Cho HC, Lai CY, Shao LE, Yu J. Identification of tumorigenic cells in Kras(G12D)-induced lung adenocarcinoma. Cancer Res 2011; 71: 7250–7258. [DOI] [PubMed] [Google Scholar]
- 30Barkauskas CE, Cronce MJ, Rackley CR, Bowie EJ, Keene DR, Stripp BR et al. Type 2 alveolar cells are stem cells in adult lung. J Clin Invest 2013; 123: 3025–3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31Sutherland KD, Song JY, Kwon MC, Proost N, Zevenhoven J, Berns A. Multiple cells-of-origin of mutant K-Ras-induced mouse lung adenocarcinoma. Proc Natl Acad Sci USA 2014; 111: 4952–4957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32Harvey JJ. An unidentified virus which causes the rapid production of tumours in mice. Nature 1964; 204: 1104–1105. [DOI] [PubMed] [Google Scholar]
- 33Kirsten WH, Mayer LA. Morphologic responses to a murine erythroblastosis virus. J Natl Cancer Inst 1967; 39: 311–335. [PubMed] [Google Scholar]
- 34Goldfarb M, Shimizu K, Perucho M, Wigler M. Isolation and preliminary characterization of a human transforming gene from T24 bladder carcinoma cells. Nature 1982; 296: 404–409. [DOI] [PubMed] [Google Scholar]
- 35Pulciani S, Santos E, Lauver AV, Long LK, Robbins KC, Barbacid M. Oncogenes in human tumor cell lines: molecular cloning of a transforming gene from human bladder carcinoma cells. Proc Natl Acad Sci USA 1982; 79: 2845–2849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36Shih C, Padhy LC, Murray M, Weinberg RA. Transforming genes of carcinomas and neuroblastomas introduced into mouse fibroblasts. Nature 1981; 290: 261–264. [DOI] [PubMed] [Google Scholar]
- 37Hall A, Marshall CJ, Spurr NK, Weiss RA. Identification of transforming gene in two human sarcoma cell lines as a new member of the ras gene family located on chromosome 1. Nature 1983; 303: 396–400. [DOI] [PubMed] [Google Scholar]
- 38Shimizu K, Goldfarb M, Perucho M, Wigler M. Isolation and preliminary characterization of the transforming gene of a human neuroblastoma cell line. Proc Natl Acad Sci USA 1983; 80: 383–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39Santos E, Martin-Zanca D, Reddy EP, Pierotti MA, Della Porta G, Barbacid M. Malignant activation of a K-ras oncogene in lung carcinoma but not in normal tissue of the same patient. Science 1984; 223: 661–664. [DOI] [PubMed] [Google Scholar]
- 40Rodenhuis S, van de Wetering ML, Mooi WJ, Evers SG, van Zandwijk N, Bos JL. Mutational activation of the K-ras oncogene. A possible pathogenetic factor in adenocarcinoma of the lung. N Engl J Med 1987; 317: 929–935. [DOI] [PubMed] [Google Scholar]
- 41DuPage M, Dooley AL, Jacks T. Conditional mouse lung cancer models using adenoviral or lentiviral delivery of Cre recombinase. Nat Protoc 2009; 4: 1064–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42Guerra C, Mijimolle N, Dhawahir A, Dubus P, Barradas M, Serrano M et al. Tumor induction by an endogenous K-ras oncogene is highly dependent on cellular context. Cancer Cell 2003; 4: 111–120. [DOI] [PubMed] [Google Scholar]
- 43Xu X, Rock JR, Lu Y, Futtner C, Schwab B, Guinney J et al. Evidence for type II cells as cells of origin of K-Ras-induced distal lung adenocarcinoma. Proc Natl Acad Sci USA 2012; 109: 4910–4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44Meuwissen R, Berns A. Mouse models for human lung cancer. Genes Dev 2005; 19: 643–664. [DOI] [PubMed] [Google Scholar]
- 45Rauen KA. HRAS and the Costello syndrome. Clin Genet 2007; 71: 101–108. [DOI] [PubMed] [Google Scholar]
- 46Sugio K, Kishimoto Y, Virmani AK, Hung JY, Gazdar AF. K-ras mutations are a relatively late event in the pathogenesis of lung carcinomas. Cancer Res 1994; 54: 5811–5815. [PubMed] [Google Scholar]
- 47Garraway LA, Sellers WR. Lineage dependency and lineage-survival oncogenes in human cancer. Nat Rev Cancer 2006; 6: 593–602. [DOI] [PubMed] [Google Scholar]
- 48Lee KS, Lee YS, Lee JM, Ito K, Cinghu S, Kim JH et al. Runx3 is required for the differentiation of lung epithelial cells and suppression of lung cancer. Oncogene 2010; 29: 3349–3361. [DOI] [PubMed] [Google Scholar]
- 49Ito Y, Bae SC, Chuang LS. The RUNX family: developmental regulators in cancer. Nat Rev Cancer 2015; 15: 81–95. [DOI] [PubMed] [Google Scholar]
- 50Westcott PM, Halliwill KD, To MD, Rashid M, Rust AG, Keane TM et al. The mutational landscapes of genetic and chemical models of Kras-driven lung cancer. Nature 2015; 517: 489–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51Maeda Y, Dave V, Whitsett JA. Transcriptional control of lung morphogenesis. Physiol Rev 2007; 87: 219–244. [DOI] [PubMed] [Google Scholar]
- 52Winslow MM, Dayton TL, Verhaak RG, Kim-Kiselak C, Snyder EL, Feldser DM et al. Suppression of lung adenocarcinoma progression by Nkx2-1. Nature 2011; 473: 101–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53Maeda Y, Tsuchiya T, Hao H, Tompkins DH, Xu Y, Mucenski ML et al. Kras(G12D) and Nkx2-1 haploinsufficiency induce mucinous adenocarcinoma of the lung. J Clin Invest 2012; 122: 4388–4400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54Snyder EL, Watanabe H, Magendantz M, Hoersch S, Chen TA, Wang DG et al. Nkx2-1 represses a latent gastric differentiation program in lung adenocarcinoma. Mol Cell 2013; 50: 185–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55Lowe SW, Cepero E, Evan G. Intrinsic tumour suppression. Nature 2004; 432: 307–315. [DOI] [PubMed] [Google Scholar]
- 56Vousden KH, Lu X. Live or let die: the cell's response to p53. Nat Rev Cancer 2002; 2: 594–604. [DOI] [PubMed] [Google Scholar]
- 57Palmero I, McConnell B, Parry D, Brookes S, Hara E, Bates S et al. Accumulation of p16INK4a in mouse fibroblasts as a function of replicative senescence and not of retinoblastoma gene status. Oncogene 1997; 15: 495–503. [DOI] [PubMed] [Google Scholar]
- 58Efeyan A, Serrano M. p53: guardian of the genome and policeman of the oncogenes. Cell Cycle 2007; 6: 1006–1010. [DOI] [PubMed] [Google Scholar]
- 59Tuveson DA, Shaw AT, Willis NA, Silver DP, Jackson EL, Chang S et al. Endogenous oncogenic K-ras(G12D) stimulates proliferation and widespread neoplastic and developmental defects. Cancer Cell 2004; 5: 375–387. [DOI] [PubMed] [Google Scholar]
- 60Palmero I, Pantoja C, Serrano M. p19ARF links the tumour suppressor p53 to Ras. Nature 1998; 395: 125–126. [DOI] [PubMed] [Google Scholar]
- 61Vogelstein B, Lane D, Levine AJ. Surfing the p53 network. Nature 2000; 408: 307–310. [DOI] [PubMed] [Google Scholar]
- 62Pardee AB. A restriction point for control of normal animal cell proliferation. Proc Natl Acad Sci USA 1974; 71: 1286–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63Blagosklonny MV, Pardee AB. The restriction point of the cell cycle. Cell Cycle 2002; 1: 103–110. [PubMed] [Google Scholar]
- 64Kobayashi S, Boggon TJ, Dayaram T, Janne PA, Kocher O, Meyerson M et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med 2005; 352: 786–792. [DOI] [PubMed] [Google Scholar]
- 65Anderson RM, Bitterman KJ, Wood JG, Medvedik O, Sinclair DA. Nicotinamide and PNC1 govern lifespan extension by calorie restriction in Saccharomyces cerevisiae. Nature 2003; 423: 181–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66Bitterman KJ, Anderson RM, Cohen HY, Latorre-Esteves M, Sinclair DA. Inhibition of silencing and accelerated aging by nicotinamide, a putative negative regulator of yeast sir2 and human SIRT1. J Biol Chem 2002; 277: 45099–45107. [DOI] [PubMed] [Google Scholar]
- 67Kim WJ, Lee JW, Quan C, Youn HJ, Kim HM, Bae SC. Nicotinamide inhibits growth of carcinogen induced mouse bladder tumor and human bladder tumor xenograft through up-regulation of RUNX3 and p300. J Urol 2011; 185: 2366–2375. [DOI] [PubMed] [Google Scholar]
- 68Park SY, Lee KB, Lee MJ, Bae SC, Jang JJ. Nicotinamide inhibits the early stage of carcinogen-induced hepatocarcinogenesis in mice and suppresses human hepatocellular carcinoma cell growth. J Cell Physiol 2012; 227: 899–908. [DOI] [PubMed] [Google Scholar]