Abstract
Objectives
This study evaluated the association between currently recommended guidelines and commonly used clinical criteria for body mass index (BMI), waist circumference (WC), and waist-to-hip ratio (WHR) and all-cause mortality in frail older women.
Design
Longitudinal, prospective, cohort study.
Setting
Women’s Health Initiative – Observational Study.
Participants
A sample of 11,070 women aged 65–84 years with complete data to characterize frailty in the 3rd year of WHI study follow-up.
Measurements
Frailty phenotype was determined using modified Fried’s criteria. Anthropometric measures, (BMI, WC, and WHR) were collected by clinical examination. Cox proportional hazard models were used to estimate the effect of BMI, WC, and WHR on the rate of mortality adjusted for demographic and health behaviors.
Results
Over a mean follow-up of 11.5 years, there were 2,911 (26%) deaths in the sample. The hazard rate ratio (HR) for deaths in participants with BMI from 25-<30 kg/m2 and 30-<35 kg/m2 was 0.80 (95% confidence interval (CI) 0.73–0.88) and 0.79 (95% CI 0.71–0.88), respectively, compared with participants whose BMI was from 18.5-<25 kg/m2. Women with WHR >0.8 had a higher rate of mortality (HR 1.16, 95% CI 1.07–1.26) compared to women with WHR ≤0.8. No differences in mortality rates were observed by WC. Stratifying by chronic morbidity or smoking status or excluding women with early death and unintentional weight loss did not substantially change these findings.
Conclusion
In frail, older women, having a BMI between 25 and <35 kg/m2 or a WHR ≤0.8 was associated with lower rates of death. Currently recommended healthy BMI guidelines should be re-evaluated for older women with frailty.
Keywords: frailty, mortality, women’s health, obesity, body mass index
INTRODUCTION
Recent research has raised doubts about the role of obesity on mortality among older adults.1 Updated guidelines recommend using a body mass index (BMI) of at least 30 kg/m2 to identify adults of all ages at elevated risk of mortality from all causes.2 However, a meta-analysis of 97 studies with a combined sample size of almost three million adults failed to demonstrate a higher risk of death for adults 65 years of age and older with a BMI above 30 kg/m2 relative to those with a BMI of 18.5 to 24.9 kg/m2. 3
In contrast to BMI, which represents total body fat, indexes of fat distribution such as waist circumference (WC) and waist-to-hip ratio (WHR) might be more pertinent to negative health outcomes associated with excessive adiposity in the general population. 4,5 Persons with higher WC or WHR have a higher risk of obesity-related morbidity and mortality.6–9 Although evidence suggests that higher anthropometric measures were associated with worse health in older persons, the relationship between adiposity indexes and mortality has not been well examined in older adults with physical frailty.
Frailty is a distinct geriatric syndrome with phenotypical representation and etiology of multisystem dysregulation10 Frail older adults are at increased risk of disability, morbidity, and mortality compared with non-frail older adults. 10–12 Yet, it is unclear whether current guidelines and commonly used clinical criteria for BMI, WC and WHR are applicable to these individuals. Studies that investigated the relationship between BMI, frailty and mortality used non-frail participants as a reference category 11,13, limiting, thus, the capacity to understand the impact of BMI and other anthropometric measures among persons with frailty.
To address this gap, we evaluated the association between BMI, WC, and WHR and all-cause mortality in a large cohort of frail only, older women. We hypothesized that overall mortality would be associated with adiposity in frail persons. Because BMI, WC and WHR are indirect indicators of metabolic health, we expected that the rates of mortality would be lower for frail older women with normal adiposity and higher for those with increased adiposity.
METHODS
Study population
The Women’s Health Initiative Observational Study (OS) comprised of 93,676 women age 50 to 79 years at baseline (1993–1998) from 40 U.S. clinical centers. Details of the WHI study design and baseline characteristics have been reported elsewhere.14 The WHI study was approved by the institutional review boards at all 40 clinic sites and all participants provided written informed consent. At baseline and the first follow-up clinic visit, which occurred three years after baseline (1997–2001), OS participants completed questionnaires on medical and psychosocial characteristics and provided anthropometric measures, including BMI, WC, and WHR, which were clinically-assessed by trained medical staff. Because the sample was limited to those characterized as frail, the first follow-up visit was required to define the weight-loss component of frailty phenotype. Thus, the eligible sample were participants aged 65 years and older with a Year 3 clinic visit (n=55,654). Participants with missing data on at least one of the frailty criteria were further excluded (n=12,464). Among those remaining, 11,070 (26%) were characterized as frail and comprised the analytical sample for this study.
Frailty criteria
Frailty was operationally defined congruently with Fried’s definition10 as the presence of three or more of the following five criteria: muscle weakness, slow walking speed, exhaustion, low physical activity, and unintentional weight loss (shrinking). This operationalization was adapted and validated in the WHI 12 and has been extensively used in the WHI OS cohort. 12,15,16 For each criterion, one or two points were assigned if the participant’s assessment was below a criterion-specific cut-point. Points were summed to provide a score ranging from zero to five. A score of three or more was used to characterize a woman as frail. 10 Criteria-specific cut-points were based on the WHI frailty index12 and were described as follows:
| Frailty Criterion | WHI Measure (Point Assignment) |
|---|---|
| Muscle weakness Slow walking speed | RAND SF-36 Physical Function 17 score below 75 (2 points) |
| Exhaustion | RAND SF-36 Vitality 17 score below 55 (1 point) |
| Low physical activity | Lowest quartile on the WHI physical activity questionnaire (1 point) |
| Unintentional weight loss / shrinking | Weight loss >5% at Year 3 from weight at baseline and self-report of non intention to lose five or more pounds in the past 2 years (1 point) |
Anthropometric measures
At the Year 3 follow-up visit, trained staff clinically collected anthropometric measurements. Weight to the nearest 0.1 kilogram (kg) and height to the nearest 0.1 centimeter (cm) were measured and used to compute BMI. WC at the natural waist or narrowest part of the torso was measured to the nearest 0.1 cm. Hip measurements were obtained to the nearest 0.5 cm over nonbinding undergarments at the level of the fullest hip circumference. BMI categories were defined according to the NIH/NHLBI 18 classification: underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), class I obesity (30–34.9 kg/m2), class II obesity (35–39.9 kg/m2), and class III obesity (≥40 kg/m2). A standard clinical definition for central adiposity, defined as WC >88 cm and WHR >0.8 for women, was used. 2,6,7
All-cause mortality
Medical updates were collected annually by mail. Participants’ deaths were adjudicated by study physicians using hospital records, autopsy or coroner reports, and/or death certificates. Periodic checks of the National Death Index (NDI) for all participants, including those lost to follow-up, were performed. At the time of this analysis, the latest WHI data on mortality were available through December 1, 2013.
Covariates
Baseline data on demographic and health variables, including age, race/ethnicity, family income, highest level of education completed, smoking status (Never, Past, or Current), and history of common diseases related to body weight and mortality, such as cancer (excluding non-melanoma skin cancer), diabetes, emphysema, and cardiovascular disease were obtained by self-report. Previous studies have indicated smoking and the abovementioned preexisting conditions confound the relationship between obesity and mortality 19,20 and were found to be associated with prevalent and incident frailty. 12 Physical activity was assessed at the first follow-up clinical visit by self-report of frequency and duration of walking and mild, moderate, and strenuous activities, with total expenditure of energy calculated in metabolic equivalents (METs). 21
Statistical approach
The demographic and health behavior characteristics of participants with incomplete criteria to classify frailty were compared with those who had complete data in order to address the possibility of selection bias. For participants with complete frailty data, descriptive characteristics were examined by six BMI categories. Frequencies and means and standard deviations (SD) were estimated for categorical and continuous variables, respectively, and Chi square tests and analysis of variance (ANOVA) and were used to compare distributions across BMI categories. Crude rates of mortality per 1000 person-years by anthropometric indexes were calculated to express a number of deaths. Cox proportional hazards models were used to estimate the association of BMI categories and WC and WHR indexes on the all-cause mortality rate. Models are reported adjusted for baseline age only and then for baseline age, race/ethnicity, education, income, smoking status, number of frailty criteria, and physical activity. The time-to-event was defined as number of years from WHI Year 3 follow-up visit to death from any cause, with censoring at the last known contact or the date of last available NDI search, whichever occurred later. Because the relationship of BMI on mortality might be distorted by reverse causality of weight loss due to prodromal disease symptoms and inadequate adjustment for the effects of smoking and chronic morbidity, 22,23 regression models that stratified by the presence or absence of chronic conditions and by smoking status were also performed. A sensitivity analysis that excluded women who died within three years after the Year 3 follow up period was also completed. Since the frailty criteria includes a body-weight-change component, models that excluded participants with unintentional weight loss were also evaluated. Finally, to account for collinearity between central adiposity and BMI, post hoc analyses were conducted that examined the association of WHR and WC on mortality at different levels of BMI. WC and WHR indexes were categorized by using currently recommended guidelines and commonly used clinical cutpoints. Shoenfeld residuals were used to test proportionality across BMI and anthropometric measures. Reported p-values were two-tailed. Statistical analysis was completed using STATA, version 11.2 (StataCorp, College Station, TX).
RESULTS
Among the eligible sample of WHI-OS participants, 22.4% (n=12,464) had missing data on at least one of the frailty criteria. Compared with participants who had all frailty criteria available, those with missing data were older, less likely to be White, less educated, and more likely to smoke, have diabetes, and be obese (Table S1).
The mean (SD) age at baseline was 72.6 (4.6) years (range: 65–82) among the 11,070 frail women in the sample. At the Year 3 follow-up, one-third of the participants were overweight and 40.1% were obese. (Table 1). Women obese at Year 3 tended to be younger, non-White, have lower family incomes, and have a history of diabetes.
Table 1.
Baseline and Year 3 Characteristics of Frail WHI OS Participants (N = 11,070), by Body Mass Index (BMI in kg/m2) Category
| Characteristic | BMI category a
|
|||||
|---|---|---|---|---|---|---|
| <18.5 | 18.5–24.9 | 25.0–29.9 | 30.0–34.9 | 35.0–39.9 | ≥40.0 | |
| No. of participants | 143 | 2,714 | 3,702 | 2,581 | 1,163 | 690 |
| Age, in y a,h | 74.1 (4.3) | 73.5 (4.6) | 72.9 (4.5) | 72.1 (4.4) | 71.4 (4.3) | 70.1 (4.1) |
| BMI, kg/m2 a | 17.2 (1.1) | 22.6 (1.6) | 27.4 (1.4) | 32.2 (1.4) | 37.2 (1.4) | 44.8 (4.9) |
| White, n (%)b,h | 115 (80.4) | 2,402 (89.0) | 3,177 (86.1) | 2,183 (84.7) | 972 (84.0) | 548 (79.5) |
| Education, n (%)b,h | ||||||
| Some School | 46 (32.2) | 992 (36.7) | 1,488 (40.5) | 1,119 (43.7) | 518 (44.9) | 341 (49.6) |
| Some College | 61 (42.7) | 1,026 (38.0) | 1,358 (37.0) | 908 (35.4) | 387 (33.6) | 220 (32.0) |
| Some Graduate | 36 (25.2) | 683 (25.3) | 828 (22.5) | 536 (20.9) | 248 (21.5) | 126 (18.3) |
| Income, n (%)b,h | ||||||
| <$20,000 | 46 (34.1) | 585 (22.5) | 901 (25.5) | 686 (27.6) | 323 (28.7) | 210 (31.3) |
| $20,000–$50.000 | 56 (41.5) | 1,283 (49.3) | 1,734 (49.0) | 1,248 (50.2) | 596 (53.0) | 330 (49.1) |
| >$50,000 | 33 (24.4) | 733 (28.2) | 902 (25.5) | 552 (22.2) | 205 (18.2) | 132 (19.6) |
| No. of frailty criteria, n (%) a,c,h | ||||||
| 3 | 57 (39.9) | 1,590 (58.6) | 2,293 (61.9) | 1,498 (58.0) | 629 (54.1) | 332 (48.1) |
| 4 | 57 (39.9) | 907 (33.4) | 1,249 (33.7) | 1,011 (39.2) | 490 (42.1) | 346 (50.1) |
| 5 | 29 (20.3) | 217 (8.0) | 160 (4.3) | 72 (2.8) | 44 (3.8) | 12 (1.7) |
| Smoking status, n (%) a,h | ||||||
| Never | 66 (47.5) | 1,393 (52.2) | 1,885 (51.6) | 1,307 (51.3) | 620 (54.1) | 347 (51.0) |
| Past | 51 (36.7) | 1,037 (38.8) | 1,538 (42.1) | 1,107 (43.4) | 489 (42.7) | 301 (44.2) |
| Current | 22 (15.8) | 241 (9.0) | 228 (6.2) | 136 (5.3) | 37 (3.2) | 33 (4.9) |
| Physical activity, MET a,h | 6.0 (11.9) | 6.7 (9.6) | 6.1 (9.5) | 5.0 (8.0) | 4.4 (8.2) | 3.8 (7/7) |
| Cancer, n (%) b | 29 (20.4) | 477 (17.7) | 599 (16.3) | 445 (17.4) | 186 (16.2) | 106 (15.5) |
| Cardiovascular disease, n (%) b | 59 (42.8) | 867 (32.7) | 1,163 (32.3) | 772 (30.6) | 366 (32.2) | 212 (31.7) |
| Diabetes, n (%) b,h | 4 (2.8) | 106 (3.9) | 225 (6.1) | 223 (8.7) | 152 (13.1) | 110 (15.9) |
| Emphysema, n (%) b,h | 28 (20.1) | 256 (9.6) | 235 (6.5) | 171 (6.8) | 83 (7.3) | 50 (7.5) |
| WC, cmg,h | 65.7 (5.8) | 76.7 (6.9) | 87.8 (7.2) | 97.7 (8.0) | 107 (8.7) | 117.0 (12.3) |
| WC >88 cm, n (%) a,h | 2 (1.4) | 177 (6.6) | 1,773 (48.4) | 2,306 (90.2) | 1,138 (99.3) | 959 (98.0) |
| WHRg,h | 0.77 (0.1) | 0.80 (0.1) | 0.84 (0.1) | 0.86 (0.1) | 0.86 (0.1) | 0.86 (0.1) |
| WHR > 0.8, n (%) a,h | 38 (27.5) | 1,257 (47.0) | 2,511 (68.7) | 1,996 (78.2) | 913 (80.0) | 524 (78.3) |
| Frailty criteria a,c | ||||||
| Poor physical function d,hn (%) | 137 (95.8) | 2,671 (98.4) | 3,666 (99.0) | 2,567 (99.5) | 1,160 (99.7) | 689 (99.9) |
| Exhaustion e, n (%) | 102 (71.3) | 2,059 (75.9) | 2,762 (74.6) | 1,947 (75.4) | 878 (75.5) | 524 (75.9) |
| Low physical activity f,hn (%) | 86 (60.1) | 1,373 (50.6) | 2,045 (55.2) | 1,584 (61.4) | 770 (66.2) | 500 (72.5) |
| Weight loss g,hn (%) | 82 (57.3) | 709 (26.1) | 536 (14.5) | 233 (9.0) | 99 (8.5) | 38 (5.5) |
Notes: BMI = body mass index; CI = confident interval; WC = Waist circumference; WHI OS = Women’s Health Initiative Observation Study; MET =metabolic equivalent task; WHR = waist-to-hip ratio.
Measured at Year 3 WHI OS follow up
Measured at WHI OS baseline
Frailty was operationally defined as the presence of three or more of the following five criteria: muscle weakness, slow walking speed, exhaustion, low physical activity, and unintentional weight loss. To align the scoring with conventional frailty measure, poor physical function was scored as 2 points because the scale indicated both muscle strength and walking ability components
The RAND-36 Physical Function scale scores below 75.
The RAND-36 Vitality scale below 55.
The lowest quartile on the WHI physical activity questionnaire.
Weight loss > 5% between Year 3 and baseline, and “yes” to the question “in the past two years, did you lose five or more pounds not on purpose at any time?”
ρ<0.001 based on ANOVA analysis for continuous measures and chi square for categorical
Over a mean follow-up of 11.5 years (range 2.6–18.8), there were 2,911 (26%) deaths from all causes. The mean (SD) age at death was 83.7 (5.9) years. In general, crude rates of death, expressed in number of deaths per 1000 person-years, demonstrated a decrease in mortality with above-normal BMI. The adjusted HR (95% CI) for frail women who were overweight and class I obese was 0.80 (0.73–0.88) and 0.79 (0.71–0.88), respectively, compared to frail women with normal weight. Frail women with a WHR >0.8 had an adjusted HR of 1.16 (95% CI 1.07–1.26)\relative to those who had a WHI ≤0.8. The rate of mortality did not differ between those with WC >0.88 and those with lower WC (Table 2).
Table 2.
Association of BMI with All-Cause Mortality in Fraild WHI OS Participants
| Characteristic | Crude rates per 1000 pr-yr | Model 1a HR (95% CI) | p value | Model 2b HR (95% CI) | p value |
|---|---|---|---|---|---|
|
|
|
||||
| N = 10,977 | N = 10,295 | ||||
| BMI category, n (%) | |||||
| Underweight (<18.5 kg/m2) | 51.24 | 2.17 (1.69–2.78) | <0.001 | 1.91 (1.48–2.47) | <0.001 |
| Normal weight (18.5–24.9 kg/m2) | 27.82 | 1.00 | 1.00 | ||
| Overweight (25.0–29.9 kg/m2) | 21.12 | 0.75 (0.69–0.83) | <0.001 | 0.80 (0.73–0.88) | <0.001 |
| Class I Obesity (30.0–34.9 kg/m2) | 19.21 | 0.73 (0.66–0.81) | <0.001 | 0.79 (0.71–0.88) | <0.001 |
| Class II Obesity (35.0–39.9 kg/m2) | 21.38 | 0.88 (0.76–1.00) | 0.05 | 0.93 (0.81–1.07) | 0.28 |
| Class III Obesity (>40.0 kg/m2) | 20.59 | 0.96 (0.81–1.13) | 0.87 | 1.01 (0.85–1.21) | 0.86 |
|
| |||||
|
N = 10,910
|
N = 10,231
|
||||
| Waist categories | |||||
| ≤88 cm | 24.10 | Ref | Ref | Ref | Ref |
| >88 cm | 21.42 | 0.98 (0.91–1.06) | 0.63 | 1.02 (0.94–1.09) | 0.69 |
|
|
|
||||
|
N = 10,885
|
N = 10,209
|
||||
| Waist-to-hip ratio | |||||
| ≤0.8 | 20.83 | Ref | Ref | Ref | Ref |
| >0.8 | 23.45 | 1.18 (1.09–1.28) | <0.001 | 1.16 (1.07–1.26) | <0.001 |
Notes: pr-yr= person years; BMI = body mass index; CI = confident interval; HR = hazard ratio; Ref = Reference.
Adjusted for age.
Adjusted for age, race, education, income, number of frailty criteria, smoking status, and physical activity
Hazard ratios per standard deviation increase.
Frailty was operationally defined as the presence of three or more of the following five criteria: muscle weakness, slow walking speed, exhaustion, low physical activity, and unintentional weight loss.
Frail underweight women with chronic morbidity had a 2.4-fold higher rate (95% CI 1.78–3.03) of death relative to frail normal weight women. In contrast, the relative rate ratio was 1.16 (95% CI 0.68–1.98) for underweight women without chronic morbidity. When chronic morbidity was present, women with class I obesity had an HR (95% CI) of 0.85 (0.74–0.98) relative to normal weight women, but this rate was lowered further when chronic morbidity was absent (HR 0.69, 95% CI 0.58–0.83). Relative to normal weight women, overweight and class I and class II obese women had lower rates of death if they were ever smokers (Table 3), but among never smokers, this protection only remained for overweight and class I obese women. In our sensitivity analysis, we found that excluding those who died within 3 years after the Year 3 follow-up visit or those who experienced unintentional weight loss did not substantially change the estimates.
Table 3.
Subgroup analysis of the Association of BMI with All-Cause Mortality in Fraile WHI OS Participants a
| Characteristic | BMI category (in kg/m2) HR (95% CI)
|
|||||
|---|---|---|---|---|---|---|
| <18.5 | 18.5–24.9 | 25.0–29.9 | 30.0–34.9 | 35.0–39.9 | ≥40 | |
| Free of selected chronic conditions b (n = 4,981) | 1.16 (0.68–1.98) | Ref | 0.79 (0.68–0.92) | 0.69 (0.58–0.83) | 0.95 (0.75–1.19) | 1.09 (0.83–1.43) |
| Not free of selected chronic conditions b (n = 4,961) | 2.42 (1.78–3.03) | Ref | 0.79 (0.69–0.90) | 0.85 (0.74–0.98) | 0.84 (0.70–1.01) | 0.95 (0.76–1.19) |
| Never smoker (n = 5,330) | 1.60 (1.05–2.44) | Ref | 0.83 (0.72–0.96) | 0.80 (0.68–0.94) | 1.01 (0.83–1.23) | 1.12 (0.87–1.44) |
| Ever smoker (n = 4,965) | 2.23 (1.61–3.08) | Ref | 0.75 (0.66–0.86) | 0.74 (0.64–0.86) | 0.79 (0.65–0.96) | 0.86 (0.68–1.09) |
| Excluding early death c (n = 10,064) | 1.73 (1.28–2.32) | Ref | 0.78 (0.71–0.87) | 0.80 (0.71–0.89) | 0.87 (0.75–1.01) | 1.04 (0.87–1.25) |
| Frailty without weight loss criteria d (n = 8,698) | 1.35 (0.86–2.15) | Ref | 0.79 (0.70–0.88) | 0.77 (0.67–0.87) | 0.95 (0.82–1.11) | 1.02 (0.85–1.23) |
Notes: BMI = body mass index; CI = confident interval; WHI OS = Women’s Health Initiative Observation Study.
Adjusted for age, race/ethnicity, education, income, number of frailty criteria, smoking status and physical activity
Cancer, emphysema, cardiovascular disease, diabetes.
Death within 3 years of this study follow up
Excluding those who screened positively for weight loss.
Frailty was operationally defined as the presence of three or more of the following five criteria: muscle weakness, slow walking speed, exhaustion, low physical activity, and unintentional weight loss.
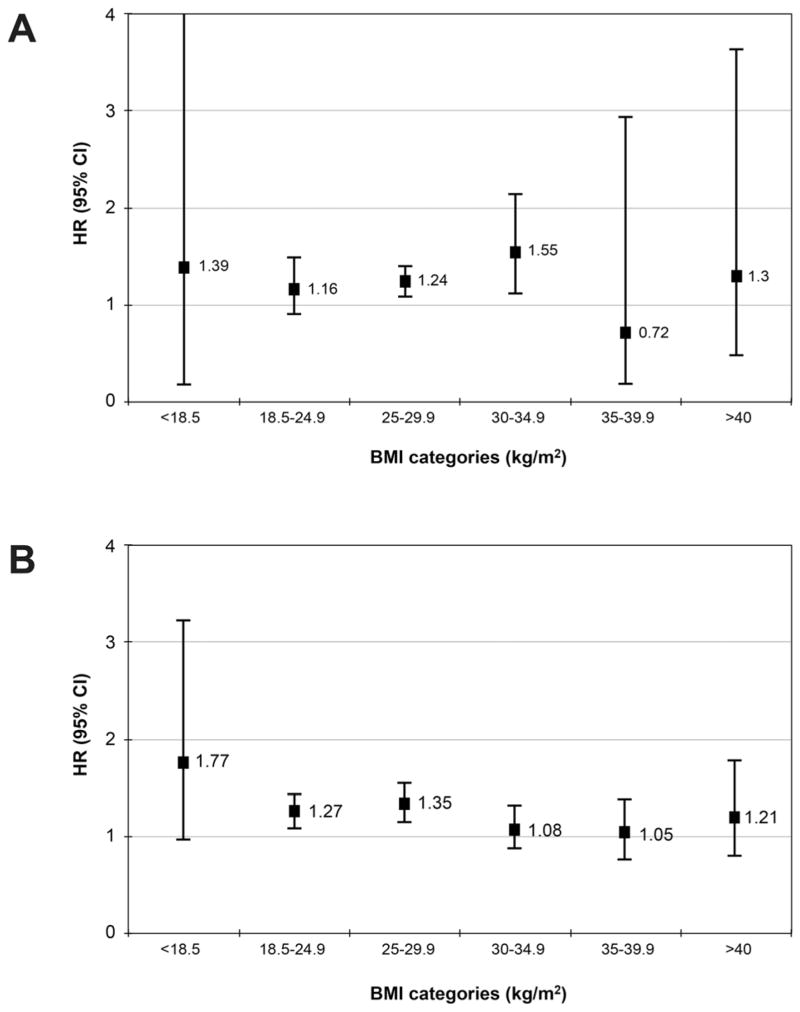
Figure 1 A illustrates that frail overweight and class I obese women with WC >88 cm had a higher rate of mortality compared with overweight and women with class I obesity who had WC ≤88 cm (HR 1.24, 95% CI 1.08–1.41 and HR 1.55, 95% CI 1.11–2.15, respectively). Frail normal and overweight women with WHR >0.8 had higher rates of death (HR 1.27, 95% CI 1.10–1.41 and HR 1.36, 95% CI 1.16–1.58, respectively) compared with the counterpart women who had WHR ≤0.8.
Figure 1.
Hazard ratios and 95% confidence intervals for all-cause mortality among frail Women’s Health Initiative Observational Study participants by body mass index category and according to (A) waist circumference ≤88cm (reference) vs. > 88 cm; (B) waist-to-hip ratio ≤0.8 (reference) vs. > 0.8. Models adjusted for age, race/ethnicity, education, income, number of frailty criteria, smoking status and physical activity. Frailty was operationally defined as the presence of three or more of the following five criteria: muscle weakness, slow walking speed, exhaustion, low physical activity, and unintentional weight loss.
DISCUSSION
Over an average 11.5 years of study follow-up, frail older women who were overweight or class I obese had a lower rate of all-cause mortality compared with frail women of normal weight. Differences in mortality rates in women with class II and class III obesity were not observed, likely because of lower power in these subgroups, and those analyses should be repeated in a larger population of frail older women with morbid obesity. In contrast, frail women with higher WHR (>0.8) had higher rates of death compared to those with lower WHR (≤0.8), while mortality rates did not differ when comparing women with higher WC (>0.88 cm) to those with lower WC (≤0.88 cm).
To our knowledge, this is the first study to evaluate the association of a variety of anthropometric measures on all-cause mortality in a sample of only frail, older adults. Most studies have examined these relationships in non-frail, older adults. A study using WHI data reported that obese women had higher odds of dying before reaching age 85 years compared to normal weight women. 24 A meta-analysis of 32 studies examining adults aged 65 years and older reported a U-shaped relationship between BMI and mortality, with the lowest hazard rates among those whose BMI was between 24 and 31 kg/m2 and with rates progressively rising for those with BMI >33 kg/m2.1 A few studies that examined the relationship of BMI and mortality compared frail to non-frail older adults. The Study of Osteoporotic Fractures in older women showed that frailty impacts mortality across all categories of BMI. However examination of the tables reported in the manuscript indicated that the impact of frailty on mortality tends to be less pronounced for overweight and obese women. 11 Another study by Lee and colleagues (2014) showed that obesity in persons with frailty was associated with increased rates of death when compared with non-frail individuals of normal weight. These findings however should be interpreted in light of the type of reference group used. Both studies used non-frail participants as the comparison category, which allowed for testing of effect modification by frailty status, rather than examining impact of BMI on mortality in those with frailty.
Consistent with our results, most studies in community-dwelling adults reported that WHR was a sensitive indicator of increased central adiposity and was associated with higher mortality risks. 4,5 In a meta-analysis that included more than 58,000 older adults higher rates of death among overweight and obese women with WC> 88 cm 8 were also observed. Likewise, several reports indicated an association between WC>88 cm and higher mortality in a subset of older and younger participants with normal BMI. 8, 25 Pending further research one caution interpretation is that an increased visceral adiposity or body shape with, to a some extent, lower trunk adiposity, may confer additional risk for mortality in those with frailty.
Stratifying by chronic morbidity, smoking status or excluding women with early death and unintentional weight loss did not substantially change our results. Although some suggested that the relationship of BMI on mortality might be influenced by reverse causality of weight loss due to pre-clinical symptoms and inadequate adjustment for the effects of smoking and chronic morbidity, 22,23 our sensitivity analyses were consistent with primary models further reinforcing the validity of the findings.
Excessive central adiposity increased the rates of all-cause mortality across most of the BMI categories, although the magnitude of the effect varied by BMI category. This suggests that body shape and fat distribution might have a different pathology for normal weight, overweight and obese women. This conclusion resonated in other studies that showed increased mortality risk for older adults with an increased WC or WHR measures across normal weight, overweight and obese BMI categories. 8,25
There are several possible methodological explanations for our findings. The first is misclassification of BMI cut-points as the best weight-for-height indicator. In older populations, BMI cut-points may be less sensitive to predict future morbidity and mortality than those seen in younger adults.26 As older adults’ body composition changes toward a decrease in lean tissue and height and an increase in fat tissue, the use of BMI may be an inherently biased proxy of overall obesity.27 Older adults have, on average, more fat than younger adults at any BMI, due to a loss of muscle mass with age. As a result, the sensitivity of BMI cut-points with respect to body fatness decreases with age, and the use of a fixed cut-point for all ages results in misclassification bias.28 The combination of increased fat mass and decreased lean body mass in frail older adults is especially pronounced,29 rendering the frail population more susceptible to this misclassification bias. Importantly, this non-differential misclassification bias can only lead to underestimation of the true strength of the associations.
A second explanation may be “survival effect.” Individuals who are susceptible to the complications of obesity may have died at a younger age, and overweight and obese individuals who survive to old age may have characteristics that protect them from the adverse effects of being overweight or obese.27
A third explanation is reverse causation.22 Unintentional weight loss caused by unrecognized systemic illness can lead to a misclasification of the mortality risk of the “healthy” weight reference group, thereby making the obese group seemingly protected.27 To address this potential concern, we repeated the analysis excluding frail women who died within 3 years of follow-up and the results did not change. Thus, reverse causation is less likely to explain our findings.
Finally, confounding factors, most importantly smoking status, were also considered in our multivariate models. Since smokers are thinner 30 and have increased risk for mortality, residual confounding of smoking may make obese groups seem protected. However, restricting the analysis to never-smokers did not reverse the lower risks observed among those with class I obesity.
Others researchers have hypothesized a causal protective association between excessive weight and lower mortality31–33. Specifically, overweight and obesity may benefit older adults by exerting a favorable effect on cognitive function,31 protecting against osteoporotic fractures,32 and serving as an energy reserve against protein-energy malnutrition.33 The last assertion might be particularly pertinent to frail, older adults because higher protein consumption, as a fraction of total energy, has been associated with a strong, independent, dose-responsive favorable effect on functioning in older women.15 Thus, pending further research, a cautious interpretation of these results is that salutary effects of overweight and obesity on long-term mortality in older frail female populations might be channeled through anabolic processes.
The strengths of this study include the large sample size of frail older women, the use of well-validated frailty criteria, the use of objectively assessed anthropometric measures, and a long study follow-up with adjudicated mortality protocols. The long follow-up is important since many years of obesity are required to induce harmful effects on health, and studies with a short follow-up may not sufficiently demonstrate an association between obesity and mortality.34 We were also able to adjust for important potential confounders including a measure of physical activity, which has been demonstrated to moderate the relationship between body mass and functional impairment 35 and adiposity and mortality. 36
Our study has limitations. Lack of objective physical performance measures in the operationalization of frailty is a likely weakness of the WHI frailty index. Although the RAND-36 physical function scores is a valid measure 17, it has been shown to have low to moderate correlation compared with objectively measured values. 12 As with any observational study, there exists the possibility of residual and unmeasured confounding. Given a preponderance of White women participants, our results may not be widely generalizable. We were unable to classify frailty in nearly a quarter of our eligible sample. Women with these missing data were older, had poorer health, and were more likely to be obese. While it is unclear how many of these women would have been regarded as frail, in light of these differences, the results should be interpreted conservatively since they might represent an overestimation of the associations. Furthermore, although our results might provide preliminary insights into the association of total and central adiposity indexes with mortality, biological validity of the findings in the context of direct measures of body composition and their effects on health outcomes in frail population have not been thoroughly examined. In the general population, body adiposity indexes and percentage body fat are highly related 37 and show consistency in the context of attributable fractions of death, 38 but these associations have not been established in those with frailty. Finally, change in adiposity over time rather than single occasion measures might provide more nuanced information on whether the risk of developing adverse outcomes is greater or less for frail persons with distinct longitudinal dynamics in body composition measures.
In conclusion, overweight and obesity may be associated with lower rates of all-cause mortality in frail, older women. Currently recommended guidelines for a healthy BMI range might not be suitable for older women with frailty and weight management recommendations should account for older adults’ functional and physiological status.
Supplementary Material
Acknowledgments
The authors thank the WHI investigators and staff for their dedication and the study participants for making the program possible. A listing of WHI investigators can be found at: https://cleo.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Short%20List.pdf
The WHI program is funded by the National Heart, Lung and Blood Institute, National Institute of Health, U.S. Department of Health, and Human Services through Contracts N01WH22110, 24152, 32100-2, 32105-6, 32108-9, 32111-13, 32115, 32118-32119, 32122, 42107-26, 42129-32, and 44221.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions
Drs. Zaslavsky, Rillamas-Sun, LaCroix and Zelber-Sagi had full access to all of the data used in the study and take responsibility for the integrity of the data and accuracy of data analysis. Zaslavsky, Rillamas-Sun, Woods, LaCroix, Zelber-Sagi: study concept, design, interpretation of data, and preparation of manuscript. Zaslavsky, Zelber-Sagi, Rillamas-Sun: data analysis and visualization. Zisberg, Shadmi, Woods, Cochrane, Edwards, Kritchevsky, Stefanick, Tinker, Vitolins, Wactawski-Wende: preparation of manuscript.
Sponsor’s Role: The funding agencies had no role in the design and conduct of this study, the analysis or interpretation of the data, or the preparation of the manuscript.
References
- 1.Winter JE, MacInnis RJ, Wattanapenpaiboon N, et al. BMI and all-cause mortality in older adults: A meta-analysis. Am J Clin Nutr. 2014;99:875–890. doi: 10.3945/ajcn.113.068122. [DOI] [PubMed] [Google Scholar]
- 2.Jensen MD, Ryan DH, Apovian CM, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society . Circulation. 2014;129(suppl 2):S102–S138. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Myint PK, Kwok CS, Luben RN, et al. Body fat percentage, body mass index and waist-to-hip ratio as predictors of mortality and cardiovascular disease. Heart. 2014;100:1613–1619. doi: 10.1136/heartjnl-2014-305816. [DOI] [PubMed] [Google Scholar]
- 5.Petursson H, Sigurdsson JA, Bengtsson C, et al. Body configuration as a predictor of mortality: Comparison of five anthropometric measures in a 12 year follow-up of the Norwegian HUNT 2 study. PLoS One. 2011;6:e26621. doi: 10.1371/journal.pone.0026621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heo M, Kabat GC, Strickler HD, et al. Optimal cutoffs of obesity measures in relation to cancer risk in postmenopausal women in the Women’s Health Initiative Study. J Womens Health. 2015;24:218–227. doi: 10.1089/jwh.2014.4977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kerwin DR, Gaussoin SA, Chlebowski RT, et al. Interaction between body mass index and central adiposity and risk of incident cognitive impairment and dementia: Results from the Women’s Health Initiative Memory Study. J Am Geriatr Soc. 2011;59:107–112. doi: 10.1111/j.1532-5415.2010.03219.x. [DOI] [PubMed] [Google Scholar]
- 8.de Hollander EL, Bemelmans WJ, Boshuizen HC, et al. WC elderly collaborators. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: A meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Int J Epidemiol. 2012;41:805–817. doi: 10.1093/ije/dys008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lisko I, Tiainen K, Stenholm S, et al. Body mass index, waist circumference, and waist-to-hip ratio as predictors of mortality in nonagenarians: The Vitality 90+ Study. J Gerontol A Biol Sci Med Sci. 2011;66:1244–1250. doi: 10.1093/gerona/glr147. [DOI] [PubMed] [Google Scholar]
- 10.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 11.Ensrud KE, Ewing SK, Taylor BC, et al. Frailty and risk of falls, fracture, and mortality in older women: The study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007;62:744–751. doi: 10.1093/gerona/62.7.744. [DOI] [PubMed] [Google Scholar]
- 12.Woods NF, LaCroix AZ, Gray SL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women’s Health Initiative Observational Study. J Am Geriatr Soc. 2005;53:1321–1330. doi: 10.1111/j.1532-5415.2005.53405.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee Y, Kim J, Han ES, et al. Frailty and body mass index as predictors of 3-year mortality in older adults living in the community. Gerontology. 2014;60:475–482. doi: 10.1159/000362330. [DOI] [PubMed] [Google Scholar]
- 14.Anderson GL, Manson J, Wallace R, et al. Implementation of the Women’s Health Initiative study design. Ann Epidemiol. 2003;13:S5–S17. doi: 10.1016/s1047-2797(03)00043-7. [DOI] [PubMed] [Google Scholar]
- 15.Beasley JM, LaCroix AZ, Neuhouser ML, et al. Protein intake and incident frailty in the Women’s Health Initiative observational study. J Am Geriatr Soc. 2010;58:1063–1071. doi: 10.1111/j.1532-5415.2010.02866.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LaCroix AZ, Gray SL, Aragaki A, et al. Statin use and incident frailty in women aged 65 years or older: Prospective findings from the Women’s Health Initiative Observational Study. J Gerontol A Biol Sci Med Sci. 2008;63:369–375. doi: 10.1093/gerona/63.4.369. [DOI] [PubMed] [Google Scholar]
- 17.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 18.National Institutes of Health. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults—The Evidence Report. Obes Res. 1998;6(suppl 2):51S–209S. [PubMed] [Google Scholar]
- 19.Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 20.Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1. 46 million white adults. N Engl J Med. 2010;363:2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM, Graubard BI, Williamson DF, et al. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am J Epidemiol. 2011;173:1–9. doi: 10.1093/aje/kwq341. [DOI] [PubMed] [Google Scholar]
- 23.Tobias DK, Pan A, Jackson CL, et al. Body-mass index and mortality among adults with incident type 2 diabetes. N Engl J Med. 2014;370:233–244. doi: 10.1056/NEJMoa1304501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rillamas-Sun E, Lacroix AZ, Waring ME, et al. Obesity and late-age survival without major disease or disability in older women. JAMA Intern Med. 2014;174:98–106. doi: 10.1001/jamainternmed.2013.12051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coutinho T, Goel K, Correa de Sa D, et al. Central obesity and survival in subjects with coronary artery disease: A systematic review of the literature and collaborative analysis with individual subject data. J Am Coll Cardiol. 2011;57:1877–1886. doi: 10.1016/j.jacc.2010.11.058. [DOI] [PubMed] [Google Scholar]
- 26.Sorkin JD. BMI, age, and mortality: The slaying of a beautiful hypothesis by an ugly fact. Am J Clin Nutr. 2014;99:759–760. doi: 10.3945/ajcn.114.084780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oreopoulos A, Kalantar-Zadeh K, Sharma AM, et al. The obesity paradox in the elderly: potential mechanisms and clinical implications. Clin Geriatr Med. 2009;25:643–659. doi: 10.1016/j.cger.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 28.Baumgartner RN, Heymsfield SB, Roche AF. Human body composition and the epidemiology of chronic disease. Obesity Res. 1995;3:73–95. doi: 10.1002/j.1550-8528.1995.tb00124.x. [DOI] [PubMed] [Google Scholar]
- 29.Cesari M, Leeuwenburgh C, Lauretani, et al. Frailty syndrome and skeletal muscle: Results from the Invecchiare in Chianti study. Am J Clin Nutr. 2006;83:1142–1148. doi: 10.1093/ajcn/83.5.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Albanes D, Jones DY, Micozzi MS, et al. Associations between smoking and body weight in the US population: Analysis of NHANES II. Am J Public Health. 1987;77:439–444. doi: 10.2105/ajph.77.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han C, Jo SA, Seo JA, et al. Adiposity parameters and cognitive function in the elderly: Application of “Jolly Fat” hypothesis to cognition. Arch Gerontol Geriatr. 2009;49:e133–e138. doi: 10.1016/j.archger.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 32.Johansson H, Kanis JA, Oden A, et al. A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res. 2014;29:223–233. doi: 10.1002/jbmr.2017. [DOI] [PubMed] [Google Scholar]
- 33.Stini WA. Body composition and longevity: Is there a longevous morphotype? Med Anthropol. 1991;13:215–229. doi: 10.1080/01459740.1991.9966049. [DOI] [PubMed] [Google Scholar]
- 34.Zamboni M, Mazzali G, Zoico E, et al. Health consequences of obesity in the elderly: A review of four unresolved questions. Int J Obes. 2005;29:1011–1029. doi: 10.1038/sj.ijo.0803005. [DOI] [PubMed] [Google Scholar]
- 35.Lang IA, Guralnik JM, Melzer D. Physical activity in middle-aged adults reduces risks of functional impairment independent of its effect on weight. J Am Geriatr Soc. 2007;55:1836–1841. doi: 10.1111/j.1532-5415.2007.01426.x. [DOI] [PubMed] [Google Scholar]
- 36.Hu FB, Willett WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. New Engl J Med. 2004;351:2694–2703. doi: 10.1056/NEJMoa042135. [DOI] [PubMed] [Google Scholar]
- 37.Flegal KM, Shepherd JA, Looker AC, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr. 2009;89:500–508. doi: 10.3945/ajcn.2008.26847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Flegal KM, Graubard BI. Estimates of excess deaths associated with body mass index and other anthropometric variables. Am J Clin Nutr. 2009;89:1213–1219. doi: 10.3945/ajcn.2008.26698. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.