Abstract
Successful clinical management of glaucoma should not simply be about control of intraocular pressure, but must equate to correct decisions about intensifying treatment when patients are at risk of developing ‘visual disability'. Yet little is known about what visual field defects, at different stages of glaucoma, specifically affect patients' abilities to perform everyday visual tasks. One way to do this is to measure patient performance in tasks in a lab setting. Another way is to ask patients themselves. The latter can be revealing and demystify views about how patients perceive the world. This short commentary highlights some of the current research in this area.
Introduction
Open angle glaucoma is a chronic disease of the optic nerve that can cause sight loss, predominantly affecting the visual field. It is common for most articles reporting clinical and research developments in glaucoma to begin with an emphasis on the risk of irreversible blindness associated with the disease. Indeed, glaucoma is a leading cause of permanent blindness worldwide and the second major cause for blind registration (severely sight impaired) in the UK. Further, a significant percentage of elderly people have a diagnosis of glaucoma yet around half of people with the condition remain undetected. Nevertheless, I would prefer the readers of this commentary to better remember the following. That is, while the risk of blindness is real and of concern for both clinician and patient it is, however, fair to say that most people with a diagnosis will not go blind. Estimates for this vary1 but it might be reasonable to suggest about 1 in 20 treated patients have a real lifetime risk of serious visual impairment and there is evidence to support this from data collected in UK clinics.2, 3 Nevertheless, loss of visual field before it reaches the stage of causing advanced loss of sight affects patients' everyday life and this is central to the discussion in this article. This should not be underestimated. Nor should the constant fear of losing sight in those diagnosed be underestimated. After all, vision is the sense that people fear losing most.4
Glaucoma certainly impacts on quality-of-life and state-of-mind5, 6 but little is known about the precise relationship between functional measurements made in the clinic and patient's visual disability. This isn't surprising because untangling the visual component from all the other factors that contribute to everyday visually guided tasks such as mobility, driving, searching for items, recognising faces, and reading is difficult to do. Nevertheless, the research activity devoted to this challenge is insufficient;7 this is a pity, because meaningful landmarks for disease progression in glaucoma would help in managing patients. Furthermore, the benchmark for a new treatment success in a clinical trial should really be aligned to measureable reduction in visual disability rather than often imperceptible changes on a clinical visual field or visual acuity chart.
This brief commentary aims to throw a spotlight on the evidence linking loss of visual field in glaucoma and the ability to carry out visually guided tasks. I also make suggestions about how the visual field should be quantified for this purpose and highlight how patients seem to perceive their vision loss. The latter is often misrepresented and misunderstood; I propose this becomes tangled up with patients' difficulties with adherence to treatment making the asymptomatic nature of the condition the real danger for the majority of people affected by the disease.
This short article, as the title suggests, is a view on glaucoma substantiated by work carried out in my research laboratory and elsewhere. It is, however, important to note that the article is not a systematic review and should not be interpreted as one. It is also very important to state that the article is not written by a clinician, although I am fortunate to work closely with many excellent ones. Moreover, I do not interact daily with patients although I have worked with many in a research environment and I have spent an inordinate amount of time (too much time) analysing vast quantities of patient data.
I was very privileged to give the Edridge Green Lecture at The Royal College of Ophthalmologists Annual Congress at Liverpool in May 2015 and this article is loosely based on the material presented at that occasion.
The burden of glaucoma
The burden of glaucoma in the UK is well-described in an excellent review by King et al.8 Treatment of glaucoma, which focuses almost entirely on lowering IOP (the only modifiable risk factor for the disease), can prevent or slow loss of vision but patients need lifelong monitoring. Therefore, management of patients absorbs significant resources. For example, more than one million glaucoma-related visits are made to UK hospital eye services per year. Moreover, the social and economic burden of glaucoma will increase as the elderly population grows.
There is a silent burden of glaucoma too because a large proportion of people remain undiagnosed. Worryingly this ‘missing' group is more likely to include socio-economically deprived people with no family history of glaucoma and people who do not visit their optometrist.9, 10 The spontaneous case-finding by the community optometrist is after all the main way the disease is detected in a timely manner in the UK. On the whole, UK optometrists do this well. Yet, in a large proportion of those that are diagnosed the disease is already quite advanced. For example, we recently assessed visual field charts from >25 000 patients diagnosed in the last 10–15 years.11 From this, we showed that one-fifth of newly diagnosed patients with VF loss have damage that automated perimetry would classify as advanced in at least one eye. This is indeed a concern because patients with more advanced glaucoma at diagnosis are at greatest risk of visual impairment.2
Of course the real burden of glaucoma lies with the individual patients and their families. This often manifests itself as ‘visual disability', which can be defined as the impact on carrying out visually guided tasks. This theme has been a subject of a programme of work in my research lab for the last few years and is now discussed. But first, how should we measure the functional impact of glaucoma?
How best to quantify functional loss in glaucoma?
As mentioned, IOP is the only modifiable risk factor for disease progression in glaucoma. It is understandable, therefore, that IOP becomes the centre of attention in follow-up and management of the patient or the glaucoma suspect. Results from audit work in several clinics across the UK support this notion.12 Examination of the optic nerve and associated structures is also central to assessment of glaucoma. After all, this is the site of glaucoma ‘injury' and is intrinsic to follow-up. Advances in imaging technology now readily available to the clinic, like optical coherence tomography, infer the feasibility of objectively measuring structural progression in glaucoma. Yet the research community still struggles with the link between these structural assessments and how they impact on visual function; an excellent recent review is given by Malik et al.13
I suggest the most important measure for disease progression in glaucoma is the functionally relevant assessment of the visual field; it certainly ought to be a key determinant in assessing effectiveness of treatments in a clinical trial setting. Unfortunately, effective visual field assessment can be difficult and identifying changes in follow-up (progression) beyond the measurement variability is a well-known thorny issue.14, 15 Perimetry is also perceived to be challenging by clinicians and patients; although listening to the latter could lead to improvements in how it is carried out.16, 17 Allocating perimetry resources correctly and installing perimetry at the centre of glaucoma follow-up is also a challenge.18
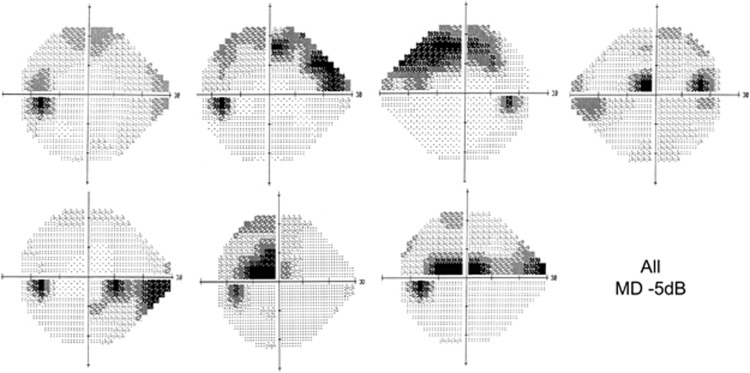
Next, how do we best summarise visual field loss and the worsening of visual field loss? This is often done with a number (or series of numbers). For example, one commonly deployed perimetric index derived from the Humphrey Visual Field Analyzer (Carl Zeiss Meditec, CA, USA) is the Mean Deviation (MD); this is a standard measure of the overall severity of a VF defect, relative to healthy age-matched observers, with more negative values indicating greater VF loss. Summarising a patient's visual field with a single number can be useful but has an important drawback as illustrated in Figure 1. Considering the actual location and spatial extent of visual field loss is likely to be more helpful, especially when considering how the visual field loss impacts on the person's sight loss. Methods of analysis quantifying every single point in the visual field (pointwise methods) are more sensitive to subtle changes in vision and these have been successfully implemented in clinical trials.19, 20 Ever more statistically sophisticated pointwise methods have been developed but their adoption is limited because they are not readily available to the clinician.21, 22, 23 We have made some progress with this, and new glaucoma progression audit tools are soon to be made available on the Medisoft Ophthalmology electronic patient record (Medisoft Ltd., Leeds, UK).
Figure 1.
Humphrey visual field grayscale representations for seven different eyes. The location and spatial extent of the visual field defect is different for each eye but the mean deviation value is—MD =−5 dB for each case. Therefore, information is 'lost' when we only consider the visual field indices.
A binocular measure is likely to be the best way to predict the impact of visual field impairment on visual disability.24 However, in clinical settings, perimetry resources are almost exclusively dedicated to monocular assessment and binocular testing is rarely carried out. An alternative to some summary measure of the better eye, such as the MD from the ‘better eye', is the integrated visual field (IVF); this is simply estimated from monocular results, taking the best sensitivity values from corresponding visual field locations and requires no extra testing. We have recently shown that monocular visual field measures can give the impression that a patient's vision is more degraded than it might be under binocular viewing, certainly in advanced cases, and the IVF is proposed to be a rapid assessment of the person's working visual field.25 The locality of an IVF defect might be much more important than a summary measure and there are some imaginative studies that have highlighted this.26 We have recently attempted to derive clinically meaningful estimates of the prevalence of different types of binocular visual field loss, because this ought to inform how we should assess those with advanced bilateral glaucoma.27
Assessing visual disability in glaucoma
The majority of studies examining visual disability in glaucoma are based on self-report questionnaires, commonly referred to as patient-reported outcome measures (PROMs). Asking patients directly is the best way to ascertain how someone actually feels about their condition. Indeed, much of the best research in the area of visual disability and glaucoma has used this methodology yielding sound evidence to show that patients with the condition have difficulties with mobility, driving, reading and other everyday tasks.28, 29 PROMs are, however, potentially limited by subjectivity, different personal expectations and knowledge of disease.30
Aside from their use in research studies, PROMs are not routinely used in clinical practice. PROMS are, however, becoming a method for measuring outcomes in clinical trials for glaucoma treatment. For example, some on-going UK trials on different treatment approaches use PROMs as the primary outcome measure.31 There is a good rationale for having outcomes that are directly relevant and meaningful to the patient. At the same time, the advantages of using PROMs in this scenario instead of clinical measures of functional loss, like automated perimetry, is open to debate, especially when the aim might be to have high sensitivity to rapidly determine small changes in vision.
From a research perspective, we can also try to understand visual disability in glaucoma by measuring the patient's actual performance in real-life tasks or surrogates of tasks they would encounter every day. Tasks previously investigated include, for example, mobility performance in terms of ability to navigate around an obstacle course, driving using simulations, and examinations of postural sway and balance. At City University London, we have used this approach to measure patients' performance in search tasks, driving hazard perception, face recognition, and reading under different conditions. It has even been shown that a set of such tasks could be used in a clinical setting if they are skillfully designed with practicality in mind.32, 33
Aspects of visual disability in glaucoma
What follows is a brief description of visually guided activities that are affected by moderate to advanced visual field loss in glaucoma, as suggested by our studies and supported by others. For more complete reviews on visual disability in glaucoma, the interested reader is directed towards two excellent surveys of the literature by Ramulu and colleagues.28, 34
Difficulty with reading is a common complaint made by patients with glaucoma. Studies measuring actual reading performance have revealed that patients with moderate-to-severe visual field loss have, on average, impaired reading speed, especially when text size is small or is presented at low contrast.35, 36 Other work has revealed that differences in average reading speeds between glaucoma patients and normally sighted peers are particularly pronounced during periods of sustained silent reading.37 Patients with advanced loss also have difficulty following a line of print.38 A common feature of these studies is that reading performance (reading speed) is subject to much between-person variability—even imaginative designs can only tease out small average differences between patients and controls.39 It is fair to say, however, that many patients with advanced visual field loss, even with preserved visual acuity, have measurable difficulty with reading.40
Patients with advanced visual field loss also have problems with mobility tasks, such as reaching and grasping objects.41 Walking and balance is affected by glaucomatous visual field loss.42 Patients are more likely to fall, with contributory factors being problems with balance and presence of a scotoma in the inferior visual field.43, 44 Interestingly many patients, even with moderate visual field loss, have a fear of falling and there is good evidence that patients limit their own mobility.45, 46, 47
Glaucoma undoubtedly impacts on an individual when visual field loss causes the removal of a driving licence, and several studies have shown that certain glaucomatous visual field defects are not compatible with safe driving.48, 49 Interestingly, it has been demonstrated that UK patients perceive this particular potential outcome of their disease to be as serious to them as the long-term risk of blindness.50 Patients are at greater risk of motor vehicle collisions and many patients stop driving even when the visual field loss is moderate.48, 51 A plausible mechanism for issues in driving among glaucoma patients is that they have more difficulty seeing peripheral objects. Indeed, one study found that patients with glaucoma were less likely to see pedestrians on the side of the road during actual road tests.48 This observation is supported by our lab-based studies using the driving hazard perception test (HPT), which is an element of the UK driving licence theory test.52 In this test the ‘learner driver' is shown a film of a real driving scene, seen from the perspective of the driver, with the task being to detect potential ‘hazards': these are defined as something that would make the camera car take evasive action, such as braking for an oncoming cyclist or a pedestrian unexpectedly crossing the road. Primarily, it is a useful educational tool allowing learner drivers to encounter ‘on road' driving scenes from the safety of a computer monitor. More recently, we have combined this with a gaze-contingent set-up to investigate the impact of simulated visual field defects on HPT performance; this allows a person with normal vision to experience a distortion in their visual field, which moves with their gaze. Results suggested that performance of drivers on the HPT was significantly impaired when parts of their superior and inferior visual fields were obscured.53 It is important to reiterate that driving is indeed consistently cited as one of the main issues for the patient with a diagnosis of glaucoma.54 We certainly need better evidence-based tests for determining those patients who are fit to drive and this might be determined by a variety of methods using driving simulators and collision data.55, 56, 57, 58
Other vision-related tasks also seem to be inhibited by glaucomatous visual field loss. The lighting conditions under which tasks are performed may be even more important that the task itself and this warrants further research. Patients self-report difficultly with glare and moving between environments where lighting changes.59 We have also shown that patients with advanced visual field loss have difficulty with searching for everyday objects and face recognition.60, 61 These studies took advantage of experiments that also tracked subjects' gaze as they carried out the tasks.62 The results suggested that eye movements may give a clue about individual's performance with a hint that compensatory behaviour is involved.63 Recently, we have shown that eye movements recorded while a patient passively watches an ordinary movie might suggest functional loss.64
How does glaucoma look? End of the black tunnel?
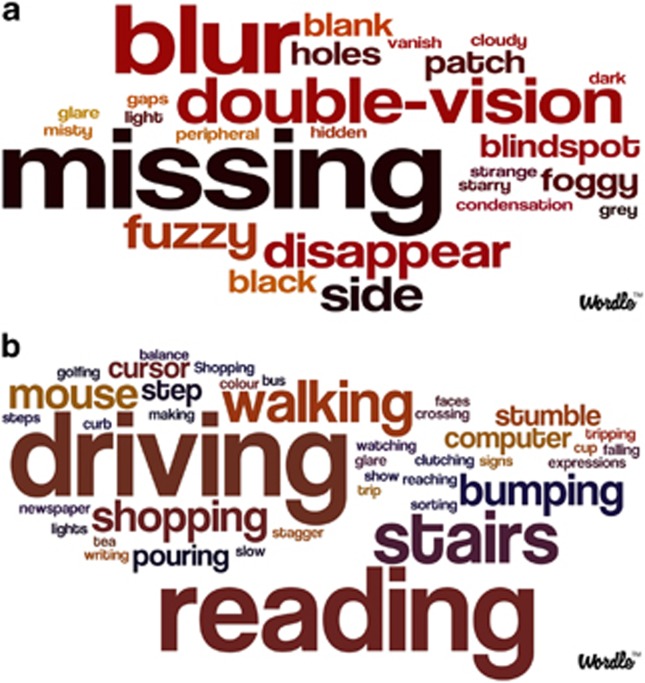
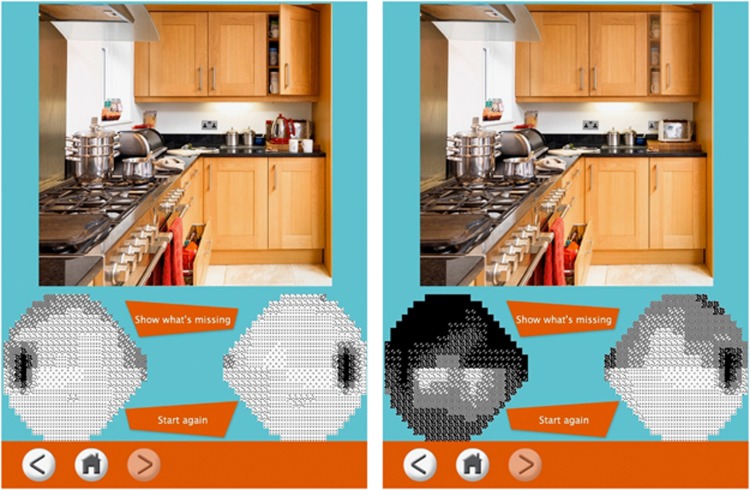
And what do patients really see when they have glaucoma? This simple question seems intrinsic to how patients perceive their condition and how it affects them. In modern times the ‘oracle' for such a question, say for a newly diagnosed patient, is the internet. Yet a cursory search yields images implying that a patient's perception of the world is through a ‘black tunnel', or with parts of the field-of-view obscured by ‘black patches'. Most clinicians and most patients know these descriptions to be misnomers. Perception with visual field loss is a complex compensatory process using both eyes and the brain filling in ‘missing parts'. More accurately portraying the symptoms of vision loss in glaucoma would aid raising awareness of the true symptoms (or lack of symptoms) of the condition—particularly important since estimates of those with the disease who remain undiagnosed are so high. Second, it might help patient adherence to treatment, especially if they have been falsely reassured about not having the ‘severe' symptoms depicted by the typical images of how glaucoma ‘looks'. We recently addressed this with a study of a very simple design where we solely asked patients to describe what they ‘see'.65 We also asked patients, all of whom had visual field loss in both eyes, to choose a picture that best depicted their visual symptoms (Figure 2). Unsurprisingly, no patients chose images with black patches or the ‘black tunnel', with many eloquently describing how parts of their field-of-view are missing or are distorted with a ‘blur' (Figure 3a). It was particularly striking that one in four of these patients reported no symptoms whatsoever even though they had bilateral VF loss, with most having at least moderate damage in their better eye. Patients also described the activities during which they noticed their impairment; these interviews were subjected to a type of semantic analysis and the results support previous findings about the daily activities most affected, along with some newer ones such as computer use, watching sports, and carrying out tasks in the kitchen, like pouring liquids (Figure 3b).
Figure 2.
Six images were shown to 50 patients with bilateral visual field defects. For all six, the same outdoor scene image was used but each was manipulated to provide views of the image obscured and degraded in a range of distinct ways. None of the 50 participants in this study chose the image altered to have ‘a tunnel with black edges' effect or the image with ‘black patches'. Thirteen participants (26%) were completely unaware of their VF defect affecting their visual function, choosing the original unedited image. Twenty-seven (54%) and eight (16%) participants chose the images with ‘blurred patches' and ‘missing patches', respectively. The ‘missing patches' is a very subtle but potentially realistic effect (see the red car) because we used a photograph filling tool to replace the missing parts with the background. Only two participants chose the image with a ‘tunnel with blurred edges' (4%).
Figure 3.
A word cloud showing the occurrence of descriptors of glaucomatous vision loss calculated as the number of participants who used the term (a). The size of a word in the visualisation is proportional to the frequency of its use. Similarly, a word cloud of named everyday activities where visual field loss was noticed by an individual is shown in b.
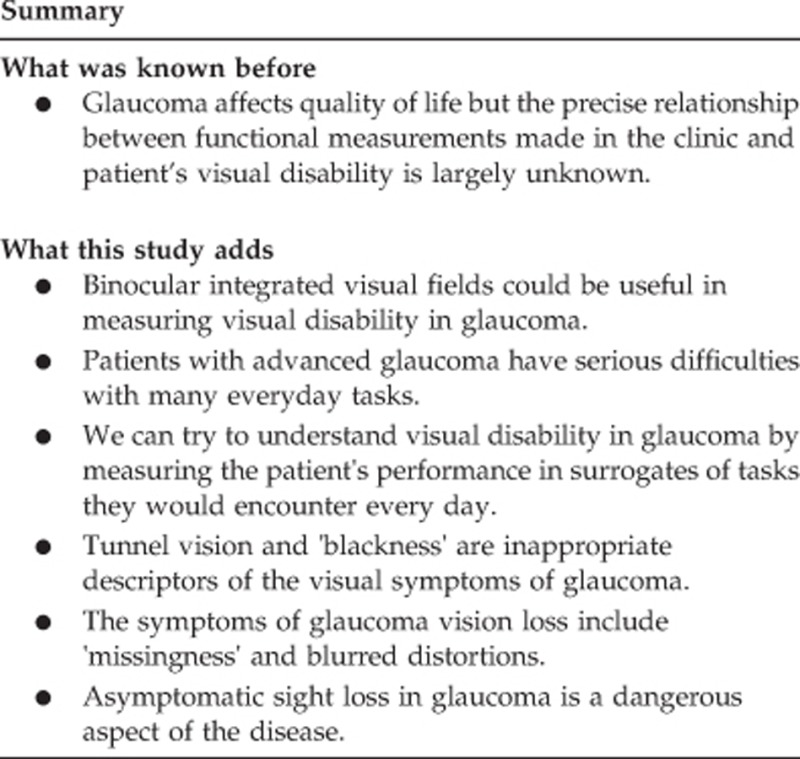
It seems sensible to provide patients and their families with better visual information about the true symptoms, or lack of symptoms with glaucoma. We have attempted to do this recently with an App (Glaucoma in Perspective, Allergan PLC, Dublin, Ireland) that can be used on a tablet computer.66 This is useful because it allows the user to directly interact with a visual field map and see the effect (or no effect) of different levels of binocular visual field loss on the degradation of everyday scenes (Figure 4).
Figure 4.
Screenshots of the Glaucoma in Perspective App designed for patients to demonstrate the subtle effect of visual field loss.66 The user can use the touch screen to draw visual field defects on both eyes. Overlapping defects manifest in the image changing. In this example, a very subtle change occurs in the kitchen scene (right), with kettle and coffee mugs disappearing from the work surface (left), an electric socket disappearing, and an open kitchen cabinet door starting to appear blurred.
Discussion
Since this article is about ‘views' it seems appropriate to offer some speculation. We have closely examined hundreds of glaucoma patients in performance tasks in London and it strikes me that many perform equally as well as their normally sighted peers. This is certainly apparent in those with early or even moderate visual field damage. It is likely that a ‘tipping point' is reached when visual field damage becomes extensive and binocular scotoma become significant. At this point many patients do badly in our tasks and are then seriously impacted even though they have remaining sight. We need to think about this tipping point and how it could be better quantified in the busy clinic.54, 67 This might need a rethink about the visual field requirements needed to cope with the real world instead of detecting fixed lights in the bowl of a perimeter.
This article briefly summarised the problems that patients have with everyday visual tasks. It is difficult to draw firm conclusions but my main observation based on our studies is that problems and difficulties only become apparent when visual field loss becomes quite advanced. Many glaucoma patients, even those with bilateral visual field loss, simply do not perceive their impaired vision as a problem or a disability. This observation is supported by those studies that have strikingly shown that less than one quarter of glaucoma patients were willing to trade any longevity for perfect vision in so-called time trade off experiments.68 For many patients, the psychological strain of the diagnosis, side-effects of treatment, and fear of blindness might be more affecting than the impact of subtle levels of sight loss. The cleverly designed study of Odberg et al69 from nearly 15 years ago highlighted that 80% of newly diagnosed patients reported serious levels of anxiety and depression because of their diagnosis, despite 83% self-reporting good or excellent vision, and half having no visual symptoms. We certainly need more data on the personal and psychological burden of the diagnosis. Equally, we ought to be wary about labelling patients with a diagnosis of ocular hypertension and look more closely at the prognosis of these patients in their lifetime.
From a health service delivery point-of-view it is absolutely essential to treat glaucoma patients on an individual level, monitoring them with quality-of-life, likely visual disability, and life expectancy in mind. At the moment, certainly in England, there is a tendency to have a ‘one size fits all' approach to monitoring the diagnosed patient.18 We ought to think more about the use of monitoring resources in glaucoma, especially in those patients who present with more advanced disease as compared with those with little visual loss at diagnosis, or those with ocular hypertension only. Moreover, there appears to be a ‘research obsession' with ‘pre-perimetric' glaucoma and newer detection technology, but are these really required to prevent visual impairment? This is an open research question but I suggest it would be more productive to better organise and better incentivize70, 71 the use of available technology in primary care, an idea that was well-articulated more than a decade ago.72
In conclusion, we need to better measure and better quantify the threshold at which glaucoma impacts on a patient's ability to carry out every day visually guided tasks. Advanced disease can significantly affect a patient's quality-of-life but I suggest a concurrent danger exists in patients with early, unnoticeable glaucomatous visual field loss for three reasons. First, asymptomatic visual field loss means the patient often remains undetected in the first place. Second, those with a diagnosis of early vision loss struggle to adhere to treatment for a symptomless condition, and this of course puts them at risk of deteriorating into an irreversible advanced state. Third, unnoticeable early vision loss in glaucoma is likely to cause rare but potentially catastrophic incidents, such as potentially life changing falls or driving accidents; the rarity of these events make them immune to measurement in most research studies. Therefore, we perhaps need to concentrate new research efforts on why it is that some patients are able to describe, notice, and navigate their ‘unnoticeable sight loss', while for others it remains an accident waiting to happen.73
Acknowledgments
I would like to thank Emeritus Professor Dave Edgar for kindly reading through a draft of this article and making suggestions; he has also been a brilliant mentor to me over the years. I would like to acknowledge my good friend Professor David Garway-Heath for being my main clinical collaborator and thank him for his kind words at the introduction of my lecture. I would like to acknowledge The International Glaucoma Association (www.glaucoma-association.com), Fight for Sight (www.fightforsight.org.uk), and Allergan Inc. (unrestricted funds) for supporting some key glaucoma research projects in recent years. I would also like to thank Dr Nick Smith and other members (past and present) of my research laboratory at City University London and all the volunteers for our studies (www.staff.city.ac.uk/crabblab).
The author declares no conflict of interest.
References
- 1Peters D, Bengtsson B, Heijl A. Lifetime risk of blindness in open-angle glaucoma. Am J Ophthalmol 2013; 156(4): 724–730. [DOI] [PubMed] [Google Scholar]
- 2Saunders LJ, Russell RA, Kirwan JF, McNaught AI, Crabb DP. Examining visual field loss in patients in glaucoma clinics during their predicted remaining lifetime. Invest Ophthalmol Vis Sci 2014; 55(1): 102–109. [DOI] [PubMed] [Google Scholar]
- 3Goh YW, Ang GS, Azuara-Blanco A. Lifetime visual prognosis of patients with glaucoma. Clin Experiment Ophthalmol 2011; 39(8): 766–770. [DOI] [PubMed] [Google Scholar]
- 4Alliance for Eye and Vision Research (AEVR). New poll: Americans fear blindness more than loss of other senses, strongly support more funding for research. (cited 4 October 2015). Available at http://www.arvo.org/About_ARVO/Press_Room/New_poll__Americans_fear_blindness_more_than_loss_of_other_senses,_strongly_support_more_funding_for_research/.
- 5McKean-Cowdin R, Wang Y, Wu J, Azen SP, Varma R, Los Angeles Latino Eye Study Group. Impact of visual field loss on health-related quality-of-life in glaucoma: the Los Angeles Latino Eye Study. Ophthalmology 2008; 115(6): 941–8.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6Popescu ML, Boisjoly H, Schmaltz H, Kergoat M-J, Rousseau J, Moghadaszadeh S et al. Explaining the relationship between three eye diseases and depressive symptoms in older adults. Invest Ophthalmol Vis Sci 2012; 53(4): 2308–2313. [DOI] [PubMed] [Google Scholar]
- 7Glen FC, Crabb DP, Garway-Heath DF. The direction of research into visual disability and quality-of-life in glaucoma. BMC Ophthalmol 2011; 11: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8King A, Azuara-Blanco A, Tuulonen A. Glaucoma. BMJ 2013; 346: f3518. [DOI] [PubMed] [Google Scholar]
- 9Ng WS, Agarwal PK, Sidiki S, McKay L, Townend J, Azuara-Blanco A. The effect of socio-economic deprivation on severity of glaucoma at presentation. Br J Ophthalmol 2010; 94(1): 85–87. [DOI] [PubMed] [Google Scholar]
- 10Prior M, Francis JJ, Azuara-Blanco A, Anand N, Burr JM, Glaucoma screening Platform Study group. Why do people present late with advanced glaucoma? A qualitative interview study. Br J Ophthalmol 2013; 97(12): 1574–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11Boodhna T, Crabb DP. Disease severity in newly diagnosed glaucoma patients with visual field loss: trends from more than a decade of data. Ophthalmic Physiol Opt 2015; 35(2): 225–230. [DOI] [PubMed] [Google Scholar]
- 12Fung SSM, Lemer C, Russell RA, Malik R, Crabb DP. Are practical recommendations practiced? A national multi-centre cross-sectional study on frequency of visual field testing in glaucoma. Br J Ophthalmol 2013; 97(7): 843–847. [DOI] [PubMed] [Google Scholar]
- 13Malik R, Swanson WH, Garway-Heath DF. ‘Structure-function relationship' in glaucoma: past thinking and current concepts. Clin Experiment Ophthalmol 2012; 40(4): 369–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14Chauhan BC, Garway-Heath DF, Goñi FJ, Rossetti L, Bengtsson B, Viswanathan AC et al. Practical recommendations for measuring rates of visual field change in glaucoma. Br J Ophthalmol 2008; 92(4): 569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15Crabb DP, Garway-Heath DF. Intervals between visual field tests when monitoring the glaucomatous patient: wait-and-see approach. Invest Ophthalmol Vis Sci 2012; 53(6): 2770–2776. [DOI] [PubMed] [Google Scholar]
- 16Malik R, Baker H, Russell RA, Crabb DP. A survey of attitudes of glaucoma subspecialists in England and Wales to visual field test intervals in relation to NICE guidelines. BMJ Open 2013; 3(5): e002067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17Glen FC, Baker H, Crabb DP. A qualitative investigation into patients' views on visual field testing for glaucoma monitoring. BMJ Open 2014; 4(1): e003996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18Crabb DP, Russell RA, Malik R, Anand N, Baker H, Boodhna T et al. Frequency of visual field testing when monitoring patients newly diagnosed with glaucoma: mixed methods and modelling [Internet]. NIHR Journals Library: Southampton, UK, 2014. (cited 5 May 2015). Available at http://www.ncbi.nlm.nih.gov/books/NBK259972/. [PubMed] [Google Scholar]
- 19Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 2002; 120(10): 1268–1279. [DOI] [PubMed] [Google Scholar]
- 20Garway-Heath DF, Crabb DP, Bunce C, Lascaratos G, Amalfitano F, Anand N et al. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet 2015; 385(9975): 1295–1304. [DOI] [PubMed] [Google Scholar]
- 21O'Leary N, Chauhan BC, Artes PH. Visual field progression in glaucoma: estimating the overall significance of deterioration with permutation analyses of pointwise linear regression (PoPLR). Invest Ophthalmol Vis Sci 2012; 53(11): 6776–6784. [DOI] [PubMed] [Google Scholar]
- 22Zhu H, Russell RA, Saunders LJ, Ceccon S, Garway-Heath DF, Crabb DP. Detecting changes in retinal function: Analysis with Non-Stationary Weibull Error Regression and Spatial enhancement (ANSWERS). PLoS One 2014; 9(1): e85654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23Zhu H, Crabb DP, Ho T, Garway-Heath DF. More accurate modeling of visual field progression in glaucoma: ANSWERS. Invest Ophthalmol Vis Sci 2015; 56(10): 6077–6083. [DOI] [PubMed] [Google Scholar]
- 24Kulkarni KM, Mayer JR, Lorenzana LL, Myers JS, Spaeth GL. Visual field staging systems in glaucoma and the activities of daily living. Am J Ophthalmol 2012; 154(3): 445–51.e3. [DOI] [PubMed] [Google Scholar]
- 25Asaoka R, Crabb DP, Yamashita T, Russell RA, Wang YX, Garway-Heath DF. Patients have two eyes!: binocular versus better eye visual field indices. Invest Ophthalmol Vis Sci 2011; 52(9): 7007–7011. [DOI] [PubMed] [Google Scholar]
- 26Murata H, Hirasawa H, Aoyama Y, Sugisaki K, Araie M, Mayama C et al. Identifying areas of the visual field important for quality-of-life in patients with glaucoma. PloS One 2013; 8(3): e58695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27Hu S, Smith ND, Saunders LJ, Crabb DP. Patterns of binocular visual field loss derived from large-scale patient data from glaucoma clinics. Ophthalmology 2015. e-pub ahead of print 18 September 2015 doi:10.1016/j.ophtha.2015.08.005. [DOI] [PubMed]
- 28Ramulu P. Glaucoma and disability: which tasks are affected, and at what stage of disease? Curr Opin Ophthalmol 2009; 20(2): 92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29Medeiros FA, Gracitelli CPB, Boer ER, Weinreb RN, Zangwill LM, Rosen PN. Longitudinal changes in quality-of-life and rates of progressive visual field loss in glaucoma patients. Ophthalmology 2015; 122(2): 293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30Somner JEA, Sii F, Bourne RR, Cross V, Burr JM, Shah P. Moving from PROMs to POEMs for glaucoma care: a qualitative scoping exercise. Invest Ophthalmol Vis Sci 2012; 53(9): 5940–5947. [DOI] [PubMed] [Google Scholar]
- 31Azuara-Blanco A, Burr JM, Cochran C, Ramsay C, Vale L, Foster P et al. The effectiveness of early lens extraction with intraocular lens implantation for the treatment of primary angle-closure glaucoma (EAGLE): study protocol for a randomized controlled trial. Trials 2011; 12: 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32Ekici F, Loh R, Waisbourd M, Sun Y, Martinez P, Nayak N et al. Relationships between measures of the ability to perform vision-related activities, vision-related quality-of-life, and clinical findings in patients with glaucoma. JAMA Ophthalmol 2015. e-pub ahead of print 1 October 2015 doi:10.1001/jamaophthalmol.2015.3426. [DOI] [PubMed]
- 33Wei H, Sawchyn AK, Myers JS, Katz LJ, Moster MR, Wizov SS et al. A clinical method to assess the effect of visual loss on the ability to perform activities of daily living. Br J Ophthalmol 2012; 96(5): 735–741. [DOI] [PubMed] [Google Scholar]
- 34van Landingham SW, Ramulu PY Glaucoma and quality-of-life. In: Scholl HPN, Massof RW, West S (eds). Ophthalmology and the Ageing Society, 2013 edn. Springer: Berlin, 2013, pp 165–180.
- 35Burton R, Crabb DP, Smith ND, Glen FC, Garway-Heath DF. Glaucoma and reading: exploring the effects of contrast lowering of text. Optom Vis Sci 2012; 89(9): 1282–1287. [DOI] [PubMed] [Google Scholar]
- 36Ishii M, Seki M, Harigai R, Abe H, Fukuchi T. Reading performance in patients with glaucoma evaluated using the MNREAD charts. Jpn J Ophthalmol 2013; 57(5): 471–474. [DOI] [PubMed] [Google Scholar]
- 37Ramulu PY, Swenor BK, Jefferys JL, Friedman DS, Rubin GS. Difficulty with out-loud and silent reading in glaucoma. Invest Ophthalmol Vis Sci 2013; 54(1): 666–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38Burton R, Saunders LJ, Crabb DP. Areas of the visual field important during reading in patients with glaucoma. Jpn J Ophthalmol 2015; 59(2): 94–102. [DOI] [PubMed] [Google Scholar]
- 39Smith ND, Glen FC, Mönter VM, Crabb DP. Using eye tracking to assess reading performance in patients with glaucoma: a within-person study. J Ophthalmol 2014; 2014: 120528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40Burton R, Smith ND, Crabb DP. Eye movements and reading in glaucoma: observations on patients with advanced visual field loss. Graefes Arch Clin Exp Ophthalmol 2014; 252(10): 1621–1630. [DOI] [PubMed] [Google Scholar]
- 41Kotecha A, O'Leary N, Melmoth D, Grant S, Crabb DP. The functional consequences of glaucoma for eye-hand coordination. Invest Ophthalmol Vis Sci 2009; 50(1): 203–213. [DOI] [PubMed] [Google Scholar]
- 42Friedman DS, Freeman E, Munoz B, Jampel HD, West SK. Glaucoma and mobility performance: the Salisbury Eye Evaluation Project. Ophthalmology 2007; 114(12): 2232–2237. [DOI] [PubMed] [Google Scholar]
- 43Kotecha A, Richardson G, Chopra R, Fahy RTA, Garway-Heath DF, Rubin GS. Balance control in glaucoma. Invest Ophthalmol Vis Sci 2012; 53(12): 7795–7801. [DOI] [PubMed] [Google Scholar]
- 44Black AA, Wood JM, Lovie-Kitchin JE. Inferior visual field reductions are associated with poorer functional status among older adults with glaucoma. Ophthalmic Physiol Opt 2011; 31(3): 283–291. [DOI] [PubMed] [Google Scholar]
- 45Yuki K, Tanabe S, Kouyama K, Fukagawa K, Uchino M, Shimoyama M et al. The association between visual field defect severity and fear of falling in primary open-angle glaucoma. Invest Ophthalmol Vis Sci 2013; 54(12): 7739–7745. [DOI] [PubMed] [Google Scholar]
- 46Ramulu PY, van Landingham SW, Massof RW, Chan ES, Ferrucci L, Friedman DS. Fear of falling and visual field loss from glaucoma. Ophthalmology 2012; 119(7): 1352–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47Ramulu PY, Hochberg C, Maul EA, Chan ES, Ferrucci L, Friedman DS. Glaucomatous visual field loss associated with less travel from home. Optom Vis Sci 2014; 91(2): 187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48Haymes SA, LeBlanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Glaucoma and on-road driving performance. Invest Ophthalmol Vis Sci 2008; 49(7): 3035–3041. [DOI] [PubMed] [Google Scholar]
- 49Blane A. Through the looking glass: a review of the literature investigating the impact of glaucoma on crash risk, driving performance, and driver self-regulation in older drivers. J Glaucoma 2014. e-pub ahead of print 9 December 2014. [DOI] [PubMed]
- 50Bhargava JS, Patel B, Foss AJE, Avery AJ, King AJ. Views of glaucoma patients on aspects of their treatment: an assessment of patient preference by conjoint analysis. Invest Ophthalmol Vis Sci 2006; 47(7): 2885–2888. [DOI] [PubMed] [Google Scholar]
- 51van Landingham SW, Hochberg C, Massof RW, Chan E, Friedman DS, Ramulu PY. Driving patterns in older adults with glaucoma. BMC Ophthalmol 2013; 13: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52Crabb DP, Smith ND, Rauscher FG, Chisholm CM, Barbur JL, Edgar DF et al. Exploring eye movements in patients with glaucoma when viewing a driving scene. PLoS ONE 2010; 5(3): e9710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53Glen FC, Smith ND, Crabb DP. Impact of superior and inferior visual field loss on hazard detection in a computer-based driving test. Br J Ophthalmol 2015; 99(5): 613–617. [DOI] [PubMed] [Google Scholar]
- 54Saunders LJ, Russell RA, Crabb DP. Practical landmarks for visual field disability in glaucoma. Br J Ophthalmol 2012; 96(9): 1185–1189. [DOI] [PubMed] [Google Scholar]
- 55Kunimatsu-Sanuki S, Iwase A, Araie M, Aoki Y, Hara T, Nakazawa T et al. An assessment of driving fitness in patients with visual impairment to understand the elevated risk of motor vehicle accidents. BMJ Open 2015; 5(2): e006379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56Tatham AJ, Boer ER, Gracitelli CPB, Rosen PN, Medeiros FA. Relationship between motor vehicle collisions and results of perimetry, useful field of view, and driving simulation in drivers with glaucoma. Transl Vis Sci Technol 2015; 4(3): 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57Owsley C, Wood JM, McGwin G. A roadmap for interpreting the literature on vision and driving. Surv Ophthalmol 2015; 60(3): 250–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58Huisingh C, McGwin G, Wood J, Owsley C. The driving visual field and a history of motor vehicle collision involvement in older drivers: a population-based examination. Invest Ophthalmol Vis Sci 2014; 56(1): 132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59Nelson P, Aspinall P, Papasouliotis O, Worton B, O'Brien C. Quality-of-life in glaucoma and its relationship with visual function. J Glaucoma 2003; 12(2): 139–150. [DOI] [PubMed] [Google Scholar]
- 60Smith ND, Crabb DP, Garway-Heath DF. An exploratory study of visual search performance in glaucoma. Ophthalmic Physiol Opt 2011; 31(3): 225–232. [DOI] [PubMed] [Google Scholar]
- 61Glen FC, Crabb DP, Smith ND, Burton R, Garway-Heath DF. Do patients with glaucoma have difficulty recognizing faces? Invest Ophthalmol Vis Sci 2012; 53(7): 3629–3637. [DOI] [PubMed] [Google Scholar]
- 62Smith ND, Glen FC, Crabb DP. Eye movements during visual search in patients with glaucoma. BMC Ophthalmol 2012; 12(1): 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63Glen FC, Smith ND, Crabb DP. Saccadic eye movements and face recognition performance in patients with central glaucomatous visual field defects. Vision Res 2013; 82: 42–51. [DOI] [PubMed] [Google Scholar]
- 64Crabb DP, Smith ND, Zhu H. What's on TV? Detecting age-related neurodegenerative eye disease using eye movement scanpaths. Front Aging Neurosci 2014; 6: 312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65Crabb DP, Smith ND, Glen FC, Burton R, Garway-Heath DF. How does glaucoma look?: patient perception of visual field loss. Ophthalmology 2013; 120(6): 1120–1126. [DOI] [PubMed] [Google Scholar]
- 66Glaucoma in perspective UK on the App Store [Internet]. App Store. (cited 5 October 2015). Available at https://itunes.apple.com/gb/app/glaucoma-in-perspective-uk/id991094773?mt=8.
- 67Peters D, Heijl A, Brenner L, Bengtsson B. Visual impairment and vision-related quality-of-life in the Early Manifest Glaucoma Trial after 20 years of follow-up. Acta Ophthalmol (Copenh) 2015. e-pub ahead of print 18 September 2015 doi:10.1111/aos.12839. [DOI] [PMC free article] [PubMed]
- 68Aspinall PA, Johnson ZK, Azuara-Blanco A, Montarzino A, Brice R, Vickers A. Evaluation of quality-of-life and priorities of patients with glaucoma. Invest Ophthalmol Vis Sci 2008; 49(5): 1907–1915. [DOI] [PubMed] [Google Scholar]
- 69Odberg T, Jakobsen JE, Hultgren SJ, Halseide R. The impact of glaucoma on the quality-of-life of patients in Norway. I. Results from a self-administered questionnaire. Acta Ophthalmol Scand 2001; 79(2): 116–120. [DOI] [PubMed] [Google Scholar]
- 70Myint J, Edgar DF, Kotecha A, Murdoch IE, Lawrenson JG. Barriers perceived by UK-based community optometrists to the detection of primary open angle glaucoma. Ophthalmic Physiol Opt 2010; 30(6): 847–853. [DOI] [PubMed] [Google Scholar]
- 71Konstantakopoulou E, Harper RA, Edgar DF, Lawrenson JG. A qualitative study of stakeholder views regarding participation in locally commissioned enhanced optometric services. BMJ Open 2014; 4(5): e004781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72Henson DB, Thampy R. Preventing blindness from glaucoma. BMJ 2005; 331(7509): 120–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73Glen FC, Crabb DP. Living with glaucoma: a qualitative study of functional implications and patients' coping behaviours. BMC Ophthalmol 2015; 15: 128. [DOI] [PMC free article] [PubMed] [Google Scholar]