Abstract
Study Objectives:
Investigate whether retirement transitions are associated with changes in sleep duration and sleep timing, and whether these associations are modified by age, sex, mental health, or circadian preference.
Methods:
The Retirement and Sleep Trajectories (REST) study is a longitudinal study consisting of four annual mailed surveys that collected information about employment, sleep, and health. Differences in reported sleep duration, bedtime and wake time between successive surveys were calculated to estimate change over 1, 2, and 3 y. Linear regression models were used to estimate changes in these sleep parameters associated with retirement 1, 2, and 3 y posttransition.
Results:
Retiring from full-time work was associated with bedtimes that were 30, 31, and 36 min later 1, 2, and 3 y postretirement; wake times that were 63, 69, and 78 min later; and sleep durations that were 15, 16, and 22 min longer 1, 2, and 3 y postretirement. These associations did not differ by sex or mental health status. Age and circadian preference modified the associations between retirement and change in sleep parameters; the increase in sleep duration was shorter and the wake time extension was lesser with advancing retirement age; those with evening preference had longer wake time extensions than those with morning preference.
Conclusion:
Transitioning to retirement is associated with longer sleep duration, later bedtimes, and later wake times. These changes were detectable about 1 y postwork transition and were persistent up to 3 y later.
Citation:
Hagen EW, Barnet JH, Hale L, Peppard PE. Changes in sleep duration and sleep timing associated with retirement transitions. SLEEP 2016;39(3):665–673.
Keywords: bedtime, retirement, sleep duration, wake time
Significance.
This study provides evidence that sleep schedules, even among older adults, are constrained by work schedules; shortly (perhaps immediately) following retiring from employment, study participants adopted later bedtimes and even later waketimes. As a result, retirees had longer sleep durations than their working counterparts. Significant interactions between working status and both age and circadian preference suggest that constraints on “naturally occurring” sleep schedules are not experienced uniformly. Younger retirees changed their sleep schedules to a greater extent than older retirees. Additionally, circadian preference strongly affected postretirement changes in sleep duration and timing, suggesting that those with evening chronotype were substantially more constrained by work schedules than those with morning chronotype.
INTRODUCTION
A recent study of time use trade-offs suggested that one of the main activities traded off for sleep is time spent working; furthermore, retired persons were more likely to report being long sleepers and less likely to report being short sleepers than workers.1 In addition, there is evidence that sleep duration declines with advancing age,2 although it may not occur steadily throughout adulthood.1,3,4 A meta-analysis that examined changes in sleep duration with aging found shorter sleep time with older age up until age 65 y, after which sleep duration did not continue to decline,3 possibly indicating retirement-related alterations to the association of aging with sleep duration.
Moreover, studies that examine sleep duration habits among adults find that study participants report shorter sleep durations on work nights compared to weekend nights. One study that used sleep diaries to estimate weekday and weekend sleep among adults found that participants reported sleeping an average 27 min longer on weekends than weeknights.5 Another study that asked respondents to report their usual weekday and weekend sleep in separate questions found that people reported longer sleep duration on the weekend by about a quarter of an hour.6
There is some evidence to suggest that sleep characteristics may change with retirement, possibly related to changes in sleep duration and sleep timing. Two longitudinal cohort studies have investigated associations between retirement and sleep problems, such as insomnia and disturbed sleep. The VISAT (Aging, Health, & Work) study investigated the effect of retirement on perceived sleep problems (i.e., insomnia symptoms) in a cohort of workers in France. They found that retirement was associated with one of the insomnia symptoms evaluated (premature awakening) but not the others.7 Additionally, the GAZEL study, a study of employees from the French national gas and electric company (GAZEL stands for GAZ and ELectricité), found that while the prevalence of sleep disturbances (an affirmative response to a question about trouble sleeping during the past 12 mo) increases slowly with advancing age, the prevalence is reduced in the years following retirement.8
However, no longitudinal studies, to our knowledge, have investigated whether retirement transitions are associated with subsequent changes in sleep duration or the timing of bedtimes and wake times. Based on studies that report different typical sleep duration times on work nights and weekend nights, as well as results from the time-use trade-off study, we hypothesized that changes in work status, in particular, retirement (partial or full), would lead to longer sleep duration among older adults, and, accordingly, to changes in either or both bedtimes and wake times. We further examined whether age, sex, mental health status, or circadian preference modified associations between the retirement transition and changes in sleep duration and timing. We measured these associations using data from the longitudinal Retirement and Sleep Trajectories (REST) Study. REST survey data were collected annually for 4 y in a sample of adults who were 46–82 y old at the time of the first survey. We evaluated sleep duration and timing changes after up to 1 y, up to 2 y, and up to 3 y postretirement transition.
METHODS
Sample and Surveys
The REST Study is a companion study of the Wisconsin Sleep Cohort Study, an ongoing longitudinal study of sleep habits and sleep disorders in a population that, at the time of recruitment, was working for the state of Wisconsin.9 Informed consent documents and study protocols were approved by the University of Wisconsin-Madison Health Sciences Institutional Review Board.
Subjects for the REST study came from the sampling frame of the Wisconsin Sleep Cohort (WSC) study.9 Individuals who participated in a specified number of previous WSC study protocols (either [1] at least three mailed surveys or [2] at least one overnight polysomnography study and one mailed survey), and who were alive as of September 2010, were eligible for this study (n = 2,427). These subjects were ∼25–60 y old in 1988 at the time of the initial recruitment into the cohort and were 46–82 y old at the beginning of the REST study.
The REST study consists of four mailed surveys, sent at approximately 1-y intervals, which include questions about occupational status, sleep, health, and sociodemographic information. Surveys were mailed to 2,427 potential REST subjects. This study evaluated pairs of surveys in which the subject reported working at the time of the first survey. Surveys sent 1 y apart (i.e., surveys 1 and 2, surveys 2 and 3, surveys 3 and 4) were used to measure 1-y change; surveys sent 2 y apart (i.e., surveys 1 and 3, surveys 2 and 4) were used to measure 2-y change; surveys mailed 3 years apart (i.e., surveys 1 and 4) were used to measure 3-y change. Subjects were included in the analysis if they did not report being retired at the time of the first survey in a survey pair. Subjects who were employed at both survey time points made up the comparison group. There were 933 respondents who provided 2,224 1-y observations (i.e., survey 1 to survey 2, survey 2 to survey 3, and survey 3 to survey 4), 1,535 2-y observations (i.e., survey 1 to survey 3, and survey 2 to survey 4) and 782 3-y observations (i.e., survey 1 to survey 4).
Outcome Variables—Bedtime, Wake Time, and Sleep Duration
We evaluated change in sleep habits associated with work or retirement transitions. Change was measured between surveys mailed 1, 2, and 3 y apart. Depending on when during that year the work/retirement transition occurred, the change reflects a difference up to 1, up to 2, and up to 3 y posttransition.
Respondents reported the time they usually turned off the lights to go to sleep on both work nights or weeknights and on the weekend. They also reported the time they usually got out of bed to start the day on both work days or weekdays and for weekend days. (Survey questions allowed for reporting bedtimes and wake times on work days or weekdays and non-work days or weekend days, which will hereafter be referred to as weekdays and weekend days.) Changes, in minutes, between bedtimes and wake times at successive time points (i.e., between surveys 1 and 2, 2 and 3, or surveys 3 and 4 for 1-y transitions; between surveys 1 and 3 or 2 and 4 for 2-y transitions; and between surveys 1 and 4 for 3-y transitions) were calculated. We evaluated overall (weighted average of weekday and weekend nights) bedtime and wake time change as well as separate weekday and weekend bedtimes and wake times as outcomes.
Subjects reported the amount of time (hours and minutes) they thought they actually slept on weeknights and on the weekend. Change in sleep duration, in minutes, between successive survey time points was evaluated with three outcomes: overall (a weighted average of weekday and weekend nights), and for weekday and weekend nights separately.
Main Predictor Variable—Employment Status Transitions
On each survey, respondents reported their occupational status. They chose which of the following descriptions reflected their current work status: working full-time, working part-time, partially retired, fully retired, not working for pay and currently looking for paid work, or not working for pay/not retired/not currently looking for work (e.g., taking leave to care for a sick family member). We combined those who reported they were partially retired and those who were working part-time into one group. Three employment transitions were evaluated as predictors of changes in the sleep habits outcomes: (1) participants who transitioned from full-time work to full retirement were compared to participants who were working full-time at each of the time points; (2) participants who transitioned from full-time to partial retirement or part-time employment were compared to participants who were working full-time at each of the time points; and (3) participants who transitioned from partial retirement or part-time work to full retirement were compared to participants who were working part-time at both time points.
Covariates and Effect-Modifying Variables
All models were adjusted for age, sex, and self-reported general health status (Excellent, Very Good, Good, Fair, Poor). We also considered the potential confounding effects of questionnaire-assessed alcohol use, caffeine consumption, and physical activity (estimated metabolic equivalent hours per weeks). Adjustment for these variables did not change the estimated association between retirement and sleep habits, so they were not included in final models.
Interactions between employment transition and age, sex, mental health status and circadian preference were examined to investigate whether these factors modified the associations between employment transition and sleep habits. Mental health status was assessed with the Short Form-12 (SF-12) mental component score.10 The SF-12 was designed to have a mean score of 50 and a standard deviation (SD) of 10 in the general population. The mental component score was evaluated as a continuous variable; higher scores indicate better mental health.
Circadian preference was measured with a highly informative three-item subset of the Morningness Eveningness Questionnaire (MEQ).11 The MEQ has been found to have good correlation (r = −0.70, P < 0.001) with the dim light melatonin onset.12 The three included items were: (1) At what time in the evening do you feel tired and, as a result, in need of sleep? (response options: 20:00–21:00, 21:00–22:15, 22:15– 24:30, 24:30–01:45, 01:45–03:00); (2) At what time of the day do you think you reach your “feeling best” peak? (response options: 24:00–05:00, 05:00–08:00, 08:00–10:00, 10:00–17:00, 17:00–22:00, 22:00–24:00; and (3) One hears about “morning” and “evening” types of people. Which one of these types do you consider yourself to be? (response options: definitely a morning type, more a morning than an evening type, more an evening than a morning type, definitely an evening type). We calculated the correlation between the full MEQ and the three-item subset included in the REST surveys, using data on the full MEQ that was previously collected on WSC subjects, and found good correlation between the full MEQ and the three items (r = 0.70, P < 0.0001).
The MEQ categorizes people by the following circadian preference groups: definitely morning type, moderately morning type, neither type, moderately evening type, and definitely evening type. We combined the moderately evening and definitely evening types into one evening preference category because of small numbers in each of these groups. Responses to each item of the MEQ are scored so that higher scores indicate more “morningness.” Modified scores were scaled based on the cut-points for the entire MEQ: “evening” preference (modified scores 2–7), “neutral” morning/evening preference (modified scores 8–10), “somewhat morning” preference (modified scores 11–12) and “most morning” preference (modified scores 13–16).
Statistical Analysis
Analyses were performed with SAS, release 9.2 (SAS Institute, Inc., Cary, NC). Descriptive statistics are reported for the entire sample that responded to two or more surveys, and thus were included in at least one of the 1-, 2-, or 3-y change analyses. The reported summary statistics are characteristics from the first survey returned by each respondent.
Linear regression was used to estimate changes in sleep duration, wake time, and bedtime associated with work-retirement transitions. Up to three observations per respondent were included in the 1-y transition models, and up to two observations per respondent were included in the 2-y transition models, using generalized linear models with repeated measures. For the 3-y transition models, each respondent contributed only one observation.
Interactions between retirement status and age, sex, mental health status, and circadian preference were tested for statistical significance (two-tailed P < 0.05) to evaluate whether these characteristics affected associations between retirement transitions and sleep habits.
Sensitivity analyses were conducted to investigate the robustness of results. For one sensitivity analysis, we restricted the sample to subjects who responded to all four surveys and, as such, were eligible to be included in each of the 1-, 2-, and 3-y transition models. Another analysis used total sleep time, including naps, to evaluate sleep duration instead of just nighttime sleep duration. Finally, an additional set of models added sleep conditions (i.e., self-reported physician-diagnosed sleep apnea and symptoms of insomnia) to the models to determine whether controlling for these conditions affected the associations between retirement transitions and changes in sleep duration and timing.
RESULTS
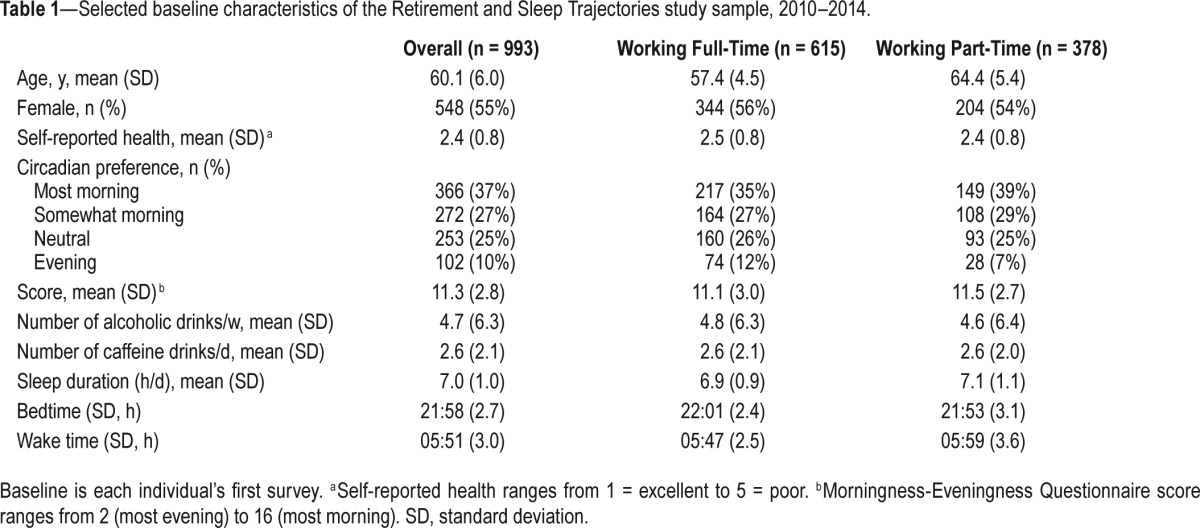
Baseline descriptive statistics (Table 1) were determined using each respondents' baseline survey (i.e., the first survey they responded to, whether it was survey 1, 2, or 3). The mean (SD) age of the entire study sample was 60.1 (6.0) y. Those working full-time at their baseline study were younger (57.4 (4.5) y) than those working part-time at baseline (64.4 (5.4) y). Fifty-five percent of respondents were women. The mean (SD) self-rated health of the sample, on a scale from 1 = Excellent to 5 = Poor was 2.4 (0.8). Respondents slept 7.0 (1.0) h at baseline, with an average bedtime of 21:58 and an average wake time of 05:51 (Table 1).
Table 1.
Selected baseline characteristics of the Retirement and Sleep Trajectories study sample, 2010–2014.
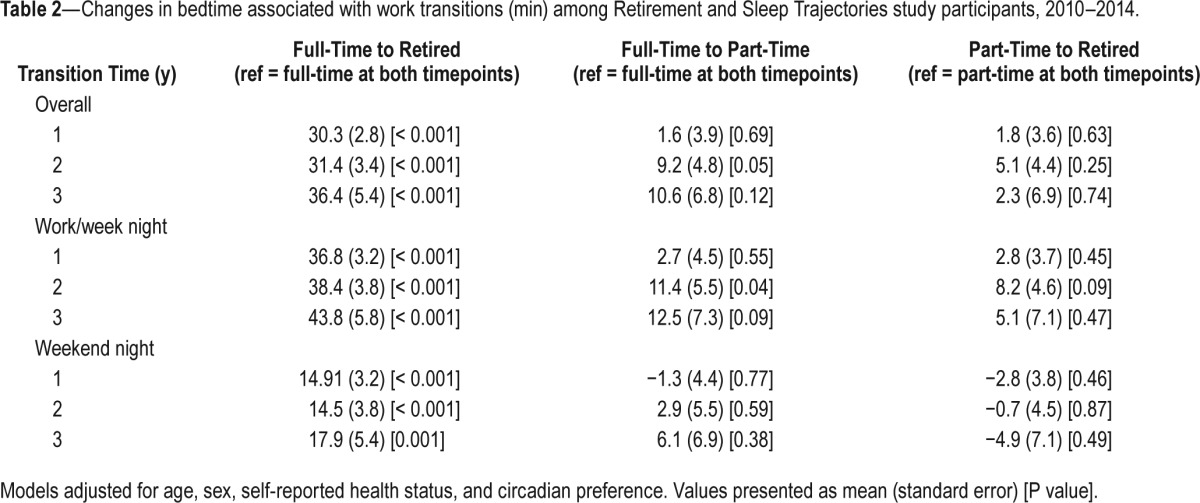
Changes in Bedtimes
Table 2 presents changes in bedtimes associated with work transitions. The difference in bedtime between two successive surveys (sent 1 y apart) for respondents who transitioned from full-time work to full retirement was 30 min later than the difference in bedtime for respondents who kept working full-time over the same time period. After up to 2 y postretirement, mean change in retired individuals' bedtimes was 31 min later than the change for respondents who were working full-time over the same time period. The difference in mean bedtime change was 36 min later for retirees compared to those working full-time up to 3 y postretirement. Most of the overall difference in the changes in bedtime was driven by differences in bedtime change on weeknights (Table 2). The difference in change in bedtime for respondents who transitioned from full-time to part-time work compared to respondents who were working full-time over the same time period was not significant 1 y or 3 y posttransition, but was 9 min (P = 0.05) later up to 2 y posttransition. There were no significant differences in changes in bedtimes between those who transitioned from partial retirement or part-time work to full retirement compared to those who were working part-time over the same time period (Table 2).
Table 2.
Changes in bedtime associated with work transitions (min) among Retirement and Sleep Trajectories study participants, 2010–2014.
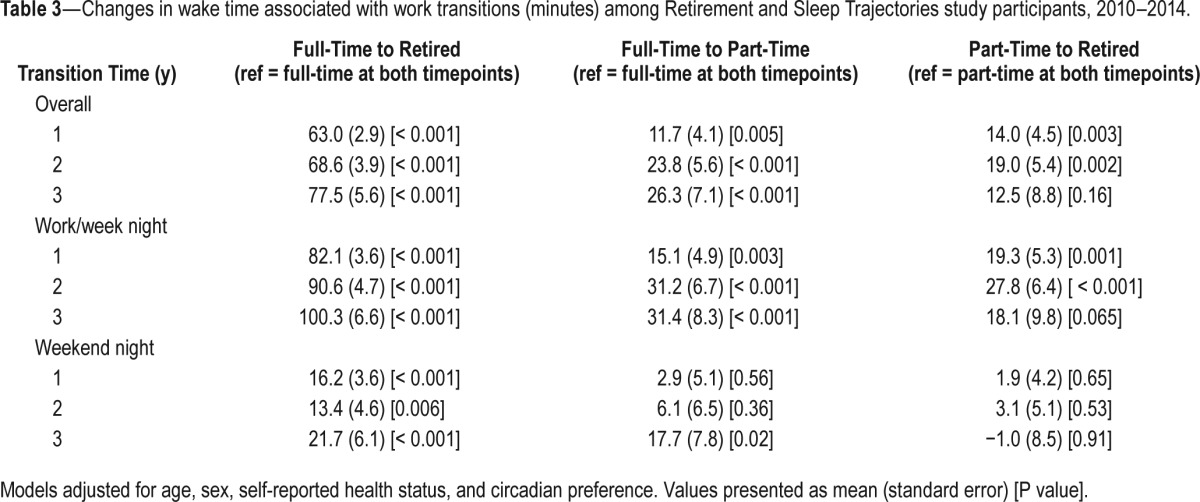
Change in Wake Times
Table 3 presents changes in wake times associated with employment transitions. The changes in wake times of participants who fully retired were 63, 69, and 78 min later up to 1, 2, and 3 y following retirement, respectively, than participants who were working full-time over the same time period. The difference in the change in wake times was due mostly to changes in weekday wake times (Table 3). Transitioning from full-time to part-time work was also associated with an overall shift to later wake times (12, 24, and 26 min up to 1, 2, and 3 y postretirement). This change was also primarily due to weekday wake time differences. Transitioning from part-time work to full retirement was associated with a significant difference in weekday wake time changes after 1 and 2 y postretirement (14 and 19 min, respectively) but the difference after 3 y of retirement was not significant. Changes in weekend wake times did not differ between respondents who were working part-time and participants who were fully retired.
Table 3.
Changes in wake time associated with work transitions (minutes) among Retirement and Sleep Trajectories study participants, 2010–2014.
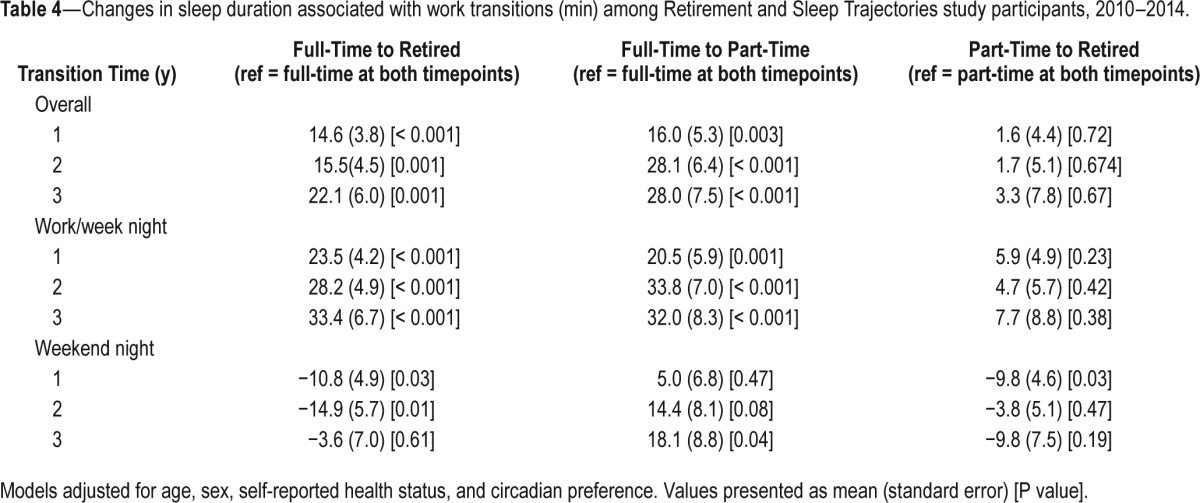
Change in Sleep Duration
Table 4 presents changes in bedtimes associated with work transitions. Change in sleep duration was longer for respondents who retired from full-time work to full retirement. Overall sleep duration change was 15, 16, and 22 min longer, respectively, for those who retired up to 1, 2, and 3 y prior. For those retiring from full-time work, sleep duration change was longer on weeknights by 24, 28, and 33 min up to 1, 2, and 3 y post-retirement than for those who kept working full- time over the same time period. Weekend sleep duration was shorter among retirees than among those who maintained employment. Sleep duration was also longer for those who transitioned from full-time work to partial retirement or part-time work compared to those who maintained full-time work over the same time period. For those who transitioned from full-time to part-time work, sleep duration change was 16, 28, and 28 min longer up to 1, 2, and 3 y posttransition, respectively. For individuals who transitioned from full-time to part-time work, weekday sleep duration change was greater than for those who were working full-time over the same time period (21, 34, and 32 min longer up to 1, 2, and 3 y posttransition). There were no significant changes in sleep duration between those who transitioned from part-time work to full retirement and those who were working part-time over the same time period.
Table 4.
Changes in sleep duration associated with work transitions (min) among Retirement and Sleep Trajectories study participants, 2010–2014.
Effect Modification
Interactions between retirement transition and sex, and retirement transition and mental health status were not statistically significant in predicting changes in sleep duration or sleep timing. However, there were significant interactions between retirement transitions and both age and circadian preference.
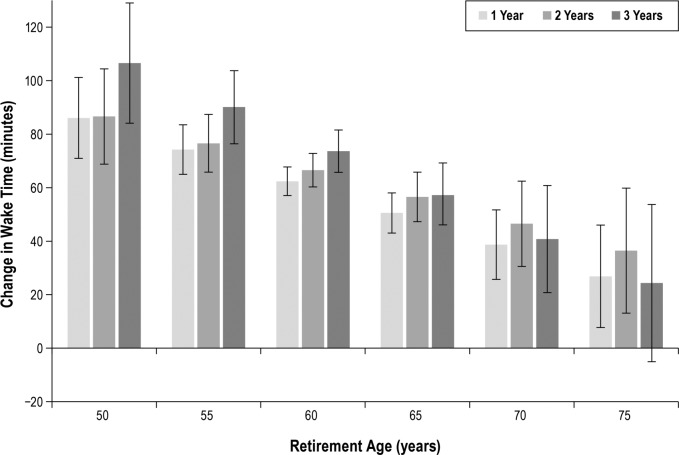
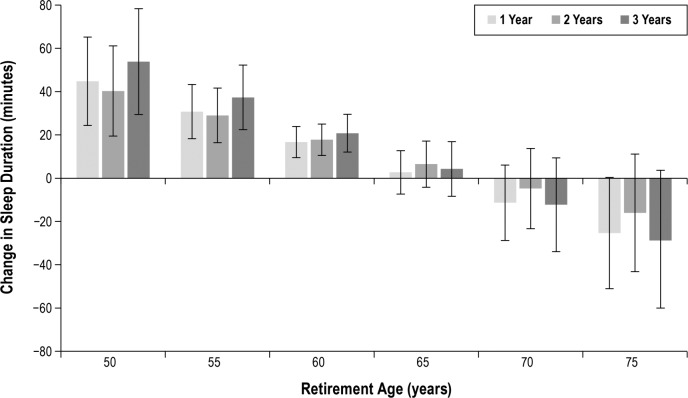
Age modified the association between retirement transitions and sleep habits; later wake times associated with retirement were not much later with older age (Figure 1), and increases in sleep duration were not as great with older age (Figure 2). Change in sleep duration was 2.6 min (P = 0.005) shorter per year of age up to 1 y postretirement; 2.3 min (P = 0.03) shorter per year at 2 y postretirement; and retiring was associated with 3.0 min (P = 0.02) shorter increase in sleep duration per year of age up to 3 y postretirement. These findings suggest that a 10-y age increment at the time of retirement is associated with a 20- to 30-min reduction in the increase in sleep duration associated with transitioning to retirement.
Figure 1.
Changes in wake time 1, 2, and 3 years postretirement by age at retirement. Model-based estimates of change in wake time (in min) with 95% confidence intervals associated with transitioning from full-time work to full retirement up to 1, 2, and 3 y posttransition from the model that included an interaction term between retirement and age at retirement. Models were adjusted for sex, self-rated health, and circadian preference.
Figure 2.
Changes in sleep duration 1, 2, and 3 years postretirement by age at retirement. Model-based estimates of change in sleep duration (in min) with 95% confidence intervals associated with transitioning from full-time work to full retirement up to 1, 2, and 3 y posttransition from the model that included an interaction term between retirement and age at retirement. Models were adjusted for sex, self-rated health, and circadian preference.
Overall, transitioning to retirement was associated with later wake times, but wake time extensions were a few minutes less with each year of advancing age. Wake time extensions were reduced 2.2 min (P = 0.002) for each year of advancing age 1 y postretirement, 1.5 (P = 0.09) min less for each year of advancing age 2 y postretirement, and 2.9 min (P = 0.02) less after 3 y. These significant interactions suggest that a 10-y age difference at the time of retirement is associated with a 22-min difference in the change in wake time 1 y postretirement and a 30-min difference in the change in wake time 3 y postretirement.
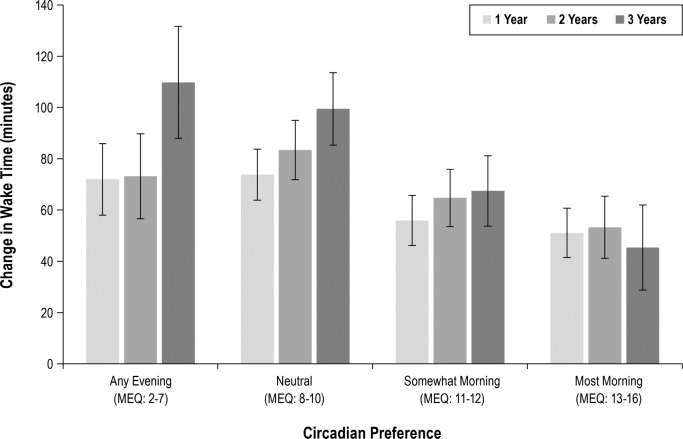
Circadian preference modified the association between retirement and wake time (Figure 3) so that, compared to respondents with the most morning preference, those with evening preferences had even larger wake time changes associated with retirement. After 1 y, those with evening preference had changes in wake time that were 19 min later (P = 0.03) than the change associated with retirement for respondents with the most morning preference. Those with a neutral morning/ evening circadian preference had changes in wake times that were 21 (P = 0.005) min later than those with the most morning preference. After 2 y postretirement, evening and neutral circadian preferences were associated with weekday wake times that were 18 (P = 0.13) and 33 (P < 0.001) later than changes in wake times for those with the most morning preference. Three years postretirement, those with evening and neutral preferences had changes in wake time that were 56 (P = 0.002) and 52 (P < 0.001) min later than changes associated with retirement for individuals with the most morning preference.
Figure 3.
Change in wake time 1, 2, and 3 years postretirement by circadian preference category. Model-based estimates of change in wake time (in min) with 95% confidence intervals associated with transitioning from full-time work to full retirement up to 1, 2, and 3 y posttransition, from the model that included an interaction term between retirement and circadian preference. Circadian preference was determined by select items of the Morningness Eveningness Questionnaire and subjects were categorized according to Evening type, Neutral (neither morning nor evening preference), Moderately Morning type, and Definitely Morning type. Models were adjusted for age, sex, and self-rated health.
Sensitivity Analyses
When the sample was restricted to subjects who responded to all four surveys, there were no changes in the conclusions about the associations between retirement and sleep outcomes (sleep duration, bedtimes, and wake times), with beta coefficients and P values very similar between the main models presented previously and the models using the restricted sample.
Another sensitivity analysis recalculated sleep duration to include naps. The difference in this total sleep time variable between those who retired and those who kept working was not appreciably different than the nighttime sleep duration variable used in the main models.
Finally, we added sleep apnea and insomnia to the models to determine whether the presence of these sleep conditions would affect our results. Neither of the two sleep conditions, when added to the models, affected the associations between retirement transitions and the sleep duration or sleep timing outcomes.
DISCUSSION
We found that transitioning to retirement or part-time work was associated with later bedtimes, and even later wake times and, as a result, in a total net average increase in sleep duration. Retirement transitions were associated with bigger differences in sleep duration and bed times and wake times than full-time to part-time transitions, and transitions from part-time work to full retirement were not associated with significantly different changes in sleep time or timing compared with those who kept working part-time. The full-time employment to full retirement transition is a much more abrupt lifestyle and time-use change than either of the other two transitions (from part-time work to retirement or from full-time work to part-time work) and so it is not surprising that the largest amount of change is happening within the full-time to full retirement group.
Because of the differences in sleep duration and sleep timing changes between weekdays and weekends associated with retirement, it appears that not getting up early for work may be the primary cause of the increase in sleep duration. Wake times on weekdays were considerably later, and retirees also reported staying up later at night, presumably because they don't have to wake up early in the morning to be on time for work.
Very few other studies have investigated the association between retirement status and sleep duration. Time use analyses suggest that nonworking adults (including retirees, as well as those who were unemployed or not in the labor force) obtain significantly more sleep than those who are employed.1,13 Our results are consistent with these analyses of time tradeoffs that people make during their daily activities. A recently published longitudinal study of the health effects associated with retirement reported that weekday sleep duration increases with retirement.14 These authors report that sleep duration increases by a mean (SD) 0.7(0.5) h. This reported difference of about 42 min is consistent with the differences we found in our results.
We found an interaction between the retirement transitions and age in predicting changes in sleep duration and wake times, such that the increase in sleep duration was shorter and the wake time extension was lesser with advancing age. These modifications to the retirement–sleep duration and retirement– wake time associations due to age are somewhat unexpected, given that studies have found that sleep duration decreases with age3,4 and that wake time has been found to be later in older age.15 However, none of these studies has examined the contribution of retirement–or other exogenous factors that may be associated with aging–to the changes in sleep duration or wake time, so it is difficult to know how much of the increase in sleep time or wake time associated with aging in these studies is due to biological aging and how much is attributable to changing roles, responsibilities, and activities associated with work and retirement. We speculate that both biology and social roles are at play and that the dampened effect of retirement seen at older ages may be due to the possibility that older people may already have altered their sleeping habits and patterns while they were working due to biologically related changes associated with aging, such that the sleep duration and timing changes associated with social role change at retirement are less drastic for retirees with more advanced age.
We found an additional interaction between circadian preference and retirement in predicting changes in wake times. While, on average, postretirement wake times were later for participants regardless of circadian preference, those reporting evening preference had significantly and substantially–more than 40 min–later wake time extensions postretirement than those endorsing morning circadian preference. This might imply that typical work schedules impose wake times that would not occur “naturally” in some adults, and the degree of imposition is greatest for persons with evening preference. Work-imposed requirements to awaken substantially earlier than optimally determined by circadian-phenotype for persons with evening circadian preference throughout the working years of life may result in poorer health outcomes related to chronic circadian misalignment.16,17 Indeed, a study of “social jet lag”–measured as the difference in midpoint of sleep between work and free days–found that greater degrees of “social jet lag” are associated with higher body mass index, glycated hemoglobin levels, heart rate, depressive symptoms, smoking, mental distress, and alcohol use.18 The substantial change we find in wake times postretirement suggests the possibility that many people may be experiencing “social jet lag” due to work schedule impositions.
For our primary study question about what happens, on average, to sleep habits upon retirement, we think our findings are likely generalizable to a wide range of blue-collar and white-collar populations undergoing a retirement transition in the broad age span represented by our sample. REST respondents were working in a myriad of job classifications at the time of retirement and retired for many reasons—as in many other work environments. There may, however, be some specific circumstances not well represented by our sample that could affect expected changes in sleep following retirement; e.g., retirement from physically strenuous jobs (e.g., timber or fishing industries), or in occupations that may impose earlier ages of retirement (e.g., law enforcement).
Study Strengths and Limitations
This study has important strengths. The large sample, followed longitudinally, consisted of older adults, many of whom were around retirement age. Many respondents did retire or transition to part-time work during the 4 y of observation, allowing us to examine the effect of these occupational transitions on wake and sleep time. The REST survey also collected a breadth of additional data so that we could adequately control for potentially important confounding factors. The four annual surveys allowed us to evaluate change in sleep habits in the year immediately following retirement and part-time work transitions, as well as follow up 2 and 3 y later to assess whether these sleep habit changes were persistent.
This study is limited in that sleep times were evaluated subjectively. Each of the annual surveys had a question asking how much sleep the respondent thought they actually got on work nights or weeknights and another question asking about how much they actually slept on weekend nights. Self-reported sleep times have been reported to be moderately associated (r = 0.47) with actigraph-measured sleep duration.19 Although objectively measuring sleep duration with wrist-worn activity monitors would have provided more accurate sleep time estimates for any given week, our subjective measure did ask subjects about a typical weeknight and a typical weekend in the same way at each survey timepoint, so our data are likely able to capture changes in usual sleep habits over time. Similarly, bed times and wake times were self-reported instead of being objectively measured.
CONCLUSIONS
Transitioning to retirement is associated with longer sleep duration, later bedtimes, and later wake times. These changes were detectable up to 1 y postwork transition and were persistent up to 3 y later. The rapid changes in sleep patterns observed post-retirement suggest that working, particularly full-time work, imposes sleep duration and timing patterns that would not otherwise occur. Furthermore, there are important differences in the degree of change in sleep patterns postretirement related to age and circadian preference suggesting that, among adults that are near retirement age, working adults who are younger and have an evening chronotype may have sleeping patterns most at odds with those that would occur in the absence of work-governed sleep-wake schedules.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was supported by grants from the National Institutes of Health (NIH): R01HL62252, 1R01AG036838, and 1UL1RR02501.This study did not include the use of any off-label or investigational drugs or devices. The authors have indicated no financial conflicts of interest. This work was performed at the University of Wisconsin-Madison.
ACKNOWLEDGMENTS
The authors thank the following people for their valuable assistance: Christine Harden, Rachel Steidl, Kayla Lacci, Haley Jelinski, Marni Sarazen, Kallie Waro, Dr. Mari Palta, Dr. F. Javier Nieto, Dr. Terry Young, and Robin Stubbs.
REFERENCES
- 1.Basner M, Spaeth AM, Dinges DF. Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep. Sleep. 2014;37:1889–906. doi: 10.5665/sleep.4238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dorffner G, Vitr M, Anderer P. The effects of aging on sleep architecture in healthy subjects. Adv Exp Med Biol. 2015;821:93–100. doi: 10.1007/978-3-319-08939-3_13. [DOI] [PubMed] [Google Scholar]
- 3.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 4.Moraes W, Piovezan R, Poyares D, Bittencourt LR, Santos-Silva R, Tufik S. Effects of aging on sleep structure throughout adulthood: a population-based study. Sleep Med. 2014;15:401–9. doi: 10.1016/j.sleep.2013.11.791. [DOI] [PubMed] [Google Scholar]
- 5.Monk TH, Buysse DJ, Rose LR, Hall JA, Kupfer DJ. The sleep of healthy people - A diary study. Chronobiol Int. 2000;17:49–60. doi: 10.1081/cbi-100101031. [DOI] [PubMed] [Google Scholar]
- 6.Lauderdale DS. Survey questions about sleep duration: does asking separately about weekdays and weekends matter? Behav Sleep Med. 2014;12:158–68. doi: 10.1080/15402002.2013.778201. [DOI] [PubMed] [Google Scholar]
- 7.Marquiae JC, Folkard S, Ansiau D, Tucker P. Effects of age, gender, and retirement on perceived sleep problems: results from the VISAT combined longitudinal and cross-sectional study. Sleep. 2012;35:1115–21. doi: 10.5665/sleep.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vahtera J, Westerlund H, Hall M, et al. Effect of retirement on sleep disturbances: the GAZEL prospective cohort study. Sleep. 2009;32:1459–66. doi: 10.1093/sleep/32.11.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 10.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 12.Kantermann T, Sung H, Burgess HJ. Comparing the morningnesseveningness questionnaire and Munich chronotype questionnaire to the dim light melatonin onset. J Biol Rhythms. 2015;30:449–53. doi: 10.1177/0748730415597520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30:1085–95. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eibich P. Understanding the effect of retirement on health: mechanisms and heterogeneity. J Health Econ. 2015;43:1–12. doi: 10.1016/j.jhealeco.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Thomas SJ, Lichstein KL, Taylor DJ, Riedel BW, Bush AJ. Epidemiology of bedtime, arising time, and time in bed: analysis of age, gender, and ethnicity. Behav Sleep Med. 2014;12:169–82. doi: 10.1080/15402002.2013.778202. [DOI] [PubMed] [Google Scholar]
- 16.Merikanto I, Lahti T, Puolijoki H, et al. Associations of chronotype and sleep with cardiovascular disease and type 2 diabetes. Chronobiol Int. 2013;30:470–77. doi: 10.3109/07420528.2012.741171. [DOI] [PubMed] [Google Scholar]
- 17.Lucassen EA, Zhao X, Rother KI, et al. Evening chronotype is associated with changes in eating behavior, more sleep apnea, and increased stress hormones in short sleeping obese individuals. Plos One. 2013;8:e56519. doi: 10.1371/journal.pone.0056519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutters F, Lemmens SG, Adam TC, et al. Is social jetlag associated with an adverse endocrine, behavioral, and cardiovascular risk profile? J Biol Rhythms. 2014;29:377–83. doi: 10.1177/0748730414550199. [DOI] [PubMed] [Google Scholar]
- 19.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]