Abstract
Background
Smoking and obesity are major causes of non-communicable diseases. We investigated the associations of heavy smoking, obesity, and underweight with general lifestyle to infer which of these risk groups has the most unfavourable lifestyle.
Methods
We used data from the population-based cross-sectional Swiss Health Survey (5 rounds 1992–2012), comprising 85,575 individuals aged≥18 years. Height, weight, smoking, diet, alcohol intake and physical activity were self-reported. Multinomial logistic regression was performed to analyse differences in lifestyle between the combinations of body mass index (BMI) category and smoking status.
Results
Compared to normal-weight never smokers (reference), individuals who were normal-weight, obese, or underweight and smoked heavily at the same time had a poorer general lifestyle. The lifestyle of obese and underweight never smokers differed less from reference. Regardless of BMI category, in heavy smoking men and women the fruit and vegetable consumption was lower (e.g. obese heavy smoking men: relative risk ratio (RRR) 1.69 [95% confidence interval 1.30;2.21]) and high alcohol intake was more common (e.g. normal-weight heavy smoking women 5.51 [3.71;8.20]). In both sexes, physical inactivity was observed more often in heavy smokers and obese or underweight (e.g. underweight never smoking 1.29 [1.08;1.54] and heavy smoking women 2.02 [1.33;3.08]). A decrease of smoking prevalence was observed over time in normal-weight, but not in obese individuals.
Conclusions
Unhealthy general lifestyle was associated with both heavy smoking and BMI extremes, but we observed a stronger association for heavy smoking. Future smoking prevention measures should pay attention to improvement of general lifestyle and co-occurrence with obesity and underweight.
Introduction
Smoking and obesity are the most important modifiable risk factors of non-communicable diseases (NCD) [1–3]. Evidence is less clear for underweight [4,5]. However, similarly to obese individuals and smokers, it was shown that underweight individuals have an increased risk of premature death [6,7]. Investigations of the health impact of extreme body mass index (BMI) combined with smoking found that obese and underweight current smokers had the highest overall, cancer and cardiovascular disease mortality risk [8]. Non-smoking and maintaining healthy BMI, but also related risk factors such as healthy diet, low to moderate alcohol intake and physical activity offer substantial potential for the reduction of premature death and NCD burden in the population [9,10].
Unfavourable lifestyle factors are likely to occur coincidentally. Studies on how lifestyle factors are related and cluster revealed that smoking and educational level are driving factors, unfortunately they did not take BMI into account [11–13]. In affluent countries like Switzerland, obesity gained relevance as its prevalence was increased over the past decades, whereas the prevalence of smoking decreased in the general population [14,15]. However, it remains unknown whether this decrease occurred also in those most at risk (i.e. obese individuals) or mainly in healthier and health conscious people. Therefore we aimed to investigate the general lifestyle of obese individuals, heavy smokers, and obese heavy smokers to get a better understanding of the distribution of lifestyle risk factors. These populations are already at high risk of NCD and the coincidence with further unhealthy lifestyles would worsen their risk profile. We also included underweight in our analysis to contribute to the discussion on whether the increased mortality risk of underweight individuals is explained by associated lifestyle factors [6,16].
It was our first objective to compare the role of obesity, underweight and heavy smoking regarding the tendency of clustering with other NCD relevant lifestyle factors and with socio-demographic factors. Secondly, we aimed at investigating the temporal changes in the prevalence of the combination of obesity and underweight respectively with heavy smoking.
Methods
Population and data collection
The Swiss Health Survey (SHS) is a population-based cross-sectional survey conducted every 5 years since 1992 by the Swiss Federal Statistical Office [17]. Study samples were obtained by stratified random sampling out of a database containing all private household landline telephone numbers. This database was built with linkage of data from resident registries and telephone companies. Since 2012, an additional recruitment option was implemented. For those subjects who were randomly selected through resident registries and had no landline telephone number available, a letter was sent out to obtain contact information (landline or mobile telephone number) by prepaid answer postcard. Data was collected with telephone interview and self-administered questionnaire, additionally. The participation rate ranged from 71% in 1992 to 54% in 2012. For this study, we restricted the sample to individuals aged≥18 years.
The data collection and data storage for the SHS does not require formal approval by an ethical committee. This data collection is specifically permitted under Swiss law (Verordnung über die Durchführung von statistischen Erhebungen des Bundes vom 30. Juni 1993 (SR 431.012.1) and Verordnung über die eidgenössische Volkszählung vom 19. Dezember 2008 (SR 431.112.1)). Individuals invited to participate received a brief description of the study and could decline to participate or withdraw at any time. Participants’ responses were treated confidentially and aggregated anonymous responses were utilized for analyses presented herein.
Outcome
Height, weight, and smoking status were self-reported by telephone interview (see S1 Table). BMI was calculated as weight in kilograms divided by the square of height in metres. We categorized BMI (kg/m2) into underweight <18.5, normal-weight ≥18.5–<25, overweight ≥25–<30, and obesity ≥30 [18]; smoking status into never, former, light (1–9 cigarettes per day), moderate (10–19), and heavy smokers (>19). Never smokers stated that they did not currently smoke and never regularly smoked during more than six months; former smokers reported not smoking currently but having smoked for more than 6 months during their life course. One cigarillo or pipe was counted as 2 cigarettes and 1 cigar as 4 cigarettes. The outcome variable had 20 categories, composed of the combination of BMI category and smoking status.
Exposure and Covariates
We selected three lifestyle proxies in order to explore the general health behaviour. These were assessed by telephone interview and self-administered questionnaire: fruit and vegetable consumption, physical activity, and alcohol intake. In Switzerland, fruit and vegetable consumption—as healthy diet proxy—was associated with lower mortality, also in combination with other NCD factors [10]. For all 5 rounds of the SHS information on the number of days per week fruits and vegetables were consumed was available. We chose to categorize as closest to the "5-a-day" recommendation as possible [19]. Because of the inconsistency of the collected information across surveys, we had to choose a fairly crude categorisation. Fruit and vegetable consumption was combined in one binary variable that comprised the information on whether both fruits and vegetables were consumed daily or not. We previously showed the importance of leisure-time physical activity in avoiding premature death [20]; hence we included weekly leisure-time physical activity in the analysis. The variable was defined as the number of days per week a subject started to sweat during leisure time physical activity and was categorized as >2 days, 1–2 days, and none. Alcohol intake was categorized into low, moderate, and high based on its sex specific risk for adverse health consequences. For men, the cut-offs were <40 to <60g of alcohol per day, for women <20 to <40g. For 4,500 participants of the SHS 1992, information on alcohol intake was only available from the telephone interview. Because this information was not comparable to that obtained from the questionnaire, we added a missing category to the alcohol variable. Education was included as highest degree obtained and was categorized into mandatory (International Standard Classification of Education, ISCED 1–2), secondary II (ISCED 3–4), and tertiary (ISCED 5–8) [21].
Statistical analysis
We pooled the data of the five SHS and included a survey variable in the model. All analyses were weighted to the general population of Switzerland [17] and stratified by sex. We stratified for sex because of existing evidence for variations between sexes which also were obvious in our data. Differences in prevalence of smoking status and BMI categories were substantial between men and women as well as in the distribution of the exposures (fruit and vegetables, physical activity, and alcohol intake). Furthermore, it is known that the reasons for smoking vary by sex and this may lead to differences in their association with further lifestyle factors [22,23]. We performed multinomial logistic regression (STATA command: mlogit) in order to examine whether heavy smoker, obese or underweight individuals as well as obese and underweight heavy smokers were prone to have additional unhealthy lifestyle factors, compared to normal-weight never smokers. Multinomial regression was used to investigate associations between a categorical outcome with more than 2 categories and the exposure. The outcome was defined as a categorical variable obtained by the combination of BMI category with smoking status category. All smoking-BMI-category-combinations (4x5) were included in the analyses. However, for this study, we focussed on the results for heavy smoking and BMI extremes (underweight and obesity) and their presentation. The three lifestyle variables were included in the model, as well as educational level, nationality, language region, survey (categorisation, see Tables 1 and 2), and age. We pooled the data of the 5 SHS rounds, which enabled us to investigate changes over time. This was done through interpreting the results of the survey variable that was entered into the multinomial regression model. The regression model provided relative risk ratios (RRR) [24].To assess the public health relevance, the absolute number of individuals per BMI category, smoking status, and selected combinations of smoking and BMI were estimated for Switzerland in 2012 by an extrapolation based on SHS 2012 and STATPOP 2012 (Statistics of population and households) [25]. All analyses were performed using STATA 13.1, College Station, TX, USA.
Table 1. Demographic characteristic, BMI category, smoking status, and survey.
| Men | Women | |||
|---|---|---|---|---|
| Mean age | 46.0* | 47.9* | ||
| n | %* | n | %* | |
| Nationality | ||||
| Swiss | 28985 | 79.3 | 37450 | 83.4 |
| Foreign | 5256 | 20.7 | 5100 | 16.6 |
| Education | ||||
| Tertiary | 10814 | 31.0 | 6772 | 15.3 |
| Secondary II | 19412 | 56.0 | 26970 | 63.7 |
| Mandatory | 4015 | 12.0 | 8808 | 21.0 |
| Language region | ||||
| German | 22761 | 72.8 | 27532 | 71.2 |
| French | 9022 | 22.8 | 11686 | 24.0 |
| Italian | 2458 | 4.4 | 3332 | 4.8 |
| BMI category | ||||
| Underweight | 302 | 0.9 | 2628 | 6.3 |
| Normal-weight | 17748 | 52.4 | 27320 | 64.7 |
| Overweight | 13196 | 38.3 | 9263 | 21.5 |
| Obese | 2995 | 8.4 | 3339 | 7.5 |
| Smoking status | ||||
| Never | 14063 | 41.3 | 24431 | 58.4 |
| Former | 9515 | 26.9 | 8117 | 18.6 |
| Light | 2799 | 08.4 | 3236 | 7.8 |
| Medium | 3100 | 09.5 | 3524 | 8.1 |
| Heavy | 4764 | 13.9 | 3242 | 7.1 |
| Survey | ||||
| 1992 | 6003 | 18.8 | 7574 | 19.0 |
| 1997 | 5063 | 19.7 | 6518 | 19.8 |
| 2002 | 7389 | 18.8 | 9489 | 19.4 |
| 2007 | 7015 | 19.7 | 9064 | 19.5 |
| 2012 | 8771 | 23.0 | 9905 | 22.3 |
| N Total | 34241 | 100.0 | 42550 | 100.0 |
* weighted according to the general population of Switzerland.
Table 2. Estimated absolute numbers (N) and proportions (%*) for smoking status, BMI, and selected smoking-BMI-combinations in Switzerland 2012.
| Men | Women | |||
|---|---|---|---|---|
| n | %* | n | %* | |
| BMI | ||||
| Underweight | 25 771 | 0.8 | 193 971 | 5.8 |
| Normal-weight | 1 523 051 | 47.3 | 2 061 801 | 61.4 |
| Overweight | 1 296 723 | 40.3 | 780 803 | 23.2 |
| Obese | 372 537 | 11.6 | 322 836 | 9.6 |
| Smoking status | ||||
| Never | 1 466 277 | 45.6 | 1 999 815 | 59.5 |
| Former | 888 659 | 27.6 | 678 057 | 20.2 |
| Light | 263 114 | 8.2 | 271 525 | 8.1 |
| Medium | 295 869 | 9.2 | 262 438 | 7.8 |
| Heavy | 304 163 | 9.4 | 147 575 | 4.4 |
| Smoking—BMI—combination | ||||
| Normal-weight/ Never smoker | 756 523 | 23.5 | 1 213 258 | 36.1 |
| Underweight/ Never smoker | 15 485 | 0.5 | 119 422 | 3.6 |
| Overweight/Never smoker | 544 589 | 16.9 | 460 612 | 13.7 |
| Obese/ Never smoker | 148 484 | 4.6 | 202 028 | 6.0 |
| Normal-weight/ Heavy smoker | 138 192 | 4.3 | 85 537 | 2.5 |
| Underweight/ Heavy smoker | 3 861 | 0.1 | 10 566 | 0.3 |
| Overweight/Heavy smoker | 121 667 | 3.8 | 38 493 | 1.1 |
| Obese/ Heavy smoker | 41 910 | 1.3 | 14 299 | 0.4 |
| Total | 3 218 082 | 100.00 | 3 359 410 | 100.00 |
Extrapolation based on SHS 2012 (prevalence) and STATPOP 2012 (Statistics of population and households), permanent resident population aged ≥ 18 years, by sex.
* weighted according to the general population of Switzerland.
Results
Descriptive
Our analysis included 85,575 individuals. Table 1 shows the distribution of BMI and smoking status categories and demographic characteristics of the study participants by sex (BMI and smoking combinations see S2 Table, lifestyle exposures see S3 Table). Women were on average older than men, whereas there were only negligible differences in nationality and distribution over language regions. The proportion of individuals with tertiary education was twice as high in men compared to women. The prevalence of obesity was comparable in men and women, but the proportion of women with underweight was 6 times higher. Heavy smoking was twice as frequent in men compared to women.
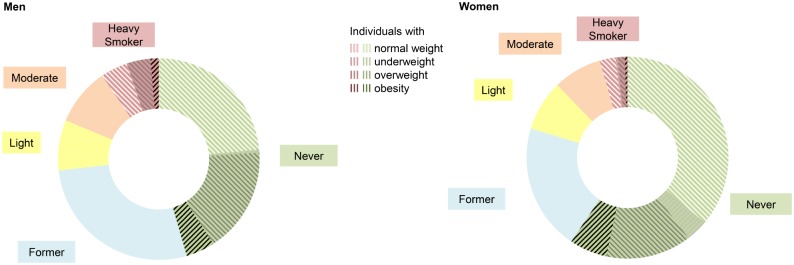
Fig 1 shows the distribution of smoking status by sex for Switzerland in 2012. For heavy and never smoking, combinations with BMI categories are presented in detail. Table 2 shows the corresponding proportions and estimated absolute numbers for Switzerland in 2012. In never and heavy smokers, the proportion of underweight and overweight individuals was comparable in both sexes. However, comparing male never with heavy smokers, the proportion of normal-weight individuals was smaller (never: 52 vs heavy: 45%) whereas the proportion of obese individuals was larger (never: 10 vs heavy: 14%). This difference was smaller in females (61 vs 57%; 10 vs 9%). Sex differences also existed with respect to the prevalence of the combination obesity plus heavy smoking. It was found to be 1.3% in men and 0.5% in women. Men were also more likely to be normal-weight heavy smokers. On the other hand, women were more often obese never smokers, underweight never and heavy smokers, respectively.
Fig 1. Prevalence of smokers by status additionally stratified by BMI for heavy and never smokers SHS 2012.
Men n = 35,880 (missing n = 2,949) and women n = 44,142 (missing n = 2,604). BMI (Body Mass Index, kg/m2): underweight <18.5, normal-weight ≥18.5–<25, overweight ≥25–<30, obesity ≥30; Smoking status: never, former, light (1–9 cigarettes per day), moderate (10–19), heavy smoker (>19); SHS: Swiss Health Survey; Results are weighted according to the general population of Switzerland.
Regression analysis
Compared to reference, i.e. normal-weight never smokers, individuals who were normal-weight, obese, or underweight and smoked heavily at the same time had a poorer lifestyle (Table 3); the lifestyle of obese and underweight never smokers differed less from reference. Heavy smokers (referred as smokers in this section) were observed to be more likely to have an unfavourable behaviour with respect to almost all modifiable lifestyle proxy factors, regardless of BMI. In contrast, physical inactivity was the only lifestyle factor that showed an association with being never smoker, except for hazardous alcohol intake in male obese never smokers. The association with the lifestyle factors was shown to be stronger in smokers compared to never smokers. Smokers of both sexes (except for heavy smoking obese women) were most likely to have a high alcohol intake.
Table 3. Lifestyle of obese and/or heavy smokers by sex, multinomial logistic regression: reference group normal-weight never smokers (adjusted for sociodemographic factors, age, and survey), weighted according to the general population of Switzerland.
| Normal-weight / Heavy smokers | Obese / Never smokers | Obese / Heavy smokers | Underweight / Never smokers | Underweight / Heavy smokers | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RRR | (95% CI) | RRR | (95% CI) | RRR | (95% CI) | RRR | (95% CI) | RRR | (95% CI) | |
| Men | ||||||||||
| Fruits and vegetables | ||||||||||
| Daily | 1 | 1 | 1 | 1 | 1 | |||||
| < Daily | 1.82 | (1.62;2.05) | 1.18 | (0.99;1.41) | 1.69 | (1.30;2.21) | 1.21 | (0.74;1.98) | 1.85 | (0.86;3.96) |
| Physical activity, leisure | ||||||||||
| > 2 | 1 | 1 | 1 | 1 | 1 | |||||
| 1 to 2 | 1.34 | (1.16;1.56) | 1.23 | (0.99;1.52) | 1.34 | (0.95;1.91) | 0.91 | (0.52;1.60) | 1.11 | (0.47;2.62) |
| Days per week | ||||||||||
| None | 2.91 | (2.50;3.37) | 1.54 | (1.24;1.89) | 3.31 | (2.38;4.62) | 1.29 | (0.72;2.30) | 3.35 | (1.43;7.87) |
| Alcohol* | ||||||||||
| Low | 1 | 1 | 1 | 1 | 1 | |||||
| Moderate | 3.35 | (2.59;4.35) | 1.18 | (0.75;1.86) | 2.15 | (1.29;3.60) | 1.06 | (0.20;5.55) | 5.33 | (1.59;17.87) |
| High | 4.75 | (3.58;6.31) | 2.00 | (1.23;3.25) | 4.29 | (2.60;7.07) | 0.24 | (0.03;1.76) | 6.83 | (2.37;19.68) |
| Missing | 1.55 | (1.20;2.00) | 1.36 | (0.83;2.22) | 1.16 | (0.65;2.10) | 1.83 | (0.53;6.27) | 0.62 | (0.17;2.18) |
| Education | ||||||||||
| Tertiary | 1 | 1 | 1 | 1 | 1 | |||||
| Secondary II | 2.04 | (1.79;2.33) | 1.74 | (1.43;2.11) | 2.86 | (2.06;3.96) | 1.93 | (1.17;3.20) | 6.97 | (2.87;16.94) |
| Mandatory | 2.19 | (1.79;2.69) | 2.67 | (2.02;3.52) | 3.26 | (2.13;4.99) | 3.53 | (1.77;7.05) | 11.67 | (3.94;34.61) |
| Nationality | ||||||||||
| Swiss | 1 | 1 | 1 | 1 | 1 | |||||
| Foreign | 1.43 | (1.23;1.67) | 1.60 | (1.25;2.05) | 1.51 | (1.08;2.13) | 1.19 | (0.66;2.12) | 1.11 | (0.44;2.82) |
| Language region** | ||||||||||
| German | 1 | 1 | 1 | 1 | 1 | |||||
| French | 1.01 | (0.89;1.15) | 0.88 | (0.73;1.07) | 0.73 | (0.55;0.99) | 1.31 | (0.77;2.23) | 1.24 | (0.62;2.48) |
| Italian | 0.83 | (0.66;1.04) | 1.07 | (0.80;1.44) | 1.00 | (0.64;1.55) | 1.41 | (0.67;2.95) | 0.81 | (0.27;2.45) |
| Survey | ||||||||||
| 1992 | 1 | 1 | 1 | 1 | 1 | |||||
| 1997 | 1.03 | (0.86;1.23) | 1.19 | (0.84;1.70) | 1.10 | (0.72;1.69) | 1.83 | (0.79;4.21) | 0.58 | (0.22;1.52) |
| 2002 | 0.86 | (0.72;1.03) | 1.58 | (1.13;2.22) | 1.19 | (0.79;1.79) | 2.31 | (0.99;5.39) | 0.81 | (0.35;1.90) |
| 2007 | 0.60 | (0.49;0.73) | 2.12 | (1.53;2.94) | 0.95 | (0.61;1.48) | 1.26 | (0.51;3.08) | 0.40 | (0.13;1.25) |
| 2012 | 0.47 | (0.39;0.58) | 2.54 | (1.85;3.48) | 1.15 | (0.76;1.73) | 1.38 | (0.58;3.28) | 0.52 | (0.18;1.50) |
| Age | 1.00 | (1.00;1.00) | 1.04 | (1.03;1.04) | 1.02 | (1.01;1.02) | 0.97 | (0.95;0.99) | 0.97 | (0.95;1.00) |
| n | 2538 | 1037 | 434 | 121 | 66 | |||||
| Women | ||||||||||
| Fruits and vegetables | ||||||||||
| Daily | 1 | 1 | 1 | 1 | 1 | |||||
| < Daily | 2.48 | (2.19;2.80) | 0.96 | (0.84;1.10) | 1.71 | (1.22;2.40) | 1.14 | (0.98;1.33) | 1.91 | (1.42;2.56) |
| Physical activity, leisure | ||||||||||
| > 2 | 1 | 1 | 1 | 1 | ||||||
| 1 to 2 | 0.86 | (0.73;1.02) | 1.01 | (0.85;1.21) | 0.90 | (0.54;1.51) | 0.96 | (0.80;1.15) | 0.92 | (0.59;1.44) |
| Days per week | ||||||||||
| None | 1.75 | (1.49;2.06) | 1.55 | (1.32;1.83) | 2.18 | (1.38;3.43) | 1.29 | (1.08;1.54) | 2.02 | (1.33;3.08) |
| Alcohol* | ||||||||||
| Low | 1 | 1 | 1 | 1 | 1 | |||||
| Moderate | 3.50 | (2.76;4.43) | 0.81 | (0.53;1.24) | 0.55 | (0.22;1.39) | 1.07 | (0.70;1.63) | 3.42 | (2.06;5.69) |
| High | 5.51 | (3.71;8.20) | 0.83 | (0.40;1.72) | 2.19 | (0.64;7.49) | 0.91 | (0.39;2.08) | 5.90 | (2.54;13.68) |
| Missing | 1.47 | (1.14;1.90) | 1.05 | (0.76;1.46) | 0.59 | (0.18;1.94) | 0.95 | (0.69;1.32) | 1.72 | (0.92;3.22) |
| Education | ||||||||||
| Tertiary | 1 | 1 | 1 | 1 | ||||||
| Secondary II | 1.91 | (1.59;2.28) | 1.78 | (1.44;2.19) | 1.83 | (1.04;3.24) | 0.78 | (0.66;0.93) | 1.51 | (0.96;2.37) |
| Mandatory | 2.07 | (1.67;2.57) | 3.43 | (2.73;4.30) | 4.28 | (2.33;7.84) | 0.69 | (0.54;0.87) | 1.62 | (0.95;2.79) |
| Nationality | ||||||||||
| Swiss | 1 | 1 | 1 | 1 | 1 | |||||
| Foreign | 0.75 | (0.62;0.90) | 1.37 | (1.15;1.65) | 0.67 | (0.40;1.13) | 0.69 | (0.55;0.87) | 0.63 | (0.39;1.00) |
| Language region** | ||||||||||
| German | 1 | 1 | 1 | 1 | 1 | |||||
| French | 1.30 | (1.14;1.47) | 0.84 | (0.73;0.96) | 0.86 | (0.60;1.23) | 1.28 | (1.10;1.50) | 1.76 | (1.30;2.39) |
| Italian | 0.97 | (0.79;1.19) | 0.68 | (0.55;0.85) | 0.79 | (0.43;1.43) | 1.58 | (1.26;1.99) | 0.94 | (0.58;1.54) |
| Survey | ||||||||||
| 1992 | 1 | 1 | 1 | 1 | 1 | |||||
| 1997 | 1.23 | (1.03;1.47) | 1.37 | (1.09;1.74) | 2.56 | (1.32;4.97) | 0.81 | (0.65;1.02) | 1.28 | (0.81;2.01) |
| 2002 | 1.01 | (0.84;1.21) | 1.58 | (1.26;1.99) | 2.31 | (1.22;4.36) | 0.88 | (0.71;1.10) | 1.03 | (0.66;1.63) |
| 2007 | 0.93 | (0.76;1.13) | 1.84 | (1.46;2.31) | 1.90 | (0.96;3.75) | 0.77 | (0.61;0.96) | 0.93 | (0.56;1.54) |
| 2012 | 0.56 | (0.46;0.70) | 2.07 | (1.66;2.59) | 2.09 | (1.05;4.15) | 0.93 | (0.75;1.15) | 0.50 | (0.30;0.82) |
| Age | 0.98 | (0.97;0.98) | 1.03 | (1.02;1.03) | 0.99 | (0.98;1.00) | 0.98 | (0.97;0.98) | 0.97 | (0.96;0.98) |
| n | 2085 | 1980 | 227 | 1347 | 313 | |||||
*Cut-offs: men <40g and <60g and women <20g and <40g of alcohol per day;
**German included Romansh; results shown only for selected combinations of BMI and smoking status.
Missing: BMI n = 1258, smoking status n = 4382, fruits and vegetables n = 1571, physical activity n = 3555, alcohol n = 4966.
The results for smokers by the investigated BMI categories are described in depth as follows. Male normal-weight and obese smokers were likely to have an infrequent fruit and vegetable consumption, low physical inactivity level, and high alcohol intake. For example in men, if an individual reported a low fruit and vegetable consumption, the relative risk ratio for being an obese smoker relative to normal-weight never smoker would be expected to be increased (RRR 1.69 [1.30;2.21]) compared to an individual having a high fruit and vegetable consumption. In underweight smoking men, significant associations were found for physical inactivity and high risk alcohol intake, despite the small stratum size and therefore wide confidence intervals. Female normal-weight and underweight smokers were likely to have an unfavourable behaviour in all three lifestyle factors. Obese smoking women were more likely to have infrequent fruit and vegetable consumption and high alcohol intake. In contrast to men, women who smoked and/or were underweight or obese were more likely to be physically inactive.
Only a selection of the smoking/BMI combination groups is shown. To briefly summarize the results for the remaining 14 outcome categories, we found that individuals in these categories were less likely to have low fruit and vegetable consumption, high alcohol intake, and physical inactivity, compared to those individuals in the categories with heavy smoking and extreme BMI (not shown). Only overweight heavy smokers showed similar poor behaviour in the three lifestyle variables investigated. In addition, we observed that the lifestyle tended to deteriorate, the more an individual smoked.
Socio-demographic adjustment variables were strongly associated with the combination of heavy smoking and obesity or underweight. In general, individuals with lower educational level were more likely to have an extreme BMI and being a smoker. However, this association was reversed in underweight women. Male foreign nationals were more likely to be normal-weight or obese smokers and obese never smokers, respectively. Being female Swiss national was associated with being normal-weight smoker or underweight never smoker, whereas foreign nationals were more likely to be obese never smokers. A significant impact of language region was observed mainly in women. Compared to women living in the German speaking part, women from the French and Italian speaking region were more likely to be underweight and less likely to be obese. Moreover, those from the French speaking part were more likely to be underweight smokers.
A decrease in the prevalence of heavy smokers between 1992 and 2012 was observed in those with normal-weight, especially in men (Table 3). Furthermore, the results suggest that the prevalence of the combination of heavy smoking with underweight and obesity changed in women only; it increased in female obese heavy smokers and decreased female underweight heavy smokers. The prevalence of obese never smokers increased in both sexes.
Discussion
Main results
In this study, we investigated how heavy smoking and extreme BMI as well as the combination of both were associated with other NCD risk factors. Heavy smokers were more likely to have a poor diet, high alcohol intake and low level of physical activity than obese or underweight individuals. While the prevalence of smoking decreased over time in combination with normal-weight, it increased in combination with obesity in women.
Clustering of lifestyle factors
In line with our results, studies on clustering effects of unfavourable lifestyle factors in adults emphasise the role of smoking as driving factor [11,26]. The association of smoking was observed to be particularly strong with high alcohol intake [27]. Clustering effects of unhealthy lifestyles were reported to be more likely in individuals with a low educational level [12,13]. In our study, this was consistently shown in men, i.e. smoking and high/low BMI were associated with low educational level. In contrast, this association was reversed in women, i.e. underweight was associated with high educational level. Others showed that men and especially women with higher socioeconomic status were more concerned about their body weight and made more efforts to control it [28,29]. Interestingly, unhealthy behaviours were found to cluster stronger than healthy behaviours [30]. We are not aware of other studies performing a comparative analysis of the lifestyle of heavy smokers, obese, and underweight individuals. However, a study looking at age-specific lifestyle risk factors for obesity observed that young and middle-aged obese adults were frequently physically inactive; in older obese adults, poor eating habits were identified as an additional risk factor [31]. So far, much less has been reported about the lifestyle of underweight individuals because in developed countries the prevalence and, therewith, public health relevance is lower compared to obesity [32]. Reverse causation due to smoking and pre-existing disease has to be taken into account when studying health effects of underweight, e.g. mortality [33,34]. Our findings suggest that underweight never smoking women were at risk for physical inactivity, which could be either an attitude or indicating an underlying disease.
Prevalence trends
We found that the prevalence of normal-weight heavy smokers decreased in Switzerland between 1992 and 2012 in both sexes. Across Europe, considerable differences in smoking prevalence exist; eastern and low income countries as well as countries with less advanced tobacco control policies have highest smoking prevalence [35]. An estimation of smoking prevalence worldwide showed that it is especially high among men in South, Southeast, and East Asia, e.g. more than 50% in Russia and Indonesia [14]. Our results show that in Switzerland the decrease in smoking prevalence mainly occurred in those with normal BMI; amongst obese individuals, the smoking prevalence stagnated (men) or even increased (women). This suggests that clustering of unhealthy lifestyles persisted or accentuated over time in part of the population, low socioeconomic status was shown to be an important factor explaining this effect [36–38].
Public health relevance
Our results support the notion of smoking as a key determinant of an unhealthy lifestyle. In light of the ongoing clustering of smoking with other unfavourable lifestyle factors, efforts aimed at reducing tobacco use in the population need to be intensified. This is supported by the recent trends of cancer death in women; in Europe lung cancer is the leading cause, thus superseded breast cancer [39]. In Switzerland, previous efforts led to a decrease of the smoking prevalence in general, but a decrease was only observed in the normal-weight part of the population. Because obese and underweight smokers have a particularly problematic health risk pattern, a decrease in smoking prevalence would be even more important than in normal-weight individuals. In Switzerland, obesity contributes to an excess in death of about 7% and costs of 8 billion Swiss Francs; smoking of about 12% and 10 billion Swiss Francs [40–43]. As shown by Li et al. [44], non-smoking and maintaining healthy body weight are the lifestyles with the greatest potential to reduce the number of premature deaths and should therefore be the main target of public health strategies improving lifestyle.
Strengths and Limitations
The SHS is a comprehensive survey collecting data on major lifestyle risk factors through a large representative sample of the general population. The large sample size allowed for the analysis of lifestyle factors in defined risk groups based on BMI category and smoking status. Potential confounders were included in the analysis, especially education. The repeated assessment (the SHS is conducted every 5 years) provided insights into changes over time in prevalence of the considered risk groups.
The participation rate decreased over the 5 SHS from 71% in 1992 to 53% in 2012 [17,45]. Two measures were implemented to account for this decrease in participation rate. First, in 2012 efforts were intensified to include persons having no landline telephone number available in the database, by sending out prepaid answer postcards to obtain further contact information to conduct the telephone interview. Second, analysis of the SHS data has to be done by applying weighting according to the general population of Switzerland. Nevertheless, it is likely that participants tend to be healthier than non-participants [46]. Self-reporting on lifestyle variables made non-differential misclassification of those variables more likely. Only a short questionnaire was used to evaluate fruit and vegetable consumption, alcohol intake and physical activity [47,48]. To draw conclusions, for example on the adherence to the “5-a-day” recommendation, more detailed information would be needed. The assessment of fruit and vegetable consumption was even aggravated by the fact that the collected information changed over the course of surveys and, therefore, it was necessary to use a dichotomized variable. BMI was shown to be underestimated in obese and overestimated in underweight [49]. For underweight, effect estimates were imprecise as strata size was small. Finally, due to the cross-sectional study design no causal relationships can be inferred.
Conclusion
Both heavy smoking and BMI extremes were associated with unhealthy general lifestyle, rendering them particularly vulnerable for NCDs. However, the relationship was stronger for heavy smoking than for obesity and underweight. Smoking prevention measures should pay special attention to improvement of general lifestyle and co-occurrence with obesity and underweight. Future research in this area should focus on how lifestyle factors are interacting in the development of NCDs, i.e. looking at lifestyle patterns rather than single lifestyle risk factors. In addition, investigating the role of lifestyle factors using a life course approach may help to deepen the understanding of their association with NCDs.
Supporting Information
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We thank the Swiss Cancer Research foundation (SCR) for supporting our study (grant no. KFS-3048-08-2012) and the Swiss Federal Statistical Office for providing data.
Data Availability
Individual data of the Swiss Health Survey are property of the Swiss Federal Statistical Office (SFSO) and may only be made available by SFSO. Requests for access have to be submitted to Mr. Marco D'Angelo (head of division, MarcoDAngelo@bfs.admin.ch). For information contact sgb12@bfs.admin.ch.
Funding Statement
This work was supported by the Swiss Cancer Research foundation (SCR), grant no. KFS-3048-08-2012, http://www.krebsliga.ch, and the Swiss Federal Statistical Office. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Danaei G, Vander Hoorn S, Lopez AD, Murray CJL, Ezzati M. Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. Lancet. 2005;366: 1784–93. 10.1016/S0140-6736(05)67725-2 [DOI] [PubMed] [Google Scholar]
- 2.Fan J, Song Y, Chen Y, Hui R, Zhang W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: a meta-analysis of prospective cohort studies. Int J Cardiol. Elsevier Ireland Ltd; 2013;168: 4761–8. 10.1016/j.ijcard.2013.07.230 [DOI] [PubMed] [Google Scholar]
- 3.Erhardt L. Cigarette smoking: an undertreated risk factor for cardiovascular disease. Atherosclerosis. 2009;205: 23–32. 10.1016/j.atherosclerosis.2009.01.007 [DOI] [PubMed] [Google Scholar]
- 4.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer : a systematic review and meta-analysis of prospective observational studies. Lancet. 2007; 569–578. [DOI] [PubMed] [Google Scholar]
- 5.Loprinzi PD, Crespo CJ, Andersen RE, Smit E. Association of Body Mass Index with Cardiovascular Disease Biomarkers. Am J Prev Med. Elsevier; 2014; 1–7. 10.1016/j.amepre.2014.08.019 [DOI] [PubMed] [Google Scholar]
- 6.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-Specific Excess Deaths Associated With Underweight, Overweight, and Obesity. JAMA. 2007;298: 2028–37. 10.1001/jama.298.17.2028 [DOI] [PubMed] [Google Scholar]
- 7.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328: 1519 10.1136/bmj.38142.554479.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma J, Jemal A, Flanders WD, Ward EM. Joint association of adiposity and smoking with mortality among U.S. adults. Prev Med (Baltim). 2013;56: 178–84. 10.1016/j.ypmed.2012.12.012 [DOI] [PubMed] [Google Scholar]
- 9.Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med (Baltim). Elsevier Inc.; 2012;55: 163–70. 10.1016/j.ypmed.2012.06.017 [DOI] [PubMed] [Google Scholar]
- 10.Martin-Diener E, Meyer J, Braun J, Tarnutzer S, Faeh D, Rohrmann S, et al. The combined effect on survival of four main behavioural risk factors for non-communicable diseases. Prev Med (Baltim). Elsevier Inc.; 2014;65: 148–152. 10.1016/j.ypmed.2014.05.023 [DOI] [PubMed] [Google Scholar]
- 11.Chiolero A, Wietlisbach V, Ruffieux C, Paccaud F, Cornuz J. Clustering of risk behaviors with cigarette consumption: A population-based survey. Prev Med (Baltim). 2006;42: 348–53. 10.1016/j.ypmed.2006.01.011 [DOI] [PubMed] [Google Scholar]
- 12.Schuit AJ, van Loon AJM, Tijhuis M, Ocké MC. Clustering of Lifestyle Risk Factors in a General Adult Population. Prev Med (Baltim). 2002;35: 219–224. 10.1006/pmed.2002.1064 [DOI] [PubMed] [Google Scholar]
- 13.De Vries H, van ‘t Riet J, Spigt M, Metsemakers J, van den Akker M, Vermunt JK, et al. Clusters of lifestyle behaviors: results from the Dutch SMILE study. Prev Med (Baltim). 2008;46: 203–8. 10.1016/j.ypmed.2007.08.005 [DOI] [PubMed] [Google Scholar]
- 14.Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA. American Medical Association; 2014;311: 183–92. 10.1001/jama.2013.284692 [DOI] [PubMed] [Google Scholar]
- 15.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roh L, Braun J, Chiolero A, Bopp M, Rohrmann S, Faeh D. Mortality risk associated with underweight: a census-linked cohort of 31,578 individuals with up to 32 years of follow-up. BMC Public Health. 2014;14: 371 10.1186/1471-2458-14-371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bundesamt für Statistik. Die Schweizerische Gesundheitsbefragung 2012 in Kürze—Konzept, Methode, Durchführung. 2013. Available: http://www.bfs.admin.ch
- 18.National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report Obes Res. 1998. [PubMed] [Google Scholar]
- 19.WHO. Fruit and Vegetable Promotion Initiative—report of the meeting. Geneva; [Google Scholar]
- 20.Wanner M, Tarnutzer S, Martin BW, Braun J, Rohrmann S, Bopp M, et al. Impact of different domains of physical activity on cause-specific mortality: a longitudinal study. Prev Med (Baltim). Elsevier Inc.; 2014;62: 89–95. 10.1016/j.ypmed.2014.01.025 [DOI] [PubMed] [Google Scholar]
- 21.UNESCO Institute for Statistics. International Standard Classification of Education—ISCED 2011. Motreal; 2012. [Google Scholar]
- 22.Bottorff JL, Haines-Saah R, Oliffe JL, Sarbit G. Gender influences in tobacco use and cessation interventions. Nurs Clin North Am. 2012;47: 55–70. 10.1016/j.cnur.2011.10.010 [DOI] [PubMed] [Google Scholar]
- 23.Higgins ST, Kurti AN, Redner R, White TJ, Gaalema DE, Roberts ME, et al. A literature review on prevalence of gender differences and intersections with other vulnerabilities to tobacco use in the United States, 2004–2014. Prev Med (Baltim). 2015; 10.1016/j.ypmed.2015.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hosmer D, Lemeshow S. Applied Logistic Regression. Second Edi New York: John Wiley & Sons; 2000. [Google Scholar]
- 25.Bundesamt für Statistik. Statistik der Bevölkerung und der Haushalte (STATPOP). 2012. Available: http://www.bfs.admin.ch
- 26.Dallongeville J, Mare N, Fruchart J, Amouyel P. Cigarette Smoking Is Associated with Unhealthy Patterns of Nutrient Intake: a Meta-analysis. Am Soc Nutr Sci. 1998;128: 1450–1457. [DOI] [PubMed] [Google Scholar]
- 27.De Leon J, Rendon DM, Baca-Garcia E, Aizpuru F, Gonzalez-Pinto A, Anitua C, et al. Association between smoking and alcohol use in the general population: Stable and unstable odds ratios across two years in two different countries. Alcohol Alcohol. 2007;42: 252–257. 10.1093/alcalc/agm029 [DOI] [PubMed] [Google Scholar]
- 28.Wardle J, Griffith J. Socioeconomic status and weight control practicesin British adults. J Epidemiol Community Heal. 2001;55: 185–190. 10.1136/jech.55.3.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choi OJE, Cho YG, Kang JH, Park HA, Kim KW, Hur YI, et al. Weight control attempts in underweight korean adults: Korea national health and nutrition examination survey, 2007–2010. Korean J Fam Med. 2013;34: 393–402. 10.4082/kjfm.2013.34.6.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tobias M, Jackson G, Yeh L-C, Huang K. Do healthy and unhealthy behaviours cluster in New Zealand? Aust N Z J Public Health. 2007;31: 155–163. 10.1111/j.1753-6405.2007.00034.x [DOI] [PubMed] [Google Scholar]
- 31.Siddarth D. Risk factors for obesity in children and adults. J Investig Med. 2013;61: 1039–42. 10.231/JIM.0b013e31829c39d0 [DOI] [PubMed] [Google Scholar]
- 32.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341: 1097–105. 10.1056/NEJM199910073411501 [DOI] [PubMed] [Google Scholar]
- 33.Flegal KM, Graubard BI, Williamson DF, Cooper RS. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am J Epidemiol. 2011;173: 1–9. 10.1093/aje/kwq341 [DOI] [PubMed] [Google Scholar]
- 34.Willett WC, Dietz WH, Colditz GA. Guidelines for Healthy Weight. N Engl J Med. 1999;341: 427–434. 10.1056/NEJM199908053410607 [DOI] [PubMed] [Google Scholar]
- 35.Gallus S, Lugo A, La Vecchia C, Boffetta P, Chaloupka FJ, Colombo P, et al. Pricing Policies And Control of Tobacco in Europe (PPACTE) project: cross-national comparison of smoking prevalence in 18 European countries. Eur J Cancer Prev. 2014;23: 177–85. 10.1097/CEJ.0000000000000009 [DOI] [PubMed] [Google Scholar]
- 36.Buck D, Frosini F. Clustering of unhealthy behaviours over time—Implications for policy and practice. London; 2012. [Google Scholar]
- 37.Marques-Vidal P, Bovet P, Paccaud F, Chiolero A. Changes of overweight and obesity in the adult Swiss population according to educational level, from 1992 to 2007. BMC Public Health. 2010;10: 87 10.1186/1471-2458-10-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Faeh D, Braun J, Bopp M. Prevalence of obesity in Switzerland 1992–2007: the impact of education, income and occupational class. Obes Rev. 2010;12: 151–66. 10.1111/j.1467-789X.2010.00793.x [DOI] [PubMed] [Google Scholar]
- 39.Malvezzi M, Bertuccio P, Rosso T, Rota M, Levi F, Vecchia C La, et al. European cancer mortality predictions for the year 2015 : does lung cancer have the highest death rate in EU women ? Ann Oncol. 2015;00: 1–8. 10.1093/annonc/mdv001 [DOI] [PubMed] [Google Scholar]
- 40.Faeh D, Braun J, Tarnutzer S, Bopp M. Obesity but not overweight is associated with increased mortality risk. Eur J Epidemiol. 2011;26: 647–55. 10.1007/s10654-011-9593-2 [DOI] [PubMed] [Google Scholar]
- 41.Maag J, Braun J, Bopp M, Faeh D. Direct estimation of death attributable to smoking in Switzerland based on record linkage of routine and observational data. Nicotine Tob Res. 2013;15: 1588–97. 10.1093/ntr/ntt023 [DOI] [PubMed] [Google Scholar]
- 42.Wieser S, Kauer L, Schmidhauser S, Pletscher M, Brügger U, Jeanrenaud C, et al. Synthesebericht– Ökonomische Evaluation von Präventionsmassnahmen in der Schweiz. Winterthur; 2010. Available: http://www.bag.admin.ch
- 43.Schneider H, Venetz W. Cost of Obesity in Switzerland in 2012. Rheinfelden; 2014. Available: http://www.bag.admin.ch
- 44.Li K, Hüsing A, Kaaks R. Lifestyle risk factors and residual life expectancy at age 40: a German cohort study. BMC Med. 2014;12: 59 10.1186/1741-7015-12-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Faeh D, Bopp M. Excess weight in the canton of Zurich, 1992–2009: Harbinger of a trend reversal in Switzerland? Swiss Med Wkly. 2010;140: 1–6. 10.4414/smw.2010.13090 [DOI] [PubMed] [Google Scholar]
- 46.Bopp M, Braun J, Faeh D, National S, Study C. Practice of Epidemiology Variation in Mortality Patterns Among the General Population, Study Participants, and Different Types of Nonparticipants : Evidence From 25 Years of Follow-up. Am J Epidemiol. 2014;180: 1028–1035. [DOI] [PubMed] [Google Scholar]
- 47.Eichholzer M, Bisig B. Daily consumption of (red) meat or meat products in Switzerland: results of the 1992/93 Swiss Health Survey. Eur J Clin Nutr. 2000;54: 136–142. 10.1038/sj.ejcn.1600907 [DOI] [PubMed] [Google Scholar]
- 48.Rehm J, Spuhler T. Measurement error in alcohol consumption: the Swiss Health Survey. Eur J Clin Nutr. 1993;47: S25–S30. [PubMed] [Google Scholar]
- 49.Stommel M, Schoenborn C. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001–2006. BMC Public Health. 2009;9: 421 10.1186/1471-2458-9-421 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Individual data of the Swiss Health Survey are property of the Swiss Federal Statistical Office (SFSO) and may only be made available by SFSO. Requests for access have to be submitted to Mr. Marco D'Angelo (head of division, MarcoDAngelo@bfs.admin.ch). For information contact sgb12@bfs.admin.ch.