Abstract
Burning mouth syndrome (BMS) is multifactorial in origin which is typically characterized by burning and painful sensation in an oral cavity demonstrating clinically normal mucosa. Although the cause of BMS is not known, a complex association of biological and psychological factors has been identified, suggesting the existence of a multifactorial etiology. As the symptom of oral burning is seen in various pathological conditions, it is essential for a clinician to be aware of how to differentiate between symptom of oral burning and BMS. An interdisciplinary and systematic approach is required for better patient management. The purpose of this study was to provide the practitioner with an understanding of the local, systemic, and psychosocial factors which may be responsible for oral burning associated with BMS, and review of treatment modalities, therefore providing a foundation for diagnosis and treatment of BMS.
Keywords: Burning mouth syndrome, Classification, Diagnosis, Pain management
INTRODUCTION
Burning mouth syndrome (BMS) is a chronic pain disorder characterized by burning, stinging, and/or itching of the oral cavity in the absence of any organic disease. The International Association for the study of pain defines it as a pain of at least 4–6 months duration located on the tongue or other mucosal membranes in the absence of clinical or laboratory findings.[1] BMS can be accompanied by dysgeusia (distortion in sense of taste) and subjective xerostomia (dry mouth).[2]
HISTORICAL BACKGROUND
First described in the mid-19th century, this condition was further characterized in the early 20th century by Butlin and Oppenheim as glossodynia. Over the ensuing years, BMS has been referred to as oral dysesthesia, sore tongue, stomatodynia, and stomatopyrosis. The most affected area is the tongue (tip and lateral borders) thus denominated the terms glossodynia (painful tongue), glossopyrosis (burning tongue), and glossalgia.[1,3]
It was first categorized as a distinct disease in 2004 by the International Headache Society, which defined primary BMS as “an intraoral burning sensation for which no medical or dental cause can be found.” The current diagnostic criteria consist of daily persistent pain in the mouth with normal oral mucosa after exclusion of local and systemic diseases.[4] This review focuses on various aspects of BMS including its epidemiology, pathophysiology, etiology, clinical presentation, differential diagnosis, classification, clinical diagnosis, current treatment, and general prognosis.
EPIDEMIOLOGY
Epidemiological studies on BMS have estimated a prevalence rate of 2.6–5.1%. Due to the lack in the consensus of diagnosing BMS, prevalence rates tend to vary across studies. The prevalence of BMS reported from international studies ranges from commonly reported range has been 0.7–4.6%.[5] The mean age of BMS is between 55 and 60 years, with occurrence under 30 being rare. The ratio between females and males varies from 3:1 to 16:1. Furthermore, up to 90% of female patients with BMS are perimenopausal women with typical onset from 3 years prior to 12 years post the beginning of menopause.[6]
CLASSIFICATION
Lamey and Lewis (1989) classified BMS into three types depending on the intensity of pain.[7]
Type 1 (35%) is characterized by patients having burning every day. The burning is absent on waking but presents as the day goes on, being maximal in the evening. This type may be linked to systemic disorders, such as nutritional deficiencies and endocrine disorders
Type 2 (55%) is characterized by burning that occurs every day, is present on awakening and often makes falling asleep at night difficult. This subgroup of patients often report mood changes, alterations in eating habits, and decreased desire to socialize, which seem to be attributable to an altered sleep pattern
Type 3 (10%) is characterized by intermittent burning, present only on some days, with burning affecting unusual sites such as the floor of the mouth, buccal mucosa, and throat. These patients frequently display anxiety and allergic reactions, particularly to food additives.
Scala et al. classified BMS into:
Primary (essential/idiopathic) BMS: For which no organic local/systemic causes are identified
Secondary BMS: Resulting from local/systemic pathological conditions, and thus this form responds well to the etiology-directed therapy.[5]
ETIOPATHOGENESIS
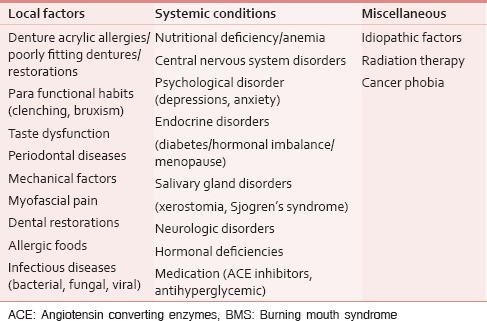
BMS is an important clinical condition with aggravating symptoms, directly and indirectly impacting the quality of life, which often places a recognizable burden on the patient and healthcare system. Because of the complex clinical behavior, the exact cause of BMS is currently unknown. The etiology is presumed to be multifactorial [Table 1] involving the interaction between neurophysiological mechanisms and psychological factors.[1,8,9]
Table 1.
Etiologic factors of BMS
The presence of taste changes and sensory anomalies indicate toward the fact that BMS has some neuropathic basis.[10] Neurophysiological studies suggest that the central and/or peripheral nervous systems are implicated in the pain of BMS.[11] This causes a loss of central inhibition and consequently hyperactivity of the trigeminal nociceptive pathway, which in turn carries a more intense response to oral irritants and eventually leads to the appearance of phantom oral pain as a result of this alteration in the taste system.[12]
Central neuropathic mechanisms have been demonstrated following thermal stimulation of the trigeminal nerve in patients with BMS. Patients with BMS show patterns of cerebral activity similar to those that appear in other neuropathic pain disorders, suggesting that the cerebral hypoactivity could be an important element in the pathogenesis of BMS.[13]
The possible theories behind the cause of BMS are enlisted here:
Abnormal interaction between the sensory functions of facial and trigeminal nerves.[12] According to this theory, certain individuals labeled as supertasters (mainly females) due to the high density of fungiform papilla present on the anterior aspect of tongue, are at risk of developing burning pain[14]
Sensory dysfunction associated with small and/or large fiber neuropathy.[15] Forssell et al. found that almost 90% of individuals with BMS had some form of altered sensory threshold and/or blink reflex reaction. Immunohistochemical and microscopic observations revealed axonal degeneration of epithelial and subpapillary nerve fibers in the affected epithelium of the oral mucosa[16]
Centrally mediated alteration in the modulation of nociceptive processing. This theory explains the fact that resulting in reduced central pain suppression in BMS individuals[17]
Disturbances in the autonomic innervation and oral blood flow[18]
Chronic anxiety or stress results in the alteration of gonadal, adrenal, and neuroactive steroid levels in skin and oral mucosa.[19]
CLINICAL PRESENTATION
A typical patient with BMS is postmenopausal woman of age 4th–6th decade with various medical comorbidities.[20] Clinical presentations may vary as some patients can be oligosymptomatic (pain and dysgeusia or xerostomia) or monosymptomatic (pain only) usually associated with dry mouth, bitter/metallic or altered taste.[21]
PAIN CHARACTERISTICS IN BURNING MOUTH SYNDROME
The patients usually complain of chronic pain of 4–6 months duration, burning or scalding type, sometimes itching sensation or numbness of the tongue, and other oral mucosal surfaces.[3] The onset of pain can be either gradual and spontaneous or sudden and related to a precipitating event such as any dental procedure. Typically, pain is localized to the tongue and sometimes involving other mucosal surfaces also such as palate, lip, buccal mucosa, and floor of the mouth. The pain will be continuous or intermittent, mild to moderate in intensity, localized to the oral cavity and does not radiate to other regions of the face. The pain typically relieves on intake of food or liquids, which is in contrast to burning symptom in other diseases; in which the pain aggravates.[4,21]
Physical examination and laboratory analysis are classically unremarkable in primary BMS. However, they can be abnormal in secondary BMS.[1]
The pain is primarily bilateral and symmetrical on the anterior two-third of the tongue (71%–78%), followed by the dorsum and lateral borders of the tongue, the anterior part of the hard palate, the labial mucosa, and gingiva, often appearing at several locations.[22]
DIAGNOSTIC CRITERIA
Diagnosis of BMS may be complex for three main reasons:
BMS is positively defined only by symptom(s) without regard to signs or etiologies
The symptomatic triad rarely occurs simultaneously in same patient[2]
Overlapping or overwhelming stomatitis may confuse the clinical presentation.
As a result, clinicians can arrive at a diagnosis of BMS by matching specific details of the main complaint with clinical oral findings that exclude oral mucosal changes.
The diagnostic criteria developed by Scala et al., for the diagnosis of BMS are as follows.[5]
Fundamental criteria
Daily deep burning sensation of the bilateral oral mucosa
Burning sensation for at least 4–6 months
Constant intensity or increasing intensity during the day
No worsening on eating or drinking. Instead, the burning sensation may reduce
No interference with sleep.
Additional criteria
Dysgeusia and/or xerostomia
Sensory or chemosensory alterations
Mood changes or psychopathological alterations.
Pain that gets worse over the day decreased pain on eating and with sleep absence of clinical finding, presence of abnormal or dysgeusia tastes, usually metallic, bitter or sour, and complaint of dry mouth in presence of normal flows are other findings which help in diagnosis of BMS.[23]
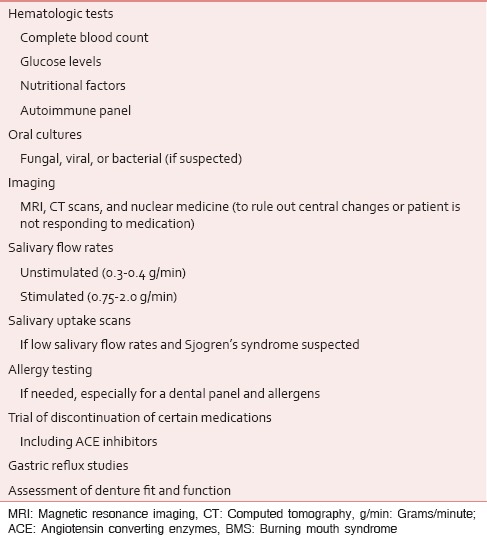
INVESTIGATIONS
Taking a thorough and comprehensive history is the key to diagnosis of BMS. Important information to be ascertained by the practitioner relates to the past and current symptoms (pain, dry mouth, and taste), their duration, intensity, character, location, onset, and factors that improve or worsen the pain and its course. Various clinical and laboratory tests [Table 2] can be carried out any possible local factors that may be responsible for the oral burning complaints.[1,24,25]
Table 2.
Investigations for BMS
MIMICKERS OF BURNING MOUTH SYNDROME
BMS presents with a main complaint of an intraoral sensation of burning, tingling, or stinging and sometimes accompanied by taste disturbances or dry mouth.[4] The mimickers of BMS may include stomatitis, atypical facial pain, atypical odontalgia, idiopathic facial arthromyalgia, pemphigoid, pemphigus, neoplastic lesions in the oral cavity, acoustic neuroma, denture design or tooth restoration failures, herpes simplex or herpes zoster, and trauma to lingual or mandibular nerves after dental surgery. Detailed history and physical examination are crucial to differentiate above medical conditions.[5,26]
TREATMENT MODALITIES
Before starting the treatment, it is important to inform the patient about nature of disease and give reassurance. Patient management involves a differential diagnosis for BMS and the discrimination between “primary BMS” and “secondary BMS” based on the identification of possible etiologic factors for the syndrome. The most used medications [Table 3] to treat this syndrome are antidepressants, antipsychotics, sedatives, antiepileptics, analgesics and oral mucosa protectors, sialagogues, and vitamin-mineral replacements.[2,10,27,28] Various alternative treatment modalities have also been implicated, which includes lasers, acupuncture, behavioral therapies, yoga, relaxation therapy, meditation, group psychotherapy, and electroconvulsive therapy; the purpose of these medications is to reduce the suffering of the patients and to bring their condition under better control and improve the quality of life. Control of parafunctional activity prosthesis adjustment in case of patient wearing prosthesis.[28,29]
Table 3.
Different treatment modalities used in the management of BMS
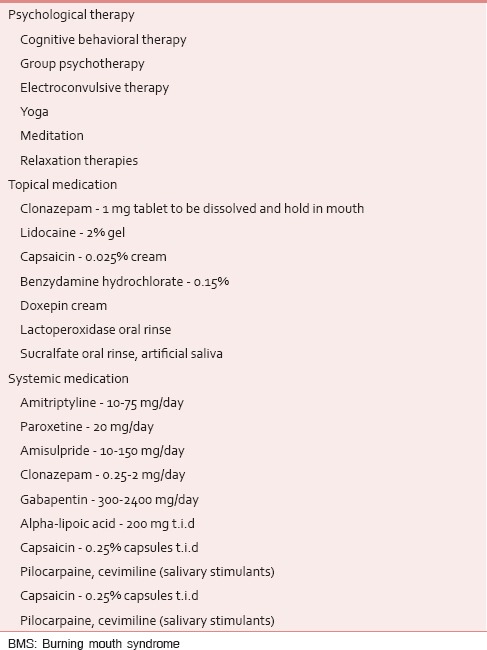
Grushka et al. suggested that the best treatment for the syndrome consists of a combination of drugs, such as clonazepam, gabapentin, and baclofen.[30] Gremeau-Richard et al., in 2004, reported significant reduction in pain with topical application of clonazepam in patients with BMS.[31] Heckmann et al. conducted a double-blind study on clonazepam in patients with BMS. They found that patients on clonazepam (0.5 mg/day) were significantly improved in pain rating as compared to placebo (lactose).[32] Local application of desensitizing agents such as topical capsaicin: The use of hot pepper sauce (a good source of capsaicin) in water in the ratio of 1:2 is also found to be effective in reducing oral pain in BMS. Capsaicin acts by depletion of substance p, so results in decreased peripheral burning.[33]
Volpe et al., in his study on postmenopausal women, found that 12 out of 22 patients experienced improvement in oral symptoms after estradiol-based treatment.[34] Femiano et al., in 2002, have shown the use of alpha lipoic acid in management of BMS, 96% of patients had shown significant improvement in their symptoms. It is a potent antioxidant and neuroprotective agent.[35] However, Cavalcanti et al., in their randomized, double-blind, placebo-controlled trial of 38 patients, did not find effectiveness of alpha lipoic acid, in comparison with the control group given placebo, in the management of BMS.[36]
Bergdahl et al. suggested the use of cognitive behavioral therapy for BMS patients. He found reduction in pain intensity following cognitive behavioral therapy (CBT) immediately, following therapy.[37] Mock and Chugh,[38] and Reamy et al.,[39] found the combination of CBT, alpha lipoic acid, and/or clonazepam as the most promising.
PROGNOSIS
Although the short-term follow-up studies may show potential symptomatic improvement with treatment in patients with BMS, the long-term outcomes for BMS remain unclear. In perspective, complete understanding of the etiology and pathogenesis is imperative to the development of novel and efficacious therapeutic strategies and will guide overall prognosis of the disease in the future.
CONCLUSION
BMS is a relatively common chronic intraoral pain disorder classically characterized by intractable burning that may be associated with dysgeusia and xerostomia. Etiology of BMS is multifactorial, and a secondary form of BMS should be diligently sought for and treated. Multidisciplinary approach including medical and psychosocial therapy may be effective in symptom relief in patients with BMS; however, further studies are necessary to establish long-term prognosis. BMS remains an important medical condition which often places a significant burden on the patient and healthcare system and requires diligent recognition and treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aggarwal A, Panat SR. Burning mouth syndrome: A diagnostic and therapeutic dilemma. J Clin Exp Dent. 2012;4:e180–5. doi: 10.4317/jced.50764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ambaldhage VK, Puttabuddi JH, Nunsavath PN. Burning mouth syndrome: An update. Indian J Pain. 2015;29:2–8. [Google Scholar]
- 3.López-Jornet P, Camacho-Alonso F, Andujar-Mateos P, Sánchez-Siles M, Gómez-Garcia F. Burning mouth syndrome: An update. Med Oral Patol Oral Cir Bucal. 2010;15:e562–8. doi: 10.4317/medoral.15.e562. [DOI] [PubMed] [Google Scholar]
- 4.Gurvits GE, Tan A. Burning mouth syndrome. World J Gastroenterol. 2013;19:665–72. doi: 10.3748/wjg.v19.i5.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scala A, Checchi L, Montevecchi M, Marini I, Giamberardino MA. Update on burning mouth syndrome: Overview and patient management. Crit Rev Oral Biol Med. 2003;14:275–91. doi: 10.1177/154411130301400405. [DOI] [PubMed] [Google Scholar]
- 6.Dahiya P, Kamal R, Kumar M, Gupta R, Chaudhary K. Burning mouth syndrome and menopause. Int J Prev Med. 2013;4:15–20. [PMC free article] [PubMed] [Google Scholar]
- 7.Lamey PJ, Lewis MA. Oral medicine in practice: Burning mouth syndrome. Br Dent J. 1989;167:197–200. doi: 10.1038/sj.bdj.4806969. [DOI] [PubMed] [Google Scholar]
- 8.Sameera A, Suman SV, Raviraj J, Murugesh J, Suresh D. Burning mouth syndrome – A review. J Adv Oral Res. 2014;3:90–5. [Google Scholar]
- 9.Aravindhan R, Vidyalakshmi S, Kumar MS, Satheesh C, Balasubramanium AM, Prasad VS. Burning mouth syndrome: A review on its diagnostic and therapeutic approach. J Pharm Bioallied Sci. 2014;6(Suppl 1):S21–5. doi: 10.4103/0975-7406.137255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma N, Kaur J, Malhotra D, Kolli GK. An overview of burning mouth syndrome. IJDS. 2012;4:106–10. [Google Scholar]
- 11.Fedele S, Fricchione G, Porter SR, Mignogna MD. Burning mouth syndrome (stomatodynia) QJM. 2007;100:527–30. doi: 10.1093/qjmed/hcm049. [DOI] [PubMed] [Google Scholar]
- 12.Grushka M, Epstein JB, Gorsky M. Burning mouth syndrome and other oral sensory disorders: A unifying hypothesis. Pain Res Manag. 2003;8:133–5. doi: 10.1155/2003/654735. [DOI] [PubMed] [Google Scholar]
- 13.Brufau-Redondo C, Martín-Brufau R, Corbalán-Velez R, de Concepción-Salesa A. Burning mouth syndrome. Actas Dermosifiliogr. 2008;99:431–40. [PubMed] [Google Scholar]
- 14.Bartoshuk LM, Snyder DJ, Grushka M, Berger AM, Duffy VB, Kveton JF. Taste damage: Previously unsuspected consequences. Chem Senses. 2005;30(Suppl 1):i218–9. doi: 10.1093/chemse/bjh192. [DOI] [PubMed] [Google Scholar]
- 15.Forssell H, Jääskeläinen S, Tenovuo O, Hinkka S. Sensory dysfunction in burning mouth syndrome. Pain. 2002;99:41–7. doi: 10.1016/s0304-3959(02)00052-0. [DOI] [PubMed] [Google Scholar]
- 16.Lauria G, Majorana A, Borgna M, Lombardi R, Penza P, Padovani A, et al. Trigeminal small-fiber sensory neuropathy causes burning mouth syndrome. Pain. 2005;115:332–7. doi: 10.1016/j.pain.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 17.Jääskeläinen SK, Rinne JO, Forssell H, Tenovuo O, Kaasinen V, Sonninen P, et al. Role of the dopaminergic system in chronic pain – A fluorodopa-PET study. Pain. 2001;90:257–60. doi: 10.1016/S0304-3959(00)00409-7. [DOI] [PubMed] [Google Scholar]
- 18.Heckmann SM, Heckmann JG, HiIz MJ, Popp M, Marthol H, Neundörfer B, et al. Oral mucosal blood flow in patients with burning mouth syndrome. Pain. 2001;90:281–6. doi: 10.1016/S0304-3959(00)00410-3. [DOI] [PubMed] [Google Scholar]
- 19.Woda A, Dao T, Gremeau-Richard C. Steroid dysregulation and stomatodynia (burning mouth syndrome) J Orofac Pain. 2009;23:202–10. [PubMed] [Google Scholar]
- 20.Brailo V, Vuéiaeeviae-Boras V, Alajbeg IZ, Alajbeg I, Lukenda J, Aeurkoviae M. Oral burning symptoms and burning mouth syndrome-significance of different variables in 150 patients. Med Oral Patol Oral Cir Bucal. 2006;11:E252–5. [PubMed] [Google Scholar]
- 21.Tatullo M, Marrelli M, Scacco S, Lorusso M, Doria S, Sabatini R, et al. Relationship between oxidative stress and “burning mouth syndrome” in female patients: A scientific hypothesis. Eur Rev Med Pharmacol Sci. 2012;16:1218–21. [PubMed] [Google Scholar]
- 22.Tanaka M, Kitago H, Ogawa S, Tokunaga E, Ikeda M, Tomita H. Incidence and treatment of dysgeusia in patients with glossodynia. Acta Otolaryngol Suppl. 2002;546:142–5. doi: 10.1080/00016480260046535. [DOI] [PubMed] [Google Scholar]
- 23.Barker KE, Savage NW. Burning mouth syndrome: An update on recent findings. Aust Dent J. 2005;50:220–3. doi: 10.1111/j.1834-7819.2005.tb00363.x. [DOI] [PubMed] [Google Scholar]
- 24.Gorsky M, Silverman S, Jr, Chinn H. Clinical characteristics and management outcome in the burning mouth syndrome. An open study of 130 patients. Oral Surg Oral Med Oral Pathol. 1991;72:192–5. doi: 10.1016/0030-4220(91)90162-6. [DOI] [PubMed] [Google Scholar]
- 25.Salort-Llorca C, Mínguez-Serra MP, Silvestre FJ. Drug-induced burning mouth syndrome: A new etiological diagnosis. Med Oral Patol Oral Cir Bucal. 2008;13:E167–70. [PubMed] [Google Scholar]
- 26.Speciali JG, Stuginski-Barbosa J. Burning mouth syndrome. Curr Pain Headache Rep. 2008;12:279–84. doi: 10.1007/s11916-008-0047-9. [DOI] [PubMed] [Google Scholar]
- 27.Grushka M, Epstein JB, Gorsky M. Burning mouth syndrome. Am Fam Physician. 2002;65:615–20. [PubMed] [Google Scholar]
- 28.Marino R, Torretta S, Capaccio P, Pignataro L, Spadari F. Different therapeutic strategies for burning mouth syndrome: Preliminary data. J Oral Pathol Med. 2010;39:611–6. doi: 10.1111/j.1600-0714.2010.00922.x. [DOI] [PubMed] [Google Scholar]
- 29.Gary DK, Joel BE, Dana V. Management of burning mouth syndrome. J Can Dent Assoc. 2011;77:151–5. [PubMed] [Google Scholar]
- 30.Grushka M, Ching V, Epstein J. Burning mouth syndrome. Adv Otorhinolaryngol. 2006;63:278–87. doi: 10.1159/000093766. [DOI] [PubMed] [Google Scholar]
- 31.Gremeau-Richard C, Woda A, Navez ML, Attal N, Bouhassira D, Gagnieu MC, et al. Topical clonazepam in stomatodynia: A randomised placebo-controlled study. Pain. 2004;108:51–7. doi: 10.1016/j.pain.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 32.Heckmann SM, Kirchner E, Grushka M, Wichmann MG, Hummel T. A double-blind study on clonazepam in patients with burning mouth syndrome. Laryngoscope. 2012;122:813–6. doi: 10.1002/lary.22490. [DOI] [PubMed] [Google Scholar]
- 33.Epstein JB, Marcoe JH. Topical application of capsaicin for treatment of oral neuropathic pain and trigeminal neuralgia. Oral Surg Oral Med Oral Pathol. 1994;77:135–40. doi: 10.1016/0030-4220(94)90275-5. [DOI] [PubMed] [Google Scholar]
- 34.Volpe A, Lucenti V, Forabosco A, Boselli F, Latessa AM, Pozzo P, et al. Oral discomfort and hormone replacement therapy in the post-menopause. Maturitas. 1991;13:1–5. doi: 10.1016/0378-5122(91)90279-y. [DOI] [PubMed] [Google Scholar]
- 35.Femiano F, Scully C. Burning mouth syndrome (BMS): Double blind controlled study of alpha-lipoic acid (thioctic acid) therapy. J Oral Pathol Med. 2002;31:267–9. doi: 10.1034/j.1600-0714.2002.310503.x. [DOI] [PubMed] [Google Scholar]
- 36.Cavalcanti DR, da Silveira FR. Alpha lipoic acid in burning mouth syndrome – A randomized double-blind placebo-controlled trial. J Oral Pathol Med. 2009;38:254–61. doi: 10.1111/j.1600-0714.2008.00735.x. [DOI] [PubMed] [Google Scholar]
- 37.Bergdahl J, Anneroth G, Perris H. Cognitive therapy in the treatment of patients with resistant burning mouth syndrome: A controlled study. J Oral Pathol Med. 1995;24:213–5. doi: 10.1111/j.1600-0714.1995.tb01169.x. [DOI] [PubMed] [Google Scholar]
- 38.Mock D, Chugh D. Burning mouth syndrome. Int J Oral Sci. 2010;2:1–4. doi: 10.4248/IJOS10008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reamy BV, Derby R, Bunt CW. Common tongue conditions in primary care. Am Fam Physician. 2010;81:627–34. [PubMed] [Google Scholar]


