Abstract
Objectives
The purpose of this study was to explore the independent associations between multiple lifestyle behaviours (physical activity, sleep, screen time (ST) and diet) and overweight and obesity in UK children. The second objective was to compare body mass index (BMI) z-score between children who meet health guidelines for each lifestyle behaviour and those who do not and to explore the impact of interactions between lifestyle behaviours on BMI z-score.
Design, setting and participants
Cross-sectional study on children aged 9–11 years in the UK (n=374).
Outcome measures
Participants were classified as overweight or obese using the WHO BMI cut-points. Moderate-to-vigorous intensity physical activity (MVPA) and sleep duration were measured using an ActiGraph GT3X+ accelerometer, whereas ST and dietary habits were assessed using questionnaires. Multilevel multiple logistic regression was employed to analyse associations between lifestyle behaviours and overweight/obesity. Participants were then categorised according to whether or not they met specific health criteria for MVPA, ST, sleep and diet. Multilevel multiple linear regression was used to compare these groupings on the outcome of BMI z-score and interactions were explored.
Results
MVPA and longer sleep duration were associated with lower odds of overweight or obesity, whereas ST and a healthy diet score were associated with increased odds of overweight/obesity. No association was found for an unhealthy diet score. Meeting MVPA guidelines was significantly associated with a lower BMI z-score in all models, and significant two-way interactions were observed for physical activity and sleep, ST and sleep, and physical activity and diet.
Conclusions
MVPA, sleep and ST are important lifestyle behaviours associated with overweight/obesity among children. More research is required to confirm the role of diet on adiposity and such work would benefit from objective assessment. Overall, this work suggests that strategies aimed at improving compliance with health guidelines are needed.
Trial registration number:
Keywords: Obesity, Child, Overweight, lifestyle, behaviour
Strengths and limitations of this study.
The role of four lifestyle behaviours (physical activity, sleep, screen time and diet) on overweight/obesity has been assessed, thereby adding to the existing literature on adiposity among UK children.
The study is limited by its cross-sectional design and predominantly white British participant group; thus, inferences about the direction of causality cannot be made and the results may not generalise to other ethnic groups.
Although physical activity and a proximal indicator of sleep were measured using accelerometry, self-reported measures were employed to assess screen time and diet, a method that is subject to social desirability and recall bias.
Introduction
Childhood obesity presents a number of immediate and long-term health risks,1 including several adverse physiological2 3 and psychological health consequences.4 Across the world, the prevalence of childhood overweight and obesity is high.5 In England, a third (33.5%) of children aged 10–11 years are classified as overweight or obese.6
Physical activity (PA), sleep, screen time (ST) (eg, TV viewing) and eating habits are four key modifiable lifestyle behaviours that can influence body weight. For example, PA may protect against adiposity among children,7–9 whereas lack of sleep,10–12 TV viewing7 13–16 and the consumption of sugar-sweetened beverages9 17 18 are potential risk factors for obesity. Mixed findings have been reported for other dietary behaviours, particularly for those considered to be ‘healthy’ (eg, fruit and vegetables).18 In a recent UK study, for example, Basterfield et al19 reported no significant dietary influence on overweight or obesity when a ‘healthy’ diet was compared to an ‘unhealthy’ diet, despite participants completing a food diary. Conversely, achieving a sufficient level of moderate-to-vigorous intensity PA (MVPA) was associated with lower odds of overweight/obesity, though this relationship was only present among boys. However, caution was noted in regard to this finding due to the small number of active female participants.19
It is important to explore multiple lifestyle behaviours that influence childhood overweight and obesity so that future interventions and policies can be developed appropriately.20 Yet, research on UK children whereby all four lifestyle behaviours have been examined simultaneously within the same sample of participants is distinctly lacking. For example, neither ST nor sleep duration was assessed in the UK study conducted by Basterfield et al,19 and the majority of research on the role of sleep has been conducted outside of the UK.21 22 A recently published paper from the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE) reported TV viewing, sleep duration and MVPA to be independently associated with obesity.15 Data from the 12 participating countries, including the UK, were presented. Using a similar analytical approach to that of Katzmarzyk et al,15 we sought to examine the effect of lifestyle behaviours on the likelihood of overweight and obesity among UK participants only.
Furthermore, exploring how lifestyle behaviours interact to influence markers of health could aid our understanding of where and how we should try to intervene.23 As such, the second objective was to explore interactive effects of lifestyle behaviours on body mass index (BMI) z-score, by comparing the outcome variable (BMI z-score) between children who achieved government-recommended behavioural standards for health and those who did not.
Methods
Participants
Data were analysed on UK children who participated in the ISCOLE study. A detailed description of the ISCOLE design, methods and power analysis has been provided elsewhere.24 Children aged 9–11 years were the target population24; thus, primary school pupils in Years 5 and 6 were recruited. A cross-sectional study design was employed which involved collecting a series of objective and subjective measures throughout term time. Data were collected across a total of 26 schools within Bath and North East Somerset and West Wiltshire from September 2011 to January 2013. Participants were included in the current study if they were aged between 9 and 11 years and provided complete data for all measures, including covariates. Informed parental consent and child assent were obtained for each participant.
Measures
Anthropometry
A series of anthropometric measurements were obtained from participants using standardised procedures by trained ISCOLE staff.24 BMI, calculated from body mass (kg) divided by height (m2), was used to define obesity. Participants’ body mass was measured using a portable Tanita SC-240 Body Composition Analyser (TANITA Corporation, Tokyo, Japan) and their stature with a Seca 213 Portable Stadiometer (Hamburg, Germany).24 Measures were repeated twice, and the average was calculated for analysis.24 A third measurement for height or weight was performed if the difference between the first two was larger than 0.5 cm or 0.5 kg, respectively, and the average of the closest two measurements was computed.24 Participants’ BMI z-score was derived from the WHO growth reference data,25 and participants were classified as overweight/obese if their score was >+1SD.25 All other participants were categorised as not overweight/obese.
Accelerometry
Participants were asked to wear an ActiGraph GT3X+ accelerometer (ActiGraph, Pensacola, Florida) attached to an elastic belt around their waist.24 They were encouraged to wear it at all times, except during water-based activities, for 1 week. This allowed for daily PA to be recorded, and this protocol has been shown to provide acceptably reliable estimates of most accelerometer-derived metrics.26 Time spent in MVPA was analysed in this study as this intensity of activity directly aligns with the UK PA guidelines27 and because MVPA has been inversely associated with adiposity as opposed to light-intensity activity previously.28 MVPA was determined using the Evenson cut-points (≥574 counts per 15 s),29 which are appropriate and valid for use in children.30 Participants were considered eligible for analysis if they had accelerometry data for at least 4 days, including one weekend day and a minimum of 10 h wear time per day; any period of 0 activity counts lasting at least 20 consecutive minutes was classified as non-wear.31
Accelerometry can also be used to provide a proximal indicator of sleep duration. Using the protocol developed via the ISCOLE study,32 nocturnal sleep duration was quantified using a published automated algorithm.33 Briefly, total sleep duration was estimated using the total minutes from all nocturnal sleep episodes, identified using a combination of the Sadeh algorithm34 and the inclinometer function to determine the probability of sleep for each individual minute.33 Lastly, mean time spent sleeping per night across the week was computed for those with at least three nights of data, including one weekend night. All accelerometry data were managed in SAS (V.9.3).
Self-reported measures
Using 24 h accelerometry data for MVPA, sleep and sedentary time would result in substantial collinearity.35 As there are advantages to having more specific indicators of sedentary time use, particularly in relation to the degree to which such behaviours could be influenced (eg, travel, study time, screen use), we chose to analyse self-reported sedentary behaviour via a questionnaire to reduce the issue of collinearity. We sought to examine the role of overall ST, in terms of both TV viewing and computer use, to capture children's engagement in more than one screen-based behaviour. ISCOLE staff were trained on how to deliver the questionnaire, including how to respond to participant questions in a standardised manner to reduce bias.24 Participants were asked how many hours they had watched TV on a school and weekend day in the last week. They could choose from seven options, coded as: I did not watch TV on school/weekend days (0); <1 h (0.5); 1 h (1); 2 h (2); 3 h (3); 4 h (4); 5 h or more (5). The equivalent was asked for how often they played video/computer games or used a computer that was not for school work, as leisure-time screen use better reflects a lifestyle choice over computer use for school work. These items were taken from the US Youth Risk Behavior Surveillance System,36 which has been deemed as a valid and reliable tool for assessing TV viewing and computer use.37 Overall ST score was computed by summing the TV and computer scores, which were calculated using weighted averages to account for school and weekend ST.
Questions pertaining to participants’ dietary habits were adapted from the Food Frequency Questionnaire (FFQ) for the Health Behaviour in School-Aged Children Study.38 There were 23 items in total, comprising a selection of foods. For each food group, participants responded how often they eat each item in a typical week: never; less than once a week; once a week; 2–4 days a week; 5–6 days a week; once a day, every day; and every day, more than once. This FFQ is considered to have acceptable reliability and validity for assessing food consumption among children aged 9–11 years.39 Using the data from the FFQ, principal components analysis (PCA) was employed to identify dietary patterns among the sample, which has been described elsewhere.40 In this paper, Mikkilä et al40 identified two dietary patterns, which were termed ‘healthy’ and ‘unhealthy’ based on the food groups that loaded onto these two components (eg, vegetables, fruits and berries, etc, and fast foods, ice cream, sugar-sweetened beverages, etc, respectively). Scores were standardised; thus, a higher ‘healthy’ diet score represents a healthier diet, whereas a higher ‘unhealthy’ diet score represents a less healthy diet.
Demographic variables
Information regarding the age and sex of participants was provided by the child's parent or guardian. Data were also obtained from parents/guardians on their highest level of education attained, which was used as an indicator of socioeconomic status (SES). Participants were categorised into one of three groups based on whether their parents/guardians had achieved a low (General Certificate of Secondary Education (GCSE) or less), medium (A Levels or equivalent) or high (university degree) education. Where data were available for both parents with different education levels, the parent with the highest education level was used.
Data handling
To facilitate the testing of our second objective (ie, to compare BMI z-score between children who meet specific health standards for lifestyle behaviours and those who do not), participants were categorised for each behaviour based on the following criteria: ‘active’ children recorded a mean of 60 min MVPA per day;27 ‘long sleepers’ were achieving enough sleep based on specific recommendations for their age group (age 9: ≥10 h; age 10: ≥9.75 h; age 11: ≥9.5 h);41 ‘low ST’ users achieved a mean ST score of ≤2.0 h/day.42 Those not meeting these guidelines were classified as ‘inactive’, ‘short sleepers’ and ‘high ST’ users, respectively. A median split was used to differentiate healthy from unhealthy eaters, along the healthy and unhealthy dietary scores, derived from past work via the use of PCA.40 This resulted in three groups for comparison: children with a healthy diet score above the median and an unhealthy diet score below the median were categorised as having a ‘healthy diet’ (n=100); children below the median for their healthy diet score and above the median for their unhealthy diet score were categorised as having an ‘unhealthy diet’ (n=100) and all other children (ie, those above the median for both a healthy and an unhealthy diet score or vice versa) were classified as displaying a ‘mixed diet’ (n=174). This method has been used previously,19 and as there are numerous guidelines currently in place for different dietary behaviours,43 we chose to adopt the same method for simplicity and comparability.
Statistical analysis
Descriptive statistics were computed and compared between those included and excluded from the analysis, using independent t tests for continuous variables and χ2 tests for categorical data. No significant interactions were found between the behavioural variables and age or sex; thus, results are presented for the total sample. However, due to their potential confounding effects, all analyses were adjusted for age, sex and SES. Relationships between lifestyle behaviours (MVPA, ST, sleep duration, a healthy diet score and an unhealthy diet score) and overweight/obesity were examined using multilevel multiple logistic regression (PROC GLIMMIX), with schools treated as random effects in all models. In model 1, relationships between each behaviour and overweight/obesity were assessed adjusting for potential covariates. In model 2, all four behaviours and covariates were included simultaneously to obtain independent associations between each behaviour and overweight/obesity. For the second objective, BMI z-score was compared between groups (eg, active vs inactive) using multilevel multiple linear regression (PROC MIXED), accounting for potential clustering within schools in all models. Age was centred at the grand mean so that all variables had a meaningful 0. In model 1, simple relationships between the categorical variables and BMI z-score were conducted, adjusting for age, sex and SES. In model 2, all categorical variables and covariates were included to produce a mutually adjusted model. Finally, all six possible two-way interactions between behavioural groups were added and any that were non-significant (p>0.10) were deleted in a stepwise manner, using the backward elimination approach until only significant interactions were left (p<0.05). The sample size of each group for all possible interactions was adequate for statistical analysis (ie, > 5% of the total sample was present in each group), and tests were conducted to check there was no severe multicollinearity.44 45 The least squares means of significant interactions were computed, and post hoc tests using the Bonferroni correction were conducted to identify which groupings were significantly different. Effect sizes of these differences were computed using Hedges’ g. All analyses were conducted using SAS Studio, release V.3.4 (SAS Institute Inc, Cary, North Carolina, 2012–2015).
Results
A total of 1114 consent forms were distributed and 541 participants provided consent, of whom 410 remained following eight withdrawals and excluding those without valid accelerometry data for both PA and sleep. Further excluding participants with missing data for SES resulted in an analytic sample of 374 participants. No significant differences were reported between those included or excluded for any of the exposure or outcome measures. Descriptive statistics for the analytic sample are displayed in table 1. The mean age of participants was 10.9 (±0.4) years, 42.8% of the analytic sample were boys and 28.6% of the analytic sample were classified as overweight/obese. Approximately half of children were classified as meeting the MVPA guidelines, whereas 32.1% and 40.4% of the total sample met the ST and sleep recommendations, respectively. The majority (77.5%) of participants obtained 7 valid days of accelerometer data, while 1.6%, 4.3% and 16.6% obtained 4, 5 and 6 valid days of data, respectively.
Table 1.
Descriptive characteristics of the analytic sample (n=374)
| Mean (SD) |
|||
|---|---|---|---|
| Continuous variables | Total sample | Boys | Girls |
| Age (years) | 10.9 (0.4) | 10.9 (0.4) | 10.9 (0.5) |
| Body height (cm) | 145.2 (7.2) | 144.5 (6.5) | 145.7 (7.6) |
| Body mass (kg) | 39.2 (8.6) | 37.9 (7.2) | 40.2 (9.4) |
| BMI z-score | 0.4 (1.1) | 0.4 (1.0) | 0.4 (1.1) |
| Sedentary time (min/day) | 500.8 (55.9) | 500.4 (56.7) | 501.0 (55.5) |
| Light intensity activity (min/day) | 288.1 (45.3) | 287.3 (43.8) | 288.6 (46.5) |
| MVPA (min/day) | 64.4 (22.7) | 73.9 (24.9) | 57.3 (17.9) |
| Sleep duration (min/night) | 568.3 (43.4) | 561.3 (42.4) | 573.6 (43.4) |
| Screen time score | 3.0 (1.7) | 3.3 (2.0) | 2.7 (1.4) |
| Healthy diet score | 0.04 (0.99) | 0.06 (0.97) | 0.02 (1.01) |
| Unhealthy diet score | −0.01 (0.99) | 0.12 (1.14) | −0.11 (0.84) |
| Accelerometer wake/wear time (min/day) | 853.2 (45.0) | 861.7 (44.2) | 846.9 (44.7) |
| Categorical variables* | N (%) | ||
| Sex | – | 160 (42.8) | 214 (57.2) |
| BMI status (% overweight/obese) | 107 (28.6) | 41 (25.6) | 66 (30.8) |
| Physical activity (% active) | 195 (52.1) | 111 (69.4) | 84 (39.3) |
| Screen time (% low ST) | 120 (32.1) | 44 (27.5) | 76 (35.5) |
| Sleep (% long sleep) | 151 (40.4) | 52 (32.5) | 99 (46.3) |
| Diet | |||
| Healthy | 100 (26.7) | 41 (25.6) | 59 (27.6) |
| Mixed | 174 (46.5) | 75 (46.9) | 99 (46.3) |
| Unhealthy | 100 (26.7) | 44 (27.5) | 56 (26.2) |
| SES (parental education level) | |||
| Low | 105 (28.1) | 38 (23.8) | 67 (31.3) |
| Medium | 94 (25.1) | 41 (25.6) | 53 (24.8) |
| High | 175 (46.8) | 81 (50.6) | 94 (43.9) |
*Categories based on children meeting specific criteria: overweight/obese: BMI SD > +1.0; active: ≥60 min MVPA; low ST: ≤ 2.0 h ST/day; long sleep: ≥ 10.0, 9.75 and 9.5 h sleep/night for children aged 9, 10 and 11 years, respectively. Diet: healthy: > median for healthy diet score and < median for unhealthy diet score; unhealthy: < median for healthy diet score and > median for unhealthy diet score; mixed: all other participants. SES: low: GCSEs/equivalent or less; medium: A levels/equivalent; high: university degree.
BMI, body mass index; GCSE, General Certificate of Secondary Education; MVPA, moderate-to-vigorous intensity physical activity; SES, socioeconomic status; ST, screen time.
The intraclass correlation revealed that approximately 2% of the variability in overweight/obesity and 3% for BMI z-score were accounted for by the school-level effect; thus, 97–98% of the variability was accounted for by individual-level factors.
Lifestyle behaviours and overweight/obesity
ORs for each lifestyle behaviour (measured as continuous variables) and overweight/obesity are displayed in table 2.i Higher MVPA and sleep duration were associated with lower odds of overweight or obesity in model 1, adjusting for potential covariates (age, sex and SES). Conversely, a higher ST was associated with higher odds of overweight/obesity. No significant relationship was observed for either dietary score. Results from model 2, in which all lifestyle behaviours were entered simultaneously, were similar in that MVPA, sleep duration and ST were independently associated with overweight/obesity. Additionally, a higher healthy diet score was independently associated with increased odds of being overweight or obese. No significant relationship was found for an unhealthy diet score.
Table 2.
Odds associated with being overweight/obese in relation to multiple lifestyle behaviours: ORs* and 95% CIs
| Model 1† | Model 2‡ | |
|---|---|---|
| MVPA (min/day) | 0.74 (0.56 to 0.97) | 0.69 (0.52 to 0.92) |
| p Value | 0.027 | 0.011 |
| Sleep duration (min/night) | 0.66 (0.52 to 0.85) | 0.65 (0.51 to 0.83) |
| p Value | 0.001 | 0.001 |
| Screen time score | 1.48 (1.13 to 1.94) | 1.50 (1.11 to 2.03) |
| p Value | 0.005 | 0.008 |
| Healthy diet score | 1.24 (0.98 to 1.59) | 1.34 (1.04 to 1.73) |
| p Value | 0.079 | 0.024 |
| Unhealthy diet score | 1.16 (0.92 to 1.46) | 1.01 (0.78 to 1.30) |
| p Value | 0.219 | 0.971 |
Italic font indicates significant results.
*ORs are expressed per SD increase in each variable (MVPA=23, sleep duration=43; screen time=2; healthy diet score=1; unhealthy diet score=1).
†Model 1: Adjusting for age, sex and SES (parental education level) with schools treated as random effects.
‡Model 2: All independent variables entered simultaneously in a mutually adjusted model, with covariates. Schools were treated as random effects.
p Values are from Type 3 Tests of Fixed Effects.
MVPA, moderate-to-vigorous intensity physical activity; SES, socioeconomic status.
Lifestyle behaviours and BMI z-score
PA, ST and sleep duration were significantly associated with BMI z-score in models 1 and 2 (table 3). Participants who were sufficiently active had a mean BMI z-score that was 0.42 units lower than those not meeting the MVPA guidelines. Participants meeting the recommended ST and sleep guidelines had a mean BMI z-score approximately 0.30 units lower than those who were not. No significant relationship was found for either dietary variable. Although superseded by interaction effects, PA remained a significant correlate of BMI z-score in all models. Significant interactions were found between PA and sleep, ST and sleep, and PA and diet. These interactions are presented graphically in figure 1.
Table 3.
Summary of results describing the relationships between BMI z-score and lifestyle behaviours, for different activity, screen time, sleep levels and dietary groups: β coefficients and 95% CIs
| Model 1* | Model 2† | Model 3‡ | |
|---|---|---|---|
| Physical activity§ | |||
| Active | −0.42 (−0.65 to −0.20) | −0.42 (−0.65 to −0.20) | −1.08 (−1.55 to −0.62) |
| p Value | <0.001 | <0.001 | <0.001 |
| Screen time§ | |||
| Low ST | −0.30 (−0.53 to −0.07) | −0.29 (−0.52 to −0.06) | −0.56 (−0.85 to −0.27) |
| p Value | 0.012 | 0.014 | 0.050 |
| Sleep duration§ | |||
| Long sleep | −0.28 (−0.50 to −0.05) | −0.30 (−0.51 to −0.08) | −0.70 (−1.03 to −0.37) |
| p Value | 0.015 | 0.008 | 0.193 |
| Diet§ | |||
| Mixed diet | 0.15 (−0.11 to 0.42) | 0.10 (−0.16 to 0.36) | −0.29 (−0.66 to 0.07) |
| Healthy diet | 0.05 (−0.26 to 0.36) | 0.11 (−0.20 to 0.42) | −0.20 (−0.63 to 0.24) |
| p Value | 0.489 | 0.707 | 0.823 |
| Physical activity×sleep¶ | |||
| Active, long sleep | 0.44 (0.01 to 0.87) | ||
| p Value | 0.044 | ||
| Screen time×sleep¶ | |||
| Low ST, long sleep | 0.66 (0.21 to 1.11) | ||
| p Value | 0.004 | ||
| Physical activity×diet¶ | |||
| Active, mixed diet | 0.74 (0.24 to 1.25) | ||
| Active, healthy diet | 0.53 (−0.04 to 1.10) | ||
| p Value | 0.016 | ||
Italic font indicates significant results.
*Model 1: Adjusted for age, sex and SES (parental education level), and schools are treated as random effects.
†Model 2: Mutually adjusted model with all covariates and independent variables entered simultaneously, with schools treated as random effects.
‡Model 3=Model 2 + significant interactions.
§Reference categories were inactive, high ST, short sleep and unhealthy diet, respectively.
¶Estimates refer to the specified groups. All other possible group combinations act as the referent group.
p Values are from Type 3 Tests of Fixed Effects.
BMI, body mass index; ST, screen time; SES, socioeconomic status.
Figure 1.
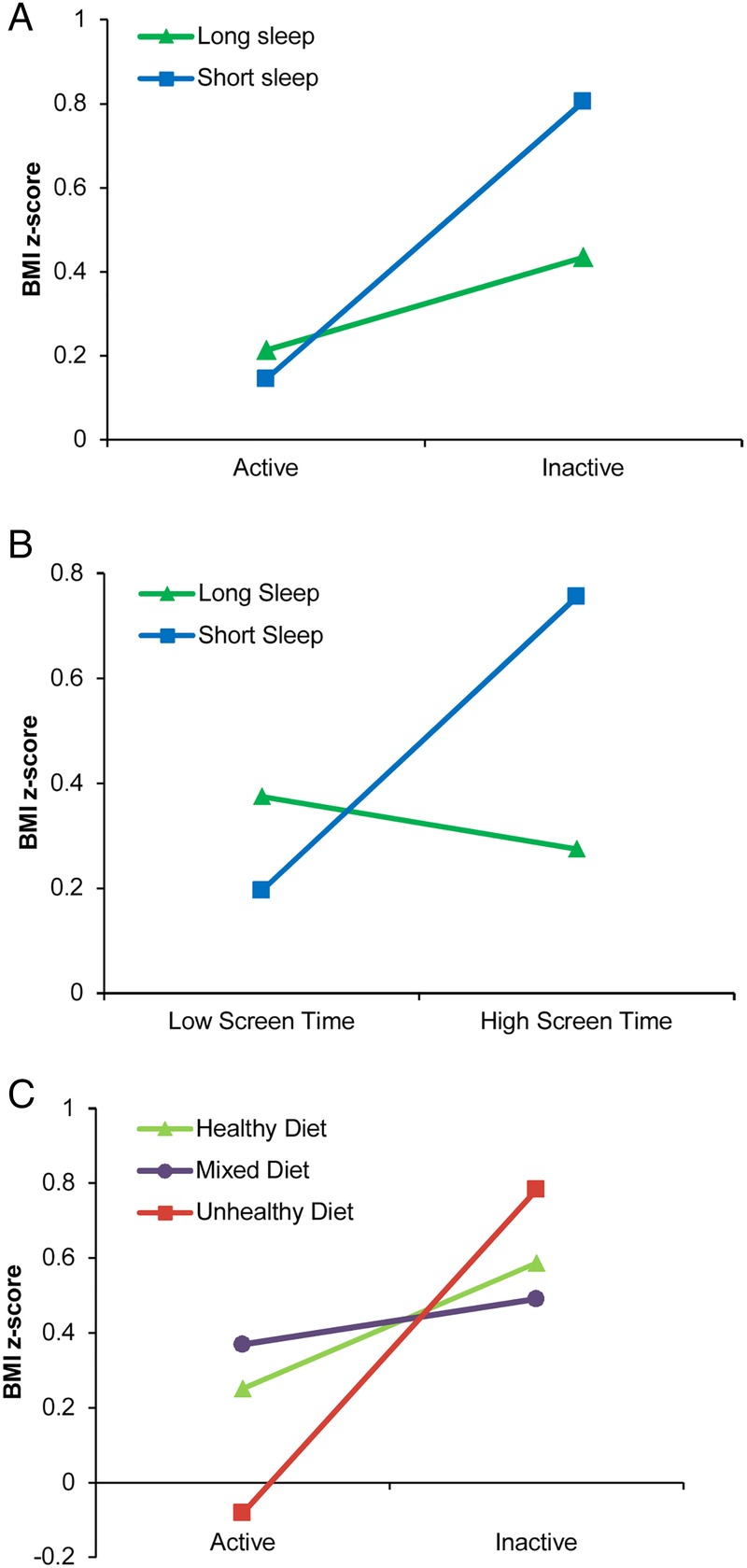
Significant interactions among behavioural groups and BMI z-score. (A) PA×sleep interaction. (B) ST×sleep interaction. (C) PA×diet interaction. BMI, body mass index; PA, physical activity; ST, screen time.
Post hoc analyses revealed that participants who did not meet either the PA or sleep guidelines had a significantly higher BMI z-score than those who were classified as active, whether they were long (p=0.003, g=0.66) or short (p<0.0001, g=0.55) sleepers (figure 1A).
As shown in figure 1B, there was a differential effect of sleep duration for those in the high ST group, with long sleepers displaying a significantly lower BMI z-score than short sleepers (p=0.002, g=0.48). For children with a short sleep duration, those in the low ST group had a significantly lower BMI z-score than high ST participants (p=0.001, g=0.58). Active children with an unhealthy diet had a significantly lower BMI z-score than inactive children for all dietary groups (healthy: p=0.031, g=0.47; mixed: p=0.022, g=0.46; unhealthy: p=0.001, g=0.72; figure 1C), whereas there was no significant difference in BMI z-score between active and inactive children with mixed or healthy diets.
Discussion
The first aim of this study was to explore the relationships between multiple lifestyle behaviours and overweight/obesity among a sample of UK children. Our results show MVPA, sleep duration, ST and a healthy diet to be independently associated with overweight and obesity. With the exception of a healthy diet score, all relationships were in expected directions, and these findings are similar to those reported across the 12-country ISCOLE sites, in which only obesity status was analysed.15 A secondary aim was to explore the impact of meeting behavioural guidelines on BMI z-score; meeting guidelines for PA, sleep and ST was significantly associated with a lower BMI z-score and three significant interactions (PA×sleep; ST×sleep; PA×diet) were observed.
Our results for PA are consistent with findings from past UK research, which has shown that higher levels of PA are associated with favourable adiposity levels across different age groups.19 28 49 50 Not only is PA of at least a moderate intensity and above likely to provide benefit,49 50 but meeting the MVPA guidelines has also been shown in past work to reduce the likelihood of overweight and obesity.19 28
Few studies have explored the role of sleep on adiposity among UK children, but the available evidence from a study on 7-year olds,13 and another on adolescents,14 is consistent with our findings of an association between short sleep duration and overweight/obesity. This could be a result of metabolic changes associated with an increase in appetite and subsequently energy intake, which may occur with reduced sleep.51 Many existing studies have relied on self-reported measures for quantifying sleep11–14; thus, our study adds to the existing literature in this area as accelerometers provide a promising indicator of sleep duration, though further research on other samples of UK children is required.
ST, encompassing both TV viewing and computer use, was positively associated with overweight/obesity. Such a finding is consistent with data from adolescents that show multiple screen-based behaviours (computer use, TV viewing and video games) to be associated with BMI z-score.14 In a study using data from the Health Survey for England,52 TV viewing was associated with obesity. In contrast, objectively measured sedentary time and other forms of self-reported leisure-based sitting were not, though their assessment of ‘non-TV sitting’ consisted of both screen-based and non-screen-based pursuits (eg, homework, drawing, computer use and video games).52 TV viewing in particular may be a risk factor for adiposity because children are more likely to consume energy-rich foods while watching TV53 54 and to be exposed to food advertising.18 However, children are now likely to be exposed to food advertisements via the internet on computers and mobile phone applications,55 and engaging in screen-based pursuits, particularly before bedtime, may disrupt children's sleep,56 which could contribute to unfavourable adiposity levels.14 55 As such, it may be insufficient to target TV viewing alone and future research on other technologies, and the possible mechanisms behind their influence with adiposity is warranted.
In addition to movement behaviours, we assessed the role of dietary behaviours on overweight/obesity. Our results were unexpected in that a healthy diet score was associated with an increased risk of overweight/obesity, whereas no such relationship was found for an unhealthy diet score. Similar findings have been reported. For example, less-frequent consumption of energy-rich foods was associated with a larger waist circumference in Swedish children aged 9–11 years,16 and among boys aged 5–11 years in Scotland, obese participants ate less ‘snacks’ than healthy weight children.57 One reason for these findings is that overweight children may be eating more healthy food types, or reducing their intake of unhealthy foods in an attempt to lose weight.16 19 Alternatively, overweight children may be more likely to exaggerate their intake of healthy foods and/or under-report their consumption of unhealthy foods. Dietary intake is a complex behaviour, and considering the potential bias which can arise from self-reported methods, direct measures of energy intake might prove useful to clarify such findings in future research.
Past work exploring the effects of meeting health behaviour guidelines shows some contrasting results to those reported in our work. For example, no significant association was found for ST group and adiposity in a UK study of children aged 9–10 years,28 nor was there a relationship reported for sleep (≥ 8 h/night) among adolescents in Spain58 and the USA.59 These differences could in part be explained by methodological differences; the proportion of participants meeting ST guidelines was substantially higher in the UK study than in our sample and different cut-off points were used to classify adequate sleep in the US and Spanish studies. Nevertheless, meeting the PA guidelines was significantly associated with favourable adiposity in all three studies, including our own.
Despite differences in the way that health behaviours have been categorised across studies, it would seem that the more risk factors an individual has (ie, the more guidelines a child does not meet), the higher the risk of adiposity.28 58 59 This corresponds with our results, as both interactions for PA×sleep and ST×sleep revealed a similar pattern in that participants who did not meet the guidelines for either behaviour had the highest BMI z-score.
Our results showed that active children classified as having an ‘unhealthy’ diet overall (ie, a higher consumption of unhealthy foods and a lower intake of healthy foods) had a significantly lower BMI z-score than their inactive counterparts, and the size of these effects ranged from moderate to large. Ottevaere et al60 previously concluded that physically active children do not necessarily consume healthier diets compared with inactive children, which supports our findings. However, our results should be taken with caution given that diet was self-reported and the direction of causality cannot be inferred. Longitudinal studies would enable researchers to determine the direction of effect and the interplay among such lifestyle behaviours, while qualitative data would provide a deeper understanding of children's and parents’ perceptions regarding these two behaviours and their importance in relation to their weight. Nonetheless, lean children who are getting their calorie requirements from unhealthy food types may not be consuming important nutrients necessary for optimal health in accordance with dietary recommendations.43 As such, parents with lean active children would do well to ensure that their children eat a healthy diet, especially since consuming a poor diet is known to have other negative health implications.61
This study adds to the existing literature on overweight and obesity among UK children by exploring the role of all four modifiable lifestyle behaviours and via the use of accelerometry-derived MVPA and sleep, for which data among UK children are limited. However, accelerometers can only provide a proxy measure of sleep duration and there are other limitations which should be noted. First, causality cannot be inferred due to the cross-sectional nature of the study design. Second, almost 90% of the analytic sample were white British, and data were collected from the South West of the UK. As such, the results may not generalise to other ethnic groups or to children living in other regions of the UK. Third, biological age/maturity was not controlled for in the current study, though the majority of participants were likely to be prepubertal. Although every attempt was made to minimise bias, the self-reported measures used in our study are subject to recall and social desirability bias, which may have influenced the results. In particular, the results for diet should be treated with caution because of the difficulties that are imposed when measuring this behaviour.18 Future research may benefit from using objective measures of dietary intake alongside the objective assessment of other lifestyle behaviours, and given that only TV viewing and computer use were assessed, the role of other screen-based pursuits should also be explored in future work. In addition, it was beyond the scope of the current study to examine the role of lifestyle behaviours across school and weekend days separately.
In conclusion, we have shown that sleep, ST and PA are important behaviours associated with adiposity. Interventions and future research should consider the correlates of overweight and obesity from a multifactorial perspective, taking into account the role of multiple lifestyle behaviours. Further research is needed to confirm our findings for dietary behaviour and sleep duration among a broader sample of UK children in addition to the role of other screen-based pursuits. Our findings confirm the importance of children meeting recommended behavioural guidelines; thus, interventions which aim to improve awareness of and compliance with these recommendations are needed.
Acknowledgments
The authors thank Lydia Emm, MSc; Julia Zakrzewski, PhD; Clemens Drenowatz, PhD; Oliver Perkins for their role in data collection for the UK site of ISCOLE, and the Coordinating Center of ISCOLE in Baton Rouge, Louisiana, particularly Denise Lambert. They also thank Stephanie Broyles, Emily Mire and Kara Dentro for their advice on the analytical component of this manuscript. The authors also thank the study participants along with their parents, teachers and head teachers for their involvement in the study. They also thank the broader ISCOLE group and the External Advisory Board for the ISCOLE project which includes Alan Batterham, PhD, Teesside University; Jacqueline Kerr, PhD, University of California, San Diego; Michael Pratt, MD, Centers for Disease Control and Prevention; Angelo Pietrobelli, MD, Verona University Medical School.
Footnotes
Contributors: PTK and Dr Timothy Church conceived and realised the overall ISCOLE study. HJW and MS conceived the basis for this paper. HJW led the analyses. HJW drafted the manuscript with input from MS. All authors provided critical edits and contributions to the paper. All authors approve the submission.
Funding: ISCOLE was funded by The Coca-Cola Company. The funder had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: University of Bath Research Ethics Approval Committee for Health (reference number EP 10/11 137, approved 13/07/11).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
This analysis was repeated using the Treuth46 MVPA cut-points and IOTF47 and CDC48 criteria for overweight/obesity, as a sensitivity analysis (data not shown). The same associations were found using the Treuth MVPA cut-points. Only MVPA and sleep duration remained significant using the CDC and IOTF criteria for overweight/obesity, though a lower proportion of participants were classified as overweight or obese using these cut-points (CDC: 20.1% and IOTF: 19.3%).
References
- 1.Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry 2012;24:176–88. 10.3109/09540261.2012.688195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Juonala M, Magnussen CG, Berenson GS et al. . Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1876–85. 10.1056/NEJMoa1010112 [DOI] [PubMed] [Google Scholar]
- 3.Falaschetti E, Hingorani AD, Jones A et al. . Adiposity and cardiovascular risk factors in a large contemporary population of pre-pubertal children. Eur Heart J 2010;31:3063–72. 10.1093/eurheartj/ehq355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Griffiths LJ, Parsons TJ, Hill AJ. Self-esteem and quality of life in obese children and adolescents: a systematic review. Int J Pediatr Obes 2010;5:282–304. 10.3109/17477160903473697 [DOI] [PubMed] [Google Scholar]
- 5.Ng M, Fleming T, Robinson M et al. . Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lifestyle statistics team. National child measurement programme: England, 2013/14 school year. The Health and Social Care Information Centre, 2014. http://www.hscic.gov.uk/catalogue/PUB16070/nati-chil-meas-prog-eng-2013-2014-rep.pdf (accessed 23 Nov 2015). [Google Scholar]
- 7.te Velde SJ, van Nassau F, Uijtdewilligen L et al. . Energy balance-related behaviours associated with overweight and obesity in preschool children: a systematic review of prospective studies. Obes Rev 2012;13(Suppl 1):56–74. 10.1111/j.1467-789X.2011.00960.x [DOI] [PubMed] [Google Scholar]
- 8.Owen CG, Nightingale CM, Rudnicka AR et al. . Physical activity, obesity and cardiometabolic risk factors in 9- to 10-year-old UK children of White European, South Asian and black African-Caribbean origin: the Child Heart And health Study in England (CHASE). Diabetologia 2010;53:1620–30. 10.1007/s00125-010-1781-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ochoa MC, Moreno-Aliaga MJ, Martínez-González MA et al. . Predictor factors for childhood obesity in a Spanish case-control study. Nutrition 2007;23:379–84. 10.1016/j.nut.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 10.Chaput JP, Lambert M, Gray-Donald K et al. . Short sleep duration is independently associated with overweight and obesity in Quebec children. Can J Public Health 2011;102:369–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Jong E, Stocks T, Visscher TLS et al. . Association between sleep duration and overweight: the importance of parenting. Int J Obes (Lond) 2012;36:1278–84. 10.1038/ijo.2012.119 [DOI] [PubMed] [Google Scholar]
- 12.Garaulet M, Ortega FB, Ruiz JR et al. . Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes (Lond) 2011;35:1308–17. 10.1038/ijo.2011.149 [DOI] [PubMed] [Google Scholar]
- 13.Reilly JJ, Armstrong J, Dorosty AR et al. . Early life risk factors for obesity in childhood: cohort study. BMJ 2005;330:1357–9. 10.1136/bmj.38470.670903.E0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arora T, Hussain S, Hubert Lam KB et al. . Exploring the complex pathways among specific types of technology, self-reported sleep duration and body mass index in UK adolescents. Int J Obes (Lond) 2013;37:1254–60. 10.1038/ijo.2012.209 [DOI] [PubMed] [Google Scholar]
- 15.Katzmarzyk PT, Barreira TV, Broyles ST et al. . Relationship between lifestyle behaviors and obesity in children ages 9–11: results from a 12-country study. Obesity (Silver Spring) 2015;23:1696–702. 10.1002/oby.21152 [DOI] [PubMed] [Google Scholar]
- 16.Lehto R, Ray C, Lahti-Koski M et al. . Health behaviors, waist circumference and waist-to-height ratio in children. Eur J Clin Nutr 2011;65:841–8. 10.1038/ejcn.2011.49 [DOI] [PubMed] [Google Scholar]
- 17.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006;84:274–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Must A, Barish EE, Bandini LG. Modifiable risk factors in relation to changes in BMI and fatness: what have we learned from prospective studies of school-aged children? Int J Obes (Lond) 2009;33:705–15. 10.1038/ijo.2009.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Basterfield L, Jones AR, Parkinson KN et al. . Physical activity, diet and BMI in children aged 6–8 years: a cross-sectional analysis. BMJ Open 2014;4:e005001. 10.1136/bmjopen-2014-005001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wofford LG. Systematic review of childhood obesity prevention. J Pediatr Nurs 2008;23:5–19. 10.1016/j.pedn.2007.07.006 [DOI] [PubMed] [Google Scholar]
- 21.Cappuccio FP, Taggart FM, Kandala NB et al. . Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008;31:619–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 2008;16:265–74. 10.1038/oby.2007.63 [DOI] [PubMed] [Google Scholar]
- 23.Spruijt-Metz D. Etiology, treatment, and prevention of obesity in childhood and adolescence: a decade in review. J Res Adolesc 2011;21:129–52. 10.1111/j.1532-7795.2010.00719.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katzmarzyk PT, Barreira TV, Broyles ST et al. . The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): design and methods. BMC Public Health 2013;13:900 10.1186/1471-2458-13-900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Onis M, Onyango AW, Borghi E et al. . Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660–7. 10.2471/BLT.07.043497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barreira TV, Schuna JM, Tudor-Locke C et al. . Reliability of accelerometer-determined physical activity and sedentary behavior in school-aged children: a 12-country study. Int J Obes Suppl 2015;5(Suppl 2):S29–35. 10.1038/ijosup.2015.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Department of Health. Start active, stay active: a report on physical activity for health from the four home countries’ Chief Medical Officers. London: Department of Health, 2011. http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216370/dh_128210.pdf (accessed 23 Nov 2015). [Google Scholar]
- 28.Steele RM, van Sluijs EM, Cassidy A et al. . Targeting sedentary time or moderate- and vigorous-intensity activity: independent relations with adiposity in a population-based sample of 10-y-old British children. Am J Clin Nutr 2009;90:1185–92. 10.3945/ajcn.2009.28153 [DOI] [PubMed] [Google Scholar]
- 29.Evenson KR, Catellier DJ, Gill K et al. . Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557–65. 10.1080/02640410802334196 [DOI] [PubMed] [Google Scholar]
- 30.Trost SG, Loprinzi PD, Moore R et al. . Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 2011;43:1360–8. 10.1249/MSS.0b013e318206476e [DOI] [PubMed] [Google Scholar]
- 31.Tudor-Locke C, Barreira TV, Schuna JM et al. . Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE). Int J Behav Nutr Phys Act 2015;12:11 10.1186/s12966-015-0172-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tudor-Locke C, Barreira TV, Schuna JM et al. . Unique contributions of ISCOLE to the advancement of accelerometry in large studies. Int J Obes Suppl 2015;5(Suppl 2):S53–S8. 10.1038/ijosup.2015.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barreira TV, Schuna JM, Mire EF et al. . Identifying children's nocturnal sleep using 24-h waist accelerometry. Med Sci Sports Exerc 2015;47:937–43. 10.1249/MSS.0000000000000486 [DOI] [PubMed] [Google Scholar]
- 34.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep 1994;17:201–7. [DOI] [PubMed] [Google Scholar]
- 35.Pedišić Ž. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research—the focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiology 2014;46:135–46. [Google Scholar]
- 36.U.S. Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System (YRBSS). http://www.cdc.gov/yrbs (accessed 23 Nov 2015).
- 37.Schmitz KH, Harnack L, Fulton JE et al. . Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. J Sch Health 2004;74:370–7. 10.1111/j.1746-1561.2004.tb06632.x [DOI] [PubMed] [Google Scholar]
- 38.Currie C, Gabhainn SN, Godeau E et al. . Inequalities in young people's health. HBSC international report from the 2005/2006 survey. WHO Regional Office for Europe, 2008. http://www.euro.who.int/__data/assets/pdf_file/0005/53852/E91416.pdf?ua=1 (accessed 23 Nov 2015). [Google Scholar]
- 39.Saloheimo T, González SA, Erkkola M et al. . The reliability and validity of a short food frequency questionnaire among 9–11-year olds: a multinational study on three middle-income and high-income countries. Int J Obes Suppl 2015;5(Suppl 2):S22–8. 10.1038/ijosup.2015.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mikkilä V, Vepsäläinen H, Saloheimo T et al. . An international comparison of dietary patterns in 9–11-year-old children. Int J Obes Suppl 2015;5(Suppl 2):S17–21. 10.1038/ijosup.2015.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.NHS Choices. How much sleep do kids need? 2015. http://www.nhs.uk/Livewell/Childrenssleep/Pages/howmuchsleep.aspx (accessed 23 Nov 2015).
- 42.Canadian Society for Exercise Physiology. Canadian Sedentary Behaviour Guidelines for Children 5–11 years. http://www.csep.ca (accessed 23 Nov 2015).
- 43.NHS Choices. The eatwell plate 2015. http://www.nhs.uk/Livewell/Goodfood/Pages/eatwell-plate.aspx (accessed 23 Nov 2015).
- 44.Cohen J, Cohen P, West SG et al. . Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 3rd edn Mahwah, NJ: Lawrence Erlbaum Associates, 2003. [Google Scholar]
- 45.Hutcheson GD, Sofroniou N. The Multivariate Social Scientist: Introductory Statistics Using Generalized Linear Models. London: Sage, 1999. [Google Scholar]
- 46.Treuth MS, Schmitz K, Catellier DJ et al. . Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc 2004;36:1259–66. [PMC free article] [PubMed] [Google Scholar]
- 47.Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 2012;7:284–94. 10.1111/j.2047-6310.2012.00064.x [DOI] [PubMed] [Google Scholar]
- 48.Kuczmarski RJ, Ogden CL, Guo SS et al. . 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11 2002;246:1–190. [PubMed] [Google Scholar]
- 49.Basterfield L, Pearce MS, Adamson AJ et al. . Physical activity, sedentary behavior, and adiposity in English children. Am J Prev Med 2012;42:445–51. 10.1016/j.amepre.2012.01.007 [DOI] [PubMed] [Google Scholar]
- 50.Riddoch CJ, Leary SD, Ness AR et al. . Prospective associations between objective measures of physical activity and fat mass in 12–14 year old children: the Avon Longitudinal Study of Parents and Children (ALSPAC). BMJ 2009;339:b4544 10.1136/bmj.b4544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Knutson KL, Spiegel K, Penev P et al. . The metabolic consequences of sleep deprivation. Sleep Med Rev 2007;11:163–78. 10.1016/j.smrv.2007.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coombs NA, Stamatakis E. Associations between objectively assessed and questionnaire-based sedentary behaviour with BMI-defined obesity among general population children and adolescents living in England. BMJ Open 2015;5:e007172 10.1136/bmjopen-2014-007172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pearson N, Biddle SJH. Sedentary behavior and dietary intake in children, adolescents, and adults. A systematic review. Am J Prev Med 2011;41:178–88. 10.1016/j.amepre.2011.05.002 [DOI] [PubMed] [Google Scholar]
- 54.Chaput JP, Klingenberg L, Astrup A et al. . Modern sedentary activities promote overconsumption of food in our current obesogenic environment. Obes Rev 2011;12:e12–20. 10.1111/j.1467-789X.2010.00772.x [DOI] [PubMed] [Google Scholar]
- 55.Arora T, Hosseini-Araghi M, Bishop J et al. . The complexity of obesity in UK adolescents: relationships with quantity and type of technology, sleep duration and quality, academic performance and aspiration. Pediatr Obes 2013;8:358–66. 10.1111/j.2047-6310.2012.00119.x [DOI] [PubMed] [Google Scholar]
- 56.Ogunleye AA, Voss C, Sandercock GR. Delayed bedtime due to screen time in schoolchildren: importance of area deprivation. Pediatr Int 2015;57:137–42. 10.1111/ped.12447 [DOI] [PubMed] [Google Scholar]
- 57.Craig LCA, McNeill G, Macdiarmid JI et al. . Dietary patterns of school-age children in Scotland: association with socio-economic indicators, physical activity and obesity. Br J Nutr 2010;103:319–34. 10.1017/S0007114509991942 [DOI] [PubMed] [Google Scholar]
- 58.Martinez-Gomez D, Moreno LA, Romeo J et al. . Combined influence of lifestyle risk factors on body fat in Spanish adolescents—the AVENA study. Obes Facts 2011;4:105–11. 10.1159/000327686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Laurson KR, Lee JA, Eisenmann JC. The cumulative impact of physical activity, sleep duration, and television time on adolescent obesity: 2011 Youth Risk Behavior Survey. J Phys Act Health 2015;12:355–60. 10.1123/jpah.2013-0402 [DOI] [PubMed] [Google Scholar]
- 60.Ottevaere C, Huybrechts I, Béghin L et al. . Relationship between self-reported dietary intake and physical activity levels among adolescents: The HELENA study. Int J Behav Nutr Phys Act 2011;8:8 10.1186/1479-5868-8-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.2010 US Dietary Guidelines Advisory Committee. Report of the dietary guidelines advisory committee on the dietary guidelines for Americans, 2010. Washington DC: USDA Department of Agriculture, US Department of Health and Human Services, 2010. http://www.nutriwatch.org/05Guidelines/dga_advisory_2010.pdf (accessed 23 Nov 2015). [Google Scholar]


