Abstract
Neuroactive steroids are endogenous neuromodulators synthesised in the brain that rapidly alter neuronal excitability by binding to membrane receptors, in addition to the regulation of gene expression via intracellular steroid receptors. Neuroactive steroids induce potent anxiolytic, antidepressant, anticonvulsant, sedative, analgesic and amnesic effects, mainly through interaction with the γ-amino-butyric type A (GABAA) receptor. They also exert neuroprotective, neurotrophic and antiapoptotic effects in several animal models of neurodegenerative diseases.
Neuroactive steroids regulate many physiological functions such as stress response, puberty, ovarian cycle, pregnancy and reward. Their levels are altered in several neuropsychiatric and neurologic diseases and both preclinical and clinical studies emphasise a therapeutic potential of neuroactive steroids for these diseases, whereby symptomatology ameliorates upon restoration of neuroactive steroid concentrations. However, direct administration of neuroactive steroids has several challenges, including pharmacokinetics, low bioavailability, addiction potential, safety and tolerability that limit its therapeutic use. Therefore, modulation of neurosteroidogenesis to restore the altered endogenous neuroactive steroid tone may represent a better therapeutic approach.
This review summarizes recent approaches that target the neuroactive steroid biosynthetic pathway at different levels in order to promote neurosteroidogenesis. These include modulation of neurosteroidogenesis through ligands of the translocator protein 18 kDa (TSPO), and the pregnane xenobiotic receptor (PXR), as well as targeting of specific neurosteroidogenic enzymes like 17β-hydroxysteroid dehydrogenase type 10 (17β-HSD10) or P450 side chain cleavage (P450scc). Enhanced neurosteroidogenesis through these targets may be beneficial for neurodegenerative diseases such as Alzheimer's disease and age-related dementia, but also for neuropsychiatric diseases, including alcohol use disorders.
Keywords: neuroactive steroids; 3α,5α-THP (allopregnanolone); translocator protein 18 kDa (TSPO); pregnane xenobiotic receptor (PXR); 17β-hydroxysteroid dehydrogenase type 10 (17β-HSD10); P450 side chain cleavage (P450scc); Alzheimer's disease; alcoholism
Introduction
Neuroactive steroids are endogenous neuromodulators that rapidly alter neuronal excitability by binding to membrane receptors (1). They can be synthesized in the brain de novo from cholesterol, in which case they have been termed neurosteroids (2), or can reach the brain from peripheral steroidogenic organs such as adrenals and gonads, and are locally metabolized (i.e. aromatization of testosterone into estradiol) (3). The synthesis of neuroactive steroids requires the translocation of cholesterol across the mitochondrial membrane, which occurs through a molecular complex formed by the translocator protein 18 kDa (TSPO), the steroidogenic acute regulatory protein (StAR), the voltage-dependent anion channel protein (VDAC), and the adenine nucleotide transporter protein (ANT). In the mitochondria, cholesterol is converted to pregnenolone by the P450 side-chain cleavage enzyme (P450scc); pregnenolone diffuses into the cytosol where it is further metabolized into different neuroactive steroids, as shown in Figure 1. Although TSPO, the rate-limiting step in neuroactive steroid synthesis, is highly expressed in microglia and astrocytes, but less abundant in neurons, neurosteroidogenesis occurs primarily in principal neurons of several brain areas that possess the necessary enzymatic machinery to convert cholesterol into neuroactive steroids (4).
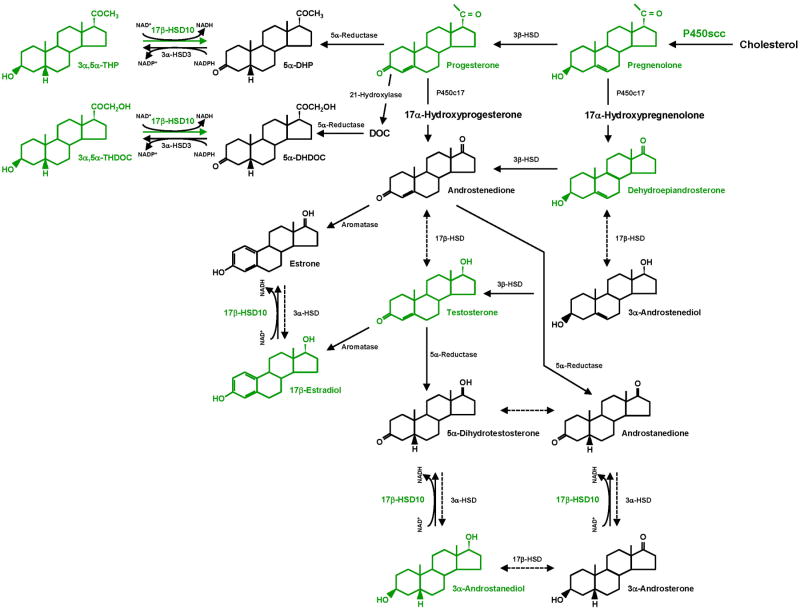
Figure 1.
Outline of neurosteroidogenesis. Neuroactive steroids and neurosteroidogenic enzymes that are potential key therapeutic targets are shown in green. The side chain of cholesterol is cleaved by P450scc as cholesterol is transported to the inner mitochondrial membrane and thus converted to pregnenolone. Soluble pregnenolone can enter into the endoplasmic reticulum unaided. 17β-HSD10 catalyzes the oxidation of neuroactive steroids in mitochondria with NAD+ as the coenzyme. This enzyme most effectively catalyzes the oxidation of 3α,5α-THP and 3α,5α-THDOC such that it is essential for the homeostasis of these neuroactive steroids, which was controlled by a dual enzyme molecular switch, composed of 17β-HSD10 and 3α-hydroxysteroid dehydrogenase type III (AKR1C2) localized in distinct subcellular compartments, mitochondria and ER, respectively (164, 168). The catalytic efficiencies (kcat/Km) of 17β-HSD10 are as high as 427 and 1,381 min-1 •mM-1 for the oxidation of 3α,5α-THP and 3α,5α-THDOC, respectively (163, 164). Abbreviations: 5α-DHP, 5α-dihydroprogesterone; DOC, deoxycorticosterone; 5α-DHDOC, 5α-dihydrodeoxycorticosterone; 3α,5α-THP, (3α,5α)-3-hydroxypregnan-20-one or allopregnanolone; 3α,5α-THDOC, (3α,5α)-3,21-dihydroxypregnan-20-one or allotetrahydrodeoxycorticosterone; HSD, hydroxysteroid dehydrogenase.
The most potent neuroactive steroids are the progesterone metabolite (3α,5α)-3-hydroxypregnan-20-one (3α,5α-THP or allopregnanolone) and the deoxycorticosterone (DOC) metabolite (3α,5α)-3,21-dihydroxypregnan-20-one (3α,5α-THDOC or allotetrahydrodeoxycorticosterone), which enhance γ-amino-butyric type A (GABAA) receptor mediated neurotransmission and produce inhibitory neurobehavioral effects (5). The 3α,5α-reduced metabolites of testosterone and dehydroepiandrosterone (DHEA), 3α,5α-androstandiol and 3α,5α-androsterone, respectively, also potentiate GABAA receptors, albeit with less potency (6). Specific binding sites for neuroactive steroids have been identified on the α subunits of the GABAA receptor that allosterically modulate binding to GABA and benzodiazepine recognition sites (7). At nanomolar concentrations, 3α,5α-THP enhances affinity of GABA for its receptor, while at micromolar concentrations, it directly activates the receptor channel. 3α,5α-THP and 3α,5α-THDOC modulate both synaptic and extrasynaptic GABAA receptors albeit with higher potency at extrasynaptic receptors that contain δ subunits (5, 6). 3α,5α-THP also modulates serotonin type 3 receptors, neuronal nicotinic acetylcholine receptors, and voltage-activated calcium channels, although with micromolar potency (8). Another site of 3α,5α-THP action, the nuclear pregnane xenobiotic receptor (PXR) has been recently identified (9). In contrast, the sulfated derivative of pregnenolone inhibits GABA release, binds with high affinity to, and promotes trafficking of N-methyl-D-aspartate (NMDA) receptors, thus exerting excitatory actions (10). It is still unclear how neuroactive steroids act on their membrane receptor targets, whether it is through paracrine or autocrine mechanisms or by intracellular lateral diffusion through the cell membrane (11). Further, in addition to 3α,5α-THP's action at the aforementioned pharmacodynamics targets, it may also have homeostatic pharmacokinetic effects through its actions at nuclear PXR (9).
Pharmacological properties
Neuroactive steroids exert several psychopharmacological actions such as anxiolytic, antidepressant, anticonvulsant, sedative, anesthetic, analgesic and amnesic effects, likely due to their actions on GABAA receptors (12-18). Moreover, 3α,5α-THP promotes sexual behavior of female rodents (19). Neuroactive steroids also possess rewarding properties in rodents (20, 21), and can modulate ethanol or cocaine intake (22-24). Indeed, acute administration of several drugs of abuse, like alcohol, nicotine, morphine, γ-hydroxy-butyric acid (GHB) or Δ9-tetrahydrocannabinol, increases brain and plasma concentrations of 3α,5α-THP and/or its precursors progesterone and pregnenolone in rats or mice (25-30) and this increase is thought to contribute to their rewarding effects.
In addition to these psychopharmacological effects, neuroactive steroids exert neuroprotective, neurotrophic and antiapoptotic effects in animal models of traumatic brain injury, spinal cord injury, peripheral neuropathy, cerebral ischemia, stroke, seizure disorder, and of neurodegenerative diseases such as multiple sclerosis, Alzheimer's disease, Parkinson's disease, Nieman Pick type C disease (31-44). More recently, an anti-tumor effect of progesterone has been reported in experimental models of glioblastoma multiforme (45).
Physiological significance
Neuroactive steroid concentrations fluctuate in response to physiological conditions like stress, development, ovarian cycle, pregnancy and post-partum and their fluctuations have been associated with changes in GABAA receptor plasticity.
Neuroactive steroids are increased in rats and humans following acute stress and this effect may represent a homeostatic mechanism to restore the altered hypothalamic-pituitary-adrenal (HPA) axis function (46, 47). The neuroactive steroid response to stress is a complex phenomenon that involves adaptations in GABAA receptor plasticity and appears to differ across species (for recent reviews see (23, 48)).
Neuroactive steroid concentrations also fluctuate across development. Brain levels of 3α,5α-THP are elevated in the embryonic rat, decrease around birth, show a transient increase on days 10-14, and remain low until puberty (49). The onset of puberty is associated with a rapid elevation in 3α,5α-THP levels and a marked increase in extrasynaptic α4βδ GABAA receptors, the main target of 3α,5α-THP, through which this steroid is thought to increase excitability and, thus exert the “paradoxical effect” of increasing anxiety in pubertal female mice (50).
Moreover, neuroactive steroids fluctuate across the ovarian cycle: progesterone and 3α,5α-THP levels are increased in mouse brain during diestrous (51) and in women's plasma during the luteal phase of the menstrual cycle (52). These changes are accompanied by increased expression of the δ subunit and decreased expression of the γ2 subunit of the GABAA receptor, with subsequent increase in tonic inhibition and decreased seizure susceptibility and anxiety (53).
Levels of progesterone and 3α,5α-THP increase markedly during pregnancy in both rats and women (54, 55) and decrease immediately prior to parturition in rats, before returning to baseline levels two days after delivery (54). These abrupt changes in steroid concentrations were associated with changes in GABAA receptor subunit expression that were thought to contribute to post-partum depressive symptoms (54, 56, 57).
Pharmacological treatments with steroids, which affect brain 3α,5α-THP levels, modify GABAA receptor plasticity. Steroid withdrawal from long-term exposure of progesterone or 3α,5α-THP markedly increases hippocampal α4 and δ subunit expression, with subsequent changes in receptor function, sensitivity to benzodiazepines and increased anxiety and seizure susceptibility (58). Long-term administration of ethinyl-estradiol and levonorgestrel, two of the synthetic steroids most frequently used in hormonal contraceptives, decreased cerebral cortical and hippocampal pregnenolone, progesterone and 3α,5α-THP concentrations and these changes were associated with increased expression of the GABAA receptor γ2 subunit, and increased anxiety-like behavior in adult female rats (59-61). Neonatal administration of β-estradiol-3-benzoate to female rats, a treatment that affects sexual differentiation of the brain (62), induces a marked and persistent decrease in the cerebrocortical and hypothalamic concentrations of 3α,5α-THP in adulthood, which is associated with compensatory changes in GABAA receptor subunit expression (63, 64). Likewise, changes in 3α,5α-THP milieu during development, induced by neonatal finasteride administration, increase the expression of hippocampal α4/δ GABAA receptors and induce anxiety-like behavior in adulthood (65).
The molecular underpinnings for the steroid-induced plasticity of GABAA receptors are not quite understood. A recent study has reported increased phosphorylation and membrane trafficking of α4 subunit-containing GABAA receptors promoted by 3α,5α-THDOC (66), a novel mechanism by which neuroactive steroids may affect GABAA receptor expression and function.
Pathological significance and therapeutic implications
Neurosteroidogenesis is impaired in several neuropsychiatric and neurodegenerative diseases (Table 1). For instance, a reduction in the concentrations of several neuroactive steroids (3α,5α-THP, 3α,5β-THP, 3α,5α-THDOC, 3α,5α- and 3α,5β-androsterone), or their precursors (pregnenolone, progesterone, DOC, DHEA) was reported in serum and/or cerebrospinal fluid of patients with major depression, premenstrual dysphoric disorder, post-traumatic stress disorder, schizophrenia, bipolar disorder, and in abstinent alcoholics (67-74). Likewise, brain concentrations of progesterone and 3α,5α-THP are altered in animal models of anxiety/depression (75-77) and post-traumatic stress disorder (78). Moreover, patients with male pattern hair loss treated with the 5α-reductase blocker finasteride report increased symptoms of depression and show altered levels of pregnenolone, progesterone, dihydroprogesterone, 3α,5α-THP, testosterone, dihydrotestosterone, 3α,5α- and 3α,5β-androstandiol, and 17β-estradiol even after drug discontinuation (79). It is not clear whether the impaired neurosteroidogenesis contributes to the disease outcome or whether it is the result of altered brain homeostasis. Interestingly, pharmacological treatment with antidepressants like fluoxetine, reboxetine, venlafaxine, imipramine or mirtazapine, but also with antipsychotics like clozapine and olanzapine, or mood stabilizers like carbamazepine or lithium, restores central and peripheral concentrations of 3α,5α-THP in rats and humans (68), suggesting that neuroactive steroids may contribute to the therapeutic efficacy of antidepressant medications.
Table 1.
Preclinical and clinical evidences for dysregulation in neurosteroidogenesis in neuropsychiatric and neurologic disorders.
| Disease | Experimental studies | |
|---|---|---|
|
| ||
| Mouse / Rat | Human | |
| Neuropsychiatric disorders | ||
| Anxiety disorders | Anxiolytic-like effects of 3α, 5α-THP in several animal models (12, 68). Anxiolytic-like effects of TSPO ligands in animal models (117). |
Increased serum levels of 3α, 5α-THP and 3α, 5β-THP, and decreased 3β, 5α-THP levels in patients with panic disorder (68). No change in 3α, 5α-THP levels in patients with generalized anxiety disorders (68). Decreased TSPO expression in platelets and lymphocytes (104). Anti-panic effects of TSPO ligands in experimental induced anxiety (117). |
| Depression | Antidepressant-like effects of 3α, 5α-THP (13). Decreased brain 3α, 5α-THP levels in animal models of depression, and normalization by antidepressant treatment (75-77). |
Decreased cerebrospinal fluid and serum 3α, 5α-THP levels, and normalization by antidepressant drugs (214, 215). Decreased serum levels of pregnenolone, progesterone, 3α, 5α-THP, 3α, 5β-THP, DHEA, 3α, 5α-androsterone and 3α, 5β-androsterone in women with a history of depression (69). |
| Premenstrual dysphoric disorder (PMDD) | Progesterone withdrawal model of PMDD associated with a upregulation of extrasynaptic α4/δ GABAA receptors and decreased sensitivity to benzodiazepines (58). | Symptoms start at ovulation, paralleling the rise in progesterone and 3α, 5α-THP levels, and severity reaches its maximum at the neuroactive steroid peak (70). Administration of progesterone or 3α, 5α-THP exacerbates negative mood symptoms in PMDD patients (70). |
| Post-traumatic stress disorder (PTSD) | Decreased brain 3α, 5α-THP in the socially isolated mouse model of PTSD (78). Ganaxolone improves behavioral deficits in the socially isolated mouse model of PTSD (216). |
Decreased cerebrospinal fluid 3α, 5α-THP concentrations (217). Decreased TSPO expression in platelets (104). |
| Bipolar disorder | -- | Increased pregnenolone and DHEA levels in posterior cingulate and parietal cortex (72). Increased plasma progesterone and 3α, 5α-THP levels (218). Decreased TSPO expression in platelets (104). |
| Schizophrenia | Increased cerebral cortical 3α, 5α-THP following olanzapine and clozapine administration in rats (80). | Increased pregnenolone and DHEA levels in posterior cingulate and parietal cortex (72). Decreased 3α, 5α-THP levels in parietal cortex (72). Decreased TSPO expression in platelets (104). Pregnenolone treatment improves cognition and negative symptoms in patients with schizophrenia (81). |
| Addiction | 3α, 5α-THP has rewarding properties (20, 21, 219). Neuroactive steroids have ethanol-like discriminative stimulus properties (22, 102, 191). Acute administration of psychoactive drugs with abuse liability increases neuroactive steroid levels (25-30). Neuroactive steroids modulate ethanol and cocaine intake (22, 204, 205, 220-222). Overexpression of P450scc in the ventral tegmental area increases 3α, 5α-THP and reduces ethanol reinforcement and consumption (161). |
Increased plasma 3α, 5α-THP levels in adolescents following alcohol intoxication (195, 196). Decreases serum 3α, 5α-THP and 3α, 5α-THDOC during alcohol withdrawal (73). Neuroactive steroids mediate subjective effects of ethanol (198, 200). |
| Neurological disorders | ||
| Epilepsy | Anticonvulsant effects of 3α, 5α-THP in several animal models (14, 84). | Clinical trials with ganaxolone (82) and progesterone (83). 3α, 5α-THP treatment for pediatric super-refractory status epilepticus (223). |
| Alzheimer's disease | Decreased neuroactive steroid precursors in brain of 3×TgAD mice (88). Neuroprotective and neurotrophic effects of 3α, 5α-THP in 3×TgAD mice (42, 94). Up-regulation of glial TSPO (104). TSPO ligands reverse AD-related neuropathology in 3×TgAD mice (116). Progesterone administration increases progesterone and 3α, 5α-THP levels in the cortex of APPswe+PSEN1Δe9 mice; it also improves cortically-mediated but not hippocampal-mediated cognitive tasks (156, 157). Increased 17β-HSD10 expression in brains of Alzheimer's disease mouse models (179). |
Decreased prefrontal cortex 3α, 5α-THP levels, which are inversely correlated with neuropathological disease stage (89). Decreased plasma 3α, 5α-THP levels in people in the early stages of AD (154). Elevated glial TSPO expression appears early in disease and co-localizes with neuropathology (121). Increased expression of 17β-HSD10 in activated astrocytes (164). |
| Parkinson's disease | 3α, 5α-THP restores tyrosine hydroxylase neurons and improves motor performance in MTPT-treated mice (43). | Decreased dihydroprogesterone and 3α, 5α-THP levels in plasma and liquor (90). |
| Multiple sclerosis | Decreased expression of 3α-HSD and 3α, 5α-THP levels in brain of mice with experimental autoimmune encephalomyelitis (39). 3α, 5α-THP treatment attenuates experimental autoimmune encephalomyelitis neuropathology in mice (39). Neuroactive steroid levels in rats are altered in a brain region and sex dependent manner (85). |
Decreased 5α-reductase expression and 3α, 5α-THP levels in the white matter (39). Increased TSPO expression in white matter lesions correlates with brain damage (104). Increased levels of neuroactive steroid precursors and decreased levels of dihydroprogesterone, 3α, 5α-THP, and dihydrotestosterone in plasma and cerebrospinal fluid of male patients (86). |
| Niemann-Pick type C disease | Decreased steroidogenic enzymes expression, as well as pregnenolone and 3α, 5α-THP brain levels in NP-C mice (44). Neuroprotective effect of 3α, 5α-THP in NP-C mice (44). |
-- |
| Diabetic neuropathy | Decreased brain and peripheral neuroactive steroid levels in rats with streptozotocin-induced diabetes (92). Neuroprotective effects of progesterone, dihydroprogesterone and 3α, 5α-THP in streptozotocin-induced diabetic neuropathy in rats (96). |
-- |
| Traumatic brain injury | Neuroprotective effects of progesterone and 3α, 5α-THP in rats (31). Progesterone and DHEA levels correlate with neurological recovery from TBI in mice (91). |
Negative outcome of clinical trials with progesterone (224). |
| Stroke | Neuroprotective effects of progesterone and 3α, 5α-THP in mice (97). | Increased TSPO expression in primary lesion and remote areas (104). |
Impaired neurosteroidogenesis has also been reported in patients with schizophrenia and it has been suggested that elevations of pregnenolone and 3α,5α-THP may contribute to the therapeutic efficacy of clozapine and olanzapine (80). Indeed, adjunct treatment with pregnenolone improves cognition and negative symptoms in patients with schizophrenia (81), suggesting that neuroactive steroids contribute to schizophrenia pathophysiology.
Given their anticonvulsant properties, neuroactive steroids have also been proposed as therapeutic agents for epilepsy. Clinical trials with ganaxolone are under way in subjects with epilepsy (82). Progesterone treatment is effective at reducing seizures among women with catamenial epilepsy and 3α,5α-THP mediates these effects (83). Neuroactive steroids are preferred over the classical benzodiazepine treatment because of their lack of anticonvulsant tolerance and because of their neuroprotective properties that contribute to reduce neuroexcitotoxicity and neuronal damage (84).
The discovery of the neuroprotective, neurotrophic and anti-inflammatory properties of neuroactive steroids has prompted numerous investigations into their therapeutic potential for neurodegenerative diseases. Impaired neurosteroidogenesis has been found in animal models as well as in humans with multiple sclerosis (39, 85, 86), Alzheimer's disease (42, 87-89), Parkinson's disease (90), traumatic brain injury (91), diabetes (92), suggesting that neuroactive steroids may contribute to the neuropathological processes of these diseases (93). Indeed, the reduction in 3α,5α-THP content correlated with severity of Alzheimer's disease in humans (89). Thus, restoring neuroactive steroid concentrations may represent a useful therapeutic approach for these neurodegenerative disorders. Several preclinical studies have been successful in this respect. For instance 3α,5α-THP promotes neurogenesis, improves learning and memory and ameliorated the pathology burden in the triple transgenic AD (3xTgAD) mouse model (42, 94, 95). 3α,5α-THP has also shown therapeutic efficacy in animal models of multiple sclerosis (39), Parkinson's disease (43), Niemann-Pick type C disease (44), diabetic neuropathy (96), traumatic brain injury (31), and stroke (97).
Taken together, this evidence suggests that neuroactive steroids may have therapeutic utility in several neuropsychiatric and neurologic disorders. However, direct administration of 3α,5α-THP has several challenges that limit its therapeutic use. These include a short half-life (98), low bioavailability and poor solubility in aqueous formulations, which limits its oral administration (99), development of tolerance (100), side effects such as sedation (98), memory impairment (101), and addiction potential (20, 21, 102). Thus, different approaches to target the neuroactive steroid biosynthetic pathway have been explored. This review summarizes recent advances in neurosteroidogenesis and highlights the importance of modulating neuroactive steroid synthesis as a putative therapeutic approach for neuropsychiatric and neurodegenerative diseases that affect millions of people worldwide.
Translocator protein as a therapeutic target for Alzheimer's disease
The translocator protein (TSPO) is a five transmembrane structure located at the outer and inner mitochondrial membrane contact sites, expression of which is enriched in steroidogenic organs (103). Activation of TSPO by synthetic TSPO ligands elicits pleiotropic neuroprotective and cognitive benefits, mechanistically linked to regulation of mitochondrial function, including the facilitation of mitochondrial cholesterol import for steroidogenesis (104). Numerous endogenous ligands of TSPO have also been identified, including diazepam binding inhibitor (DBI), triakontatetraneuropeptide (TTN), phospholipase A2 (PLA2), and protoporphyrin IX, which also have the ability to stimulate mitochondrial cholesterol import and neurosteroidogenesis (104-106). Recent studies using TSPO-knockout mice indicate that TSPO function in steroidogenesis may be tissue specific, playing a crucial role in the adrenal but not the testes (107-111). Although the role of TSPO in steroidogenesis in the brain remains to be addressed using similar models, numerous studies have demonstrated the ability of TSPO ligands to increase neuroactive steroid hormone production in the brain by increasing cholesterol supply to P450scc at the inner mitochondrial membrane, which is the rate-limiting step in neurosteroidogenesis (112-118).
Alzheimer's disease is a neurodegenerative disorder that leads to memory loss and cognitive impairment; it is characterized by the accumulation of beta amyloid plaques and neurofibrillary tangles in the brain (119). Age-related depletion of neuroactive steroid levels is an established risk factor for Alzheimer's disease, with neuroactive steroids having numerous beneficial effects in animal models of Alzheimer's disease, including reducing accumulation of the toxic beta amyloid (Aβ) peptide, thought to be the toxic principle driving Alzheimer's disease degenerative cascades (119). TSPO ligands that stimulate the synthesis of protective neuroactive steroids directly in the brain offer a novel therapeutic approach aimed at harnessing the protective actions of neuroactive steroids for the prevention and/or treatment of Alzheimer's disease.
In the brain, TSPO is predominantly expressed in astrocytes and microglia, with low levels also observed in neurons following injury or during repair (120). TSPO is a sensitive marker of gliosis, becoming markedly upregulated in glial cells during aging, following injury and in Alzheimer's disease (104). Although TSPO expression is closely linked to gliosis, the specific role of TSPO in glial function remains poorly understood. In Alzheimer's disease, elevated glial TSPO expression is observed early in the disease process and co-localizes with degeneration and neuropathology (121). Consequently TSPO ligands are also under widespread investigation as potential inflammatory biomarkers for in vivo PET imaging in Alzheimer's disease, leading to the development of many new-generation, safe TSPO ligands with the potential to be repurposed for Alzheimer's disease therapy.
The translocator protein forms part of a complex with the VDAC and ANT, and has been implicated in mitochondrial cholesterol import (104). Mitochondrial cholesterol import is the rate limiting step in neuroactive steroid formation. Once localized at the inner mitochondrial membrane, cholesterol is converted to pregnenolone, the precursor to all other neuroactive steroids (see Figure 1). TSPO has a cholesterol recognition amino acid consensus sequence (CRAC) at the C-terminal identified as a cholesterol binding site (122), which is proposed to play a functional role in mediating the transportation of cholesterol across the hydrophilic intermembrane space. Structural studies indicate that ligand binding stabilizes the tertiary structure of TSPO facilitating cholesterol import (123). A common polymorphism at the C-terminal of human TSPO results in conformational changes interfering with the cholesterol binding site (124), which is associated with impaired cholesterol binding and metabolism (122) and reduced ability to produce pregnenolone (125). In addition to cholesterol import, TSPO has also been implicated in other important mitochondrial functions including mitochondrial respiration and ATP production (126), which may also contribute to the protective actions of TSPO ligands.
TSPO ligands have been shown to promote nerve regeneration, increase neuronal survival, reduce oxidative damage, inhibit apoptosis, attenuate gliosis and decrease Aβ accumulation in animal models of traumatic brain injury, excitotoxicity, axotomy and neuropathy, inflammatory disease and Alzheimer's disease (104, 116, 120). For example, in rats, the TSPO ligand, Ro5-4864, reduced reactive gliosis and neuronal loss following kainate acid-induced excitotoxicity (127). In vitro evidence indicates TSPO ligands act directly on glia to reduce inflammatory responses (128, 129), with the TSPO ligand, PK11195, decreasing pro-inflammatory cytokine production in cultured human microglia in response to LPS stimulation. Chronic inflammation and glial dysfunction contribute to the pathological degenerative cascade in Alzheimer's disease, and anti-inflammatory drugs have shown therapeutic promise for Alzheimer's disease (130). In the triple transgenic Alzheimer's disease mouse model (3xTgAD), the TSPO ligand, Ro5-4864, has been shown to reduce gliosis as well as lower accumulation of Aβ and improve functional behavioural outcomes (116). Interestingly, protection against Alzheimer's disease-related pathology was associated with increased brain levels of the protective neuroactive steroids in young-adult but not aged animals, suggesting that neuroactive steroid regulation may not be essential for the TSPO-mediated protective effects in this model.
TSPO ligands also have diverse neuropsychiatric benefits, including anxiolytic, anti-depressive and cognitive-enhancing properties commonly attributed to their ability to increase levels of 3α,5α-THP, progesterone and testosterone (104, 116, 131). Consequently, TSPO ligands may offer symptomatic therapeutic opportunities for a range of neurological disorders, including Alzheimer's disease. For example, the new generation TSPO ligand, XBD-173, reduced anxiety-related behaviour in both rats and humans (117, 132). Mechanistically, the anxiolytic effect of XBD-173 was linked to enhanced GABA neurotransmission as a result of increased production of the neuroactive steroid 3α,5α-THP, which is an allosteric GABAA receptor modulator (117). Neuroactive steroids have well defined, potent, and broad cognitive, behavioural and psychological benefits including improved mood, and reduced anxiety and depression; this is coupled with a favourable side-effect profile, including the absence of sedation, tolerance, withdrawal symptoms or motor impairment (104). Therefore, neurosteroidogenic TSPO ligands may also be therapeutically useful for the treatment of not only the cognitive, but also the neuropsychiatric symptoms of Alzheimer's disease, including anxiety, agitation, depression, apathy and aggression. The treatment of neuropsychiatric symptoms in Alzheimer's disease is difficult and currently available therapies are not particularly effective in the management of these symptoms (133). These neuropsychiatric symptoms drive institutionalization; therefore improvement of currently offered pharmacotherapies has the potential to be valuable in terms of patient and caregiver quality of life.
TSPO offers a promising therapeutic target for Alzheimer's disease, with diverse neuroprotective and psychological benefits identified. Further, many new generation, safe TSPO ligands have been developed for in vivo imaging in humans, which may also prove therapeutically useful in the treatment of Alzheimer's disease. However, determination of the key mechanism(s) of TSPO action is critical for identifying the most efficacious TSPO ligands, optimally translating preclinical findings into clinical use, and rationally developing new TSPO ligands for therapeutic use (131). The recent development of numerous TSPO knockout mouse models will prove invaluable in addressing the role of TSPO in both normal and diseased states, as well as confirming the specificity of drug action.
Pregnane xenobiotic receptor (PXR): a novel target for neuroactive steroid synthesis and action
Neuroactive steroids can have rapid and robust actions in the central nervous system for behaviour. A model that has been utilized to elucidate the requisite role that production of pregnane steroids, such as 3α,5α-THP, have in the brain for behaviours has focused on reproductive endpoints. Several molecules, including TSPO, P450scc, StAR, 3α-hydroxysteroid dehydrogenase, and 5α-reductase, are downstream of cholesterol in the pregnane neurosteroidogenesis pathway (134-137). Pharmacologically blocking these at any point in this pathway reduces 3α,5α-THP formation in the brain and abolishes the lordosis response of female rodents (reviewed in (138)). More recently, the PXR has been identified as a potential factor upstream of cholesterol metabolism. PXR is a nuclear receptor that binds steroids, such as 3α,5α-THP, and influences transcription of cytochrome P450 enzymes that are involved in metabolism of many factors, including cholesterol and steroids (139-141). Although PXR is generally regarded for its role in the liver, it has been identified in brain regions, involved in motivation, affect and cognition, such as the ventral tegmental area, hippocampus, and cortex in mammals (9, 142-145). PXR is required for production of 3α,5α-THP and its actions for lordosis in the VTA, as well as for anxiety-related behaviours in the hippocampus (9, 143, 144, 146-149). Indeed, these effects of PXR may involve the well-known targets of 3α,5α-THP such as, NMDA and GABAA receptors (149). A question of interest is the role of PXR in other brain targets of steroids for behavioural plasticity, such as that underlying cognitive performance.
Pregnane steroids can enhance cognitive performance in young female rodents. Increased production of 3α,5α-THP with oestrous cycle fluctuations or replacement of progesterone or 3α,5α-THP to ovariectomised rodents is associated with better performance in hippocampal and cortical tasks, such as the object recognition task, as well as increased 3α,5α-THP in these regions (150). These effects persist in the absence of progestin receptors, which are not a typical target of 3α,5α-THP, but not with genetic knockout of 5α-reductase (151, 152). We have been examining the cognitive sequelae of rats with PXR knockout, on a Sprague-Dawley background, generated by Sage Labs. In the object recognition task, PXR-replete rats perform at chance (50 +/- 2% of object investigation time exploring the novel object); however, rats lacking functional PXRs perform below chance (40 +/- 2% of time exploring the novel object). Thus, capacity to form 3α,5α-THP may be critical for object memory among young female rodents.
With aging, there is a different pattern of effects of pregnane steroids in the hippocampus and cortex for cognitive performance, suggesting greater responses to progesterone decline and replacement in the cortex. For example, in addition to age-related decline in reproductive success, there is decline in 3α,5α-THP levels in frontal cortex of female rats (153). Variability in the cognitive response in this rat model of reproductive senescence or “menopause” is associated with 3α,5α-THP levels in the cortex (153). Thus, 3α,5α-THP can have pro-cognitive effects in healthy systems, but the target and patterns of these effects may be sensitive to aging; a question is whether pregnane steroids can improve hippocampal and cortical function in both healthy and compromised systems.
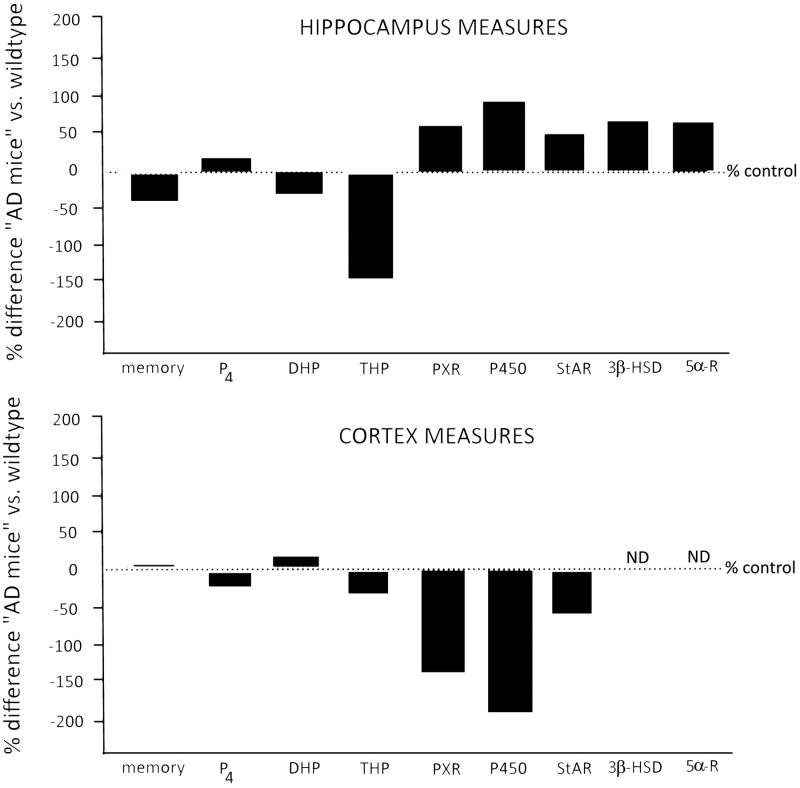
Another approach to investigate the role of pregnane neurosteroidogenesis as a critical target is to assess effects in age-related dementia. We, and others, have shown that people in the early stages of Alzheimer's disease or dementia have lower circulating levels of 3α,5α-THP than do non-demented peers matched for age, gender, education and socioeconomic factors (154). We have also used a double transgenic mouse model of early-onset familial Alzheimer's disease that co-overexpresses mutant forms of amyloid precursor protein and presenilin 1 Δ exon 9 mutation (APPswe+PSEN1Δe9; (155-157)). Comparisons were made following ovariectomy at 6 months of age and administration of chronic subcutaneous pellets of placebo (cholesterol) or progesterone for 6 months. In this mouse model, genetic mutations cause them to develop β-amyloid deposits after 5 months of age, and by 9 months old severe plaque deposits build up in the cortex and hippocampus (155). APPswe+PSEN1Δe9, compared to wild-type mice, had poorer performance on hippocampally-mediated tasks (worse object placement performance and more depressive behaviour in the forced swim task); progesterone improved responding in the wild-type, but not the APPswe+PSEN1e9, mice in these tasks (156, 157; Figure 2). Baseline differences were not observed in cortically-mediated tasks (object recognition or T maze) between the mouse strains, and progesterone improved performance of both wild-type and APPswe-PSEN1Δe9 mice in both of these tasks (156, 157; Figure 2). Additionally, progesterone, compared to vehicle, increased progesterone and 3α,5α-THP in the cortex of both wild-type and APPswe+PSEN1Δe9, but only increased 3α,5α-THP in the hippocampus of wild-type mice (156, 157). Thus, these data suggest that progesterone does not improve APPswe-PSEN1Δe9 behaviour in hippocampally-mediated tasks, like that of wild-type mice, and that they also show deficiencies in their capacity to form 3α,5α-THP in the hippocampus. Whereas, in the prefrontal cortex, they were able to form 3α,5α-THP, and wild-type and APPswe-PSEN1Δe9 mice performed similarly in these tasks, with progesterone administration improving their overall performance.
Figure 2.
Figure depicts behaviour, pregnane steroid concentrations, and expression patterns in the hippocampus (top panel) and cortex (bottom panel) for 12 month old transgenic mice that co-overexpress mutant forms of amyloid precursor protein and presenilin 1 Δ exon 9 mutation (APPswe+PSEN1Δe9; a murine model of early-onset familial Alzheimer's disease- AD), compared to their age-matched wild-type controls (n = 4-6). For all measures, mice had data collected at 12 months of age, following 6 months of continuous progesterone (P4) administration via subcutaneously implanted pellets (25 mg, 90-day release at 6 months of age and then 9 months of age; purchased from Innovative Research of America). Behaviour: Performance in a memory task assessing the hippocampus (object placement) and cortex (object recognition) is depicted and based upon comparing the Alzheimer's disease mice to wild-type controls (methods and raw data published in (146)). Pregnane steroid concentrations: Levels of P4, dihydroprogesterone (DHP), and 3α,5α-THP (THP) were measured using radioimmunoassay of dissected out hippocampus and cortex (methods and raw data published in (146)). Protein expression: Expression patterns in hippocampus and cortex were determined by western blotting, of specific proteins (pregnane xenobiotic receptor (PXR), cytochrome P450-dependent side chain cleavage- P450scc, steroidogenic acute regulatory protein- StAR, 3β-hydroxysteroid dehydrogenase- 3β-HSD, and 5α-reductase- 5α-R). The mean of relative intensity (relative density of protein of interest to actin control) in hippocampus and cortex of Alzheimer's disease mice were compared to that determined in wild-type controls. A standard western blotting protocol (146) was employed to assess these factors in hippocampus and prefrontal cortex tissues (a description of tissue collection from animal subjects, brain storage, dissection and preparation is described in (146)). Protein concentration for each sample was determined with a Nanodrop spectrometer. Samples of equal protein concentrations were then prepared for loading on to NuPAGE Bis-Tris Mini Gels (4-12% SDS Polyacrylamide) by combining them with 2.5 μl of NuPAGE LDS (4×) sample buffer, 1 μl of NuPAGE Reducing Agent (10×), 6.5 μl of deionized water (Invitrogen). Electrophoresis was then conducted with running gels with 1× MOPS running buffer with one lane reserved for the protein ladder and one for the positive control (liver homogenate). Protein was then transferred to nitrocellulose using 1× NuPAGE Transfer buffer. The blots were blocked in 5% milk PBS-10% tween solution. All blots were probed with primary antibodies (Ab) at 4°C overnight. Primary (1°) Ab for PXR, P450, StAR, and 5α-reductase were purchased from Santa Cruz Biotechnology; 3β-HSD was received from Dr. Penning, and actin was purchased from Sigma. The secondary (2°) Ab was a Goat Anti-Mouse IG (H+L) Horseradish Peroxidase Conjugate (Bio-rad, Hercules, CA, USA). Concentrations of Ab were: PXR (1° Ab concentration 1:1000; 2° Ab concentration 1:2500); P450 (1° Ab concentration 1:2500; 2° Ab concentration 1:2500); StAR (1° Ab concentration 1:1000; 2° Ab concentration 1:2500); 3β-HSD (1° Ab concentration 1:2500; 2° Ab concentration 1:2500); 5α-reductase (1° Ab concentration 1:1500; 2° Ab concentration 1:2500), actin (1° Ab concentration 1:500; 2° Ab concentration 1:2500). Blots were probed with 2° Ab for 1 hour on a shaker at room temperature (Bio-rad). Results were visualized using DuoLuX Chemiluminescent/Fluorescent Substrate Kit for Peroxidase (Vector Laboratories), imaged on a ChemiDoc XRS (Bio-rad), and analyzed using ImageJ software. Expression was not detected (ND) for 3β-HSD in either group or for 5α-reductase in the wild-type controls, albeit Alzheimer's disease mice showed 2.0 relative intensity. Relative intensity values in the hippocampus (mean ± sem) for PXR (wildtype 0.4 ± 0.2; AD 1.0 ± 0.2), P450 (wildtype 0.3 ± 0.1; AD 1.4 ± 0.3), StAR (wildtype 0.6 ± 0.1; AD 1.0 ± 0.3), 3α-HSD (wildtype 0.4 ± 0.2; AD 0.8 ± 0.5) and 5α-reductase (wildtype 0.5 ± 0.2; AD 1.0 ± 0.7). Relative intensity values in the cortex (mean ± sem) for PXR (wildtype 2.2 ± 1.2; AD 1.0 ± 0.3), P450 (wildtype 1.7 ± 0.8; AD 0.6 ± 0.1), StAR (wildtype 1.4 ± 0.8; AD 0.9 ± 0.2), 3α-HSD (wildtype ND; AD ND) and 5α-reductase (wildtype ND; AD 2.0 ± 1.2).
Studies in people that have been diagnosed with probable Alzheimer's disease and using other Alzheimer's disease mouse models suggests that there may be faulty metabolism effects in Alzheimer's disease relating to pregnane neuroactive steroids (as discussed herein and see (89, 99, 154)). A question of interest is the importance of PXR acting upstream of cholesterol for these effects. Levels of PXR as well as downstream enzymes required to 3α,5α-THP formation, such as P450scc, StAR, 3β-hydroxysteroid dehydrogenase, and 5α-reductase, were measured by western blotting in the hippocampus and frontal cortex of behaviourally-assessed wild-type and APPswe+PSEN1Δe9 mice. The greatest increases in expression among the APPswe+PSEN1Δe9 mice, compared to their wild-type controls, was for PXR, P450scc, 3β-hydroxysteroid dehydrogenase, and 5α-reductase in the hippocampus (Figure 2). A different pattern was observed in the cortex with the greatest reductions in expression being for PXR and P450scc (Figure 2). This pattern of effects complements the behavioural effects observed as well as pregnane steroid levels in the hippocampus and cortex (Figure 2), and suggests the importance of additional consideration to neurosteroidogenic enzyme expression and activity in relation to behaviour and steroid levels in future studies. For example, an important follow-up study would be to assess levels of 3α-hydroxysteroid dehydrogenase. The findings that 5α-reductase was increased in the hippocampus of the APPswe+PSEN1Δe9 mice, with little difference in progesterone and dihydroprogesterone levels, but a large decrease in 3α,5α-THP levels, suggests that perhaps 3α-hydroxysteroid dehydrogenase activity is altered in the transgenic mice. Of further interest is the role of PXR in models of successful cognitive aging as well as neurodegeneration.
There may be beneficial effects of low body mass index and regular fasting to protect against Alzheimer's disease and promote longevity, albeit this is a controversial notion. Although a speculation, it may be that low body mass index and/or fasting may reduce burdens associated with switching from gluconeogenesis and lipolysis and demands for clearance, which would involve PXR and related factors, such as liver X receptor (42, 158, 159). A consideration about protein aggregation is faulty cholesterol metabolism may ultimately result in a neuropathological process. How PXR is related to pro-cognitive and protective effects of pregnane and other steroids and/or as pro-hormones for 3α,5α-THP is of interest. It may be that PXR is acting in the central nervous system, much like in the liver, to regulate metabolising enzymes, receptors, and efflux transporters, to promote homeostasis and brain health. Further investigations to directly address this are needed.
Roles of 17β-hydroxysteroid dehydrogenase type 10 (17β-HSD10) in neurosteroidogenesis
The circulating lipoprotein is a major source for neurosteroidogenesis even though cholesterol can be de novo synthesized from acetate in neurons and other brain cells. The molecular mechanism for lipoprotein transport into brain cells and for “free” cholesterol transport into mitochondrion has recently been reviewed (160). StAR on the outer mitochondrial membrane plays a key role in importing cholesterol into mitochondrion. StAR interacts with a complex machinery, of which the translocator protein TSPO serves as a downstream portal for cholesterol to move to the inner mitochondrial membrane where the side chain of cholesterol is cleaved by P450scc. As a result, cholesterol is converted to soluble pregnenolone. Since this is a rate-limiting step, overexpression of this side chain cleavage enzyme would generally elevate neuroactive steroid levels (161). Pregnenolone can be further oxidized to progesterone under the catalysis of 3β-hydroxysteroid dehydrogenase or exit the mitochondrion without active transport. It was reported (162) that in rat brain 3β-hydroxysteroid dehydrogenase is also present in the endoplasmic reticulum. However, the mitochondrion appears to possess a more favourable environment for an oxidative reaction catalyzed by 3β-hydroxysteroid dehydrogenase, since the ratio of NAD+/NADH in mitochondrion is about two orders of magnitude greater than that in the endoplasmic reticulum. It was also reported (116) that TSPO ligands elicit pleiotropic neuroprotective and cognitive benefits. Whether these effects are linked to the regulation of neuroactive steroid synthesis remains to be determined.
Pregnenolone and progesterone become substrates for P450c17 in the endoplasmic reticulum, where they are converted to DHEA and androstenedione, respectively. As shown in Figure 1, DHEA can be oxidized to androstenedione under the catalysis of 3β-hydroxysteroid dehydrogenase, and then be further converted to testosterone or estrone, and subsequently to more potent androgen (5α-dihydrotestosterone) and estrogen (17β-estradiol), respectively. On the other hand, progesterone can be oxidized to DOC under the catalysis of 21-hydroxylase. Progesterone and DOC are reduced by NADPH in the endoplasmic reticulum under the catalysis of 5α-reductase and then by AKR1C2 sequentially to form 3α,5α-THP and 3α,5α-THDOC, respectively. 3α,5α-THP as well as 3α,5α-THDOC facilitate affective and motivated social behaviour through non-genomic targets, such as GABAA receptors, glutamate, and dopamine receptors (5, 6, 9). Human AKR1C2 (3α-hydroxysteroid dehydrogenase type III) plays almost no actual role in the oxidation of 3α,5α-THP and/or 3α,5α-THDOC, because its catalytic efficiency is 7-fold less than that for its backward reduction and only one seventh of its oxidative reaction catalyzed by 17β-HSD10 (163). A more unfavourable factor for its oxidation in the endoplasmic reticulum is the disparity of redox coenzyme concentrations, e.g., the concentration of NADPH is at least one order of magnitude higher than that of NADP+. It seems unfeasible for 3α,5α-THP and/or 3α,5α-THDOC to be effectively inactivated by an oxidative reaction catalyzed by AKR1C2 (3α-hydroxysteroid dehydrogenase type III). Abnormal levels of 3α,5α-THP and/or 3α,5α-THDOC would certainly be harmful to brain functions. This puzzle was never really solved by implication of 3α-hydroxysteroid dehydrogenase catalyzing a reverse reaction between 5α-DHP and 3α,5α-THP as depicted in the figure 2 of Ref. (95). In fact, it was already found (163, 164) and emphasized (165-168) that mitochondrial 17β-HSD10 is essential for the maintenance of homeostasis of 3α,5α-THP and/or 3α,5α-THDOC (see Figure 1). 3α,5α-THP and/or 3α,5α-THDOC metabolism is mainly controlled by a dual enzyme molecular switch, composed of 17β-HSD10 and 3α-hydroxysteroid dehydrogenase type III (AKR1C2) localized in distinct subcellular compartments, mitochondria and endoplasmic reticulum, respectively (164, 168). With regard to the role of 17β-HSD10 in the metabolism of 3α,5α-THP, 17β-HSD10 had been twisted to ABAD (Aβ-binding alcohol dehydrogenase) for unknown reasons, as noticed in Figure 2 of Ref. (95).
The 17β-HSD10, a fascinating protein, is encoded by the HSD17B10 gene, which was first cloned from human brain in 1997 (GenBank accession No. AF037438). The role of 17β-HSD10, after many debates and criticisms, has been clarified in more recent studies (163-174): it plays essential roles in neurosteroidogenesis as well as in the isoleucine degradation pathway. This explains why a mutation(s) of this gene, HSD17B10, may delay the brain development and/or result in the regression of brain functions even in the absence of Aβ peptide (167, 168, 174-176).
It was reported (165, 168-170, 177) that 17β-HSD10 can catalyze the oxidative reaction of 17β-estradiol to oestrone, an inactive oestrogen (see Figure 1). Binding of the oestrogen receptor-α to 17β-HSD10 would inhibit the enzymatic activities of 17β-HSD10 whereas 17β-estradiol itself facilitates the dissociation of a 17β-HSD10-estrogen receptor-α complex (178). As is well known, 17β-estradiol exhibits significant neuroprotective effects. Elevated levels of 17β-HSD10 found in Alzheimer's disease brains (164, 165, 168, 179) may take a part in the pathogenesis of Alzheimer's disease due to an imbalance of neuroactive steroid metabolism (164-170, 174, 177).
It was found that a weak androgen, 3α-androstanediol, could be effectively converted to the most potent androgen, 5α-dihydrotestosterone (5α-DHT), under the catalysis of 17β-HSD10 (172, 173). Mitochondrial 17β-HSD10 plays a key role in the ‘back door’ androgen synthesis pathway especially in castrated animals (165, 168, 172, 173).
17β-HSD10 is involved in the metabolism of several neuroactive steroids such as 17β-estradiol, oestrone, 3α-androstanediol and 3α,5α-THP (see Figure 1). It was demonstrated (180) that such neuroactive steroids are able to improve neuronal bioenergetics significantly. Missense mutation(s) would abolish the catalytic activity of 17β-HSD10 in the isoleucine degradation pathway such that an accumulation of tiglylglycine and 2-methyl-3- hydroxybutyric acid in blood and the excretion of such isoleucine metabolites from urine is a common symptom in patients with 17β-HSD10 deficiency, which was therefore designated as 2-methyl-3- hydroxybutyryl-CoA dehydrogenase (MHBD) deficiency (181). It was reported (174) that mental retardation did not result from the accumulation of isoleucine metabolite, while an imbalance of neuroactive steroid metabolism could be a major cause of neurological handicap associated with brain-type 17β-HSD10 deficiency patients. Elucidation of the roles of 17β-HSD10 in neurosteroidogenesis provides further supports to this hypothesis.
Among the many factors essential for keeping mitochondria healthy, the homeostasis of neuroactive steroids is particularly significant because of its impact on the bioenergetics of brain cells (180). Abnormality of mitochondrial structure and function underlies pathophysiological basis of neurodegenerative disorders such as Alzheimer's disease and Parkinson's disease. Enzymes involved in neurosteroidogenesis are potential therapeutic targets in treatment of neurodegenerative disorders including brain-type HSD10 deficiency and Alzheimer's disease (168, 174-177, 179-181) as well as prostate cancer (172, 173).
Divergent neuroactive steroid responses across species: the case of ethanol-induced neurosteroidogenesis
Alcohol's effects on neuroactive steroid concentrations are the most well characterized among species. Pioneering studies in rats showed that systemic administration of ethanol (1-2.5 g/kg) increases plasma, cerebrocortical and hippocampal levels of the neuroactive steroids 3α,5α-THP and 3α,5α-THDOC in Sprague-Dawley rats (25, 182) and Sardinian alcohol-preferring rats (183). More recently, Cook et al. (184) showed that alcohol differentially affects cellular 3α,5α-THP immunostaining throughout the brain of Wistar rats. In fact, acute ethanol increased 3α,5α-THP immunoreactivity in the medial prefrontal cortex, the hippocampal CA1 pyramidal cell layer, the polymorph cell layer of the dentate gyrus, the bed nucleus of the stria terminalis, and the paraventricular nucleus of the hypothalamus. In contrast, ethanol decreased 3α,5α-THP immunoreactivity in the nucleus accumbens and the central nucleus of the amygdala. No changes were observed in the ventral tegmental area, dorsomedial striatum, granule cell layer of the dentate gyrus, or the lateral or basolateral amygdala (184).
The ethanol-induced increase in plasma neuroactive steroids is mediated by the HPA axis, since it is no longer observed in hypophysectomized and adrenalectomized rats (27, 185-187). However, ethanol has also been found to increase 3α,5α-THP in hippocampal minces from intact and adrenalectomized/gonadectomized rats (188, 189), suggesting that it is capable of inducing brain neurosteroidogenesis, independent from peripheral sources. Accordingly, the ethanol-induced increase in cellular 3α,5α-THP immunoreactivity is independent of adrenal activation in the CA1 pyramidal cell layer, dentate gyrus polymorphic layer, bed nucleus of the stria terminalis, and paraventricular nucleus of the hypothalamus of Wistar rats (190). Likewise, ethanol decreases 3α,5α-THP labelling in the nucleus accumbens “shore” (core-shell border), and central nucleus of the amygdala, independent of adrenal activation. However, in the medial prefrontal cortex ethanol increases 3α,5α-THP immunoreactivity in sham-operated animals, but not in adrenalectomized ones, suggesting that ethanol, directly and independently from peripheral sources, regulates local 3α,5α-THP levels in several subcortical regions, except for the medial prefrontal cortex (190).
Ethanol-induced elevations in neuroactive steroids reach physiologically relevant concentrations that enhance GABAergic transmission and thus, contribute to several behavioural effects of ethanol in rats. Neuroactive steroids modulate ethanol's anticonvulsant effects, sedation, impairment of spatial memory, anxiolytic-like and antidepressant-like actions (see (191) and (23) for review). Each of these behavioural responses is prevented by pre-treatment with the neuroactive steroid biosynthesis inhibitor finasteride and/or by prior adrenalectomy. The hypnotic effect of ethanol is partially blocked by adrenalectomy. Moreover, administration of 5α-dihydroprogesterone, the immediate precursor of 3α,5α-THP, to adrenalectomized rats restores effects of ethanol, showing that brain neuroactive steroid synthesis modulates effects of ethanol. Taken together, these studies suggest that elevations in neuroactive steroids influence many of the GABAergic effects of ethanol in vivo and contribute to sensitivity to behavioural effects of ethanol in rats (23, 191).
Studies on the neurosteroidogenic effects of ethanol in mice have yielded different results depending on the strains and the experimental conditions used. C57BL/6J mice have higher basal plasma neuroactive steroid levels compared to DBA/2J mice and that plasma 3α,5α-THP levels are decreased in C57BL/6J mice and not altered in DBA/2J mice following injection of 2 g/kg ethanol (182). Moreover, acute ethanol administration (1-4 g/kg) failed to alter cerebrocortical and hippocampal levels of 3α,5α-THP and progesterone in male C57BL/6J and DBA/2J mice, despite inducing a marked increase in brain and plasma corticosterone levels, a measure of HPA axis activation (192). Other studies reported that injection of 2 g/kg ethanol increased whole brain 3α,5α-THP levels in male DBA/2J (193) but not C57BL/6J mice (194), while orally consumed ethanol increased whole brain 3α,5α-THP levels in male C57BL/6J mice (194). Overall, these results highlight important species differences in ethanol's neurosteroidogenic effects between rats and mice.
The ethanol-induced changes in 3α,5α-THP content in mice appear to be related to the genetic background of the strain. In the genetic reference population of the C57BL/6J (B6) × DBA/2J (D2) (BXD) recombinant inbred strains, basal cerebral cortical 3α,5α-THP levels across selected strains ranged between 1.81 and 3.72 ng/g, while ethanol-induced changes in cerebral cortical 3α,5α-THP ranged between +4% and +63% (23). Both basal and ethanol-induced cerebral cortical 3α,5α-THP levels in the BXD strains were correlated with some phenotypes of ethanol intake, suggesting that neuroactive steroid responses to ethanol may be associated with excessive alcohol consumption (23).
The neurosteroidogenic effects of ethanol in humans have been examined in few studies, leading to inconsistent results. Elevated 3α,5α-THP plasma levels were reported in male and female adolescents seen in the emergency room for alcohol intoxication (195, 196), which likely resulted in high blood ethanol concentrations. In contrast, laboratory administration of low or moderate doses of ethanol was found not to alter plasma levels of 3α,5α-THP and other GABAergic neuroactive steroids (182, 197) or to decrease 3α,5α-THP levels (198) in healthy volunteers. Different ethanol doses, analytic methods to measure neuroactive steroids, age of the subjects or environmental factors that influence neuroactive steroid synthesis in humans may account for these inconsistent results. Indeed, the same dose of ethanol consumed in the human laboratory studies mentioned above (∼80 mg/dl) produced no effect in rats when administered systemically (182), suggesting that dose might be a key factor in the difference between rat and human studies. However, the possibility that ethanol may increase brain levels of 3α,5α-THP, without affecting its peripheral concentrations, remains open. In fact, some subjective effects of ethanol are diminished by prior administration of finasteride (199) or dutasteride (200), two inhibitors of 3α,5α-THP biosynthesis, suggesting that 3α,5α-THP may play a role in ethanol's actions in humans. Moreover, dutasteride reduced subsequent alcohol consumption in subjects classified as heavy drinkers (200). Likewise, men, who took finasteride for treatment of male pattern hair loss, reported a decrease in alcohol consumption, which was greater in those subjects who consumed the most alcohol (201). Taken together, these results further support the hypothesis that neuroactive steroids may mediate sensitivity to alcohol in humans.
Studies on the role of GABAergic neuroactive steroids in alcohol dependence have shown that chronic ethanol consumption in rats induces tolerance to the neurosteroidogenic effects of ethanol and ethanol-dependent rats have a blunted elevation in plasma and brain neuroactive steroid content, likely the result of a blunted HPA axis function (191). In ethanol-dependent C57BL/6J mice, cellular 3α,5α-THP immunoreactivity is increased in the CA3 hippocampus, but decreased in medial prefrontal cortex, ventral tegmental area, nucleus accumbens core, dorsolateral striatum and lateral amygdala (202). Likewise, 3α,5α-THP and 3α,5α-THDOC serum levels are decreased in human alcoholics during alcohol withdrawal and return to normal levels upon recovery (73). Overall, these findings suggest that chronic ethanol consumption leads to a dysregulation in neuroactive steroid biosynthesis, with a blunted neuroactive steroid tone that might attenuate ethanol sensitivity and thus contribute to alcohol dependence. Indeed, risk of alcohol dependence is associated with polymorphic variation in the enzymes 5α-reductase and 3α-hydroxysteroid dehydrogenase implicated in the conversion of progesterone and deoxycorticosterone to their neuroactive metabolites 3α,5α-THP and 3α,5α-THDOC, further providing indirect evidence that neuroactive steroids may contribute to alcohol sensitivity in humans (203).
Ethanol-induced elevations of GABAergic neuroactive steroids may protect against the risk for alcohol dependence (191). Diminished elevations of GABAergic neuroactive steroids following ethanol exposure would result in reduced sensitivity to the anxiolytic, sedative, anticonvulsant, cognitive-impairing and discriminative stimulus properties of ethanol. Reduced sensitivity to ethanol is associated with greater risk for the development of alcoholism; thus, restoration of ethanol sensitivity by re-establishing the neuroactive steroid tone in alcohol-dependent subjects may have therapeutic utility for prevention of alcohol consumption and/or relapse. In agreement, preclinical studies have found that administration of endogenous (epiallopregnanolone) or synthetic (3α,5β-20-oxo-pregnane-3-carboxylic acid) neuroactive steroids, as well as of the precursor pregnenolone, reduced ethanol self-administration in alcohol-preferring rats (204, 205). Likewise, recombinant adeno-associated serotype 2 vector mediated over-expression of P450 side chain cleavage (P450scc; the rate limiting enzyme in steroid synthesis) in the ventral tegmental area of alcohol preferring rats reduced ethanol reinforcement and consumption (161). This effect was long-lasting and was associated with an increase in 3α,5α-THP immunoreactivity in this brain area, suggesting that GABAergic neuroactive steroids may contribute to ethanol reinforcement. Indeed, P450scc over-expression in the nucleus accumbens, a brain region that plays a key role in ethanol reinforcement, but is insensitive to ethanol-induced neurosteroidogenesis (184), did not alter operant ethanol self-administration or 3α,5α-THP immunoreactivity (190), suggesting that the neuroactive steroid response to ethanol plays a role in the mechanisms that regulate its voluntary consumption. Increased 3α,5α-THP levels modulate the activity of neurons in the ventral tegmental area or influence ethanol's action upon these cells, thereby reducing ethanol reinforcement and consumption.
Thus, targeted modulation of neuroactive steroid synthesis through administration of neuroactive steroid precursors or through increased expression of specific neurosteroidogenic enzymes may represent a useful therapeutic approach for alcoholism, as well as for other neurological or psychiatric diseases associated with altered neurosteroidogenesis. Species differences in the neurosteroidogenic effects of ethanol may be the result of genetic diversity, which is also often observed across individuals of the same species. Thus, it will be important to consider genetic diversity in neuroactive steroid biosynthesis for their therapeutic actions.
Conclusions
The concept that neuroactive steroids may represent potential protective agents for different pathologies of the central and peripheral nervous system has been explored in detail in several experimental models. However, since steroid receptors are widely expressed in many tissues, a therapeutic strategy that uses exogenous neuroactive steroids could also evoke endocrine side effects. Therefore, alternative strategies, based on pharmacological agents or gene therapy tools, able to increase the synthesis of endogenous neuroactive steroids directly in the nervous system have been recently explored. Thus, the present review discussed the potential therapeutic activity elicited by targeting of steroidogenic enzymes, like 17β-HSD10, or P450scc, as well as that elicited by inducers of steroidogenesis, like for instance the TSPO and PXR. Indeed, even if the role of TSPO in steroid hormone biosynthesis has been recently challenged (108, 111, 206), the protective effects exerted by ligands of this mitochondrial receptor remain a promising field of research for neurodegeneration occurring in central and peripheral nervous system (207, 208). On this line of thinking, together with PXR, it is important to recall that also the activation of liver X receptor has been demonstrated to be an interesting pharmacological tool. Indeed, liver X receptor in adrenal glands modulates StAR (209), and its activation induces genes involved in cholesterol efflux, promoting cholesterol utilization (209). Moreover, as recently demonstrated in an experimental model of diabetes, activation of liver X receptor increases neuroactive steroid levels directly in the central (210) as well as the peripheral nervous system (211). In agreement, activation of liver X receptors exerts protective effects in diabetic peripheral neuropathy (211), global or focal cerebral ischemia (212), as well as in neurodegenerative diseases, such as multiple sclerosis, Alzheimer's and Parkinson's diseases (93, 213).
Altogether, the observations here reported indicate that the assessment of neurosteroidogenesis and of its physiological and pharmacological control may represent a promising topic of research that deserves further exploration in preclinical and clinical studies.
Acknowledgments
The data discussed in this review were presented in a round table organized during the 8th International Meeting on Steroids and Nervous System (Torino, February 14-18, 2015) with the support of the British Society for Neuroendocrinology and of Wiley & Sons publisher. We acknowledge financial support from NIH UO1-AA013641 and Sardinia Region (L.R. n3/2008) to P.P., JSPS KAKENHI Grant Number 26830038 to A.M.B., NIMH MH06769801 and RMH067698B, and NIGMS P20GM103395 to C.A.F., New York State Office for People With Developmental Disabilities to S.Y.Y., NIH UO1-AA020935 and the Bowles Center for Alcohol Studies to A.L.M., Fondazione Cavalieri Ottolenghi to G.C.P., Fondazione Cariplo (grant number 2012-0547) to R.C.M.
References
- 1.Paul SM, Purdy RH. Neuroactive steroids. FASEB J. 1992;6(6):2311–22. [PubMed] [Google Scholar]
- 2.Baulieu EE. Neurosteroids: a novel function of the brain. Psychoneuroendocrinology. 1998;23(8):963–87. doi: 10.1016/s0306-4530(98)00071-7. [DOI] [PubMed] [Google Scholar]
- 3.Charlier TD, Cornil CA, Patte-Mensah C, Meyer L, Mensah-Nyagan AG, Balthazart J. Local modulation of steroid action: rapid control of enzymatic activity. Front Neurosci. 2015;9:83. doi: 10.3389/fnins.2015.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agis-Balboa RC, Pinna G, Zhubi A, Maloku E, Veldic M, Costa E, Guidotti A. Characterization of brain neurons that express enzymes mediating neurosteroid biosynthesis. Proc Natl Acad Sci U S A. 2006;103(39):14602–7. doi: 10.1073/pnas.0606544103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belelli D, Lambert JJ. Neurosteroids: endogenous regulators of the GABAA receptor. Nat Rev Neurosci. 2005;6(7):565–75. doi: 10.1038/nrn1703. [DOI] [PubMed] [Google Scholar]
- 6.Carver CM, Reddy DS. Neurosteroid interactions with synaptic and extrasynaptic GABAA receptors: regulation of subunit plasticity, phasic and tonic inhibition, and neuronal network excitability. Psychopharmacology (Berl) 2013;230(2):151–88. doi: 10.1007/s00213-013-3276-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hosie AM, Wilkins ME, da Silva HM, Smart TG. Endogenous neurosteroids regulate GABAA receptors through two discrete transmembrane sites. Nature. 2006;444(7118):486–9. doi: 10.1038/nature05324. [DOI] [PubMed] [Google Scholar]
- 8.Rupprecht R. Neuroactive steroids: mechanisms of action and neuropsychopharmacological properties. Psychoneuroendocrinology. 2003;28(2):139–68. doi: 10.1016/s0306-4530(02)00064-1. [DOI] [PubMed] [Google Scholar]
- 9.Frye CA, Paris JJ, Walf AA, Rusconi JC. Effects and mechanisms of 3α,5α,-THP on emotion, motivation, and reward functions involving pregnane xenobiotic receptor. Front Neurosci. 2012;5:136. doi: 10.3389/fnins.2011.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith CC, Gibbs TT, Farb DH. Pregnenolone sulfate as a modulator of synaptic plasticity. Psychopharmacology (Berl) 2014;231(17):3537–56. doi: 10.1007/s00213-014-3643-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akk G, Covey DF, Evers AS, Steinbach JH, Zorumski CF, Mennerick S. Mechanisms of neurosteroid interactions with GABAA receptors. Pharmacol Ther. 2007;116(1):35–57. doi: 10.1016/j.pharmthera.2007.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bitran D, Hilvers RJ, Kellogg CK. Anxiolytic effects of 3α-hydroxy-5α[β]-pregnan-20-one: endogenous metabolites of progesterone that are active at the GABAA receptor. Brain Res. 1991;561(1):157–61. doi: 10.1016/0006-8993(91)90761-j. [DOI] [PubMed] [Google Scholar]
- 13.Khisti RT, Chopde CT, Jain SP. Antidepressant-like effect of the neurosteroid 3α-hydroxy-5α-pregnan-20-one in mice forced swim test. Pharmacol Biochem Behav. 2000;67(1):137–43. doi: 10.1016/s0091-3057(00)00300-2. [DOI] [PubMed] [Google Scholar]
- 14.Belelli D, Bolger MB, Gee KW. Anticonvulsant profile of the progesterone metabolite 5α-pregnan-3α-ol-20-one. Eur J Pharmacol. 1989;166(2):325–9. doi: 10.1016/0014-2999(89)90077-0. [DOI] [PubMed] [Google Scholar]
- 15.Hogskilde S, Wagner J, Carl P, Sorensen MB. Anaesthetic properties of pregnanolone emulsion. A comparison with alphaxolone/alphadolone, propofol, thiopentone and midazolam in a rat model. Anaesthesia. 1987;42(10):1045–50. doi: 10.1111/j.1365-2044.1987.tb05166.x. [DOI] [PubMed] [Google Scholar]
- 16.Kavaliers M, Wiebe JP. Analgesic effects of the progesterone metabolite, 3α-hydroxy-5α-pregnan-20-one, and possible modes of action in mice. Brain Res. 1987;415(2):393–8. doi: 10.1016/0006-8993(87)90228-9. [DOI] [PubMed] [Google Scholar]
- 17.Ladurelle N, Eychenne B, Denton D, Blair-West J, Schumacher M, Robel P, Baulieu E. Prolonged intracerebroventricular infusion of neurosteroids affects cognitive performances in the mouse. Brain Res. 2000;858(2):371–9. doi: 10.1016/s0006-8993(00)01953-3. [DOI] [PubMed] [Google Scholar]
- 18.Johansson IM, Birzniece V, Lindblad C, Olsson T, Backstrom T. Allopregnanolone inhibits learning in the Morris water maze. Brain Res. 2002;934(2):125–31. doi: 10.1016/s0006-8993(02)02414-9. [DOI] [PubMed] [Google Scholar]
- 19.Frye CA, Bayon LE, Pursnani NK, Purdy RH. The neurosteroids, progesterone and 3α,5α-THP, enhance sexual motivation, receptivity, and proceptivity in female rats. Brain Res. 1998;808(1):72–83. doi: 10.1016/s0006-8993(98)00764-1. [DOI] [PubMed] [Google Scholar]
- 20.Finn DA, Phillips TJ, Okorn DM, Chester JA, Cunningham CL. Rewarding effect of the neuroactive steroid 3α-hydroxy-5α-pregnan-20-one in mice. Pharmacol Biochem Behav. 1997;56(2):261–4. doi: 10.1016/s0091-3057(96)00218-3. [DOI] [PubMed] [Google Scholar]
- 21.Sinnott RS, Mark GP, Finn DA. Reinforcing effects of the neurosteroid allopregnanolone in rats. Pharmacol Biochem Behav. 2002;72(4):923–9. doi: 10.1016/s0091-3057(02)00776-1. [DOI] [PubMed] [Google Scholar]
- 22.Purdy RH, Valenzuela CF, Janak PH, Finn DA, Biggio G, Backstrom T. Neuroactive steroids and ethanol. Alcohol Clin Exp Res. 2005;29(7):1292–8. doi: 10.1097/01.alc.0000171486.97638.bc. [DOI] [PubMed] [Google Scholar]
- 23.Porcu P, Morrow AL. Divergent neuroactive steroid responses to stress and ethanol in rat and mouse strains: relevance for human studies. Psychopharmacology (Berl) 2014;231(17):3257–72. doi: 10.1007/s00213-014-3564-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anker JJ, Carroll ME. The role of progestins in the behavioral effects of cocaine and other drugs of abuse: human and animal research. Neurosci Biobehav Rev. 2010;35(2):315–33. doi: 10.1016/j.neubiorev.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.VanDoren MJ, Matthews DB, Janis GC, Grobin AC, Devaud LL, Morrow AL. Neuroactive steroid 3α-hydroxy-5α-pregnan-20-one modulates electrophysiological and behavioral actions of ethanol. J Neurosci. 2000;20(5):1982–9. doi: 10.1523/JNEUROSCI.20-05-01982.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Porcu P, Sogliano C, Cinus M, Purdy RH, Biggio G, Concas A. Nicotine-induced changes in cerebrocortical neuroactive steroids and plasma corticosterone concentrations in the rat. Pharmacol Biochem Behav. 2003;74(3):683–90. doi: 10.1016/s0091-3057(02)01065-1. [DOI] [PubMed] [Google Scholar]
- 27.Porcu P, Sogliano C, Ibba C, Piredda M, Tocco S, Marra C, Purdy RH, Biggio G, Concas A. Failure of gamma-hydroxybutyric acid both to increase neuroactive steroid concentrations in adrenalectomized-orchiectomized rats and to induce tolerance to its steroidogenic effect in intact animals. Brain Res. 2004;1012(1-2):160–8. doi: 10.1016/j.brainres.2004.03.059. [DOI] [PubMed] [Google Scholar]
- 28.Grobin AC, VanDoren MJ, Porrino LJ, Morrow AL. Cortical 3α-hydroxy-5α-pregnan-20-one levels after acute administration of Δ9-tetrahydrocannabinol, cocaine and morphine. Psychopharmacology (Berl) 2005;179(3):544–50. doi: 10.1007/s00213-004-2084-3. [DOI] [PubMed] [Google Scholar]
- 29.Concas A, Sogliano C, Porcu P, Marra C, Brundu A, Biggio G. Neurosteroids in nicotine and morphine dependence. Psychopharmacology (Berl) 2006;186(3):281–92. doi: 10.1007/s00213-005-0111-7. [DOI] [PubMed] [Google Scholar]
- 30.Vallee M, Vitiello S, Bellocchio L, Hebert-Chatelain E, Monlezun S, Martin-Garcia E, Kasanetz F, Baillie GL, Panin F, Cathala A, Roullot-Lacarriere V, Fabre S, Hurst DP, Lynch DL, Shore DM, Deroche-Gamonet V, Spampinato U, Revest JM, Maldonado R, Reggio PH, Ross RA, Marsicano G, Piazza PV. Pregnenolone can protect the brain from cannabis intoxication. Science. 2014;343(6166):94–8. doi: 10.1126/science.1243985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Djebaili M, Guo Q, Pettus EH, Hoffman SW, Stein DG. The neurosteroids progesterone and allopregnanolone reduce cell death, gliosis, and functional deficits after traumatic brain injury in rats. J Neurotrauma. 2005;22(1):106–18. doi: 10.1089/neu.2005.22.106. [DOI] [PubMed] [Google Scholar]
- 32.Labombarda F, Gonzalez S, Lima A, Roig P, Guennoun R, Schumacher M, De Nicola AF. Progesterone attenuates astro- and microgliosis and enhances oligodendrocyte differentiation following spinal cord injury. Exp Neurol. 2011;231(1):135–46. doi: 10.1016/j.expneurol.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 33.Panzica GC, Balthazart J, Frye CA, Garcia-Segura LM, Herbison AE, Mensah-Nyagan AG, McCarthy MM, Melcangi RC. Milestones on Steroids and the Nervous System: 10 years of basic and translational research. J Neuroendocrinol. 2012;24(1):1–15. doi: 10.1111/j.1365-2826.2011.02265.x. [DOI] [PubMed] [Google Scholar]
- 34.Melcangi RC, Giatti S, Pesaresi M, Calabrese D, Mitro N, Caruso D, Garcia-Segura LM. Role of neuroactive steroids in the peripheral nervous system. Front Endocrinol (Lausanne) 2011;2:104. doi: 10.3389/fendo.2011.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Giatti S, Boraso M, Melcangi RC, Viviani B. Neuroactive steroids, their metabolites, and neuroinflammation. J Mol Endocrinol. 2012;49(3):R125–34. doi: 10.1530/JME-12-0127. [DOI] [PubMed] [Google Scholar]
- 36.Sayeed I, Stein DG. Progesterone as a neuroprotective factor in traumatic and ischemic brain injury. Prog Brain Res. 2009;175:219–37. doi: 10.1016/S0079-6123(09)17515-5. [DOI] [PubMed] [Google Scholar]
- 37.Guennoun R, Labombarda F, Gonzalez Deniselle MC, Liere P, De Nicola AF, Schumacher M. Progesterone and allopregnanolone in the central nervous system: response to injury and implication for neuroprotection. J Steroid Biochem Mol Biol. 2015;146:48–61. doi: 10.1016/j.jsbmb.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 38.Ciriza I, Carrero P, Frye CA, Garcia-Segura LM. Reduced metabolites mediate neuroprotective effects of progesterone in the adult rat hippocampus. The synthetic progestin medroxyprogesterone acetate (Provera) is not neuroprotective. J Neurobiol. 2006;66(9):916–28. doi: 10.1002/neu.20293. [DOI] [PubMed] [Google Scholar]
- 39.Noorbakhsh F, Ellestad KK, Maingat F, Warren KG, Han MH, Steinman L, Baker GB, Power C. Impaired neurosteroid synthesis in multiple sclerosis. Brain. 2011;134(Pt 9):2703–21. doi: 10.1093/brain/awr200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giatti S, Caruso D, Boraso M, Abbiati F, Ballarini E, Calabrese D, Pesaresi M, Rigolio R, Santos-Galindo M, Viviani B, Cavaletti G, Garcia-Segura LM, Melcangi RC. Neuroprotective effects of progesterone in chronic experimental autoimmune encephalomyelitis. J Neuroendocrinol. 2012;24(6):851–61. doi: 10.1111/j.1365-2826.2012.02284.x. [DOI] [PubMed] [Google Scholar]
- 41.Giatti S, Rigolio R, Romano S, Mitro N, Viviani B, Cavaletti G, Caruso D, Garcia-Segura LM, Melcangi RC. Dihydrotestosterone as a protective agent in chronic experimental autoimmune encephalomyelitis. Neuroendocrinology. 2015;101(4):296–308. doi: 10.1159/000381064. [DOI] [PubMed] [Google Scholar]
- 42.Brinton RD. Neurosteroids as regenerative agents in the brain: therapeutic implications. Nat Rev Endocrinol. 2013;9(4):241–50. doi: 10.1038/nrendo.2013.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adeosun SO, Hou X, Jiao Y, Zheng B, Henry S, Hill R, He Z, Pani A, Kyle P, Ou X, Mosley T, Farley JM, Stockmeier C, Paul I, Bigler S, Brinton RD, Smeyne R, Wang JM. Allopregnanolone reinstates tyrosine hydroxylase immunoreactive neurons and motor performance in an MPTP-lesioned mouse model of Parkinson's disease. PLoS One. 2012;7(11):e50040. doi: 10.1371/journal.pone.0050040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Griffin LD, Gong W, Verot L, Mellon SH. Niemann-Pick type C disease involves disrupted neurosteroidogenesis and responds to allopregnanolone. Nat Med. 2004;10(7):704–11. doi: 10.1038/nm1073. [DOI] [PubMed] [Google Scholar]
- 45.Atif F, Yousuf S, Stein DG. Anti-tumor effects of progesterone in human glioblastoma multiforme: role of PI3K/Akt/mTOR signaling. J Steroid Biochem Mol Biol. 2015;146:62–73. doi: 10.1016/j.jsbmb.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 46.Purdy RH, Morrow AL, Moore PH, Jr, Paul SM. Stress-induced elevations of gamma-aminobutyric acid type A receptor-active steroids in the rat brain. Proc Natl Acad Sci U S A. 1991;88(10):4553–7. doi: 10.1073/pnas.88.10.4553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Girdler SS, Straneva PA, Light KC, Pedersen CA, Morrow AL. Allopregnanolone levels and reactivity to mental stress in premenstrual dysphoric disorder. Biol Psychiatry. 2001;49(9):788–97. doi: 10.1016/s0006-3223(00)01044-1. [DOI] [PubMed] [Google Scholar]
- 48.Gunn BG, Cunningham L, Mitchell SG, Swinny JD, Lambert JJ, Belelli D. GABAA receptor-acting neurosteroids: a role in the development and regulation of the stress response. Front Neuroendocrinol. 2015;36:28–48. doi: 10.1016/j.yfrne.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Grobin AC, Morrow AL. 3α-hydroxy-5α-pregnan-20-one levels and GABAA receptor-mediated 36Cl- flux across development in rat cerebral cortex. Brain Res Dev Brain Res. 2001;131(1-2):31–9. doi: 10.1016/s0165-3806(01)00242-5. [DOI] [PubMed] [Google Scholar]
- 50.Shen H, Gong QH, Aoki C, Yuan M, Ruderman Y, Dattilo M, Williams K, Smith SS. Reversal of neurosteroid effects at α4β2δ GABAA receptors triggers anxiety at puberty. Nat Neurosci. 2007;10(4):469–77. doi: 10.1038/nn1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Corpechot C, Collins BE, Carey MP, Tsouros A, Robel P, Fry JP. Brain neurosteroids during the mouse oestrous cycle. Brain Res. 1997;766(1-2):276–80. doi: 10.1016/s0006-8993(97)00749-x. [DOI] [PubMed] [Google Scholar]
- 52.Wang M, Seippel L, Purdy RH, Backstrom T. Relationship between symptom severity and steroid variation in women with premenstrual syndrome: study on serum pregnenolone, pregnenolone sulfate, 5α-pregnane-3,20-dione and 3α-hydroxy-5α-pregnan-20-one. J Clin Endocrinol Metab. 1996;81(3):1076–82. doi: 10.1210/jcem.81.3.8772579. [DOI] [PubMed] [Google Scholar]
- 53.Maguire JL, Stell BM, Rafizadeh M, Mody I. Ovarian cycle-linked changes in GABAA receptors mediating tonic inhibition alter seizure susceptibility and anxiety. Nat Neurosci. 2005;8(6):797–804. doi: 10.1038/nn1469. [DOI] [PubMed] [Google Scholar]
- 54.Concas A, Mostallino MC, Porcu P, Follesa P, Barbaccia ML, Trabucchi M, Purdy RH, Grisenti P, Biggio G. Role of brain allopregnanolone in the plasticity of γ-aminobutyric acid type A receptor in rat brain during pregnancy and after delivery. Proc Natl Acad Sci U S A. 1998;95(22):13284–9. doi: 10.1073/pnas.95.22.13284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gilbert Evans SE, Ross LE, Sellers EM, Purdy RH, Romach MK. 3α-reduced neuroactive steroids and their precursors during pregnancy and the postpartum period. Gynecol Endocrinol. 2005;21(5):268–79. doi: 10.1080/09513590500361747. [DOI] [PubMed] [Google Scholar]
- 56.Maguire J, Mody I. GABAAR plasticity during pregnancy: relevance to postpartum depression. Neuron. 2008;59(2):207–13. doi: 10.1016/j.neuron.2008.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sanna E, Mostallino MC, Murru L, Carta M, Talani G, Zucca S, Mura ML, Maciocco E, Biggio G. Changes in expression and function of extrasynaptic GABAA receptors in the rat hippocampus during pregnancy and after delivery. J Neurosci. 2009;29(6):1755–65. doi: 10.1523/JNEUROSCI.3684-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Smith SS, Shen H, Gong QH, Zhou X. Neurosteroid regulation of GABAA receptors: Focus on the α4 and δ subunits. Pharmacol Ther. 2007;116(1):58–76. doi: 10.1016/j.pharmthera.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Follesa P, Porcu P, Sogliano C, Cinus M, Biggio F, Mancuso L, Mostallino MC, Paoletti AM, Purdy RH, Biggio G, Concas A. Changes in GABAA receptor γ2 subunit gene expression induced by long-term administration of oral contraceptives in rats. Neuropharmacology. 2002;42(3):325–36. doi: 10.1016/s0028-3908(01)00187-3. [DOI] [PubMed] [Google Scholar]
- 60.Sassoè-Pognetto M, Follesa P, Panzanelli P, Perazzini AZ, Porcu P, Sogliano C, Cherchi C, Concas A. Fluctuations in brain concentrations of neurosteroids are not associated to changes in gephyrin levels. Brain Res. 2007;1169:1–8. doi: 10.1016/j.brainres.2007.06.057. [DOI] [PubMed] [Google Scholar]
- 61.Porcu P, Mostallino MC, Sogliano C, Santoru F, Berretti R, Concas A. Long-term administration with levonorgestrel decreases allopregnanolone levels and alters GABAA receptor subunit expression and anxiety-like behavior. Pharmacol Biochem Behav. 2012;102(2):366–72. doi: 10.1016/j.pbb.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 62.McCarthy MM. Estradiol and the developing brain. Physiol Rev. 2008;88(1):91–124. doi: 10.1152/physrev.00010.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Calza A, Sogliano C, Santoru F, Marra C, Angioni MM, Mostallino MC, Biggio G, Concas A. Neonatal exposure to estradiol in rats influences neuroactive steroid concentrations, GABAA receptor expression, and behavioral sensitivity to anxiolytic drugs. J Neurochem. 2010;113(5):1285–95. doi: 10.1111/j.1471-4159.2010.06696.x. [DOI] [PubMed] [Google Scholar]
- 64.Berretti R, Santoru F, Locci A, Sogliano C, Calza A, Choleris E, Porcu P, Concas A. Neonatal exposure to estradiol decreases hypothalamic allopregnanolone concentrations and alters agonistic and sexual but not affective behavior in adult female rats. Horm Behav. 2014;65(2):142–53. doi: 10.1016/j.yhbeh.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 65.Modol L, Casas C, Navarro X, Llido A, Vallee M, Pallares M, Darbra S. Neonatal finasteride administration alters hippocampal α4 and δ GABAAR subunits expression and behavioural responses to progesterone in adult rats. Int J Neuropsychopharmacol. 2014;17(2):259–73. doi: 10.1017/S1461145713000989. [DOI] [PubMed] [Google Scholar]
- 66.Abramian AM, Comenencia-Ortiz E, Modgil A, Vien TN, Nakamura Y, Moore YE, Maguire JL, Terunuma M, Davies PA, Moss SJ. Neurosteroids promote phosphorylation and membrane insertion of extrasynaptic GABAA receptors. Proc Natl Acad Sci U S A. 2014;111(19):7132–7. doi: 10.1073/pnas.1403285111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Melcangi RC, Panzica GC. Allopregnanolone: state of the art. Prog Neurobiol. 2014;113:1–5. doi: 10.1016/j.pneurobio.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 68.Schule C, Nothdurfter C, Rupprecht R. The role of allopregnanolone in depression and anxiety. Prog Neurobiol. 2014;113:79–87. doi: 10.1016/j.pneurobio.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 69.Girdler SS, Lindgren M, Porcu P, Rubinow DR, Johnson JL, Morrow AL. A history of depression in women is associated with an altered GABAergic neuroactive steroid profile. Psychoneuroendocrinology. 2012;37(4):543–53. doi: 10.1016/j.psyneuen.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Backstrom T, Bixo M, Johansson M, Nyberg S, Ossewaarde L, Ragagnin G, Savic I, Stromberg J, Timby E, van Broekhoven F, van Wingen G. Allopregnanolone and mood disorders. Prog Neurobiol. 2014;113:88–94. doi: 10.1016/j.pneurobio.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 71.Pinna G. Targeting neurosteroidogenesis as therapy for PTSD. Front Pharmacol. 2014;4:166. doi: 10.3389/fphar.2013.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Marx CE, Stevens RD, Shampine LJ, Uzunova V, Trost WT, Butterfield MI, Massing MW, Hamer RM, Morrow AL, Lieberman JA. Neuroactive steroids are altered in schizophrenia and bipolar disorder: relevance to pathophysiology and therapeutics. Neuropsychopharmacology. 2006;31(6):1249–63. doi: 10.1038/sj.npp.1300952. [DOI] [PubMed] [Google Scholar]
- 73.Romeo E, Brancati A, De Lorenzo A, Fucci P, Furnari C, Pompili E, Sasso GF, Spalletta G, Troisi A, Pasini A. Marked decrease of plasma neuroactive steroids during alcohol withdrawal. Clin Neuropharmacol. 1996;19(4):366–9. doi: 10.1097/00002826-199619040-00011. [DOI] [PubMed] [Google Scholar]
- 74.Porcu P, O'Buckley TK, Morrow AL, Adinoff B. Differential hypothalamic-pituitary-adrenal activation of the neuroactive steroids pregnenolone sulfate and deoxycorticosterone in healthy controls and alcohol-dependent subjects. Psychoneuroendocrinology. 2008;33(2):214–26. doi: 10.1016/j.psyneuen.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Serra M, Pisu MG, Littera M, Papi G, Sanna E, Tuveri F, Usala L, Purdy RH, Biggio G. Social isolation-induced decreases in both the abundance of neuroactive steroids and GABAA receptor function in rat brain. J Neurochem. 2000;75(2):732–40. doi: 10.1046/j.1471-4159.2000.0750732.x. [DOI] [PubMed] [Google Scholar]
- 76.Serra M, Sanna E, Mostallino MC, Biggio G. Social isolation stress and neuroactive steroids. Eur Neuropsychopharmacol. 2007;17(1):1–11. doi: 10.1016/j.euroneuro.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 77.Uzunova V, Ceci M, Kohler C, Uzunov DP, Wrynn AS. Region-specific dysregulation of allopregnanolone brain content in the olfactory bulbectomized rat model of depression. Brain Res. 2003;976(1):1–8. doi: 10.1016/s0006-8993(03)02577-0. [DOI] [PubMed] [Google Scholar]
- 78.Pibiri F, Nelson M, Guidotti A, Costa E, Pinna G. Decreased corticolimbic allopregnanolone expression during social isolation enhances contextual fear: A model relevant for posttraumatic stress disorder. Proc Natl Acad Sci U S A. 2008;105(14):5567–72. doi: 10.1073/pnas.0801853105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Caruso D, Abbiati F, Giatti S, Romano S, Fusco L, Cavaletti G, Melcangi RC. Patients treated for male pattern hair with finasteride show, after discontinuation of the drug, altered levels of neuroactive steroids in cerebrospinal fluid and plasma. J Steroid Biochem Mol Biol. 2015;146:74–9. doi: 10.1016/j.jsbmb.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 80.Marx CE, VanDoren MJ, Duncan GE, Lieberman JA, Morrow AL. Olanzapine and clozapine increase the GABAergic neuroactive steroid allopregnanolone in rodents. Neuropsychopharmacology. 2003;28(1):1–13. doi: 10.1038/sj.npp.1300015. [DOI] [PubMed] [Google Scholar]
- 81.Marx CE, Keefe RS, Buchanan RW, Hamer RM, Kilts JD, Bradford DW, Strauss JL, Naylor JC, Payne VM, Lieberman JA, Savitz AJ, Leimone LA, Dunn L, Porcu P, Morrow AL, Shampine LJ. Proof-of-concept trial with the neurosteroid pregnenolone targeting cognitive and negative symptoms in schizophrenia. Neuropsychopharmacology. 2009;34(8):1885–903. doi: 10.1038/npp.2009.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pieribone VA, Tsai J, Soufflet C, Rey E, Shaw K, Giller E, Dulac O. Clinical evaluation of ganaxolone in pediatric and adolescent patients with refractory epilepsy. Epilepsia. 2007;48(10):1870–4. doi: 10.1111/j.1528-1167.2007.01182.x. [DOI] [PubMed] [Google Scholar]
- 83.Herzog AG, Frye CA. Allopregnanolone levels and seizure frequency in progesterone-treated women with epilepsy. Neurology. 2014;83(4):345–8. doi: 10.1212/WNL.0000000000000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rogawski MA, Loya CM, Reddy K, Zolkowska D, Lossin C. Neuroactive steroids for the treatment of status epilepticus. Epilepsia. 2013;54(Suppl 6):93–8. doi: 10.1111/epi.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Caruso D, D'Intino G, Giatti S, Maschi O, Pesaresi M, Calabrese D, Garcia-Segura LM, Calza L, Melcangi RC. Sex-dimorphic changes in neuroactive steroid levels after chronic experimental autoimmune encephalomyelitis. J Neurochem. 2010;114(3):921–32. doi: 10.1111/j.1471-4159.2010.06825.x. [DOI] [PubMed] [Google Scholar]
- 86.Caruso D, Melis M, Fenu G, Giatti S, Romano S, Grimoldi M, Crippa D, Marrosu MG, Cavaletti G, Melcangi RC. Neuroactive steroid levels in plasma and cerebrospinal fluid of male multiple sclerosis patients. J Neurochem. 2014;130(4):591–7. doi: 10.1111/jnc.12745. [DOI] [PubMed] [Google Scholar]
- 87.Schumacher M, Weill-Engerer S, Liere P, Robert F, Franklin RJ, Garcia-Segura LM, Lambert JJ, Mayo W, Melcangi RC, Parducz A, Suter U, Carelli C, Baulieu EE, Akwa Y. Steroid hormones and neurosteroids in normal and pathological aging of the nervous system. Prog Neurobiol. 2003;71(1):3–29. doi: 10.1016/j.pneurobio.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 88.Caruso D, Barron AM, Brown MA, Abbiati F, Carrero P, Pike CJ, Garcia-Segura LM, Melcangi RC. Age-related changes in neuroactive steroid levels in 3xTg-AD mice. Neurobiol Aging. 2013;34(4):1080–9. doi: 10.1016/j.neurobiolaging.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Marx CE, Trost WT, Shampine LJ, Stevens RD, Hulette CM, Steffens DC, Ervin JF, Butterfield MI, Blazer DG, Massing MW, Lieberman JA. The neurosteroid allopregnanolone is reduced in prefrontal cortex in Alzheimer's disease. Biol Psychiatry. 2006;60(12):1287–94. doi: 10.1016/j.biopsych.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 90.di Michele F, Longone P, Romeo E, Lucchetti S, Brusa L, Pierantozzi M, Bassi A, Bernardi G, Stanzione P. Decreased plasma and cerebrospinal fluid content of neuroactive steroids in Parkinson's disease. Neurol Sci. 2003;24(3):172–3. doi: 10.1007/s10072-003-0115-1. [DOI] [PubMed] [Google Scholar]
- 91.Lopez-Rodriguez AB, Acaz-Fonseca E, Giatti S, Caruso D, Viveros MP, Melcangi RC, Garcia-Segura LM. Correlation of brain levels of progesterone and dehydroepiandrosterone with neurological recovery after traumatic brain injury in female mice. Psychoneuroendocrinology. 2015;56:1–11. doi: 10.1016/j.psyneuen.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 92.Pesaresi M, Maschi O, Giatti S, Garcia-Segura LM, Caruso D, Melcangi RC. Sex differences in neuroactive steroid levels in the nervous system of diabetic and non-diabetic rats. Horm Behav. 2010;57(1):46–55. doi: 10.1016/j.yhbeh.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 93.Melcangi RC, Giatti S, Calabrese D, Pesaresi M, Cermenati G, Mitro N, Viviani B, Garcia-Segura LM, Caruso D. Levels and actions of progesterone and its metabolites in the nervous system during physiological and pathological conditions. Prog Neurobiol. 2014;113:56–69. doi: 10.1016/j.pneurobio.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 94.Wang JM, Singh C, Liu L, Irwin RW, Chen S, Chung EJ, Thompson RF, Brinton RD. Allopregnanolone reverses neurogenic and cognitive deficits in mouse model of Alzheimer's disease. Proc Natl Acad Sci U S A. 2010;107(14):6498–503. doi: 10.1073/pnas.1001422107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Irwin RW, Brinton RD. Allopregnanolone as regenerative therapeutic for Alzheimer's disease: translational development and clinical promise. Prog Neurobiol. 2014;113:40–55. doi: 10.1016/j.pneurobio.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Leonelli E, Bianchi R, Cavaletti G, Caruso D, Crippa D, Garcia-Segura LM, Lauria G, Magnaghi V, Roglio I, Melcangi RC. Progesterone and its derivatives are neuroprotective agents in experimental diabetic neuropathy: a multimodal analysis. Neuroscience. 2007;144(4):1293–304. doi: 10.1016/j.neuroscience.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 97.Liu A, Margaill I, Zhang S, Labombarda F, Coqueran B, Delespierre B, Liere P, Marchand-Leroux C, O'Malley BW, Lydon JP, De Nicola AF, Sitruk-Ware R, Mattern C, Plotkine M, Schumacher M, Guennoun R. Progesterone receptors: a key for neuroprotection in experimental stroke. Endocrinology. 2012;153(8):3747–57. doi: 10.1210/en.2012-1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Timby E, Balgard M, Nyberg S, Spigset O, Andersson A, Porankiewicz-Asplund J, Purdy RH, Zhu D, Backstrom T, Poromaa IS. Pharmacokinetic and behavioral effects of allopregnanolone in healthy women. Psychopharmacology (Berl) 2006;186(3):414–24. doi: 10.1007/s00213-005-0148-7. [DOI] [PubMed] [Google Scholar]
- 99.Irwin RW, Solinsky CM, Brinton RD. Frontiers in therapeutic development of allopregnanolone for Alzheimer's disease and other neurological disorders. Front Cell Neurosci. 2014;8:203. doi: 10.3389/fncel.2014.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhu D, Birzniece V, Backstrom T, Wahlstrom G. Dynamic aspects of acute tolerance to allopregnanolone evaluated using anaesthesia threshold in male rats. Br J Anaesth. 2004;93(4):560–7. doi: 10.1093/bja/aeh233. [DOI] [PubMed] [Google Scholar]
- 101.Kask K, Backstrom T, Nilsson LG, Sundstrom-Poromaa I. Allopregnanolone impairs episodic memory in healthy women. Psychopharmacology (Berl) 2008;199(2):161–8. doi: 10.1007/s00213-008-1150-7. [DOI] [PubMed] [Google Scholar]
- 102.Grant KA, Helms CM, Rogers LS, Purdy RH. Neuroactive steroid stereospecificity of ethanol-like discriminative stimulus effects in monkeys. J Pharmacol Exp Ther. 2008;326(1):354–61. doi: 10.1124/jpet.108.137315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wang HJ, Fan J, Papadopoulos V. Translocator protein (Tspo) gene promoter-driven green fluorescent protein synthesis in transgenic mice: an in vivo model to study Tspo transcription. Cell Tissue Res. 2012;350(2):261–75. doi: 10.1007/s00441-012-1478-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rupprecht R, Papadopoulos V, Rammes G, Baghai TC, Fan J, Akula N, Groyer G, Adams D, Schumacher M. Translocator protein (18 kDa) (TSPO) as a therapeutic target for neurological and psychiatric disorders. Nat Rev Drug Discov. 2010;9(12):971–88. doi: 10.1038/nrd3295. [DOI] [PubMed] [Google Scholar]
- 105.Costa E, Guidotti A. Diazepam binding inhibitor (DBI): a peptide with multiple biological actions. Life Sci. 1991;49(5):325–44. doi: 10.1016/0024-3205(91)90440-m. [DOI] [PubMed] [Google Scholar]
- 106.Do-Rego JL, Mensah-Nyagan AG, Feuilloley M, Ferrara P, Pelletier G, Vaudry H. The endozepine triakontatetraneuropeptide diazepam-binding inhibitor [17-50] stimulates neurosteroid biosynthesis in the frog hypothalamus. Neuroscience. 1998;83(2):555–70. doi: 10.1016/s0306-4522(97)00362-x. [DOI] [PubMed] [Google Scholar]
- 107.Tu LN, Morohaku K, Manna PR, Pelton SH, Butler WR, Stocco DM, Selvaraj V. Peripheral benzodiazepine receptor/translocator protein global knock-out mice are viable with no effects on steroid hormone biosynthesis. J Biol Chem. 2014;289(40):27444–54. doi: 10.1074/jbc.M114.578286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Morohaku K, Pelton SH, Daugherty DJ, Butler WR, Deng W, Selvaraj V. Translocator protein/peripheral benzodiazepine receptor is not required for steroid hormone biosynthesis. Endocrinology. 2014;155(1):89–97. doi: 10.1210/en.2013-1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Banati RB, Middleton RJ, Chan R, Hatty CR, Kam WW, Quin C, Graeber MB, Parmar A, Zahra D, Callaghan P, Fok S, Howell NR, Gregoire M, Szabo A, Pham T, Davis E, Liu GJ. Positron emission tomography and functional characterization of a complete PBR/TSPO knockout. Nat Commun. 2014;5:5452. doi: 10.1038/ncomms6452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fan J, Campioli E, Midzak A, Culty M, Papadopoulos V. Conditional steroidogenic cell-targeted deletion of TSPO unveils a crucial role in viability and hormone-dependent steroid formation. Proc Natl Acad Sci U S A. 2015;112(23):7261–6. doi: 10.1073/pnas.1502670112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gut P, Zweckstetter M, Banati RB. Lost in translocation: the functions of the 18-kD translocator protein. Trends Endocrinol Metab. 2015;26(7):349–56. doi: 10.1016/j.tem.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bitran D, Foley M, Audette D, Leslie N, Frye CA. Activation of peripheral mitochondrial benzodiazepine receptors in the hippocampus stimulates allopregnanolone synthesis and produces anxiolytic-like effects in the rat. Psychopharmacology (Berl) 2000;151(1):64–71. doi: 10.1007/s002130000471. [DOI] [PubMed] [Google Scholar]
- 113.Romeo E, Cavallaro S, Korneyev A, Kozikowski AP, Ma D, Polo A, Costa E, Guidotti A. Stimulation of brain steroidogenesis by 2-aryl-indole-3-acetamide derivatives acting at the mitochondrial diazepam-binding inhibitor receptor complex. J Pharmacol Exp Ther. 1993;267(1):462–71. [PubMed] [Google Scholar]
- 114.Serra M, Madau P, Chessa MF, Caddeo M, Sanna E, Trapani G, Franco M, Liso G, Purdy RH, Barbaccia ML, Biggio G. 2-Phenyl-imidazo[1,2-a]pyridine derivatives as ligands for peripheral benzodiazepine receptors: stimulation of neurosteroid synthesis and anticonflict action in rats. Br J Pharmacol. 1999;127(1):177–87. doi: 10.1038/sj.bjp.0702530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Verleye M, Akwa Y, Liere P, Ladurelle N, Pianos A, Eychenne B, Schumacher M, Gillardin JM. The anxiolytic etifoxine activates the peripheral benzodiazepine receptor and increases the neurosteroid levels in rat brain. Pharmacol Biochem Behav. 2005;82(4):712–20. doi: 10.1016/j.pbb.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 116.Barron AM, Garcia-Segura LM, Caruso D, Jayaraman A, Lee JW, Melcangi RC, Pike CJ. Ligand for translocator protein reverses pathology in a mouse model of Alzheimer's disease. J Neurosci. 2013;33(20):8891–7. doi: 10.1523/JNEUROSCI.1350-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rupprecht R, Rammes G, Eser D, Baghai TC, Schule C, Nothdurfter C, Troxler T, Gentsch C, Kalkman HO, Chaperon F, Uzunov V, McAllister KH, Bertaina-Anglade V, La Rochelle CD, Tuerck D, Floesser A, Kiese B, Schumacher M, Landgraf R, Holsboer F, Kucher K. Translocator protein (18 kD) as target for anxiolytics without benzodiazepine-like side effects. Science. 2009;325(5939):490–3. doi: 10.1126/science.1175055. [DOI] [PubMed] [Google Scholar]
- 118.Korneyev A, Pan BS, Polo A, Romeo E, Guidotti A, Costa E. Stimulation of brain pregnenolone synthesis by mitochondrial diazepam binding inhibitor receptor ligands in vivo. J Neurochem. 1993;61(4):1515–24. doi: 10.1111/j.1471-4159.1993.tb13647.x. [DOI] [PubMed] [Google Scholar]
- 119.Barron AM, Pike CJ. Sex hormones, aging, and Alzheimer's disease. Front Biosci (Elite Ed) 2012;4:976–97. doi: 10.2741/e434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Papadopoulos V, Lecanu L. Translocator protein (18 kDa) TSPO: an emerging therapeutic target in neurotrauma. Exp Neurol. 2009;219(1):53–7. doi: 10.1016/j.expneurol.2009.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zimmer ER, Leuzy A, Benedet AL, Breitner J, Gauthier S, Rosa-Neto P. Tracking neuroinflammation in Alzheimer's disease: the role of positron emission tomography imaging. J Neuroinflammation. 2014;11:120. doi: 10.1186/1742-2094-11-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Li F, Liu J, Valls L, Hiser C, Ferguson-Miller S. Identification of a key cholesterol binding enhancement motif in translocator protein 18 kDa. Biochemistry. 2015;54(7):1441–3. doi: 10.1021/bi5015453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jaremko L, Jaremko M, Giller K, Becker S, Zweckstetter M. Structure of the mitochondrial translocator protein in complex with a diagnostic ligand. Science. 2014;343(6177):1363–6. doi: 10.1126/science.1248725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Li F, Liu J, Zheng Y, Garavito RM, Ferguson-Miller S. Protein structure. Crystal structures of translocator protein (TSPO) and mutant mimic of a human polymorphism. Science. 2015;347(6221):555–8. doi: 10.1126/science.1260590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Costa B, Pini S, Gabelloni P, Da Pozzo E, Abelli M, Lari L, Preve M, Lucacchini A, Cassano GB, Martini C. The spontaneous Ala147Thr amino acid substitution within the translocator protein influences pregnenolone production in lymphomonocytes of healthy individuals. Endocrinology. 2009;150(12):5438–45. doi: 10.1210/en.2009-0752. [DOI] [PubMed] [Google Scholar]
- 126.Banati RB, Gehrmann J, Czech C, Monning U, Jones LL, Konig G, Beyreuther K, Kreutzberg GW. Early and rapid de novo synthesis of Alzheimer beta A4-amyloid precursor protein (APP) in activated microglia. Glia. 1993;9(3):199–210. doi: 10.1002/glia.440090305. [DOI] [PubMed] [Google Scholar]
- 127.Veiga S, Azcoitia I, Garcia-Segura LM. Ro5-4864, a peripheral benzodiazepine receptor ligand, reduces reactive gliosis and protects hippocampal hilar neurons from kainic acid excitotoxicity. J Neurosci Res. 2005;80(1):129–37. doi: 10.1002/jnr.20430. [DOI] [PubMed] [Google Scholar]
- 128.Veiga S, Carrero P, Pernia O, Azcoitia I, Garcia-Segura LM. Translocator protein 18 kDa is involved in the regulation of reactive gliosis. Glia. 2007;55(14):1426–36. doi: 10.1002/glia.20558. [DOI] [PubMed] [Google Scholar]
- 129.Choi HB, Khoo C, Ryu JK, van Breemen E, Kim SU, McLarnon JG. Inhibition of lipopolysaccharide-induced cyclooxygenase-2, tumor necrosis factor-alpha and [Ca2+]i responses in human microglia by the peripheral benzodiazepine receptor ligand PK11195. J Neurochem. 2002;83(3):546–55. doi: 10.1046/j.1471-4159.2002.01122.x. [DOI] [PubMed] [Google Scholar]
- 130.Szekely CA, Thorne JE, Zandi PP, Ek M, Messias E, Breitner JC, Goodman SN. Nonsteroidal anti-inflammatory drugs for the prevention of Alzheimer's disease: a systematic review. Neuroepidemiology. 2004;23(4):159–69. doi: 10.1159/000078501. [DOI] [PubMed] [Google Scholar]
- 131.Nothdurfter C, Rammes G, Baghai TC, Schule C, Schumacher M, Papadopoulos V, Rupprecht R. Translocator protein (18 kDa) as a target for novel anxiolytics with a favourable side-effect profile. J Neuroendocrinol. 2012;24(1):82–92. doi: 10.1111/j.1365-2826.2011.02166.x. [DOI] [PubMed] [Google Scholar]
- 132.Kita A, Kinoshita T, Kohayakawa H, Furukawa K, Akaike A. Lack of tolerance to anxiolysis and withdrawal symptoms in mice repeatedly treated with AC-5216, a selective TSPO ligand. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(6):1040–5. doi: 10.1016/j.pnpbp.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 133.Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA. 2005;293(5):596–608. doi: 10.1001/jama.293.5.596. [DOI] [PubMed] [Google Scholar]
- 134.Do Rego JL, Seong JY, Burel D, Leprince J, Vaudry D, Luu-The V, Tonon MC, Tsutsui K, Pelletier G, Vaudry H. Regulation of neurosteroid biosynthesis by neurotransmitters and neuropeptides. Front Endocrinol (Lausanne) 2012;3:4. doi: 10.3389/fendo.2012.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.King SR, Manna PR, Ishii T, Syapin PJ, Ginsberg SD, Wilson K, Walsh LP, Parker KL, Stocco DM, Smith RG, Lamb DJ. An essential component in steroid synthesis, the steroidogenic acute regulatory protein, is expressed in discrete regions of the brain. J Neurosci. 2002;22(24):10613–20. doi: 10.1523/JNEUROSCI.22-24-10613.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mellon SH, Deschepper CF. Neurosteroid biosynthesis: genes for adrenal steroidogenic enzymes are expressed in the brain. Brain Res. 1993;629(2):283–92. doi: 10.1016/0006-8993(93)91332-m. [DOI] [PubMed] [Google Scholar]
- 137.Papadopoulos V, Baraldi M, Guilarte TR, Knudsen TB, Lacapere JJ, Lindemann P, Norenberg MD, Nutt D, Weizman A, Zhang MR, Gavish M. Translocator protein (18kDa): new nomenclature for the peripheral-type benzodiazepine receptor based on its structure and molecular function. Trends Pharmacol Sci. 2006;27(8):402–9. doi: 10.1016/j.tips.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 138.Frye CA. Novel substrates for, and sources of, progestogens for reproduction. J Neuroendocrinol. 2011;23(11):961–73. doi: 10.1111/j.1365-2826.2011.02180.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bertilsson G, Heidrich J, Svensson K, Asman M, Jendeberg L, Sydow-Backman M, Ohlsson R, Postlind H, Blomquist P, Berkenstam A. Identification of a human nuclear receptor defines a new signaling pathway for CYP3A induction. Proc Natl Acad Sci U S A. 1998;95(21):12208–13. doi: 10.1073/pnas.95.21.12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kliewer SA, Moore JT, Wade L, Staudinger JL, Watson MA, Jones SA, McKee DD, Oliver BB, Willson TM, Zetterstrom RH, Perlmann T, Lehmann JM. An orphan nuclear receptor activated by pregnanes defines a novel steroid signaling pathway. Cell. 1998;92(1):73–82. doi: 10.1016/s0092-8674(00)80900-9. [DOI] [PubMed] [Google Scholar]
- 141.Lamba V, Yasuda K, Lamba JK, Assem M, Davila J, Strom S, Schuetz EG. PXR (NR1I2): splice variants in human tissues, including brain, and identification of neurosteroids and nicotine as PXR activators. Toxicol Appl Pharmacol. 2004;199(3):251–65. doi: 10.1016/j.taap.2003.12.027. [DOI] [PubMed] [Google Scholar]
- 142.Dutheil F, Dauchy S, Diry M, Sazdovitch V, Cloarec O, Mellottee L, Bieche I, Ingelman-Sundberg M, Flinois JP, de Waziers I, Beaune P, Decleves X, Duyckaerts C, Loriot MA. Xenobiotic-metabolizing enzymes and transporters in the normal human brain: regional and cellular mapping as a basis for putative roles in cerebral function. Drug Metab Dispos. 2009;37(7):1528–38. doi: 10.1124/dmd.109.027011. [DOI] [PubMed] [Google Scholar]
- 143.Frye CA, Koonce CJ, Walf AA. Pregnane xenobiotic receptors and membrane progestin receptors: role in neurosteroid-mediated motivated behaviours. J Neuroendocrinol. 2013;25(11):1002–11. doi: 10.1111/jne.12105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Frye CA, Koonce CJ, Walf AA. Involvement of pregnane xenobiotic receptor in mating-induced allopregnanolone formation in the midbrain and hippocampus and brain-derived neurotrophic factor in the hippocampus among female rats. Psychopharmacology (Berl) 2014;231(17):3375–90. doi: 10.1007/s00213-014-3569-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Marini S, Nannelli A, Sodini D, Dragoni S, Valoti M, Longo V, Gervasi PG. Expression, microsomal and mitochondrial activities of cytochrome P450 enzymes in brain regions from control and phenobarbital-treated rabbits. Life Sci. 2007;80(10):910–7. doi: 10.1016/j.lfs.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 146.Frye CA, Koonce CJ, Walf AA, Rusconi JC. Motivated behaviors and levels of 3α,5α-THP in the midbrain are attenuated by knocking down expression of pregnane xenobiotic receptor in the midbrain ventral tegmental area of proestrous rats. J Sex Med. 2013;10(7):1692–706. doi: 10.1111/jsm.12173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Frye CA, Koonce CJ, Walf AA. Novel receptor targets for production and action of allopregnanolone in the central nervous system: a focus on pregnane xenobiotic receptor. Front Cell Neurosci. 2014;8:106. doi: 10.3389/fncel.2014.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Frye CA, Koonce CJ, Walf AA. Role of pregnane xenobiotic receptor in the midbrain ventral tegmental area for estradiol- and 3α,5α-THP-facilitated lordosis of female rats. Psychopharmacology (Berl) 2014;231(17):3365–74. doi: 10.1007/s00213-013-3406-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Frye CA, Koonce CJ, Walf AA. The pregnane xenobiotic receptor, a prominent liver factor, has actions in the midbrain for neurosteroid synthesis and behavioral/neural plasticity of female rats. Front Syst Neurosci. 2014;8:60. doi: 10.3389/fnsys.2014.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Walf AA, Rhodes ME, Frye CA. Ovarian steroids enhance object recognition in naturally cycling and ovariectomized, hormone-primed rats. Neurobiol Learn Mem. 2006;86(1):35–46. doi: 10.1016/j.nlm.2006.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Frye CA, Walf AA. Progesterone enhances learning and memory of aged wildtype and progestin receptor knockout mice. Neurosci Lett. 2010;472(1):38–42. doi: 10.1016/j.neulet.2010.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Frye CA, Koonce CJ, Walf AA. Progesterone, compared to medroxyprogesterone acetate, to C57BL/6, but not 5α-reductase mutant, mice enhances object recognition and placement memory and is associated with higher BDNF levels in the hippocampus and cortex. Neurosci Lett. 2013;551:53–7. doi: 10.1016/j.neulet.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Paris JJ, Walf AA, Frye CA., II Cognitive performance of middle-aged female rats is influenced by capacity to metabolize progesterone in the prefrontal cortex and hippocampus. Brain Res. 2011;1379:149–63. doi: 10.1016/j.brainres.2010.10.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Smith CD, Wekstein DR, Markesbery WR, Frye CA. 3α,5α-THP: a potential plasma neurosteroid biomarker in Alzheimer's disease and perhaps non-Alzheimer's dementia. Psychopharmacology (Berl) 2006;186(3):481–5. doi: 10.1007/s00213-005-0186-1. [DOI] [PubMed] [Google Scholar]
- 155.Borchelt DR, Ratovitski T, van Lare J, Lee MK, Gonzales V, Jenkins NA, Copeland NG, Price DL, Sisodia SS. Accelerated amyloid deposition in the brains of transgenic mice coexpressing mutant presenilin 1 and amyloid precursor proteins. Neuron. 1997;19(4):939–45. doi: 10.1016/s0896-6273(00)80974-5. [DOI] [PubMed] [Google Scholar]
- 156.Frye CA, Walf AA. Effects of progesterone administration and APPswe+PSEN1Deltae9 mutation for cognitive performance of mid-aged mice. Neurobiol Learn Mem. 2008;89(1):17–26. doi: 10.1016/j.nlm.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 157.Frye CA, Walf AA. Progesterone reduces depression-like behavior in a murine model of Alzheimer's Disease. Age (Dordr) 2009;31(2):143–53. doi: 10.1007/s11357-009-9091-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Mandrekar-Colucci S, Karlo JC, Landreth GE. Mechanisms underlying the rapid peroxisome proliferator-activated receptor-γ-mediated amyloid clearance and reversal of cognitive deficits in a murine model of Alzheimer's disease. J Neurosci. 2012;32(30):10117–28. doi: 10.1523/JNEUROSCI.5268-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wang K, Wan YJ. Nuclear receptors and inflammatory diseases. Exp Biol Med (Maywood) 2008;233(5):496–506. doi: 10.3181/0708-MR-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Miller WL. Steroid hormone synthesis in mitochondria. Mol Cell Endocrinol. 2013;379(1-2):62–73. doi: 10.1016/j.mce.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 161.Cook JB, Werner DF, Maldonado-Devincci AM, Leonard MN, Fisher KR, O'Buckley TK, Porcu P, McCown TJ, Besheer J, Hodge CW, Morrow AL. Overexpression of the steroidogenic enzyme cytochrome P450 side chain cleavage in the ventral tegmental area increases 3α,5α-THP and reduces long-term operant ethanol self-administration. J Neurosci. 2014;34(17):5824–34. doi: 10.1523/JNEUROSCI.4733-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Pradhan DS, Lau LY, Schmidt KL, Soma KK. 3β-HSD in songbird brain: subcellular localization and rapid regulation by estradiol. J Neurochem. 2010;115(3):667–75. doi: 10.1111/j.1471-4159.2010.06954.x. [DOI] [PubMed] [Google Scholar]
- 163.He XY, Wegiel J, Yang YZ, Pullarkat R, Schulz H, Yang SY. Type 10 17beta-hydroxysteroid dehydrogenase catalyzing the oxidation of steroid modulators of gamma-aminobutyric acid type A receptors. Mol Cell Endocrinol. 2005;229(1-2):111–7. doi: 10.1016/j.mce.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 164.He XY, Wegiel J, Yang SY. Intracellular oxidation of allopregnanolone by human brain type 10 17β-hydroxysteroid dehydrogenase. Brain Res. 2005;1040(1-2):29–35. doi: 10.1016/j.brainres.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 165.Yang SY, He XY, Schulz H. Multiple functions of type 10 17β-hydroxysteroid dehydrogenase. Trends Endocrinol Metab. 2005;16(4):167–75. doi: 10.1016/j.tem.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 166.Yang SY, He XY, Miller D. HSD17B10: a gene involved in cognitive function through metabolism of isoleucine and neuroactive steroids. Mol Genet Metab. 2007;92(1-2):36–42. doi: 10.1016/j.ymgme.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 167.Yang SY, He XY, Miller D. Hydroxysteroid (17β) dehydrogenase X in human health and disease. Mol Cell Endocrinol. 2011;343(1-2):1–6. doi: 10.1016/j.mce.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 168.Yang SY, He XY, Isaacs C, Dobkin C, Miller D, Philipp M. Roles of 17β-hydroxysteroid dehydrogenase type 10 in neurodegenerative disorders. J Steroid Biochem Mol Biol. 2014;143:460–72. doi: 10.1016/j.jsbmb.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 169.He XY, Yang YZ, Schulz H, Yang SY. Intrinsic alcohol dehydrogenase and hydroxysteroid dehydrogenase activities of human mitochondrial short-chain L-3-hydroxyacyl-CoA dehydrogenase. Biochem J. 2000;345(Pt 1):139–43. [PMC free article] [PubMed] [Google Scholar]
- 170.He XY, Merz G, Mehta P, Schulz H, Yang SY. Human brain short chain L-3-hydroxyacyl coenzyme A dehydrogenase is a single-domain multifunctional enzyme. Characterization of a novel 17β-hydroxysteroid dehydrogenase. J Biol Chem. 1999;274(21):15014–9. doi: 10.1074/jbc.274.21.15014. [DOI] [PubMed] [Google Scholar]
- 171.He XY, Merz G, Yang YZ, Mehta P, Schulz H, Yang SY. Characterization and localization of human type10 17β-hydroxysteroid dehydrogenase. Eur J Biochem. 2001;268(18):4899–907. doi: 10.1046/j.0014-2956.2001.02421.2421.x. [DOI] [PubMed] [Google Scholar]
- 172.He XY, Yang YZ, Peehl DM, Lauderdale A, Schulz H, Yang SY. Oxidative 3α-hydroxysteroid dehydrogenase activity of human type 10 17β-hydroxysteroid dehydrogenase. J Steroid Biochem Mol Biol. 2003;87(2-3):191–8. doi: 10.1016/j.jsbmb.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 173.He XY, Merz G, Yang YZ, Pullakart R, Mehta P, Schulz H, Yang SY. Function of human brain short chain L-3-hydroxyacyl coenzyme A dehydrogenase in androgen metabolism. Biochim Biophys Acta. 2000;1484(2-3):267–77. doi: 10.1016/s1388-1981(00)00014-7. [DOI] [PubMed] [Google Scholar]
- 174.Yang SY, He XY, Olpin SE, Sutton VR, McMenamin J, Philipp M, Denman RB, Malik M. Mental retardation linked to mutations in the HSD17B10 gene interfering with neurosteroid and isoleucine metabolism. Proc Natl Acad Sci U S A. 2009;106(35):14820–4. doi: 10.1073/pnas.0902377106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Seaver LH, He XY, Abe K, Cowan T, Enns GM, Sweetman L, Philipp M, Lee S, Malik M, Yang SY. A novel mutation in the HSD17B10 gene of a 10-year-old boy with refractory epilepsy, choreoathetosis and learning disability. PLoS One. 2011;6(11):e27348. doi: 10.1371/journal.pone.0027348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Yang SY, Dobkin C, He XY, Philipp M, Brown WT. A 5-methylcytosine hotspot responsible for the prevalent HSD17B10 mutation. Gene. 2013;515(2):380–4. doi: 10.1016/j.gene.2012.12.064. [DOI] [PubMed] [Google Scholar]
- 177.Yang SY, He XY. Role of type 10 17β-hydroxysteroid dehydrogenase in the pathogenesis of Alzheimer's disease. Adv Exp Med Biol. 2001;487:101–10. doi: 10.1007/978-1-4615-1249-3_8. [DOI] [PubMed] [Google Scholar]
- 178.Jazbutyte V, Kehl F, Neyses L, Pelzer T. Estrogen receptor alpha interacts with 17β-hydroxysteroid dehydrogenase type 10 in mitochondria. Biochem Biophys Res Commun. 2009;384(4):450–4. doi: 10.1016/j.bbrc.2009.04.139. [DOI] [PubMed] [Google Scholar]
- 179.He XY, Wen GY, Merz G, Lin D, Yang YZ, Mehta P, Schulz H, Yang SY. Abundant type 10 17β-hydroxysteroid dehydrogenase in the hippocampus of mouse Alzheimer's disease model. Brain Res Mol Brain Res. 2002;99(1):46–53. doi: 10.1016/s0169-328x(02)00102-x. [DOI] [PubMed] [Google Scholar]
- 180.Grimm A, Schmitt K, Lang UE, Mensah-Nyagan AG, Eckert A. Improvement of neuronal bioenergetics by neurosteroids: implications for age-related neurodegenerative disorders. Biochim Biophys Acta. 2014;1842(12 Pt A):2427–38. doi: 10.1016/j.bbadis.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 181.Yang SY, He XY, Dobkin C, Isaacs C, Brown WT. Mental retardation and isoleucine metabolism. In: Rajendram R, Preedy VR, Patel VB, editors. Branched Chain Amino Acids in Clinical Nutrition: Volume I, Nutrition and Health. New York: Springer; 2015. pp. 157–70. [Google Scholar]
- 182.Porcu P, O'Buckley TK, Alward SE, Song SC, Grant KA, de Wit H, Morrow AL. Differential effects of ethanol on serum GABAergic 3α,5α/3α,5β neuroactive steroids in mice, rats, cynomolgus monkeys, and humans. Alcohol Clin Exp Res. 2010;34(3):432–42. doi: 10.1111/j.1530-0277.2009.01123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Barbaccia ML, Affricano D, Trabucchi M, Purdy RH, Colombo G, Agabio R, Gessa GL. Ethanol markedly increases “GABAergic” neurosteroids in alcohol-preferring rats. Eur J Pharmacol. 1999;384(2-3):R1–2. doi: 10.1016/s0014-2999(99)00678-0. [DOI] [PubMed] [Google Scholar]
- 184.Cook JB, Dumitru AM, O'Buckley TK, Morrow AL. Ethanol administration produces divergent changes in GABAergic neuroactive steroid immunohistochemistry in the rat brain. Alcohol Clin Exp Res. 2014;38(1):90–9. doi: 10.1111/acer.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Khisti RT, VanDoren MJ, O'Buckley T, Morrow AL. Neuroactive steroid 3α-hydroxy-5α-pregnan-20-one modulates ethanol-induced loss of righting reflex in rats. Brain Res. 2003;980(2):255–65. doi: 10.1016/s0006-8993(03)02978-0. [DOI] [PubMed] [Google Scholar]
- 186.O'Dell LE, Alomary AA, Vallee M, Koob GF, Fitzgerald RL, Purdy RH. Ethanol-induced increases in neuroactive steroids in the rat brain and plasma are absent in adrenalectomized and gonadectomized rats. Eur J Pharmacol. 2004;484(2-3):241–7. doi: 10.1016/j.ejphar.2003.11.031. [DOI] [PubMed] [Google Scholar]
- 187.Boyd KN, Kumar S, O'Buckley TK, Porcu P, Morrow AL. Ethanol induction of steroidogenesis in rat adrenal and brain is dependent upon pituitary ACTH release and de novo adrenal StAR synthesis. J Neurochem. 2010;112(3):784–96. doi: 10.1111/j.1471-4159.2009.06509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Sanna E, Talani G, Busonero F, Pisu MG, Purdy RH, Serra M, Biggio G. Brain steroidogenesis mediates ethanol modulation of GABAA receptor activity in rat hippocampus. J Neurosci. 2004;24(29):6521–30. doi: 10.1523/JNEUROSCI.0075-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Tokuda K, Izumi Y, Zorumski CF. Ethanol enhances neurosteroidogenesis in hippocampal pyramidal neurons by paradoxical NMDA receptor activation. J Neurosci. 2011;31(27):9905–9. doi: 10.1523/JNEUROSCI.1660-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Cook JB, Nelli SM, Neighbors MR, Morrow DH, O'Buckley TK, Maldonado-Devincci AM, Morrow AL. Ethanol alters local cellular levels of (3α,5α)-3-hydroxypregnan-20-one (3α,5α-THP) independent of the adrenals in subcortical brain regions. Neuropsychopharmacology. 2014;39(8):1978–87. doi: 10.1038/npp.2014.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Morrow AL, Porcu P, Boyd KN, Grant KA. Hypothalamic-pituitary-adrenal axis modulation of GABAergic neuroactive steroids influences ethanol sensitivity and drinking behavior. Dialogues Clin Neurosci. 2006;8(4):463–77. doi: 10.31887/DCNS.2006.8.4/amorrow. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Porcu P, Locci A, Santoru F, Berretti R, Morrow AL, Concas A. Failure of acute ethanol administration to alter cerebrocortical and hippocampal allopregnanolone levels in C57BL/6J and DBA/2J mice. Alcohol Clin Exp Res. 2014;38(4):948–58. doi: 10.1111/acer.12329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Gabriel KI, Cunningham CL, Finn DA. Allopregnanolone does not influence ethanol-induced conditioned place preference in DBA/2J mice. Psychopharmacology (Berl) 2004;176(1):50–6. doi: 10.1007/s00213-004-1862-2. [DOI] [PubMed] [Google Scholar]
- 194.Finn DA, Sinnott RS, Ford MM, Long SL, Tanchuck MA, Phillips TJ. Sex differences in the effect of ethanol injection and consumption on brain allopregnanolone levels in C57BL/6 mice. Neuroscience. 2004;123(4):813–9. doi: 10.1016/j.neuroscience.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 195.Torres JM, Ortega E. Alcohol intoxication increases allopregnanolone levels in female adolescent humans. Neuropsychopharmacology. 2003;28(6):1207–9. doi: 10.1038/sj.npp.1300170. [DOI] [PubMed] [Google Scholar]
- 196.Torres JM, Ortega E. Alcohol intoxication increases allopregnanolone levels in male adolescent humans. Psychopharmacology (Berl) 2004;172(3):352–5. doi: 10.1007/s00213-003-1662-0. [DOI] [PubMed] [Google Scholar]
- 197.Holdstock L, Penland SN, Morrow AL, de Wit H. Moderate doses of ethanol fail to increase plasma levels of neurosteroid 3α-hydroxy-5α-pregnan-20-one-like immunoreactivity in healthy men and women. Psychopharmacology (Berl) 2006;186(3):442–50. doi: 10.1007/s00213-005-0187-0. [DOI] [PubMed] [Google Scholar]
- 198.Pierucci-Lagha A, Covault J, Feinn R, Khisti RT, Morrow AL, Marx CE, Shampine LJ, Kranzler HR. Subjective effects and changes in steroid hormone concentrations in humans following acute consumption of alcohol. Psychopharmacology (Berl) 2006;186(3):451–61. doi: 10.1007/s00213-005-0231-0. [DOI] [PubMed] [Google Scholar]
- 199.Pierucci-Lagha A, Covault J, Feinn R, Nellissery M, Hernandez-Avila C, Oncken C, Morrow AL, Kranzler HR. GABRA2 alleles moderate the subjective effects of alcohol, which are attenuated by finasteride. Neuropsychopharmacology. 2005;30(6):1193–203. doi: 10.1038/sj.npp.1300688. [DOI] [PubMed] [Google Scholar]
- 200.Covault J, Pond T, Feinn R, Arias AJ, Oncken C, Kranzler HR. Dutasteride reduces alcohol's sedative effects in men in a human laboratory setting and reduces drinking in the natural environment. Psychopharmacology (Berl) 2014;231(17):3609–18. doi: 10.1007/s00213-014-3487-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Irwig MS. Decreased alcohol consumption among former male users of finasteride with persistent sexual side effects: a preliminary report. Alcohol Clin Exp Res. 2013;37(11):1823–6. doi: 10.1111/acer.12177. [DOI] [PubMed] [Google Scholar]
- 202.Maldonado-Devincci AM, Cook JB, O'Buckley TK, Morrow DH, McKinley RE, Lopez MF, Becker HC, Morrow AL. Chronic intermittent ethanol exposure and withdrawal alters (3α,5α)-3-hydroxy-pregnan-20-one immunostaining in cortical and limbic brain regions of C57BL/6J mice. Alcohol Clin Exp Res. 2014;38(10):2561–71. doi: 10.1111/acer.12530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Milivojevic V, Kranzler HR, Gelernter J, Burian L, Covault J. Variation in genes encoding the neuroactive steroid synthetic enzymes 5α-reductase type 1 and 3α-reductase type 2 is associated with alcohol dependence. Alcohol Clin Exp Res. 2011;35(5):946–52. doi: 10.1111/j.1530-0277.2010.01425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.O'Dell LE, Purdy RH, Covey DF, Richardson HN, Roberto M, Koob GF. Epipregnanolone and a novel synthetic neuroactive steroid reduce alcohol self-administration in rats. Pharmacol Biochem Behav. 2005;81(3):543–50. doi: 10.1016/j.pbb.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 205.Besheer J, Lindsay TG, O'Buckley TK, Hodge CW, Morrow AL. Pregnenolone and ganaxolone reduce operant ethanol self-administration in alcohol-preferring p rats. Alcohol Clin Exp Res. 2010;34(12):2044–52. doi: 10.1111/j.1530-0277.2010.01300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Papadopoulos V. On the role of the translocator protein (18-kDa) TSPO in steroid hormone biosynthesis. Endocrinology. 2014;155(1):15–20. doi: 10.1210/en.2013-2033. [DOI] [PubMed] [Google Scholar]
- 207.Giatti S, Garcia-Segura LM, Melcangi RC. New steps forward in the neuroactive steroid field. J Steroid Biochem Mol Biol. 2015;153:127–34. doi: 10.1016/j.jsbmb.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 208.Giatti S, Romano S, Pesaresi M, Cermenati G, Mitro N, Caruso D, Tetel MJ, Garcia-Segura LM, Melcangi RC. Neuroactive steroids and the peripheral nervous system: An update. Steroids. 2015;103:23–30. doi: 10.1016/j.steroids.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Cummins CL, Mangelsdorf DJ. Liver X receptors and cholesterol homoeostasis: spotlight on the adrenal gland. Biochem Soc Trans. 2006;34(Pt 6):1110–3. doi: 10.1042/BST0341110. [DOI] [PubMed] [Google Scholar]
- 210.Mitro N, Cermenati G, Giatti S, Abbiati F, Pesaresi M, Calabrese D, Garcia-Segura LM, Caruso D, Melcangi RC. LXR and TSPO as new therapeutic targets to increase the levels of neuroactive steroids in the central nervous system of diabetic animals. Neurochem Int. 2012;60(6):616–21. doi: 10.1016/j.neuint.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 211.Cermenati G, Giatti S, Cavaletti G, Bianchi R, Maschi O, Pesaresi M, Abbiati F, Volonterio A, Saez E, Caruso D, Melcangi RC, Mitro N. Activation of the liver X receptor increases neuroactive steroid levels and protects from diabetes-induced peripheral neuropathy. J Neurosci. 2010;30(36):11896–901. doi: 10.1523/JNEUROSCI.1898-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Sironi L, Mitro N, Cimino M, Gelosa P, Guerrini U, Tremoli E, Saez E. Treatment with LXR agonists after focal cerebral ischemia prevents brain damage. FEBS Lett. 2008;582(23-24):3396–400. doi: 10.1016/j.febslet.2008.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Xu P, Li D, Tang X, Bao X, Huang J, Tang Y, Yang Y, Xu H, Fan X. LXR agonists: new potential therapeutic drug for neurodegenerative diseases. Mol Neurobiol. 2013;48(3):715–28. doi: 10.1007/s12035-013-8461-3. [DOI] [PubMed] [Google Scholar]
- 214.Uzunova V, Sheline Y, Davis JM, Rasmusson A, Uzunov DP, Costa E, Guidotti A. Increase in the cerebrospinal fluid content of neurosteroids in patients with unipolar major depression who are receiving fluoxetine or fluvoxamine. Proc Natl Acad Sci U S A. 1998;95(6):3239–44. doi: 10.1073/pnas.95.6.3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Romeo E, Strohle A, Spalletta G, di Michele F, Hermann B, Holsboer F, Pasini A, Rupprecht R. Effects of antidepressant treatment on neuroactive steroids in major depression. Am J Psychiatry. 1998;155(7):910–3. doi: 10.1176/ajp.155.7.910. [DOI] [PubMed] [Google Scholar]
- 216.Pinna G, Rasmusson AM. Ganaxolone improves behavioral deficits in a mouse model of post-traumatic stress disorder. Front Cell Neurosci. 2014;8:256. doi: 10.3389/fncel.2014.00256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Rasmusson AM, Pinna G, Paliwal P, Weisman D, Gottschalk C, Charney D, Krystal J, Guidotti A. Decreased cerebrospinal fluid allopregnanolone levels in women with posttraumatic stress disorder. Biol Psychiatry. 2006;60(7):704–13. doi: 10.1016/j.biopsych.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 218.Hardoy MC, Serra M, Carta MG, Contu P, Pisu MG, Biggio G. Increased neuroactive steroid concentrations in women with bipolar disorder or major depressive disorder. J Clin Psychopharmacol. 2006;26(4):379–84. doi: 10.1097/01.jcp.0000229483.52955.ec. [DOI] [PubMed] [Google Scholar]
- 219.Fish EW, Whitman BJ, DiBerto JF, Robinson JE, Morrow AL, Malanga CJ. Effects of the neuroactive steroid allopregnanolone on intracranial self-stimulation in C57BL/6J mice. Psychopharmacology (Berl) 2014;231(17):3415–23. doi: 10.1007/s00213-014-3600-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Anker JJ, Zlebnik NE, Carroll ME. Differential effects of allopregnanolone on the escalation of cocaine self-administration and sucrose intake in female rats. Psychopharmacology (Berl) 2010;212(3):419–29. doi: 10.1007/s00213-010-1968-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Ford MM, Mark GP, Nickel JD, Phillips TJ, Finn DA. Allopregnanolone influences the consummatory processes that govern ethanol drinking in C57BL/6J mice. Behav Brain Res. 2007;179(2):265–72. doi: 10.1016/j.bbr.2007.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Finn DA, Mark GP, Fretwell AM, Gililland-Kaufman KR, Strong MN, Ford MM. Reinstatement of ethanol and sucrose seeking by the neurosteroid allopregnanolone in C57BL/6 mice. Psychopharmacology (Berl) 2008;201(3):423–33. doi: 10.1007/s00213-008-1303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Broomall E, Natale JE, Grimason M, Goldstein J, Smith CM, Chang C, Kanes S, Rogawski MA, Wainwright MS. Pediatric super-refractory status epilepticus treated with allopregnanolone. Ann Neurol. 2014;76(6):911–5. doi: 10.1002/ana.24295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Howard RB, Sayeed I, Stein D. Suboptimal dosing parameters as possible factors in the negative Phase III clinical trials of progesterone in TBI. J Neurotrauma. 2015 doi: 10.1089/neu.2015.4179. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]