Abstract
Objectives
To investigate the teaching of antimicrobial stewardship (AS) in undergraduate healthcare educational degree programmes in the United Kingdom (UK).
Participants and Methods
Cross-sectional survey of undergraduate programmes in human and veterinary medicine, dentistry, pharmacy and nursing in the UK. The main outcome measures included prevalence of AS teaching; stewardship principles taught; estimated hours apportioned; mode of content delivery and teaching strategies; evaluation methodologies; and frequency of multidisciplinary learning.
Results
80% (112/140) of programmes responded adequately. The majority of programmes teach AS principles (88/109, 80.7%). ‘Adopting necessary infection prevention and control precautions’ was the most frequently taught principle (83/88, 94.3%), followed by 'timely collection of microbiological samples for microscopy, culture and sensitivity’ (73/88, 82.9%) and ‘minimisation of unnecessary antimicrobial prescribing’ (72/88, 81.8%). The ‘use of intravenous administration only to patients who are severely ill, or unable to tolerate oral treatment’ was reported in ~50% of courses. Only 32/88 (36.3%) programmes included all recommended principles.
Discussion
Antimicrobial stewardship principles are included in most undergraduate healthcare and veterinary degree programmes in the UK. However, future professionals responsible for using antimicrobials receive disparate education. Education may be boosted by standardisation and strengthening of less frequently discussed principles.
Introduction
The threat posed by antimicrobial resistance has been equated to climate change [1], with the inappropriate use of antimicrobials in human and animal health resulting in resistant organisms, which in turn create, at a minimum, unresolved challenges such as increased health care utilisation and costs [2], and at the extreme, excess morbidity and mortality [3]. The contributions to antimicrobial resistance are multidimensional and range from behavioural dynamics of healthcare workers to the biology of the microorganisms [4], and thus multimodal interventions have been suggested to be of most benefit. Antimicrobial stewardship (AS), an integrated and multidisciplinary approach that includes the selection of appropriate drugs, enhanced surveillance of prescribing and use, implementation of prescribing guidelines and policies, inclusion of infection prevention and control strategies, and increased efforts on audit and education, has been promoted to arrest the rise of antimicrobial resistance [5].
Despite considerations of education as a fundamental tool to combat antimicrobial resistance [6], some studies have identified gaps in the provision of skills, knowledge and attitudes related to antimicrobials necessary to deliver effective and safe care [7], therefore suggesting an unclear understanding of what is contributing to these gaps in skills and knowledge. Furthermore, such gaps appear to be coupled with reports of undergraduate students demonstrating an interest in receiving increased antimicrobial education during their degree programmes [8,9], suggesting that not enough emphasis is placed on antimicrobial prescribing and stewardship in healthcare educational degree programmes.
To date, however, there has been limited investigation into human and animal health students' knowledge and perceptions of antimicrobial stewardship, and no study to our knowledge has explored the stewardship education delivered by universities. We intended therefore to describe the antimicrobial stewardship learning delivered in undergraduate curricula across disciplines involved in prescribing, administering or reviewing antimicrobials (medicine, nursing, pharmacy, dentistry and veterinary medicine) in the United Kingdom (UK). We aimed to explore how key antimicrobial stewardship principles were delivered, the pedagogies utilised, and the background of those providing education, with a view to identify areas for improvement and aid future capacity building initiatives in education.
Participants and Methods
Design and setting
We conducted a cross-sectional survey exploring recommended antimicrobial stewardship principles (S1 Box) included in the curriculum of undergraduate medicine, pharmacy, nursing, dentistry and veterinary medicine university courses in the UK. The selected principles reflect key dimensions in current antimicrobial stewardship policy in the UK [10].
Participants and recruitment
We identified universities from the official Universities and Colleges Admissions Service (UCAS) list in 2013. Course organisers or module leaders of university programmes offering undergraduate degrees in human and veterinary medicine, dentistry, pharmacy and nursing were identified via the information available on universities’ web pages and invited to complete an electronic survey on Google Forms. The survey was available online for a period of 8 weeks between March and May 2013. Participation was voluntary and the responses were anonymous. No incentives were offered.
Data collection
A team of investigators including an academic research nurse and an educational manager developed the survey instrument (S1 Appendix). We collected information on university and degree programme characteristics; presence of antimicrobial stewardship in the course curriculum; principles of stewardship taught; estimate of number of hours apportioned to antimicrobial stewardship; professional background of lecturers in stewardship sessions; mode of stewardship content delivery (face to face, online or mixture of both); teaching strategies employed in antimicrobial stewardship sessions (lectures, case studies, student presentations, activities in clinical settings, use of simulators or other virtual environments, etc.); methodologies used to evaluate students, as well as arrangements for multidisciplinary learning for some or all of the content. The survey content and the usability of the electronic platform was piloted amongst hospital doctors, nurses and pharmacists as well as MSc Infection students that included nurses and pharmacists. Participants were able to review their options as all questions appeared on one single page.
As secondary source of data, in July 2013 we submitted a request to each university under the provisions of the UK Freedom of Information Act (2000). As public bodies, universities are required to submit a response within 20 working days of the request. However, the stipulations included in the Act allow universities to refuse the request for information on grounds of cost or business sensitivity.
Statistical analysis
Descriptive analysis was conducted. Analyses included cross tabulations and tests of central tendency and dispersion. Associations between disciplines and antimicrobial stewardship components, teaching and evaluation were explored. Differences in antimicrobial stewardship hours between different disciplines were compared using parametric or nonparametric tests, depending on the normality of distributions. Statistical analysis was performed with STATA v10.1 (STATA Corp, College Station, TX).
Ethical approval
The study obtained approval by Imperial College Research Ethics Committee. All participants received an information sheet with information about the research team, the purpose of the study, the survey completion time, and the confidential and anonymous nature of responses. We considered that submission of responses via the electronic form indicated agreement to participate in the survey.
Results
We contacted 140 UK undergraduate programmes in medicine, nursing, veterinary medicine, dentistry or pharmacy. Of these, 112 (80%) submitted a response, but only 109 (77.85%) were sufficiently completed to be analysed (three universities provided a generic response or marketing brochures). Table 1 presents response rates for each discipline.
Table 1. Number of participating courses, by discipline.
| Discipline | Response rate n/N (%) |
|---|---|
| Dentistry | 16/16 (100) |
| Medicine | 24/34 (70.5) |
| Nursing | 51/58 (87.9) |
| Pharmacy | 15/26 (57.6) |
| Veterinary medicine | 6/6 (100) |
| Total | 112/140 (80) |
Courses including AS in their curriculum
Of the 109 courses submitting adequately completed responses, 88 (80.7%, 95% Confidence Interval [CI] 73.29–88.10) reported explicitly teaching AS in their curriculum. However, there was some variation in frequency amongst disciplines. All dentistry and veterinary medicine schools reported teaching AS, with similar percentages in medical (23/24, 95.8%, 95% CI 87.77–100) and pharmacy schools (13/15, 86.6%, 95% CI 69.36–100). On the contrary, only 31/49 (63.2%, 95% CI 49.69–76.70) nursing schools incorporated any teaching about stewardship.
Teaching of recommended AS principles
Whilst 88 courses stated the inclusion of antimicrobial stewardship in their curricula, only 32/88 (36.3%, 95% CI 26.25–46.34) included all recommended principles. The differences between disciplines were notable, ranging from 4/31 (12.9%, 95% CI 11–24.69) nursing schools to 16/23 (69.5%, 95% CI 50.68–88.31) medical schools. Fig 1 presents the results for all disciplines.
Fig 1. Faculties teaching all recommended AS principles, by discipline.
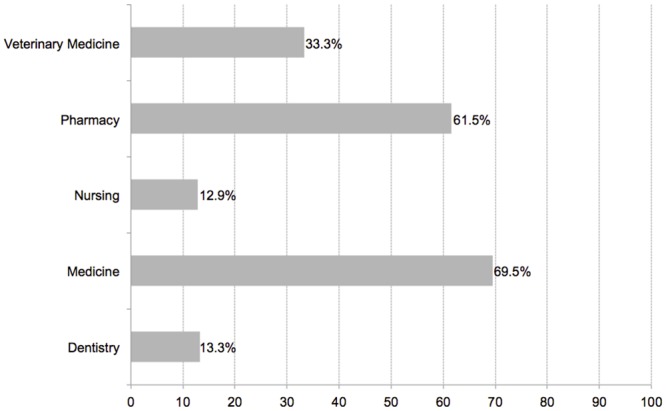
Table 2 displays the frequency of teaching for each principle recommended in antimicrobial stewardship guidelines, presented by discipline. The most frequently cited principle (83/88, 94.3%, 95% CI 89.45–99.14) was ‘adopting necessary infection prevention and control precautions’, followed by 'timely collection of microbiological samples for microscopy, culture and sensitivity’ (73/88, 82.9%, 95% CI 75.03–90.76) and ‘minimisation of unnecessary antimicrobial prescribing’ (72/88, 81.8%, 95% CI 73.73–89.86). In contrast, the ‘use of intravenous administration only to patients who are severely ill, unable to tolerate oral treatment, or where oral therapy would not provide adequate tissue penetration’ was reported in ~50% of courses. These percentages were maintained even if only responses from human health courses (medicine, nursing, pharmacy and dentistry) were considered.
Table 2. Antimicrobial stewardship principles included in undergraduate education programmes, by discipline.
| Antimicrobial stewardship principle | Dentistry n/N (%) | Medicine n/N (%) | Nursing n/N (%) | Pharmacy n/N (%) | Veterinary Medicine n/N (%) | Total n/N(%) |
|---|---|---|---|---|---|---|
| Minimisation of unnecessary prescribing of antimicrobials | 13/13 (100) | 21/22 (95.4) | 19/33 (57.5) | 14/14 (100) | 5/6 (83.3) | 72/88 (81.8) |
| Timing of antimicrobial administration | 13/13 (100) | 21/22 (95.4) | 19/33 (57.5) | 14/14 (100) | 5/6 (83.3) | 72/88 (81.8) |
| Therapeutic drug monitoring | 2/12 (16.6) | 20/22 (90.9) | 13/32 (40.6) | 11/14 (78.5) | 4/6 (66.6) | 50/86 (58.1) |
| Need for standard infection prevention and control precautions | 13/13 (100) | 22/22 (100) | 32/33 (96.9) | 12/14 (85.7) | 5/6 (83.3) | 83/88 (94.3) |
| Collection of appropriate specimens for microscopy, culture and sensitivity | 9/13 (69.2) | 21/22 (95.4) | 26/33 (78.7) | 12/14 (85.7) | 5/6 (83.3) | 73/88 (82.9) |
| Intravenous use only in severely ill patients, unable to tolerate oral treatment, or where oral treatment would not guarantee coverage or tissue penetration | 7/13 (53.8) | 18/22 (81.8) | 14/32 (43.7) | 10/13 (76.9) | 4/6 (66.6) | 53/86 (61.6) |
| Review microbiology results daily and de-escalate to pathogen-directed narrow-spectrum treatment promptly | 4/13 (30.7) | 18/22 (81.8) | 10/32 (31.2) | 11/14 (78.5) | 4/6 (66.6) | 47/87 (54.0) |
| Review need for intravenous treatment daily and switch to oral route promptly | 3/13 (23.0) | 18/22 (81.8) | 9/32 (28.1) | 10/14 (71.4) | 4/6 (66.6) | 44/87 (50.5) |
| Require single dose surgical prophylaxis regimens as appropriate | 5/13 (38.4) | 16/22 (72.7) | 9/32 (28.1) | 9/14 (64.2) | 4/6 (66.6) | 43/87 (49.4) |
Background of teachers delivering AS content
We explored the profession of teachers in the 88 courses reporting antimicrobial stewardship in their curriculum, with the view that exposing students to multidisciplinary instructors may positively influence their antimicrobial clinical teamwork. Overall, 55/88 courses (62.5%, 95% CI 52.38–72.61) included tutors with professional backgrounds different to the students they were teaching to (for instance, 13/15 (86.6%) dentist courses employed antimicrobial stewardship lecturers with backgrounds other than dentistry. In medicine 19/23 (82.6%) of courses employed antimicrobial lecturers with backgrounds other than medicine. The results for the rest of disciplines were nursing 21/31 (67.7%), pharmacy 8/13 (61.5%), and veterinary medicine 3/6 (50%).
Mode of AS content delivery
The delivery of stewardship teaching included a mixture of face-to-face and online pedagogies. However, there was heterogeneity amongst the disciplines in the uptake of online platforms and the use of blended learning (combining face-to-face and online methods). Nursing (22/30, 73.3%, 95% CI 57.46–89.13) reported the highest use of blended approaches, whilst the majority of pharmacy (11/13, 84.6%, 95% CI 64.97–100) and dentistry courses (11/15, 73.3%, 95% CI 50.91–95.68) were delivered face-to-face. Around 50% (12/23, 52.1%, 95% CI 31.68–72.51) of medical courses reported the use of face-to-face methods.
AS teaching methodologies
The variety of teaching strategies reported by is presented in Table 3. In nine cases (10.2%), lectures would be the only teaching methodology employed.
Table 3. Antimicrobial stewardship teaching methodologies used in undergraduate education programmes, by discipline.
| Dentistry (n = 15) | Vet Med (n = 6) | Pharmacy (n = 14) | Medicine (n = 24) | Nursing (n = 29) | Total(n = 88) | |
|---|---|---|---|---|---|---|
| Lecture | 4 | 0 | 2 | 1 | 2 | 9 |
| Lecture + case studies | 4 | 0 | 2 | 3 | 1 | 10 |
| Lecture + case studies + other | 0 | 0 | 5 | 2 | 3 | 10 |
| Lecture + clinical setting | 1 | 0 | 0 | 0 | 1 | 2 |
| Lecture + clinical setting + other | 0 | 1 | 0 | 0 | 5 | 6 |
| Lecture + case studies + clinical setting | 3 | 0 | 1 | 2 | 3 | 9 |
| Lectures + case studies + clinical setting + other | 2 | 3 | 3 | 13 | 8 | 29 |
| Other methodologies/ combined methodologies | 1 | 2 | 1 | 3 | 6 | 13 |
Clinical setting = activities in clinical setting; Other includes use of simulators, problem-based learning activity, student presentations, reflective practice journals.
AS evaluation approaches
The diversity of teaching methodologies was mirrored by the multiple evaluation approaches reported by the universities, and is presented in Table 4. The use of objective structured examinations, alone or in combination with short-answer questions and essays, was the preferred practice. One of the institutions reported no formal assessment or evaluation for students in the area of antimicrobial stewardship.
Table 4. Antimicrobial stewardship evaluation methodologies used in undergraduate programmes, by discipline.
| Dentistry (n = 15) | Vet Med (n = 6) | Pharmac (n = 14) | Medicine (n = 24) | Nursing (n = 26) | Total per approach | |
|---|---|---|---|---|---|---|
| OSCE | 0 | 0 | 0 | 0 | 4 | 4 |
| Written exam | 0 | 0 | 0 | 2 | 2 | 4 |
| No formal assessment | 0 | 0 | 0 | 0 | 1 | 1 |
| Essay | 0 | 0 | 0 | 0 | 1 | 1 |
| Clinical assessment | 0 | 0 | 0 | 0 | 1 | 1 |
| Essay + OSCE | 1 | 0 | 0 | 2 | 1 | 4 |
| Essay + written exam | 2 | 1 | 1 | 3 | 3 | 10 |
| Essay + OSCE + other | 3 | 1 | 4 | 8 | 4 | 20 |
| Essay + clinical assessment + other | 0 | 0 | 0 | 0 | 2 | 2 |
| OSCE + written exam | 6 | 2 | 4 | 6 | 2 | 7 |
| OSCE + presentation + other | 1 | 0 | 2 | 2 | 3 | 5 |
| OSCE + portfolio + other | 0 | 0 | 1 | 1 | 0 | 2 |
| Other grouped categories | 2 | 3 | 2 | 0 | 4 | 11 |
Other includes any of the following, single or in combination: Objective structured clinical examination (OSCE); multiple choice question; short assessment; long assessment; single best answer; student presentation.
Availability of multidisciplinary learning opportunities
18/88 (20.4%, 95% CI 11.98–28.81) of courses with antimicrobial stewardship in the curriculum facilitated information about the availability of multidisciplinary learning opportunities. Pharmacy schools (4/13, 30.7%, 95% CI 5.62–55.77) were more likely to include opportunities were some or all of the content was learned together with students from other disciplines than medical (6/23, 26.1%, 95% CI 8.15–44.04) dental (3/15, 20%, 95% CI 0–40.24) schools, veterinary medicine (1/6, 16.6%, 95% CI 0–46.37) or nursing schools (4/31, 12.9%, 95% CI 1.10–24.69).
Hours of AS included in curriculum, by discipline
Of 88 courses reporting AS in their curricula, 69 (78.4%, 95% CI 69.80–86.99) provided the number of hours. The median number of hours for all courses was 10 (interquartile range 3–100), with 17.75 (interquartile rage 8.87–42.62) hours in medical schools (n = 13); veterinary medicine 15.5 (interquartile rage 12.25–40.87) hours (n = 4); pharmacy 12 (interquartile rage 7–25) hours (n = 12); nursing 10 (interquartile rage 4.5–13.5) hours (n = 27); and dentistry 8.5 (interquartile rage 5–10) hours (n = 13) (Kruskal-Wallis H test χ2(4) = 9.165, p = 0.0571).
Discussion
Our nationwide survey suggests that antimicrobial stewardship is included in the majority of undergraduate medicine, pharmacy, nursing, dentistry and veterinary medicine courses in the UK. However, there are marked differences in the elements of stewardship included within the curricula of the different programmes. Practical elements such as obtaining suitable microbiological samples and the use of adequate infection prevention and control measures appear to take precedence over steps involving executive decision-making, such as reviewing broad-spectrum antibiotic agents once microbiological results are reported back, or considering oral instead of IV administration route. Amongst the different disciplines, nursing faculties presented the most varied profile with ~63% of schools teaching AS but less than 13% including all the recommended steps of stewardship; such results may be attributed to perspectives about the participation of nursing from AS activities [11].
Whilst other studies have measured different aspects of undergraduate students’ understanding, attitudes and behaviours regarding antimicrobials, antimicrobial prescribing or antimicrobial resistance, to our knowledge this is the first published study exploring antimicrobial stewardship as provided by universities in the UK. Additionally, we are the first investigators collecting information from all the main disciplines that prescribe, manage and/or administer antimicrobials, thus providing a richness and comprehensiveness not considered by other surveys that have focused on medical doctors [12–15] or pharmacists [16] exclusively, or from European perspectives that, whilst useful, may be unable to provide detailed information about local contexts [17]. Our findings replicate the variations in exposure to recommended principles and concepts experienced by the students in those studies, including the poor coverage of major principles (e.g. reassessment and duration of antibiotic therapy), as well as observing wide variations in exposure for student within similar educational programmes.
Our use of standardised principles recommended in current UK policy and with extensive common elements with other international antimicrobial stewardship guidelines would ensure that results could be directly compared with future investigations, appearing at a crucial time when national antimicrobial stewardship competencies have been developed [18]. The inclusion of an item referred to adequate infection prevention and control precautions, not strictly an antimicrobial stewardship principle, recognised the close relation of such precautions with the safe collection of microbiological samples.
Our study, however, presents limitations. We did not approach midwifery programmes in our study. We recognize that antimicrobial stewardship knowledge may be delivered in separate sessions across different modules; however, we suggest that if stewardship is to be approached as a cohesive and coherent ‘bundle’ of optimal prescribing behaviours, it would be more appropriate to provide all steps together. In addition, our study identified only the antimicrobial stewardship education provided by universities through selected but broad antimicrobial components, which may have not allowed us to study with accuracy the extent of stewardship teaching. Equally, students may be likely to acquire additional knowledge during clinical placements.
Future professionals responsible for using and managing antimicrobials receive disparate education about stewardship. The impact of education initiatives and continued professional development for graduates in this area may be boosted by curricula standardisation and a focus on strengthening the education about components such as single-dose surgical antibiotic prophylaxis, which seem to be less frequently discussed, using multimodal approaches [19, 20]. Focusing on these components is likely to improve suboptimal clinical practice. The variability in hours and content delivered in UK universities merits further exploration, with consideration towards the technical skills and knowledge involved in stewardship, as well as expertise in communication, negotiation and decision-making. Clearly, applying our selection of antimicrobial stewardship principles, not tailored to each discipline, might explain the variation of the prevalence of teaching of all principles between disciplines. Future studies exploring associations between the educational content provided by universities and the performance or confidence of students in their antimicrobial stewardship skills and knowledge could be of benefit to clarify most favourable approaches. Determining the optimal number of hours to be devoted to antimicrobial stewardship may prove to be problematic, though, due to requirements to incorporate subjective and objective elements, but may be aided by curriculum standardisation efforts. Finally in this regard, our study describes hours of academic learning and does not take into account the educational content that may be acquired by students on clinical placements.
Prescribing and management of antimicrobials appears to be mediated by social interactions between different professions [21,22], with multidisciplinary teamwork practice and training influencing optimal patient outcomes [23]. A proportion of universities in our study offered combined multidisciplinary learning; however, implementing complex educational programmes across disciplines may present logistical difficulties and be unfeasible for all institutions. The frequent use of blended learning platforms highlighted in our study amongst undergraduate institutions may resolve those logistical difficulties and lend sustenance to the development and evaluation of electronic, computerised and/or smartphone-based applications and clinical decision support tools [24].
Whilst antimicrobial stewardship is incorporated explicitly in most human health and veterinary undergraduate courses in the United Kingdom, educators may strengthen the concept by adopting a comprehensive approach with standardised content that emphasises stewardship as a bundle of optimal antimicrobial prescribing behaviours.
However, a majority of programmes do not touch upon all the recommended antimicrobial stewardship principles. In addition, the hours devoted by each discipline to stewardship, together with the teaching and evaluation approaches vary widely and suggest a lack of standardisation in this area.
Supporting Information
(DOCX)
(DOCX)
(DOCX)
Only publicly available responses included here.
(CSV)
Acknowledgments
We thank all participating universities. Preliminary results of this work were presented at the 16th International Congress on Infectious Diseases, Cape Town (South Africa), 2–5 April 2014, and 24th ECCMID Conference, Barcelona (Spain), 10–13 May 2014.
Data Availability
Relevant data is within the paper and its Supporting Information files. Additional data that is restricted due to participant consent and copyright may be available upon request. Please contact rdm-enquiries@imperial.ac.uk. Access to the data will only be granted in line with that consent, subject to approval by the institutional ethics board and under a formal Data Sharing Agreement.
Funding Statement
This work was supported by the National Institute for Health Research (NIHR) Health Protection Research Unit (HPRU) in Healthcare Associated Infection and Antimicrobial Resistance at Imperial College London in partnership with Public Health England (PHE). ECS, MG, AHH also acknowledge the UK Clinical Research Council (CRC) who funds the National Centre for Infection Prevention and Management at Imperial College London (UKCRC G0800777). AHH acknowledges the support of the Imperial College Healthcare Trust NIHR Biomedical Research Centre (funding number not applicable) and is affiliated with the Imperial Centre for Patient Safety and Service Quality funded by the UK NIHR. LND is funded in part by an NIHR Career Development Fellowship (#CDF-2011-04-017) and in part by the Cambridge Biomedical Research Centre (BRC). The study funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health or Public Health England.
References
- 1.Annual report of the Chief Medical Officer. Volume 2. Infections and the rise of antimicrobial resistance. Department of Health, 2011.
- 2.Coast J, Smith RD, Millar MR. Disentangling value: assessing the benefits of containing antimicrobial resistance In: Roberts J, editor. The economics of infectious disease. Oxford, UK: Oxford University Press; 2006. pp 201–14. [Google Scholar]
- 3.Cosgrove S. The Relationship between Antimicrobial Resistance and Patient Outcomes: Mortality, Length of Hospital Stay, and Health Care Costs. Clin Infect Dis. 2006; 42: S82–S89 10.1086/499406 [DOI] [PubMed] [Google Scholar]
- 4.Levy SB. The 2000 Garrod Lecture: Factors impacting on the problem of antibiotic resistance. J Antimicrob Chemother. 2002; 49: 25–30 [DOI] [PubMed] [Google Scholar]
- 5.Moody J, Cosgrove SE, Olmsted R, Septimus E, Aureden K, Oriola S, et al. Antimicrobial stewardship: a collaborative partnership between infection preventionists and healthcare epidemiologists. ICHE. 2012; 33: 328–330. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. The evolving threat of antimicrobial resistance: options for action. WHO, 2012. [Google Scholar]
- 7.Dyar OJ, Pulcini C, Howard P, Nathwani D, ESGAP (the ESCMID Study Group for Antibiotic Policies). European medical students: a first multicentre study of knowledge, attitudes and perceptions of antibiotic prescribing and antibiotic resistance. J Antimicrob Chemother. 2014; 69: 842–6. 10.1093/jac/dkt440 [DOI] [PubMed] [Google Scholar]
- 8.Dyar OJ, Howard P, Nathwani D, Pulcini C; ESGAP (the ESCMID [European Society of Clinical Microbiology, Infectious Diseases] Study Group for Antibiotic Policies). Knowledge, attitudes, and beliefs of French medical students about antibiotic prescribing and resistance. Med Mal Infect. 2013; 43:423–30. 10.1016/j.medmal.2013.07.010 [DOI] [PubMed] [Google Scholar]
- 9.Abbo LM, Cosgrove SE, Pottinger PS, Pereyra M, Sinkowitz-Cochran R, Srinivasan A, et al. Medical students’ perceptions and knowledge about antimicrobial stewardship: how are we educating our future prescribers? Clin Infect Dis. 2013; 57: 631–8. 10.1093/cid/cit370 [DOI] [PubMed] [Google Scholar]
- 10.Department of Health Advisory Committee on Antimicrobial Resistance and Healthcare Associated Infection (ARHAI). Antimicrobial Stewardship: “Start Smart—Then Focus” Guidance for antimicrobial stewardship in hospitals (England). 2011.
- 11.Edwards R, Drumright LN, Kiernan M, Holmes A. Covering more territory to fight resistance: considering nurses’ role in antimicrobial stewardship. J Inf Prev. 2011; 12: 6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davey P, Hudson S, Ridgway G, Reeves D; British Society of Antimicrobial Chemotherapy Working Party on Antimicrobial Use. A survey of undergraduate and continuing medical education about antimicrobial chemotherapy in the United Kingdom. Br J Clin Pharmacol. 1993; 36: 511–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naqvi A, Pulcini C. Bacterial resistance and antibiotic prescription: a survey of hospital physician perception, attitude, and knowledge. Med Mal Infect. 2010; 40: 625–31 [DOI] [PubMed] [Google Scholar]
- 14.Pulcini C, Williams F, Molinari N, Davey P, Nathwani D. Junior doctors’ knowledge and perceptions of antibiotic resistance and prescribing: a survey in France and Scotland. Clin Microbiol Infect. 2011; 17: 80–7. 10.1111/j.1469-0691.2010.03179.x [DOI] [PubMed] [Google Scholar]
- 15.Steinberg M, Dresser LD, Daneman N, Smith OM, Matte A, Marinoff N, et al. A National Survey of Critical Care Physicians' Knowledge, Attitudes, and Perceptions of Antimicrobial Stewardship Programs. J Intensive Care Med. 2014; pii: 0885066614541922 [DOI] [PubMed] [Google Scholar]
- 16.Wickens HJ, Farrell S, Ashiru-Oredope DAI, Jacklin A, Holmes A. The increasing role of pharmacists in antimicrobial stewardship in English hospitals. in collaboration with the Antimicrobial Stewardship Group of the Department of Health Advisory Committee on Antimicrobial Resistance and Health Care Associated Infections (ASG-ARHAI). J Antimicrob Chemother. 2013; 68: 2675–81. [DOI] [PubMed] [Google Scholar]
- 17.Pulcini C, Wencker F, Frimodt-Møller N, Kern WV, Nathwani D, Rodríguez-Baño J, et al. European survey on principles of prudent antibiotic prescribing teaching in undergraduate students. Clin Microbiol Infect. 2015;21(4):354–61. 10.1016/j.cmi.2014.11.015 [DOI] [PubMed] [Google Scholar]
- 18.Ashiru-Oredope D, Cookson B, and Fry C on behalf of the Advisory Committee on Antimicrobial Resistance and Healthcare Associated Infection Professional Education Subgroup. Developing the first national antimicrobial prescribing and stewardship competences. J Antimicrob Chemother. 2014; 69: 2886–2888. 10.1093/jac/dku350 [DOI] [PubMed] [Google Scholar]
- 19.Riggi G, Castillo M, Fernandez M, Wawrzyniak A, Vigoda M, Eber S, et al. Improving compliance with timely intraoperative redosing of antimicrobials in surgical prophylaxis. Infect Control Hosp Epidemiol. 2014;35(10):1236–40. 10.1086/678058 [DOI] [PubMed] [Google Scholar]
- 20.Ohl CA, Luther VP. Health care provider education as a tool to enhance antibiotic stewardship practices. Infect Dis Clin North Am. 2014;28(2):177–93. 10.1016/j.idc.2014.02.001 [DOI] [PubMed] [Google Scholar]
- 21.Charani E, Castro-Sánchez E, Sevdalis N, Kyratsis Y, Drumright L, Shah N, et al. Understanding the Determinants of Antimicrobial Prescribing Within Hospitals: The Role of "Prescribing Etiquette". Clin Infect Dis. 2013; 57:188–96 10.1093/cid/cit212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davey P, Brown E, Charani E, Fenelon L, Gould IM, Holmes A, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev 2013; 4:CD003543 10.1002/14651858.CD003543.pub3 [DOI] [PubMed] [Google Scholar]
- 23.George PP, Papachristou N, Belisario JM, Wang W, Wark PA, Cotic Z, et al. Online eLearning for undergraduates in health professions: A systematic review of the impact on knowledge, skills, attitudes and satisfaction. J Glob Health. 2014; 4: 010406 10.7189/jogh.04.010406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Castro-Sánchez E, Charani E, Moore LSP, Gharbi M, Holmes A. “On call: antibiotics”- development and evaluation of a serious antimicrobial prescribing game for hospital care. In: Schouten B, Fedtke S, Schijven M, Vosmeer M, editors. Proceedings of the 4th conference on gaming and playful interaction in healthcare Games for Health 2014. Springer Vieweg; 2014. Pp. 1–8
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Only publicly available responses included here.
(CSV)
Data Availability Statement
Relevant data is within the paper and its Supporting Information files. Additional data that is restricted due to participant consent and copyright may be available upon request. Please contact rdm-enquiries@imperial.ac.uk. Access to the data will only be granted in line with that consent, subject to approval by the institutional ethics board and under a formal Data Sharing Agreement.


