Abstract
Background and aim
Dental fear and anxiety is a major barrier for dental care provision. Identifying anxious patients can help dental professionals manage them appropriately. The study aimed at assessing dental fear and anxiety among a deaf population in Cluj-Napoca, Romania and their associated and contributing factors.
Method
In this cross sectional study 165 deaf participants were invited to complete a questionnaire comprising three sections. The first section contained questions about social and economical status, the second comprised a Romanian version of the Modified Dental Anxiety Scale (MDAS) while part three was the Dental Fear Survey (DFS). Data was introduced and analyzed with the Statistical Package for Social Sciences (SPSS) program, version 20.0 (SPSS Inc., Chicago, Illinois, USA).
Results
Thirty four point nine percent (34.9%) of respondents were found to be insignificantly anxious, 59.7% were moderately or extremely anxious with 5.3% being identified with dental phobia based on the MDAS scores. Mean total score for dental anxiety on the MDAS scale was 13.7. Patients suffering from a prior negative experience were found to be more anxious (p<0.05).
Conclusions
Dental fear and anxiety is widespread in the deaf communities. Higher percentages were observed among women and people with a previous traumatic dental experience.
Keywords: deaf, dental anxiety, dental fear, modified dental anxiety scale, dental fear survey
Introduction
Pain, fear and anxiety have always been associated with dental treatments [1].
Fear is defined as one’s response facing threat or danger to protect one’s life [2].
Patients coming to a dental office often experience fear and anxiety. It is a well known fact that a fearful person is a more problematic patient [1]. Despite of recent advances in dental technologies and treatment [3], fearful and anxious patients report experiences of pain, fear of specific procedures such as drilling, root canal treatment, extractions or injections [4].
Dentists are confronted with different degrees of dental fear on a daily basis [5]. Patient’s anxiety has a negative effect on the performances of the dental practitioner and dental care may be hampered, giving rise to a constant source of occupational stress [4]. Treating anxious patients might take more time and they are often unsatisfied with their treatment [2].
Fearful and anxious patients often avoid or delay dental care [3] and are three times more predisposed to postpone or cancel their appointments [2] requiring 20% more dental chair time [6]. Since many people delay or avoid dental care because of fear and expectation of pain [7], managing dental anxieties is recognized as an important issue in dental practice [8].
The treatment of a patient’s pain is one of the most challenging aspects of dental care that dentists face today [3]. Previous experiences, expectations, current emotional states are involved in the experience of pain. In the last years, the definition of pain has included the understanding that pain is influenced by our cognitions, our affective and somatic states [1]. Most dentists focus upon decreasing the somatic aspect of the perception of the pain and do not take in consideration the affective and cognitive elements [6]. Pain perception has a strong psychological component and conscious attention is required.
Dental anxiety can be found worldwide and affects a significant number of people from all social backgrounds. It is a serious concern for both dentist and patient for provision of dental care [9].
Anxiety has psychological and emotional components. Dental anxiety appears due to three factors. The first one is novelty. People feel comfortable with the familiar and feel discomfort or anxiety with a novel experience. New experiences are often interpreted as threatening and frightening involving thoughts of fear. The second factor is uncertainty which contributes to the increased general arousal of the patient. In general, people do not like unknown experiences. Lastly is the issue of expectation. The information conveyed by parents or friends can lead to a heightened aroused and anxious state. This often takes the form of negative cognitions which encourage the growing of fear and anxiety [1].
Fear and anxiety increase when a patient feels loss or is out of control, so it is recommended to allow the patient to signal a temporary interruption of the dental procedure when his/her fear or pain has increased. This will provide control over the perceived threat [1].
Due to the occurrence of fear, pain and anxiety from many causes, in the dental offices, it is obvious that behavioral management is needed. They can be also controlled through pharmacology, psychology, cognitive behavioral psychotherapy [10] or hypnosis [3].
The dentist should be assertive in dealing with psychological aspects of the fearful and anxious patient [6]. Prior to dental treatment, identifying anxious patients [9] can enable dentists to anticipate one’s behavior and by using specific management techniques [2] will help alleviate a patient’s anxiety [9]. Dentists do not usually screen dental fear or anxiety. The study conducted by Saatchi et all [2] revealed that only 20% of dental practitioners regularly use a screening method in order to assess their patient’s level of fear [2]. The dentist can measure the levels of fear and anxiety through self report or by administrating a test. Several scales have been developed of which two were used in the current study: the dental fear survey (DFS) and the modified dental anxiety scale (MDAS) [2]. For patients manifesting moderate amounts of anxiety, attention to basic aspects of good clinical care is sufficient. For patients exhibiting high levels of anxiety, a special treatment program conducted by a dental assistant is recommended. A consultation with a psychologist regarding fear and dental anxiety is also strongly encouraged [6].
The effect of dental fear and anxiety on oral health has been reported by many studies [2,4,5]. Dental fear is associated with a lower frequency of dental visits, resulting in a worsening oral health status. In absence of proper dental treatments, oral diseases will inevitably worsen, resulting in more severe oral problems [11]. A fearful or anxious patient has a poorer oral health status: decays, missing or less filled teeth which can produce negative effects on their social life [2]. Oral health has a significant impact on the quality of life and self esteem of a person [9]. Many people who avoid dental treatment also avoid talking or laughing in public [5].
Saatchi et al. [2] indicated that an important factor in dental anxiety genesis is a previous traumatic experience [2].
Some researchers described “a vicious cycle of dental fear” where subjects with dental anxiety avoid dental care, contributing to a deterioration of their dental condition, awareness of their worsening condition leading to increased anxiety. Dental anxiety has been identified as a barrier in receiving dental health care among people with hearing sensory impairment [12].
A multidisciplinary approach using special behavior guidance strategies [7] can be useful in preventing dental fear and promoting oral health in this particular group [11].
Deaf people are unable to understand speech through their auditory sense. In addition, they experience communication barriers so they are more often victims of emotional or physical abuse than hearing people. This increases the risk of mental health problems through their life. There is a negative correlation between hearing loss and reported quality of life. Kvam described an increased risk of mental distress among deaf people [13].
Doctor-patient relationship is often viewed as the cornerstone of healthcare delivery. Due to complex individual, interpersonal and systemic factors, deaf individuals are often times the recipients of inappropriate or even unethical dental care [14]. Deaf individuals are reported to have a poorer health status than the general population [14].
People with disabilities encounter practical and social problems, poor social relationships beyond those experienced by non-disabled subjects [13]. It is commonly accepted that individuals with physical disabilities may encounter difficulties in everyday life that reduce their activity levels. An individual’s activity limitations are predictive of the level of psychological problems he may experience [13].
The study performed by Kvam in the United States related that the risk for clinically significant emotional distress was 2 to 4 times higher among persons with disabilities than among non-disabled [13].
Deaf people are known to be vulnerable to alienation and other negative outcomes including delays in cognitive processing, social maladaptation and psychological distress or disorder [14].
The aim of our study was to assess factors associated with dental fear and anxiety among a sample of deaf patients. We evaluated prevalence of dental fear and anxiety and its relation to gender, educational level, previous dental experiences and frequency of visits was also researched and evaluated.
Material and methods
Participants
A cross-sectional quantitative study was conducted among deaf patients, who were seeking dental checkups or dental treatment at the Department of Conservative Odontology of the Iuliu Hatieganu University of Medicine and Pharmacy or at Ortoelitte Dental Center in the city of Cluj-Napoca, Romania. One hundred and sixty five patients were recruited randomly.
The inclusion criteria were: hearing impaired individuals, subject’s reading and understanding abilities and agreement to participate in the study. Eleven subjects from the study were excluded for not completing the survey form or for refusal to sign informed consent. The final sample consisted of 154 individuals.
The response rate was 93.33%, with a gender distribution of 66 male (42.86%) and 88 female respondents (57.14%). The majority of participants (81.16%) were 30 years of age or younger.
Most of them (92.20%) were born deaf or lost their hearing before the age of 4, 3.24% were aged 4–8 years, 2.59% aged 9–18, and 1.94% was 19 years of age or above when they became deaf.
Etiology, specific levels of hearing or the use of hearing aids were not reported.
Most of them (95.45%) attended a school for deaf using sign language as a mean of communication; the rest had attended local schools.
The purpose of the study was explained to each patient and an informed consent was handed out to those who agreed to participate. Additionally, all participants signed a statement attesting that the information provided will be maintained confidential.
Evaluation of the sample
Questionnaire
Data was collected using a questionnaire made up of three distinct parts. The first section contained questions concerning to obtain sociodemographic information such as name, age, gender, educational level, details of previous dental visits, duration since last visit (choices were given within last 6 months, within the last 6 months to 1 year, 1–2 years ago, more than 2 years back), self perceived oral health status (options were excellent, good, fair, bad), postponement of dental treatment due to dental anxiety, reasons for irregular attendance (high cost, lack of time, not needing treatment, fear, communication difficulties) and existence of post traumatic experiences.
The second section was a Romanian version of MDAS, used to assess the level of anxiety. This scale included 5 multiple choice questions concerning patient’s anxiety in the following situations: anticipating a visit to a dental office, waiting in the office, waiting in the dental chair for tooth drilling, scaling or for receiving an anesthetic injection. Each question was scored from 1 (not anxious at all) to 5 (extremely anxious). The sum of values ranged from 5 to 25. Patients with scores ranging from 5 to 9 were not considered anxious, 10 to 18 moderately anxious while patient scores exceeding 19 were considered extremely anxious [2].
The third section was a Romanian version of the DFS questionnaire. It was pre-validated by a committee formed by a pediatric specialist, a dentist and a psychologist. This scale included 20 questions in three components: avoidance of dental care, physiologic reactions and fear provoked by different procedures. Each question was provided with 5 possible answers ranging from 1 to 5. Scoring 1 to 2 for a question expressed that the subject isn’t fearful in a particular dental situation. Scoring 3 or more for each question indicated one’s fear. Summation of values assembled a score that ranged from 20 to 100 [2].
There was no time limit for completing the survey in order to ensure that any difficulty with language was accommodated. Explanation of items was provided if needed. None of the participants needed sign language support.
Statistical data analysis
The collected data was electronically introduced in a Microsoft Excel 2012 spreadsheet and then transferred to a Statistical Package for Social Sciences (SPSS) program, version 20.0 (SPSS Inc., Chicago, Illinois, USA). The significance of the observed associations and/or differences between variables was tested using student t test, ANOVA and chi square statistic. A difference was considered to be statistically significant if P<0.05.
Results
Mean age of the participants was 29.6 (standard deviation SD=12.35). The majority of the respondents belonged to the ≤30 years of age group (81.16%).
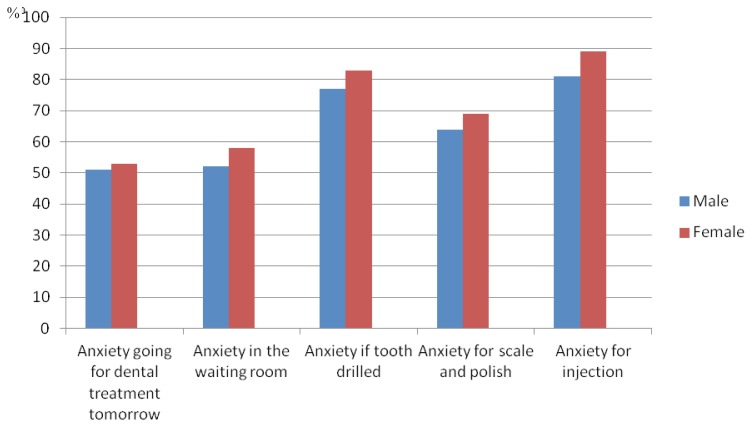
Prevalence of dental anxiety was at a value of 68.83% as is shown in Figure 1.
Figure 1.
Prevalence (%) of dental anxiety related to each MDAS questionnaire item.
Women demonstrated significantly higher MDAS (p<0.012) and DFS scores (p<0.013) than men.
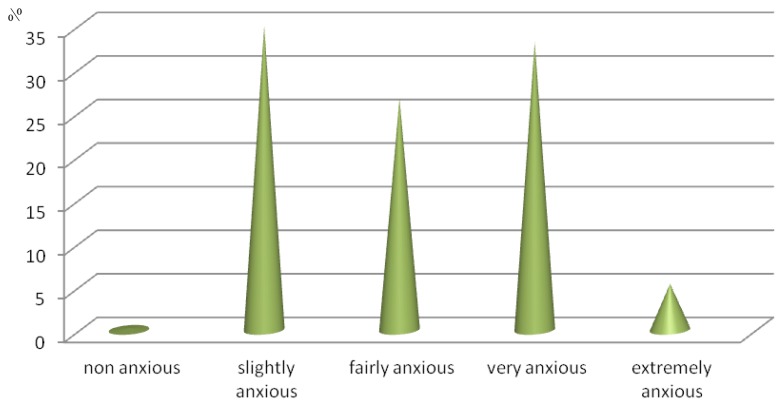
Mean total score for dental anxiety on MDAS was 13.7, 34.9% of respondents were found to be less anxious (5–9 total score), 59.7% moderately or extremely anxious (10–18 total score), 5.3% were found to suffer from dental phobia (≥19 total score) as illustrated in Figure 2.
Figure 2.
Distribution (%) of mean total score for dental anxiety on MDAS.
Uneducated or unemployed respondents reported greater anxiety towards dental treatments (p<0.001).
Evaluation of economic status revealed that participants with no income or who are financially dependent on another family member were more anxious than financially independent participants (p<0.05).
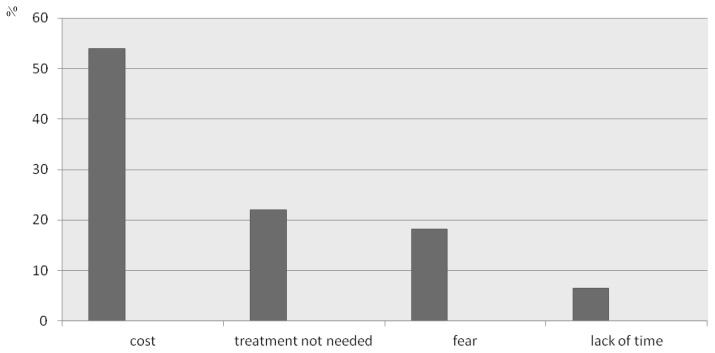
The major reason given by 53.89% of the subjects for not attending a dentist was cost, 22.07 % thought that treatment is not needed, 18.18% of subjects delayed or avoided treatment because of fear while 6.49% for lack of time as is shown in Figure 3. Only 10.38% of participants reported regular visits to a dentist’s office.
Figure 3.
Main reasons for not attending a dentist (%).
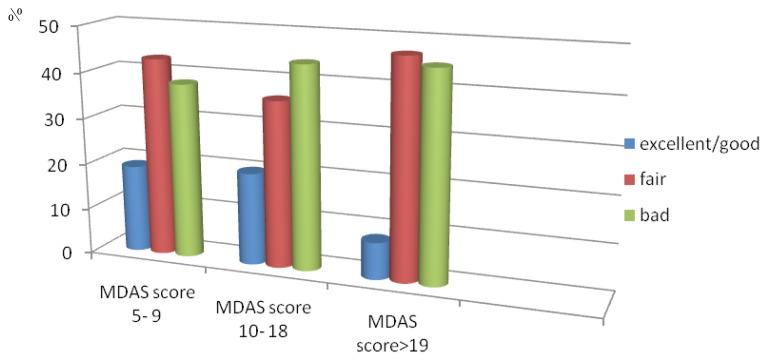
Oral health was perceived as fair or bad by the majority of participants as presented in Figure 4 and there was an inverse relationship between anxiety and frequency of dental treatment (r=−0.119 p=0.009).
Figure 4.
Self-assessed dental health related to MDAS score (%).
It was seen that 42.86% of the respondents were not anxious regarding their dental visit with 46.10% reporting no anxiety while sitting in the waiting room of the dental office. Most of the subjects (83.11%) felt anxious if tooth drilling or injection with local anesthetic were to occur, injection being the most feared dental procedure of all.
DFS scores were ranged from 18–67, with a mean value of 28±6.29 with a statistically significant difference observed between males and females (p<0.001).
Independent t-test demonstrated that DFS scores (48.4±15.14) and MDAS scores (17.3±4.2) in patients with previous traumatic experiences were significantly higher (p<0.001) than in patients without a prior negative dental experience (36.6±17.8).
Discussion
This study is one of few attempts to characterize dental fear and anxiety among deaf patients using a standardized scale. Our findings suggest that there should be increased efforts to screen people with disabilities for dental anxiety. The delivery of health care services to individuals with hearing loss is poorly understood by the average physician. In addition limited research has been done on this subject to date [15–17].
Dental fear can act as a hindrance to dental care delivery and this psychological problem can turn into a health concern [11,18]. Managing dental fear and anxiety is recognized as an important issue in dental offices since many people delay or avoid dental procedures because of their fear, anxiety or expectation of pain [8]. Brief cognitive and behavioral approaches for dental anxiety are already established as effective treatment strategies [10,19]. The dentist’s office should provide a program antagonistic with novelty, uncertainty, negative expectations and cognitions or feelings of insecurity. Medical assistants can implement programs that relax the patient, producing a positive expectation and a sense of security [6,20,21]. A variety of distraction interventions can be used on a daily basis in medical offices in order to help patients to cope with unpleasant procedures; these include watching television, listening to music, video games, and virtual reality (VR) goggles. Forests, botanical gardens, snowy canyons are the most effective VR surroundings at reducing stress and creating positive experiences [6,22]. Also it is considered beneficial for a deaf patient to have the opportunity to visit the dental office in advance of the appointment so that he/she can familiarize with the dental care provider, office staff and smells.
In our study, people who experienced previous traumatic dental episodes showed higher levels of dental anxiety, which was also observed in the findings conducted by Do Nascimento et al. [2]. A history of urgent dental care may predispose people to be fearful of the dental practitioner. Better knowledge of the antecedents of dental fear and anxiety are needed in order to design effective programs aimed to prevent dental fear and its oral health related consequences.
Evaluation of economic status showed that those with lower economic status (with no income, who are financially dependent of another family member) were more anxious than independent respondents. Uneducated and unemployed people scored high on the anxiety scale while educated people cope better. Lower or mediocre socioeconomic conditions lead to poor physical health and also psychological pathology such as depression or anxiety [2,19,24–26]. Shiboski reported that low income is a barrier to dental care and it may lead to a deteriorated state of oral health that may prompt such patients to seek oral health care only when experiencing acute pain.
Comparison between genders showed that anxiety is more commonly found in women. This is in agreement with studies recently performed by Pawlicki and Saatchi [1,2]. This can be explained by the fact that women are more able to express their feelings of fear. In addition, physiological conditions such as stress, social phobia and fear are more common in females. Dental anxiety is associated with such emotions. Females usually admit their fears readily than men and have a lower tolerance to pain, thus exhibiting higher levels of neuroticism [2,26–28]. Other studies performed by Kagen et all and El-Housseiny showed no significant differences between gender and dental anxiety [2,7,29].
Even if people with hearing loss visited doctor’s offices significantly more often than hearing people, they reported less satisfaction with health care services [15]. Only about 10.38% of our participants claimed to visit dental offices regularly, while Saatchi et al reported in general population 16.5% or up to 50–72% in developed countries [2].
Our findings showed that the most feared dental procedure is the injection. Similar observations were also seen in hearing people studies performed by El-Housseiny et al. This is probably because some dentists use the threat of injection as a method of child discipline [7].
The prevalence of dental anxiety in the present study was found to be 68.83% while Saatchi et all reported 58.8% in hearing populations, suggesting that despite technological advances made in the field of modern dentistry, dental treatment related anxiety is still widespread [2]. Our results were higher than those reported by Do Nascimento et al. (23%) and Mafca et al. (63%) [2]. Higher prevalence of dental anxiety among deaf people raises concern that its negative impact has the potential for serious health consequences [12].
The concept of treating the patient and not just the tooth is essential. An important aspect of patient management in the dental chair is managing dental fear and anxiety [16]. In order to reduce dental fear, regular checkups could provide people with positive and neutral dental treatment related experiences. When a patient is known to be fearful and anxious, knowledge of the patient’s cognition is a major first step in reducing fears and anxieties. Behavioral management techniques are meant to reduce the need for excessive and unsafe use of medication [16]. Information coming from the dentist provides security for the dental procedures to come. Modifying the atmosphere, taking time to ensure adequate anesthesia, being warm, providing treatment in short appointments rather than in a long visit, acting in a calm and confident manner are all essential management methods [16,17]. Touching the patient’s hand or shoulder is a mean of establishing warmth, security and caring which is antagonistic to fear. It is recommended to refer the extremely anxious patient to a clinical psychologist who will consult the patient at the dental office during off hours [11]. Studies by Sharath et all have shown that dental anxiety is not only a mental health concern but also a public health one. Fear of dental procedures and delayed/cancelled dental visits contribute to severe oral symptoms [2,11]. Breaking the fear and anxiety cycle requires a multidisciplinary approach involving. Proper use of management techniques can improve behavior, making things easier for patient and dental practitioner alike [16,30].
Limitations of our study include its cross sectional design, a limited population with lower economic status and educational level, convenience sampling, self assessment questionnaire, therefore studies on larger populations are needed in order to reveal dental fear and anxiety in modern society [2].
Results clearly demonstrated the vulnerability of deaf facing dental treatment which is co morbidity.
Conclusions
It can be observed from our study that dental fear and anxiety are widespread among the deaf populations. Our research highlighted the importance of using behavioral techniques in the field of dentistry in order to improve patient management strategies and policy making.
Dental anxiety was found to be higher in females while people who visit the dental practitioner regularly were less anxious.
Empowering deaf patients to actively address oral health care with their dentist can establish a positive framework, thus breaking the vicious cycle of dental fear and treatment avoidance.
Use of a standardized scale may enable dentists to detect the procedures that provoke fear and guide the patient’s behavior accordingly using a cognitive approach.
Treating deaf patients is a challenge in need of close interdisciplinary collaboration between psychotherapist and dentist.
Acknowledgements
This paper was published under the frame of European Social Fund, Human Resources Development Operational Programme 2007–2013, project no. POSDRU/159/1.5/S/138776.
References
- 1.Pawlicki RE. Psychological/behavioral techniques in managing pain and anxiety in the dental patient. Anesth Prog. 1991;38(4–5):120–127. [PMC free article] [PubMed] [Google Scholar]
- 2.Saatchi M, Abtahi M, Mohammadi G, Mirdamadi M, Binandeh ES. The prevalence of dental anxiety and fear in patients referred to Isfahan Dental School, Iran. Dent Res J (Isfahan) 2015;12(3):248–253. [PMC free article] [PubMed] [Google Scholar]
- 3.Wiederhold MD, Gao K, Wiederhold BK. Clinical use of virtual reality distraction system to reduce anxiety and pain in dental procedures. Cyberpsychol Behav Soc Netw. 2014;17(6):359–365. doi: 10.1089/cyber.2014.0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berggren U. Long-term management of the fearful adult patient using behavior modification and other modalities. J Dent Educ. 2001;65(12):1357–1368. [PubMed] [Google Scholar]
- 5.Lenk M, Berth H, Joraschky P, Petrowski K, Weidner K, Hannig C. Fear of dental treatment--an under recognized symptom in people with impaired mental health. Dtsch Arztebl Int. 2013;110(31–32):517–522. doi: 10.3238/arztebl.2013.0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pawlicki R. Psychologic interventions for the anxious dental patient. Anesth Prog. 1987;34(6):220–227. [PMC free article] [PubMed] [Google Scholar]
- 7.El-Housseiny AA, Alamoudi NM, Farsi NM, El Derwi DA. Characteristics of dental fear among Arabic-speaking children: a descriptive study. BMC Oral Health. 2014;14:118. doi: 10.1186/1472-6831-14-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tanja-Dijkstra K, Pahl S, White MP, Andrade J, May J, Stone RJ, et al. Can virtual nature improve patient experiences and memories of dental treatment? A study protocol for a randomized controlled trial. Trials. 2014;15:90. doi: 10.1186/1745-6215-15-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Appukuttan D, Subramanian S, Tadepalli A, Damodaran LK. Dental anxiety among adults: an epidemiological study in South India. N Am J Med Sci. 2015;7(1):13–18. doi: 10.4103/1947-2714.150082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson KI, Davies JG. A joint approach to treating dental phobics between community dental services and specialist psychotherapy services--a single case report. Br Dent J. 2001;190(8):431–432. doi: 10.1038/sj.bdj.4800993. [DOI] [PubMed] [Google Scholar]
- 11.Crego A, Carrillo-Díaz M, Armfield JM, Romero M. From public mental health to community oral health: the impact of dental anxiety and fear on dental status. Front Public Health. 2014;2:16. doi: 10.3389/fpubh.2014.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singer R, Cardenas G, Xavier J, Jeanty Y, Pereyra M, Rodriguez A, et al. Dental anxiety and the use of oral health services among people attending two HIV primary care clinics in Miami. Public Health Rep. 2012;127(Suppl 2):36–44. doi: 10.1177/00333549121270S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kvam MH, Loeb M, Tambs K. Mental health in deaf adults: symptoms of anxiety and depression among hearing and deaf individuals. J Deaf Stud Deaf Educ. 2007;12(1):1–7. doi: 10.1093/deafed/enl015. [DOI] [PubMed] [Google Scholar]
- 14.Kent BA. Identity Issues for Hard-of-Hearing Adolescents Aged 11, 13, and 15 in Mainstream Setting. J Deaf Stud Deaf Educ. 2003;8(3):315–324. doi: 10.1093/deafed/eng017. [DOI] [PubMed] [Google Scholar]
- 15.Harmer L. Health care delivery and deaf people: practice, problems, and recommendations for change. J Deaf Stud Deaf Educ. 1999;4(2):73–110. doi: 10.1093/deafed/4.2.73. [DOI] [PubMed] [Google Scholar]
- 16.Sharath A, Rekka P, Muthu MS, Rathna Prabhu V, Sivakumar N. Children’s behavior pattern and behavior management techniques used in a structured postgraduate dental program. J Indian Soc Pedod Prev Dent. 2009;27(1):22–26. doi: 10.4103/0970-4388.50812. [DOI] [PubMed] [Google Scholar]
- 17.Armfield JM, Slade GD, Spencer AJ. Dental fear and adult oral health in Australia. Community Dent Oral Epidemiol. 2009;37(3):220–230. doi: 10.1111/j.1600-0528.2009.00468.x. [DOI] [PubMed] [Google Scholar]
- 18.Pramila M, Krishna-Murty A, Chandrakala B, Ranganath S. Dental fear in children and its relation to dental caries and gingival condition: a cross sectional study in Bangalore city, India. Int J Clin Dent Sci. 2010;1(1):1–5. [Google Scholar]
- 19.Sghaireen MG, Zwiri AM, Alzoubi IA, Qodceih SM, Al-Omiri MK. Anxiety due to dental treatment and procedures among university students and its correlation with their gender and field of study. Int J Dent. 2013;2013:647436. doi: 10.1155/2013/647436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mohammed RB, Lalithamma T, Varma DM, Sudhakar KN, Srinivas B, Krishnamraju PV, et al. Prevalence of dental anxiety and its relation to age and gender in coastal Andhra (Visakhapatnam) population, India. J Nat Sci Biol Med. 2014;5(2):409–414. doi: 10.4103/0976-9668.136210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marya CM, Grover S, Jnaneshwar A, Pruthi N. Dental anxiety among patients visiting a dental institute in Faridabad, India. West Indian Med J. 2012;61(2):187–190. [PubMed] [Google Scholar]
- 22.Majstorović M, Skrinjarić T, Szirovicza L, Glavina D, Veerkamp JS. Dental anxiety in relation to emotional and behavioral problems in Croatian adolescents. Coll Antropol. 2007;31(2):573–578. [PubMed] [Google Scholar]
- 23.Chhabra N, Chhabra A, Walia G. Prevalence of dental anxiety and fear among five to ten year old children: a behaviour based cross sectional study. Minerva Stomatol. 2012;61(3):83–89. [PubMed] [Google Scholar]
- 24.Bedi R, Sutcliffe P, Donnan PT, McConnachie J. The prevalence of dental anxiety in a group of 13- and 14-year-old Scottish children. Int J Paediatr Dent. 1992;2(1):17–24. doi: 10.1111/j.1365-263x.1992.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 25.Oliveira MM, Colares V. The relationship between dental anxiety and dental pain in children aged 18 to 59 months: A study in Recife, Pernambuco State, Brazil. Cad Saude Publica. 2009;25:743–750. doi: 10.1590/s0102-311x2009000400005. [DOI] [PubMed] [Google Scholar]
- 26.Hakeberg M, Berggren U, Carlsson SG. Prevalence of dental anxiety in an adult population in a major urban area in Sweden. Community Dent Oral Epidemiol. 1992;20(2):97–101. doi: 10.1111/j.1600-0528.1992.tb00686.x. [DOI] [PubMed] [Google Scholar]
- 27.do Nascimento DL, Silva Araújo AC, Gusmão ES, Cimões R. Anxiety and fear of dental treatment among users of public health services. Oral Health Prev Dent. 2011;9(4):329–337. [PubMed] [Google Scholar]
- 28.Dailey YM, Humphris GM, Lennon MA. The use of dental anxiety questionnaires: a survey of a group of UK dental practitioners. Br Dent J. 2001;190(8):450–453. doi: 10.1038/sj.bdj.4801000. [DOI] [PubMed] [Google Scholar]
- 29.Kanegane K, Penha SS, Borsatti MA, Rocha RG. Dental anxiety in an emergency dental service. Rev Saude Publica. 2003;37(6):786–792. doi: 10.1590/s0034-89102003000600015. [DOI] [PubMed] [Google Scholar]
- 30.Armfield JM. Development and psychometric evaluation of the Index of Dental Anxiety and Fear (IDAF-4C+) Psychol Assess. 2010;22(2):279–287. doi: 10.1037/a0018678. [DOI] [PubMed] [Google Scholar]
- 31.Malvania EA, Ajitkrishnan CG. Prevalence and socio- demographic correlates of dental anxiety among group of adult patients attending a dental institution in Vadodara city, Gujarat, India. Indian J Dent Res. 2011;22:179–180. doi: 10.4103/0970-9290.79989. [DOI] [PubMed] [Google Scholar]