Abstract
A Dutch family (family A) with inherited antithrombin-III deficiency and an increased incidence of venous thrombosis was investigated. Antithrombin-III levels were measured by means of a coagulation assay in plasma and by single radial immunodiffusion in plasma and serum.
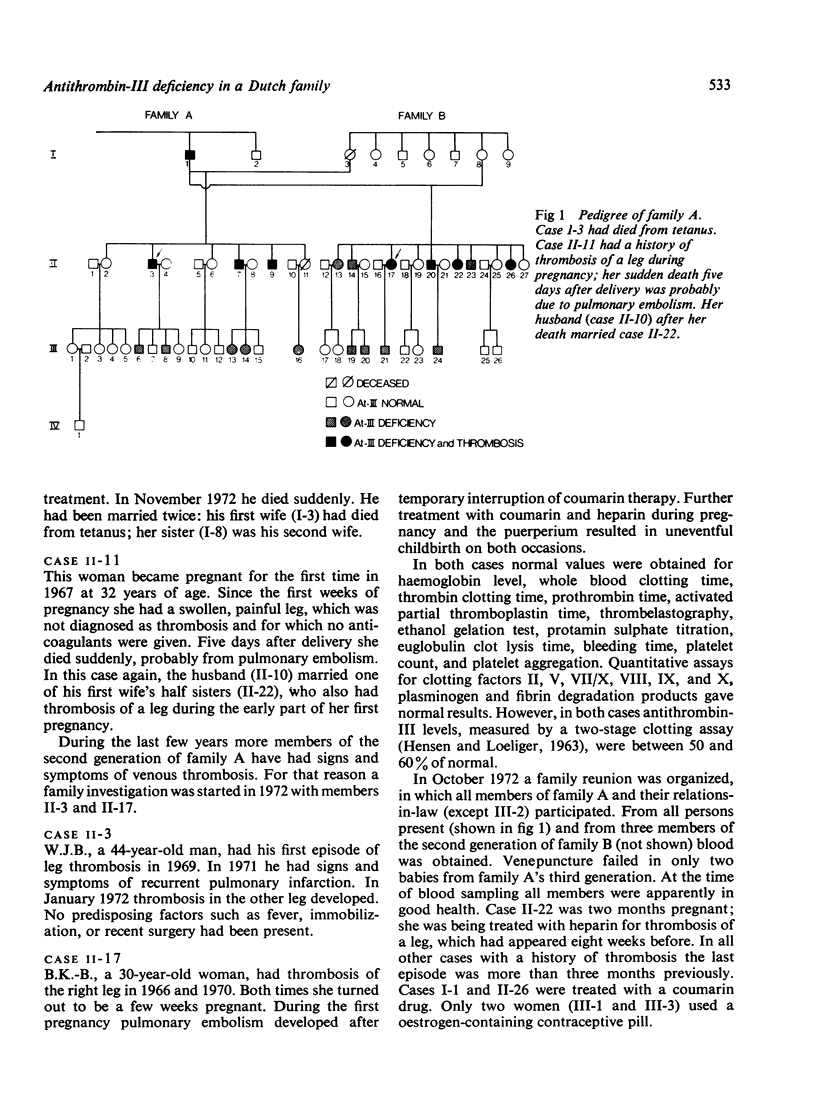
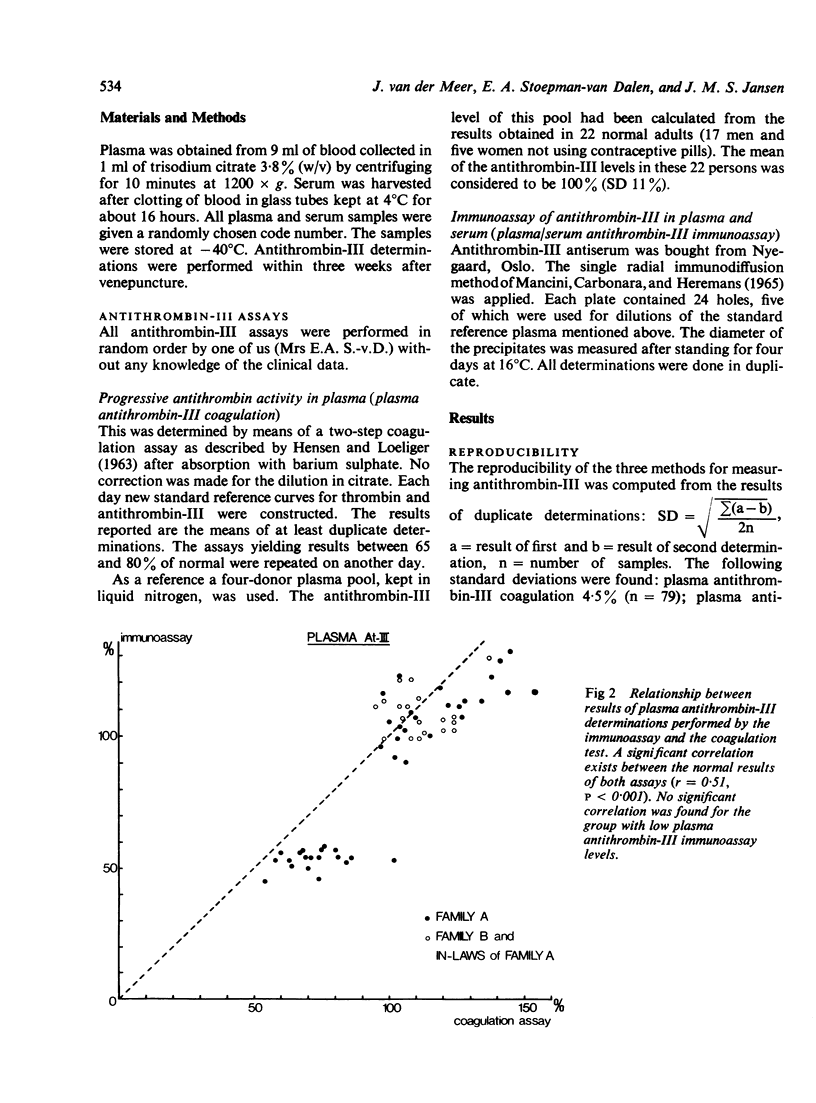
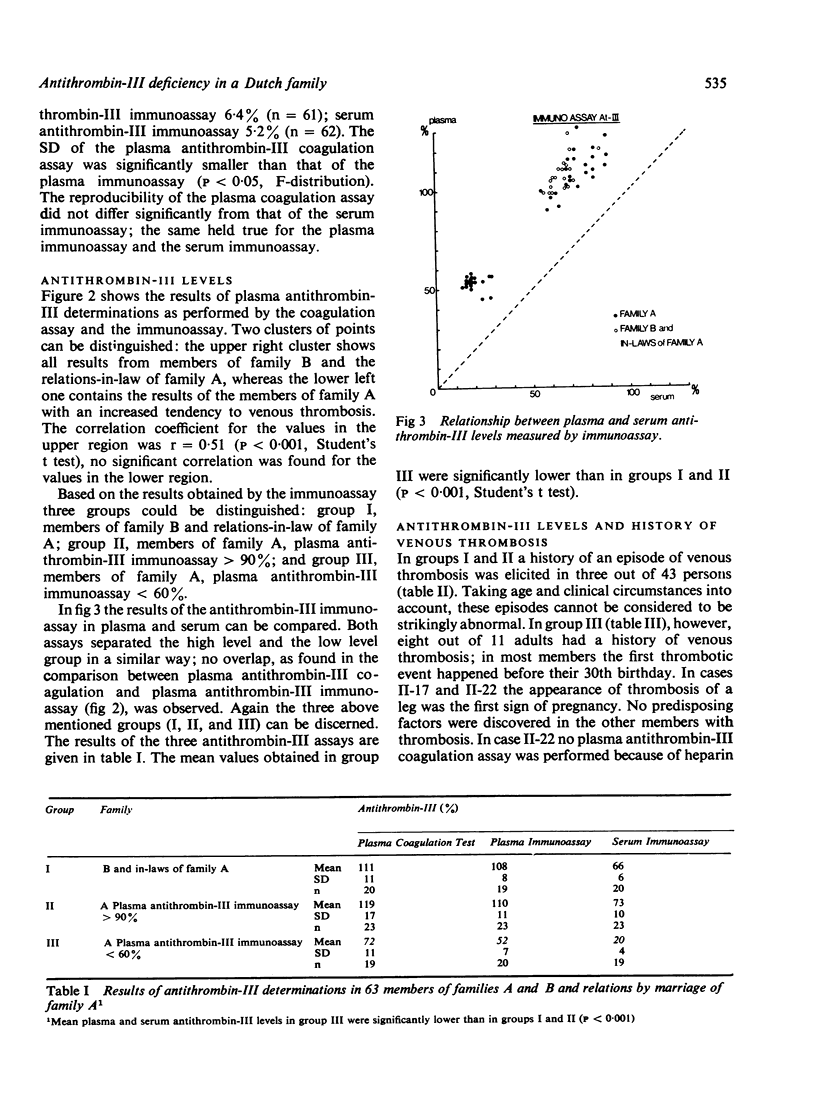
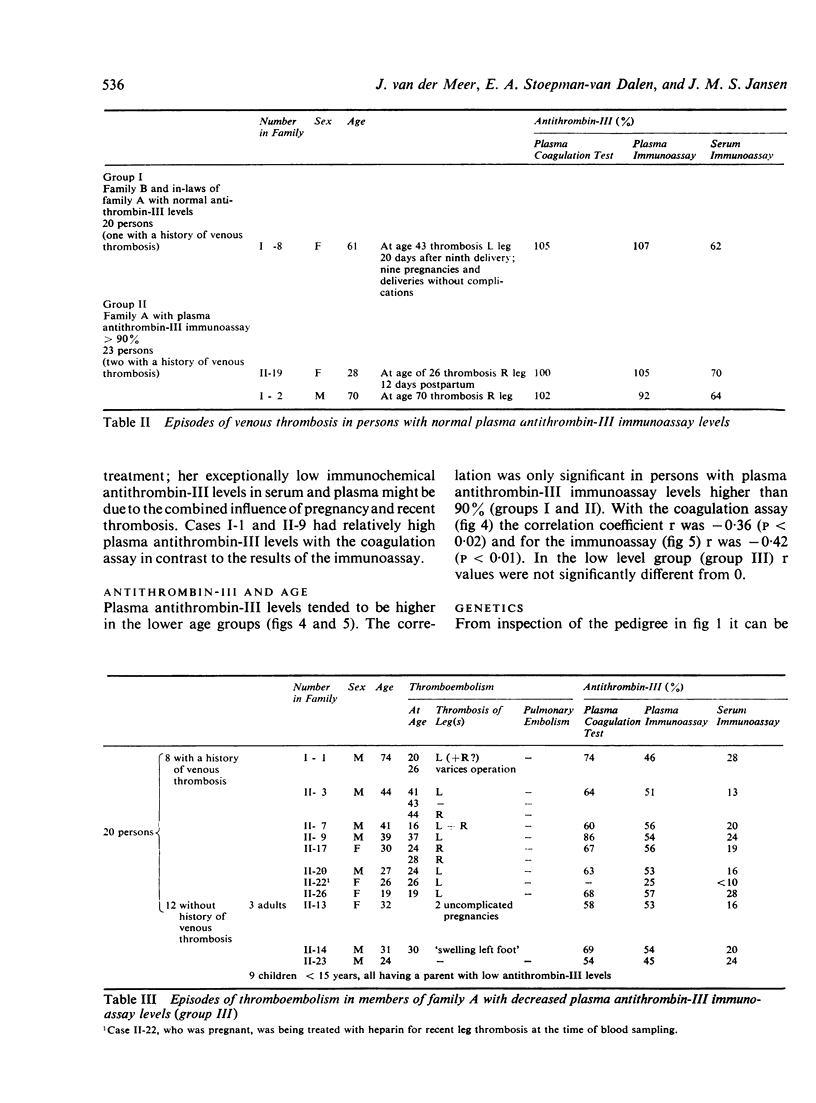
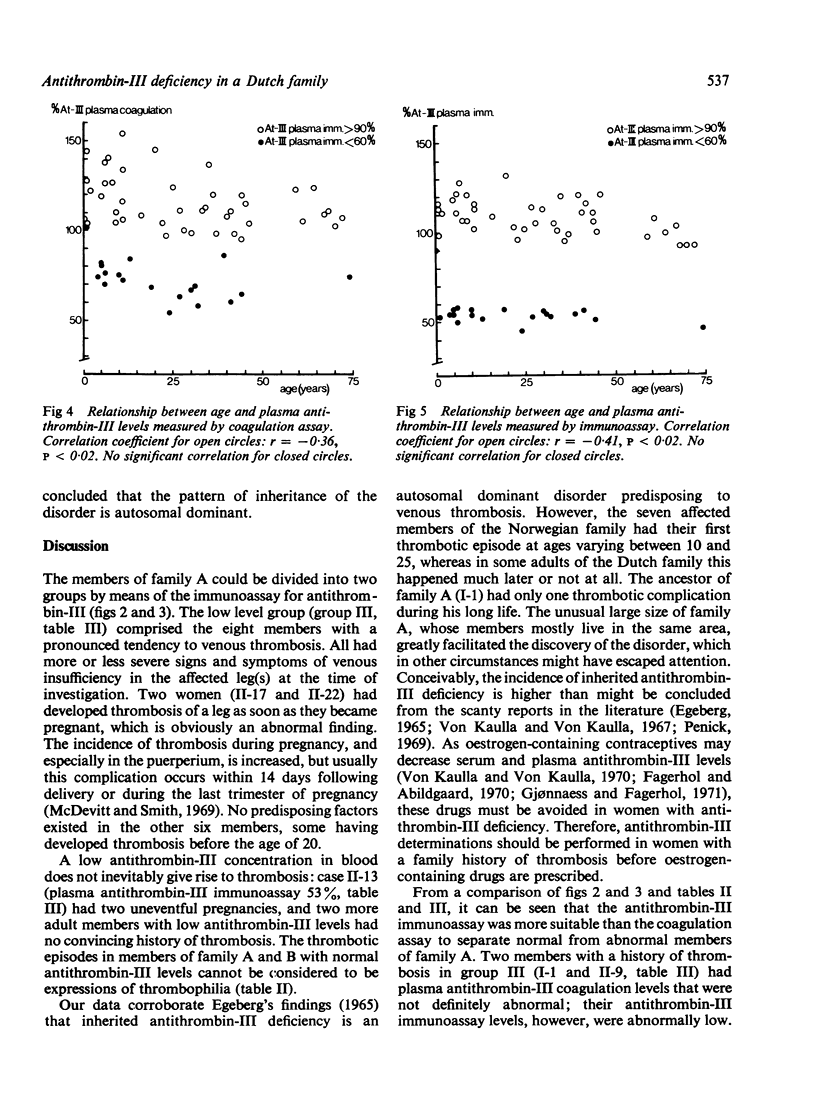
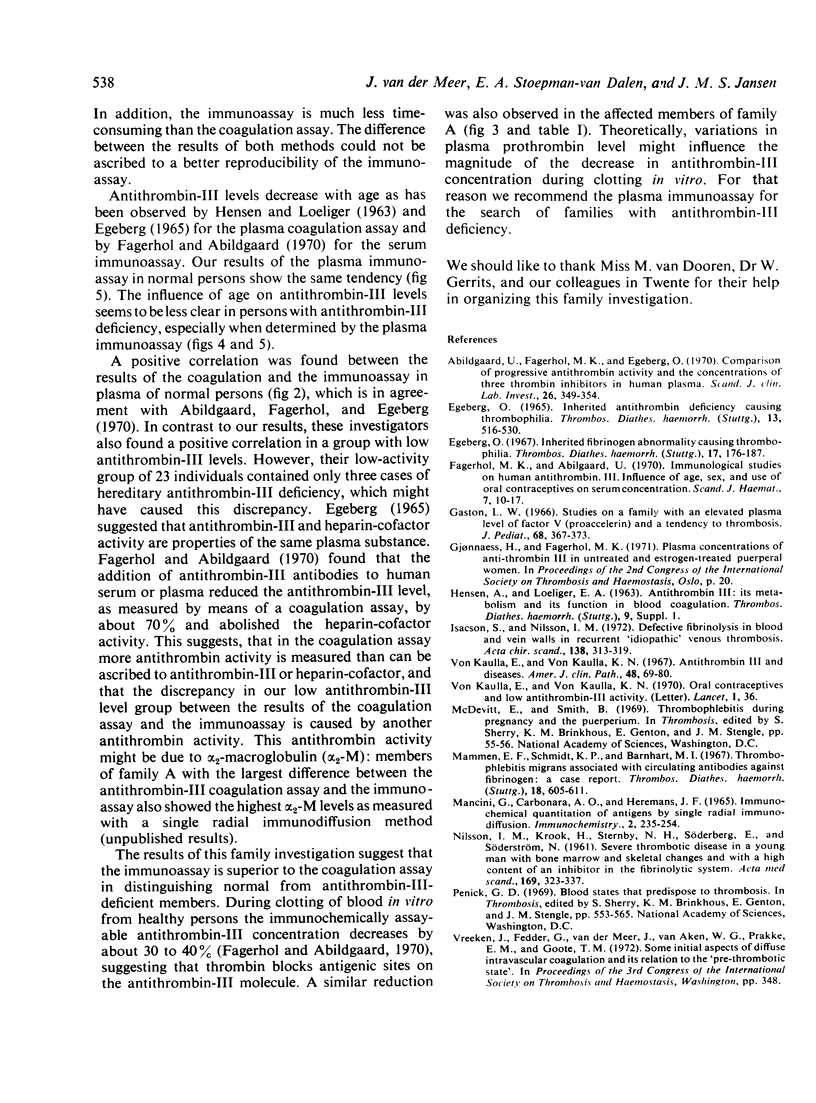
Three groups could be distinguished: group I comprised the relations-in-law of family A, group II the members of family A with a plasma antithrombin-III level higher than 90% of normal, when determined by the immunoassay, and group III the members of family A with an antithrombin-III level of less than 60%. To group III belonged all eight adults with an abnormal tendency to thrombosis, and furthermore nine children, all having a parent with abnormally low antithrombin-III levels. Mean plasma and serum antithrombin-III levels were significantly decreased in group III. However, the results of the coagulation assay showed some overlap between groups II and III. In addition, the immunoassay appeared to be much less laborious than the coagulation assay. Therefore, the former assay is recommended in any search for similar families.
The results of our family investigation confirm the findings of Egeberg (1965) that inherited antithrombin-III deficiency, giving rise to plasma levels between 50 and 60% of normal, causes thrombophilia and that the pattern of inheritance is autosomal dominant.
Full text
PDF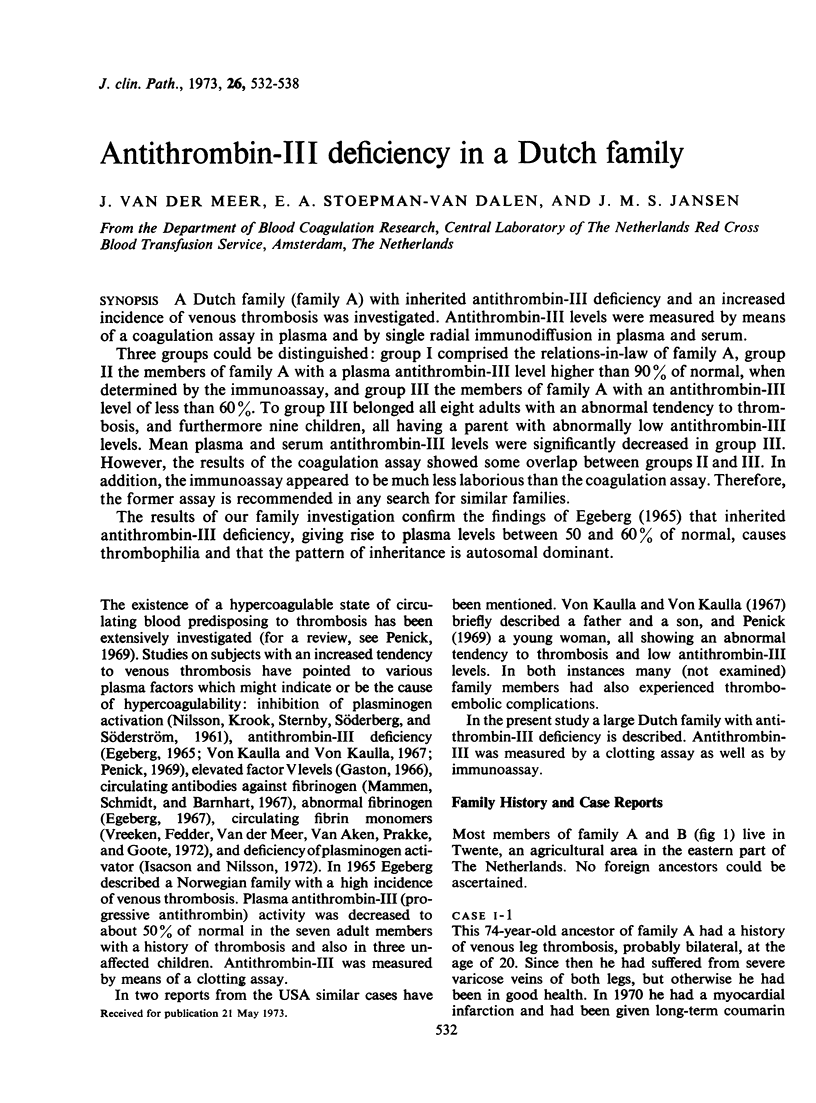
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abildgaard U., Fagerhol M. K., Egeberg O. Comparison of progressive antithrombin activity and the concentration of three thrombin inhibitors in human plasma. Scand J Clin Lab Invest. 1970 Dec;26(4):349–354. doi: 10.3109/00365517009046245. [DOI] [PubMed] [Google Scholar]
- EGEBERG O. INHERITED ANTITHROMBIN DEFICIENCY CAUSING THROMBOPHILIA. Thromb Diath Haemorrh. 1965 Jun 15;13:516–530. [PubMed] [Google Scholar]
- Egeberg O. Inherited fibrinogen abnormality causing thrombophilia. Thromb Diath Haemorrh. 1967 Feb 28;17(1-2):176–187. [PubMed] [Google Scholar]
- Fagerhol M. K., Abildgaard U. Immunological studies on human antithrombin 3. Influence of age, sex and use of oral contraceptives on serum concentration. Scand J Haematol. 1970;7(1):10–17. [PubMed] [Google Scholar]
- Gaston L. W. Studies on a family with an elevated plasma level of factor V (proaccelerin) and a tendency to thrombosis. J Pediatr. 1966 Mar;68(3):367–373. doi: 10.1016/s0022-3476(66)80239-1. [DOI] [PubMed] [Google Scholar]
- Isacson S., Nilsson I. M. Defective fibrinolysis in blood and vein walls in recurrent "idiopathic" venous thrombosis. Acta Chir Scand. 1972;138(4):313–319. [PubMed] [Google Scholar]
- Mammen E. F., Schmidt K. P., Barnhart M. I. Thrombophlebitis migrans associated with circulating antibodies against Fibrinogen. A case report. Thromb Diath Haemorrh. 1967 Dec 31;18(3-4):605–611. [PubMed] [Google Scholar]
- Mancini G., Carbonara A. O., Heremans J. F. Immunochemical quantitation of antigens by single radial immunodiffusion. Immunochemistry. 1965 Sep;2(3):235–254. doi: 10.1016/0019-2791(65)90004-2. [DOI] [PubMed] [Google Scholar]
- NILSSON I. M., KROOK H., STERNBY N. H., SODERBERG E., SODERSTROM N. Severe thrombotic disease in a young man with bone marrow and skeletal changes and with a high content of an inhibitor in the fibrinolytic system. Acta Med Scand. 1961 Mar;169:323–337. doi: 10.1111/j.0954-6820.1961.tb07838.x. [DOI] [PubMed] [Google Scholar]
- Von Kaulla E., Von Kaulla K. N. Antithrombin 3 and diseases. Am J Clin Pathol. 1967 Jul;48(1):69–80. doi: 10.1093/ajcp/48.1.69. [DOI] [PubMed] [Google Scholar]
- von Kaulla E., von Kaulla K. N. Oral contraceptives and low antithrombin-3 activity. Lancet. 1970 Jan 3;1(7636):36–36. doi: 10.1016/s0140-6736(70)90543-x. [DOI] [PubMed] [Google Scholar]


