Abstract
Objective
To understand decision-making when bringing a child to an emergency department.
Design
A cross-sectional survey of parents attending with children allocated a minor triage category.
Setting
Emergency department in South West England, serving 450,000 people per annum.
Participants
All English-speaking parents/caregivers whose children attended the emergency department and were triaged as minor injury/illness.
Main outcome measures
Parental and child characteristics, injury/illness characteristics, advice seeking behaviour, views regarding emergency department service improvement, GP access and determinants of emergency department use.
Results
In sum, 373 responses were analysed. The majority of attendances were for minor injury, although illness was more common in <4 year olds. Most presentations were within 4 h of injury/illness and parents typically sought advice before attending. Younger parents reported feeling more stressed. Parents of younger children perceived the injury/illness to be more serious, reporting greater levels of worry, stress, helplessness and upset and less confidence. Parents educated to a higher level were more likely to administer first-aid/medication. Around 40% did not seek advice prior to attending and typically these were parents aged <24 and parents of <1 year olds. The main determinants of use were: advised by someone other than a GP; perceived urgency; perceived appropriateness. The need for reassurance also featured.
Conclusions
The findings suggest that it is difficult for parents to determine whether their child’s symptoms reflect minor conditions. Efforts should focus on building parental confidence and self-help and be directed at parents of younger children and younger parents. This is in addition to appropriate minor injury/illness assessment and treatment services.
Keywords: attitude to health, behaviour, decision-making, emergency departments, parents
Introduction
There has been a drive in the UK and abroad to identify strategies to reduce emergency department presentations. An examination of attendances in England from April 2011 to March 2012 (n = 15,056,095) categorised 11.7% as ‘inappropriate’. These were found to peak in early childhood and be elevated throughout late-teens and young adulthood, reducing steadily after age 27 years.1
Hospital Episode Statistics and Quarterly-Monitoring-Accident-and-Emergency returns provide an epidemiological picture of emergency department attendances in England. However, as the decision to attend with a child typically falls to parents, neither dataset enables examination of the processes behind their actions. Only a small number of studies have examined parents’ use of emergency departments for minor injury/illness.2–10 Surveys with parents of children assigned to non-urgent triage categories identified that 35%–48% made contact with primary care prior to attending and were then referred to the emergency department (48%–83.3%).8–10 Other commonly cited reasons for attendance were that the emergency department was viewed as the most appropriate place for care or that caregivers felt the expertise of staff or resources was required. Similar themes have been identified in interviews including the need for immediate reassurance and issues accessing primary care.2–6
Whilst these studies provide a picture of parents’ motivations, only one investigated a British population (based in Edinburgh in 2005).8 The aim of the present study was to use a semi-structured questionnaire to understand the decision-making processes and actions of parents who bring their children to an emergency department in South West England with minor injury or illness. The focus was not to determine ‘appropriateness’ of use but to supplement existing knowledge and inform local policy. This research was also timely given the current focus on reducing emergency department waiting times.
Methods
Study design and setting
In a cross-sectional design, the Use-of-Paediatric-Emergency-Department Questionnaire (Supplementary File 1) was administered to parents/caregivers (referred to as parents throughout) attending a Type 1 emergency department located in a residential area of Plymouth, South West England. Questions were based on a previous study8 and a local emergency department survey. The Use-of-Paediatric-Emergency-Department Questionnaire covered: (1) ‘You’ (information about the responder); (2) ‘The child who has come to the emergency department today’; (3) ‘Your visit to the emergency department today’. The questionnaire was piloted in the emergency department prior to use with an average completion time of 9.6 min (details available from the authors).
The hospital serves 450,000 people, with its emergency department providing full services 24/7 to 90,000 patients per year, of whom 16,000 are aged ≤18 years. There is no walk-in centre or Minor Injuries Unit on site although they are provided in other areas of the city.
Study population
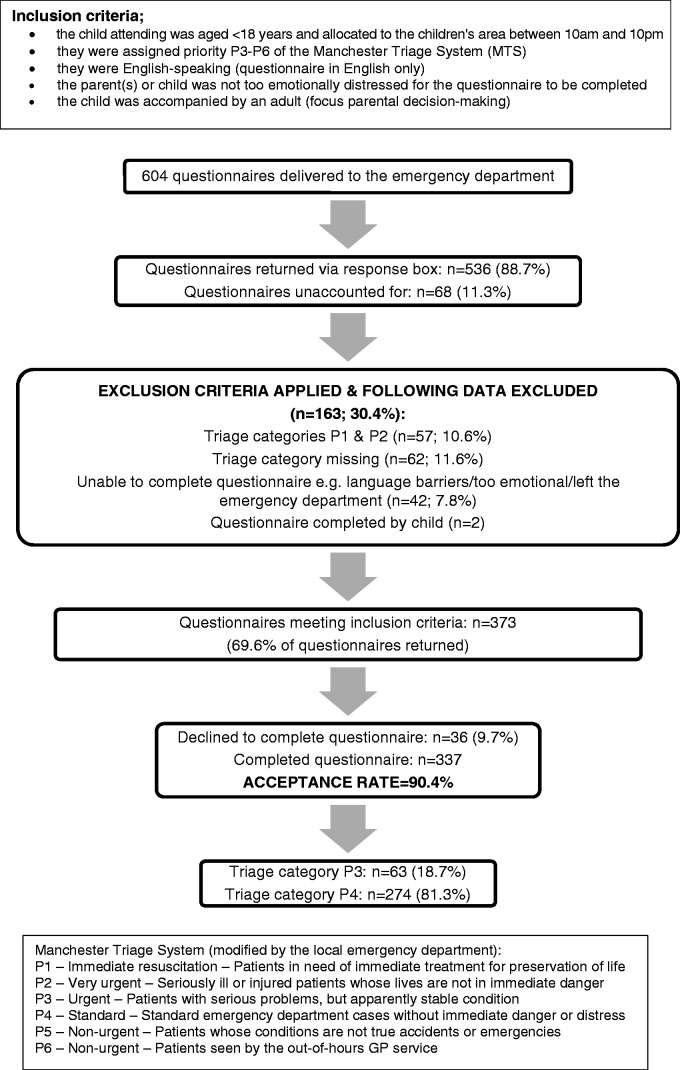
All parents who met the inclusion/exclusion criteria (Figure 1) were eligible. The Manchester Triage System (http://www.triagenet.net/en/) is widely implemented in the UK and a modified scale was used prospectively to identify parents of children triaged as P3–P6 (Figure 1). P3 and P4 include a mixture of standard emergency department cases and those who could have received treatment elsewhere.
Figure 1.
Flow of participants through study recruitment.
Study procedure
Parents attending the emergency department from 10:00 to 22:00, with a child aged ≤18 years old, are asked to wait in a children’s area prior to being seen (constituting 60% to 70% of all children attending at any time). During the study period (1–30 November 2012), a coded questionnaire was added to the booking packs by emergency department receptionists. Once the pack was completed, staff were asked to complete a detachable sheet on the questionnaire (Supplementary File 1). If allocated P3–P6, staff invited the parent to complete a questionnaire using a script. Parents were informed that completion/refusal to take part would not delay the child being seen or any treatment. All responses were non-identifiable.
Data analysis
The data were analysed using SPSS (V12). Responses were reported descriptively. Respondent and child characteristics were compared using appropriate parametric and non-parametric tests with adjusted p values following a Bonferoni correction (p = 0.01).
Results
Flow of participants through study recruitment
Figure 1 shows study recruitment (final n = 337). Based on local audits, 500–600 non-urgent attenders are expected at the emergency department each month. Using a 95% confidence interval with a 5% margin for error, and accounting for a 70% response rate (estimate based on previous survey), a sample size of 311 was required to detect a difference at p < 0.05. The sample represented 29.2% of all children (aged ≤ 18 years) who had attended the emergency department during November 2012 (17.8% of those triaged as P3; 34.1% P4).
Respondent characteristics
Table 1 shows that respondents were more likely to be parents (96.1%), female (79.5%), aged 25–44 years of age (71.2%) and co-habiting with a partner (75.1%). A greater proportion of respondents were living in more disadvantaged areas of the city. Most children were aged 1–4 years (30.3%) or 10–14 years (34.7%); 14.8% had an existing chronic condition.
Table 1.
Respondent characteristics (n = 337).
| Respondent characteristic | Frequency (%) | Respondent characteristic | Frequency (%) |
|---|---|---|---|
| Gender | Index of Multiple Deprivation deciles | ||
| Female | 268 (79.5) | 1 – Most deprived | 64 (19.0) |
| Male | 67 (19.9) | 2 | 77 (22.8) |
| Missing | 2 | 3 | 68 (20.2) |
| Age groupa | 4 | 58 (17.2) | |
| ≤24 years | 23 (6.8) | 5 – Least deprived | 43 (12.8) |
| 25–34 | 110 (32.6) | Missing | 27 (8.0) |
| 35–44 | 130 (38.6) | Ethnicity | |
| ≥45 | 49 (14.5) | White | 327 (97.0) |
| Missing | 25 (7.4) | Other (Black, Mixed, Asian, Arabic, British/Egyptian) | 8 |
| Relationship to childb | Missing | 2 | |
| Parent/Guardian | 324 (96.1) | Relationship status | |
| Grandparent | 8 | Married/living with partner | 253 (75.1) |
| Friend | 2 | Single | 78 (23.1) |
| Other (unknown) | 2 | Missing | 2 |
| Missing | 1 | Employment | |
| Qualifications | Working full-time | 117 (34.7) | |
| No qualifications | 39 (11.6) | Working part-time | 101 (30.0) |
| GCSE/equivalent | 67 (19.9) | Full-time caring for home/family | 70 (20.8) |
| NVQ | 96 (28.5) | Full-time education | 16 (4.7) |
| Further education | 38 (11.3) | Unemployed | 21 (6.2) |
| Higher education | 87 (25.8) | Other | 8 |
| Missing | 10 | Missing | 4 |
| Child Gender | Number of siblings | ||
| Female | 162 (48.1) | Only child | 62 (18.4) |
| Male | 171 (50.7) | 1 sibling | 154 (45.7) |
| Missing | 4 | 2 siblings | 72 (21.4) |
| Child age group | 3 or more siblings | 44 (13.1) | |
| <1 year | 22 (6.5) | Missing | 5 |
| 1–4 years | 102 (30.3) | Child chronic conditionsc | |
| 5–9 years | 67 (19.9) | None | 274 (81.3) |
| 10–14 years | 117 (34.7) | 1 or more condition | 50 (14.8) |
| 15–18 years | 25 (7.4) | Missing | 13 (3.9) |
| Missing | 4 |
Adult age was normally distributed but grouped into categories for the purpose of the analysis. Categories were chosen due to small numbers in the younger age groups.
Relationship to child was re-coded for the purposes of the analysis into ‘parent/guardian’ and ‘other’.
Chronic conditions were re-grouped into ‘none’ and ‘1 or more’ because a number of cell counts had expectancies <5.
Emergency department attendance and injury/illness characteristics
Table 2 reports emergency department attendance and injury/illness characteristics. Children attended the emergency department from 09:09 to 21:45, with an average distance travelled (home-hospital) of four miles (90.0% located within 10 miles). Most children presented with an injury (81.3%). There was a significant association between child age and reason for attendance (X2 = 39.518, df = 8, p ≤ 0.001) – with 10–14 year olds making up the greatest proportion of all those presenting with injuries (38.1%), followed by 1–4 year olds (29.3%). One- to 4-year olds made up the greatest proportion of all those presenting with an illness (40.8%) followed by <1 year olds (24.5%).
Table 2.
Emergency department attendance and injury/illness characteristics (n = 337).
| Emergency department attendance characteristic | Frequency (%) | Emergency department attendance characteristic | Frequency (%) |
|---|---|---|---|
| Day of attendance | Mode of travel to emergency department | ||
| Monday | 53 (15.7) | Ambulance | 8 |
| Tuesday | 50 (14.8) | Own car | 261 (77.4) |
| Wednesday | 35 (10.4) | Lift in another car | 42 (12.5) |
| Thursday | 57 (16.9) | Bus | 6 |
| Friday | 40 (11.9) | Taxi | 13 (3.9) |
| Saturday | 39 (11.6) | Walked | 2 |
| Sunday | 57 (16.9) | Missing | 5 |
| Missing | 6 | ||
| Reason for attendance | Duration of injury/illness | ||
| INJURY (TOTAL) | 274 (81.3) | <4 h | 197 (58.5) |
| Injury P3 | 35 (10.4) | 4–24 h | 75 (22.3) |
| Injury P4 | 239 (70.9) | 2–7 days | 37 (11.0) |
| ILLNESS (TOTAL) | 52 (15.4) | >7 days | 23 (6.8) |
| Illness P3 | 25 (7.4) | Missing | 5 |
| Illness P4 | 27 (8.0) | ||
| REASON NOT CLEAR | 11 (3.3) | ||
| P3 | 3 | ||
| P4 | 8 | ||
| Perceived need for assessment (urgency) | Reported self-help administered prior to attendance | ||
| Immediately | 145 (43) | None given | 187 (55.5) |
| Today | 178 (52.8) | Self-help used | 141 (41.8) |
| Within a few days | 7 | Medicine | 91 (27) |
| Missing | 7 | First aid | 37 (11) |
| Medicine & first aid | 10 | ||
| Other | 3 | ||
| Missing | 9 | ||
| Previous emergency department attendance(s) for same injury/illness | Number of emergency department attendances for same injury/illness | ||
| Yes | 76 (22.6) | n | 55 |
| No | 247 (73.3) | Median | 1 |
| Don’t know | 6 | Interquartile range | 5 |
| Missing | 8 | Range (min–max) | 1–6 |
| Perceived seriousness of injury/illness | Level of confidence in dealing with the injury/illness | ||
| n | 323 | n | 321 |
| Possible scale | 1 (very serious) to 10 (not at all serious) | Possible scale | 1 (not at all confident) to 10 (very confident) |
| Mean | 5.25 | Median | 10 |
| Standard deviation | 1.895 | Interquartile range | 9 |
| Range (min–max) | 1–10 | Range (min–max) | 1–10 |
| Perceived helplessness | Level of stress | ||
| n | 315 | n | 318 |
| Possible scale | 1 (very helpless) to 10 (not at all helpless) | Possible scale | 1 (very stressed) to 10 (not at all stressed) |
| Median | 10 | Median | 9 |
| Interquartile range | 9 | Interquartile range | 9 |
| Range (min–max) | 1–10 | Range (min–max) | 1–10 |
| Level of worry | Level of upset | ||
| n | 318 | n | 314 |
| Possible scale | 1 (very worried) to 10 (not at all worried) | Possible scale | 1 (very upset) to 10 (not at all upset) |
| Median | 7 | Median | 8 |
| Interquartile range | 9 | Interquartile range | 9 |
| Range (min–max) | 1–10 | Range (min–max) | 1–10 |
| Level of confidence in looking after unwell child generally | Advice sought prior to attendance? | ||
| n | 327 | No | 130 (38.6) |
| Possible scale Median Interquartile range Range (min-max) | 1 (not at all confident) to 10 (very confident) 10 7 3–10 | Yes Child’s GP Walk in centre/ Minor Injuries Unit Family School/nursery NHS direct GP receptionist Friend/neighbour Out-of-hours doctors Other GP Internet Called emergency department Pharmacy Health visitor/Midwife Book Other (range given) | 201 (59.6) 49 (14.5) 39 (11.6) 36 (10.7) 35 (10.4) 34 (10.1) 16 (4.7) 12 (3.6) 11 (3.3) 10 9 9 6 3 1 14 (4.2) |
| GP Advice (if sought) | Missing | 6 | |
| n | 71 | Useful resources identified to help look after a child who is injured/unwell: | |
| Go to emergency department Injury Illness Missing | 42 (12.5) 28 (66.7) 13 (31) 1 | ||
| Told how to treat problem | 16 (4.7) | Leaflets | 130 (39) |
| Make urgent GP appointment | 6 | Internet | 114 (33.8) |
| Other (not known) | 4 | Better access to GP during non-working hours | 114 (33.8) |
| Make non-urgent GP appointment | 3 | Better access to GP during working hours | 106 (31.5) |
| Access to a GP at the emergency department | 47 (13.9) |
Parent variables
Whilst self-reported stress in dealing with the child’s injury/illness was typically low (Table 2), parents aged ≤24 years reported feeling significantly more stressed than parents aged 25–34 (U = 661.500, p = 0.002), 35–44 (U = 690.500, p ≤ 0.0005) and ≥45 years (U = 288.50, p = 0.009).
Level of confidence in looking after an ill child generally was significantly associated with Index of Multiple Deprivation 2010 scores (X2 = 7.778, df = 4, p = 0.018): confidence was lower for respondents in the least deprived quintile (median = 8, interquartile range = 2) compared to respondents in the most deprived quintile (median = 10, interquartile range = 1) – a lower score from 1 to 10 indicated less confidence (Table 2).
Table 3 (Supplementary File 2) shows that child age was significantly associated with perceived seriousness, level of worry, level of stress, perceived helplessness and level of upset: parents of younger children reported feeling more worried, more stressed, more helpless, more upset, and less confident in looking after the child with illness or injury. Parents also perceived significantly greater severity if the child was aged <1 year old compared to older children up to 15 years.
Advice seeking
Parents aged ≤24 years were less likely to seek advice than older parents (X2 = 11.447, df = 3, p = 0.010). There was also a significant association between child age and seeking advice (X2 = 9.875, df = 4, p = 0.043): parents of <1 year olds (8.0%) and 15–18 year olds (8.0%) were less likely to seek advice prior to using the emergency department.
Parents who had been educated to a higher level were significantly more likely to use first aid or medication than parents with no recorded qualifications (X2 = 9,914, df = 4, p = 0.042). Of those who spoke to a GP prior to coming to the emergency department (n = 71), 59.2% were advised to attend (66.7% injury vs. 31% illness) (Table 2).
Health service improvement
33.8% of parents reported that they wanted better access to their GP during non-working hours, 31.5% during working hours, and 13.9% felt that access to a GP at the emergency department would be beneficial. A minority of parents commented on the lack of appropriate provision for paediatric cases at Minor Injuries Units.
Determinants of emergency department use
The main self-reported determinants of emergency department use were as follows: someone other than a GP advising attendance (28.5% reported this as a determinant, with 18.7% reporting this as the main influence); perceived urgency (30.9% reported this as a determinant, 14.8% as the main influence); and perceived appropriateness of destination (35.0% reported this as a determinant, 11.3% as the main influence) (Table 4, Supplementary File 3). Referrals to the emergency department were predominantly by the local Minor Injuries Unit, NHS Direct and schools. The need for reassurance was a key determinant for parents of children presenting with illness. Most parents reported one (30.7%) or two (29.6%) determinants of emergency department use, although 19% reported four or more influences.
Discussion
The majority of presentations were for minor injury, although illness was more common in <4 year olds. Most presentations were within 4 h of symptoms or injury and parents typically sought advice before attending. The main determinants of attendance were: someone other than a GP advising attendance; perceived urgency; perceived appropriateness of destination. The need for reassurance was a key determinant for parents of children presenting with an illness.
Overall the response rate was high, however 11.3% of questionnaires went missing and 9.7% declined to take part which may introduce bias, particularly as data regarding non-responders was not collected. Whilst the questionnaire was based on previous surveys and piloted, it relied on self-report and may be subject to recall bias. Moreover, as most young adults aged 16–18 are unlikely to use the children’s area, some may have been excluded.
As respondents were mostly White British, recruited via one emergency department in South West England, and sampling failed to capture seasonal variation and represented one third of attenders, the external validity of the findings may have been compromised. The finding that 22.6% reported a previous attendance for the same illness or injury needs to be explored as this seems particularly high. A positive association between lower deprivation category and increased frequency of previous attendances (p = 0.01) has been reported previously and positive past experiences were found to influence future use.8
The finding that injury formed the majority of minor attendances, despite the existence of a local Minor Injuries Unit and the study taking place late autumn/early winter, warrants investigation. As perceived urgency was high, and self-reported duration short, this supports the suggestion that the decision to come to the emergency department is based on the belief that the child needs to be seen quickly and that this is the most appropriate service destination.8 Previous research has found that parents were more likely to attend the emergency department promptly if the child presented with an injury.9
This study highlights the demand on paediatric the emergency departments, particularly from parents of young infants who typically reported higher perceived severity, and feeling more worried, stressed, helpless and upset, and less confident, than older parents. Previous interviews have found that perceptions of vulnerability increased perceptions of severity, and this was related to being an infant/toddler or first child and the family’s medical history.4
The emergency department self-referral rate of 40% was lower than reported previously (52–70%).7–9 Across all ages, parents were more likely to seek advice than not, especially if aged ≤24 years. This may be related to the finding that levels of stress were significantly higher for these parents. Similarly, parents of very young children were typically less likely to seek advice than parents of older children, which could be related to perceived urgency and the need for reassurance.
Although lack of access to primary care has been highlighted as a key determinant of emergency department use,1,3,4,7,9,10 this was not a finding of the present study. Interestingly, although parents’ feedback was generally positive, the proportion contacting primary care prior to attendance was considerably less than identified previously (35%–48%).8–10 Of those who did make contact, referrals to the emergency department by GPs were high (around 60%) and in the middle of the range reported previously (48%–83.3%).8–10 Indeed, around 14% of parents reported that they would not use primary care because the ‘GP would advise them to come to the emergency department anyway’. Exploration of GP referrals by symptom revealed that nearly 70% of children had an injury, suggesting that emergency department referral was appropriate. However, as one third of referrals presented with an illness, it can also be speculated that these children could have received treatment in primary care.
Parental interviews have identified the need for reassurance as an essential part of decision-making, along with the view that the emergency department is equipped to deal with any situation.2,6,7 Previous research found that parents of injured children commonly thought that it was an emergency, whereas parents of non-injured children were more likely to be seeking reassurance.6 The findings of the present study suggest that both parental and child age may also be a factor.
The suggestion that around half of parents did not administer any first-aid/medication prior to attendance, and those educated to a higher level were more likely to use self-help, indicates that first-aid education could be beneficial. Previous non-UK studies have reported higher levels of self-help9,10 although this may reflect cultural differences. Qualitative research is also needed to explore the finding that parents in the least deprived quintile reported significantly lower levels of confidence in looking after an ill or injured child as evidence suggests that attendances are most frequent amongst disadvantaged communities.1
As reported previously,8 parents did not appear to be using the emergency department for geographical or social convenience (Table 4). The finding that the emergency department was perceived to be the most appropriate service has been reported previously.8 However, as ‘advised by a Minor Injuries Unit, school or NHS Direct’ was frequently reported as the main determinant, this warrants investigation. It is possible that the local Minor Injuries Unit may not be adequately equipped to deal with P4 injuries. For example, some do not have x-ray capability beyond certain times of the day yet remain open. The appropriateness of NHS Direct advice could be further explored and work with schools may be beneficial.
Conclusion
The need for reassurance was a key determinant for parents of children presenting with an illness. The College of Emergency Medicine has recently produced a multi-agency report (https://www.rcplondon.ac.uk/sites/default/files/acute_and_emergency_care_prescribing_the_remedy.pdf) outlining recommendations to address the pressures faced by emergency services. The report states that it is unreasonable to expect patients to determine whether their symptoms reflect serious illness or more minor conditions. They suggest that co-locating a primary care out-of-hours facility alongside the emergency department would allow patients to be streamed to the most appropriate care providers without being turned away.
The findings that parents (particularly of younger children) attend early, admit to feeling worried or unable to cope, and overestimate the seriousness of the illness or injury support these recommendations. Future work is needed to explore the views of service providers and those who do not attend the emergency department or use other services. It will also be important to examine the impact of NHS 111 telephone line on decision-making as this was introduced following the study.
Supplementary Material
Supplementary Material
Supplementary Material
Acknowledgements
The authors would like to thank all emergency department staff, patients and their parents/caregivers at Derriford Hospital’s Emergency Department who contributed to this study. In particular, the authors would like to thank Anita Dykes, Sarah-Jane Sharman, Rosalyn Squire, Dr Richard Crosthwaite-Eyre, Dr Dafydd Jones and Dr Julie Frier for their comments on the study protocol and questionnaire. Anita Dykes was instrumental in setting up the study within the emergency department. The authors also thank Dr Iain Lang for his comments on a draft of the paper. Finally, the authors would like to thank the Office of the Director of Public Health, Plymouth City Council, and in particular Professor Kelechi Nnoaham (Director of Public Health), for covering the costs associated with the publication of this paper.
Declarations
Competing Interests
None declared
Funding
All study costs were covered by the Public Health Development Unit (NHS Plymouth) where SO and KH were based at the time of the research. The PHDU has since transitioned into the Office of the Director of Public Health, Plymouth City Council. The Office of the Director of Public Health covered the costs associated with publishing this paper.
Ethical approval
The study was assessed by the Cornwall and Plymouth Research Ethics Committee and did not require approval. The protocol was approved locally by Plymouth Hospitals NHS Trust.
Guarantor
SO
Contributorship
SO and KH: study concept and design, questionnaire development, data collection, data analysis, data interpretation and drafting of the manuscript. IH, AI, JS: assistance with setting up the project in emergency department, critical review of the study protocol and questionnaire and commenting on manuscript drafts.
Provenance
Not commissioned; peer-reviewed by Eugen-Matthias Strehle
References
- 1.McHale P, Wood S, Hughes K, Bellis MA, Demnitz U, Wykes S. Who uses emergency departments inappropriately and when – a national cross-sectional study using a monitoring data system. BMC Med 2013; 11: 258–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brousseau DC, Nimmer MR, Yunk NL, Nattinger AB, Greer A. Nonurgent emergency-department care: analysis of parent and primary physician perspectives. Pediatrics 2011; 127: e375–e375. [DOI] [PubMed] [Google Scholar]
- 3.Berry A, Brousseau D, Brotanek JM, Tomany-Korman S, Flores G. Why do parents bring children to the emergency department for nonurgent conditions? A qualitative study. Ambul Pediatr 2008; 8: 360–367. [DOI] [PubMed] [Google Scholar]
- 4.Woolfenden S, Ritchie J, Hanson R, Nossar V. Parental use of a paediatric emergency department as an ambulatory care service. Aust N Z J Public Health 2000; 24: 204–206. [DOI] [PubMed] [Google Scholar]
- 5.Chin NP, Goepp JG, Malia T, Harris L, Poordabbagh A. Nonurgent use of a pediatric emergency department: a preliminary qualitative study. Pediatr Emerg Care 2006; 22: 22–27. [DOI] [PubMed] [Google Scholar]
- 6.Stanley R, Zimmerman J, Hashikawa C, Clark SJ. Appropriateness of children’s nonurgent visits to selected Michigan Emergency Departments. Pediatr Emerg Care 2007; 23: 442–446. [DOI] [PubMed] [Google Scholar]
- 7.Gawronski O, Cerulli C. Non-urgent use of the Emergency Department of the Bambino Gesu Hospital: a cross sectional survey of parents’ motivations. Paediatr Child Health 2009; 19: S1–S1. [Google Scholar]
- 8.Hendry SJ, Beattie TF, Heaney D. Minor illness and injury: factors influencing attendance at a paediatric accident and emergency department. Arch Dis Child 2005; 90: 629–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Truman C, Rutter L. Care-giving and care-seeking behaviours of parents who take their children to an emergency department (ED) for non-urgent care. Can J Public Health 2002; 93: 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams A, O’Rourke P, Keogh S. Making choices: why parents present to the emergency department for non-urgent care. Arch Dis Child 2009; 94: 817–820. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.