Abstract
Background
The Affordable Care Act (ACA) requires that privately insured women can obtain contraceptive services and supplies without cost sharing. This may substantially affect women who prefer an intrauterine device (IUD), a long-acting reversible contraceptive, because of high upfront costs that they would otherwise face. However, imperfect enforcement of and exceptions to this provision could limit its effect.
Study design
We analyzed administrative data for 417,221 women whose physicians queried their insurance plans from January 2012 to March 2014 to determine whether each woman had insurance coverage for a hormonal IUD and the extent of that coverage.
Results
In January 2012, 58% of women would have incurred out-of-pocket costs for an IUD, compared to only 13% of women in March 2014. Differentials by age and region virtually dissolved over the period studied, which suggests that the ACA reduced inequality among insured women.
Conclusions
Our findings suggest that the cost of hormonal IUDs fell to US$0 for most insured women following the implementation of the ACA.
Implications
Financial barriers to one of the most effective methods of contraception fell substantially following the ACA. If more women interested in this method can access it, this may contribute to a decline in unintended pregnancies in the United States.
Keywords: Contraception, Healthcare reform, Out-of-pocket costs, IUD, LARC, Insurance
1. Introduction
In the United States, 43 million women are at risk of unintended pregnancy, and 39 million of them (90%) use contraception [1,2]. Some 30 million (78% of contraceptors) use a method more effective than condoms, and 4 million (10%) use an intrauterine device (IUD), while fewer than a half million use another long-acting reversible method [1,3]. Fewer than 1% of women who use IUDs will become pregnant within a year, in contrast to 18% of women who use condoms to prevent pregnancy, and 9% of women who use the pill [4].
Women who would otherwise prefer the IUD face barriers that can lead them to use less effective contraceptives; these include high upfront costs that can exceed a thousand dollars[5–11]. Greater uptake of the IUD and the implant preceded fewer births in Colorado and fewer abortions in Iowa, and in St. Louis, teenagers provided these methods at no-cost exhibited rates of pregnancy, birth and abortion far lower than the national average [8,12,13].
Insurance mandates may help women to access the contraceptive of their choice. In 1993, 32% of insurers covered the IUD [14]. By 2002, in part because insurance mandates came into effect in many states, this increased to 94% [14]. However, when an insurance company covers a contraceptive, a woman may still incur costs — for example, women may incur copayments for the prescription and visits to a doctor’s office or clinic.
A provision of the Affordable Care Act (ACA) requires that patients do not face out-of-pocket costs for contraceptive services and supplies at in-network providers. This provision matters particularly in the context of the high upfront costs of an IUD. This ACA mandate phased in starting in August 2012, and it took effect for many health insurance plans in January 2013. This may improve the ability of millions of women to afford safe and effective contraception [15].
The ACA can affect insurers exempt from state mandates, whereas states lacked authority over self-funded employer plans. However, other exceptions may limit the effect of the ACA’s contraceptive coverage mandate. These include grandfathered insurance plans and the contraceptive exclusion. Grandfathered plans are those that came into being no later than March 2010 and have not seen substantial benefit changes since then [16]. The contraceptive exclusion exempts certain religious employers from the ACA’s contraceptive coverage provision. As such, even if insurance companies adhere perfectly to the law, some women covered by private insurance may still have to pay the full cost of the IUD and other contraceptives.
Women interested in an IUD may face a higher financial burden if their insurance plan requires out-of-pocket costs. In addition to the cost of the device itself and the initial doctor’s visit, women may also face costs to insert and remove their IUD [5–7,10,17]. In 2002, a year after the hormonal IUD came on the market (complementing the nonhormonal copper IUD, which had been available in the United States since 1988), 94% of insurers covered IUDs, but cost sharing continued to make the IUD unaffordable for many women interested in it [8,9,14].
To understand the impact of the ACA’s contraceptive coverage provision on IUD cost sharing, we would need to know what costs women faced before and after the ACA. Unfortunately, the extant literature on IUD cost sharing after the ACA went into effect is limited. One analysis estimated that full coverage increased from 45% to 62% after the ACA, based on data from 165 privately insured women [18]. Data from the National Survey of Family Growth (NSFG), the best available representative survey of women’s contraceptive behavior, do not indicate when women obtained their IUDs or how much they paid. Even if the NSFG asked women how much they paid, this information would not provide us the percentage of women seeking an IUD who faced out-of-pocket costs: if cost inhibits IUD uptake, the extant data will underrepresent women with higher costs [8–10]. All surveys that measure cost based on women who obtained IUDs share this limitation, as do claims data. Finally, none of these surveys address the effect of the contraceptive exclusion, which exempts certain religious employers from providing full coverage.
To help address these limitations, we analyzed data on insurance inquiries; these show what an insured woman would have paid if she had chosen to obtain an IUD, between January 2012 and March 2014, a period covering the introduction of the ACA’s contraceptive coverage provision and its initial implementation for many plans.
2. Materials and methods
2.1. Data
Bayer HealthCare, the manufacturer of the Mirena® and Skyla® IUDs, used by some 3 of 4 million American IUD users [3] offers a voluntary “benefit inquiry” service to healthcare providers to determine the type and extent of a patient’s insurance coverage for an IUD and whether the patient’s insurance company requires cost sharing. Bayer utilizes an outside benefits-verification contractor and does not obtain the data directly. Within a few days after a healthcare provider’s inquiry, typewritten reports with a narrative summary of coverage are faxed by the contractor to healthcare providers, and details of each benefit inquiry are recorded in the contractor’s database1. Though healthcare providers can pursue this information independently, they may elect to use this free service to reduce their administrative caseload.
The dataset we obtained contained 444,316 women whose physicians inquired about a Mirena or Skyla IUD between January 2012 and March 2014. Of these, we excluded 27,095 women from the analysis because they were minors (4,577, in order to focus on adults who were likely to have their own insurance), they had no insurance (11,363)2, a woman’s insurer would not reveal benefit information to a third party (10,382), women or their healthcare providers did not completely fill out the form (763), or the healthcare provider canceled the inquiry (10). The resulting number of cases we analyzed was 417,221.
The analysis period includes time both before and after the ACA’s key provision regarding contraceptive coverage took effect, which allowed us to study its impact. We hypothesized that there would be a sharp decline in the percentage of women subject to cost sharing in the first quarter of 2013, since patients with existing coverage typically sign up for new plans or renew their insurance at the beginning of a calendar year, and January 2013 was the first new year after the implementation of the ACA’s contraceptive coverage provision.
2.2. Methods
We analyzed changes between January 2012 and March 2014 in the percentage of women who would have had out-of-pocket costs for a hormonal IUD. The ACA’s contraceptive coverage provision came into effect in August 2012, but did not affect most women until January 2013, as most employer-based insurance plans are typically renewed on January 1.
For 2013 onward (n=231,086), we assessed how these results were affected when taking into account two additional factors that affect cost sharing: copayment for insertion and cost sharing owing to a deductible (data not available in 2012). This may affect our results as, for example, women whose insurers covered the cost of the device might not have interpreted the ACA mandate to apply to services as well as supplies.
We estimated trends for all women by month in whether a woman’s insurance coverage required cost sharing. We also estimated trends by quarter for age and region subgroups to examine inequality in coverage before, and after, the ACA came into effect.
In an analysis of a very large dataset, trivial fluctuations can reach statistical significance. It is therefore inappropriate to compare p-values, as, for example, a trivial decline of 0.01%, which might only reflect random fluctuations, may be described as “statistically” significant [19]. Therefore, we highlight the substantive size of change over time3.
In order to understand how much women who still have costs would be required to pay, we also computed cost estimates at the median and 90th percentiles. A woman’s out-of-pocket cost is the sum of a fixed copayment and the product of the IUD’s price and her coinsurance rate. Unfortunately, we do not know the price that a healthcare provider would charge a patient for the IUD. Therefore, for the 13% of women subject to coinsurance, we multiplied their coinsurance rate by the most recent published estimates for Mirena’s wholesale price, US$844 [7]. This strategy understates the actual cost because patients may also be required to pay for an initial visit to their healthcare provider and for the device’s insertion.
Finally, the dataset indicates whether a woman’s coverage was subject to the contraceptive exclusion for religious employers, and we use this to estimate the percentage of women without coverage who would have had coverage if not for this exclusion.
2.3. Sensitivity analyses
Of the women in our data, 50,804 have multiple insurers. We do not know their insurers’ names or why they have duplicative coverage. We suspect, for example, that some may have private insurance from their employer, as well as secondary insurance from Medicaid or their spouse’s employer. In our main analysis, we assumed that women with multiple insurers can choose which insurer to use. They may not have this choice, however4. Therefore, we performed a sensitivity analysis in which we assume that a woman with duplicative coverage must use whichever insurer offers the worst coverage.
3. Results
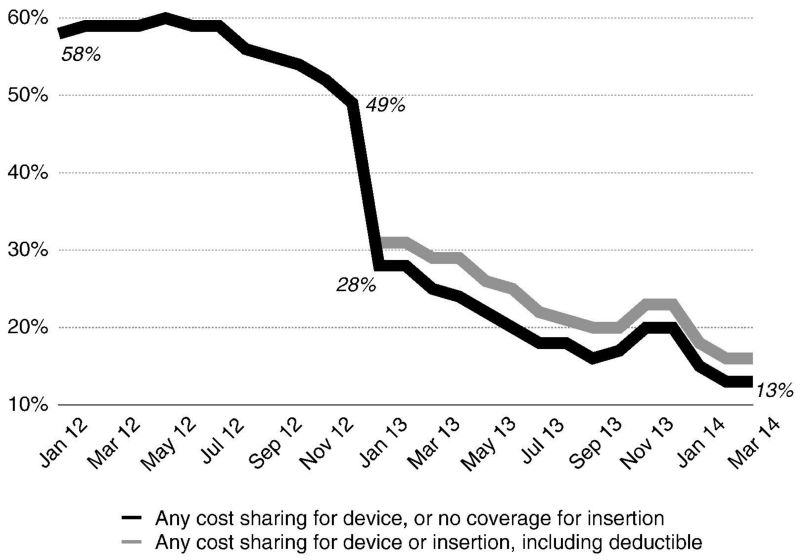
The black line in Fig. 1 shows the decreasing percentage of women who faced out-of-pocket costs for a hormonal IUD (and at least some cost for its insertion) over the 27 months between January 2012 and March 2014. In January 2012, out-of-pocket costs were required of 58% of insured patients; by March 2014, this number dropped to 13%. The percentage of women who faced out-of-pocket costs did not decrease during the first half of 2012; we first observe decreases toward the end of 2012, as the ACA’s contraceptive coverage requirement first took effect for patients signing up for new health plans. Coverage increased substantially at the end of 2012, when many patients’ annual plans were renewed and the ACA took effect for those without grandfathered plans; the percent with out-of-pocket costs declined 3 percentage points in December 2012, from 52% to 49%, and 21 points in January 2013, from 49% to 28%. Over the next 15 months, from February 2013 through March 2014, the percentage of women who faced out-of-pocket costs fell to 13%, or by 1 percentage point per month.
Fig. 1.
Percentage of women who would have had out-of-pocket costs for a hormonal IUD, by month. Note: The lighter line begins in January 2013 because the 2012 data do not contain insertion copayments and deductible applicability.
We analyzed whether a woman’s insurer required a copayment for the device’s insertion or otherwise required cost sharing due to a deductible from 2013 onwards (as these data were not available for 2012). The results did not substantively differ from the trend described above for full coverage. The gray line in Fig. 1 shows that 16% rather than 13% of women faced out-of-pocket costs for both the device and its insertion. These estimates of change over time may be conservative, however, as the percentage of women with insurers who required them to share in the cost of the device’s insertion might have been higher in 2012 than in 2013.
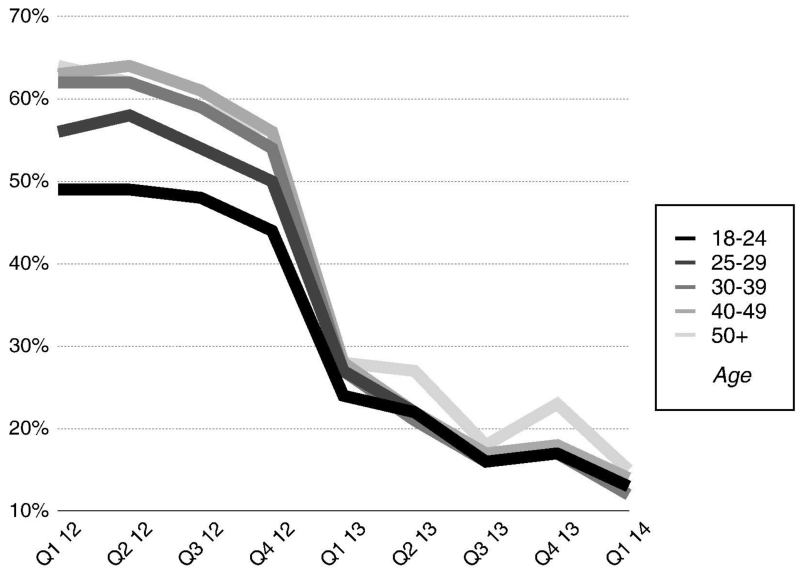
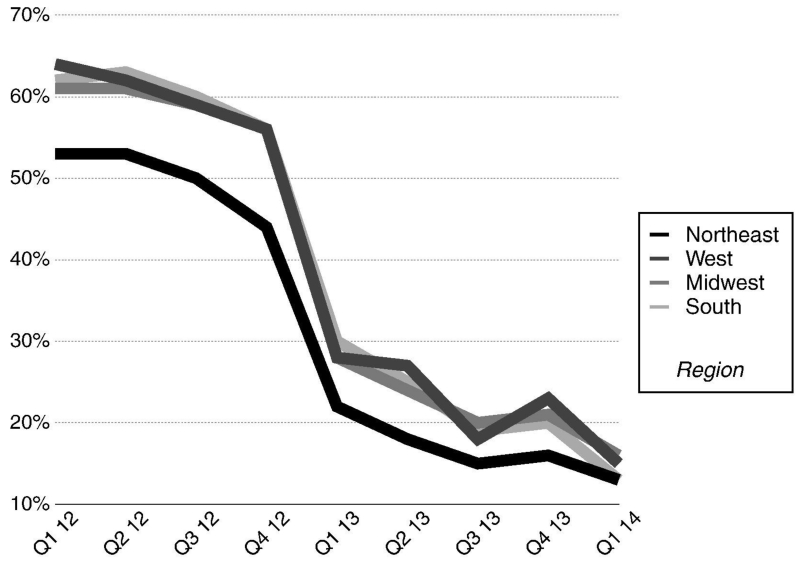
Figs. 2 and 3 show trends in IUD coverage by age and region, respectively. Before the implementation of the ACA provision, young and Northeastern women experienced higher levels of coverage than other women; after implementation, differences by age and region narrowed sharply. In Q1 2012, 49% and 63%, respectively, of women aged 18–24 and 40–49 years would have had to pay out of pocket, a 14-point difference (Fig. 2). In Q1 2013, less than a third of this gap remained (4 points, 24% versus 28%); differences by age nearly dissolved by the end of the analysis period. Similarly, in Q1 2012, 53% and 61–64%, respectively, of women in the Northeast and elsewhere would have had to pay something out of pocket (Fig. 3). In Q1 2013, four fifths of this gap remained, and after another year, differences by region nearly dissolved (to 0–3 points). Differences by region dissolved as much as differences by age but less rapidly.
Fig. 2.
In each age group: percentage of women who would have had out-of-pocket costs for a hormonal IUD, by quarter.
Fig. 3.
In each region: percentage of women would have had out-of-pocket costs for a hormonal IUD, by quarter.
Table 1 reports the percentage of women with full coverage for a hormonal IUD (and at least partial coverage for its insertion), with partial coverage for the IUD or without coverage, by quarter, between Q1 2012 and Q1 2014. The table indicates that very few women in these data had no coverage at all. Thus, most of the increase in full coverage appears to be driven by insurance companies moving from partial to full coverage.
Table 1.
Percentage of women with different levels of coverage for a hormonal IUD and percentage affected by the contraceptive exclusion for religious employers, by quarter.
| 2012 |
2013 |
2014 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | |
| Percentage of women with coverage | |||||||||
| No coverage | 11.0 | 11.7 | 10.6 | 9.2 | 5.7 | 5.2 | 4.5 | 4.1 | 3.3 |
| Coverage but with cost sharing | 47.8 | 47.7 | 46.1 | 42.9 | 21.4 | 17.2 | 13.0 | 14.6 | 10.3 |
| No-cost coverage for the device and coverage for the insertion | 41.2 | 40.6 | 43.3 | 47.9 | 72.8 | 77.6 | 82.5 | 81.4 | 86.4 |
| Contraceptive exclusion | |||||||||
| Percentage of women | – | – | – | – | 2.2 | 1.5 | 0.6 | 0.4 | 0.7 |
| Percentage ofwomen with no coverage | – | – | – | – | 37.9 | 28.6 | 13.7 | 8.8 | 21.6 |
| N (1000s) | 49.6 | 46.8 | 46.0 | 43.6 | 45.6 | 51.1 | 46.2 | 41.5 | 46.7 |
Note: The data do not contain information on the contraceptive exclusion in 2012.
Table 1 also reports that the percentage of women in these data affected by the contraceptive exclusion for religious employers varies from 0.4% to 2.2% in the five quarters between January 2013 and January 2014. Dividing the percentage without coverage due to the contraceptive exclusion by the percentage of women with no coverage shows, however, that these 0.4–2.2% of women who sought an IUD amount to 8.8–37.9% of women who sought an IUD and had no coverage; this may suggest that a nontrivial portion of women with interest in an IUD but without any coverage worked for a religious employer that denies contraceptive coverage. Considering the wide variation in these numbers, however, they should be interpreted with caution.
Table 2 reports cost estimates for the IUD itself at the median and 90th percentiles. The 90th percentile declines to $169 in the first quarter of 2013 and to $15 in the first quarter of 2014, from $844 in the first three quarters of 2012. Median estimates are much smaller, at $20 in the first half of 2012, and fall to $0 in Q4 2012, as by then fewer than half of women (49.9%) faced out-of-pocket costs for the IUD itself.
Table 2.
Median and 90th percentile cost estimates for a hormonal IUD, by quarter.
| 2012 |
2013 |
2014 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | |
| Median | 20 | 20 | 15 | 0 | 0 | 0 | 0 | 0 | 0 |
| 90th percentile | 844 | 844 | 844 | 338 | 169 | 169 | 84 | 50 | 15 |
In a sensitivity analysis, we examined the percentage of women who faced out-of-pocket costs for obtaining an IUD under the assumption that women with multiple insurers — for example, backed up by Medicaid — could not rely on the insurance with the lowest out-of-pocket cost available to them. In this scenario, 20% of women would have had out-of-pocket costs for the IUD and insertion in March 2014, compared to 16% as shown in Fig. 1. In both coverage scenarios, 58–59% faced out-of-pocket costs in January 2012, so this sensitivity analysis corroborates the overall analysis.
4. Discussion
Following implementation of the ACA, we observed a substantial decline in the percentage of women having to pay out of pocket for a hormonal IUD and the elimination of cost disparities by age and region. Potential for further decline remains, as 13% of women still did not have complete coverage as of March 2014.
Some of the decrease in women who face costs could follow from other causes aside from the ACA. However, we note the complete absence of any trend prior to the point in time at which the ACA’s provisions came into effect.
Either the ACA reduces differences between the Northeast and other regions or the characteristics of the healthcare providers who use the benefit inquiry service differ in the Northeast. If so, then these findings may reflect a convergence in coverage not by region but by unobserved socioeconomic characteristics. We cannot identify effects by individual characteristics such as income or race, but trends by region suggest that IUD coverage increased substantially under ACA throughout the United States.
To address the representativeness of the benefit inquiry data, we compared the available demographics — age and geographic region — to U.S. Census data and the NSFG. With regard to age, the women in the benefit inquiry data do not differ significantly from all women of reproductive age. With regard to geography, the comparisons indicate that the benefit inquiry data overrepresent women in the Northeast and underrepresent women in the West, although women in the West are more likely to have an IUD in the NSFG and in a recent Centers for Disease Control and Prevention analysis of services provided to teenagers in Title X clinics [3,20]; this may reflect differences by region in the use of the benefit inquiry service.
We note several limitations of our approach. A key limitation is that we rely upon both the manufacturer of the hormonal IUDs and the manufacturer’s benefits-verification contractor for the data’s authenticity and accuracy. We also cannot determine how many of the 13% of women who remain without complete coverage in March 2014 do so because of imperfect adherence to the ACA requirement or because they have a grandfathered insurance plan. Evidence of imperfect adherence leads advocates like the National Women’s Law Center to publish advice to women faced with costs in spite of the federal mandate [21–23]. Also, as previously noted, these data do not represent all women seeking Mirena or Skyla, nor do we know the percentage of these women who actually went on to obtain an IUD or the number of IUDs sold. Finally, we expect but cannot confirm that these data predominantly represent women with private insurance, as a doctor familiar with the public insurance plans within his or her state would likely know a publicly insured woman’s coverage. While we note these limitations, our findings corroborate similar results from other studies that analyze other contraceptives [17,18].
Earlier studies reported that most women with private insurance had at least partial coverage [10,14,17,18,24], but these studies could have underestimated the number of women with no coverage because they analyzed women who obtained an IUD, and women who discovered that their insurance did not cover an IUD might not obtain one. In contrast to these earlier studies, our results are not biased by this limitation.
Noticeable gaps in the percentage of women who are covered and not subject to cost sharing, between women by region and women by age, dissolved after the ACA took effect. This convergence suggests that the ACA reduced inequality among insured women. Were race or income available in these data, it would have been interesting to test whether race or income inequality in coverage declined over time. We believe that this is worth further study.
Our study also contributes the first nonanecdotal estimates of the extent to which the contraceptive exclusion for religious employers inhibits women’s access to the contraceptive of their choice. We interpret these results with caution, however, given the between-quarter fluctuations in the percentage of women denied IUD coverage due to the exclusion. We might expect that as the share of women without coverage declines, the proportion of uncovered women subject to the religious exclusion would increase, but we observe the opposite, with a higher proportion of women without coverage affected by the religious exclusion in the first quarter of 2013 than in the first quarter of 2014.
Between 2006 and 2010, unintended pregnancy rates declined in all but 2 of the 41 states for which data are available [25]. This decline corresponded with a national increase in long-acting reversible contraceptive (LARC) use, predominantly of the IUD, from 3.7% in 2007 to 8.5% in 2009 [26]. As noted earlier, IUD use has since risen further, reaching 10% in 2011–2013 [3], and prior research shows that eliminating costs can lead to increased LARC use, which in turn can contribute to lower pregnancy, abortion and birth rates [8,9,12]. Other factors may also contribute to the decline in unintended pregnancy. However, if the ACA leads to additional uptake, this may contribute to continued declines in unintended pregnancy.
Acknowledgments
We would like to thank Adam Sonfield and Rebecca Wind of the Guttmacher Institute for reviewing an earlier draft of this manuscript and Gwendolyn Mayes, Jerome Su and Amy Law of Bayer HealthCare for facilitating access to the data. We also wish to thank the JPB Foundation for funding this analysis. Neither Bayer nor Guttmacher provided financial or any other compensation to the other entity. Bayer staff reviewed the manuscript for technical accuracy, but the authors made the final determination as to the content of the paper, and the conclusions and opinions expressed are theirs alone.
Footnotes
The data record whether patients were subject to cost sharing, and if so, what the copayment or coinsurance rate was and not what providers charge.
This could arise if, for example, a woman’s coverage is not yet active or is no longer active, but the data do not record this. Because our goal was an analysis of insured women’s IUD benefits, we excluded these women.
Results of logistic regressions, which compare each month to January 2013 or each quarter to the first quarter of 2013, are available from the authors upon request.
We speculate, for example, that a woman’s employer’s insurance may be her primary insurer in some cases, and she may also have insurance from her spouse’s employer; she may have to use her employer’s insurer even if her spouse’s insurer offers a lower copay. Alternatively, a woman’s primary insurer may cover the IUD but may require a copayment; if she has Medicaid, then, Medicaid should cover the copayment.
References
- [1].Daniels K, Daugherty J, Jones J. Current Contraceptive Status Among Women Aged 15-44: United States, 2011-2013. NCHS Data Brief; 20141-8. [PubMed] [Google Scholar]
- [2].Contraceptive Use in the United States. at http://www.guttmacher.org/pubs/fb_contr_use.html#2.
- [3].Kavanaugh M, Jerman J, Finer L. Changes in use of long-acting reversible contraceptive methods among United States women. Obstet Gynecol. 2015;83:2009–12. doi: 10.1097/AOG.0000000000001094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Trussell J, Lalla A, Doan Q, Reyes E. Cost effectiveness of contraceptives in the United States. Contraception. 2009;79(1):5–4. doi: 10.1016/j.contraception.2008.08.003. at http://www.sciencedirect.com/science/article/pii/S0010782408004101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Trussell J. Update on the cost-effectiveness of contraceptives in the United States. Contraception. 2010;82:391. doi: 10.1016/j.contraception.2010.04.008. [DOI] [PubMed] [Google Scholar]
- [7].Trussell J. Update on and correction to the cost effectiveness of contraceptives in the United States. Contraception. 2012;85:218. doi: 10.1016/j.contraception.2011.06.011. [DOI] [PubMed] [Google Scholar]
- [8].Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46:125–32. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- [9].Postlethwaite D, Trussell J, Zoolakis A, Shabear R, Petitti D. A comparison of contraceptive procurement pre- and post-benefit change. Contraception. 2007;76:360–5. doi: 10.1016/j.contraception.2007.07.006. [DOI] [PubMed] [Google Scholar]
- [10].Gariepy A, Simon E, Patel D. The impact of out-of-pocket expense on IUD utilization among women with private insurance. Contraception. 2011;84(6):39–42. doi: 10.1016/j.contraception.2011.07.002. at http://www.sciencedirect.com/science/article/pii/S001078241100432X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Secura GM, Madden T, McNicholas C, Mullersman J, Buckel CM, Zhao Q, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med. 2014;371:1316–23. doi: 10.1056/NEJMoa1400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Biggs MA, Rocca CH, Brindis CD, Hirsch H, Grossman D. Did increasing use of highly effective contraception contribute to declining abortions in Iowa? Contraception. 2015;91:167–73. doi: 10.1016/j.contraception.2014.10.009. [DOI] [PubMed] [Google Scholar]
- [13].Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120:1291–7. doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Sonfield A, Gold RB, Frost JJ, Darroch JE. U.S. insurance coverage of contraceptives and the impact of contraceptive coverage mandates, 2002. Perspect Sex Reprod Health. 2004;36:72–9. doi: 10.1363/psrh.36.72.04. [DOI] [PubMed] [Google Scholar]
- [15].Sonfeld A. Implementing the federal contraceptive coverage guarantee: progress and prospects. Guttmacher, Policy Rev. 16:2013. [Google Scholar]
- [16].Marketplace options for grandfathered health insurance plans. HealthCare.gov. at https://www.healthcare.gov/health-care-law-protections/grandfathered-plans/
- [17].Finer LB, Sonfield A, Jones RK. Changes in out-of-pocket payments for contraception by privately insured women during implementation of the federal contraceptive coverage requirement. Contraception. 2014;89:97–02. doi: 10.1016/j.contraception.2013.11.015. [DOI] [PubMed] [Google Scholar]
- [18].Sonfield A, Tapales A, Jones RK, Finer LB. Impact of the federal contraceptive coverage guarantee on out-of-pocket payments for contraceptives: 2014 update. Contraception. 2015;91:44–8. doi: 10.1016/j.contraception.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Lin M, Lucas HC, Shmueli G. Research commentary — too big to fail: large samples and the p-value problem. Inf Syst Res. 2013;24:906–17. [Google Scholar]
- [20].Vital Signs: Trends in Use of Long-Acting Reversible Contraception Among Teens Aged 15-19 Years Seeking Contraceptive Services — United States, 2005-2013. at http://www.cdc.gov/mmwr/preview/mmwrhtml/mm64e0407a1.htm?s_cid=mm64e0407a1_e. [PMC free article] [PubMed]
- [21].State of Women’s Coverage: Health Plan Violations of the Affordable Care Act. National Women’s Law Center; 2015. at http://www.nwlc.org/stateofcoverage. [Google Scholar]
- [22].National Women’s Law Center . Getting the Coverage You Deserve: What to Do If You Are Charged a Co-Payment, Deductible, or Co-Insurance for a Preventive Service. National Women’s Law Center; 2014. [Google Scholar]
- [23].Laurie Sobel, Salganicoff A, Kurani N. Coverage of Contraceptive Services: A Review of Health Insurance Plans in Five States. at http://kff.org/private-insurance/report/coverage-of-contraceptive-services-a-review-of-health-insurance-plans-in-five-states/2015.
- [24].Dusetzina SB, Dalton VK, Chernew ME, Pace LE, Bowden G, Fendrick AM. Cost of contraceptive methods to privately insured women in the United States. Womens Health Issues. 2013;23:e69–71. doi: 10.1016/j.whi.2013.01.002. [DOI] [PubMed] [Google Scholar]
- [25].Kost K. Unintended Pregnancy Rates at the State Level: Estimates for 2010 and Trends Since 2002. doi: 10.1363/4307811. at http://www.guttmacher.org/pubs/StateUP10.pdf?utm_source=Master+List&utm_campaign=e5cff5fe20-State_Unintended_Pregnancy_2010&utm_medium=email&utm_term=0_9ac83dc920-e5cff5fe20-2442939492015. [DOI] [PubMed]
- [26].Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007-2009. Fertil Steril. 2012;98:893–7. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]