Abstract
Introduction:
Ayurveda is regarded as most ancient traditional system of medicine originated in India having its root back in the Vedas. Medicinal herbs have been long employed to improve the oral health by means of frequently used therapeutic procedures Kavala (gargling) and Gandusha (holding of medicated liquids in the mouth). Gingivitis is most common ailment that results in bleeding gums and halitosis.
Aim:
To evaluate the efficacy of turmeric gel as an anti-plaque and anti-gingivitis agent compared to chlorhexidine gel.
Materials and Methods:
Sixty patients with plaque-induced gingivitis were divided into two groups, Group A was given turmeric gel and Group B was given chlorhexidine gel for 21 days in vaccupress trays. Plaque and gingival index were taken at baseline, 14 days and 21 days. Subjective and objective criteria were evaluated at 14 and 21 days.
Results:
On comparison of Group A and Group B, statistically insignificant difference was observed at 14 and 21 days. Reduction in plaque index at 0 and 21 days was 60.81% and 60.21% for turmeric and chlorhexidine group, respectively. Reduction in the gingival index at 0 and 21 days was 71.79% and 71.20% for turmeric and chlorhexidine group, respectively.
Conclusion:
Both groups reported a comparable reduction in plaque and gingival index. Turmeric gel reported better acceptance due to pleasant odor and no staining of teeth in comparison to chlorhexidine gel that reported a bitter taste and staining of teeth.
Keywords: Anti-gingivitis, anti-plaque, chlorhexidine, Curcuma longa L., plaque-induced gingivitis
Introduction
Ayurveda is the ancient Indian system of medicine and is the rich storehouse of time-tested and effective herbal remedies. Since few decades, there is an enormous awareness and scientific trials on medicinal herbs and its formulations worldwide. In recent times, medicinal herbs have received recognition from international researchers and health sectors around the world due to its preventive and comprehensive health care approach.
Dentistry is described in Ayurveda under Shalakya, one among the eight branches of Ayurveda. A lot of emphases has been given to oral health care in Ayurveda. Among the various practices for oral health care in Ayurveda, Gandusha (holding of medicated liquids in the mouth) and Kavala (gargling),[1] are two very important therapeuticprocedures and are studied in the present clinical trial.
The first evidence of the use of turmeric also known as Haridra (Curcuma longa L.) is found in the Atharvaveda and further in Charaka Samhita, Sushruta Samhita and many others.[2] Haridra is a perennial herb of 2–3 feet height found throughout the tropical countries and specially cultivated in Indian sub-continent.[3]
Gingivitis is one of the most common ailment of oral cavity with a prevalence of 85–90%.[4,5] Gingiva is a investing connective soft tissue surrounding the teeth, inflammation of gingiva is known as gingivitis. Some amount of sub-clinical gingivitis is always present in the oral cavity as soon as the first teeth erupts. Plaque bioflims are bio-aggregation of various bacterial colonies together on teeth, and it is the prime requisite to initiate gingivitis which if left unchecked can lead to periodontitis that is the loss of alveolar bone.[4] All this will finally result in tooth mobility and tooth loss due to loss of surrounding soft and hard tissues. Thus, the foremost aim becomes to control the plaque buildup on teeth (anti-plaque effect) and control the soft tissue inflammation (anti-inflammatory).[5]
Chlorhexidine is a time tested and the gold standard for controlling the gingivitis and is widely used as a chemical plaque control aid for routine oral hygiene maintenance. This study was designed to evaluate the efficacy of C. longa (Curenext gel, Abbott Pharmaceuticals) for its anti-plaque and anti-gingivitis effect using chlorhexidine as control.
Materials and Methods
Sixty patients with plaque-induced gingivitis reporting to the Department of Dental Surgery were enrolled for this randomized controlled clinical trial. Informed consent was taken, and ethical clearance was obtained from Ethical Committee of Himalayan Institute of Medical Sciences, Dehradun, (Letter No.: HIHTU/HIMS/RC/2013/129) in accordance to Helsinki Declaration.
Inclusion criteria
Age above 18 years
Systemically healthy
Plaque-induced gingivitis.
Exclusion criteria
Mouthwash use in past 3 months
Antibiotic therapy in past 3 months
Orthodontic and prosthetic appliances use
Systemic disorders such as diabetes mellitus, renal failure, etc
Pregnancy
Smoking
Chemotherapy and radiotherapy
Patients with established periodontitis.
Grouping and posology
Two groups of 30 patients each were formed based on randomization by computer allocation In Group A turmeric (10 mg C. longa extract) gel (trade name - Curenext gel manufactured by Abbott Pharmaceuticals, Batch No. IAFA 2017) and in Group B chlorhexidine 2% gel (chlorhex mouthwash manufactured by Dr. Reddys Batch No. BCP2067) was advised for topical application on gums via vaccupress customized applicator trays for 5 min duration, twice daily and 30 min after brushing [Figure 1] Total duration of treatment schedule was 21 days.
Figure 1.
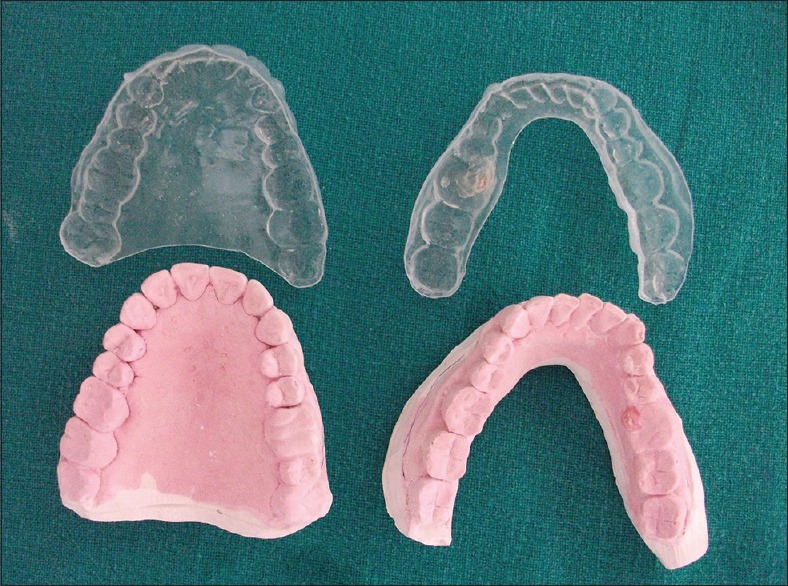
Customized vaccupress application trays and patient model of maxillary and mandibular arch
Turmeric gel used was commercially available in aqueous form consisted of 10 mg of C. longa extract and artificial sweetener to mask the bitter taste of turmeric.
Criteria for assessment
Clinical data including Silness and Loe plaque index for plaque biofilm and Loe and Silness gingival index for gingival inflammation was recorded for all subjects.[6,7] After recording all indices, thorough scaling and polishing was carried out to get all subjects at baseline. No antimicrobial therapy was initiated in this period all patients were recalled after 1 month to be enrolled in the study. Scaling was done 1 month before the initiation of study to bring all the subjects to baseline. Plaque build-up and gingivitis onset require roughly a period of 1 month was given to access the anti-plaque and anti-gingivitis efficacy of the turmeric and chlorhexidine gels.
The parameters were recorded for plaque, and gingival index at 0, 14th, and 21st day. Taste, dryness of gingiva, any odor, ulcer, staining of teeth, any oral mucosal reactions were assessed throughout the study.
Statistical analysis
All data collected was analyzed by statistical software SPSS (BM Corp. Released 2010. IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY). Student's t-test was used for analysis of intra and intergroup comparison. P < 0.05 was considered as statistically significant difference.
Observations and Results
Effect of therapy on plaque index
In Group A, the value of mean ± standard deviation (SD) for plaque index at baseline was 2.337 ± 0.192; at 14 days was 1.307 ± 0.222 and at 21 days was 0.913 ± 0.138 [Table 1]. There was statistically significant difference in plaque index from baseline to 14 days and 21 days [Figures 2 and 3]. In Group B, the value of mean ± SD for plaque index at baseline was 2.32 ± 0.169, at 14 days was 1.27 ± 0.168 and at 21 days was 0.923 ± 0.147 [Table 2]. There was statistically significant difference in plaque index from baseline to 14 days and 21 days [Figures 4 and 5].
Table 1.
Effect of turmeric gel on plaque and gingival index in Group A
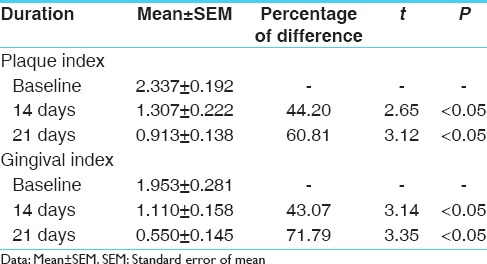
Figure 2.

Group A: Clinical picture at baseline
Figure 3.

Group A: Clinical picture at 21 days
Table 2.
Effect of chlorhexidine gluconate gel on plaque and gingival index in Group B
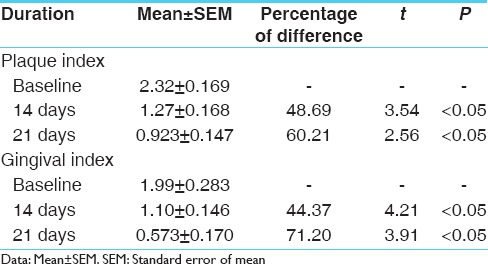
Figure 4.

Group B: Clinical picture at baseline
Figure 5.

Group B: Clinical picture at 21 days
On comparison of plaque index in Group A and B, the reduction from baseline to 14 days was 44.20% and 48.69%, respectively, while from baseline to 21 days it was 60.81% and 60.21%, respectively. Both treatment groups reported a significant reduction in plaque index from baseline [Table 3]. There was statistically insignificant difference observed between the two treatment groups [Table 2 and Chart 1]
Table 3.
Comparison of therapeutic effect in Group A and B
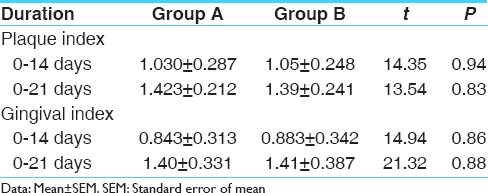
Chart 1.
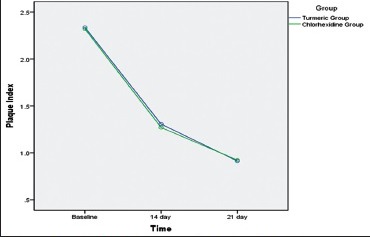
Comparison of plaque index between two groups at different time intervals
Effect of therapy on gingival index
In Group A, value of mean ± SD for gingival index at baseline was 1.953 ± 0.281, at 14 days was 1.110 ± 0.158 and at 21st day 0.550 ± 0.145 [Table 1]. There was a statistically significant difference in the gingival index from baseline to 14 and 21 days.
In Group B, the value of mean ± SD for the gingival index at baseline was 1.99 ± 0.283, at 14 days was 1.10 ± 0.146 at 21 days and 0.573 ± 0.170 [Table 2]. There was statistically significant difference in the gingival index from baseline to 14 days and 21 days.
On comparison of the gingival index in Group A and Group B, the reduction in the gingival index from baseline to 14 days was 43.07% and 44.37%, respectively while from baseline to 21 days was 71.79% and 71.20%, respectively [Chart 2].
Chart 2.
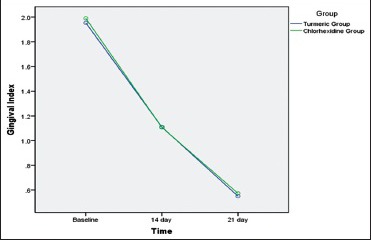
Comparison of gingival index between two groups at different time intervals
Both treatment groups reported a significant reduction in plaque index from baseline. There was statistically insignificant difference observed within the two treatment groups.
None of the patients from both the groups were reported ulceration, dryness, and any mucosal reaction during the 21 days course of the trial. Chlorhexidine group reported 14 cases of minor tooth staining while none were reported the same in turmeric group during the study period.
Discussion
According to Ayurveda turmeric has five qualities, Rasa (taste) - Tikta (bitter) and Katu (pungent); Guna (properties) - Ruksha (dry, rough); Veerya (potency) - Ushna (hot); Vipaka (metabolic property) - Katu (pungent); Karma (actions) - Vishaghna, Varnya, Kushthaghna, Krimighna (anthelmintic)and Pramehaghna (ant diabetic).[8]
Due to Ushna Veerya, it alleviates Kapha and Vata Doshas (humors) and due to Tikta Rasa, it alleviates Pitta Dosha. Being hot, light, acrid, and dry, it is able to reduce corpulence and clear channels. Charaka included Haridra (turmeric) in Lekhaniya group (reducing corpulence).[9]
Sheetada (gingivitis) is an early stage of periodontal diseases, and it occurs mainly due to vitiation of Kapha and Rakta, so mainly considered as Kapha and Rakta Pradhana Vyadhi (disease).[10]
According to Ayurvedic pharamacological properties turmeric is Tridoshahara in nature. Because of its Lekhaniya and anti-Kapha property, turmeric prevents plaque formation and capable of removing the plaques. This could propose the detachment of plaque biofilms and inhibits co-aggregation thus exhibiting the anti-plaque effect. Due to Katu Rasa, it has an anti-inflammatory action that helps in gingivitis. Its anti-Vata property helps in reducing the pain.[8,9]
Some of its therapeutic qualities employed in the field of dental surgery are anti-inflammatory, anti-bacterial, antiseptic, anti-tumor, anti-allergic, blood purifier, antioxidant, and detoxifier. The active constituent of turmeric is curcumin and has a wide range of actions. Because of its strong antioxidant values, it protects the free radical damage, these free radical results in faster progression of gingivitis to periodontitis eventually resulting in tooth loss eventually.[11]
Chlorhexidine gluconate has been referred to as a gold standard for treatment of plaque and gingivitis and as an effective chemical plaque control aid. Chlorhexidine is supplied as mouthwash, topical gel and biodegradable chips for local drug delivery in the periodontal pocket, i.e., space between gingival and tooth. Chlorhexidine gluconate efficient broad spectrum antimicrobial agent. It is a cationic molecule that results in bacterial cell wall lysis and rupture. Cationic molecules binds to the negatively charged surfaces such teeth surface, dental pellicle and bacterial cell wall.[12] Chlorhexidine has a substantivity of 12 h and hence is used twice daily. Various studies have quoted the significant reduction in gingivitis by use of 2% chlorhexidine gluconate gel on topical application.[13] Present study also reported a significant reduction in gingival and plaque index on the use of 2% chlorhexidine gel topically twice daily for 5 min.
Results of this study observed a similar findings for turmeric are reported in previous research work, in which herbal mouthwash mixture containing turmeric compared with chlorhexidine mouthwash.[14] A significant reduction noted in the periodontal pocket, gingival index and gingival index compared to control when 2% turmeric gel was used as a local drug delivery in patients with periodontitis.[15] Similar results in terms of reduction of gingival and plaque index was observed in the present study.
Anti-plaque effect of turmeric gel was comparable to chlorhexidine gel, this is in accordance with the results of previous research work.[16] These effects were enhanced as the tray application resulted in longer and closer contact of gels to the site of interest. The anti-inflammatory effect of turmeric gel was similar to reported in previous studies.[14,16,17] Chlorhexidine group reported a similar reduction in gingival index and plaque index as those reported in previous research works.[17,18]
Chlorhexidine group described the gel as colorless, odorless with a bitter taste, few patient reported gagging to the taste. Turmeric group describe turmeric gel (commercially available flavored) as yellow to orange in color with a sweet taste and pleasant odor. The bitter taste of turmeric was masked by the use of artificial sweetener in the commercial preparation while the root property of turmeric that is Katu-Tikta Rasa, anti Kapha and Lekhaniya properties remains unaltered. This was readily accepted by patients, and none reported any gagging while on tray application.
On the basis of the finding of the present study, it is clear that turmeric mouthwash has effective anti-plaque and anti-gingivitis effect similar to chlorhexidine. Both gels were efficient in reducing gingival and plaque index further turmeric gel was more readily accepted due to sweet taste, pleasant odor, and no staining potential of teeth over chlorhexidine gel.
Conclusion
The observation of this study states that both turmeric and chlorhexidine gel have comparable anti-plaque and anti-gingivitis effect, and both can be efficiently used to control plaque-induced gingivitis. Turmeric gel is biocompatible and free of any adverse effects, it is well-accepted by the patient as it dose not causes dryness, ulceration, and staining of teeth. Five minutes application of turmeric gel with vaccupress tray reported a significant reduction in plaque-induced gingivitis. Further studies are required to identify the minimum dose and duration of application for optimum plaque and gingival inflammation control.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Srikanthamurthi KR. 4ed. Ch. 3, Ver. 28-30. Varanasi: Chaukhambha Orientalia; 2001. Translator: Astanga Sangraha of Vagbhata, Sutra Sthana; p. 37. [Google Scholar]
- 2.Sharam PV. 1st ed. Ch. 38, Ver. 54. Varanasi: Chaukhanbha Vishwabharti; 1999. Translator: Sushruta Samhita of Sushruta. Sutra Sthana; p. 363. [Google Scholar]
- 3.Sharma P. Reprint Edition. Vol. 2. Varanasi: Chaukhambha Bharti Academy; 2005. Dravya Guna Vigyan; p. 37. [Google Scholar]
- 4.Pihlstrom BL, Ammons WF. Treatment of gingivitis and periodontitis. Research, science and therapy committee of the American academy of periodontology. J Periodontol. 1997;68:1246–53. [PubMed] [Google Scholar]
- 5.Löe H, Schiott CR. The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man. J Periodontal Res. 1970;5:79–83. doi: 10.1111/j.1600-0765.1970.tb00696.x. [DOI] [PubMed] [Google Scholar]
- 6.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 7.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(Suppl (6)):610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 8.Chunekar KC, Commentator, Pandey GS, editors. Ver. 196-197 Reprint Edition. Varanasi: Chaukhambha Bharti Academy Varanasi; 2002. Bhavprakash Nighantu of Sri Bhav Mishra, Haritakyadi Varga; p. 114. [Google Scholar]
- 9.Sharam PV. 7th ed. Ch. 4, Ver. 8-9. Varanasi: Chaukhambha Orientalia; 2001. Translator: Charak Samhita of Agnivesha, Part-I, Sutra Sthana; pp. 24–5. [Google Scholar]
- 10.Srikantah Murthy KR. Uttara Sthana. 2nd ed. Ch. 21, Ver. 20. III. Varanasi: Krishanadas Academy; 1997. English Translation, Astanga Hridyam; p. 188. [Google Scholar]
- 11.Pendyala G, Thomas B, Kumari S. The challenge of antioxidants to free radicals in periodontitis. J Indian Soc Periodontol. 2008;12:79–83. doi: 10.4103/0972-124X.44100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jenkins S, Addy M, Wade W. The mechanism of action of chlorhexidine. A study of plaque growth on enamel inserts in vivo. J Clin Periodontol. 1988;15:415–24. doi: 10.1111/j.1600-051x.1988.tb01595.x. [DOI] [PubMed] [Google Scholar]
- 13.Lindhe J, Hamp SE, Löe H, Schiott CR. Influence of topical application of chlorhexidine on chronic gingivitis and gingival wound healing in the dog. Scand J Dent Res. 1970;78:471–8. doi: 10.1111/j.1600-0722.1970.tb02100.x. [DOI] [PubMed] [Google Scholar]
- 14.Bhandari H, Shankwalkar GB. Clinical Assessment of Action of Combination of Indigenous Drugs on Dental Plaque, Calculus and Gingivitis. Dissertation Submitted to the University of Bombay. 1980 [Google Scholar]
- 15.Behal R, Mali AM, Gilda SS, Paradkar AR. Evaluation of local drug-delivery system containing 2% whole turmeric gel used as an adjunct to scaling and root planing in chronic periodontitis: A clinical and microbiological study. J Indian Soc Periodontol. 2011;15:35–8. doi: 10.4103/0972-124X.82264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mali AM, Behal R, Gilda SS. Comparative evaluation of 0.1% turmeric mouthwash with 0.2% chlorhexidine gluconate in prevention of plaque and gingivitis: A clinical and microbiological study. J Indian Soc Periodontol. 2012;16:386–91. doi: 10.4103/0972-124X.100917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van der Weijden GA, Timmer CJ, Timmerman MF, Reijerse E, Mantel MS, van der Velden U. The effect of herbal extracts in an experimental mouthrinse on established plaque and gingivitis. J Clin Periodontol. 1998;25:399–403. doi: 10.1111/j.1600-051x.1998.tb02462.x. [DOI] [PubMed] [Google Scholar]
- 18.Leyes Borrajo JL, Garcia VL, Lopez CG, Rodriguez-Nuñez I, Garcia FM, Gallas TM, et al. Efficacy of chlorhexidine mouthrinses with and without alcohol: A clinical study. J Periodontol. 2002;73:317–21. doi: 10.1902/jop.2002.73.3.317. [DOI] [PubMed] [Google Scholar]


