Adult cancer survivors are significantly more likely to report being in fair or poor health, have comorbidities, one or more limitations in activities of daily living, and poorer functional status when compared with similar age adults without a cancer diagnosis. Occupational therapy is specifically designed to evaluate and treat functional deficits, yet it remains underused in cancer care.
Keywords: Functional status, Occupational therapy, Activities of daily living, Quality of life
Abstract
Adults with cancer may be at risk for limitations in functional status and quality of life (QOL). Occupational therapy is a supportive service with the specific mission to help people functionally engage in life as safely and independently as possible with the primary goal of improving QOL. Unfortunately, for people with cancer, occupational therapy remains underused. The overall purpose of this review is to provide an understanding of what occupational therapy is and its relevance to patients with cancer, highlight the reasons to refer, and, last, provide general advice on how to access services.
Implications for Practice:
Adults with cancer are at risk for functional decline, which can lead to increased hospitalization, poor tolerance of cancer treatment, and increased health-care costs. Occupational therapy is specifically designed to evaluate and treat functional deficits, yet it remains underused in cancer care. This article describes what occupational therapy is, how to identify those who may need it, and how to access services.
Introduction
Occupational therapy is a patient-centered service whose interventions focus on improving health, well-being, and functional capacity [1]. Among the many millions of adult cancer survivors, many report decrements in quality of life and limitations in basic activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Such limitations in functional status may be due to the cancer itself, but many are actually a result of treatment-related side effects and age-related functional decline [2, 3]. Cancer-related disability arises from these limitations and puts adults with cancer at a higher risk for long-term disability, institutionalization, and overall increased mortality [4–7].
For adults with cancer, occupational therapy has the potential to limit and reverse cancer-related disability, yet it remains severely underused in adults with cancer [8]. Barriers to patients receiving occupational therapy are (a) the poor awareness of occupational therapy, (b) lack of knowledge of whom occupational therapy would benefit, and (c) practical accessibility to the service [9, 10]. The purpose of this review is to address these barriers to the use of occupational therapy for adults with cancer.
Occupational Therapy
Occupational therapy uses a variety of techniques and tools to improve functional capacity. Goals are written in collaboration with the patient to identify the activities most important to their quality of life (QOL). Occupational therapy can increase functional status, decrease risk of falling, improve social participation, and improve overall QOL [11]. Occupational therapy interventions also improve life satisfaction and participation in one’s life roles, pain control, and overall mental health. Occupational therapy interventions can lead to improvements in short- and long-term outcomes and are cost effective [11–14].
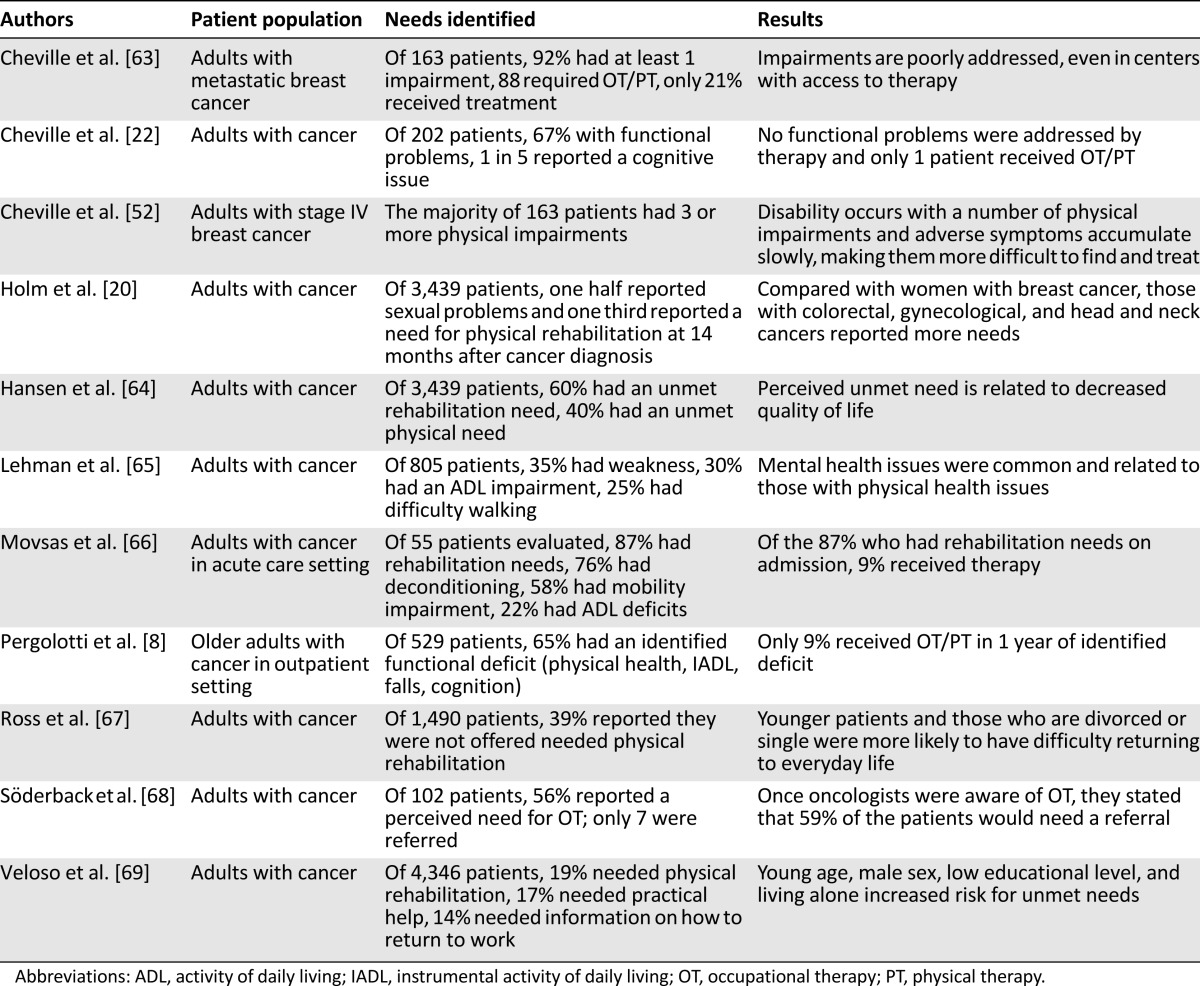
Unfortunately, adults with cancer are at a higher risk for functional limitations, poorer QOL, and falling [2, 8, 15–18]. Poor QOL and functional limitations are associated with decreased ability to complete full treatment, increased risk of receiving a less intense treatment regimen, increased risk for chemotherapy toxicity, and, in turn, decreased survival [19]. Adults with cancer who have any level of comorbidity (mild to severe) have been shown to report a need for rehabilitation services [20, 21]. In patients with metastatic disease, one in five adults with cancer reported cognitive difficulties and 66% reported functional deficits [22]. Adults stated they had difficulty with bending, stooping, lifting, and getting out of bed and they needed help with ADLs, yet there was no documentation of impairment or any referral for occupational therapy to address their difficulties [22]. Table 1 describes several studies highlighting the need for occupational therapy in adults with cancer.
Table 1.
Summary of relevant research evaluating the needs for occupational therapy
Specific Factors Amendable to Occupational Therapy Intervention
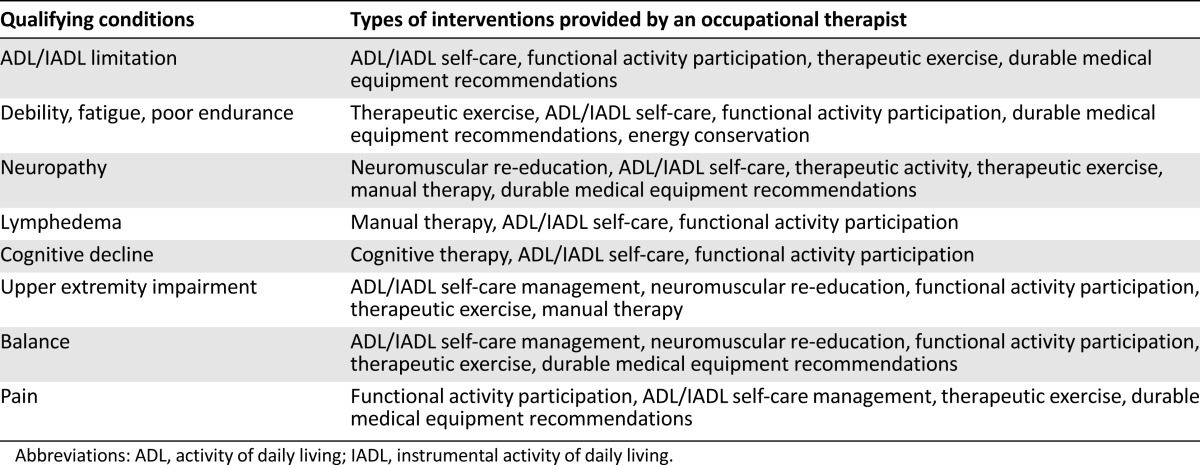
Many impairments related to cancer and its treatments are amendable to occupational therapy. In this section, we address specific cancer-related impairments and the potential occupational therapy interventions. This is not an exhaustive list, and it should be understood that these impairments do not occur in isolation but often in relation to one another. Table 2 provides a quick overview of occupational therapy needs and subsequent intervention strategies.
Table 2.
Qualifying conditions and potential interventions for occupational therapy
Falls
Older adults with cancer are at a higher risk for falls compared with those without cancer [23]. In one study, 44% of the patients who fell also reported a limitation in IADLs [24]. Yet, studies have consistently reported that oncology providers rarely report a fall or respond with appropriate and timely intervention [8, 24–26]. For fall prevention in community-dwelling older adults, the most effective interventions include home modifications and adaptations, which are most effective when completed by an occupational therapist [27–30]. In a randomized control trial of older adults, home occupational therapy decreased the risk of falling in those who had fallen before [28]. In a meta-analysis, in-home modifications by a skilled service, such as occupational therapy, reduced falls by 21% overall and 39% in high-risk groups [31]. Home-based modifications can include grab bars in the tub or shower to help getting in and out of the bath or near the toilet to assist with rising from a sitting to a standing position and toileting safely. Other modifications include stair handrails, removal of hazardous objects and clutter, and use of nonslip mats [30].
Cognitive Function Impairment
Cancer-related cognitive impairment (CRCI) presents as difficulties related to memory, attention, information-processing speed, and organization, and can affect all age groups [32]. For example, women with breast CRCI report mild cognitive decline impacting their ability to function, making previously easy activities more difficult and causing distressing loss of independence in family life roles [33]. For this issue, occupational therapy intervention will work toward adapting or remediating the functional impairment through different cognitive strategies. The occupational therapist will generally incorporate adaptive strategies so that the patient learns how to compensate for impaired memory or attention while performing particular tasks, or use restorative activities to improve cognition functions during the performance of specific tasks. For example, for a patient with memory and attention issues, an occupational therapist would help create individualized systems to set reminders for medications, schedule appointments, and handle to-do type tasks for shopping, cooking, and money management. Another example of interventions for cognitive decline would be training or retraining on the use of paper maps and/or global positioning system devices to enhance independence in community navigation.
Cancer-Related Fatigue
Cancer-related fatigue (CRF) is a commonly reported issue among cancer survivors that can disrupt daily routines and restrict participation in meaningful activity. Ninety-one percent of adults with cancer report fatigue as a symptom that has “prevented them from leading a ‘normal’ life” and 88% have to modify their daily routine [34]. Patients with CRF can benefit from energy conservation training taught in occupational therapy. This translates into practical strategies to manage fatigue for resumption of roles and routines [35]. Structured activity modification and prioritization, as well as use of a daily activity log to monitor task-based activity and energy patterns, are a part of this training. Patients thus have personalized adjustments (e.g., placing frequently used objects in the refrigerator at easy-to-reach heights, timing showers at night) to conserve energy to enjoy the activities that contribute most to their QOL.
Upper-Extremity Impairments
In breast and other cancers, surgery has the potential to cause short- and long-term physical impairments that are potentially modifiable with occupational therapy. Restricted upper-extremity range of motion, arm swelling (lymphedema), pain, and numbness are all common impairments of the upper extremity in patients after surgery for breast cancer [36]. Disability related to arm range of motion was most often associated with ADL and IADL impairments such as putting on a sweater, making a bed, doing yard work, carrying groceries, and lifting anything weighing more than 10 pounds (i.e., children) [37].
Occupational therapy for patients with limitations in their upper extremities could include a combination of exercise, stretching, and modalities to improve range of motion and muscle strength, followed by training in the performance of functional tasks and adaptation of the activity or environment, as needed. Many tools commonly used and recommended by occupational therapists can improve independence (e.g., a rocker knife used to cut food using one hand) and limit the effect of upper-extremity limitations on QOL.
Lymphedema
Lymphedema causes decreased QOL, altered body image, decreased work/leisure participation, and impaired occupational engagement [38]. Occupational therapists can help patients identify meaningful activities and apply activity modifications for successful completion, use stress management and relaxation techniques to decrease anxiety, and address concerns related to changes in body image. Lymphedema education includes the identification of risk for exacerbation and activities that may worsen the swelling, appropriate activity modifications, energy conservation techniques, self-massage, and management of the swelling with complete decongestive therapy.
Chemotherapy-Induced Peripheral Neuropathy
Paclitaxel, docetaxel, vincristine, oxaliplatin, cisplatin, and taxanes can potentially cause chemotherapy-related peripheral neuropathy [39]. Patients may experience weakness, numbness, tingling, and/or pain in their extremities that can lead to reduced QOL [40, 41]. Patients with chemotherapy-induced sensory neuropathy report high levels of functional disability [22]. Adults report difficulty with housekeeping, distinguishing items in their hands (tactile agnosia), and an increase in overall dependence on others [40]. Occupational therapy interventions for peripheral neuropathy focus on adaptation and remediation through sensory and functional activities (e.g., cooking) and adapting specific tools to maintain independence with ADLs and IADLs (e.g., a button hook to assist with fastening buttons when dressing).
Functional Impairments
For adults with cancer, occupational therapists also address how cancer-specific issues, such as fatigue, cognition, pain, and peripheral neuropathy, may affect changes in functional status and daily routines [42]. For adults who present with functional impairments, occupational therapy interventions would assist with skills ranging from dressing, bathing, and using the toilet, to the more complex IADL tasks of organizing one’s schedule for the day, balancing a checkbook, cooking, and being able to care for children or aging relatives. This type of intervention significantly reduced readmissions, overall disability, and improved functional outcomes in adults without cancer but with similar functional limitations [43–47]. Patients with primary and metastatic brain tumors made significant functional gains with inpatient and outpatient rehabilitation [48], and the presence of metastatic disease did not appear to influence gains [49]. In a novel, telemedicine-based occupational therapy intervention, women worked through their reported functional challenges [50]. The longitudinal findings demonstrated improved QOL, active coping and reframing of problems, and decreased self-blame [51].
How to Assess the Need for Occupational Therapy Referral
Cancer-related functional impairment is a slow process and can be difficult to recognize [52]. Obvious impairments and referrals to occupational therapy occur most often during an inpatient hospital stay where functional decline may be more apparent with issues of hemiplegia, hip fracture, or amputation [53]. When disablement is slowly developing and without a structured and consistent assessment of function, cognition, and falls, it can be difficult to determine quickly, in a busy outpatient oncology office visit, when to refer to occupational therapy [52]. Incorporating a few, brief patient-reported measures or questions that specifically relate to interventions, such as occupational therapy, could help with determining which patients will benefit from these services. The following are examples of validated screening tools: a brief geriatric assessment (GA), developed by Hurria and colleagues, that measures functional status, falls, physical health cognition, and other constructs [54]; the Patient-Reported Outcomes Measurement Information System (PROMIS), which was developed to assess QOL, functional status, and participation in social activites [55]; the Disabilities of Arm, Shoulder, and Hand (DASH) assessment developed to assess functional ability of the upper extremity [56]; and the Functional Independence Measure (FIM), a seven-item assessment of functional and mobility burden widely used in rehabilitation settings [57]. Quick screening questions can include the following:
Has the patient had any falls in the last 6 months?
Has the patient experienced difficulty with ADL or IADL tasks over the past several weeks?
Are there new upper-extremity flexibility restrictions or pain limiting everyday activities?
Has the patient experienced new limitations in leisure or social activities?
Has the patient experienced changes in memory, attention, or focus that have impacted participation in routine daily activities?
These simple questions can easily identify patients who could benefit from a referral to occupational therapy. In addition, completing a comprehensive GA can provide a wealth of information regarding other supportive care needs, including nutrition, pharmacy, geriatrics, or psychiatry.
How to Obtain Occupational Therapy for Your Patient
Most medical centers have occupational therapy services, and if an institution does not have an occupational therapy department, a referral or prescription may be given to the patient to obtain occupational therapy services through a home-care agency or an outpatient clinic. A written referral by a physician, nurse practitioner, or physician’s assistant (depending on the state) is required. Once a referral is made, patients can contact any rehabilitation facility or hospital-based occupational therapy department to find outpatient offices in their area. Patients who are leaving the hospital and need additional therapy services may receive occupational therapy either in inpatient rehabilitation or in subacute rehabilitation centers often found in nursing homes. Table 3 describes different occupational therapy settings and levels of care.
Table 3.
Settings and levels of rehabilitation
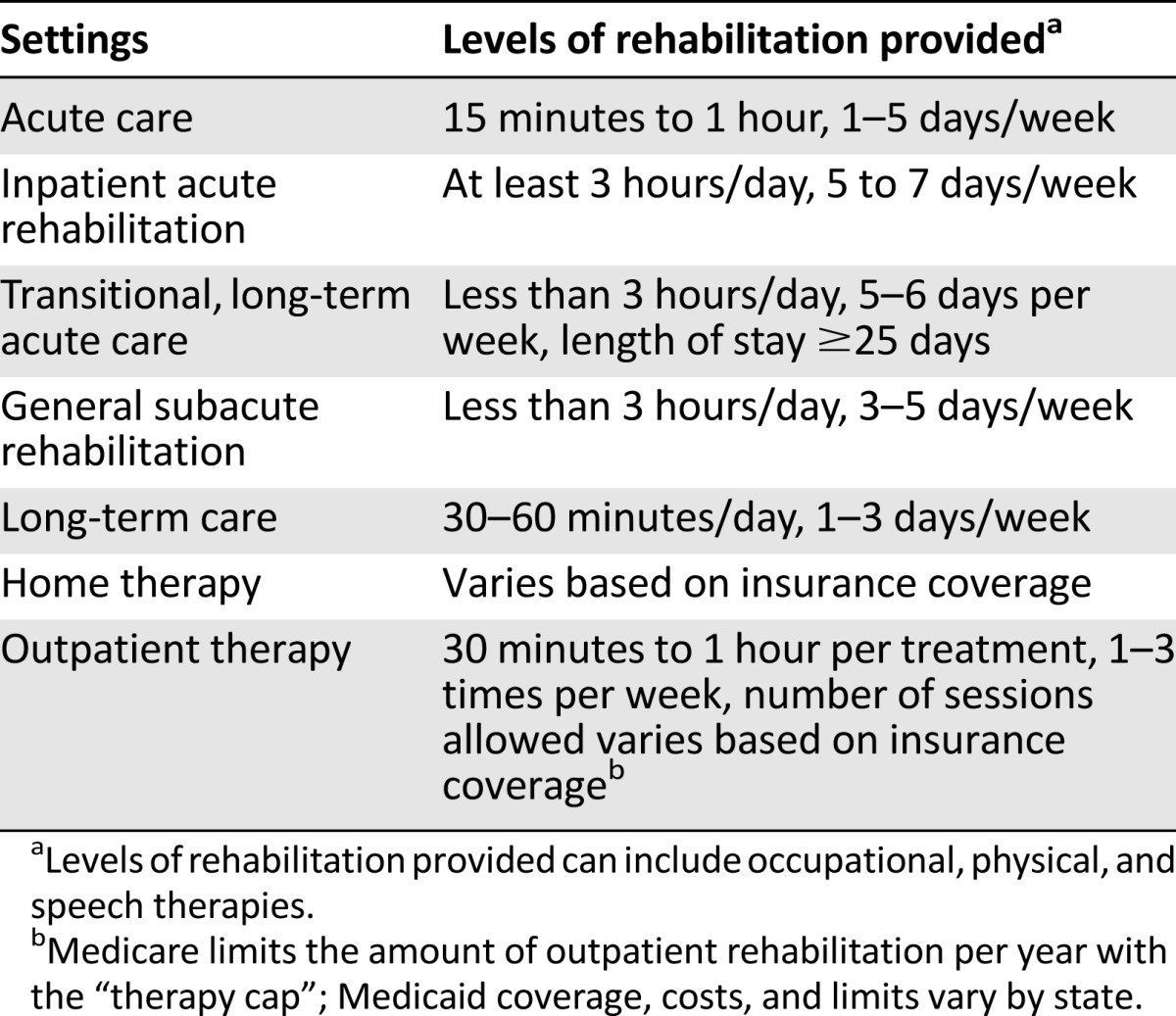
A social worker or case/discharge manager can help facilitate a referral for either outpatient or home occupational therapy services when a patient is not able to access the community independently or is generally home bound. Patients, nurse navigators, social workers, and case managers may also call or check the patient’s supplemental insurance company’s website to find occupational therapists in the area who are covered under the patient’s insurance. For adults over the age of 65 years who have Medicare, outpatient occupational therapy is covered under Part B, and most patients also have supplemental insurance to help cover the cost of coinsurance for outpatient care. To best assist patients in getting optimal therapy, defining the reason for referral in terms of needs or specific concerns (e.g., ADL need, cognitive decline, lymphedema) should be included.
Cancer Rehabilitation Team
Occupational therapy is often obtained in combination with other rehabilitation services such as physical therapy and speech and language pathology. Physical therapy and speech and language pathology are vital parts of the rehabilitation team but differ from occupational therapy in their primary focus. Physical therapy has a strong emphasis on strength and endurance capacity, whereas speech and language pathology focuses on swallowing and speech production. In some ways, the occupational, physical, and speech therapy goals and techniques may overlap, but, as a team, they all work to improve each patient’s QOL and cognitive/functional performance.
Emerging Research
Research specifically examining the benefits of occupational therapy in adults with cancer is emerging as clinical care in this area continues to grow [50, 58–61]. There is an ongoing randomized controlled trial looking at the effectiveness of both occupational and physical therapies provided in the outpatient setting specifically designed for older adults with cancer [62]. There is also an ongoing study that is developing novel occupational therapy interventions for women after they have had ovarian cancer surgery. Another study is examining a problem-solving approach to changes in ADLs and IADLs to reduce disability of older adults with cancer. These and other emerging studies that are focused on adults of all ages will help further define the important role of occupational therapy in cancer care.
Conclusion
An analysis of the National Health Interview Survey confirmed that cancer survivors are significantly more likely to report being in fair or poor health, have three or more chronic comorbid conditions, psychological problems, one or more limitations in ADLs or IADLs, and poorer functional status when compared with similar age adults without a cancer diagnosis [2]. One third of patients who reported having limitations with ADL or IADL believed that cancer caused their limitations [2]. Occupational therapy is designed to help people with these impairments and other needs improve their overall QOL by facilitating engagement in meaningful everyday activities. As more cancer rehabilitation programs are developed and the scope of occupational therapy becomes better understood by all consumers, accessing an occupational therapist will become more standard practice. Occupational therapists treat each patient holistically and use creative solutions to improve the overall cognitive and functional capacity of older adults with cancer, making the occupational therapist a critical member of the interprofessional cancer care team.
Acknowledgments
This research was supported by National Cancer Institute (NCI) Grant R25CA116339. Grant R. Williams is supported by NCI Grant 5K12CA120780.
Author Contributions
Conception/Design: Mackenzi Pergolotti, Hyman B. Muss
Provision of study material or patients: Mackenzi Pergolotti
Collection and/or assembly of data: Mackenzi Pergolotti
Data analysis and interpretation: Mackenzi Pergolotti, Grant R. Williams, Claudine Campbell, Lauro A. Munoz, Hyman B. Muss
Manuscript writing: Mackenzi Pergolotti, Grant R. Williams, Claudine Campbell, Lauro A. Munoz, Hyman B. Muss
Final approval of manuscript: Mackenzi Pergolotti, Grant R. Williams, Claudine Campbell, Lauro A. Munoz, Hyman B. Muss
Disclosures
Hyman B. Muss: Pfizer (C/A). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.American Occupational Therapy Association. Standards of practice for occupational therapy. Available at http://ajot.aota.org/article.aspx?articleid=2477354. Accessed December 15, 2015.
- 2.Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: Age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58:82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- 3.Palmadottir G. The role of occupational participation and environment among Icelandic women with breast cancer: A qualitative study. Scand J Occup Ther. 2010;17:299–307. doi: 10.3109/11038120903302874. [DOI] [PubMed] [Google Scholar]
- 4.Reuben DB, Rubenstein LV, Hirsch SH, et al. Value of functional status as a predictor of mortality: Results of a prospective study. Am J Med. 1992;93:663–669. doi: 10.1016/0002-9343(92)90200-u. [DOI] [PubMed] [Google Scholar]
- 5.Ponzetto M, Maero B, Maina P, et al. Risk factors for early and late mortality in hospitalized older patients: The continuing importance of functional status. J Gerontol A Biol Sci Med Sci. 2003;58:1049–1054. doi: 10.1093/gerona/58.11.m1049. [DOI] [PubMed] [Google Scholar]
- 6.Mor V, Wilcox V, Rakowski W, et al. Functional transitions among the elderly: Patterns, predictors, and related hospital use. Am J Public Health. 1994;84:1274–1280. doi: 10.2105/ajph.84.8.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: A prospective multicenter study. J Clin Oncol. 2011;29:3457–3465. doi: 10.1200/JCO.2011.34.7625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pergolotti M, Deal AM, Lavery J, et al. The prevalence of potentially modifiable functional deficits and the subsequent use of occupational and physical therapy by older adults with cancer. J Geriatr Oncol. 2015;6:194–201. doi: 10.1016/j.jgo.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halkett GK, Ciccarelli M, Keesing S, et al. Occupational therapy in palliative care: Is it under-utilised in Western Australia? Aust Occup Ther J. 2010;57:301–309. doi: 10.1111/j.1440-1630.2009.00843.x. [DOI] [PubMed] [Google Scholar]
- 10.Kealey P, McIntyre I. An evaluation of the domiciliary occupational therapy service in palliative cancer care in a community trust: A patient and carers perspective. Eur J Cancer Care (Engl) 2005;14:232–243. doi: 10.1111/j.1365-2354.2005.00559.x. [DOI] [PubMed] [Google Scholar]
- 11.Clark F, Azen SP, Zemke R, et al. Occupational therapy for independent-living older adults. A randomized controlled trial. JAMA. 1997;278:1321–1326. [PubMed] [Google Scholar]
- 12.Clark F, Jackson J, Carlson M, et al. Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: Results of the Well Elderly 2 Randomised Controlled Trial. J Epidemiol Community Health. 2012;66:782–790. doi: 10.1136/jech.2009.099754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hay J, LaBree L, Luo R, et al. Cost-effectiveness of preventive occupational therapy for independent-living older adults. J Am Geriatr Soc. 2002;50:1381–1388. doi: 10.1046/j.1532-5415.2002.50359.x. [DOI] [PubMed] [Google Scholar]
- 14.Clark F, Azen SP, Carlson M, et al. Embedding health-promoting changes into the daily lives of independent-living older adults: Long-term follow-up of occupational therapy intervention. J Gerontol B Psychol Sci Soc Sci. 2001;56:P60–63. doi: 10.1093/geronb/56.1.p60. [DOI] [PubMed] [Google Scholar]
- 15.Quach C, Sanoff HK, Williams GR, et al. Impact of colorectal cancer diagnosis and treatment on health-related quality of life among older Americans: A population-based, case-control study. Cancer. 2015;121:943–950. doi: 10.1002/cncr.29125. [DOI] [PubMed] [Google Scholar]
- 16.Holley S. A look at the problem of falls among people with cancer. Clin J Oncol Nurs. 2002;6:193–197. doi: 10.1188/02.CJON.193-197. [DOI] [PubMed] [Google Scholar]
- 17.Chen T-Y, Janke M. Predictors of falls among community-dwelling older adults with cancer: results from the health and retirement study. Supportive Care Cancer. 2014;22:479–485. doi: 10.1007/s00520-013-2000-7. [DOI] [PubMed] [Google Scholar]
- 18.Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: A systematic review. JAMA. 2002;288:3137–3146. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- 19.Maione P, Perrone F, Gallo C, et al. Pretreatment quality of life and functional status assessment significantly predict survival of elderly patients with advanced non-small-cell lung cancer receiving chemotherapy: A prognostic analysis of the multicenter Italian lung cancer in the elderly study. J Clin Oncol. 2005;23:6865–6872. doi: 10.1200/JCO.2005.02.527. [DOI] [PubMed] [Google Scholar]
- 20.Holm LV, Hansen DG, Johansen C, et al. Participation in cancer rehabilitation and unmet needs: A population-based cohort study. Support Care Cancer. 2012;20:2913–2924. doi: 10.1007/s00520-012-1420-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holm LV, Hansen DG, Kragstrup J, et al. Influence of comorbidity on cancer patients’ rehabilitation needs, participation in rehabilitation activities and unmet needs: A population-based cohort study. Support Care Cancer. 2014;22:2095–2105. doi: 10.1007/s00520-014-2188-1. [DOI] [PubMed] [Google Scholar]
- 22.Cheville AL, Beck LA, Petersen TL, et al. The detection and treatment of cancer-related functional problems in an outpatient setting. Support Care Cancer. 2009;17:61–67. doi: 10.1007/s00520-008-0461-x. [DOI] [PubMed] [Google Scholar]
- 23.Spoelstra SL, Given BA, Schutte DL, et al. Do older adults with cancer fall more often? A comparative analysis of falls in those with and without cancer. Oncology Nurs Forum. 2013;40:E69–78. doi: 10.1188/13.ONF.E69-E78. [DOI] [PubMed] [Google Scholar]
- 24.Guerard EJ, Deal AM, Williams GR, et al. Falls in older adults with cancer: Evaluation by oncology providers. J Oncol Pract. 2015;11:470–474. doi: 10.1200/JOP.2014.003517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams GR, Deal AM, Nyrop KA, et al. Geriatric assessment as an aide to understanding falls in older adults with cancer. Support Care Cancer. 2015;23:2273–2280. doi: 10.1007/s00520-014-2598-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Puts MT, Monette J, Girre V, et al. The fall rate of older community-dwelling cancer patients. Support Care Cancer. 2013;21:775–783. doi: 10.1007/s00520-012-1579-4. [DOI] [PubMed] [Google Scholar]
- 27.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cumming RG, Thomas M, Szonyi G, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: A randomized trial of falls prevention. J Am Geriatr Soc. 1999;47:1397–1402. doi: 10.1111/j.1532-5415.1999.tb01556.x. [DOI] [PubMed] [Google Scholar]
- 29.Michael YL, Whitlock EP, Lin JS, et al. Primary care-relevant interventions to prevent falling in older adults: A systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2010;153:815–825. doi: 10.7326/0003-4819-153-12-201012210-00008. [DOI] [PubMed] [Google Scholar]
- 30.Harvey LA, Mitchell RJ, Lord SR, et al. Determinants of uptake of home modifications and exercise to prevent falls in community-dwelling older people. Aust N Z J Public Health. 2014;38:585–590. doi: 10.1111/1753-6405.12243. [DOI] [PubMed] [Google Scholar]
- 31.Clemson L, Mackenzie L, Ballinger C, et al. Environmental interventions to prevent falls in community-dwelling older people: A meta-analysis of randomized trials. J Aging Health. 2008;20:954–971. doi: 10.1177/0898264308324672. [DOI] [PubMed] [Google Scholar]
- 32.Hurria A, Somlo G, Ahles T. Renaming “chemobrain”. Cancer Invest. 2007;25:373–377. doi: 10.1080/07357900701506672. [DOI] [PubMed] [Google Scholar]
- 33.Player L, Mackenzie L, Willis K, et al. Women's experiences of cognitive changes or ‘chemobrain’ following treatment for breast cancer: A role for occupational therapy? Aust Occup Ther J. 2014;61:230–240. doi: 10.1111/1440-1630.12113. [DOI] [PubMed] [Google Scholar]
- 34.Curt GA, Breitbart W, Cella D, et al. Impact of cancer-related fatigue on the lives of patients: New findings from the Fatigue Coalition. The Oncologist. 2000;5:353–360. doi: 10.1634/theoncologist.5-5-353. [DOI] [PubMed] [Google Scholar]
- 35.Vockins H. Occupational therapy intervention with patients with breast cancer: A survey. Eur J Cancer Care (Engl) 2004;13:45–52. doi: 10.1111/j.1365-2354.2004.00443.x. [DOI] [PubMed] [Google Scholar]
- 36.Bosompra K, Ashikaga T, O’Brien PJ, et al. Swelling, numbness, pain, and their relationship to arm function among breast cancer survivors: A disablement process model perspective. Breast J. 2002;8:338–348. doi: 10.1046/j.1524-4741.2002.08603.x. [DOI] [PubMed] [Google Scholar]
- 37.Thomas-MacLean RL, Hack T, Kwan W et al. Arm morbidity and disability after breast cancer: New directions for care. Oncol Nurs Forum 2008;35:65–71. [DOI] [PubMed] [Google Scholar]
- 38.Shigaki CL, Madsen R, Wanchai A, et al. Upper extremity lymphedema: Presence and effect on functioning five years after breast cancer treatment. Rehabil Psychol. 2013;58:342–349. doi: 10.1037/a0034657. [DOI] [PubMed] [Google Scholar]
- 39.Kuroi K, Shimozuma K. Neurotoxicity of taxanes: Symptoms and quality of life assessment. Breast Cancer. 2004;11:92–99. doi: 10.1007/BF02968010. [DOI] [PubMed] [Google Scholar]
- 40.Beijers A, Mols F, Dercksen W, et al. Chemotherapy-induced peripheral neuropathy and impact on quality of life 6 months after treatment with chemotherapy. J Community Support Oncol. 2014;12:401–406. doi: 10.12788/jcso.0086. [DOI] [PubMed] [Google Scholar]
- 41.Mols F, Beijers T, Vreugdenhil G, et al. Chemotherapy-induced peripheral neuropathy and its association with quality of life: A systematic review. Support Care Cancer. 2014;22:2261–2269. doi: 10.1007/s00520-014-2255-7. [DOI] [PubMed] [Google Scholar]
- 42.Stubblefield MD. Cancer rehabilitation. Paper presented at: Seminars in oncology 2011. [DOI] [PubMed] [Google Scholar]
- 43.Walker MF, Gladman JRF, Lincoln NB, et al. Occupational therapy for stroke patients not admitted to hospital: A randomised controlled trial. Lancet. 1999;354:278–280. doi: 10.1016/s0140-6736(98)11128-5. [DOI] [PubMed] [Google Scholar]
- 44.Walker MF, Leonardi-Bee J, Bath P, et al. Individual patient data meta-analysis of randomized controlled trials of community occupational therapy for stroke patients. Stroke. 2004;35:2226–2232. doi: 10.1161/01.STR.0000137766.17092.fb. [DOI] [PubMed] [Google Scholar]
- 45.Corr S, Bayer A. Occupational therapy for stroke patients after hospital discharge—a randomized controlled trial. Clin Rehabil. 1995;9:291–296. [Google Scholar]
- 46.Gilbertson L, Langhorne P, Walker A, et al. Domiciliary occupational therapy for patients with stroke discharged from hospital: Randomised controlled trial. BMJ. 2000;320:603–606. doi: 10.1136/bmj.320.7235.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Legg LA, Drummond AE, Langhorne P. Occupational therapy for patients with problems in activities of daily living after stroke. Cochrane Database Syst Rev. 2006;(4):CD003585. doi: 10.1002/14651858.CD003585.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marciniak CM, Sliwa JA, Heinemann AW, Semik PE. Functional outcomes of persons with brain tumors after inpatient rehabilitation. Arch Phys Med Rehabil. 2001;82:457–463. doi: 10.1053/apmr.2001.21862. [DOI] [PubMed] [Google Scholar]
- 49.Marciniak CM, Sliwa JA, Spill G, et al. Functional outcome following rehabilitation of the cancer patient. Arch Phys Med Rehabil. 1996;77:54–57. doi: 10.1016/s0003-9993(96)90220-8. [DOI] [PubMed] [Google Scholar]
- 50.Lyons KD, Erickson KS, Hegel MT. Problem-solving strategies of women undergoing chemotherapy for breast cancer. Can J Occup Ther. 2012;79:33–40. doi: 10.2182/cjot.2012.79.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lyons KD, Hull JG, Kaufman PA, et al. Development and initial evaluation of a telephone-delivered, behavioral activation, and problem-solving treatment program to address functional goals of breast cancer survivors. J Psychosoc Oncol. 2015;33:199–218. doi: 10.1080/07347332.2014.1002659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cheville AL, Kornblith AB, Basford JR. An examination of the causes for the underutilization of rehabilitation services among people with advanced cancer. Am J Phys Med Rehabil. 2011;90(suppl 1):S27–S37. doi: 10.1097/PHM.0b013e31820be3be. [DOI] [PubMed] [Google Scholar]
- 53.Silver JK, Gilchrist LS. Cancer rehabilitation with a focus on evidence-based outpatient physical and occupational therapy interventions. Am J Phys Med Rehabil. 2011;90(Suppl 1):S5–S15. doi: 10.1097/PHM.0b013e31820be4ae. [DOI] [PubMed] [Google Scholar]
- 54.Hurria A, Gupta S, Zauderer M, et al. Developing a cancer-specific geriatric assessment: A feasibility study. Cancer. 2005;104:1998–2005. doi: 10.1002/cncr.21422. [DOI] [PubMed] [Google Scholar]
- 55.Hays RD, Bjorner J, Revicki RA, et al. Development of physical and mental health summary scores from the Patient Reported Outcomes Measurement Information System (PROMIS) global items. Qual Life Res. 2009;18:873–880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 57.Hamilton BB, Laughlin JA, Fiedler RC, et al. Interrater reliability of the 7-level functional independence measure (FIM) Scand J Rehabil Med. 1994;26:115–119. [PubMed] [Google Scholar]
- 58.Hindley M, Johnston S. Stress management for breast cancer patients: Service development. Int J Palliat Nurs. 1999;5:135–141. [Google Scholar]
- 59.Hegel MT, Lyons KD, Hull JG, et al. Feasibility study of a randomized controlled trial of a telephone-delivered problem-solving-occupational therapy intervention to reduce participation restrictions in rural breast cancer survivors undergoing chemotherapy. Psychooncology. 2011;20:1092–1101. doi: 10.1002/pon.1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lyons KD, Hull JG, Root LD, et al. A pilot study of activity engagement in the first six months after stem cell transplantation. Oncol Nurs Forum. 2011;38:75–83. doi: 10.1188/11.ONF.75-83. [DOI] [PubMed] [Google Scholar]
- 61.Purcell A, Fleming J, Bennett S, et al. Development of an educational intervention for cancer-related fatigue. Br J Occup Ther. 2010;73:327–333. [Google Scholar]
- 62.Pergolotti M, Deal AM, Williams GR, et al. A randomized controlled trial of outpatient CAncer REhabilitation for older adults: The CARE Program. Contemp Clin Trials. 2015;44:89–94. doi: 10.1016/j.cct.2015.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cheville AL, Troxel AB, Basford JR, et al. Prevalence and treatment patterns of physical impairments in patients with metastatic breast cancer. J Clin Oncol. 2008;26:2621–2629. doi: 10.1200/JCO.2007.12.3075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hansen DG, Larsen PV, Holm LV, et al. Association between unmet needs and quality of life of cancer patients: A population-based study. Acta Oncol. 2013;52:391–399. doi: 10.3109/0284186X.2012.742204. [DOI] [PubMed] [Google Scholar]
- 65.Lehmann JF, DeLisa JA, Warren CG, et al. Cancer rehabilitation: Assessment of need, development, and evaluation of a model of care. Arch Phys Med Rehabil. 1978;59:410–419. [PubMed] [Google Scholar]
- 66.Movsas SB, Chang VT, Tunkel RS, et al. Rehabilitation needs of an inpatient medical oncology unit. Arch Phys Med Rehabil. 2003;84:1642–1646. doi: 10.1053/s0003-9993(03)00345-9. [DOI] [PubMed] [Google Scholar]
- 67.Ross L, Petersen MA, Johnsen AT, et al. Are different groups of cancer patients offered rehabilitation to the same extent? A report from the population-based study “The Cancer Patient’s World”. Support Care Cancer. 2012;20:1089–1100. doi: 10.1007/s00520-011-1189-6. [DOI] [PubMed] [Google Scholar]
- 68.Söderback I, Paulsson EH. A needs assessment for referral to occupational therapy. Nurses’ judgment in acute cancer care. Cancer Nurs. 1997;20:267–273. doi: 10.1097/00002820-199708000-00006. [DOI] [PubMed] [Google Scholar]
- 69.Veloso AG, Sperling C, Holm LV, et al. Unmet needs in cancer rehabilitation during the early cancer trajectory--a nationwide patient survey. Acta Oncol. 2013;52:372–381. doi: 10.3109/0284186X.2012.745648. [DOI] [PubMed] [Google Scholar]