Abstract
Study Objectives:
This prospective cohort study examined previously underexplored relations between psychological/social work factors and troubled sleep in order to provide practical information about specific, modifiable factors at work.
Methods:
A comprehensive evaluation of a range of psychological/social work factors was obtained by several designs; i.e., cross-sectional analyses at baseline and follow-up, prospective analyses with baseline predictors (T1), prospective analyses with average exposure across waves as predictor ([T1 + T2] / 2), and prospective analyses with change in exposure from baseline to follow-up as predictor. Participants consisted of a sample of Norwegian employees from a broad spectrum of occupations, who completed a questionnaire at two points in time, approximately two years apart. Cross-sectional analyses at T1 comprised 7,459 participants, cross-sectional analyses at T2 included 6,688 participants. Prospective analyses comprised a sample 5,070 of participants who responded at both T1 and T2. Univariable and multivariable ordinal logistic regressions were performed.
Results:
Thirteen psychological/social work factors and two aspects of troubled sleep, namely difficulties initiating sleep and disturbed sleep, were studied. Ordinal logistic regressions revealed statistically significant associations for all psychological and social work factors in at least one of the analyses. Psychological and social work factors predicted sleep problems in the short term as well as the long term.
Conclusions:
All work factors investigated showed statistically significant associations with both sleep items, however quantitative job demands, decision control, role conflict, and support from superior were the most robust predictors and may therefore be suitable targets of interventions aimed at improving employee sleep.
Citation:
Vleeshouwers J, Knardahl S, Christensen JO. Effects of psychological and social work factors on self-reported sleep disturbance and difficulties initiating sleep. SLEEP 2016;39(4):833–846.
Keywords: sleep, psychosocial, prospective, occupational, longitudinal
Significance.
The results of the present study are of a clear practical and theoretical significance by disclosing relationships of several underexplored psychological and social work factors with difficulties initiating sleep and disturbed sleep. Factors such as quantitative job demands, decision control, role conflict, and support from superior should be modifiable, and thus suitable targets for interventions aimed at improving sleep. While the present study demonstrated both short-term effects, as well as effects after a two-year interval, little is known about the specific mechanisms through which work may affect sleep. Hence, future research should explore in detail how work may affect sleep and when effects occur, possibly through time-series design.
INTRODUCTION
Sleeping problems may affect many aspects of daily life, including job performance, mood state, social functioning, and physical and mental health.1–4 Cost estimates for troubled sleep in Norway do not currently exist, but a 2011 US study estimated the socioeconomic costs roughly between 63 and 91 billion dollars per year.5 The aim of the present study was to determine contributions of psychological work factors to sleep problems in working individuals.
There are over 80 different sleep disorders according to the International Classification of Sleep Disorders.6 However, many may suffer considerable consequences of sleeping problems that are not diagnosed. Many people suffering from troubled sleep may not seek medical help, and physicians may not enquire about sleep problems.7 Additionally, even when quality of life is affected by troubled sleep, sufferers may not satisfy criteria for diagnosis with a specific sleep disorder. The current study investigated sleep problems that may affect everyday life in Norwegian employees, whether this involves a diagnosed sleep problem or not.
Considering the magnitude of the problem (estimated prevalence rates of sleep problems in adults range from 11% to 33%8,9) surprisingly little research seems to have focused on potentially preventable causes of sleep problems. Psychological and social work factors may represent a significant source of such preventable causes. A large number of studies have considered the effects of shift work on sleep or included only a single organization or a single type of work.10–12 The current study incorporated a large number of organizations, covering a wide variety of jobs, comprising a diverse large sample. Moreover, most studies investigating psychological/social work factors and sleep have been cross-sectional, while the current study utilized a full panel prospective design in order to comprehensively explore relationships between work factors and self-reported difficulties initiating sleep and disturbed sleep, cross-sectionally as well prospectively.
The Demand-Control-(Support) Model (DCS)13 is often referred to when explaining adverse health effects of psychological work factors, such as poor sleep.9,14,15 According to the DCS theory, the interaction between job demands and job control determines psychological well-being and health complaints. More specifically, a combination of high job demands and low job control may result in negative health effects. However, this relationship is buffered by social and instrumental support from supervisors and/or colleagues. Research on the effects of work factors on sleep has almost exclusively been based on the DCS model; proposing that job strain (a combination of high job demands and low job control) and social support affect sleep.16–21
In one of the few longitudinal studies investigating work factors and sleep, Magnusson Hanson et al. reported a weak relationship between job demands and subsequent sleep.22 Ota and colleagues found that overcommitment to work (a trait-like factor) and high job strain (the combination of high demands and low control) increased the persistence of sleep problems in insomnia patients.23 However, the causal directions of these associations remain largely unknown, and sleep problems may influence the perception, appraisal, and reporting of work (“reverse” causality).22
The present study considered the relations between psychological/social work factors and sleep problems. A comprehensive set of possible predictors was included, some of which have been associated with other health outcomes in the previous studies,24–28 and some of which are relatively novel in this field. While most previous studies have focused on a small set of fairly general and abstract factors (“stress,” demand, control), the current study focused on specific factors that should be amendable to modification, and could therefore be targeted in employee health and well-being interventions. Furthermore, the present study incorporated the two separate outcomes “difficulties initiating sleep” and “disturbed sleep” to reflect different aspects of sleep problems, both of which are considered symptoms of insomnia.6
The study adopted both univariable and multivariable cross-sectional and prospective regression models to explore possible effects over time within the complex relationship between work factors and sleep. Therefore analyses with baseline exposure as predictor, analyses with average exposure across two waves as predictor, and analyses with change in exposure between two waves as predictor were included.
METHODS
Design
This two-wave prospective study was part of the research project “The new workplace: Work, health, and participation in the new work life”—a project carried out by the Norwegian National Institute of Occupational Health. It is a repeated-measures web-based survey, encompassing data on background information, work organization, psychological and social work factors, coping strategies, attitudes towards work, personality dispositions, and mental and somatic health complaints. The current study is based on parts of this questionnaire. Within this project several work factors have been associated with health outcomes such as neck and back pain, headache, and mental distress.24–28
The mechanisms of putative impacts of psychological and social work factors on sleep are unknown and most likely diverse, and the nature of longitudinal effects of work factors on sleep are still underexplored.9,14,22 Moreover, the duration of exposure needed to produce effects is unknown—as is the expected duration of troubled sleep after exposure is discontinued. Furthermore, these time periods may vary depending on the work factor. In order to capture some of this complexity both prospective and cross-sectional analyses were performed, with different ways of modeling exposure, which will be described below.
Baseline (T1) data were collected from November 2004 until November 2012, and follow-up data (T2) data were collected from September 2006 until November 2014. For all participants follow-up data were collected approximately 2 years after baseline.
Ethical approval was obtained from the Regional Committee for Medical and Health Research Ethics (REK), and the study followed strict guidelines as set by the Norwegian Data inspectorate, who approved the data collection and storage.
Participants
Data included respondents from 63 different companies, covering a wide range of job types. Participants were recruited at the organizational level. Participating organizations received reports and presentations both before and after measurements. Oral presentations of the general aims of the comprehensive research project were delivered prior to the survey, and standardized written reports, as well as oral presentations of results were given after the completion of the survey. The reports were generated by the same template for all organizations and did not focus specifically on sleep problems. Organizations may use information as developmental tools in order to improve the working conditions, but the researchers were not involved in any interventions.
Participants received an information letter including a unique code to complete the survey online or a paper version of the survey with a return envelope. Questionnaires could be completed at work or from home, although all participating companies were obligated to provide opportunities and time for their employees to complete the questionnaire during working hours.
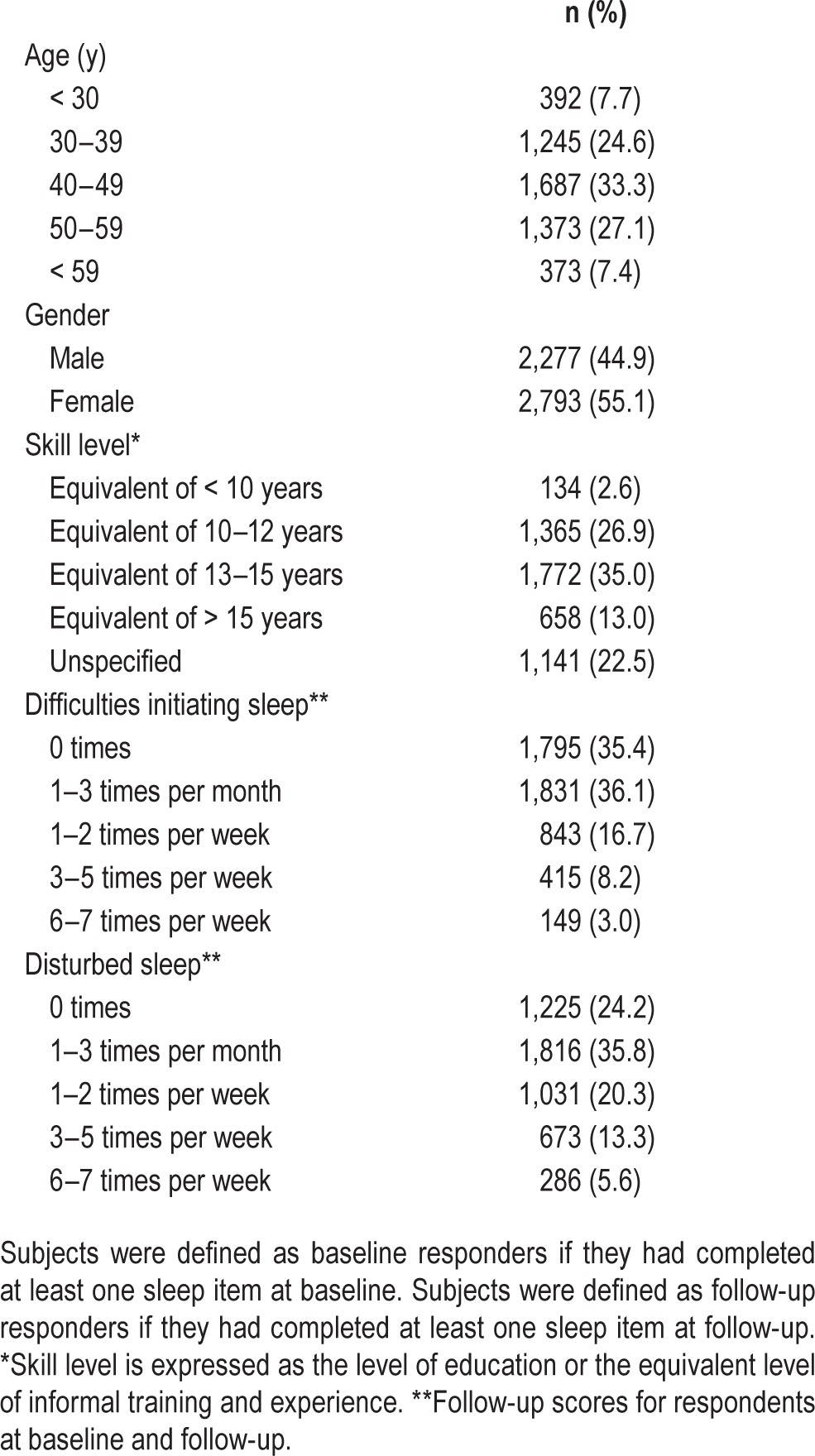
At the time of analysis, a total of 12,659 participants had been invited to participate at both baseline and follow-up. Of the baseline respondent group, 7,459 (58.9%) completed at least one sleep item. These respondents formed the sample for the first cross-sectional analysis. Of the follow-up respondent group, 6,688 (52.8%) completed at least one sleep item. This group formed the sample for the second cross-sectional analysis. A total of 5,070 (40.1%) participants responded at both baseline and follow-up, of whom 44.9% were male and 55.1% were female (see Table 1 for sample characteristics).
Table 1.
Sample characteristics of employees who responded at baseline and follow-up (n = 5,842).
Outcome: Sleep Measures
The two aspects of troubled sleep that were measured were (1) difficulties initiating sleep and (2) disturbed sleep. Items were measured and analyzed separately since these items reflect two distinctly separate symptoms within sleep disorder and insomnia research.6,29
The sleep question was worded as follows: “Have you experienced the following symptoms in the last 4 weeks?” with the following two items: “difficulties falling asleep” and “disturbed sleep.” Response alternatives were as follows: “0 times,” “1–3 times per month,” “1–2 times per week,” “3–5 times per week,” and “6–7 times per week.” The two sleep items were highly correlated with a baseline correlation of ρ 0.68, P < 0.01.
Exposure Measures
Psychological and social work factors were measured with the General Nordic Questionnaire for Psychological and Social Factors at Work (QPSNordic).30 The following factors were investigated: quantitative job demands (4 items, α coefficient at baseline = 0.75 and α coefficient at follow-up = 0.76), decision demands (3 items, α = 0.63 and α = 0.63), decision control (5 items, α = 0.74 and α = 0.73), control of work pacing (4 items, α = 0.82 and α = 0.82), role clarity (3 items, α = 0.82 and α = 0.81), role conflict (3 items, α = 0.70 and α = 0.70), predictability during the next month (3 items, α = 0.62 and α = 0.65), support from superior (3 items, α = 0.86 and α = 0.73), empowering leadership (3 items, α = 0.87 and α = 0.88), fair leadership (3 items, α = 0.81 and α = 0.82), social climate (3 items, α = 0.71 and α = 0.72), commitment to the organization (3 items, α = 0.86 and α = 0.87), and positive challenges at work (3 items, α = 0.78 and α = 0.79). Items were measured with a 5-point Likert scale of frequency of occurrence ranging from “1 = very seldom or never” to “5 = very often or always,” with the exception of social climate which has answer categories ranging from “1 = very little or not at all” to “5 = very much,” and commitment to the organization with answer categories from “1 = completely disagree” to “5 = completely agree.” In order to compare effects of the different levels of exposure, the scores were categorized as follows; scores between 1.00 and 1.80 received value “1,” 1.81–2.60 received value “2,” 2.61–3.40 received value “3,” 3.41–4.20 received value “4,” and 4.21–5.00 received value “5.”
Confounders
Age, sex, skill level, and baseline levels of outcome measures were entered a priori in all regression analyses as potential confounders. Age was categorized into 5 separate age groups; < 30, 30–39, 40–49, 50–59, and > 59. Skill level was determined through classification of occupation, and reflects the corresponding level of education or equivalent level of working experience for said occupation as described in the STYRK classifications, developed by Statistics Norway and based on the International Standard for Classification of Education (ISCED-ISCO88). Categories ranged from occupations that require no more than 9 years of primary education to occupations that normally require a first or postgraduate University degree, or college exams based on a similar length of study (> 15 years of education). Unspecified educations were also accounted for within a category, which is why skill level was treated as a nominal variable.
Prior to the main analyses steps were taken in order to establish the extent to which possible confounding work factors influenced the analyses. The procedure followed was recommended by Rothman31 and is described by Christensen and Knardahl24,25 in similar studies. For both baseline sleep items, a series of separate univariable logistic regressions were conducted with each exposure variable at baseline as predictor. After this, regressions were run with all other exposure variables entered separately for each single exposure variable. Odds ratios from the univariable and bivariable regressions were then compared and changes of 10% or more in the odds ratios when including another exposure variable would lead to that exposure variable being treated as a confounder in all subsequent multivariable analyses for the relevant exposure measure.
Statistical Analyses
All analyses were carried out using IBM SPSS Statistics, version 22.0 (IBM, Armonk, NY). Because of the large number of exposure measures and the multiple testing within the present study the risk of type I error increased. In order to attenuate the likelihood of type I error, 99% confidence intervals were increased and Bonferroni-adjusted, calculated as the overall significance level divided by the number of factors studied (i.e., 0.01/13 = 0.0008); P values were also reported.
Cross-sectional analyses were conducted at baseline as well as follow-up. First univariable ordinal logistic regressions were performed for each exposure variable individually and for both outcome measures, after which multivariable ordinal logistic regressions, using the generalized linear models option within SPSS, were performed for both baseline and follow-up data and for both outcome measures.
Main analyses included prospective analyses with baseline exposure measures as predictors, average exposure as predictors, and change in exposure as predictors (see details below). Estimated confounders as well as age, sex, skill level, and baseline levels of outcome were included in multivariable analyses.
In order to explore the effects of exposure over time, average exposure to the individual psychological/social work factors from baseline to follow-up was calculated by adding values at T1 to values at T2 and dividing these by 2. Additionally, in order to explore how increased, decreased, or unchanged different levels of exposure from baseline to follow-up affected difficulties initiating sleep and sleep disturbance, univariable and multivariable analyses were also carried out with change in exposure from baseline to follow-up as predictor. First, measures were trichotomized into “low” (scores of 1 and 2 on the categorized exposure variable), “middle” (scores of 3), and “high” (scores of 4 and 5), after which change within these categories between baseline and follow-up were reflected in the following categories: “constant low,” “constant middle,” “constant high,” “decrease,” and “increase.”
RESULTS
Non-Response Analysis
A non-response analysis using binary logistic regression with sex and age as predictors showed that being in one of the age groups > 30 (e.g., age 30–39 OR 1.30, 95% CI 1.18–1.44) and being female (OR 1.24, 95% CI 1.20–1.28) statistically significantly (P < 0.05) increased the odds of responding to at least one sleep item at baseline (analyses not shown).
Attrition Analysis
A multivariable binary logistic regression with age, sex, sleep items at baseline, and all work factors as predictors showed a significant decrease in the odds of responding at both baseline and follow-up for those who had also responded at baseline, in the first two age groups (< 30 OR 0.68 and 30–39 OR 0.79) (analyses not shown). Decision demands (category 2 and 4), control of work pacing (category 1–2), role clarity (category 4), positive challenges at work (category 4), role conflict (category 4), social climate (categories 2–4), and commitment to the organization (category 3–4) all exhibited independent, statistically significant positive associations with response at follow-up. Sex, difficulties initiating sleep, and disturbed sleep did not significantly alter the odds of responding at follow-up.
Cross-Sectional Analyses
Univariable regressions at baseline and follow-up were performed, and details of which work factors showed significant associations can be found in the overview table (Table 2).
Table 2.
Overview of statistically significant associations between psychological/social work factors and difficulties initiating sleep (reported on the left hand side of the “/”) and disturbed sleep (reported on the right hand side of the “/”) in univariable and multivariable analyses.
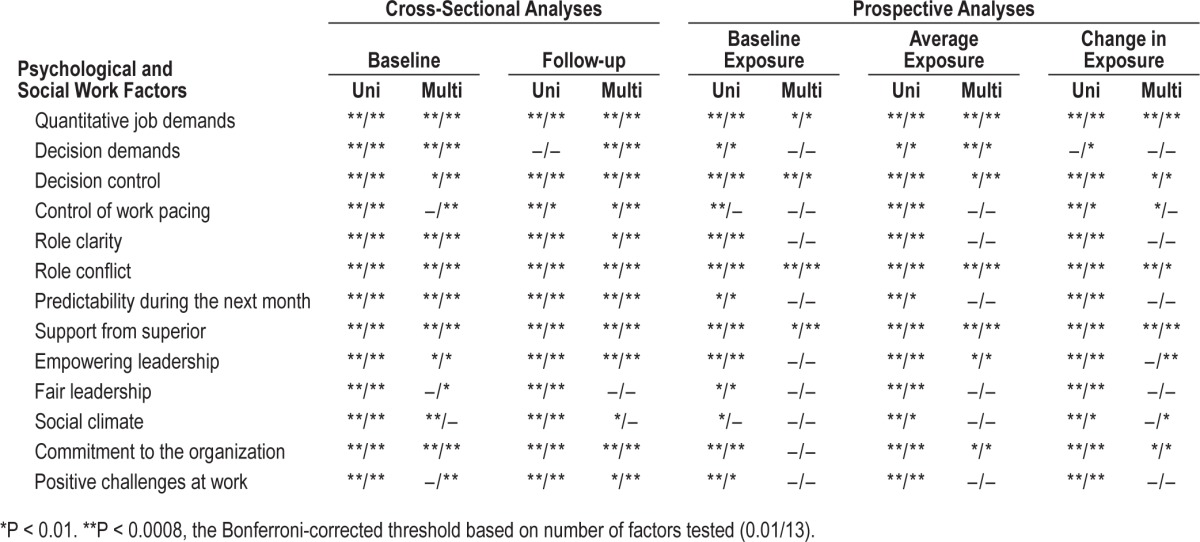
Multivariable regressions for “difficulties initiating sleep” at baseline (see Table S1A in the supplemental material) showed statistically significant associations (P < 0.01) for 10 of the 13 work factors, of which 8 remained statistically significant after Bonferroni correction. At follow-up the same work factors showed statistically significant (P < 0.01) associations, with the addition of control of work pacing and positive challenges at work. Eight work factors remained statistically significant after Bonferroni correction (P < 0.0008). ORs were lowest for support from superior (OR 0.34, 99% CI 0.25–0.47 in category 5 at baseline and OR 0.31, 99% CI 0.22–0.43 in category 5 at follow-up) and highest for role conflict (OR 4.75, 99% CI 3.36–6.73 in category 5 at baseline and OR 4.27, 99% CI 2.88–6.32 in category 5 at follow-up).
Multivariable regressions for sleep item “disturbed sleep” (see Table S1B in the supplemental material) at baseline showed statistically significant (P < 0.01) associations for all work factors apart from social climate. Two factors did not remain significant after Bonferroni correction (P < 0.0008). The same work factors showed statistically significant (P < 0.0008) associations at follow-up, apart from fair leadership (P > 0.01). All work factors remained statistically significant at follow-up after Bonferroni corrections. ORs were lowest for support from superior (OR 0.34, 99% CI 0.25–0.47 in category 5 at baseline and OR 0.29, 99% CI 0.21–0.41 in category 5 at follow-up) and highest for role conflict (OR 4.75, 99% CI 3.36–6.73 in category 5 at baseline and OR 3.17, 99% CI 2.16–4.66 in category 5 at follow-up).
Prospective Analyses
Baseline Exposure
Univariable regressions with baseline exposures as predictors were performed for both outcome measures, and showed statistically significant (P < 0.01) prospective associations with all work factors for “difficulties initiating sleep,” and for all work factors, except for control of work pacing for “disturbed sleep.” After Bonferroni corrections (P < 0.0008), 9 factors remained statistically significant for “difficulties initiating sleep,” while 8 remained significant for “disturbed sleep.”
Multivariable regressions for “difficulties initiating sleep” with baseline exposure as predictor showed statistically significant (P < 0.01) associations for quantitative job demands (OR 1.52, 99% CI 1.03–2.23), decision control (OR 0.53, 99% CI 0.35–0.82), role conflict (OR 2.04, 99% CI 1.28–3.25), and support from superior (OR 0.90, 99% CI 0.82–0.98) (Table 3A). However, quantitative job demands and support from superior did not remain statistically significant at P < 0.0008. ORs ranged from 0.53 at category 5 for decision control to 2.04 at category 5 for role conflict.
Table 3A.
Prospective analyses: multivariable ordinal logistic regression with psychological and social work factors as independent variables and difficulties initiating sleep at follow-up as dependent variable.
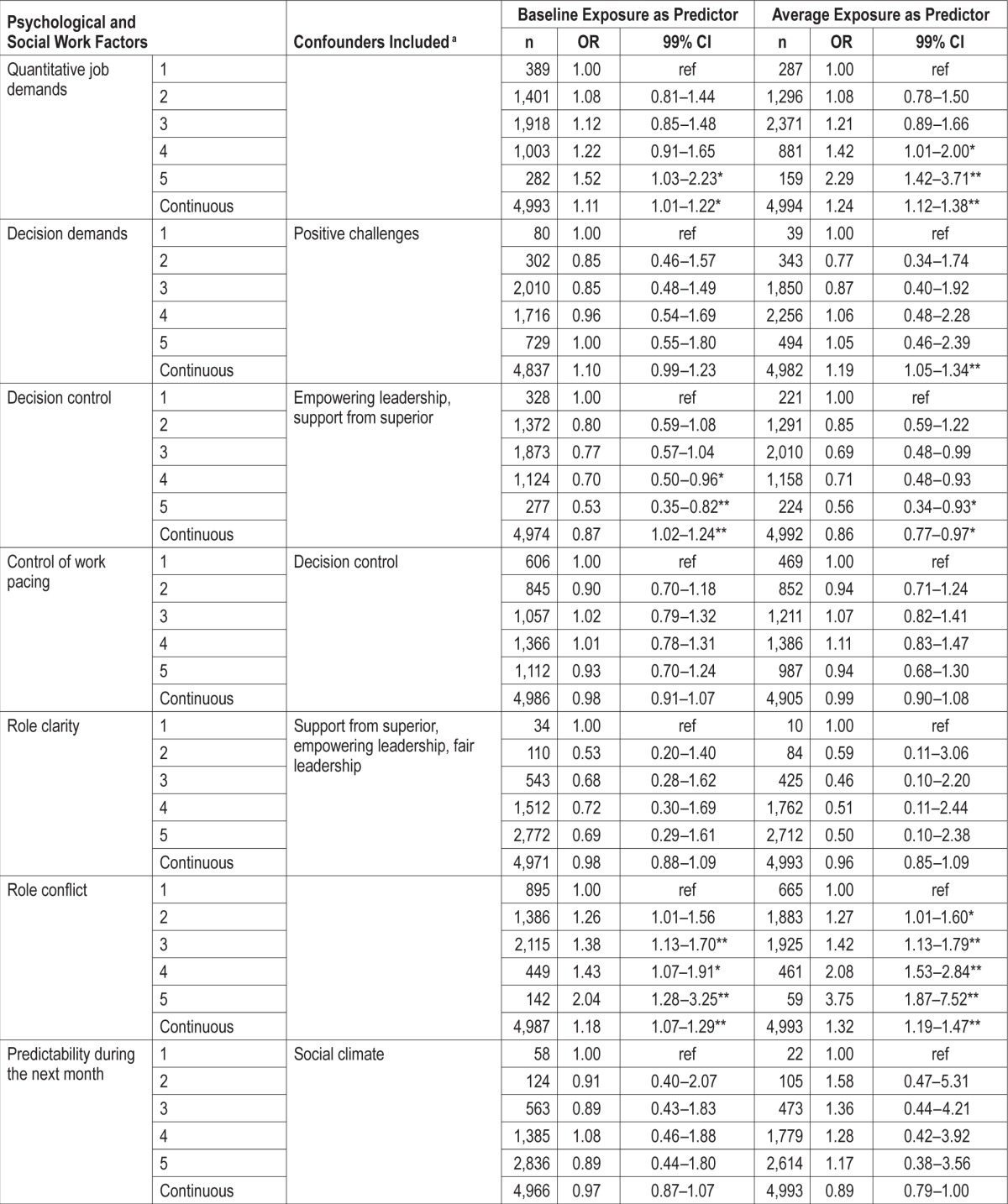
Multivariable regressions for “disturbed sleep” (Table 3B) with baseline exposure as predictor showed statistically significant (P < 0.01) associations for quantitative job demands (OR 1.52, 99% CI 1.05–2.21), decision control (OR 0.71, 99% CI 0.52–0.96), role conflict (OR 1.73, 99% CI 1.09–2.74), and support from superior (OR 0.86, 99% CI 0.79–0.93). However, quantitative job demands and decision control did not remain statistically significant after Bonferroni correction (P < 0.0008). ORs ranged from 0.86 at category 5 for support from superior to 1.73 at category 5 for role conflict.
Table 3B.
Prospective analyses: multivariable ordinal logistic regression with psychological and social work factors as independent variables and disturbed sleep at follow-up as dependent variable.
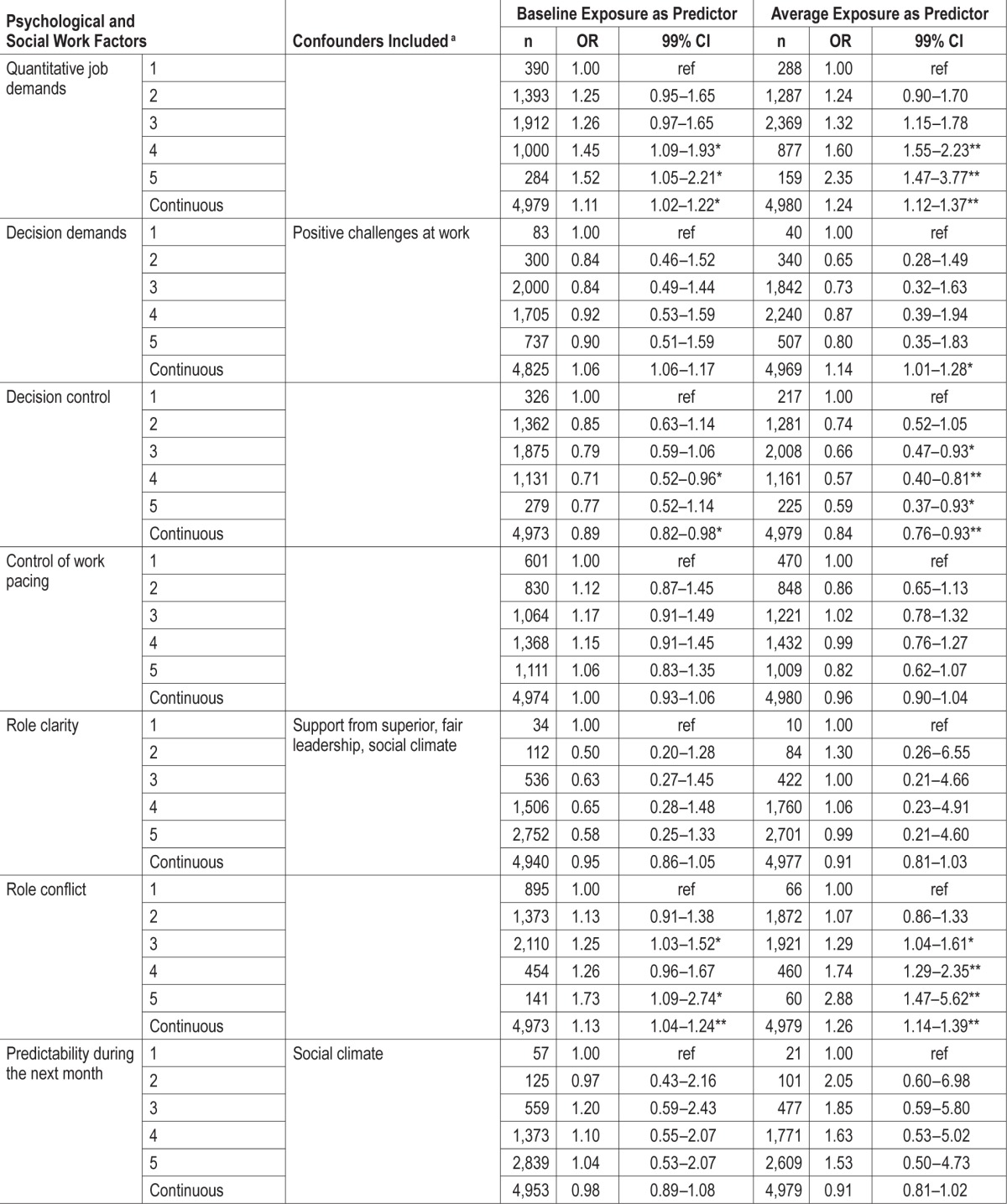
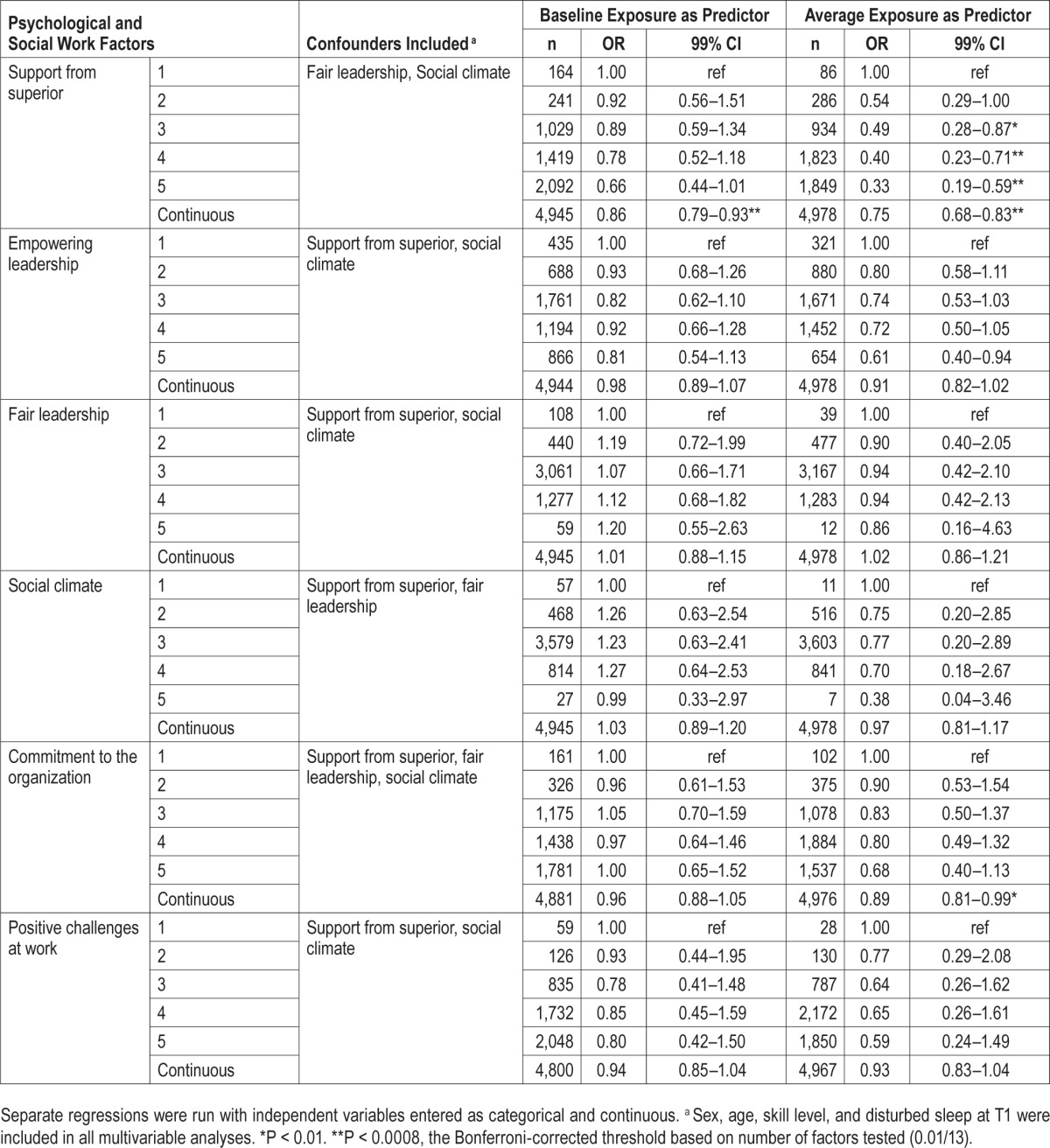
Average Exposure
Univariable logistic regressions were performed with average exposures as predictors for each follow-up sleep item. All averaged work showed statistically significant (P < 0.01) associations with both “difficulties initiating sleep” and “disturbed sleep.” Decision demands did not remain statistically significantly associated with “difficulties initiating sleep” and “disturbed sleep” at P < 0.0008, while predictability during the next month and social climate did not remain statistically significantly associated with “disturbed sleep” at P < 0.0008.
Multivariable regressions for both “difficulties initiating sleep” and “disturbed sleep” with averaged exposures as predictors showed statistically significant (P < 0.01) associations for 7 out of 13 work factors (Table 3A and 3B). Of these quantitative job demands (OR 2.29, 99% CI 1.42–3.71), decision demands (OR 1.19, 99% CI 1.05–1.34), role conflict (OR 3.75, 99% CI 1.87–7.52), and support from superior (e.g. OR 0.39, 99% CI 0.22–0.70) remained statistically significantly associated with “difficulties initiating sleep” at P < 0.0008, while quantitative job demands (OR 2.35, 99% CI 1.47–3.77), decision control (0.57, 99% 0.40–0.81), role conflict (OR 2.88, 99% CI 1.47–5.62), and support from superior (OR 0.33, 99% CI 0.19–0.59) remained statistically significantly associated with “disturbed sleep.” ORs for “difficulties initiating sleep” ranged from 0.39 at category 5 for support from superior to 3.75 at category 5 for role conflict. ORs for “disturbed sleep” ranged from 0.33 at category 5 for support from superior to 2.88 at category 5 for role conflict.
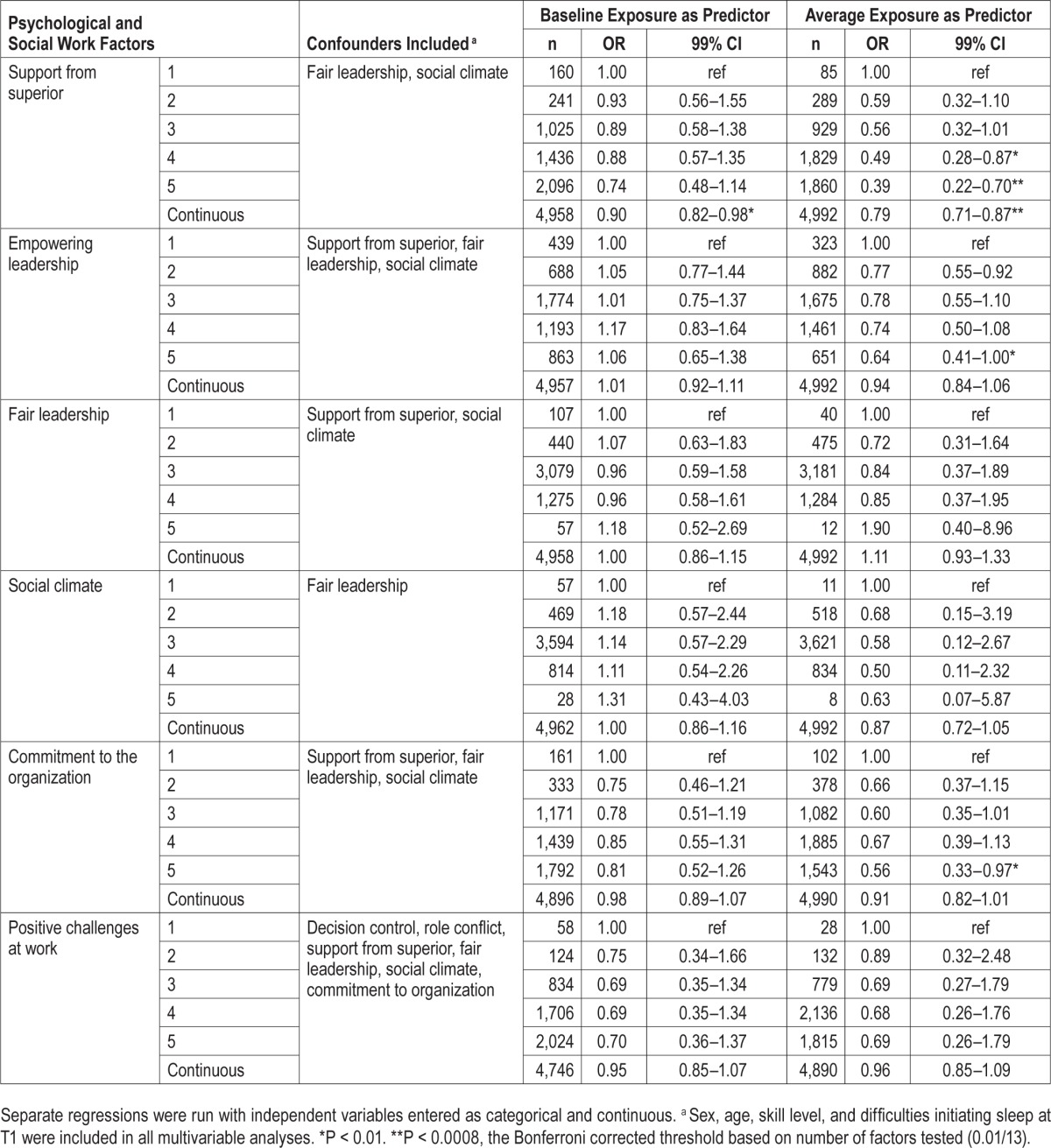
Change in Exposure
Univariable regressions with change in exposure as predictors and “difficulties initiating sleep” as outcome showed statistically significant associations for all work factors, even after Bonferroni corrections, except for decision demands, which remained statistically significant at P < 0.01. ORs ranged from 0.60 (99% CI 0.46–0.80) for constant high social climate to 1.84 (99% CI 1.26–2.68) for constant low support for superior. Univariable regressions with change in exposure as predictor and “disturbed sleep” as outcome showed statistically significant associations for all work factors, however after Bonferroni corrections decision demands, control of work pacing, and social climate did not remain significant. ORs ranged from 0.66 (99% CI 0.59–0.74) for constant high support from superior to 1.98 (99% CI 1.44–2.70) for constant high role conflict. Multivariable ordinal logistic regressions with change in exposure as predictor and “difficulties initiating sleep” as outcome (Table 4) revealed significant associations for 6 of the 13 work factors, and quantitative job demands (constant high, OR 1.72, 99% CI 1.37–2.17), role conflict (constant high, OR 2.08, 99% CI 1.45–2.96), and support from superior (constant high, OR 0.51, 99% CI 0.33–0.79) showed to be most robust associations as these factors remained statistically significant after Bonferroni corrections.
Table 4.
Multivariable ordinal logistic regression with change in exposure to psychological and social work factors as independent variables and difficulties initiating sleep and disturbed sleep at follow-up as dependent variables.
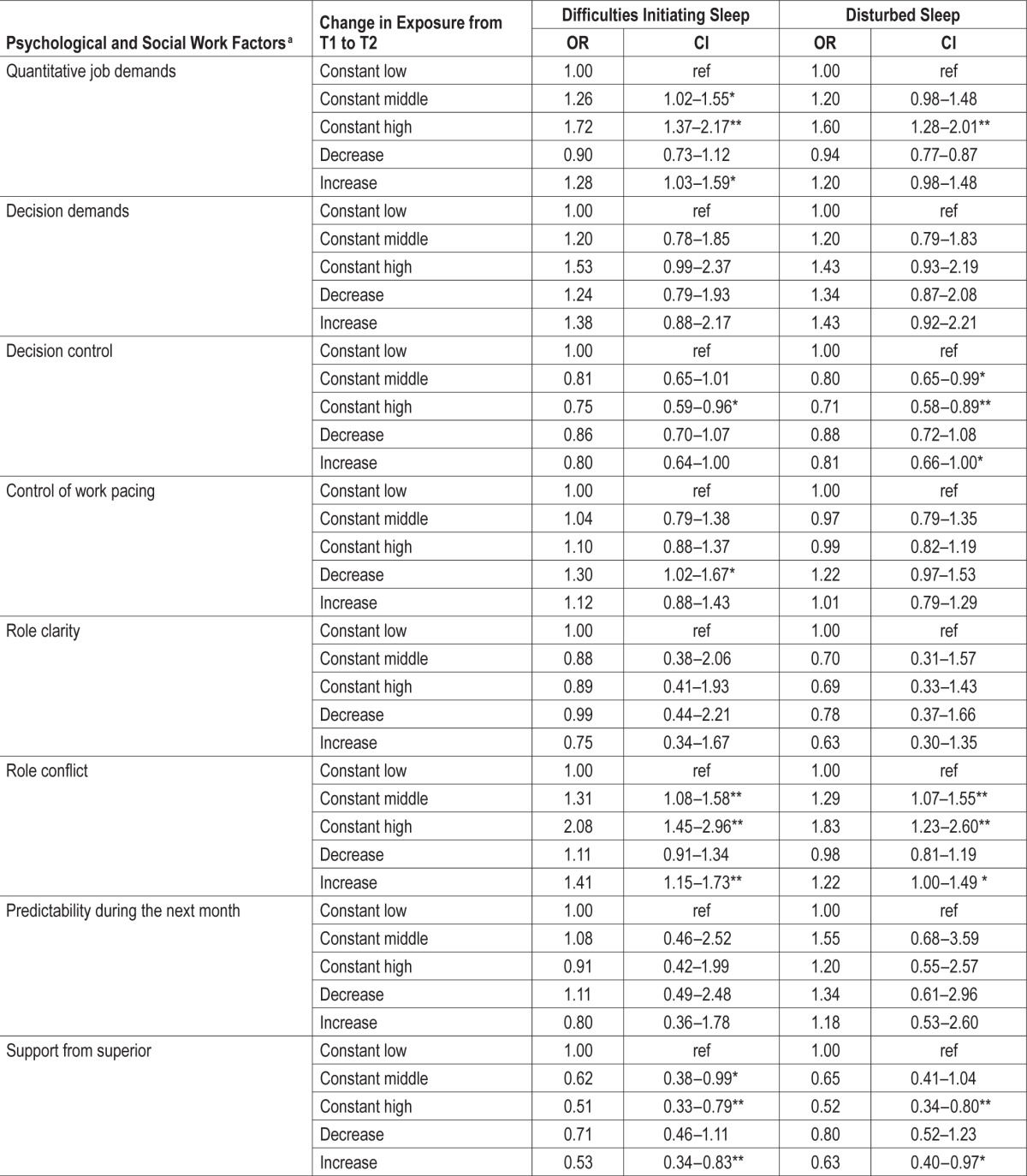
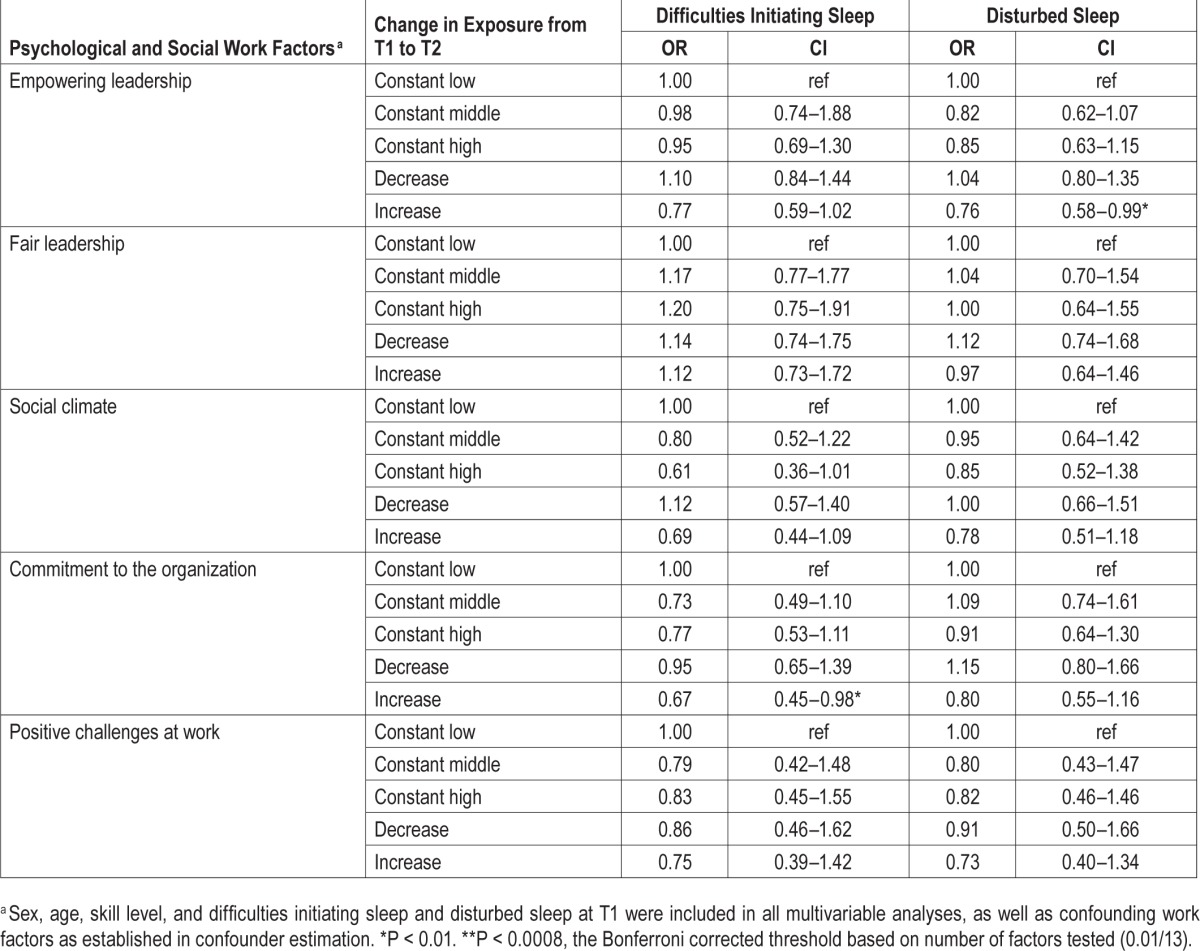
The same analyses but with “disturbed sleep” as outcome (see Table 4), revealed significant associations for 5 of the 13 work factors, with quantitative job demands (constant high, OR 1.60, 99% CI 1.28–2.01), decision control (constant high, OR 0.71, 99% CI 0.58–0.89), role conflict (constant high, OR 1.83, CI 1.23–2.60), and support from superior (constant high, OR 0.52, 99% CI 0.34–0.80) remaining statistically significant after Bonferroni corrections.
An overview of statistically significant associations can be found in Table 2.
DISCUSSION
This study incorporated a broad range of analyses and utilized a full-panel prospective design in order to investigate the extent to which many specific psychological and social work factors predicted two elements of troubled sleep. Of the 13 work factors investigated, quantitative job demands, decision control, role conflict, and support from superior most consistently predicted sleep problems, as these factors exhibited robust statistically significant associations across all analyses. Commitment to the organization was also a robust predictor of troubled sleep, showing significant associations in 9 of the total 10 analyses. Decision demands, control of work pacing, role clarity, fair leadership, social climate, and positive challenges at work on the other hand show significant associations in 4 to 7 of the 10 analyses, but may nonetheless still be important predictors of troubled sleep.
While the diverse analyses have shown some minor differences in associations between the work factors and the two measures of troubled sleep (e.g. social climate shows statistically significant associations with “difficulties initiating sleep” in 7 of 10 analyses, but only shows statistically significant associations with “disturbed sleep” in 5 of 10 analyses), there are no major differential effects, and the four strongest predictors are equally robust for both measures of sleeping problems.
Although previous studies have explored relations between work factors and sleep, to our knowledge this study is the first to reflect such a broad range of psychological/social work factors and occupations while incorporating cross-sectional as well as prospective designs to investigate the effects over time. Findings from the present study showed that a number of different psychological and social work factors predicted difficul-ties falling asleep and disturbed sleep.
Strengths of the present study are the broad set of specific psychological/social work factors and the large amount of different organizations and occupations included. Additionally, the cross-sectional and prospective analyses of the present study explored different time frames of effects of the work factors on sleep, testing both immediate and longer-term effects.
Sleep may influence work factors, i.e., poor sleep may influence mood state and thus influence perceptions of work factors; however the prospective design used in the present study helped establish that work factors predict sleep, therefore relieving some of the issues with causality.
Results of the present study are in line with other prospective studies investigating relations between work factors and sleep. While Ota and colleagues23 discovered positive associations for job strain (job demands/decision control) with insomnia, our study also revealed quantitative job demands and decision control to be statistically significantly associated with troubled sleep. In fact, these two work factors were statistically significant in all our analyses, and quantitative job demands remained significant at P < 0.0008 in 9 of 10 analyses for both sleep outcome measures. Magnusson Hanson et al.22 discovered positive associations between demands and subsequent sleep problems. However, they did not observe an effect of decision authority, while in the present study decision control was one of the strongest predictors of sleep problems.
While in the current study support from supervisor predicted subsequent disturbed sleep and difficulties initiating sleep, Ota and colleagues, and Magnusson Hanson and colleagues both did not find statistically significant effects of support on future sleep problems. However, Ota and colleagues suggested that support may predict persistence of insomnia when sleep problems already exist, while Magnusson Hanson and colleagues found effects of support on subsequent awakening problems.
Role conflict, the last of the four most consistent predictors identified within this study, has also been linked to sleep problems before. Nixon and colleagues in their meta-analysis of 79 cross-sectional and longitudinal studies identified role conflict as significantly related to troubled sleep.32 However, only four studies with role conflict as a predictor had been analyzed, utilizing a combined sample size of only 487 participants. Moreover, it is unclear if any of the studies analyzed are longitudinal. Therefore, examining effects of role conflict on sleep problems in a prospective analysis represented an important contribution to existing research.
As mentioned before, the present study was part of a large project carried out by the Norwegian National Institute of Occupational Health. Previous studies from this project have found associations between work factors and health outcomes such as neck and back pain, headache, and mental distress.24–28 While some work factors seem to have associations with all investigated health outcomes, such as decision control, other work factors which the present study has found to be a strong predictor, such as quantitative job demands, do not show associations with other health outcomes. Future research may want to explore interactions between work factors, sleep, and other health outcomes such as pain.
The design of the QPSNordic (i.e., reversed items and scales based on frequency of occurrence) should have relieved potential issues with reporting bias. Type II error may have occurred due to possible over-adjustment, while on the other hand, incorporating continuous predictors in the prospective analyses should lower chances of type II error.
A priori power calculations were not conducted, since the dataset was available before commencement of the study. The sample was large, but there may be issues of power to detect statistically significant associations in some cases, particularly with categorical variables, as categorization results in information loss. In the prospective analyses with “baseline exposure” and “average exposure,” we included analyses of exposure measures as continuous variables. In some cases, the continuous exposure measures indicated effects that were not evident from the corresponding categorized exposure measures. For instance, when observing the effect of baseline levels of support from superior on difficulties initiating sleep (Table 3A), it seems reasonable to suspect that the nonsignificance of effects of specific levels of exposure is partly due to the limited number of employees reporting low support.
Effects on difficulties initiating sleep and sleep disturbance could occur at a threshold of the outcome variable. That is, the effect of aversive working conditions can be thought to manifest only as severe sleep problems, such as insomnia, rather than rare or occasional sleeping difficulties. However, prior to analyses assumptions of ordinal logistic regression were tested, including the assumption of proportional odds, indicating that the difference in risk was proportional across all cut points of the outcome. Moreover, multinomial logistic regressions were performed for each separate exposure variable with every outcome category compared to “never” as reference category. Results indicated that there is a consistent incline in ORs for each level of the outcome variables, with no clear cutoff point, suggesting a linear change in risk.
An additional issue could be that there may be other factors at play, such as family life, economic situation, depression, or personality, which could have affected perceptions of work factors and therefore influenced sleep. While the present study has corrected for a large amount of confounding factors, future research may wish to incorporate other relevant confounders. For example, impaired daytime functioning, a key factor of insomnia, may be involved in the relationship between work factors and troubled sleep.33 Impaired daytime functioning may influence appraisal of working conditions, as well as interpersonal relationships and execution of tasks, which in turn may affect sleep. The scope of the current study did not permit detailed investigation of reciprocal causal processes, so this remains an important task for future projects, and daytime functioning is one factor that could be included in such investigations. Also, assessing daytime functioning will provide valuable insight regarding the extent to which sleep problems affect health and quality of life.
Participating companies received reports and presentations of findings after each round of data collection. It is possible that organizations used this information to improve working conditions after T1, which could have had an effect on exposure measures at T2. In order to take into account possible changes in exposure measures from T1 to T2, we incorporated the “average exposure as predictor” and “change in exposure” analyses. However, post hoc analyses revealed no significant differences in exposure measures between T1 and T2 in the overall sample (analyses not shown).
Associations found in change in exposure as a predictor may be interpreted in different ways. For example, constant high levels of quantitative job demands significantly predict troubled sleep. One could argue that this finding is irrelevant, as cross-sectional analyses had already established relations between quantitative job demands and the two sleep items. Constant high quantitative job demands could simply pick up the relation between high job demands at T2 and sleep at T2. However, when comparing the ORs of cross-sectional analyses at follow-up to ORs of prospective analyses with change in exposure as predictor, the ORs for change in exposure are slightly higher (1.72 as compared to 1.29 for difficulties initiating sleep, and 1.60 as compared to 1.32 for disturbed sleep). This may indicate the importance of work factors at baseline on future troubled sleep. Moreover, prospective effects of quantitative job demands were established in baseline exposure as predictor and average exposure as predictor analyses. Change in exposure then gives insight in how adapting psychological and social work factors may improve sleep, e.g., an increase in support from superior may improve difficulties initiating sleep (OR 0.53, 99% 0.34–0.83), while an increase in support from superior may improve disturbed sleep (OR 0.63, 99% 0.40–0.97). Additionally, the effect of constant high demands was stronger than that of an increase, i.e., the effect of high exposure at both time points is stronger than the effect of high exposure only at follow-up. This suggests that repeated high exposure has greater consequences for sleep than high exposure at one time point, further strengthening assumptions of causality.
Åkerstedt and colleagues also investigated the effects of change in work factors over time on sleep, and suggested that constant high or an increase in demands may predict future sleep problems 5 years later.15 While the present study did find that constant high quantitative demands may predict both difficulties initiating and disturbed sleep, no significant results were found for increase in quantitative demands. Moreover, while Åkerstedt and colleagues concluded that change in control at work did not predict later onset of sleep difficulties, the present study found that constant low decision control may in fact predict future difficulties initiating and future disturbed sleep. Differences in findings may be due to the use of different timespans. The present findings are in concordance with those of Jansson and Linton,34 who discovered that high work demands and low influence over decisions were associated with the continuation of self-reported insomnia over the course of one year, and suggested these work factors, along with leader support, may predict onset and continuation of insomnia.
Although the present study with two-year interval indicated that work factors predict troubled sleep disturbance over time, the change in exposure analyses did not contain information about when or how such changes occurred. Gradual change from, e.g., high levels of role conflict to lower levels of role conflict could have occurred due to an employee getting more acquainted with their role and what is expected from him/her, but immediate change could have also occurred, for instance due to a new superior or new role descriptions. Immediate change may have occurred directly after T1 measurements or right before T2 measurements. Potentially, the effects of change in work factors on sleep may weaken over time; however, it was outside the scope of the present study to test this. Future research should explore the details of how change in work factors may affect sleep, potentially through the use of time-series design.
In conclusion, findings from this prospective cohort study suggest that modifiable psychological and social work factors affect sleep, both short-term as well as over time. While quantitative job demands, decision control, role conflict, and support from superior were found to be the most robust predictors of sleep problems, potential interventions to change employees' appraisals of all work factors investigated may lead to improved sleep, which could in turn affect health, sickness absence, and productivity.
DISCLOSURE STATEMENT
This study was funded by the Norwegian Research Council (grant number: 185209). The funders had no role in study design, data collection and analysis, decision to publish, ore preparation of the manuscript. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank all participating companies, as well as Bjørn Lau, Anne Lene Andersen, Shahrooz Elka, Elisabeth Petersen, Margrethe Schøning, and Jan S. Emberland for their help in survey administration.
REFERENCES
- 1.Barone MT, Menna-Barreto L. Diabetes and sleep: a complex cause-and-effect relationship. Diabetes Res Clin Pract. 2011;91:129–37. doi: 10.1016/j.diabres.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 2.Colten HR, Altevogt BM Institute of Medicine (U.S.) Washington, DC: Institute of Medicine: National Academies Press; 2006. Committee on Sleep Medicine and Research. Sleep disorders and sleep deprivation: an unmet public health problem. [PubMed] [Google Scholar]
- 3.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesce Health. 2010;46:124–32. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 4.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kessler RC, Berglund PA, Coulouvrat C, et al. Insomnia and the performance of US workers: results from the America insomnia survey. Sleep. 2011;34:1161–71. doi: 10.5665/SLEEP.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thorpy MJ. Classification of sleep disorders. Neurotherapeutics. 2012;9:687–701. doi: 10.1007/s13311-012-0145-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Namen AM, Landry SH, Case LD, McCall WV, Dunagan DP, Haponik EF. Sleep histories are seldom documented on a general medical service. South Med J. 2001;94:874–9. [PubMed] [Google Scholar]
- 8.Hossain JL, Shapiro CM. The prevalence, cost implications, and management of sleep disorders: an overview. Sleep Breath. 2002;6:85–102. doi: 10.1007/s11325-002-0085-1. [DOI] [PubMed] [Google Scholar]
- 9.Magnusson Hanson LL, Chungkham HS, Akerstedt T, Westerlund H. The role of sleep disturbances in the longitudinal relationship between psychosocial working conditions, measured by work demands and support, and depression. Sleep. 2014;37:1977–85. doi: 10.5665/sleep.4254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Axelsson J, Akerstedt T, Kecklund G, Lowden A. Tolerance to shift work-how does it relate to sleep and wakefulness? Int Arch Occup Environ Health. 2004;77:121–9. doi: 10.1007/s00420-003-0482-1. [DOI] [PubMed] [Google Scholar]
- 11.Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27:1453–62. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- 12.Pilcher JJ, Lambert BJ, Huffcutt AI. Differential effects of permanent and rotating shifts on self-report sleep length: a meta-analytic review. Sleep. 2000;23:155–63. [PubMed] [Google Scholar]
- 13.Karasek RA. Job demands, job decision latitude, and mental strain -implications for job redesign. Admin Sci Quart. 1979;24:285–308. [Google Scholar]
- 14.Akerstedt T. Psychosocial stress and impaired sleep. Scand J Work Environ Health. 2006;32:493–501. [PubMed] [Google Scholar]
- 15.Akerstedt T, Nordin M, Alfredsson L, Westerholm P, Kecklund G. Predicting changes in sleep complaints from baseline values and changes in work demands, work control, and work preoccupation--the WOLF-project. Sleep Med. 2012;13:73–80. doi: 10.1016/j.sleep.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Eriksen W, Bjorvatn B, Bruusgaard D, Knardahl S. Work factors as predictors of poor sleep in nurses' aides. Int Arch Occup Environ Health. 2008;81:301–10. doi: 10.1007/s00420-007-0214-z. [DOI] [PubMed] [Google Scholar]
- 17.Kalimo R, Tenkanen L, Härmä M, Poppius E, Heinsalmi P. Job stress and sleep disorders: findings from the Helsinki Heart Study. Stress Health. 2000;16:65–75. [Google Scholar]
- 18.Knudsen HK, Ducharme LJ, Roman PM. Job stress and poor sleep quality: data from an American sample of full-time workers. Soc Sci Med. 2007;64:1997–2007. doi: 10.1016/j.socscimed.2007.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakata A, Haratani T, Takahashi M, et al. Job stress, social support, and prevalence of insomnia in a population of Japanese daytime workers. Soc Sci Med. 2004;59:1719–30. doi: 10.1016/j.socscimed.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Nomura K, Nakao M, Takeuchi T, Yano E. Associations of insomnia with job strain, control, and support among male Japanese workers. Sleep Med. 2009;10:626–9. doi: 10.1016/j.sleep.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 21.Akerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G. Sleep disturbances, work stress and work hours: a cross-sectional study. J Psychosom Res. 2002;53:741–8. doi: 10.1016/s0022-3999(02)00333-1. [DOI] [PubMed] [Google Scholar]
- 22.Hanson LL, Akerstedt T, Naswall K, Leineweber C, Theorell T, Westerlund H. Cross-lagged relationships between workplace demands, control, support, and sleep problems. Sleep. 2011;34:1403–10. doi: 10.5665/SLEEP.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ota A, Masue T, Yasuda N, et al. Psychosocial job characteristics and insomnia: a prospective cohort study using the Demand-Control-Support (DCS) and Effort-Reward Imbalance (ERI) job stress models. Sleep Med. 2009;10:1112–7. doi: 10.1016/j.sleep.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Christensen JO, Knardahl S. Work and neck pain: a prospective study of psychological, social, and mechanical risk factors. Pain. 2010;151:162–73. doi: 10.1016/j.pain.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Christensen JO, Knardahl S. Work and back pain: a prospective study of psychological, social and mechanical predictors of back pain severity. Eur J Pain. 2012;16:921–33. doi: 10.1002/j.1532-2149.2011.00091.x. [DOI] [PubMed] [Google Scholar]
- 26.Christensen JO, Knardahl S. Time-course of occupational psychological and social factors as predictors of new-onset and persistent neck pain: a three-wave prospective study over 4 years. Pain. 2014;155:1262–71. doi: 10.1016/j.pain.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 27.Finne LB, Christensen JO, Knardahl S. Psychological and social work factors as predictors of mental distress: a prospective study. Plos One. 2014:9. doi: 10.1371/journal.pone.0102514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Christensen JO, Knardahl S. Work and headache: a prospective study of psychological, social, and mechanical predictors of headache severity. Pain. 2012;153:2119–32. doi: 10.1016/j.pain.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 29.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 30.Lindström K. Copenhagen: Nordic Council of Ministers; 2000. User's guide for the QPSNordic: general Nordic questionnaire for psychological and social factors at work. [Google Scholar]
- 31.Rothman KJ, Greenland S. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1998. Modern epidemiology. [Google Scholar]
- 32.Nixon A, Mazzola J, Bauer J, Krueger J, Spector P. Can work make you sick? A meta-analysis of the relationships between job stressors and physical symptoms. Work Stress. 2011;25:1–22. [Google Scholar]
- 33.Varkevisser M, Kerkhof GA. Chronic insomnia and performance in a 24-h constant routine study. J Sleep Res. 2005;14:49–59. doi: 10.1111/j.1365-2869.2004.00414.x. [DOI] [PubMed] [Google Scholar]
- 34.Jansson M, Linton SJ. Psychological mechanisms in the maintenance of insomnia: arousal, distress, and sleep-related beliefs. Behav Res Ther. 2007;45:511–21. doi: 10.1016/j.brat.2006.04.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


