Abstract
Study Objectives:
We examined the association of objectively and subjectively measured sleep disturbances with depression, and explored if race/ethnicity, socioeconomic status, and sex modified these associations.
Methods:
We used data from the cross-sectional Multi-Ethnic Study of Atherosclerosis Sleep Study. Participants included 1,784 adults (ages 54–93 y), 36.8% non-Hispanic Whites, 28.0% African Americans, 23.7% Hispanics, 11.5% Chinese, and 46.0% males. Sleep was assessed with actigraphy, polysomnography, and self-report. Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression (CES-D) scale. We used relative risk regression to evaluate the association of sleep measures and depression (CES-D score ≥ 16) adjusting for site, sociodemographics, and behavioral and medical risk factors.
Results:
Overall, 14.5% had depression, 29.3% had insomnia symptoms, 14.1% had excessive daytime sleepiness (EDS), 15.1% had apnea-hypopnea index (AHI) ≥ 30, and 30.4% experienced short sleep (< 6 h). Depression was associated with short sleep duration (adjusted prevalence ratio [PR] = 1.47, 95% confidence interval [CI] = 1.11, 1.94), < 10% rapid eye movement [REM] sleep (PR = 1.57, 95% CI = 1.08, 2.27), ≥ 25% REM sleep (PR = 1.42, 95% CI = 1.03, 1.95), insomnia (PR = 1.83, 95% CI = 1.39, 2.40), excessive daytime sleepiness (EDS) (PR = 1.61, 95% CI = 1.19, 2.18), and AHI > 15 + EDS (PR = 1.55, 95% CI = 1.01, 2.39). Short sleep duration was associated with depression among those with high school education or beyond, but not among those with less education. Insomnia was more strongly associated with depression among men than women.
Conclusions:
Sleep disturbances are associated with depression among middle-aged and older adults; these associations may be modified by education and sex. Future research should further test these hypotheses, evaluate whether early detection or treatment of sleep disturbances ameliorate depression, and explore subpopulation differences.
Citation:
Alcántara C, Biggs ML, Davidson KW, Delaney JA, Jackson CL, Zee PC, Shea SJ, Redline S. Sleep disturbances and depression in the multi-ethnic study of atherosclerosis. SLEEP 2016;39(4):915–925.
Keywords: actigraphy, polysomnography, psychosocial, race/ethnicity, socioeconomic factors
Significance.
Our aims were to examine whether or not sleep disturbances were associated with depression, and to explore if sociodemographic characteristics modified these associations in a middle-aged and older adult multiethnic community sample. Objectively- and subjectively-measured sleep disturbances—short sleep duration (< 6 hours), insomnia, excessive daytime sleepiness, low and high proportion of rapid eye movement sleep— were consistently associated with a higher prevalence of depression. Exploratory analyses suggest that educational attainment and sex may modify the association of specific sleep disturbances (i.e., short sleep duration, insomnia) with depression. Future research should further test these hypotheses, and evaluate whether early detection or treatment of sleep disturbances improves depression outcomes.
INTRODUCTION
Sleep disturbances—short sleep duration, insomnia, poor sleep quality, alterations in sleep architecture and obstructive sleep apnea (OSA)—often precede, co-occur with, or in some cases, result from the onset of depression.1–8 For example, more than 90% of patients with depression report some type of sleep disturbance (e.g., insomnia symptoms, daytime sleepiness)8,9 and those with OSA have a nearly double odds of depression compared to those without OSA.7 Further, adults with depression often exhibit alterations in their sleep architecture such as an alteration in regulation of rapid eye movement (REM) sleep and poor sleep efficiency.6,10 Although separate literature has documented differences in the prevalence of sleep disturbances and depression by race/ethnicity, socioeconomic status (SES), and sex,11–13 to our knowledge, no studies to date have explored whether the association between sleep disturbances and depression substantially (or importantly) differs by these sociodemographic characteristics. Thus, important gaps remain in the literature regarding the association of specific sleep dimensions with depression and potential sociodemographic modifiers; knowledge into these factors could in turn inform the development of targeted preventive efforts to improve sleep and mental health.
Sociodemographic factors have been inconsistently linked to sleep disturbances because of study-specific factors such as how sleep was assessed (subjective versus objective measurement), and whether race/ethnicity and SES were simultaneously included in statistical models.14 For example, most studies using objective measures of sleep such as polysomnography (PSG) or actigraphy find that African Americans, individuals from low SES backgrounds, and men are more likely than their non-Hispanic White, high SES, and women counterparts to exhibit short sleep duration, or disrupted sleep continuity and sleep architecture.11,15–18 Relatedly, racial/ethnic minorities are more likely than Whites to have persistent, severe, and under-diagnosed sleep disorders such as OSA.18–20 Research using subjective measures of sleep such as self-report questionnaires documents similar trends; women and African Americans are more likely to endorse insomnia and poor overall sleep quality.15,18 However, at least one study shows no difference between men and women or between racial/ethnic groups in self-reports of sleep quality and insomnia.21
The literature on sociodemographic differences in depression is far more consistent. Women and individuals with low SES are more likely than their counterparts to meet criteria for depression and/or endorse elevated depressive symptoms.13,22 Indeed, women have a 40% increased risk of past-month depression than men, and those with income levels below the poverty line have doubled risks of depression.13 In contrast, most studies indicate that, on average, racial/ethnic minorities and non-Hispanic Whites do not have different prevalence rates for depression, but the chronicity or severity of depression is markedly higher among racial/ethnic minorities, and the likelihood of receiving adequate care for their depression is quite low, and remains low even after accounting for SES.13,23,24
Racial/ethnic and socioeconomic disparities in health are often the consequence of differential access to resources that promote good health.25–27 With regard to sleep, racial/ethnic minorities and those with low SES are more likely than their counterparts to have fewer psychosocial, economic, and environmental resources that promote adequate sleep or the prompt resolution of sleep problems, as evidenced by less access to effective sleep treatment, high rates of nonadherence to sleep treatment regimens, and greater exposure to contextual disadvantage, discrimination, and stress.15,19,28–32 However, investigations into sociodemographic modifiers of sleep have been few, and limited by small sample sizes (especially the numbers of racial/ethnic minorities), exclusive use of subjective measures of sleep, and constricted socioeconomic ranges.
To address these prior limitations, we examined the association of objectively and subjectively measured sleep disturbances (i.e., short sleep duration, poor sleep continuity, alterations in sleep architecture, symptoms of insomnia and excessive daytime sleepiness [EDS], OSA, sleep apnea syndrome) with depression among community-dwelling adults enrolled in the Multi-Ethnic Study of Atherosclerosis (MESA) Sleep Ancillary Study. We also investigated in exploratory analyses whether race/ethnicity, socioeconomic status (education and income), and sex were significant effect modifiers. We hypothesized that each of the sleep disturbances would be associated with a higher prevalence ratio (PR) of depression after controlling for potential confounders. We also expected that: (1) the association of objectively measured short sleep duration with depression would be stronger for African Americans when compared to their non-Hispanic White counterparts; and (2) the association of subjectively measured sleep quality (e.g., insomnia, EDS) with depression would be stronger among individuals from low socioeconomic backgrounds and women relative to individuals from high socioeconomic backgrounds and men.
METHODS
Data Source and Sample
MESA is a multisite prospective cohort study of 6,814 men and women from racially and ethnically diverse backgrounds recruited from six community sites in the United States: Baltimore City and Baltimore County, MD; Chicago, IL; Forsyth County, NC; Los Angeles County, CA; Northern Manhattan and the Bronx, NY; and St. Paul, MN.33 MESA was specifically designed to study the distribution of subclinical cardiovascular disease (CVD) across racial/ethnic groups, and factors associated with progression of the subclinical disease. Thus, as part of eligibility criteria for MESA, participants could have no evidence of clinical CVD at enrollment.33 We used cross-sectional data from the MESA Sleep Ancillary Study,34 which collected quantitative measures of sleep and sleep disordered breathing to evaluate how sleep measures and sleep disorders are associated with cardiovascular risk. At MESA Exam 5 (2010–2013), 10 y after the initial examination, all MESA participants other than those reporting regular use of oral devices, nocturnal oxygen, or nightly positive airway pressure devices were invited to participate in the MESA Sleep Ancillary Study, composed of 1 night of in-home PSG, 7-d actigraphy, and sleep questionnaire data collected during an in-home examination visit. Of 4,077 participants approached, 147 (6.5%) were ineligible (95 due to a history of the positive airway pressure machine use [2%]; 4 due to use of an oral appliance; and 4 due to oxygen use) and 141 participants resided too far from the study sites to participate. Of those remaining (n = 3,789), 59.7% participated in the sleep examination (n = 2,261). A minimum of 3 d of actigraphy data with > 50% reliable data were required for a “passed” actigraphic study. Studies with fewer than 4 weekdays and 1 weekend day of acceptable data were repeated when possible. Of the passed actigraphic studies (97%), there was an average of 6.9 (0.54) d of acceptable data, 5.0 (0.42) d of weekday data, and 2.0 (0.27) d of weekend data. Of the PSG studies, 4.9% failed minimal study quality, and 80% were judged to be in the very good to outstanding quality. Overall, 2,060 had successful PSG data, 2,156 had actigraphy data, and 2,240 participants had completed sleep questionnaires. Our final sample included 1,784 participants with complete sleep, depression, and covariate data; we excluded participants with any missing covariate data (< 4% of those with complete sleep and depression data). Institutional Review Board approval was obtained at each study site and written informed consent was obtained from all participants.
Measures
Sleep Duration and Sleep Continuity
Actigraphy was used to measure mean sleep duration and sleep continuity. Actigraphy-measured sleep duration is a more representative index of habitual sleep duration than PSG-measured sleep duration and we had an a priori interest in understanding the association of habitual or typical sleep duration and prevalence of depression. Actigraphy was performed using the Actiwatch Spectrum wrist actigraph (Philips Respironics, Murrysville, PA, USA) worn on participants' nondominant wrist for 7 consecutive days.35 Actigraphic data were scored during 30-sec epochs as sleep or wake by Actiware-Sleep version 5.59 analysis software (Mini Mitter Co, Inc, Bend, OR, USA.). A validated algorithm was used in which activity counts recorded during the measured epoch were modified by the level of activity in the surrounding 2-min time period (e.g., ± 2 min) to yield the final activity count for each epoch.36 Self-reported sleep diary information and data on light from the wrist actigraphy were used to annotate the records, and determine a lights-off period and sleep onset latency. Sleep duration and sleep quality (sleep maintenance efficiency) were estimated for each day. Short sleep duration was defined a priori as mean sleep duration of < 6 h. Long sleep duration was defined as a mean sleep duration of > 9 h. The reference category for sleep duration (6–9 h) was based on prior literature.37 Poor sleep continuity was defined as having a mean sleep maintenance efficiency (percentage of sleep time after sleep onset/sleep period) < 85%.38 We also calculated the mean sleep onset latency (min).
Sleep Architecture, OSA, and Sleep Apnea Syndrome
PSG was used to measure sleep architecture and OSA. PSG was conducted using a 15-channel monitor (Compumedics Somte System; Compumedics Ltd., Abbotsville, AU). The recording montage included electroencephalography (EEG), bilateral electrooculograms, chin electromyography (EMG), bipolar electrocardiography (ECG), thoracic and abdominal respiratory inductance plethysmography, airflow measured by thermocouple and nasal pressure cannula, finger pulse oximetry, and bilateral limb movements. PSG provided quantitative assessments of levels of overnight hypoxemia, apneas and hypopneas, and sleep stage distributions. Sleep stages and EEG (cortical) arousals were scored according to published guidelines.39,40 Based on the literature implicating REM sleep dysregulation with depression, our primary measure of sleep architecture was the proportion of REM sleep, defined as a percentage of the sleep period. We also calculated REM latency, defined as the delay in minutes between sleep onset and first epoch of REM sleep (excluding wake period). Apneahypopnea index (AHI) was calculated based on the average number of all apneas plus hypopneas associated with a 4% desaturation per hour of sleep. Severe OSA was defined as an AHI ≥ 30 events/h; we also examined the association of AHI > 15, a level considered to denote moderate OSA, with depression.
Sleep Quality
Self-administered questionnaires were used to measure sleep quality. Insomnia was measured using the Women's Health Initiative Insomnia Rating Scale (WHIIRS).41 The WHIIRS is a five-item questionnaire that asks respondents to rate how frequently they experience difficulty with sleep initiation and maintenance (i.e., sleep latency, sleep maintenance, early morning awakening, sleep quality) over the past 4 w. Each question is scored on a five-point scale (0 to 4), where 0 corresponds to “no, not in the past 4 weeks” and 4 corresponds to “yes, 5 or more times a week.” Scores range from 0 to 20, and a total score was calculated. WHIIRS scores ≥ 10 were considered clinically significant insomnia symptoms, because this cutoff is associated with high specificity and sensitivity for differentiating those with and without diagnostic insomnia.41 Sleepiness was measured using the Epworth Sleepiness Scale (ESS).42 The ESS is an eight-item questionnaire that asks respondents to rate his or her likelihood of falling asleep in eight different contexts, and each question is rated on a four-point scale (0–3); scores range from 0–24, and a total score was calculated. EDS was defined as an ESS > 10 based on prior research indicating that this cutoff differentiates between healthy controls and those with recognizable sleep disorders.42 Sleep apnea syndrome was defined as AHI > 15 plus ESS > 10. An AHI of 15 was used rather than a lower threshold given the older age of the sample and very high prevalence of mildly elevated AHI levels.
Depression
Depressive symptoms at Exam 5 were measured with the Center for Epidemiologic Studies Depression scale (CES-D), which is a 20-item self-report questionnaire that asks respondents to rate how often in the past-week they have experienced depressive symptoms on a four-point scale (0–3).43–45 The CES-D has excellent psychometric properties; scores 16 and higher indicate moderate to severe depressive symptoms and probable depression at the population level.43–45 Because MESA is a community-based epidemiological sample, we used a CES-D score of 16 or higher to indicate probable depression in these analyses.
Sociodemographics
Sex and race/ethnicity (non-Hispanic White, African American, Hispanic, Chinese) were self-reported. Education (high school or less, some college or technical school, graduate or professional school), and total gross family income (< $25,000, $25,000–$49,999, $50,000–$74,999, > $74,999) were self-reported as indicators of socioeconomic status.
Covariates
Age at Exam 5 was calculated from Exam 5 date and birthdate. Body mass index (kg/m2) was calculated from measured weight and height. Hypertension at Exam 5 was based on the criteria of the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI), which defined hypertension as systolic blood pressure ≥ 140 mm Hg, diastolic blood pressure ≥ 90 mm Hg, or both self-reported diagnosis of hypertension and use of any antihypertensive medication.46 Diabetes was defined as fasting plasma glucose ≥ 126 mg/dL or self-reported use of a diabetes medication. Current smoker status (yes/no) and frequency of alcohol consumption at Exam 5 were self-reported. Medication use was assessed in-home using a standard medication inventory approach.47 Cardiovascular disease was defined as myocardial infarction, resuscitated cardiac arrest, and stroke and was adjudicated from medical records by study physicians.48
Statistical Analysis
We computed means or proportions of descriptive characteristics for the overall sample and by depression status. For the primary analyses, we used relative risk regression (a generalized linear model (GLM) with log link, Gaussian error structure, and robust standard error estimates)49 to compute the PR of depression associated with each sleep measure. Prior to fitting models, we used generalized additive models (GAM) to test potential nonlinearity of the association of sleep measures with depression. We found no evidence of appreciable non-linearity, except for sleep duration and % time in REM, which were categorized for analyses. Sleep duration was categorized as < 6 h, 6–9 h, and > 9 h based on previous literature37 and % time in REM was categorized as < 10, 10–24.9, and > 24.9 based on visual inspection of the GAM plot. All other sleep measures were analyzed as continuous terms. We fit a series of sequential models. Model 1 adjusted for MESA field site and age, per 10-y increase. Model 2 further adjusted for race/ethnicity and sex. Model 3 additionally adjusted for education (high school or less, some college or technical school, graduate or professional school) and income (< $25,000, $25,000–$49,999, $50,000–$74,999, > $74,999). Model 4 included a final adjustment for body mass index, hypertension, diabetes mellitus, and current smoker status. For the exploratory analyses, we evaluated whether the association of sleep disturbances with depression was modified by race/ ethnicity, socioeconomic status, or sex using interaction terms (e.g., insomnia*sex), which were entered in separate models. If significant differences were present in these exploratory analyses, stratified results are reported. Because of sparse cells in the education and income categories, we collapsed education and income into two categories for all of the interaction analyses (high school or less versus more than a high school diploma; < $25,000 versus $25,000 or more). Also given the sparse cells for the long sleep duration group, we compared only those with short sleep versus average sleep duration in interaction analyses. To determine the robustness of our findings, we conducted five sensitivity analyses. First, we calculated a modified total depression score that subtracted out the sleep question item. We then fit models with CES-D score as a continuous term, comparing sleep measure coefficients from the model with the original depression score to coefficients with the modified depression score. Second, we re-ran our models (depression as a binary outcome) excluding participants taking anti-depressant medication with somnolent effects (tricyclic antidepressants [TCAs] and trazodone). Third, we re-ran our final models using an alternative definition of the depression, CES-D score of ≥ 16 or use of antidepressants. Fourth, we fit models with an additional adjustment for alcohol consumption. Fifth, we re-ran our final models with an adjustment for prevalent cardiovascular disease. Statistical analyses were performed using Stata (StataCorp. 2011. Stata Statistical Software: Release 12.1. College Station, TX, USA: StataCorp LP.). The significance levels were set at P < 0.05 for two-sided analyses.
RESULTS
Table 1 presents the distribution of characteristics of the total sample and by depression status. Of the 1,784 participants, 36.8% were non-Hispanic White, 28.0% were African American, 23.7% were Hispanics, and 11.5% were Chinese (Table 1). Prevalence of CVD (myocardial infarction, resuscitated cardiac arrest, and stroke,) in this sample was low at 3.3%. Overall, 259 participants (14.5%) had scores consistent with depression. Those with depression were younger, and more likely to be Hispanic than those without depression. Compared to individuals without depression, more individuals with depression had a high school education or less, a total gross family income of less than $25,000, diabetes, and were current smokers. The distribution of sex and mean body mass index were similar in both depression status groups.
Table 1.
Characteristics of participants by depression status in the Multi-Ethnic Study of Atherosclerosis sleep ancillary study (MESA Exam 5; 2010–2013) (n = 1,784).
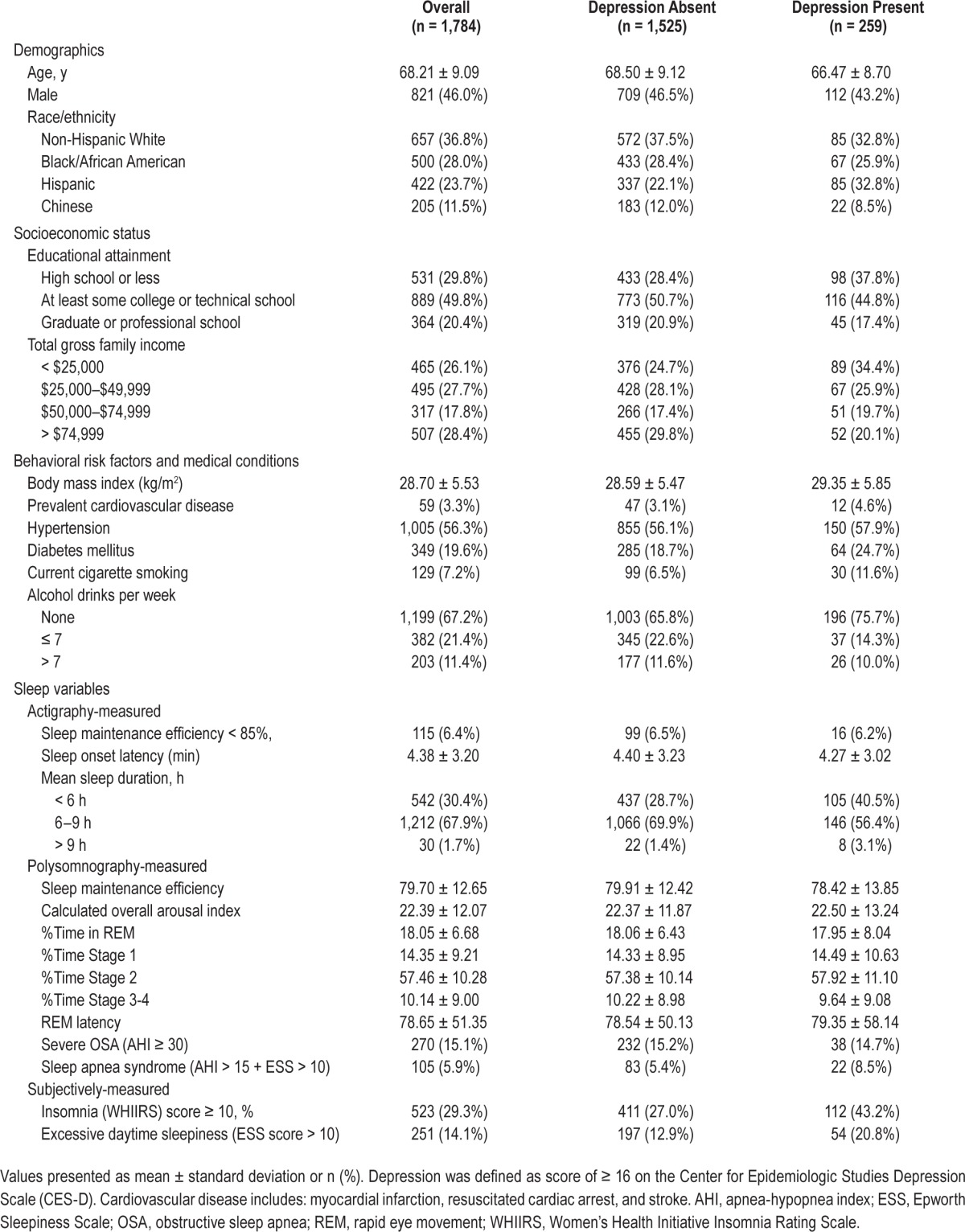
Sleep disturbances were common, but varied by depression status group. Overall, 29.3% had insomnia (WHIIRS ≥ 10), 14.1% had EDS, 15.1% had severe OSA (AHI ≥ 30), 5.9% had sleep apnea syndrome (AHI > 15 + EDS), 30.4% had short sleep duration (< 6 h), and 1.7% had long sleep duration (> 9 h). Actigraphy-assessed mean short sleep duration, long sleep duration, and subjectively measured insomnia and EDS were more common among those with depression. Although fewer adults with depression had severe OSA (AHI ≥ 30) than those without depression, more adults with depression met the criteria for sleep apnea syndrome (AHI > 15 + EDS) compared to those without depression. Mean measures of sleep continuity and sleep stage distributions were similar across depression status groups. Overall summary statistics for actigraphy-assessed and PSG-assessed wake after sleep onset, sleep onset latency, time in bed, total sleep time, and sleep efficiency for the total sample and by depression status are also reported in Table S1 (supplemental material).
Sleep Duration, Sleep Continuity, and Depression
Those with actigraphy-assessed short sleep duration (< 6 h) (PR = 1.53, 95% confidence interval [CI]: 1.20, 1.94), and those with long sleep duration (> 9 h) (PR = 2.45; 95% CI: 1.25, 4.79) had increased prevalence of depression relative to those with average sleep duration (6–9 h) in site- and age-adjusted models (Table 2). The higher PRs associated with long sleep duration were attenuated after adjustment for the full set of covariates, but the estimate associated with short sleep duration remained statistically significant (PR = 1.47; 95% CI: 1.11, 1.94) (Table 2).
Table 2.
Association of sleep duration and sleep continuity with depression in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study (MESA Exam 5; 2010–2013) (n = 1,784).

With regard to measures of sleep continuity (Table 2), PSG-assessed low sleep maintenance efficiency was associated with a 47% increase in the PRs of depression in site- and age-adjusted models (PR = 1.47; 95% CI: 1.08, 2.01). The PRs did not change appreciably with final adjustment (PR = 1.50; 95% CI: 1.06, 2.13). In contrast, actigraphy-assessed low sleep maintenance efficiency, actigraphy-assessed sleep onset latency (Table 2), and PSG-calculated overall arousal index (Table 2) were not associated with depression.
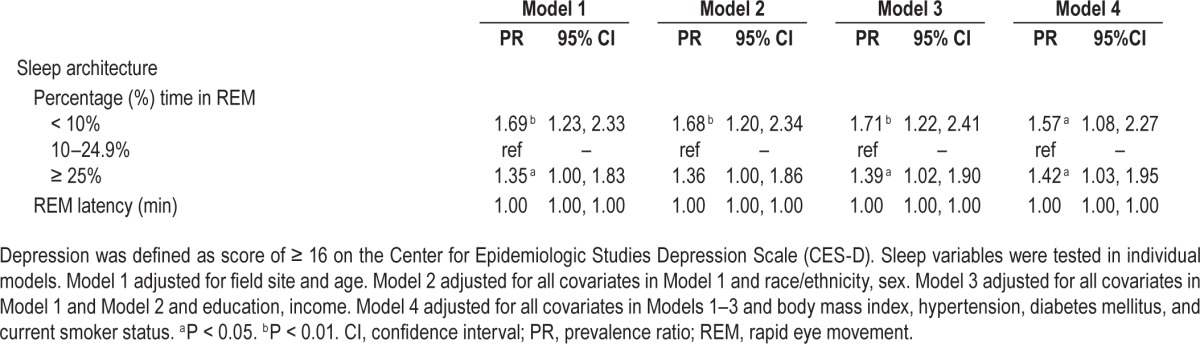
Sleep Architecture and Depression
Alterations in sleep architecture were significantly associated with depression. Those who spent less than 10% in REM sleep had increased prevalence of depression (PR = 1.69, 95% CI: 1.23, 2.33) when compared to those with an intermediate proportion of REM sleep duration (10–24.9%) in site- and age-adjusted models (Table 3). The adverse association of low proportion of REM sleep with depression remained significant in models that further adjusted for demographics, education, and income (PR = 1.71, 95% CI: 1.22, 2.41), as well as behavioral risk factors and medical conditions (PR = 1.57, 95% CI: 1.08, 2.27). Similarly, those with a high proportion of REM sleep (25% or more) had an increased prevalence of depression (PR = 1.42, 95% CI: 1.03, 1.95) relative to those with average proportion of REM sleep in fully adjusted models. REM latency was not associated with depression (Table 3).
Table 3.
Association of polysomnography-measured sleep architecture with depression in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study (MESA Exam 5; 2010–2013) (n = 1,784).
Insomnia, Sleepiness, OSA, Sleep Apnea Syndrome, and Depression
Insomnia (WHIIRS ≥ 10) was adversely associated with depression, such that those with insomnia had higher prevalence of depression relative to those without insomnia (PR = 1.82; 95% CI: 1.44, 2.29) in site- and age-adjusted models (Table 4). The PRs associated with insomnia did not change appreciably with further adjustment for sex, education, income, behavioral risk factors, and medical conditions (PR = 1.83; 95% CI: 1.39, 2.40).
Table 4.
Association of sleep quality, obstructive sleep apnea, and sleep apnea syndrome with depression in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study (MESA Exam 5; 2010–2013) (n = 1,784).

EDS was also adversely associated with depression. Those with EDS had a 62% increased prevalence of depression (PR = 1.62; 95% CI: 1.23, 2.13) relative to those without EDS. The magnitude of the PR for EDS did not change appreciably with additional covariates, and remained significantly associated with depression in the fully adjusted model (PR = 1.61; 95% CI: 1.19, 2.18) (Table 4). Importantly, severe OSA (AHI ≥ 30) was not associated with depression in any of the regression models (fully adjusted model PR = 0.88, 95% CI: 0.60, 1.30); AHI > 15 was also not associated with depression in any of the regression models (fully adjusted model PR = 0.92; 95% CI: 0.70, 1.22) (Table 4). However, sleep apnea syndrome (AHI > 15 + EDS) was associated with depression in ageand-site adjusted models (PR = 1.61, 95% CI: 1.05, 2.46) and remained significant with additional adjustment for sociodemographics and in the fully-adjusted model (PR = 1.55, 95% CI: 1.01, 2.39).
Exploratory Analyses of Sociodemographic Effect Modifiers
The exploratory analyses indicate that educational attainment modified the association of mean sleep duration and depression (P for interaction = 0.05). Among those with more than a high school education, short sleep duration relative to average sleep duration was associated with a higher prevalence of depression (PR = 1.61; 95% CI = 1.09, 2.36). Short-sleep duration was not associated with depression among those with less than a high school education (PR = 1.11; 95% CI = 0.66, 2.36). Sex modified the association of insomnia on depression (P for interaction = 0.06). Sex-stratified models indicated that among men, insomnia was associated with a markedly high PR for depression (PR = 2.51; 95% CI: 1.68, 3.75). In contrast, the PR for depression associated with insomnia was weaker among women (PR = 1.40; 95% CI: 0.99, 1.99), although the PR was in the expected direction. None of the other sleep disturbance by sociodemographic factors (education, income, or sex) interactions tested approached statistical significance (P for interactions > 0.05) and thus are not reported.
Sensitivity Analyses
Estimates for sleep measures from the sensitivity analyses using the modified CES-D score were modestly attenuated compared to the model using the original CES-D score, but remained statistically significant (Table S2, supplemental material). Second, when we excluded from the analysis those taking antidepressant medications with somnolent effects (tri-cyclic antidepressants [TCAs] and trazodone) the PRs for depression associated with each sleep disturbance did not change appreciably in this restricted sample (Table S3, supplemental material). Third, when we used an alternative definition of depression (CES ≥ 16 or antidepressant medication use), the PRs for depression associated with each sleep disturbance also did not change appreciably using this alternative definition, although the association of sleep efficiency (PSG) with depression was attenuated (Table S4, supplemental material). Further adjustment for alcohol consumption did not change our results appreciably, although the association of sleep architecture with depression was attenuated. Lastly, final adjustment for prevalent CVD at Exam 5 did not change our results.
DISCUSSION
Overall, our results show that sleep disturbances—alterations in sleep duration, continuity, quality, and architecture— were more common among those with depression than those without depression in a multiethnic community-based cohort of middle-aged and older adults. Of the objective measures, actigraphy-assessed short sleep duration and PSG-assessed low and high proportion of nightly REM sleep, were most consistently and strongly associated with depression. Of the subjective measures, insomnia and EDS were associated most strongly with depression. Of the measures of sleep continuity, only PSG-assessed low sleep maintenance efficiency was associated with increased relative risk of depression. Although severe OSA (AHI ≥ 30) was not associated with depression (even when we used alternative cutoffs for OSA [AHI > 15], sleep apnea syndrome (AHI > 15 + EDS) was associated with depression, likely reflecting the influence of sleepiness in this association. In exploratory analyses, sex marginally modified the association of insomnia with depression, and educational attainment modified the association of sleep duration with depression; race/ethnicity did not modify the association of sleep disturbances with depression.
Consistent with prior research,1,50–52 we found evidence suggestive of a U-shaped relationship between actigraphy-assessed sleep duration and depression; the age-adjusted prevalence of depression among those with actigraphy-assessed short sleep duration (< 6 h), and long sleep duration (> 9 h) was 53% and 2.45-fold higher, respectively, in comparison to their average sleep duration counterparts. However, the association of long sleep duration with depression became nonsignificant in the final model, possibly as a result of low statistical power due to the small number of participants in the > 9 h category (n = 30), or due to the potentially large effects of confounders. Supplemental analyses using an alternative cutoff for long sleep duration (> 8 h), also did not observe a statistically significant association between long sleep duration and depression (results not shown). Importantly, in contrast to our hypothesis, we found that those with more than a high school education appear to harbor a stronger association with depression when experiencing short sleep versus average sleep, whereas those with a high school education or less do not exhibit the same association with depression in the context of short sleep. Short sleep duration may independently confer excess risks for depression and greater education might be a marker for stresses associated with occupational stress that in turn would magnify the effect of short sleep on depression. Indeed, prior research shows that increasingly professional roles are a consistent predictor of short sleep duration.53 Future research should advance our understanding of the contexts under which insufficient sleep occurs and its association to depression. Public health interventions that focus on the screening for short sleep duration or that target sleep extension, particularly among those with greater years of education, may be particularly important for identifying those who may be at greatest risk of depression or potentially for lowering depression prevalence among this segment of the population.
Although most prior research has found evidence of an increased proportion of REM sleep among people with depression,6,54 we found that both a low proportion (less than 10%) and a high proportion of nightly REM sleep (25% or more) relative to an average proportion (10% to 24.9%) of nightly REM sleep was associated with an increased prevalence of depression among older adults. These findings converge with prior literature showing an adverse association between extreme values of nightly REM sleep and mortality,55 and short proportion of REM sleep and depression among older men.56 Importantly, REM latency, was not associated with depression in this sample, although prior research documents shorter REM latency among those with depression.54 There are a number of psychobiological mechanisms potentially linking short and prolonged REM sleep with depression. Dysregulated cholinergic and noradrenergic/serotonergic physiological systems are often observed among those with affective disorders, and also influence REM and non-REM sleep distributions,1,6,52,54 and thus abnormalities in REM sleep may reflect cholinergic hypersensitivity that underlies both depression and increased REM sleep.6 A causal relationship between REM sleep and mood is supported by the REM-reducing effects of antidepressant medications as well as the role of REM sleep in modulating emotional regulation. Notably, the association of proportion REM sleep and depression remained even in sensitivity analyses excluding those taking antidepressant medications with somnolent effects. The distribution of extreme values of REM sleep proportion and its association to depression observed in this sample might reflect these varied influences, as well as reflect the complex interactions between age-related changes in sleep architecture and depression risk among older adults.52 Prior EEG studies of sleep parameters and depression have often included younger participants54; thus, how REM disruptions are related to depression among aging older adults is largely unknown. Additionally, future research is needed to understand how age-related changes in REM sleep interplay with depression risk and cognitive decline, as REM sleep is implicated in both depression and cognitive dysfunction in older adults.57–59
In line with our hypotheses and prior research,2,60–62 insomnia symptoms and EDS were both common in this sample and strongly linked to depression even after adjustment for known confounders, including body mass index. However, contrary to our initial hypothesis, our exploratory analyses suggested that the association of insomnia with depression was stronger among men compared to women. These sex-specific parameter estimates remained unchanged even in secondary analyses adjusting for OSA. Because female sex is a predis-posing factor for depression, other factors such as insomnia might exert less of an influence on depression risk among women. Further, although prior research from single studies has found a consistent association of female sex with both insomnia and depression in middle-aged adults, the sample composition in most of these single studies differs markedly from the sample composition of the MESA Sleep cohort. In particular, our study participants were older and composed of roughly equal numbers of community-dwelling men and women from diverse multiethnic backgrounds, whereas data from most prior research have been drawn from younger, predominantly female, and predominantly non-Hispanic White clinical samples. As such, our findings may reflect differences in sample composition. Importantly, the recent meta-analysis2 on the prospective association of insomnia and depression did not explore sex-specific effect modification because of reporting norms, specifically a tendency in most studies to report summarized coefficients instead of sex-specific coefficients. Thus, this manuscript contributes toward an understanding of the gendered association of sleep parameters and mental health. These results suggest that public health campaigns that target screening and/or treatment of insomnia symptoms particularly among middle-aged and older men may be helpful in reducing depressive symptoms in this at-risk and understudied population. Future research should seek to understand further the prospective association of insomnia and depression particularly among middle-aged and older men.
Notably, we did not find a significant association between AHI elevations and depression prevalence. It is increasingly recognized that there are substantial individual differences in the association of elevations in AHI and cognitive and neurobehavioral effects. Thus, the lack of an observation between AHI cutoffs and depression may reflect the wide variability in the sequela of OSA, particularly among middle-aged and older adults. Future research should explore age-dependent and dose-response relationships between OSA severity cutoffs and depression. Further, although OSA (defined as AHI ≥ 30 or AHI > 15) was not associated with depression, sleep apnea syndrome (AHI > 15 + EDS) was adversely associated with depression; it is possible that sleepiness might be driving this association. Indeed, a growing number of cross-sectional and prospective studies indicate a strong and consistent relationship between depression and incident EDS, and vice versa. More research is needed to understand the independent and combined effect of sleepiness and OSA on depression and its temporal associations.
Exploratory analyses did not indicate that race/ethnicity modified the association of sleep disturbances with depression. Although the dataset included sizeable samples of Hispanics, Chinese, African Americans, and non-Hispanic Whites, we ultimately had limited statistical power to detect significant race/ ethnicity and sleep disturbances interactions as we often had small cells. Additionally, it is possible that a fourth variable acting on the same causal pathway between sleep disturbances and depression may need to be present in order to observe race/ ethnicity effect modification. For example, racial/ethnic differences in the association of sleep with depression may only appear in the context of high neighborhood disorder. Alternatively, race/ethnicity may not modify the sleep and depression association. Future prospective research with larger population-based samples adequately powered to explore two-way and three-way interactions would help clarify these unanswered questions.
Our study is not without its limitations. First, this was a cross-sectional study, and thus we were not able to assess causality and directionality. It is possible that depression preceded the onset of sleep disturbances and vice versa; additionally, the relationship between sleep disturbances and depression may also be bidirectional.5 Future research efforts should use prospective cohort designs to determine whether sleep disturbances are early prodromal or prognostic indicators of depression and more confidently establish temporality. Additionally, further understanding the psychobiological mechanisms linking these different dimensions of sleep to depression, or depression to sleep, are important to explore.63 Second, although we used a well-validated self-report scale to assess depressive symptoms, it is possible that depression classifications might differ with use of a clinical psychiatric interview. Future research should replicate these findings using larger multiethnic samples that are adequately powered to detect significant interactions and with multimethod assessments of depression as well as related psychosocial factors known to affect sleep and depression (e.g., discrimination, occupational stress). Third, though we had specific hypotheses about the association of sleep disturbances and depression and potential sociodemographic effect modifiers, this resulted in multiple comparisons, and readers should interpret these findings with this limitation in mind. Fourth, as is common in most large epidemiological observational studies, PSG was conducted over 1 night and thus may not be reflective of typical sleep and further subject to “first-night” effects.
CONCLUSIONS
In one of the first empirical reports to leverage both the objective and subjective measurement of sleep disturbances in a large multiethnic cohort, our results suggest that actigraphyand PSG-measured sleep disturbances are common among middle-aged and older adults with depression and associated with increased prevalence of depression. Indeed, short sleep duration, a low as well as a high proportion of REM sleep, insomnia, EDS, and sleep apnea syndrome were associated with a 47% to 83% increased prevalence of depression even after adjustment for known confounders. Public health interventions that target early detection and treatment of these sleep disturbances may lower depression prevalence, though future research is needed to understand why specific dimensions of sleep, namely, quality, timing, duration, and continuity, are related to depression and the time course involved in these relations. Sex and education may be significant modifiers of the effect of insomnia on depression, and short sleep duration on depression, respectively. Particularly, our results from the exploratory analyses suggest that among middle-aged and older individuals, men with insomnia, and those with more than a high school education and short sleep duration, may bear a disproportionate burden of depression. Future research is needed that replicates the findings from the exploratory analyses on sociodemographic effect modifiers (race/ethnicity, education, sex), and that subsequently, determines whether interventions that target early screening or detection of insomnia and short sleep duration in these specific groups would yield substantial public health benefit. Importantly, our results also call attention to the need for more research on the complex interactions of age-related changes in sleep characteristics and depression prevalence among middle-aged and older adults and how sociodemographic factors such as education and sex pattern such associations.
DISCLOSURE STATEMENT
This was not an industry supported study. C. Alcántara is supported by K23 HL125748-01 from the National Heart, Lung, and Blood Institute of the National Institutes of Health. S Redline and MESA-Sleep is supported by NIH 1R01HL083075. K.W. Davidson is supported by National Institute of Health grants HL114924, HL115941, HL088117 and HL084034, and a grant from New York Presbyterian Hospital. C. Jackson is supported by Harvard Catalyst (1UL1 TR001102-01). J.A. Delaney is supported by R01 HL 103729-01A1 from the National Heart, Lung, and Blood Institute. MESA is supported by contracts N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, and N01-HC-95169 from the National Heart, Lung, and Blood Institute. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66:1254–69. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- 2.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 3.Riemann D, Voderholzer U. Primary insomnia: a risk factor to develop depression? J Affect Disord. 2003;76:255–9. doi: 10.1016/s0165-0327(02)00072-1. [DOI] [PubMed] [Google Scholar]
- 4.Cheng P, D Casement M, Chen CF, Hoffmann RF, Armitage R, Deldin PJ. Sleep-disordered breathing in major depressive disorder. J Sleep Res. 2013;22:459–62. doi: 10.1111/jsr.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36:1059–68. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palagini L, Baglioni C, Ciapparelli A, Gemignani A, Riemann D. Rem sleep dysregulation in depression: state of the art. Sleep Med Rev. 2013;17:377–90. doi: 10.1016/j.smrv.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28:1405–11. doi: 10.1093/sleep/28.11.1405. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez-Mendoza J, Vgontzas AN, Kritikou I, Calhoun SL, Liao D, Bixler EO. Natural history of excessive daytime sleepiness: role of obesity, weight loss, depression, and sleep propensity. Sleep. 2015;38:351–60. doi: 10.5665/sleep.4488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mendlewicz J. Sleep disturbances: core symptoms of major depressive disorder rather than associated or comorbid disorders. World J Biol Psychiatry. 2009;10:269–75. doi: 10.3109/15622970802503086. [DOI] [PubMed] [Google Scholar]
- 10.Armitage R, Trivedi M, Hoffmann R, Rush AJ. Relationship between objective and subjective sleep measures in depressed patients and healthy controls. Depress Anxiety. 1997;5:97–102. doi: 10.1002/(sici)1520-6394(1997)5:2<97::aid-da6>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 11.Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2004;164:406–18. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- 12.Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the united states. Psychol Med. 2005;35:317–27. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the national comorbidity survey replication (ncs-r) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 14.Fiorentino L, Marler M, Stepnowsky C, Johnson S, Ancoli-Israel S. Sleep in older african americans and caucasians at risk for sleep-disordered breathing. Behav Sleep Med. 2006;4:164–78. doi: 10.1207/s15402010bsm0403_3. [DOI] [PubMed] [Google Scholar]
- 15.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- 16.Mezick EJ, Matthews KA, Hall M, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosom Med. 2008;70:410–6. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 18.Chen X, Redline S, Shields AE, Williams DR, Williams MA. Associations of allostatic load with sleep apnea, insomnia, short sleep duration, and other sleep disturbances: findings from the National Health and Nutrition Examination Survey 2005 to 2008. Ann Epidemiol. 2014;24:612–9. doi: 10.1016/j.annepidem.2014.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kingsbury JH, Buxton OM, Emmons KM. Sleep and its relationship to racial and ethnic disparities in cardiovascular disease. Curr Cardiovasc Risk Rep. 2013;7:387–94. doi: 10.1007/s12170-013-0330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Redline S, Sotres-Alvarez D, Loredo J, et al. Sleep-disordered breathing in hispanic/latino individuals of diverse backgrounds. The hispanic community health study/study of latinos. Am J Respir Crit Care Med. 2014;189:335–44. doi: 10.1164/rccm.201309-1735OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Voderholzer U, Al-Shajlawi A, Weske G, Feige B, Riemann D. Are there gender differences in objective and subjective sleep measures? A study of insomniacs and healthy controls. Depress Anxiety. 2003;17:162–72. doi: 10.1002/da.10101. [DOI] [PubMed] [Google Scholar]
- 22.Miranda J, McGuire TG, Williams DR, Wang P. Mental health in the context of health disparities. Am J Psychiatry. 2008;165:1102–8. doi: 10.1176/appi.ajp.2008.08030333. [DOI] [PubMed] [Google Scholar]
- 23.Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305–15. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 24.Gonzalez HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the united states. J Psychiatr Res. 2010;44:1043–51. doi: 10.1016/j.jpsychires.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diez Roux AV. Conceptual approaches to the study of health disparities. Annu Rev Public Health. 2012;33:41–58. doi: 10.1146/annurev-publhealth-031811-124534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gallo LC, Bogart LM, Vranceanu A-M, Matthews KA. Socioeconomic status, resources, psychological experiences, and emotional responses: a test of the reserve capacity model. J Personality Social Psychol. 2005;88:386–99. doi: 10.1037/0022-3514.88.2.386. [DOI] [PubMed] [Google Scholar]
- 27.Myers HF. Ethnicity- and socio-economic status-related stresses in context: an integrative review and conceptual model. J Behav Med. 2009;32:9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- 28.Boss EF, Smith DF, Ishman SL. Racial/ethnic and socioeconomic disparities in the diagnosis and treatment of sleep-disordered breathing in children. Int J Pediatr Otorhinolaryngol. 2011;75:299–307. doi: 10.1016/j.ijporl.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Desantis AS, Diez Roux AV, Moore K, Baron KG, Mujahid MS, Nieto FJ. Associations of neighborhood characteristics with sleep timing and quality: the Multi-Ethnic Study of Atherosclerosis. Sleep. 2013;36:1543–51. doi: 10.5665/sleep.3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pabayo R, Molnar BE, Street N, Kawachi I. The relationship between social fragmentation and sleep among adolescents living in Boston, Massachusetts. J Public Health (Oxf) 2014;36:587–98. doi: 10.1093/pubmed/fdu001. [DOI] [PubMed] [Google Scholar]
- 31.Slopen N, Williams DR. Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep. 2014;37:147–56. doi: 10.5665/sleep.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lewis TT, Troxel WM, Kravitz HM, Bromberger JT, Matthews KA, Hall MH. Chronic exposure to everyday discrimination and sleep in a multiethnic sample of middle-aged women. Health Psychol. 2013;32:810–9. doi: 10.1037/a0029938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 34.Chen X, Wang R, Zee P, et al. Racial/ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA) Sleep. 2015;38:877–88. doi: 10.5665/sleep.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morgenthaler T, Alessi C, Friedman L, et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. 2007;30:519–29. doi: 10.1093/sleep/30.4.519. [DOI] [PubMed] [Google Scholar]
- 36.Oakley NR. Bend, OR: Mini Mitter Co., Inc, Cambridge Neurotechnology; 1997. Validation with polysomnography of the Sleepwatch sleep/wake scoring algorithm used by the Actiwatch activity monitoring system. [Google Scholar]
- 37.Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010;24:731–43. doi: 10.1016/j.beem.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fung MM, Peters K, Ancoli-Israel S, Redline S, Stone KL, Barrett-Connor E. Total sleep time and other sleep characteristics measured by actigraphy do not predict incident hypertension in a cohort of community-dwelling older men. J Clin Sleep Med. 2013;9:585–91. doi: 10.5664/jcsm.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Redline S, Budhiraja R, Kapur V, et al. The scoring of respiratory events in sleep: reliability and validity. J Clin Sleep Med. 2007;3:169–200. [PubMed] [Google Scholar]
- 40.Silber MH, Ancoli-Israel S, Bonnet MH, et al. The visual scoring of sleep in adults. J Clin Sleep Med. 2007;3:121–31. [PubMed] [Google Scholar]
- 41.Levine DW, Lewis MA, Bowen DJ, Kripke DF, Kaplan RM, Naughton MJ, Shumaker SA. Reliability and validity of women's health initiative insomnia rating scale. Psychol Assess. 2003;15:137–48. doi: 10.1037/1040-3590.15.2.137. [DOI] [PubMed] [Google Scholar]
- 42.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 43.Radloff L. Center for epidemiological studies depression scale. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 44.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the ces-d (center for epidemiological studies depression) depression symptoms index. J Aging Health. 1993;5:179–93. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 45.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item center for epidemiological studies depression scale (ces-d) Arch Intern Med. 1999;159:1701–4. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 46.The sixth report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–46. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 47.Psaty BM, Lee M, Savage PJ, Rutan GH, German PS, Lyles M. Assessing the use of medications in the elderly: methods and initial experience in the cardiovascular health study. The cardiovascular health study collaborative research group. J Clin Epidemiol. 1992;45:683–92. doi: 10.1016/0895-4356(92)90143-b. [DOI] [PubMed] [Google Scholar]
- 48.Bluemke DA, Kronmal RA, Lima JA, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52:2148–55. doi: 10.1016/j.jacc.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lumley T, Kronmal R, Ma S. Relative risk regression in medical research: models, contrasts, estimators, and algorithms. UW Biostatistics Working Paper Series. Working Paper 293. 2006 [Google Scholar]
- 50.van Mill JG, Vogelzangs N, van Someren EJ, Hoogendijk WJ, Penninx BW. Sleep duration, but not insomnia, predicts the 2-year course of depressive and anxiety disorders. J Clin Psychiatry. 2014;75:119–26. doi: 10.4088/JCP.12m08047. [DOI] [PubMed] [Google Scholar]
- 51.Swinkels CM, Ulmer CS, Beckham JC, Buse N, Calhoun PS. The association of sleep duration, mental health, and health risk behaviors among u.S. Afghanistan/iraq era veterans. Sleep. 2013;36:1019–25. doi: 10.5665/sleep.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders. A meta-analysis. Arch Gen Psychiatry. 1992;49:651–68. doi: 10.1001/archpsyc.1992.01820080059010. discussion 669-70. [DOI] [PubMed] [Google Scholar]
- 53.Jackson CL, Redline S, Kawachi I, Williams MA, Hu FB. Racial disparities in short sleep duration by occupation and industry. Am J Epidemiol. 2013;178:1442–51. doi: 10.1093/aje/kwt159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pillai V, Kalmbach DA, Ciesla JA. A meta-analysis of electroencephalographic sleep in depression: evidence for genetic biomarkers. Biol Psychiatry. 2011;70:912–9. doi: 10.1016/j.biopsych.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 55.Dew MA, Hoch CC, Buysse DJ, et al. Healthy older adults' sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65:63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- 56.Smagula SF, Reynolds CF, 3rd, Ancoli-Israel S, et al. Sleep architecture and mental health among community-dwelling older men. J Gerontol B Psychol Sci Soc Sci. 2015;70:673–81. doi: 10.1093/geronb/gbt125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half-century of multidisciplinary research. Perspect Psychol Sci. 2015;10:97–137. doi: 10.1177/1745691614556680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Song Y, Blackwell T, Yaffe K, Ancoli-Israel S, Redline S, Stone KL. Relationships between sleep stages and changes in cognitive function in older men: the MrOS sleep study. Sleep. 2015;38:411–21. doi: 10.5665/sleep.4500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Scullin MK, Bliwise DL. Is cognitive aging associated with levels of rem sleep or slow wave sleep? Sleep. 2015;38:335–6. doi: 10.5665/sleep.4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Basta M, Lin HM, Pejovic S, Sarrigiannidis A, Bixler E, Vgontzas AN. Lack of regular exercise, depression, and degree of apnea are predictors of excessive daytime sleepiness in patients with sleep apnea: sex differences. J Clin Sleep Med. 2008;4:19–25. [PMC free article] [PubMed] [Google Scholar]
- 61.Troxel WM, Kupfer DJ, Reynolds CF, 3rd, et al. Insomnia and objectively measured sleep disturbances predict treatment outcome in depressed patients treated with psychotherapy or psychotherapy-pharmacotherapy combinations. J Clin Psychiatry. 2012;73:478–85. doi: 10.4088/JCP.11m07184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fernandez-Mendoza J, Shea S, Vgontzas AN, Calhoun SL, Liao D, Bixler EO. Insomnia and incident depression: role of objective sleep duration and natural history. J Sleep Res. 2015;24:390–8. doi: 10.1111/jsr.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alcantara C, Davidson KW. Mental disorders and coronary heart disease risk: could the evidence elude us while we sleep? Circulation. 2014;129:139–41. doi: 10.1161/CIRCULATIONAHA.113.006515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


