Abstract
Introduction
Falls are the leading cause of unintentional injuries in the U.S.; however, national estimates for all community-dwelling adults are lacking. This study estimated the national incidence of falls and fall-related injuries among community-dwelling U.S. adults by age and gender and the trends in fall-related injuries across the adult life span.
Methods
Nationally representative data from the National Health Interview Survey (NHIS) 2008 Balance and Dizziness supplement was used to develop national estimates of falls, and pooled data from the NHIS was used to calculate estimates of fall-related injuries in the U.S. and related trends from 2004–2013. Costs of unintentional fall-related injuries were extracted from the CDC’s Web-based Injury Statistics Query and Reporting System.
Results
Twelve percent of community-dwelling U.S. adults reported falling in the previous year for a total estimate of 80 million falls at a rate of 37.2 falls per 100 person-years. On average, 9.9 million fall-related injuries occurred each year with a rate of 4.38 fall-related injuries per 100 person-years. In the previous three months, 2.0% of older adults (65+), 1.1% of middle-aged adults (45–64) and 0.7% of young adults (18–44) reported a fall-related injury. Of all fall-related injuries among community-dwelling adults, 32.3% occurred among older adults, 35.3% among middle-aged adults and 32.3% among younger adults. The age-adjusted rate of fall-related injuries increased 4% per year among older women (95% CI 1%–7%) from 2004 to 2013. Among U.S. adults, the total lifetime cost of annual unintentional fall-related injuries that resulted in a fatality, hospitalization or treatment in an emergency department was 111 billion U.S. dollars in 2010.
Conclusions
Falls and fall-related injuries represent a significant health and safety problem for adults of all ages. The findings suggest that adult fall prevention efforts should consider the entire adult lifespan to ensure a greater public health benefit.
Introduction
Advances in medicine, healthier and safer lifestyles, and technological developments have helped reduce morbidity and mortality in the U.S. and worldwide, with substantial declines in deaths due to communicable and non-communicable diseases such as cardiovascular disease and cancer, and motor vehicle traffic-related injuries.[1, 2] However, injuries due to falls, the leading cause of non-fatal injuries and the third leading cause of fatal injuries in the U.S., have been increasing in recent years.[2–7] In 2010, 37% of all medically consulted injury and poisoning episodes were due to falls.[6, 8] The Global Burden of Disease Study 2010 reported that between 1990 and 2010 Falls increased in rank from the 24th to the 15th leading cause of U.S. disability-adjusted life years (DALYs) with over a 50% increase in DALYs.[9, 10]
Primary prevention would be the most effective approach to reducing the burden of fall-related injuries. Several research studies and prevention programs have focused on fall prevention and examined falls as their main outcome of interest.[11] However, important baseline data, including a national estimate of the incidence of falls among community-dwelling U.S. adults, is lacking. Data from cohort studies on falls among older adults are cited widely.[12–14] However, data on fall incidence among young and middle-aged adults (working age adults) is rare.
In addition, despite being the leading cause of injury-related emergency department visits in nearly every adult age stratum, there remains a lack of detailed national estimates of fall-related injuries by age and gender. Using the National Health Interview Survey (NHIS), we estimated the national incidence of falls, the incidence of injuries resulting from falls, injury types, and the trend over time by age and gender among community-dwelling U.S. adults. As another measure of burden, we also report the national cost burden of fall-related injuries by age-group using the Centers for Disease Control (CDC) and Prevention’s Web-based Injury Statistics Query and Reporting System (WISQARS).
Methods
The NHIS is an in-person household survey which is the principal source of information on the health of the civilian, noninstitutionalized population of the United States.[15] For each sampled household in the NHIS, interviews are conducted with an adult resident who answers questions related to the demographic, personal and health status characteristics of each member of the household.[16–18] The NHIS also surveys one Sample Adult (18+, SA) from each household on more detailed health and lifestyle topics. This study utilized existing publically available NHIS data and was exempted from Institutional Review Board approval.
Fallers and Falls (NHIS 2008 Supplement)
In 2008, with sponsorship by the National Institute on Deafness and Other Communication Disorders (NIDCD), the SA Core of the NHIS included questions relating to balance/fall issues in adults in the previous 12 months. We defined Fallers (adults who experienced at least one fall in the previous 12 months) and Non-Fallers and the number of falls in the previous 12 months, regardless of injury, using the 2008 Balance and Dizziness supplement. Fallers and number of falls were determined by following questions:
“During the past 12 months, have you fallen at least once a month on average?”
“During the past 12 months, how many times have you fallen?”
SA who responded “yes” to the first question (During the past 12 months, have you fallen at least once a month on average?) were designated Fallers and their number of falls in the past 12 months was set to 12, and they were not asked the second question.
SA who responded “no” to the first question were then asked the second question (During the past 12 months, how many times have you fallen?). SA responding “0” to the second question were designated as Non-Fallers; and SA responding “1 time,” “2 times,” “3–4 times,” “5–7 times,” and “8 or more times” to the second question were designated as Fallers and the number of falls in the past 12 months were quantified as 1, 2, 3.5, 6, and 10, respectively, to calculate the total number of falls and the rate of falls per 100 persons.
In 2008, out of 20,752 sampled adults in the NHIS, 2,549 reported a fall in the previous year. The response rate in 2008 was 63%.
Persons Injured from a Fall-Related Injury Episode and Total Fall-Related Injury Episodes (NHIS Annual Survey 2004–2013)
The NHIS collects information on medically consulted injury or poisoning episodes in the 3 months prior to the interview. Episodes are coded using the Ninth Revision of the International Classification of Disease external cause codes (ICD-9-CM). Persons experiencing a fall-related injury episode and the number of fall-related injury episodes between 2004 and 2013 were identified using ICD-9-CM codes: E880 -E888, “Accidental Falls” and ICD-9-CM codes 800–999, “Injury and Poisoning” were used to identify injury types. All analyses were performed using the Sample Adult subset to avoid proxy responses.
Over the study period (2004–2013), out of 289,187 sampled adults in the NHIS, 3,408 reported a fall-related injury in the previous three months. The average response rate was 66% during this period.
Cost of Fall-Related Injuries
Costs of unintentional fatal and non-fatal fall-related injuries were extracted for the year 2010 from the CDC’s Web-based Injury Statistics Query and Reporting System (WISQARS).[19] The estimated cost is based on two primary components: 1) U.S. national frequency of injury fatality, hospitalization, and emergency department visits for the year 2010, and 2) unit (per case) lifetime medical and work loss cost estimates expressed in year 2010 U.S. prices. The methodology used to develop these unit cost estimates is documented in the Pacific Institute for Research and Evaluation methods report and by Finkelstein et al.[20] A detailed description of the calculations used to estimate total and average costs associated with injury-related deaths, hospitalizations, and emergency department visits can be found at http://www.cdc.gov/injury/wisqars/cost_help/calculations_toc.html. The total lifetime costs of unintentional fall-related injuries that resulted in a fatality, hospitalization or treatment in an emergency department in each age group were divided by the total population in the age group to calculate lifetime costs of fall-related injuries per person.
Data Analysis
Using sample weights available in the NHIS data and the PROC SURVEYMEANS procedure in SAS 9.4, we estimated: 1) the number and proportion of adults (18+ years of age) who reported a fall in the past 12 months, 2) the number of falls experienced by adults in the past 12 months and the rate of falls per 100 person-years, 3), the number and proportion of adults 18+ reporting a fall-related injury in previous 3 months, and 4) the number of fall-related injuries to adults 18+ in the previous three months and the rate of fall-related injuries per 100 person-years. We annualized the estimates obtained from data pooled over multiple years (2004–2013). We examined the trend in the rate of fall-related injuries from 2004 to 2013 for 6 age-gender groups (18–44, 45–64, 65+; male and female). Poisson generalized linear models which accounted for sampling weight and clustering were used to examine the association between survey year and the rate of fall-related injuries in each age-gender group. The models were adjusted for age to account for change in average age by survey year in each age-gender group. We also estimated the number and proportion of injury types in these six age-gender groups.
Results
Fallers and Falls
Based upon the data from the NHIS 2008 supplement, 11.9% of community-dwelling U.S. adults fell in the previous 12 months (Table 1). The proportion of Fallers in the previous 12 months was 10.6% in the 18–44 year age-group, 11.4% in the 45–64 year age-group and 16.4% in the 65+ age-group. An estimated 80 million falls were reported in the prior year at a rate of 37.2 falls per 100 person-years. Among middle-aged (45–64 year age-group) and older adults (65+), 26.56 million (95% CI 23.01–30.12) and 17.05 million (95% CI 14.29–19.81) falls were reported, respectively.
Table 1. Number and Proportion of Community-dwelling Adults who Experienced One or More Falls in the Previous 12 Months and Number and Rate of Falls per 100 Person-Years by Age and Gender Groups.
| NHIS 2008 Fallers | NHIS 2008 Falls | ||||
|---|---|---|---|---|---|
| Gender | Age-Groups | Number of Persons (000s)a | Proportion per 100 Persons in the Previous 12 Monthsb (95% CI) | Number of Falls (000s)c | Incidence Rate per 100 Persons in the Last 12 Monthsd (95% CI) |
| Overall | 25,654 | 11.93(11.27–12.59) | 80,007 | 37.21 (34.30–40.11) | |
| Females | |||||
| Overall | 15,125 | 13.61(12.75–14.48) | 45,316 | 40.79 (36.81–44.77) | |
| 18–24 | 1,794 | 12.89 (10.89–14.89) | 6,712 | 48.25 (37.48–59.01) | |
| 25–34 | 2,253 | 11.70 (10.02–13.38) | 6,041 | 31.36 (24.55–38.17) | |
| 35–44 | 2,343 | 11.57 (9.94–13.21) | 7,683 | 37.95 (30.10–45.79) | |
| 45–54 | 2,587 | 12.15 (10.33–13.96) | 8,559 | 40.18 (31.37–49.00) | |
| 55–64 | 2,533 | 15.49 (13.31–17.66) | 7,008 | 42.84 (34.87–50.81) | |
| 65–74 | 1,553 | 15.20 (12.75–17.66) | 4,354 | 42.62 (30.89–54.36) | |
| 75+ | 2,062 | 21.02 (18.44–23.60) | 4,960 | 50.56 (40.81–60.31) | |
| Males | |||||
| Overall | 10,529 | 10.13 (9.28–10.98) | 34,691 | 33.38 (29.76–37.00) | |
| 18–24 | 1,366 | 9.86 (7.88–11.85) | 5,322 | 38.44 (28.86–48.02) | |
| 25–34 | 1,715 | 8.91 (7.36–10.47) | 5,140 | 26.71 (19.99–33.44) | |
| 35–44 | 1,803 | 9.15 (7.43–10.88) | 5,498 | 27.91 (20.38–35.44) | |
| 45–54 | 1,811 | 8.85 (7.33–10.37) | 5,831 | 28.51 (21.87–35.15) | |
| 55–64 | 1,642 | 10.75 (8.94–12.56) | 5,165 | 33.81 (25.30–42.32) | |
| 65–74 | 1,066 | 12.11 (9.92–14.31) | 3,637 | 41.32 (28.18–54.46) | |
| 75+ | 1,127 | 17.05 (14.18–19.92) | 4,097 | 61.97(49.48–74.46) | |
aEstimated frequency of people who reported falling in past 12 months (NHIS, 2008), in thousands.
bEstimated proportion (per 100 persons) of persons who fell in past 12 months (NHIS, 2008)
cEstimated frequency of falls in the past 12 months (NHIS, 2008), in thousands.
dEstimated incidence rate (per 100 persons) of falls in past 12 months (NHIS, 2008)
The proportion of male and female Fallers generally increased with each decade of age range after the 25–34 year age-group (Table 1). Similarly, the rate of falls increased with age after the 25–34 year age-group. Point estimates for fall rates were higher for women than men within each age stratum except in the 75+ age-group (95% CI overlapped for all the age-groups).
Persons Injured from a Fall and Total Fall-Related Injury Episodes
Based upon this pooled NHIS annual survey data (2004 to 2013), 1.04% of community-dwelling U.S. adults reported a fall-related injury in the previous three months, resulting in approximately 9.9 million fall-related injuries annually (Table 2). An estimated 3.2 million fall-related injuries occurred among young adults (18–44 years), 3.5 million among middle-aged adults (45–64 years) and 3.2 million in older adults (65+).
Table 2. Number and Proportion of Community-dwelling Adults who Experienced a Fall-related Injury in the Previous 3 Months, Average Number of Fall-related Injuries in One Year and the Rate of Fall-related Injuries per 100 Person-Years in the U.S. NHIS 2004–2013.
| Persons Injured Due to a Fall | Injury Episodes from a Fall | ||||
|---|---|---|---|---|---|
| Gender | Age-Groups | Number (000s)a | Proportion per 100 Persons per Three Months (95% CI))b | Number (000s)c | Incidence Rate (per 100 Persons per Year (95% CI))d |
| Overall | 2,348 | 1.04 (0.99–1.08) | 9,914 | 4.38 (4.18–4.58) | |
| Females | |||||
| Overall | 1,487 | 1.27 (1.20–1.34) | 6,278 | 5.36 (5.08–5.65) | |
| 18–24 | 111 | 0.76 (0.60–0.93) | 451 | 3.11 (2.44–3.78) | |
| 25–34 | 141 | 0.70 (0.59–0.81) | 586 | 2.90 (2.44–3.35) | |
| 35–44 | 168 | 0.80 (0.67–0.93) | 730 | 3.49 (2.87–4.11) | |
| 45–54 | 262 | 1.18 (1.05–1.31) | 1,120 | 5.05 (4.50–5.61) | |
| 55–64 | 278 | 1.57 (1.37–1.77) | 1,183 | 6.69 (5.85–7.52) | |
| 65–74 | 211 | 1.89 (1.66–2.12) | 877 | 7.85 (6.86–8.85) | |
| 75+ | 316 | 3.04 (2.72–3.37) | 1,330 | 12.8 (11.43–14.17) | |
| Males | |||||
| Overall | 861 | 0.79 (0.73–0.84) | 3,636 | 3.33 (3.10–3.57) | |
| 18–24 | 105 | 0.72 (0.54–0.90) | 430 | 2.94 (2.21–3.66) | |
| 25–34 | 108 | 0.54 (0.43–0.65) | 447 | 2.22 (1.76–2.68) | |
| 35–44 | 135 | 0.67 (0.55–0.78) | 563 | 2.77 (2.29–3.26) | |
| 45–54 | 150 | 0.71 (0.57–0.84) | 663 | 3.13 (2.50–3.76) | |
| 55–64 | 127 | 0.77 (0.64–0.90) | 533 | 3.25 (2.69–3.80) | |
| 65–74 | 95 | 0.99 (0.80–1.19) | 412 | 4.29 (3.35–5.24) | |
| 75+ | 140 | 2.04 (1.64–2.44) | 588 | 8.55 (6.88–10.23) | |
aEstimated average frequency of persons reporting a medically-consulted injury due to a fall in past 3 months (NHIS, 2004–2013), in thousands.
bEstimated average incidence rate (per 100 persons) of persons who reported an injury episode due to a fall in past 3 months (NHIS, 2004–2013)
cEstimated average number of injury episodes due to a fall reported in past 3 months, annualized to one year (NHIS, 2004–2013), in thousands.
dEstimated average incidence rate (per 100 persons) of injury episodes resulting from a fall in past 3 months, annualized to one year (NHIS, 2004–2013)
The proportion of persons injured due to a fall increased monotonically with age after the 25–34 year age-group (Table 2). In the previous three months, 2.0% of older adults, 1.1% of middle-aged adults and 0.7% of young adults reported a fall-related injury. The rate of fall-related injuries also increased with age after the 25–35 year age group, and women over 75 years of age had the highest rate of fall-related injuries.
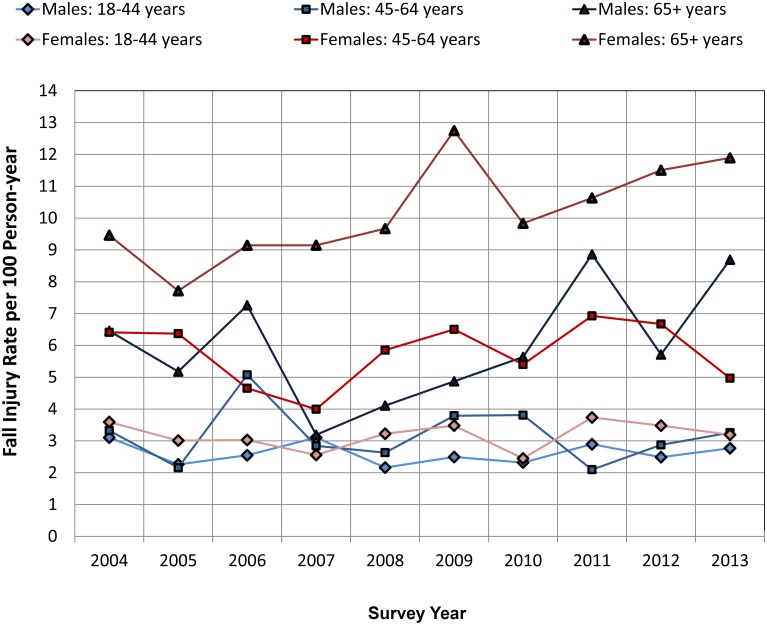
Fig 1 presents trends in the rates of fall-related injuries for community-dwelling adults from the pooled NHIS data by age-gender groups. Females and males in the 18–44 year age-groups had the lowest rate of fall-related injuries, and females over 65 years of age had the highest rate of fall-related injuries. The rates of fall-related injuries among females in the 45–64 year age-group and males over 65 years of age were very similar. Among all adults (18+), the increasing trend of the rate of fall-related injuries (after adjusting for age and gender) was 1% per year (95% CI 0%–3%, p < .10, not statistically significant at 0.05 level) over the survey years. Of the six age-gender groups, the age-adjusted rate of fall-related injuries increased 4% per year among older women (95% CI 1%–7%, p < .05) and 5% among older men (5% per year, 95% CI 0% -10%, p < .10, not statistically significant at 0.05 level) from 2004–2013.
Fig 1. Incidence Rate of Fall-related Injuries per 100 Person-year by Age-Gender Groups from 2004 to 2013 in the U.S.
Medically consulted fall-related injury episodes occurring in the previous three months among community-dwelling adults were identified in the National Health Interview Survey. We annualized the fall-related injury estimates and calculated rates of fall-related injuries per 100 Person-year by age and gender groups using population weights.
In the overall adult population, the most common fall-related injury was “Sprains And Strains Of Joints And Adjacent Muscles” (38%, Table 3). However, among older adults, “Contusion With Intact Skin Surface” was the most common injury type (31% among males 65+, and 38% among females 65+). The proportion of fall-related injury “Open Wounds” was higher among men as compared to women. In the overall community-dwelling adult population, 28% of the fall-related injuries were fractures.
Table 3. Annual Average Fall-related injurya types in thousands (000s) and their Proportionb c by Age and Gender Groups.
NHIS 2004–2013.
| Nature of Injury (ICD-9 Code) | All Persons (18+) n,(%) | Males: 18–44 n,(%) | Males: 45–64 n,(%) | Males: 65+ n,(%) | Females: 18–44 n,(%) | Females: 45–64 n,(%) | Females: 65+ n,(%) |
|---|---|---|---|---|---|---|---|
| Fractures (800–829) | 2791 (28.2) | 349 (24.3) | 363 (30.3) | 261 (26.1) | 381 (21.5) | 630 (27.4) | 807 (36.6) |
| Dislocation (830–839) | 183 (1.8) | 71 (5.0) | 15 (1.2) | 5 (0.5) | 58 (3.3) | 18 (0.8) | 16 (0.7) |
| Sprains And Strains Of Joints And Adjacent Muscles (840–848) | 3722 (37.6) | 663 (46.1) | 435 (36.3) | 278 (27.8) | 923 (52.2) | 962 (41.8) | 462 (20.9) |
| Intracranial Injury, Excluding Those With Skull Fracture (850–854) | 136 (1.4) | 17 (1.2) | 10 (0.9) | 15 (1.6) | 32 (1.8) | 36 (1.6) | 26 (1.2) |
| Open Wounds (870–897) | 1212 (12.2) | 207 (14.4) | 200 (16.7) | 208 (20.8) | 126 (7.1) | 233 (10.1) | 238 (10.8) |
| Superficial Injury (910–919) | 646 (6.5) | 75 (5.2) | 64 (5.3) | 112 (11.2) | 94 (5.3) | 133 (5.8) | 167 (7.6) |
| Contusion With Intact Skin Surface (920–924) | 2710 (27.3) | 176 (12.2) | 292 (24.4) | 306 (30.6) | 393 (22.2) | 710 (30.8) | 832 (37.7) |
| Certain Traumatic Complications And Unspecified Injuries (958–959) | 409 (4.1) | 38 (2.7) | 57 (4.8) | 55 (5.5) | 34 (1.9) | 108 (4.7) | 116 (5.3) |
| Total b d | 11809 (119.1) | 1596 (111.1) | 1436 (119.9) | 1240 (124.1) | 2041 (115.3) | 2830 (123.0) | 2664 (120.8) |
a Estimated average number of injury episodes due to a fall reported in past 3 months, annualized to one year (NHIS, 2004–2013), in thousands.
b Proportions are calculated as Number of Fall-injury events resulting in an injury type ÷ Total number of fall-related injury events. Mutliple injuries may result from a fall-injury event and thus proportions add upto more than 100%.
c Injury types with less than 1% proportion of all fall injuries are excluded from the table.
d Total excludes injury types with less than 1% proportion of all fall injuries
Lifetime Unintentional Fall-related Injury Costs (CDC’s WISQARS, 2010)
Table 4 presents average and total lifetime costs of annual unintentional fall-related injuries resulting in death, hospitalization or an emergency department visit in the U.S. by age-groups. Average cost values under the headings for Death, Hospitalization and Emergency department visits are the average lifetime cost per fall-related injury that resulted in those outcomes, respectively. Total cost values under those same headings are the total lifetime cost of all fall-related injuries that resulted in the respective outcomes. For example, the total cost of fall-related injuries that resulted in death is equal to the average lifetime cost per fall-related injury resulting in death multiplied by the total number of fall-related injuries that resulted in death (e.g. in 18–24 age group, fall-related injuries resulted in 189 deaths, 1,887,705*189 = 356,776,245). “Total Cost of Fall-related Injuries” is the sum of the total costs of fall injuries that resulted in death, hospitalization and emergency department visits. “Cost of Fall-Related Injury per Person” represents the lifetime cost of fall-related injury per person (Total cost of fall-related injury in an age group ÷ total population in the age group).
Table 4. Average and total lifetime cost (US $) of Annual Unintentional Fall-Related Injuries Resulting in Death, Hospitalization or an Emergency Department Visit in the U.S. by age-groups, 2010*.
| Death | Hospitalization | Emergency Department Visits | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age-groups | Average Cost c ($) | Total Costa d ($,000) | Average Cost c ($) | Total Costa d ($,000) | Average Cost c ($) | Total Costa d ($,000) | Total Cost of Fall-related Injuries a e ($,000) | Population in Each Age-group (2010) b | Cost of Fall-Related Injury per Person f (Total Cost/Person, $) |
| 18–24 | 1,887,705 | 356,776 | 181,949 | 2,938,802 | 6,575 | 4,011,673 | 7,307,251 | 30,672,088 | 238.24 |
| 25–34 | 1,908,136 | 570,533 | 183,753 | 5,159,815 | 6,648 | 5,296,202 | 11,026,550 | 41,063,948 | 268.52 |
| 35–44 | 1,550,187 | 764,242 | 197,013 | 7,781,336 | 6,938 | 5,179,236 | 13,724,814 | 41,070,606 | 334.18 |
| 45–54 | 1,083,457 | 1,390,075 | 185,623 | 14,988,049 | 7,107 | 6,349,632 | 22,727,756 | 45,006,716 | 504.99 |
| 55–64 | 600,934 | 1,208,478 | 117,596 | 12,362,819 | 5,783 | 4,321,450 | 17,892,747 | 36,482,729 | 490.44 |
| 65–74 | 275,964 | 824,580 | 84,523 | 12,305,483 | 4,895 | 2,740,821 | 15,870,884 | 21,713,429 | 730.92 |
| 75+ | 109,387 | 2,041,268 | 61,866 | 17,218,034 | 4,107 | 2,746,470 | 22,005,772 | 18,554,555 | 1186.00 |
| All Adults (18+) | 276,036 | 7,155,952 | 104,909 | 72,754,338 | 6,102 | 30,645,484 | 110,555,774 | 234,564,071 | 471.32 |
* Data extracted from WISQARS http://www.cdc.gov/injury/wisqars/
a In thousands
b Census data from 2010
c Average lifetime cost of fall-related injury that resulted in death, hospitalization or emergency department visit, respectively
d Total lifetime cost of fall-related injury that resulted in death, hospitalization or emergency department visit, respectively (average cost * number of injuries)
e Total cost of fall-related injuries (sum of the total lifetime cost of fall-related injury that resulted in death, hospitalization or emergency department visit
f Lifetime cost of fall-related injury per person (Total cost of fall-related injuries in an age group ÷ total population in the age group)
Among U.S. adults, the total lifetime cost of annual unintentional fall-related injuries that resulted in a fatality, hospitalization or treatment in emergency department was 111 billion U.S. dollars (Table 4). The highest total lifetime cost of unintentional fall-related injuries was in the 45–54 year age-group (23 billion U.S. dollars, Table 4). The costs of fall-related injuries per person were $1186, $731, $490 and $505 for the 75+, 65–74, 55–64 and 45–54 years age-groups, respectively.
Discussion
Using a special supplement of the NHIS, one of the largest national health surveys in the U.S., we found that 12% of community-dwelling U.S. adults reported falling in the previous year for a total estimate of 80 million falls at a rate of 37.2 falls per 100 person-years. While this is the best estimate available at the national level and demonstrates a significant exposure to falling, it is likely an underestimate of the number of individuals every year exposed to falls. Fall incidents, especially those without an injury, are difficult to recall over a 12-month period. The proportion of Fallers in the oldest age group (65+) was 16.4%. This estimate, for the aforementioned reasons, is comparably lower than other estimates for this age group; a number of prior studies have reported that about a third of community-dwelling adults over 65 years of age report falling in one year.[12–14]
We found that the proportion of Fallers in the previous 12 months was 10.6% in the 18–44 year age-group, and 11.4% in the 45–64 year age-group. For comparison, a study using the data from the Baltimore Longitudinal Study on Aging found that 18.5% of young adults (20–45 years), 21% of middle-aged adults (46–65 years) and 35% of older adults (65+) reported one or more falls in the previous two years.[21] In this case, the recall period was twice as long as in the current study, and these proportions are correspondingly about double the values we report. Mertz et al., using the data from the Aerobics Center Longitudinal Study, which included participants referred (by self or employer) for the purpose of fitness evaluation and lifestyle counselling, found that 20% of the participants aged 20–87 years reported falling during the past year.[22] Some of the estimates from longitudinal studies are higher than those we observed using the NHIS 2008 Balance and Dizziness Supplement sample. However, these studies also assessed smaller samples, were conducted at a local level, and did not provide a national estimate.
Regardless of the variability in the findings across studies and the values we estimated from the NHIS 2008 Balance and Dizziness Supplement, the number of community-dwelling adults who report falling is high and represents a significant public health concern for not only older adults but for adults of all ages. As the number and the rate of fall-related injuries have increased in recent years, it is possible that the number of falls and falls rates have also increased from 2008. Therefore, in addition to collecting surveillance information about fall-related injuries, it is essential to also regularly collect information on falls as the high frequency of falls makes it possible for national and state-based surveillance systems to provide stable estimates, even for smaller geographic regions and, thus, assess risk factors for falls and trends over time. In addition, an emphasis on falls also provides the opportunity to efficiently conduct prospective studies and randomized controlled trials to evaluate fall prevention strategies in older adults as well as among middle-aged and younger adults. Finally, regular assessment of falls across all ages may help in early interventions to reduce the risk of falls and, ultimately, prevent fall-related injuries.
About 9.9 million fall-related injuries were reported each year among community-dwelling U.S. adults at a rate of 4.38 fall-related injuries per 100 person-years, according to the pooled NHIS data from 2004 to 2013. Corso et al. also reported a similar rate of fall-related injuries in the U.S. (4.2 per 100 person-years) using data from the Medical Expenditure Panel Survey, Healthcare Cost and Utilization Project—Nationwide Inpatient Sample and National Electronic Injury Surveillance System—All Injury Program.[23] The Centers for Disease Control and Prevention’s (CDC) Vital and Health Statistics publication reported 9.8 million fall-related injuries among U.S. adults in the year 2012.[24]
In the previous three months, 2.0% of older adults, 1.1% of middle-aged adult and 0.7% of young adults reported a fall-related injury and the rate of fall-related injuries increased with age. In general, older adults are more vulnerable to falls and injuries resulting from them. The injuries from falls are also more severe in older adults. Therefore, the focus of research and fall prevention has been predominantly on the older adult population[11] with only a few studies examining falls in middle-aged and young adults in the general population.[21, 25–33] The number of middle-aged adults in the U.S. is presently higher than the number of older adults, and even with lower rates of fall-related injury, the number of fall-related injuries among middle-aged adults (45–64) was similar to, if not higher than, older adults (65+).
Middle-aged adults may progressively start to experience higher incidence of disease and medication use along with decreasing postural stability, proprioception, and balance.[34–37] Furthermore, in most developed countries, wage earnings peak when individuals are in their 40s and 50s and, of all age-groups, middle-aged adults have the highest average household income in the U.S.[38] Injuries and concomitant loss of income during this phase of the life course may lead to a significant economic impact at the individual and family level.
The cost of injury data from WISQARS showed that the cost of fall-related injuries per person among middle-aged adults was about half of the cost among older adults.[19] A recent study from CDC reported that Otago Exercise Program, Tai Chi, and Stepping On were cost-beneficial for older adults with a positive return on investment.[39] Given the lower average cost of fall-related injuries, these programs may not be cost-beneficial for middle-aged adults. Thus, there is a need for more efficient fall risk assessment approaches that take into account multiple risk factors for falls in addition to age to identify middle-aged adults who are at a higher risk of falls and fall-related injuries, and focus fall prevention interventions towards these high risk individuals. Broad-based low cost fall prevention interventions could also be implemented earlier in the adult lifespan. Improved muscle strength, balance, and proprioception developed and maintained during middle-age may be carried over when the individual gets older, aiding in the reduction of falls and fall-related injuries in the older adult population.[40]
We observed an increasing trend (age- and gender-adjusted) in the rate of fall-related injuries from 2004 to 2013 among community-dwelling U.S adults (p <0.10, not statisically significant at 0.05 level) and, particularly, among older adults. We observed a similar magnitude of increasing trend among older adults of both genders (4% per year for older women and 5% per year for older men). However, the trend was not statistically significant for older men at 0.05 level. There was a smaller estimated number of men in comparison to women among those in the 65+ year age group (22 million vs. 36 million, table 1), which could have led to a higher year-to-year variability in fall-related injury incidence rate among older men. Hu and Baker reported a 6% increase from 2001 to 2007 in the rate of emergency department visits due to falls among older adults.[41] Two recent reports also observed age adjusted increases in fall incidence and emergency department-treated and hospitalization fall-related injuries among older U.S. adults.[42, 43] It is unclear whether increased awareness has led to improved reporting or if a true increase in fall-related injuries is occurring. As falls and fall-related injuries are increasing beyond demographic changes, more research is needed to understand possible reasons. Addressing the burden of fall-related injuries will require improved identification of adults who are at a higher risk for falls with evidence-based fall risk assessment approaches and the development and implementation of effective fall prevention programs across the adult life span.
More research is also needed regarding built environment design characteristics which can lower the risk of falls and fall-related injuries. For example, recently published studies have highlighted the need for more research in the areas of changes in floor level, stairs, slip-resistance of floor surfaces, lighting and visual cues.[44, 45] Studies have also demonstrated that impact-absorbing flooring significantly reduces the risk of injury in the event of a fall.[46] Other strategies to attenuate the impact force, such as hip protectors and martial arts training, may also reduce the risk of hip fracture following a fall.[47–49] In addition, a few laboratory studies have reported that repeated-slip training focusing on dynamic stability and weight support may be an effective intervention in reducing falls after a slipping event.[50–52] Lastly, measures to increase bone strength may lead to a reduced risk of fracture given a fall event.[53–55]
Strengths and Limitations with Regards to Falls Surveillance
An important strength of this study is that it uses data from a large-scale, nationally representative, population-based survey which is conducted through in-person interviews—the NHIS. The 2008 Balance and Dizziness Supplement provided a unique opportunity to estimate the incidence of falls among U.S adults at the national level. The 2008 supplement questions relating to falls in adults had a 12-month recall period. A one-year recall period could lead to lower reported falls, particularly falls that do not result in an injury, potentially underestimating the number of Fallers and falls reported in this study. Older adults may have more difficulty recalling a fall event. Cumming et al. found that older adults often do not recall falls that occurred during specific periods of time over the preceding 3 to 12 months.[56] Warner et al., using data from the NHIS, previously suggested a recall period of 5 weeks to adequately recall less severe injuries.[57] The Prevention of Falls Network Europe (ProFaNE) recommends prospective daily recording with a minimum of monthly reporting.[58] Daily recordings could be difficult to accommodate in current national surveillance systems. However, given the high incidence of falls, a recall period of one month could be evaluated for use in these systems.
In addition, in the 2008 supplement, the number of falls was stratified for those who fell 3 or more times. We used the mid-points of strata “3–4 times (3.5 falls),” “5–7 times (6 falls),” and “8 or more times (10 falls, a midpoint between 8 and 12 falls)” to assign the number of falls. For more than 12 falls in the previous year, the number of falls was set to 12. The assignment of the number of falls based on stratum may have led to overestimation or underestimation of the total number of falls. We conducted a sensitivity analysis using the lower and upper boundaries of each stratum to assign the number of falls and observed that changing the assignment protocol did not significantly affect the overall estimate of the number of falls.
The NHIS does not include institutionalized individuals. Elderly individuals who fall and get injured are more likely to be institutionalized [59, 60] and, thus, are more likely to be excluded from the study. In addition, the excluded institutionalized population is composed primarily of the population in correctional institutions and nursing homes (91% of the 4.1 million institutionalized people in U.S. Census 2000).[61] Older adults in nursing homes are at a higher risk of falls and fall-related injuries.[62] Therefore, estimates based on NHIS data may underestimate the burden of falls and fall-related injuries, and the underestimation may be particularly significant for older adults.
Conclusion
This study provides national estimates of falls and fall-related injuries among community-dwelling U.S. adults across the adult life span. Based on the 2008 NHIS Balance and Dizziness Supplement and the pooled NHIS annual data, about 12% of community-dwelling U.S. adults fall every year, experiencing an approximate national total of 80 million falls, and 9.9 million fall-related injuries occur every year among community-dwelling U.S. adults at a rate of 4.38 injuries per 100 person-years. In the previous three months, 2.0% of older adults, 1.1% of middle-aged adult and 0.7% of young adults reported a fall-related injury. Of all fall-related injuries to adults, 32.3% occurred among older adults, 35.3% among middle-aged adults and 32.3% among younger adults. Age-gender adjusted rates of fall-related injuries are increasing in the U.S.; more research is needed to understand possible reasons and to develop and implement effective fall and fall-related injury prevention strategies across all ages to significantly reduce the burden of injuries from falls.
Acknowledgments
We would like to thank Drs. Tin-Chi Lin, and Mary Lesch for insightful reviews, and Ms. Peg Rothwell for editorial input on the final article.
Data Availability
The data for the National Health Interview Survey are collected by the National Center for Health Statistics in the Centers for Disease Control and Prevention and are made publically available at the following website: http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm. The Web-based Injury Statistics Query and Reporting System (WISQARS) is collected by the Injury Center in the Centers for Disease Control and prevention and are publically available at the following website: http://www.cdc.gov/injury/wisqars/cost_help/calculations_toc.html.
Funding Statement
The authors have no support or funding to report.
References
- 1.Murphy SL, Xu J, Kochanek KD. Deaths: final data for 2010. National Vital Statistics Reports. 61(4):1–118. [PubMed] [Google Scholar]
- 2.Sise RG, Calvo RY, Spain DA, Weiser TG, Staudenmayer KL. The epidemiology of trauma-related mortality in the United States from 2002 to 2010. J Trauma Acute Care Surg. 2014;76(4):913–9. 10.1097/TA.0000000000000169 [DOI] [PubMed] [Google Scholar]
- 3.Gorina Y, Hoyert D, Lentzner H, Goulding M. Trends in causes of death among older persons in the United States Washington, DC: Centers for Disease Control and Prevention, National Center for Health Statistics; 2005. Available: http://www.cdc.gov/nchs/data/ahcd/agingtrends/06olderpersons.pdf. [PubMed] [Google Scholar]
- 4.Orces CH. Trends in fall-related mortality among older adults in Texas. Tex Med. 2008;104(5):55–9. [PubMed] [Google Scholar]
- 5.Hu G, Baker SP. Trends in unintentional injury deaths, U.S., 1999–2005: age, gender, and racial/ethnic differences. Am J Prev Med,. 2009;37(3):188–94. 10.1016/j.amepre.2009.04.023 [DOI] [PubMed] [Google Scholar]
- 6.Adams PE, Martinez ME, Vickerie JL, Kirzinger WK. Summary health statistics for the US population: National Health Interview Survey, 2010. Vital and Health Statistics Series 10, Data from the National Health Survey. 2010;(251):1–117. [PubMed] [Google Scholar]
- 7.Curry P, Ramaiah R, Vavilala MS. Current trends and update on injury prevention. Int J Crit Illn Inj Sci. 2011;1(1):57–65. 10.4103/2229-5151.79283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. 10 Leading Causes of Injury Deaths by Age Group Highlighting Unintentional Injury Deaths, United States– 2010 2010. Available: http://web.archive.org/web/20140911181934/http://www.cdc.gov/injury/wisqars/pdf/10LCID_Unintentional_Deaths_2010-a.pdf.
- 9.Collaborators USBoD. The state of us health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–606. 10.1001/jama.2013.13805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Institute for Health Metrics and Evaluation (IHME). GBD Profile: United States Seattle, WA: University of Washington; 2013. [updated 5 March, 2013; cited 2014]. Available: https://web.archive.org/web/20140826200910/http://www.healthdata.org/sites/default/files/files/country_profiles/GBD/ihme_gbd_country_report_united_states.pdf. [Google Scholar]
- 11.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community: Cochrane Database of Systematic Reviews 2012. The Cochrane database of systematic reviews. 2012;(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehab. 2001;82(8):1050–6. [DOI] [PubMed] [Google Scholar]
- 13.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. The New England journal of medicine. 1988;319(26):1701–7. Epub 1988/12/29. 10.1056/nejm198812293192604 . [DOI] [PubMed] [Google Scholar]
- 14.Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age and Ageing. 1990;19(2):136–41. 10.1093/ageing/19.2.136 WOS:A1990CY04700012. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. National Health Interview Survey 2014. Available: http://www.cdc.gov/NCHS/NHIS.htm.
- 16.Lombardi DA, Folkard S, Willetts JL, Smith GS. Daily sleep, weekly working hours, and risk of work-related injury: US National Health Interview Survey (2004–2008). Chronobiol Int. 2010;27(5):1013–30. 10.3109/07420528.2010.489466 [DOI] [PubMed] [Google Scholar]
- 17.Smith GS, Wellman HM, Sorock GS, Warner M, Courtney TK, Pransky GS, et al. Injuries at work in the US adult population: contributions to the total injury burden. Am J Public Health. 2005;95(7):1213–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warner M, Barnes PM, Fingerhut LA. Injury and poisoning episodes and conditions: National Health Interview Survey, 1997. Vital Health Stat. 2000;10(202):1–38. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Data & Statistics (WISQARS™): Cost of Injury Reports 2012. Available from: http://wisqars.cdc.gov:8080/costT/cost_Part1_Intro.jsp.
- 20.Finkelstein E, Phaedra C, Miller T. The Incidence and Economic Burden of Injuries in the United States. New York, NY: Oxford University Press; 2006. 187 p. [Google Scholar]
- 21.Talbot LA, Musiol RJ, Witham EK, Metter EJ. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health. 2005;5(1):86 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mertz KJ, Lee DC, Sui X, Powell KE, Blair SN. Falls among adults: the association of cardiorespiratory fitness and physical activity with walking-related falls. American journal of preventive medicine. 2010;39(1):15–24. 10.1016/j.amepre.2010.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2006;12(4):212–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adams PF, Kirzinger WK, Martinez ME. Summary health statistics for the U.S. population: National Health Interview Survey, 2012. National Center for Health Statistics Vital and Health Statistics Series 10 (259) 2013. [PubMed] [Google Scholar]
- 25.Kool B, Ameratunga S, Robinson E. Association between prescription medications and falls at home among young and middle-aged adults. Inj Prev. 2012;18(3):200–3. 10.1136/injuryprev-2011-040202 [DOI] [PubMed] [Google Scholar]
- 26.Andresen EM, Wolinsky FD, Miller JP, Wilson MM, Malmstrom TK, Miller DK. Cross-sectional and longitudinal risk factors for falls, fear of falling, and falls efficacy in a cohort of middle-aged African Americans. Gerontologist. 2006;46(2):249–57. [DOI] [PubMed] [Google Scholar]
- 27.Hoidrup S, Sorensen TI, Gronbaek M, Schroll M. Incidence and characteristics of falls leading to hospital treatment: a one-year population surveillance study of the Danish population aged 45 years and over. Scand J Public Health. 2003;31(1):24–30. [DOI] [PubMed] [Google Scholar]
- 28.Li W, Keegan TH, Sternfeld B, Sidney S, Quesenberry CP Jr., Kelsey JL. Outdoor falls among middle-aged and older adults: a neglected public health problem. Am J Public Health. 2006;96(7):1192–200. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sihvonen S, Era P, Helenius M. Postural balance and health-related factors in middle-aged and older women with injurious falls and non-fallers. Aging Clin Exp Res. 2004;16(2):139–46. [DOI] [PubMed] [Google Scholar]
- 30.Kool B, Ameratunga S, Hazell W, Ng A. Unintentional falls at home among young and middle-aged New Zealanders resulting in hospital admission or death: context and characteristics. N Z Med J. 2010;123(1316):75–84. [PubMed] [Google Scholar]
- 31.Barrett-Connor E, Weiss TW, McHorney CA, Miller PD, Siris ES. Predictors of falls among postmenopausal women: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int. 2009;20(5):715–22. 10.1007/s00198-008-0748-2 [DOI] [PubMed] [Google Scholar]
- 32.Brown MJ, Jacobs DE. Residential light and risk for depression and falls: results from the LARES study of eight European cities. Public Health Rep. 2011;1:131–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Falls—Older Adults 2014. Available: http://www.cdc.gov/HomeandRecreationalSafety/Falls/Index.html.
- 34.Choy NL, Brauer S, Nitz J. Changes in postural stability in women aged 20 to 80 years. J Gerontol A Biol Sci Med Sci. 2003;58(6):525–30. [DOI] [PubMed] [Google Scholar]
- 35.Isles RC, Choy NL, Steer M, Nitz JC. Normal values of balance tests in women aged 20–80. J Am Geriatr Soc. 2004;52(8):1367–72. [DOI] [PubMed] [Google Scholar]
- 36.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the united states: The Slone survey. JAMA. 2002;287(3):337–44. [DOI] [PubMed] [Google Scholar]
- 37.Nitz JC, Choy NL, Isles RC. Medial-lateral postural stability in community-dwelling women over 40 years of age. Clin Rehabil. 2003;17(7):765–7. [DOI] [PubMed] [Google Scholar]
- 38.Bureau of Labor Statistics. Usual Weekly Earnings of Wage and Salary Workers, Second Quarter 2014. Available: https://web.archive.org/web/20140908172557/http://www.bls.gov/news.release/pdf/wkyeng.pdf.
- 39.Carande-Kulis V, Stevens JA, Florence CS, Beattie BL, Arias I. A cost-benefit analysis of three older adult fall prevention interventions. J Safety Res. 2015;52:65–70. 10.1016/j.jsr.2014.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Caban-Martinez AJ, Courtney TK, Chang W-R, Lombardi DA, Huang Y-H, Brennan MJ, et al. Leisure-time physical activity, falls, and fall injuries in middle-aged adults. American journal of preventive medicine. 2015;49(6):888–901. 10.1016/j.amepre.2015.05.022 [DOI] [PubMed] [Google Scholar]
- 41.Hu G, Baker SP. An explanation for the recent increase in the fall death rate among older Americans: a subgroup analysis. Public Health Reports. 2012;127(3):275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cigolle CT, Ha J, Min LC, Lee PG, Gure TR, Alexander NB, et al. The Epidemiologic Data on Falls, 1998–2010: More Older Americans Report Falling. JAMA Intern Med. 2015;175(3):443–5. 10.1001/jamainternmed.2014.7533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Orces CH, Alamgir H. Trends in fall-related injuries among older adults treated in emergency departments in the USA. Inj Prev. 2014;20(6):421–3. 10.1136/injuryprev-2014-041268 [DOI] [PubMed] [Google Scholar]
- 44.Cohen HH, Sloan GD. The science behind codes and standards for safe pedestrian walkways: lighting and visual cues. Applied ergonomics. 2015;52:112–9. 10.1016/j.apergo.2015.07.002 [DOI] [PubMed] [Google Scholar]
- 45.Nemire K, Johnson DA, Vidal K. The science behind codes and standards for safe walkways: changes in level, stairways, stair handrails and slip resistance. Applied ergonomics. 2015;52:309–16. 10.1016/j.apergo.2015.07.021 [DOI] [PubMed] [Google Scholar]
- 46.Gustavsson J, Bonander C, Andersson R, Nilson F. Investigating the fall-injury reducing effect of impact absorbing flooring among female nursing home residents: initial results. Injury Prevention. 2015. 10.1136/injuryprev-2014-041468 [DOI] [PubMed] [Google Scholar]
- 47.Santesso N, Carrasco-Labra A, Brignardello-Petersen R. Hip protectors for preventing hip fractures in older people. The Cochrane database of systematic reviews. 2014;3:Cd001255 Epub 2014/04/02. 10.1002/14651858.CD001255.pub5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weerdesteyn V, Groen BE, van Swigchem R, Duysens J. Martial arts fall techniques reduce hip impact forces in naive subjects after a brief period of training. Journal of electromyography and kinesiology: official journal of the International Society of Electrophysiological Kinesiology. 2008;18(2):235–42. Epub 2007/09/04. 10.1016/j.jelekin.2007.06.010 . [DOI] [PubMed] [Google Scholar]
- 49.Groen BE, Weerdesteyn V, Duysens J. Martial arts fall techniques decrease the impact forces at the hip during sideways falling. Journal of biomechanics. 2007;40(2):458–62. Epub 2006/02/17. 10.1016/j.jbiomech.2005.12.014 . [DOI] [PubMed] [Google Scholar]
- 50.Liu J, Lockhart TE, Parijat P, McIntosh JD, Chiu YP. Comparison of Slip Training in VR Environment And on Moveable Platform. Biomedical sciences instrumentation. 2015;51:189–97. Epub 2015/05/23. . [PubMed] [Google Scholar]
- 51.Parijat P, Lockhart TE, Liu J. Effects of perturbation-based slip training using a virtual reality environment on slip-induced falls. Annals of biomedical engineering. 2015;43(4):958–67. Epub 2014/09/24. 10.1007/s10439-014-1128-z ; PubMed Central PMCID: PMCPmc4384510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pai YC, Bhatt TS. Repeated-slip training: an emerging paradigm for prevention of slip-related falls among older adults. Physical therapy. 2007;87(11):1478–91. Epub 2007/08/23. 10.2522/ptj.20060326 ; PubMed Central PMCID: PMCPmc2826275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Avenell A, Mak JC, O'Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. The Cochrane database of systematic reviews. 2014;4:Cd000227 Epub 2014/04/15. 10.1002/14651858.CD000227.pub4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. The Cochrane database of systematic reviews. 2011;(7):Cd000333 Epub 2011/07/08. 10.1002/14651858.CD000333.pub2 . [DOI] [PubMed] [Google Scholar]
- 55.Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. The Cochrane database of systematic reviews. 2008;1(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36(7):613–6. [DOI] [PubMed] [Google Scholar]
- 57.Warner M, Schenker N, Heinen MA, Fingerhut LA. The effects of recall on reporting injury and poisoning episodes in the National Health Interview Survey. Inj Prev. 2005;11(5):282–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–22. Epub 2005/09/03. JGS53455 [pii] 10.1111/j.1532-5415.2005.53455.x . [DOI] [PubMed] [Google Scholar]
- 59.Porell FW, Carter MW. Risk of mortality and nursing home institutionalization after injury. J Am Geriatr Soc. 2012;60(8):1498–503. Epub 2012/08/07. 10.1111/j.1532-5415.2012.04053.x . [DOI] [PubMed] [Google Scholar]
- 60.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. The New England journal of medicine. 1997;337(18):1279–84. Epub 1997/11/05. 10.1056/nejm199710303371806 . [DOI] [PubMed] [Google Scholar]
- 61.Brault MW. Americans with disabilities: 2010: Household economic studies: US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2012.
- 62.Luukinen H, Koski K, Honkanen R, Kivela SL. Incidence of injury-causing falls among older adults by place of residence: a population-based study. J Am Geriatr Soc. 1995;43(8):871–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data for the National Health Interview Survey are collected by the National Center for Health Statistics in the Centers for Disease Control and Prevention and are made publically available at the following website: http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm. The Web-based Injury Statistics Query and Reporting System (WISQARS) is collected by the Injury Center in the Centers for Disease Control and prevention and are publically available at the following website: http://www.cdc.gov/injury/wisqars/cost_help/calculations_toc.html.