Abstract
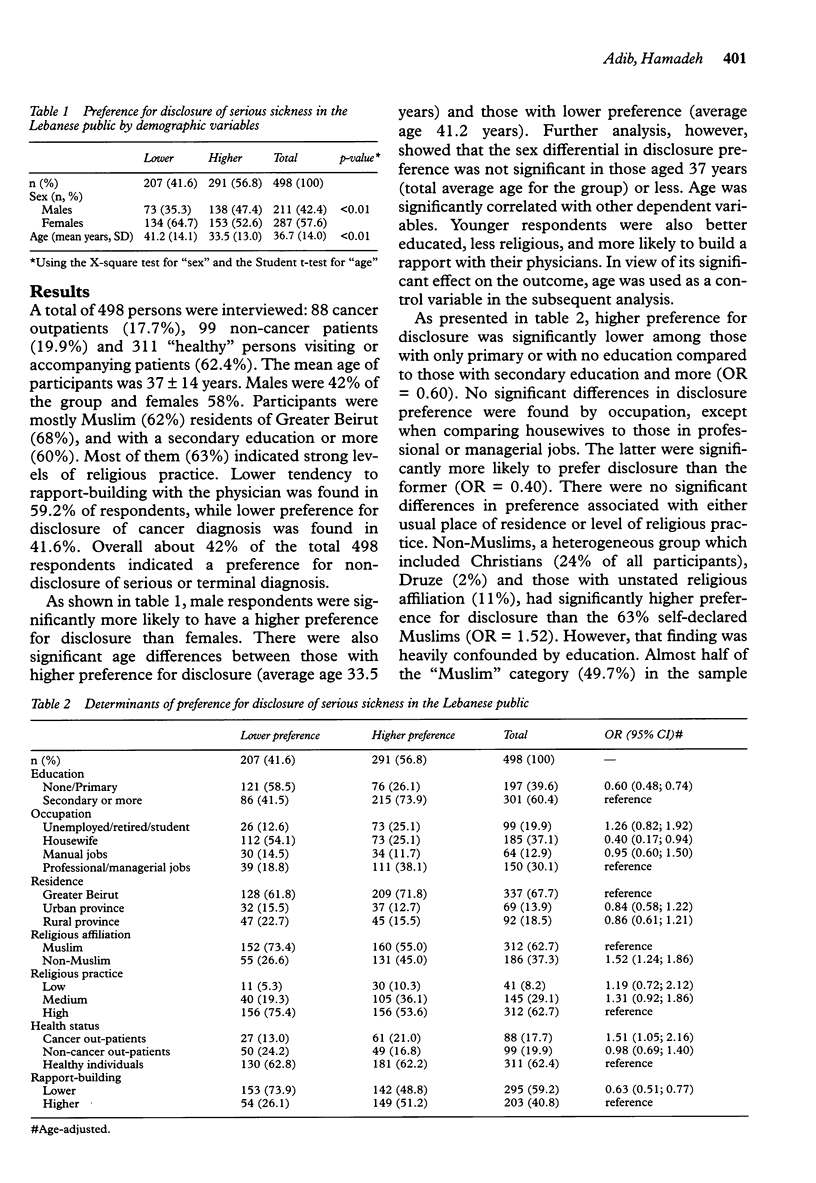
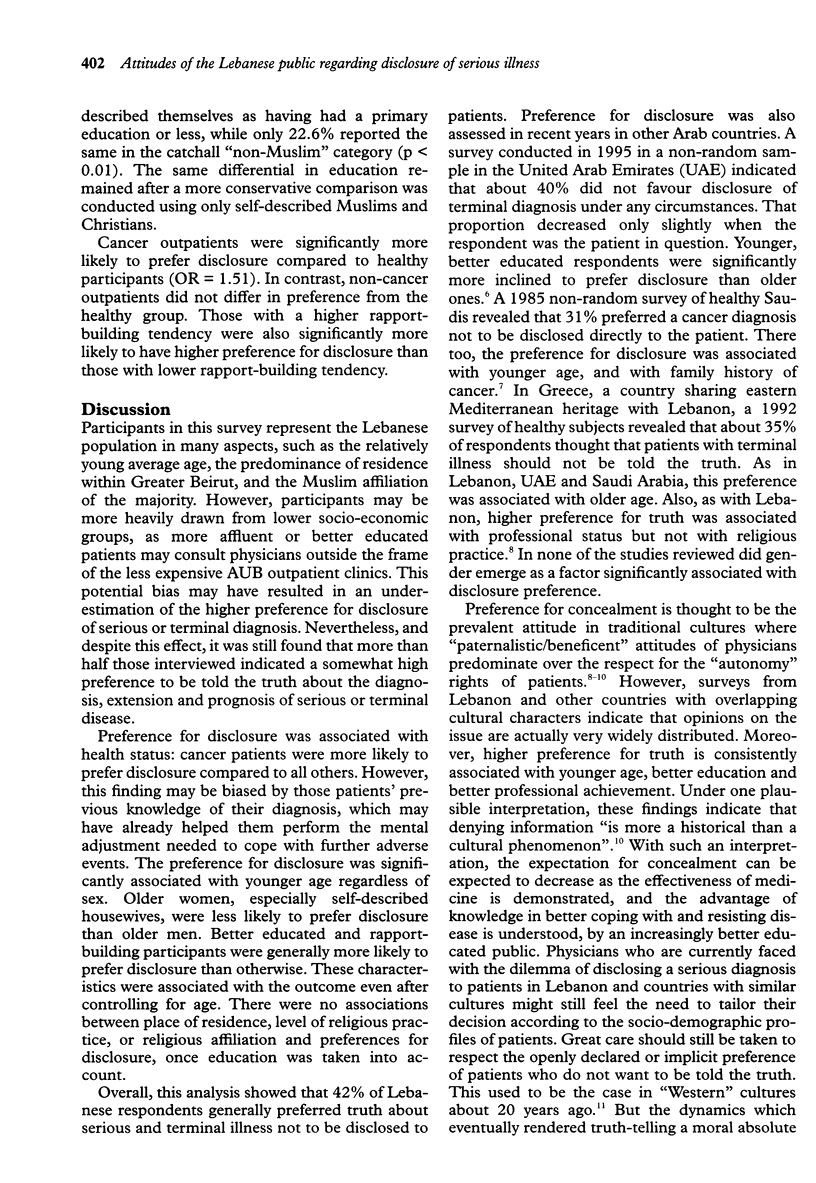
OBJECTIVES: To measure the preference regarding disclosure of a serious diagnosis, and its determinants, of the Lebanese public. DESIGN AND SETTING: Non-random sample survey of 400 persons interviewed in health care facilities in Beirut in 1995. RESULTS: Forty-two per cent of respondents generally preferred truth not to be disclosed directly to patients. Preference for disclosure was associated with younger age, better education and tendency to rapport-building with physicians. There were no meaningful associations between place of residence (urban/rural), level of religious practice, or religious affiliation, and preference for disclosure. CONCLUSIONS: Under one plausible interpretation, this survey suggests that the expectation for concealment will decrease as the advantage of knowledge in better coping with disease is understood by an increasingly better educated public, and that the Lebanese public will increasingly come to expect direct and full disclosure of serious diagnoses.
Full text
PDF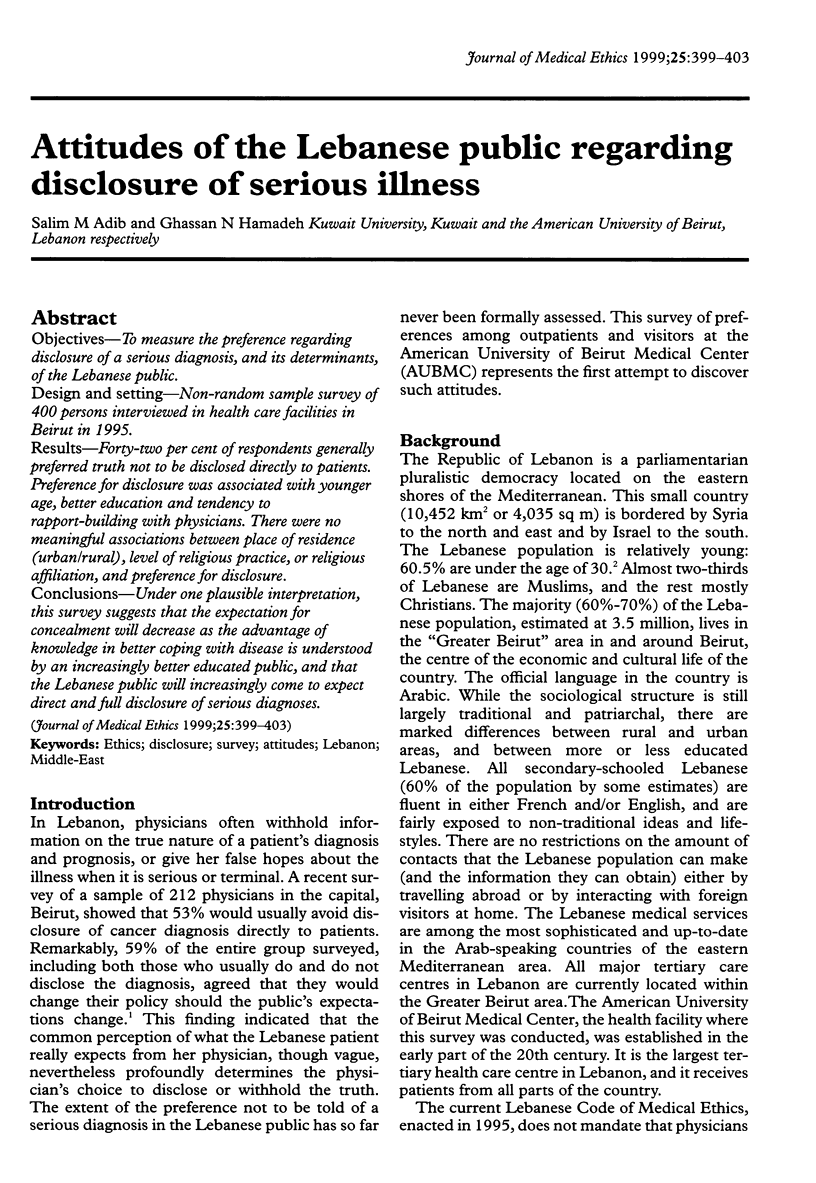
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brusamolino E., Surbone A. Telling the truth to the patient with cancer. A cross-cultural dialogue. Ann N Y Acad Sci. 1997 Feb 20;809:411–421. doi: 10.1111/j.1749-6632.1997.tb48104.x. [DOI] [PubMed] [Google Scholar]
- Cassileth B. R., Zupkis R. V., Sutton-Smith K., March V. Information and participation preferences among cancer patients. Ann Intern Med. 1980 Jun;92(6):832–836. doi: 10.7326/0003-4819-92-6-832. [DOI] [PubMed] [Google Scholar]
- Dalla-Vorgia P., Katsouyanni K., Garanis T. N., Touloumi G., Drogari P., Koutselinis A. Attitudes of a Mediterranean population to the truth-telling issue. J Med Ethics. 1992 Jun;18(2):67–74. doi: 10.1136/jme.18.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamadeh G. N., Adib S. M. Cancer truth disclosure by Lebanese doctors. Soc Sci Med. 1998 Nov;47(9):1289–1294. doi: 10.1016/s0277-9536(98)00203-2. [DOI] [PubMed] [Google Scholar]
- Harrison A., al-Saadi A. M., al-Kaabi A. S., al-Kaabi M. R., al-Bedwawi S. S., al-Kaabi S. O., al-Neaimi S. B. Should doctors inform terminally ill patients? The opinions of nationals and doctors in the United Arab Emirates. J Med Ethics. 1997 Apr;23(2):101–107. doi: 10.1136/jme.23.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrino E. D. Is truth telling to the patient a cultural artifact? JAMA. 1992 Oct 7;268(13):1734–1735. [PubMed] [Google Scholar]
- Sardell A. N., Trierweiler S. J. Disclosing the cancer diagnosis. Procedures that influence patient hopefulness. Cancer. 1993 Dec 1;72(11):3355–3365. doi: 10.1002/1097-0142(19931201)72:11<3355::aid-cncr2820721135>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]


