Abstract
Besides its anti-inflammatory, analgesic and anti-pyretic properties, aspirin is used for the prevention of cardiovascular disease and various types of cancer. The multiple activities of aspirin likely involve several molecular targets and pathways rather than a single target. Therefore, systematic identification of these targets of aspirin can help us understand the underlying mechanisms of the activities. In this study, we identified 23 putative targets of aspirin in the human proteome by using binding pocket similarity detecting tool combination with molecular docking, free energy calculation and pathway analysis. These targets have diverse folds and are derived from different protein family. However, they have similar aspirin-binding pockets. The binding free energy with aspirin for newly identified targets is comparable to that for the primary targets. Pathway analysis revealed that the targets were enriched in several pathways such as vascular endothelial growth factor (VEGF) signaling, Fc epsilon RI signaling and arachidonic acid metabolism, which are strongly involved in inflammation, cardiovascular disease and cancer. Therefore, the predicted target profile of aspirin suggests a new explanation for the disease prevention ability of aspirin. Our findings provide a new insight of aspirin and its efficacy of disease prevention in a systematic and global view.
Keywords: Target, Cancer, Molecular docking, Aspirin, Cardiovascular disease, Binding site
Introduction
Aspirin, also known as acetylsalicylic acid, is a nonsteroidal anti-inflammatory drug (NSAID). The primary molecular mechanism of aspirin is the selective acetylaton of Ser-530 of cyclooxygenase-1 (COX-1) (Alfonso et al., 2014; Dovizio et al., 2013; Ghooi, Thatte & Joshi, 1995; Vane, 1971; Vane & Botting, 2003), thereby inhibiting prostaglandin synthesis. This was the basis for its anti-inflammatory, antipyretic, and analgesic effects (Vane & Botting, 2003). In addition, recent studies revealed that phospholipases A2 (PLA2) is functionally coupled with cyclooxygenase-1 and 2 pathway and part of its anti-inflammatory effects of aspirin may be due to its binding with PLA2 (Balsinde et al., 1999; Singh et al., 2005; Touqui & Alaoui-El-Azher, 2001).
Besides its the anti-inflammatory, analgesic, and anti-pyretic properties, aspirin is used for the prevention of cardiovascular disease and various types of cancer (Alfonso et al., 2014; Dovizio et al., 2013). Aspirin prevents myocardial infarction, and ischemic stroke when used in the primary prevention of cardiovascular disease (Berger, Brown & Becker, 2008; Nemerovski et al., 2012; Raju et al., 2011; Schnell, Erbach & Hummel, 2012; Younis et al., 2010). Furthermore, aspirin is also highly effective in preventing several common cancers (Avivi et al., 2012; Burn et al., 2011; Hassan et al., 2012; Rothwell et al., 2010; Rothwell et al., 2012; Thun, Jacobs & Patrono, 2012). Taking aspirin daily reduced risk of distant metastasis by 30–40% and reduced the risk of metastatic adenocarcinoma by almost a half (Rothwell et al., 2012). Although it has been convincingly shown that aspirin can prevent cardiovascular disease and several cancer types, the molecular mechanisms underlying these effects of aspirin are not entirely clear. The multiple activities of aspirin cannot be attributed wholly to a single target and most likely involve several molecular targets and pathways (Deng & Fang, 2012; Din et al., 2012; Sclabas et al., 2005; Singh et al., 2005). Therefore, systematic identification of molecular targets of aspirin can help in understanding the mechanisms underlying the activities and adverse reactions of aspirin. Unfortunately, studies on the proteome-wide target profile of aspirin are very limited.
In this study, we predicted the targets of aspirin whole proteome-wide by combining structural bioinformatics and systems biology approaches. Starting with the binding sites of aspirin (BSiteAs), the potential targets of aspirin were discovered by using contact matrix based local structural alignment algorithm (CMASA) which was developed in our lab (Li & Huang, 2010). Then, molecular docking and free energy calculation were applied to filter the improper targets to which the aspirin can not bind. We also analyzed the diversity of the putative targets and binding modes of aspirin. Finally, we performed the pathway analysis for the putative targets. We found several new targets for aspirin which are enriched in the pathways that are strongly involved in inflammatory, cardiovascular disease and cancer, such as vascular endothelial growth factor (VEGF), mitogen-activated protein kinase(MAPK), Fc epsilon RI signaling and arachidonic acid metabolism signaling pathways.
Methods
Overview of pipeline for proteome-wide prediction of aspirin targets
The pipeline for proteome-wide prediction of aspirin targets is outlined in Fig. 1. Firstly, we constructed the structural database of human proteins (17,425 non-redundant structures), and the binding sites of aspirin (BSiteAs) were used to search against this database using the program CMASA. Secondly, the binding abilities of aspirin to these putative off-targets were estimated using molecular docking. If aspirin docked unsuccessfully to the predicted binding pocket of a particular protein, this protein was removed from the target list of aspirin. Thirdly, the remaining putative targets were subject to molecular mechanics Poisson–Boltzmann surface area (MM-PBSA) free energy calculation. Finally, we performed the pathway enrichment analysis for these putative targets.
Figure 1. The pipeline of the structural proteome-wide prediction of aspirin targets.
Starting with the binding sites of aspirin (BSiteAs), the pipeline integrates local structure detecting, molecular docking, free energy calculation, and pathway analysis.
The structure database of human proteins
The query database was built by integrating three available sources of protein structure. The first source is the Protein Data Bank managed by Research Collaboratory for Structural Bioinformatics (RCSB PDB) (http://www.rcsb.org) (Rose et al., 2011), which contains 6,983 structures of human proteins. The other two repositories are structure models built by homology modeling techniques from Structure Atlas of Human Genome (Motono et al., 2011) (http://bird.cbrc.jp/sahg) and GPCR Research Database (GPCR-RD) (Zhang & Zhang, 2010), which have 16,529 and 1,028 structures, respectively. This procedure yielded a total of 24,540 human protein structures. The three available sources of protein structure were integrated and removed the redundancy using CD-HIT Suite (Huang et al., 2010). The identity cut-off was set to 0.95. There are totally 17,425 structures in our self-built ‘non-redundant’ structural database of human proteins. The structural database represents a relatively complete and accurate library of human proteins.
To detect and compare the aspirin binding sites in the structure database
We used all representative aspirin-protein complexes in our study. There are a total of six aspirin-protein complex structures currently available (1OXR, 1TGM, 2QQT, 3GCL, 4NSB and 3IAZ). Both 1OXR and 1TGM are structures of phospholipase A2, we only used 1OXR in this study (Fig. 2A). 2QQT and 3GCL are bovine lactoperoxidase, and we used 3GCL in this study. 4NSB and 3IAZ are structures of buffalo chitinase-3-like protein 1 and bovine lactotransferrin, respectively. The two structures were also used in our study. In addition, 1PTH, the complex structure of salicylic acid and COX-1, was also used in this study (Fig. 2A). Therefore, a total of five complex structures (1OXR, 3GCL, 4NSB, 3IAZ and 1PTH) were used in this study. The binding sites of aspirin (BSiteAs) were defined as amino acid residues lying within 5 Å from atoms of the aspirin. The BSiteAs were used to search against 17,425 non-redundant structures using the program CMASA (http://bsb.kiz.ac.cn/CMASA_flex) which was developed in our lab. The accuracy and sensitivity of this tool were 0.96 and 0.86, respectively. The workflow of CMASA was as following. First, the CMASA parsed the query binding site and the database to be searched. Second, for each structure in database, based on the query binding site, the CMASA enumerated all possible combination of residues in the structure using amino acid substitute. The blocks substitution matrix 62 (BLOSUM62, cutoff = 1) was used. These residue combinations are similar to that in the query binding site. Each residue combination forms a possible local structure. Third, the CMASA used contact matrix average deviation (CMAD) between the query binding site and these local structures to filter the candidate matches. Then, the CMASA calculated the RMSD and the RMSD based P-value if the CMAD < cutoff. At last, the CMASA ranked all of the hits and add their information. Hits are considered significant if the CMASA E-value <0.01.
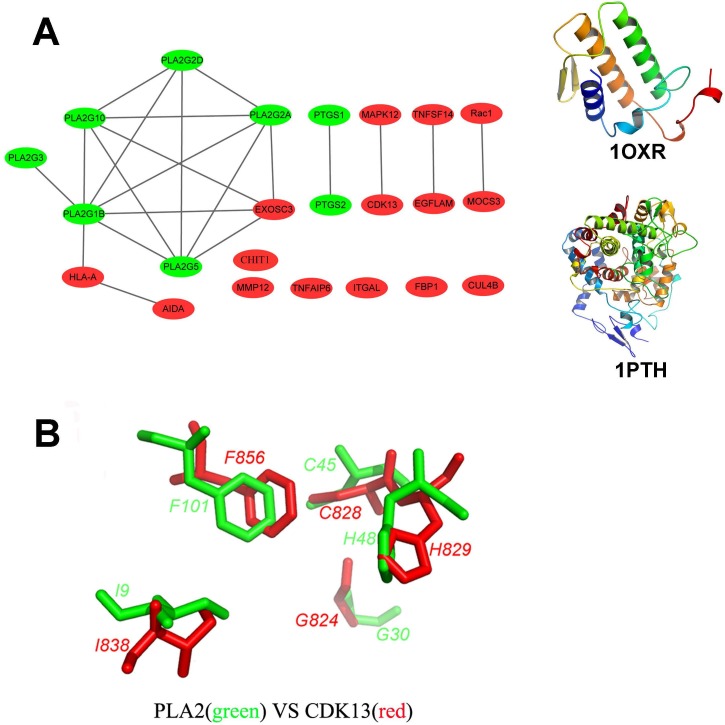
Figure 2. Structural diversity of the putative targets.
(A) The structural similarity network of the putative targets and the structures of 1OXR and 1PTH are also shown. We analyzed the structural similarity of the 23 putative targets by structural alignment. The RMSD between two linked proteins in the network is smaller than 4 Å. The primary targets of aspirin are colored with green, and the newly identified targets are colored with red. (B) Structural alignment of the putative binding sites of aspirin (BSiteAs) from two proteins PLA2G1B (green) and CDK13 (red).
Molecular docking
The hit proteins have similar local structures with BSiteAs and potential to bind to aspirin. However, it does not mean that aspirin can certainly bind to these proteins. To assess whether aspirin can bind to these proteins, flexible ligand-rigid protein docking was performed using CHARMm-based DOCKER (CDOCKER) (Wu et al., 2003) in the Discovery Studio v3.1. The following steps are included in the CDOCKER protocol. (1) A set of ligand conformations are generated using high-temperature molecular dynamics with different random seeds. (2) Random orientations of the conformations are produced by translating the center of the ligand to a specified location within the receptor active site, and performing a series of random rotations. A softened energy is calculated and the orientation is kept if the energy is less than a specified threshold. This process continues until either the desired number of low-energy orientations is found, or the maximum number of bad orientations have been tried. (3) Each orientation is subjected to simulated annealing molecular dynamics. The temperature is heated up to a high temperature then cooled to the target temperature. (4) A final minimization of the ligand in the rigid receptor using non-softened potential is performed. (5) For each final pose, the CHARMm energy (interaction energy plus ligand strain) and the interaction energy alone are calculated. The poses are sorted by CHARMm energy and the top scoring (most negative, thus favorable to binding) poses are retained. In this study, we generated 10 random conformations for each ligand. The parameters of the dynamic steps, the dynamic target temperature and include electrostatics are set to 1,000 steps, 1,000 K and True, respectively, which is the default setting in CDOCKER. The binding sphere of CDOCKER is defined around the local structure detected by CMASA. The center of binding sphere is set as the center of the local structure. And the radius of binding sphere is set as 10 Å, which allows the free rotation of aspirin. If aspirin docked successfully to a particular protein, the binding poses of aspirin showing the lowest energy were retained and used for MM-PBSA (Kollman et al., 2000; Kuhn et al., 2005) free energy calculation. The 3-D structures of docked complexes were visualized using PyMol v1.5.
MM-PBSA free energy calculation and entropy change estimation
The complex structures of aspirin and putative targets were further used to obtain more accurate estimate of binding free energy. Binding free energies (ΔGbind) of aspirin at the binding site on these target proteins were calculated by using the MM-PBSA free energy calculation protocol in Pipeline pilot v8.5 (http://accelrys.com/products/collaborative-science/biovia-pipeline-pilot/) as follows:
| (1) |
where Gcomplex, Greceptor, Gligand are the free energies of the complex, receptor and ligand respectively. The free energy of each molecule on the right hand side can be considered as the sum of molecular mechanics energy in gas phase(EMM) and solvation free energy(Δsol).
As the entropy change (TΔS) is the most time-intensive part, it was not included in the above calculation. We estimate the entropy change in another way. In the study of Chang & Gilson (2004), they computed the entropy changes for different receptors upon same ligand binding. The results showed the entropy changes for different receptors were similar. Therefore, we can estimate an approximate entropy change. The process of entropy change estimation is as following: (1) Based on the formula:—RTlnK = ΔG = ΔH − TΔS (where R is the gas constant, T is the absolute temperature), the entropy changes (TΔS) is equal to the sum of ΔH and RTlnK; (2) The experiment study have shown that aspirin binds to PLA2 enzyme (PDBID: 1OXR) specifically with a binding constant (K) of 1.56 × 105M−1 (Singh et al., 2005). For this complex, the enthalpy change (ΔH) was calculated as −2.327 kcal/mol using the MM-PBSA and RTln K was calculated as 7.055 kcal/mol. So the entropy change (TΔS) is 4.728 kcal/mol (equal to −2.327 kcal/mol + 7.055 kcal/mol) for this complex. 3) Based on above assumption and computation, we set the entropy change in the process of aspirin binding to various putative targets as approximate value 4.728 kcal/mol.
Pathway enrichment analysis and interaction network construction
To analyze the significance of KEGG pathways associated with our predicted targets, we collected UniProtKB accession number (AC) of these targets and performed KEGG pathway annotation using the DAVID tool (http://david.abcc.ncifcrf.gov/). The significantly over-represented KEGG pathways were identified based on the Bonferroni-adjusted P value (P < 0.01) (Huang, Sherman & Lempicki, 2009). In addition, based on these pathways, an integrated targets-cellular effect interaction network was constructed.
Results
Identification of putative targets of aspirin in human proteome
We presented a proteome-wide prediction of aspirin targets using structural bioinformatics and system biology approaches. We used comparison of BSiteAs to recognize putative targets and further refined by docking and MM-PBSA in structural bioinformatics part whereas pathway enrichment analysis and interaction network construction were performed in system biology section. The steps in our pipeline for proteome-wide prediction of aspirin-binding proteins are shown in Fig. 1. Firstly, the binding sites of aspirin (BSiteAs) were used as queries to search against 17,425 non-redundant structures of human proteins in our self-build structure database using the program CMASA. Totally, 79 proteins with putative BSiteAs were identified (Table S1). Of these proteins, the top 10 ranked proteins are members of the phospholipase A2. cyclooxygenase, lactoperoxidase and Chitotriosidase families, which are the primary targets of aspirin. The remaining 69 proteins have different structural folds from the primary targets.
The hit proteins have similar local structures with BSiteAs and potential to bind to aspirin. However, it does not mean that aspirin can certainly bind to these proteins. In the second step, molecular docking was used to assess whether aspirin can bind to these proteins. CDOCKER in the Discovery Studio v3.1 was used to dock aspirin to the predicted binding site on these proteins. Proteins that failed to dock aspirin were removed from the target list. Only 26 proteins were considered for further analysis after filtering by molecular docking, 10 proteins of which are the primary targets of aspirin (Table S1).
Finally, MM-PBSA free energy calculation was performed for the lowest-energy protein-aspirin complex obtained in the docking step. In total, 23 proteins bind to aspirin with binding free energies (ΔGbind) < 0 listed in Table 1 and selected as the putative targets of aspirin. Next, we analyzed the binding modes and affinities of aspirin to these targets, the structural similarity and pathway enrichment of these targets and clinical outcomes of aspirin.
Table 1. The putative targets with binding free energies calculated by MM-PBSA.
| Gene name | UniProtKB entry | Family | (kcal/mol) |
|---|---|---|---|
| EXOSC3 | Q9NQT5 | RRP40 family | −33.0 |
| MAPK12 | P53778 | Kinase family | −28.6 |
| ITGAL | O43746 | Integrin alpha chain family | −28.0 |
| PTGS2 | P35354 | Prostaglandin G/H synthase family | −20.2 |
| PTGS1 | P23219 | Prostaglandin G/H synthase family | −27.6 |
| PLA2G10 | O15496 | Phospholipase A2 family | −25.7 |
| FBP1 | P09467 | FBPase class 1 family | −25.3 |
| CUL4B | Q13620 | Cullin family | −23.0 |
| MMP12 | P39900 | Peptidase M10A family | −18.6 |
| CDK13 | Q14004 | kinase family | −18.4 |
| TNFAIP6 | P98066 | Hyaluronan-binding protein family | −16.8 |
| PLA2G3 | Q9NZ20 | Phospholipase A2 family | −14.7 |
| HLA-A | O19619 | MHC class I family | −12.1 |
| MOCS3 | O95396 | HesA/MoeB/ThiF family | −12.0 |
| AIDA | Q96BJ3 | AIDA family | −11.1 |
| RAC1 | P63000 | Rho family | −11.0 |
| PLA2G5 | P39877 | Phospholipase A2 family | −10.8 |
| PLA2G1B | P04054 | Phospholipase A2 family | −10.6 |
| PLA2G2A | P14555 | Phospholipase A2 family | −10.6 |
| TNFSF14 | O43557 | Tumor necrosis factor family | −10.3 |
| CHIT1 | Q13231 | Chitotriosidase family | −10.0 |
| EGFLAM | Q63HQ2 | Pikachurin family | −9.2 |
| PLA2G2D | Q9UNK4 | Phospholipase A2 family | −6.0 |
Structural diversity of the putative targets
In order to analyze the structural similarity of the 23 putative targets, each pair of these targets were structurally aligned using the program Combinatorial Extension (CE) (Shindyalov & Bourne, 2001). The targets were considered to be similar if the root-mean-square deviation (RMSD) between two structures is less than 4 Å. A network of targets was generated by linking structurally similar targets (Fig. 2A). The primary targets of aspirin are colored with green, and the newly identified targets are colored with red. Only two proteins HLA class I histocompatibility antigen, A-2 alpha chain (HLA-A) and axin interactor, dorsalization-associated protein (AIDA) clustered with the phospholipase A2 family. Proteins cyclooxygenase-1 and 2 are linked together but not similar with the other proteins. Therefore, the overall structures of the newly identified targets and the primary targets were not similar. It indicates the structural diversity of the 23 putative targets. However, the 23 targets have similar local structures. For example, proteins group IB phospholipase A2 (PLA2G1B) and cyclin-dependent kinase 13 (CDK13) which belong to different protein families have very similar binding sites of aspirin (BSiteAs) (Fig. 2B).
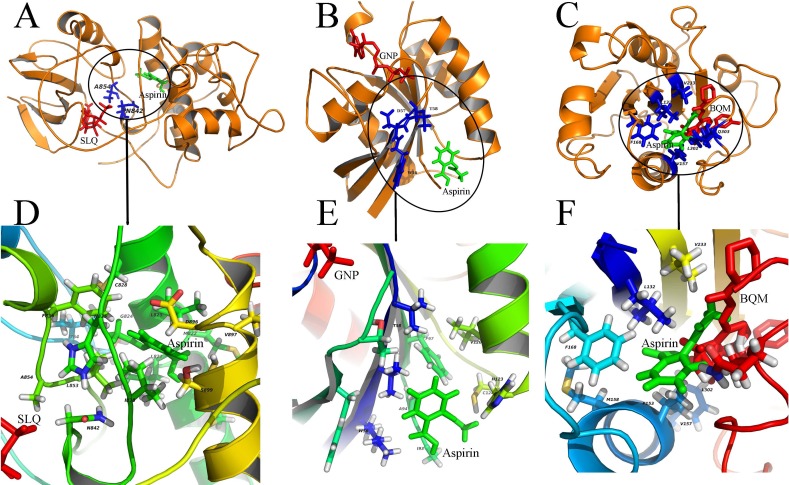
Diverse binding modes of aspirin to the putative targets
In our study, aspirin was docked to the predicted binding sites on putative targets. Results of these docking experiments reveal diverse binding modes of aspirin to these targets (Fig. 3). Some examples are given follows. As a first example, aspirin binds to protein CDK13 with a novel mode compared to ATP-analog inhibitor of the kinase (Fig. 3A). ATP-analog inhibitors exhibit inhibitory activity of kinase by competitive binding to its ATP binding site. In contrast, aspirin binds to CDK13 in the vicinity of the ATP binding site and interact with loops (L1 and L2) which are important for ATP binding. Another example is that aspirin binds to protein ras-related C3 botulinum toxin substrate 1 (RAC1), which is very different from GTP binding (Fig. 3B). Aspirin binds to the other side of RAC1 and interact with the N-terminal part of switch II (sequence 56 WDTAG), which is crucial for interaction between RAC1 and protein Arfaptin (Tarricone et al., 2001). The Arfaptin mediates cross-talk between Rac and Arf signaling pathways. The last example is that aspirin binds to protein integrin alpha-L (ITGAL) in the binding site of its inhibitor BQM (Guckian et al., 2008) (Fig. 3C). The analysis of the binding mode of aspirin to the other 19 putative targets is shown in the Figs. S1–S23. The statistic of 23 putative binding pockets of aspirin is shown in the Fig. S24. The coordinates of 23 putative binding pockets are shown in Table S2. The size of the 23 binding pockets is ranging from 10 to 26 residues, if we define the residues lying within 5 Å from aspirin as binding pockets. The pocket size of aspirin binding to phospholipase A2 (PDBID: 1OXR) and cyclooxygenase-1 (PDBID: 1PTH) is fall in this range. The most used amino acids in pockets are leucine (L), cysteine (C), valine (V), glycine (G), tyrosine (Y), isoleucine (I), alanine (A) and phenylalanine (F). The eight amino acids appeared in the pockets more than 20 times. All the eight amino acids are with hydrophobic side chain except cysteine (C). It suggests that hydrophobic interaction is important for aspirin binding. Additionally, the H-bond is also important for aspirin binding because 78% (18/23) binding pockets formed H-bonds with aspirin. The most used amino acids involved in H-bond formation are aspartic acid (D), lysine (K) and histidine (H). Therefore, the combinations of these charged amino acids (D, K and H) and hydrophobic amino acids (L, V, G, Y, I, A and F) may form the pocket that aspirin prefers to bind to.
Figure 3. Diverse binding modes of aspirin to the putative targets.
The docking experiments reveal diverse binding modes of aspirin to these targets (A) Aspirin binding to protein CDK13 (3LQ5.pdb). (B) Aspirin binding to protein RAC1 (1RYH.pdb). © Aspirin binding to protein ITGAL (3BQM.pdb). The overview and close-up view of the binding mode of aspirin to their putative targets are shown in A-C and D-F, respectively. The close-up view (D-F) show all amino acids in the vicinity of aspirin. Aspirin and the known ligands of the three proteins are colored with green and red, respectively (A-C). The residues involved in binding to both aspirin and the ligands are shown as sticks and colored with blue (A-C). SLQ (A), GNP (B) and BQM © are ATP-analog inhibitor of the kinase CDK13, the substrate of the protein RAC1 and the inhibitor of protein ITGAL, respectively.
The binding affinities of aspirin to putative targets
To obtain accurate estimate of the binding energy of different putative targets with aspirin, MM-PBSA free energy calculation protocol was used. In the combination of the experimental study (Singh et al., 2005) and MM-PBSA free energy calculation, we obtained the estimated entropy change (TΔS = 4.728 kcal/mol) upon aspirin binding. The entropy changes do not have large fluctuations when the same ligand binds to a different acceptor based on the study of Chang & Gilson (2004). Therefore, the entropy changes when aspirin binds to various putative targets was assumed as 4.728 kcal/mol to compare free energies associated with different aspirin binding putative targets. The binding free energies including entropy change for the 23 proteins binding to aspirin were calculated and listed in Table 1. The binding free energies of the 23 proteins with aspirin are varied from −6.0 (group IID secretory phospholipase A2, PLA2G2D) to −33.0 (exosome component 3, EXOSC3) kcal/mol. Overall, the binding free energies for newly identified targets (the average −18.4 kcal/mol) are comparable to that for the primary targets (the average −15.3 kcal/mol).
Pathway enrichment and interaction network of putative targets
Using the DAVID tool, we find that our predicted targets are significantly overrepresented for several pathways (p < 0.01) (Table 2). Some of these pathways are strongly involved in inflammation, cardiovascular disease and cancer, such as VEGF signaling, Fc epsilon RI signaling, arachidonic acid metabolism, gonadotropin-releasing hormone (GnRH) signaling and MAPK signaling. To illustrate the relationship between the putative targets and their cellular effect, an integrated interaction network of targets-cellular effect based on their associated pathways was constructed (Fig. 4). The interactions between predicted targets and the major effects involved in cancer development, inflammation and cardiovascular disease were present in this network. Represented by green circles in the network, the predicted targets regulate VEGF, epsilon RI signaling, arachidonic acid metabolism, and MAPK pathways through interactions with other proteins (gray circles) connecting the pathways. Inhibition of predicted targets is expected to down-regulate these pathways, and then prevent inflammation and decrease the risk of cardiovascular disease and cancer.
Table 2. The pathways significantly overrepresented by our predicted targets (p < 0.01).
| Pathway | Count | Percentage | Adjust P-valuea | Referenceb |
|---|---|---|---|---|
| VEGF signaling pathway | 9 | 40.9 | 4.60E−10 | Cross et al. (2003) |
| Arachidonic acid metabolism | 8 | 36.4 | 2.00E−09 | Spector et al. (2004) |
| Fc epsilon RI signaling pathway | 8 | 36.4 | 1.50E−08 | Kawakami & Galli (2002) |
| Alpha-Linolenic acid metabolism | 6 | 27.3 | 1.10E−08 | Hamberg et al. (2003) |
| Linoleic acid metabolism | 6 | 27.3 | 1.00E−07 | Shureiqi et al. (2003) |
| Ether lipid metabolism | 6 | 27.3 | 2.80E−07 | Nagan & Zoeller (2001) |
| GnRH signaling pathway | 7 | 31.8 | 1.40E−06 | Ruf & Sealfon (2004) |
| Glycerophospholipid metabolism | 6 | 27.3 | 6.40E−06 | Racenis et al. (1992) |
| Long-term depression | 6 | 27.3 | 6.10E−06 | Ito (2002) |
| MAPK signaling pathway | 8 | 36.4 | 2.30E−05 | Dent et al. (2003) |
| Vascular smooth muscle contraction | 6 | 27.3 | 5.50E−05 | Kim et al. (2008) |
Notes.
P-value was adjusted using Benjamini & Hochberg method.
The literature references link the refined putative targets with pathways.
Figure 4. An integrated interaction network of targets-cellular effect based on their associated pathways.
Predicted targets, represented by green circles in the network, regulate VEGF, epsilon RI signaling, arachidonic acid metabolism, and MAPK pathways through direct or indirect interactions with intermediate proteins (gray circles) connecting the pathways. Red squares represent cellular effects. Black lines represent activation.
We use the protein RAC1 as an example to show how inhibition by aspirin leads to anti-inflammation and anti-cancer effect. RAC1, which belongs to the Rho GTPase family, can regulate the machinery that controls the assembly and disassembly of cytoskeletal elements (Bid et al., 2013). RAC1 is required for the VEGF-induced increase in vascular permeability (Monaghan-Benson & Burridge, 2009). Increased vascular permeability is often observed in inflammation (Wilhelm, 1973). Therefore, RAC1 can promote the development of inflammation through VEGF and Fc epsilon RI signaling pathway. Furthermore, RAC1 is involved in gonadotropins expression, cytokine transcription and actin reorganization, which play a critical role for proliferation, migration and evading apoptosis of cancer cell. The inhibition of RAC1 by aspirin will attenuate these processes, which may provide an alternative explanation for the anti-inflammation and cancer effect of aspirin.
Discussion
The overall structures of the 23 putative targets of aspirin identified in this study are very different (Fig. 2A). However, the 23 targets have similar local structures. It indicates the power of the CMASA for detecting and comparing binding sites similarities from whole structures of proteins. Further, the CMASA is not only highly accurate but also sensitive and fast for detecting the binding pocket similarities (Li & Huang, 2010). It can be applied in annotating and detecting similar binding pocket from two proteins which are not homologous (Flores, Sotelo-Mundo & Brizuela, 2014; Li & Huang, 2010).
Of these targets, 14 targets are new and need experimental validation. We have performed literature research about aspirin and the 14 new targets. Although no direct evidence for binding of aspirin to these 14 new targets was found in the literature, possible associations with aspirin or aspirin metabolites are supported by direct or indirect evidence for half of the targets (Table 3). The seven new targets (MAPK12, ITGAL, MMP12, TNFAIP6, HLA-A, RAC1, and TNFSF14) were reported to be associated with aspirin. Slattery, Lundgreen & Wolff (2012) evaluated genetic variation of MAPK12 and colon and rectal cancer risk using data from population-based case-control studies. They found that for rectal cancer, aspirin users had a greater reduced risk if patients had a variant allele of MAP3K1 rs2548663 or MAPK12 rs2272857. In addition, another study reported that the gene expression of MAPK12 showed a significant down-regulation in the colorectal cancer cell line SW480 treated with 1 mM aspirin (Dibra et al., 2010). The gene expression of MMP12, TNFAIP6 and RAC1 also showed differences between pre- and post-aspirin treatment (Choi et al., 2005; Hardwick et al., 2004; Jiang et al., 2015). In the future, we will select several identified targets in this study to perform experimental validation.
Table 3. Literature evidence for the association between aspirin and the new targets.
| Gene name | Protein name | Evidence | Reference |
|---|---|---|---|
| MAPK12 | Mitogen-activated protein kinase 12 | MAPK12 gene polymorphism affect the efficacy of aspirin for prevention of rectal cancer; Treatment of the cell line SW480 with 1 mM aspirin for 48 h caused a significant down-regulation of MAPK12 expression. | Dibra et al., 2010; Slattery, Lundgreen & Wolff (2012) |
| ITGAL | Integrin alpha-L | ITGAL gene is hypomethylated and associated with aspirin hypersensitivity in asthma. | Cheong et al. (2011) |
| MMP12 | Macrophage metalloelastase | Aspirin inhibits LPS-induced MMP12 gene expression in human bronchial epithelial cells. | Jiang et al. (2015) |
| TNFAIP6 | Tumor necrosis factor-inducible protein 6 | TNFAIP6 gene expression was up-regulated 2.33 fold by aspirin treatment in human peripheral blood mononuclear cells. | Choi et al. (2005) |
| HLA-A | MHC class I antigen | HLA-DQw2 allele is involved in the pathogenesis of aspirin-sensitive asthma. | Mullarkey et al. (1986) |
| RAC1 | Ras-related C3 botulinum toxin substrate 1 | RAC1 gene is highly induced in the HT29 colon cancer cell by aspirin. This study pointed towards a role for RAC1 in the action of aspirin in colon cancer. | Hardwick et al. (2004) |
| TNFSF14 | Tumor necrosis factor ligand superfamily member 14 | Aspirin significantly reduced plasma levels of LIGHT in 12 healthy controls when given for 7 days (160 mg once a day). | Otterdal et al. (2006) |
We are not sure whether the acetylation will certainly occur when aspirin exerts the effects other than as an anti-inflammatory. The primary action mechanism of aspirin is covalent binding to COX-1. There are also some evidences show aspirin may exhibit non-covalent binding (Mir et al., 2009; Singh et al., 2005). We analyzed the possible acetylation sites in the binding pockets of all 23 targets. We found 78% (18/23) binding pockets have possible acetylation site if we assume that the three amino acids lysine (K), serine (S) and threonine (T) can be acetylated. This analysis suggests the identified targets in our study may be acetylated after binding of aspirin.
Identification of putative targets of aspirin is restricted by the available data of the 3-D structures of human protein. We used all available structural data to construct our query database. Our query database contains totally 17,425 non-redundant structures of human protein from three sources: RCSB PDB database (Rose et al., 2011), Structure atlas of human genome (SAHG) (Motono et al., 2011) and GPCR Research Database (GPCRRD) (Zhang & Zhang, 2010). With the increase number of crystal structures in the future, other new targets of aspirin may be identified. Another limitation of this study is that aspirin can bind to different targets with same or different binding sites. For example, the binding sites of aspirin to PLA2 and COX-1 are different. Therefore, it is possible to miss other potential targets to which aspirin can bind. Therefore, we used all available aspirin-protein complexes in our study.
The combination of multiple methods in structural bioinformatics and system biology can improve the prediction of protein target (Grinter & Zou, 2014). Kumar et al. (2014a) used pseudoreceptor-based pharmacophore to predict probable protein targets and explore the protein structural profile of Zea mays. They suggested that the combination of total probabilities and docking energies can increase the confidence in prediction of probable protein targets using docking methods. Kumar et al., (2014b) also used receptor-centric and ligand-centric methods for compound prioritization. Furthermore, they combined both inverse docking and ligand-based similarity search to predict the protein targets of kinetin (Kumar et al., 2015). In this study, we combined structural bioinformatics and inverse docking to predict the targets of aspirin. We also compared our methods with the PharmMapper tool (Liu et al., 2010). The top 20 targets identified by PharmMapper tool are shown in Table S3. The targets COX-1 and COX-1 were not found in the top 20 list. Only the member in phospholipase A2 family was found in the rank 17. Therefore, for the prediction of aspirin targets, the PharmMapper tool may be not suitable. In future, we will combine multiple available methods including those of Kumar et al. to further analyze the identified targets in this study.
Aspirin, as a common household drug, has been around for more than a century. Its basic mechanism of anti-inflammation is well documented (Vane, 1971), yet newer beneficial effects keep on adding to ever-expanding therapeutic repertoire. Aspirin is used for the prevention of cardiovascular disease and various types of cancer (Alfonso et al., 2014; Dovizio et al., 2013; Dovizio et al., 2012; Jacobs et al., 2007). However, the molecular mechanisms underlying these effects of aspirin remain unclear. Based on the primary targets of aspirin, the traditional explanation for these effects is that both the cardioprotective and cancer preventive effects of aspirin may be attributed to inhibition of platelet activation (Alfonso et al., 2014; Dovizio et al., 2013; Su et al., 2014; Thun, Jacobs & Patrono, 2012). Additionally, aspirin may restore the balance of pro- and anti-angiogenic factors released from platelet and modify tumor microenvironment via antiplatelet effect (Su et al., 2014).
Our study provides an alternative explanation for the pleiotropic effects of aspirin in various diseases. The results suggest aspirin has the capacity to modulate various targets in different protein family, such as peptidase, protein kinase, prostaglandin synthase, phospholipase. As shown in the Fig. 4, aspirin can not only inhibit COX-1 and 2 but also modulate the proteins ITGAL, RAC1, MAPK12 and so on. These targets are involved in a number of biology processes, such as angiogenesis, inflammation, cell proliferation, evading apoptosis, migration (Fig. 4). Therefore, the preventive effect of aspirin for cardiovascular disease and various types of cancer may be due to modulation of these proteins. Of course, additional experimental studies are needed to validate our results. Our study provides some new directions for experimental verification about this potential mechanism of action of aspirin. With more studies on the mechanisms of action in the future, the unknown side of aspirin will be uncovered.
In conclusion, we characterized the target profile of aspirin in human proteome by integrating methods from local structure detecting, molecular docking, and free energy calculation. These targets have diverse folds and are from different protein family. However, they have similar aspirin-binding pockets. The binding free energy with aspirin for newly identified targets is comparable to that for the primary targets. Pathway analysis revealed that the targets were enriched in several pathways such as VEGF signaling, Fc epsilon RI signaling and Arachidonic acid metabolism, which are strongly involved in inflammation, cardiovascular disease and cancer. Therefore, the predicted target profile of aspirin suggests a new explanation for the ability of aspirin to prevent these diseases. Our findings enable us to understand aspirin and its efficacy of disease prevention in a systematic and global view.
Supplemental Information
Of these proteins, 23 proteins were identified as putative targets of aspirin after molecular docking and binding free energy calculation.
The raw data contains all strucures of the identified 79 proteins. The Protocols show how to prepare protein strucure and run CDOCKER.
Acknowledgments
We thank our colleagues, Drs. Zi-Zhang Sheng and Dong-Qiang Cheng and Yu-Qi Zhao for helpful comments on the manuscript. We also thank four anonymous reviewers for valuable comments.
Funding Statement
This work was supported by the National Basic Research Program of China (Grant No. 2013CB835100) and the National Natural Science Foundation of China (Grant No. 31401142 to D.S.X, NO. 31401137 to G.H.L and No. 31123005 to J.F.H). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Gong-Hua Li, Email: ligonghua@mail.kiz.ac.cn.
Jing-Fei Huang, Email: huangjf@mail.kiz.ac.cn.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Shao-Xing Dai conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Wen-Xing Li performed the experiments, analyzed the data, reviewed drafts of the paper.
Gong-Hua Li conceived and designed the experiments, performed the experiments, analyzed the data, reviewed drafts of the paper.
Jing-Fei Huang conceived and designed the experiments, analyzed the data, reviewed drafts of the paper.
Data Availability
The following information was supplied regarding data availability:
The research in this article did not generate any raw data.
References
- Alfonso et al. (2014).Alfonso L, Ai G, Spitale RC, Bhat GJ. Molecular targets of aspirin and cancer prevention. British Journal of Cancer. 2014;111:61–67. doi: 10.1038/bjc.2014.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avivi et al. (2012).Avivi D, Moshkowitz M, Detering E, Arber N. The role of low-dose aspirin in the prevention of colorectal cancer. Expert Opinion on Therapeutic Targets. 2012;16:S51–S62. doi: 10.1517/14728222.2011.647810. [DOI] [PubMed] [Google Scholar]
- Balsinde et al. (1999).Balsinde J, Balboa MA, Insel PA, Dennis EA. Regulation and inhibition of phospholipase A(2) Annual Review of Pharmacology and Toxicology. 1999;39:175–189. doi: 10.1146/annurev.pharmtox.39.1.175. [DOI] [PubMed] [Google Scholar]
- Berger, Brown & Becker (2008).Berger JS, Brown DL, Becker RC. Low-dose aspirin in patients with stable cardiovascular disease: a meta-analysis. The American Journal of Medicine. 2008;121:43–49. doi: 10.1016/j.amjmed.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Bid et al. (2013).Bid HK, Roberts RD, Manchanda PK, Houghton PJ. RAC1: an emerging therapeutic option for targeting cancer angiogenesis and metastasis. Molecular Cancer Therapeutics. 2013;12:1925–1934. doi: 10.1158/1535-7163.MCT-13-0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burn et al. (2011).Burn J, Gerdes AM, Macrae F, Mecklin JP, Moeslein G, Olschwang S, Eccles D, Evans DG, Maher ER, Bertario L, Bisgaard ML, Dunlop MG, Ho JWC, Hodgson SV, Lindblom A, Lubinski J, Morrison PJ, Murday V, Ramesar R, Side L, Scott RJ, Thomas HJW, Vasen HF, Barker G, Crawford G, Elliott F, Movahedi M, Pylvanainen K, Wijnen JT, Fodde R, Lynch HT, Mathers JC, Bishop DT, Investigators C. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet. 2011;378:2081–2087. doi: 10.1016/S0140-6736(11)61049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang & Gilson (2004).Chang CE, Gilson MK. Free energy, entropy, and induced fit in host-guest recognition: calculations with the second-generation mining minima algorithm. Journal of the American Chemical Society. 2004;126:13156–13164. doi: 10.1021/ja047115d. [DOI] [PubMed] [Google Scholar]
- Cheong et al. (2011).Cheong HS, Park SM, Kim MO, Park JS, Lee JY, Byun JY, Park BL, Shin HD, Park CS. Genome-wide methylation profile of nasal polyps: relation to aspirin hypersensitivity in asthmatics. Allergy. 2011;66:637–644. doi: 10.1111/j.1398-9995.2010.02514.x. [DOI] [PubMed] [Google Scholar]
- Choi et al. (2005).Choi S, Park HS, Cheon MS, Lee K. Expression profile analysis of human peripheral blood mononuclear cells in response to aspirin. Archivum Immunologiae et Therapiae Experimentalis. 2005;53:151–158. [PubMed] [Google Scholar]
- Cross et al. (2003).Cross MJ, Dixelius J, Matsumoto T, Claesson-Welsh L. VEGF-receptor signal transduction. Trends in Biochemical Sciences. 2003;28:488–494. doi: 10.1016/S0968-0004(03)00193-2. [DOI] [PubMed] [Google Scholar]
- Deng & Fang (2012).Deng HY, Fang Y. Aspirin metabolites are GPR35 agonists. Naunyn-Schmiedebergs Archives of Pharmacology. 2012;385:729–737. doi: 10.1007/s00210-012-0752-0. [DOI] [PubMed] [Google Scholar]
- Dent et al. (2003).Dent P, Yacoub A, Fisher PB, Hagan MP, Grant S. MAPK pathways in radiation responses. Oncogene. 2003;22:5885–5896. doi: 10.1038/sj.onc.1206701. [DOI] [PubMed] [Google Scholar]
- Dibra et al. (2010).Dibra HK, Brown JE, Hooley P, Nicholl ID. Aspirin and alterations in DNA repair proteins in the SW480 colorectal cancer cell line. Oncology Reports. 2010;24:37–46. doi: 10.3892/or_00000826. [DOI] [PubMed] [Google Scholar]
- Din et al. (2012).Din FVN, Valanciute A, Houde VP, Zibrova D, Green KA, Sakamoto K, Alessi DR, Dunlop MG. Aspirin inhibits mTOR signaling, activates AMP-activated protein kinase, and induces autophagy in colorectal cancer cells. Gastroenterology. 2012;142:1504–1515. doi: 10.1053/j.gastro.2012.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovizio et al. (2013).Dovizio M, Bruno A, Tacconelli S, Patrignani P. Prospects for chemoprevention of colorectal neoplasia. New York: Springer; 2013. Mode of action of aspirin as a chemopreventive agent; pp. 39–65. [DOI] [PubMed] [Google Scholar]
- Dovizio et al. (2012).Dovizio M, Tacconelli S, Sostres C, Ricciotti E, Patrignani P. Mechanistic and pharmacological issues of aspirin as an anticancer agent. Pharmaceuticals. 2012;5:1346–1371. doi: 10.3390/ph5121346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores, Sotelo-Mundo & Brizuela (2014).Flores DI, Sotelo-Mundo RR, Brizuela CA. A simple extension to the CMASA method for the prediction of catalytic residues in the presence of single point mutations. PLoS ONE. 2014;9:e1791. doi: 10.1371/journal.pone.0108513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghooi, Thatte & Joshi (1995).Ghooi RB, Thatte SM, Joshi PS. The mechanism of action of aspirin–is there anything beyond cyclo-oxygenase? Medical Hypotheses. 1995;44:77–80. doi: 10.1016/0306-9877(95)90073-X. [DOI] [PubMed] [Google Scholar]
- Grinter & Zou (2014).Grinter SZ, Zou XQ. Challenges, applications, and recent advances of protein-ligand docking in structure-based drug design. Molecules. 2014;19:10150–10176. doi: 10.3390/molecules190710150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guckian et al. (2008).Guckian KM, Lin EY, Silvian L, Friedman JE, Chin D, Scott DM. Design and synthesis of a series of meta aniline-based LFA-1 ICAM inhibitors. Bioorganic & Medicinal Chemistry Letters. 2008;18:5249–5251. doi: 10.1016/j.bmcl.2008.08.061. [DOI] [PubMed] [Google Scholar]
- Hamberg et al. (2003).Hamberg M, Sanz A, Rodriguez MJ, Calvo AP, Castresana C. Activation of the fatty acid alpha-dioxygenase pathway during bacterial infection of tobacco leaves. Formation of oxylipins protecting against cell death. Journal of Biological Chemistry. 2003;278:51796–51805. doi: 10.1074/jbc.M310514200. [DOI] [PubMed] [Google Scholar]
- Hardwick et al. (2004).Hardwick JC, Van Santen M, Van den Brink GR, Van Deventer SJ, Peppelenbosch MP. DNA array analysis of the effects of aspirin on colon cancer cells: involvement of Rac1. Carcinogenesis. 2004;25:1293–1298. doi: 10.1093/carcin/bgh118. [DOI] [PubMed] [Google Scholar]
- Hassan et al. (2012).Hassan C, Rex DK, Cooper GS, Zullo A, Launois R, Benamouzig R. Primary prevention of colorectal cancer with low-dose aspirin in combination with endoscopy: a cost-effectiveness analysis. Gut. 2012;61:1172–1179. doi: 10.1136/gutjnl-2011-300206. [DOI] [PubMed] [Google Scholar]
- Huang et al. (2010).Huang Y, Niu B, Gao Y, Fu L, Li W. CD-HIT Suite: a web server for clustering and comparing biological sequences. Bioinformatics. 2010;26:680–682. doi: 10.1093/bioinformatics/btq003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Sherman & Lempicki (2009).Huang DW, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nature Protocols. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- Ito (2002).Ito M. The molecular organization of cerebellar long-term depression. Nature Reviews Neuroscience. 2002;3:896–902. doi: 10.1038/nrn962. [DOI] [PubMed] [Google Scholar]
- Jacobs et al. (2007).Jacobs EJ, Thun MJ, Bain EB, Rodriguez C, Henley SJ, Calle EE. A large cohort study of long-term daily use of adult-strength aspirin and cancer incidence. Journal of the National Cancer Institute. 2007;99:608–615. doi: 10.1093/jnci/djk132. [DOI] [PubMed] [Google Scholar]
- Jiang et al. (2015).Jiang R, Wei L, Zhu M, Wu J, Wang L. Aspirin inhibits LPS-induced expression of PI3K/Akt, ERK, NF-kappaB, CX3CL1, and MMPs in human bronchial epithelial cells. Inflammation. 2015:1–8. doi: 10.1007/s10753-015-0289-8. Epub ahead of print Dec 04 2015. [DOI] [PubMed] [Google Scholar]
- Kawakami & Galli (2002).Kawakami T, Galli SJ. Regulation of mast-cell and basophil function and survival by IgE. Nature Reviews Immunology. 2002;2:773–786. doi: 10.1038/nri914. [DOI] [PubMed] [Google Scholar]
- Kim et al. (2008).Kim HR, Appel S, Vetterkind S, Gangopadhyay SS, Morgan KG. Smooth muscle signalling pathways in health and disease. Journal of Cellular and Molecular Medicine. 2008;12:2165–2180. doi: 10.1111/j.1582-4934.2008.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollman et al. (2000).Kollman PA, Massova I, Reyes C, Kuhn B, Huo SH, Chong L, Lee M, Lee T, Duan Y, Wang W, Donini O, Cieplak P, Srinivasan J, Case DA, Cheatham TE. Calculating structures and free energies of complex molecules: combining molecular mechanics and continuum models. Accounts of Chemical Research. 2000;33:889–897. doi: 10.1021/ar000033j. [DOI] [PubMed] [Google Scholar]
- Kuhn et al. (2005).Kuhn B, Gerber P, Schulz-Gasch T, Stahl M. Validation and use of the MM-PBSA approach for drug discovery. Journal of Medicinal Chemistry. 2005;48:4040–4048. doi: 10.1021/jm049081q. [DOI] [PubMed] [Google Scholar]
- Kumar et al. (2014a).Kumar SP, Jha PC, Pandya HA, Jasrai YT. Implementation of pseudoreceptor-based pharmacophore queries in the prediction of probable protein targets: explorations in the protein structural profile of Zea mays. Molecular BioSystems. 2014a;10:1833–1844. doi: 10.1039/C4MB00058G. [DOI] [PubMed] [Google Scholar]
- Kumar et al. (2014b).Kumar SP, Pandya HA, Desai VH, Jasrai YT. Compound prioritization from inverse docking experiment using receptor- centric and ligandcentric methods: a case study on Plasmodium falciparum Fab enzymes. Journal of Molecular Recognition. 2014b;27:215–229. doi: 10.1002/jmr.2353. [DOI] [PubMed] [Google Scholar]
- Kumar et al. (2015).Kumar SP, Parmar VR, Jasrai YT, Pandya HA. Prediction of protein targets of kinetin using in silico and in vitro methods: a case study on spinach seed germination mechanism. Journal of Chemical Biology. 2015;8:95–105. doi: 10.1007/s12154-015-0135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li & Huang (2010).Li GH, Huang JF. CMASA: an accurate algorithm for detecting local protein structural similarity and its application to enzyme catalytic site annotation. BMC Bioinformatics. 2010;11:439. doi: 10.1186/1471-2105-11-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu et al. (2010).Liu X, Ouyang S, Yu B, Liu Y, Huang K, Gong J, Zheng S, Li Z, Li H, Jiang H. PharmMapper server: a web server for potential drug target identification using pharmacophore mapping approach. Nucleic Acids Research. 2010;38:W609–W614. doi: 10.1093/nar/gkq300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mir et al. (2009).Mir R, Singh N, Vikram G, Kumar RP, Sinha M, Bhushan A, Kaur P, Srinivasan A, Sharma S, Singh TP. The structural basis for the prevention of nonsteroidal antiinflammatory drug-induced gastrointestinal tract damage by the C-lobe of bovine colostrum lactoferrin. Biophysical Journal. 2009;97:3178–3186. doi: 10.1016/j.bpj.2009.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaghan-Benson & Burridge (2009).Monaghan-Benson E, Burridge K. The regulation of vascular endothelial growth factor-induced microvascular permeability requires Rac and reactive oxygen species. Journal of Biological Chemistry. 2009;284:25602–25611. doi: 10.1074/jbc.M109.009894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motono et al. (2011).Motono C, Nakata J, Koike R, Shimizu K, Shirota M, Amemiya T, Tomii K, Nagano N, Sakaya N, Misoo K, Sato M, Kidera A, Hiroaki H, Shirai T, Kinoshita K, Noguchi T, Ota M. SAHG, a comprehensive database of predicted structures of all human proteins. Nucleic Acids Research. 2011;39:D487–D493. doi: 10.1093/nar/gkq1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullarkey et al. (1986).Mullarkey MF, Thomas PS, Hansen JA, Webb DR, Nisperos B. Association of aspirin-sensitive asthma with HLA-DQw2. The American Review of Respiratory Disease. 1986;133:261–263. doi: 10.1164/arrd.1986.133.2.261. [DOI] [PubMed] [Google Scholar]
- Nagan & Zoeller (2001).Nagan N, Zoeller RA. Plasmalogens: biosynthesis and functions. Progress in Lipid Research. 2001;40:199–229. doi: 10.1016/S0163-7827(01)00003-0. [DOI] [PubMed] [Google Scholar]
- Nemerovski et al. (2012).Nemerovski CW, Salinitri FD, Morbitzer KA, Moser LR. Aspirin for primary prevention of cardiovascular disease events. Pharmacotherapy. 2012;32:1020–1035. doi: 10.1002/phar.1127. [DOI] [PubMed] [Google Scholar]
- Otterdal et al. (2006).Otterdal K, Smith C, Oie E, Pedersen TM, Yndestad A, Stang E, Endresen K, Solum NO, Aukrust P, Damas JK. Platelet-derived LIGHT induces inflammatory responses in endothelial cells and monocytes. Blood. 2006;108:928–935. doi: 10.1182/blood-2005-09-010629. [DOI] [PubMed] [Google Scholar]
- Racenis et al. (1992).Racenis PV, Lai JL, Das AK, Mullick PC, Hajra AK, Greenberg ML. The acyl dihydroxyacetone phosphate pathway enzymes for glycerolipid biosynthesis are present in the yeast Saccharomyces cerevisiae. Journal of Bacteriology. 1992;174:5702–5710. doi: 10.1128/jb.174.17.5702-5710.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raju et al. (2011).Raju N, Sobieraj-Teague M, Hirsh J, O’Donnell M, Eikelboom J. Effect of aspirin on mortality in the primary prevention of cardiovascular disease. The American Journal of Medicine. 2011;124:621–629. doi: 10.1016/j.amjmed.2011.01.018. [DOI] [PubMed] [Google Scholar]
- Rose et al. (2011).Rose PW, Beran B, Bi CX, Bluhm WF, Dimitropoulos D, Goodsell DS, Prlic A, Quesada M, Quinn GB, Westbrook JD, Young J, Yukich B, Zardecki C, Berman HM, Bourne PE. The RCSB protein data bank: redesigned web site and web services. Nucleic Acids Research. 2011;39:D392–D401. doi: 10.1093/nar/gkq1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothwell et al. (2010).Rothwell PM, Wilson M, Elwin CE, Norrving B, Algra A, Warlow CP, Meade TW. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet. 2010;376:1741–1750. doi: 10.1016/S0140-6736(10)61543-7. [DOI] [PubMed] [Google Scholar]
- Rothwell et al. (2012).Rothwell PM, Wilson M, Price JF, Belch JFF, Meade TW, Mehta Z. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. Lancet. 2012;379:1591–1601. doi: 10.1016/S0140-6736(12)60209-8. [DOI] [PubMed] [Google Scholar]
- Ruf & Sealfon (2004).Ruf F, Sealfon SC. Genomics view of gonadotrope signaling circuits. Trends in Endocrinology & Metabolism. 2004;15:331–338. doi: 10.1016/j.tem.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Schnell, Erbach & Hummel (2012).Schnell O, Erbach M, Hummel M. Primary and secondary prevention of cardiovascular disease in diabetes with aspirin. Diabetes & Vascular Disease Research. 2012;9:245–255. doi: 10.1177/1479164112441486. [DOI] [PubMed] [Google Scholar]
- Sclabas et al. (2005).Sclabas GM, Uwagawa T, Schmidt C, Hess KR, Evans DB, Evans DB, Abbruzzese JL, Chiao PJ. Nuclear factor kappa B activation is a potential target for preventing pancreatic carcinoma by aspirin. Cancer. 2005;103:2485–2490. doi: 10.1002/cncr.21075. [DOI] [PubMed] [Google Scholar]
- Shindyalov & Bourne (2001).Shindyalov I, Bourne P. CE: a resource to compute and review 3-D protein structure alignments. Nucleic Acids Research. 2001;29:228–229. doi: 10.1093/nar/29.1.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shureiqi et al. (2003).Shureiqi I, Jiang W, Zuo X, Wu Y, Stimmel JB, Leesnitzer LM, Morris JS, Fan HZ, Fischer SM, Lippman SM. The 15-lipoxygenase-1 product 13-S-hydroxyoctadecadienoic acid down-regulates PPAR-delta to induce apoptosis in colorectal cancer cells. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:9968–9973. doi: 10.1073/pnas.1631086100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh et al. (2005).Singh RK, Ethayathulla AS, Jabeen T, Sharma S, Kaur P, Singh TP. Aspirin induces its anti-inflammatory effects through its specific binding to phospholipase A(2): crystal structure of the complex formed between phospholipase A(2) and aspirin at 1.9 angstrom resolution. Journal of Drug Targeting. 2005;13:113–119. doi: 10.1080/10611860400024078. [DOI] [PubMed] [Google Scholar]
- Slattery, Lundgreen & Wolff (2012).Slattery ML, Lundgreen A, Wolff RK. MAP kinase genes and colon and rectal cancer. Carcinogenesis. 2012;33:2398–2408. doi: 10.1093/carcin/bgs305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spector et al. (2004).Spector AA, Fang X, Snyder GD, Weintraub NL. Epoxyeicosatrienoic acids (EETs): metabolism and biochemical function. Progress in Lipid Research. 2004;43:55–90. doi: 10.1016/S0163-7827(03)00049-3. [DOI] [PubMed] [Google Scholar]
- Su et al. (2014).Su BB, Chen JH, Shi H, Chen QQ, Wan J. Aspirin may modify tumor microenvironment via antiplatelet effect. Medical Hypotheses. 2014;83:148–150. doi: 10.1016/j.mehy.2014.05.007. [DOI] [PubMed] [Google Scholar]
- Tarricone et al. (2001).Tarricone C, Xiao B, Justin N, Walker PA, Rittinger K, Gamblin SJ, Smerdon SJ. The structural basis of Arfaptin-mediated cross-talk between Rac and Arf signalling pathways. Nature. 2001;411:215–219. doi: 10.1038/35075620. [DOI] [PubMed] [Google Scholar]
- Thun, Jacobs & Patrono (2012).Thun MJ, Jacobs EJ, Patrono C. The role of aspirin in cancer prevention. Nature Reviews Clinical Oncology. 2012;9:259–267. doi: 10.1038/nrclinonc.2011.199. [DOI] [PubMed] [Google Scholar]
- Touqui & Alaoui-El-Azher (2001).Touqui L, Alaoui-El-Azher M. Mammalian secreted phospholipases A2 and their pathophysiological significance in inflammatory diseases. Current Molecular Medicine. 2001;1:739–754. doi: 10.2174/1566524013363258. [DOI] [PubMed] [Google Scholar]
- Vane (1971).Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nature-New Biology. 1971;231:232–235. doi: 10.1038/newbio231232a0. [DOI] [PubMed] [Google Scholar]
- Vane & Botting (2003).Vane JR, Botting RM. The mechanism of action of aspirin. Thrombosis Research. 2003;110:255–258. doi: 10.1016/S0049-3848(03)00379-7. [DOI] [PubMed] [Google Scholar]
- Wilhelm (1973).Wilhelm DL. Mechanisms responsible for increased vascular permeability in acute inflammation. Agents Actions. 1973;3:297–306. doi: 10.1007/BF01986484. [DOI] [PubMed] [Google Scholar]
- Wu et al. (2003).Wu GS, Robertson DH, Brooks CL, Vieth M. Detailed analysis of grid-based molecular docking: A case study of CDOCKER - A CHARMm-based MD docking algorithm. Journal of Computational Chemistry. 2003;24:1549–1562. doi: 10.1002/jcc.10306. [DOI] [PubMed] [Google Scholar]
- Younis et al. (2010).Younis N, Williams S, Ammori B, Soran H. Role of aspirin in the primary prevention of cardiovascular disease in diabetes mellitus: a meta-analysis. Expert Opinion on Pharmacotherapy. 2010;11:1459–1466. doi: 10.1517/14656561003792538. [DOI] [PubMed] [Google Scholar]
- Zhang & Zhang (2010).Zhang J, Zhang Y. GPCRRD: G protein-coupled receptor spatial restraint database for 3D structure modeling and function annotation. Bioinformatics. 2010;26:3004–3005. doi: 10.1093/bioinformatics/btq563. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Of these proteins, 23 proteins were identified as putative targets of aspirin after molecular docking and binding free energy calculation.
The raw data contains all strucures of the identified 79 proteins. The Protocols show how to prepare protein strucure and run CDOCKER.
Data Availability Statement
The following information was supplied regarding data availability:
The research in this article did not generate any raw data.