Abstract
Background:
There has been a substantial increase in the amount of systematic reviews and meta-analyses published on the anterior cruciate ligament (ACL).
Purpose:
To quantify the number of systematic reviews and meta-analyses published on the ACL in the past decade and to provide an overall summary of this literature.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review of all ACL-related systematic reviews and meta-analyses published between January 2004 and September 2014 was performed using PubMed, MEDLINE, and the Cochrane Database. Narrative reviews and non-English articles were excluded.
Results:
A total of 1031 articles were found, of which 240 met the inclusion criteria. Included articles were summarized and divided into 17 topics: anatomy, epidemiology, prevention, associated injuries, diagnosis, operative versus nonoperative management, graft choice, surgical technique, fixation methods, computer-assisted surgery, platelet-rich plasma, rehabilitation, return to play, outcomes assessment, arthritis, complications, and miscellaneous.
Conclusion:
A summary of systematic reviews on the ACL can supply the surgeon with a single source for the most up-to-date synthesis of the literature.
Keywords: anterior cruciate ligament, surgery, systematic review, meta-analysis
In an effort to help physicians stay current on the most recent evidence-based findings, the past decade has seen an explosion in the number of systematic reviews and meta-analyses. The purposes of these articles are to provide the most up-to-date information on a given topic by synthesizing all of the available evidence using rigorous methods. However, as these types of studies increase, it can be difficult for providers to even stay abreast of this literature. Anterior cruciate ligament (ACL) injury and surgery is one of the most researched subjects in the sports medicine literature, with 469 articles found using a simple PubMed search in 2014 alone. To assist researchers and providers as they strive to remain current on this topic, we sought to quantify the number of systematic reviews and meta-analyses published on the ACL in the past decade and provide a summary of this literature for easy reference.
Methods
A systematic review was performed of all ACL-related systematic reviews and meta-analyses published between January 2004 and September 2014. The search engines used include PubMed, MEDLINE, and the Cochrane Database of Systematic Reviews. The search terms were anterior cruciate ligament or ACL in combination with systematic review or meta-analysis. Exclusion criteria were articles not published in English and narrative review articles that did not report a systematic literature search. Two reviewers independently conducted the same literature search, and the results of each search were compared. Three authors reviewed each study in detail and summarized the study results. The articles were divided into 17 topics: anatomy, epidemiology, prevention, associated injuries, diagnosis, operative versus nonoperative management, graft choice, surgical technique, fixation methods, computer-assisted surgery (CAS), platelet-rich plasma (PRP), rehabilitation, return to play, outcomes assessment, arthritis, complications, and miscellaneous.
Results
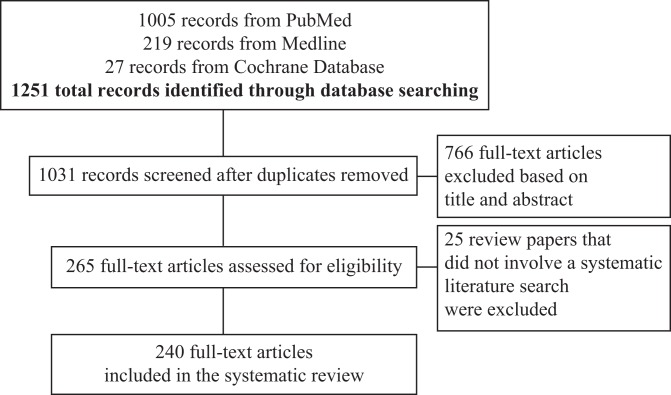
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart is presented in Figure 1.131 A total of 1031 articles were identified, and 265 articles were reviewed and assessed for inclusion. The number of articles included for each ACL topic are listed in Table 1.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart of literature search process.
TABLE 1.
Number of Articles by ACL Topica
| Topic of Systematic Review | Articles Found, n |
|---|---|
| Anatomy | 4 |
| Epidemiology | 19 |
| Prevention | 22 |
| Associated injuries | 12 |
| Diagnosis | 4 |
| Nonoperative vs operative management | 16 |
| Graft choice | 39 |
| Surgical technique | 29 |
| Fixation methods | 10 |
| Computer-assisted surgery | 3 |
| Platelet-rich plasma | 4 |
| Rehabilitation | 17 |
| Return to play | 8 |
| Outcomes assessment | 35 |
| Arthritis | 5 |
| Complications | 8 |
| Miscellaneous | 4 |
aTopics are not mutually exclusive. ACL, anterior cruciate ligament.
Anatomy of the ACL
Recent attempts to more accurately reproduce the ACL anatomy during surgery have been accompanied by a more detailed description of the origin and insertion of the ACL bundles on the femur and tibia. A 2009 systematic review of 20 studies by Kopf et al99 outlined the range of dimensions for both footprints, which are noted in Table 2. Only 1 study compared ACL anatomy in males versus females and found greater length and area of the ACL in males, but there was no statistically significant sex-based difference regarding ACL width.
TABLE 2.
Anterior Cruciate Ligament Dimensionsa
| Tibial footprint | |
|---|---|
| Mean length (range), mm | 14 (9-18) to 29.3 (23-38) |
| Area, mm2, range, | |
| Total | 114-229 |
| Anteromedial bundle | 56-136 |
| Posterolateral bundle | 52-93 |
| Femoral footprint | |
| Area, mm2, range | 83-197 |
aReprinted with permission from Kopf et al.99
In 2011, Hensler et al75 sought to determine the effect of drilling via a medial femoral portal on femoral tunnel aperture morphology and performed a systematic review of the anatomy of the femoral origin of the ACL. The mean femoral insertion site was 8.9 mm wide and 16.3 mm long, with a mean area of 136.0 mm2.
A systematic review by Hwang et al85 examined the anatomy of the tibial insertion of the ACL in 5 radiographic studies and 10 anatomic studies. Based on radiographic evidence, the center of the anteromedial bundle of the ACL is located approximately one-third of the anteroposterior (AP) distance of the plateau while the center of the posterolateral bundle is located approximately 40% to 50% of the AP distance. Since the posterior cruciate ligament (PCL) was found to be the most consistent reference point in the AP direction, measurements were made from the PCL to each structure in the anatomic studies, as shown in Table 3. Finally, the medial-to-lateral location of the ACL centroid was found to be approximately two-fifths of the total interspinous distance.
TABLE 3.
Anterior Cruciate Ligament Tibial Anatomya
| Structure | Distance From Posterior Cruciate Ligament, mm |
|---|---|
| Anterior cruciate ligament | 15 |
| Anteromedial bundle | 20 |
| Posterolateral bundle | 11 |
aReprinted with permission from Hwang et al.85
Piefer et al165 summarized measurements for the femoral footprint in terms of percentages of the total distance from the proximal articular margin, a technique that can readily be used during intraoperative evaluation (Table 4). Additionally, the posterior edge of the footprint was found to be 2.5 mm from the posterior articular margin.
TABLE 4.
Measurements of the Femoral Footprint of the Anterior Cruciate Ligamenta
| Structure | Distance From the Proximal Articular Margin, % of Total Distance |
|---|---|
| Anterior cruciate ligament | 43 |
| Anteromedial bundle | 29.5 |
| Posterolateral bundle | 50 |
aReprinted with permission from Piefer et al.165
Epidemiology of ACL Injury
Biomechanics and Mechanism of ACL Injury
Noncontact ACL injury is caused by a multiplane mechanism in individuals who possibly lack dynamic knee joint stability.174,188,192 There is weak evidence supporting the notion that fatigue reduces vertical ground reaction force of the hip and knee joint moments causing increased anterior tibial translation; however, further research is needed.186,188 Brown et al27 reviewed 6 studies and determined that there were differences between planned and unplanned sidestepping tasks, especially for loading associated with weight acceptance rather than during push-off. The authors recommended that unplanned tasks should be incorporated into screening and injury prevention training programs. Louw et al120 found that lack of vision during kinematic testing did not affect knee biomechanics. Drop landing, squatting, stepping down, cutting, and hopping movements were tested in the studies included in their review, although there were some inconsistencies and a relatively small data set. Due to these limitations, it was recommended that practitioners should individualize rehabilitation of vision based on individual ability and performance.
Benjaminse et al17 found small sex-based differences in biomechanics that are unlikely to contribute to the increased injury risk recognized in female athletes. In a review of 27 studies by Carson and Ford,29 females were found to land from a jump with increased knee abduction motion, including abduction angle (22/24 studies), abduction angular motion (15/24 studies), and abduction moment (3/8 studies) when compared with males. Other reviews have found conflicting data regarding quadriceps dominance in females as a contributor to noncontact ACL injury.17,192 Finally, Fox et al58 systematically reviewed and summarized the normal values for females during tasks often related to ACL injury, including single-leg drop landing, double-leg drop vertical jump, and side-step cutting tasks. Mean angles and standard deviations for initial contact results are shown in Table 5 and peak results in Table 6.
TABLE 5.
Initial Contact Resultsa
| HFLEX/EXT | HADD/ABD | HINT/EXT | KEXT/FLEX | KVAR/VALG | KINT/EXT | |
|---|---|---|---|---|---|---|
| Single-leg drop landing task | ||||||
| Weighted mean ± SD | 13.33 ± 10.52 | –10.17 ± 6.76 | NA | –16.92 ± 13.02 | 1.55 ± 3.24 | –6.00 ± 4.33 |
| N | 52 | 38 | NA | 95 | 97 | 43 |
| Double-leg drop vertical jump task | ||||||
| Weighted mean ± SD | 37.54 ± 16.20 | –7.75 ± 5.61 | –11.08 ± 11.85 | –28.05 ± 8.82 | –0.30 ± 5.00 | 4.93 ± 15.96 |
| N | 79 | 40 | 40 | 199 | 191 | 160 |
| Side-step cutting task | ||||||
| Weighted mean ± SD | 46.98 ± 10.98 | –7.20 ± 9.23 | 6.78 ± 14.15 | –27.13 ± 9.35 | –0.97 ± 5.18 | –0.17 ± 9.51 |
| N | 72 | 57 | 57 | 108 | 89 | 74 |
aFirst listed joint rotation denoted by positive (+) angles; second listed joint rotation denoted by negative (–) angles. Reprinted with permission from Fox et al.58 HADD/ABD, hip adduction/abduction; HFLEX/EXT, hip flexion/extension; HINT/EXT, hip internal/external rotation; KEXT/FLEX, knee extension/flexion; KINT/EXT, knee internal/external rotation; KVAR/VALG, knee varus/valgus; N, pooled number of subjects from included studies; NA, not applicable.
TABLE 6.
Peak Valuesa
| HFLEX/EXT | HADD/ABD | HINT/EXT | KEXT/FLEX | KVAR/VALG | KINT/EXT | |
|---|---|---|---|---|---|---|
| Single-leg drop landing task | ||||||
| Weighted mean ± SD | 27.89 ± 8.30 | 8.90 ± 5.14 | NA | –60.46 ± 10.51 | 1.85 ± 4.67 | 7.76 ± 13.78 |
| N | 37 | 37 | NA | 82 | 61 | 105 |
| Double-leg drop vertical jump task | ||||||
| Weighted mean ± SD | 63.02 ± 17.26 | –1.63 ± 7.51 | –8.74 ± 16.13 | –83.44 ± 8.16 | –8.71 ± 9.08 | 16.64 ± 21.04 |
| N | 122 | 96 | 59 | 457 | 274 | 179 |
| Side-step cutting task | ||||||
| Weighted mean ± SD | 45.72 ± 10.39 | –16.60 ± 9.99 | 11.14 ± 13.67 | –56.57 ± 7.44 | –11.05 ± 7.38 | 18.96 ± 7.23 |
| N | 52 | 25 | 25 | 52 | 40 | 25 |
aFirst listed joint rotation denoted by positive (+) angles; second listed joint rotation denoted by negative (–) angles. Reprinted with permission from Fox et al.58 HADD/ABD, hip adduction/abduction; HFLEX/EXT, hip flexion/extension; HINT/EXT, hip internal/external rotation; KEXT/FLEX, knee extension/flexion; KINT/EXT, knee internal/external rotation; KVAR/VALG, knee varus/valgus; N, pooled number of subjects from included studies; NA, not applicable.
In summary, there is some evidence suggesting that unplanned sidestepping can alter knee biomechanics and it may be beneficial to incorporate these tasks into injury prevention programs. There was weak or null evidence for fatigue and lack of vision affecting knee biomechanics. Knee biomechanics in females tends to differ from males during tasks related to injury, such as landing from a jump.
Intrinsic and Extrinsic Risk Factors for ACL Injury
Four systematic reviews and 1 meta-analysis evaluated specific intrinsic risk factors of ACL injury.168,188,224,239,240 Wordeman et al224 performed a meta-analysis of 14 studies that examined the effect of tibial plateau slope on ACL injury risk. Although a large discrepancy among anatomical measurements was found between studies, measurement of the lateral tibial plateau slope was significantly increased in patients with ACL injuries, noted in magnetic resonance imaging (MRI)–based studies. A review by Zeng et al239 showed that while there was a wide range of tibial plateau slopes for both control groups and those with ACL rupture, those with rupture had a significantly greater plateau slope than those without rupture. Again, lateral tibial plateau slope (weighted mean difference [WMD], 1.8°; 95% CI, 1.3°-2.3°) was greater than medial plateau slope (WMD, 1.1°; 95% CI, 0.5°-1.7°) in patients with ACL rupture.
Intercondylar notch stenosis has also been considered an intrinsic risk factor of ACL injury. One meta-analysis240 and 1 systematic review168 both found that a narrow notch was a significant risk factor for ACL injury. Other potential intrinsic risk factors of ACL injury identified by 2 systematic reviews include: ACL geometry in females, foot pronation, pelvic tilt, generalized joint laxity, anterior knee laxity in females, menstrual cycle phase, dynamic knee valgus and knee flexor/extensor preactivation in females, familial predisposition, and the presence of collagen type I alpha 1 (COL1A1) gene, height, and body mass index (BMI).168,188
Two systematic reviews examined extrinsic risk factors of ACL injury.13,188 A shoe-surface interface that increased ground friction and a position of play that predisposed the athlete to unanticipated sidestepping may influence ACL injury according to Serpell et al.188 Balazs et al13 found an increased risk of ACL injury in football players who performed on synthetic playing surfaces but, interestingly, no increased risk in soccer players on similar surfaces.
In summary, several intrinsic and extrinsic risk factors of ACL injury have been found. The 2 most established intrinsic risk factors are increased tibial plateau slope and a narrow intercondylar notch. Many other potential intrinsic factors have been noted such as joint laxity, familial predisposition, and BMI, to name a few. Shoe-surface interface and position of play have been found to be extrinsic risk factors of ACL injury.
Menstrual Cycle
The increased risk of ACL injury found in female athletes is most likely multifactorial; however, there have been multiple studies indicating a contribution from hormonal factors.16,81,168,188,237 Risk of ACL injury related to timing of the menstrual cycle has been evaluated in 3 recent systematic reviews that focused on risk in female athletes16,81,237 and 2 general risk factor systematic reviews.168,188 Each review arrives at a similar conclusion, demonstrating increased risk of ACL injury in female athletes due to increased ligamentous laxity in the first half of the menstrual cycle during the preovulatory phase. The biochemical explanation for these changes is most likely related to the increased levels of relaxin and the estrogen-mediated reduction in procollagen I resulting in altered ligamentous tensile properties.168,188 Oral contraceptive use, in addition to neuromuscular training, may increase dynamic knee stability and lessen the risk of ACL injury secondary to hormonal changes during the menstrual cycle.81 Additional research is needed on this subject, and the definitions of the menstrual cycle phases, based on hormonal peaks and fluctuations, must be clarified in future studies.
Incidence in Specific Populations
The traditional view regarding the incidence of ACL injury in specific athletic populations has been recently reevaluated in the literature.88,137,170 Prodromos et al170 performed a meta-analysis of 25 epidemiologic studies and found a 5% rate of ACL tear in females that participated in year-round soccer and basketball; females had a 3-fold greater risk of ACL tear than males participating in the same sport. There was no sex-based difference in the risk of ACL injury in Alpine skiers or lacrosse players. However, recreational Alpine skiers demonstrated a greater incidence of ACL injury, with the lowest incidence occurring in expert skiers. Furthermore, the incidence of ACL injury associated with volleyball is much less than previously thought and was classified by the authors as a low-risk sport. Moses and Orchard137 found that male athletes have a greater incidence of ACL injuries based on increased exposure to higher risk sports, specifically football. They found that professional athletes, including those involved in football, basketball, soccer, rugby, skiing, handball, volleyball, and dancers, actually have a greater rate of ACL injury that is likely attributed to increased exposure to intense training and more frequent competition. The authors determined that there is high variability in reporting differences in the incidence of ACL injury in the literature and suggested reporting ACL injuries using common units, such as annual incidence rates, to allow for improved comparisons between various populations and sporting groups. Last, a review by Jacobs et al88 evaluated ACL injury in dancers and found an incidence of 0.0009 per 1000 exposures. The authors concluded that the relationship between fatigue and injury in dancers needs further research.
Prevention of ACL Injury
Prevention in Males and Females
Only 3 systematic reviews have examined studies of prevention of ACL injury in males.3,4,182 Alentorn-Geli et al3 performed a systematic review of 34 articles and found that dry weather conditions, artificial turf, and increased posterior tibial slope were associated with increased risk of ACL injury in males. Three of 7 studies included in another review by Alentorn-Geli et al4 found that prevention programs were successful in reducing ACL injuries or modifying risk factors for ACL injuries in males. In 2012, Sadoghi et al182 estimated an 85% reduction in ACL injuries in males after participation in an injury prevention program.
The majority of systematic reviews examining the effects of prevention programs on ACL injury have focused on female athletes. The most common areas of study in female athletes have been overall effectiveness, effectiveness of specific program components, effectiveness by age, and compliance on effectiveness.
ACL Prevention Program Effectiveness
Seven meta-analyses§ have investigated the overall effectiveness of ACL prevention programs and have shown decreases in ACL injuries in female athletes participating in prevention programs. Reductions in ACL injuries of approximately 40% to 75% were reported in 6 studies.62,141,182,202,205,235 The number needed to treat as calculated by Sugimoto et al was 108 female athletes to prevent a noncontact ACL injury and 120 to prevent an ACL injury from all causes.202 Multiple systematic reviews have also examined overall effectiveness of ACL injury prevention programs,∥ of which only 1 of these reviews did not find sufficient evidence to support the effectiveness of ACL injury prevention in females.69
Effectiveness of Prevention Program Components
Five meta-analyses investigated the effectiveness of program components,62,79,182,205,235 of which only 3 made recommendations for preventing ACL injury based on various program components.79,205,235 Yoo et al235 found that programs utilizing both preseason and in-season training were more effective in preventing ACL injury than those that performed either preseason or in season training.235 Also, plyometric and strength training were effective in preventing ACL injury where balance training was not. Taylor et al205 reported a decrease in ACL injuries after static stretching and an increase in ACL injuries after longer duration of balance training. Session duration, total training time, and technique feedback were not associated with ACL injuries. Hewett et al79 recommended a combination of plyometrics, strength training, and balance with supervision for longer than 6 weeks with at least 1 session per week, as well as feedback.
Multiple systematic reviews have also investigated the effectiveness of ACL injury prevention program components19,130,152,158,199 and have recommended that ACL prevention programs should incorporate both preseason and in-season training and a combination of plyometrics, balance, and proprioception for longer than 6 weeks with at least 1 session per week. Benjaminse et al19 and Padua and DiStefano152 also recommended using instructors or trainers with multimodal feedback to improve safety and results of training sessions.
Influence of Program Compliance on Effectiveness
Sugimoto et al201 investigated the relationship between compliance and success of ACL prevention protocols in a meta-analysis of 6 studies. In studies with less than 66% compliance, the risk of ACL injury was 3 to 5 times greater than studies with greater than 66% compliance. Attendance and completion of ACL prevention programs appear to be important factors in patient success.
Influence of Age on Program Effectiveness
Two studies investigated the association between participant age and effectiveness of ACL injury prevention.141,235 Yoo et al235 and Myer et al141 found odds ratios favoring participants younger than 18 years (0.27 and 0.28, respectively) versus those older than 18 years (0.78 and 0.84 respectively), demonstrating a greater prophylactic effect in participants younger than 18 years.
Associated Injuries
Meniscal Tears
Pujol and Beaufils172 examined healing rates of lateral and medial meniscus tears left in situ during ACL reconstruction. Patients with lateral meniscus tears had slightly greater healing (55%-74% vs 50%-61%) and fewer unhealed or extended tears (1%-22.5% vs 1%-50%) versus patients with medial meniscus tears. As a result, fewer lateral meniscectomies were performed.
Due to the relationship between ACL rupture, resultant instability, and later meniscal tears, treatment of meniscal tears without instability management has been a subject of debate. Since meniscal preservation is standard of care, Beaufils et al15 reported that meniscal symptoms in the face of chronic laxity suggest the need for ACL reconstruction. Furthermore, this review recommended that meniscectomy without ACL reconstruction only be performed in the presence of a symptomatic, irreparable meniscal lesion and lack of functional instability in an inactive or elderly patient.
Salata et al183 demonstrated that meniscal tears found during ACL reconstruction are not predictive of a poor clinical or radiographic outcome, although there were worse clinical and radiographic outcomes in ACL-deficient versus ACL-intact knees. Intact or repaired menisci were associated with favorable outcomes in ACL-reconstructed knees, while repair of degenerative meniscal tears was not. The morphology of the meniscal tear generally directs treatment, and Noyes and Barber-Westin146 found that partial meniscectomy was performed 2 to 3 times more often than meniscal repair. Paxton et al162 demonstrated that meniscal repair has a lower reoperation rate if it is performed with a concomitant ACL reconstruction and that lateral meniscus repair had a lower reoperation rate than medial meniscus repair. In contrast to these short-term studies, Nepple et al144 found no significant difference in the rate of meniscal repair failure for ACL-intact (22.7%) versus ACL-deficient (22.1%) or ACL-reconstructed (26.9%) knees at long-term (>5 years) follow-up. However, this study may have been underpowered.
Multiligament Tears
There is limited evidence regarding treatment of combined ACL and medial collateral ligament (MCL) tears.68,156 Papalia et al156 only found 1 randomized controlled trial that compared conservative with surgical treatment of ACL-MCL injuries, which showed a greater rate of return to activity with surgery compared with conservative treatment (61% vs 31%). Heterogeneity in study design, patient characteristics, treatment methods, and outcome assessment of the 23 studies included in this review prevented comparison of pooled outcomes. More prospective randomized clinical trials comparing conservative and surgical treatment of ACL-MCL injuries are needed. Grant et al68 systematically reviewed 4 studies of patients with combined complete tears of the ACL and MCL and found that ACL reconstruction should be delayed in this group until range of motion (ROM) returns. If valgus instability still persists at that time, repair or reconstruction of the MCL should be considered.
Bonanzinga et al25 reviewed studies examining the management and outcomes of combined injuries of the ACL and posterolateral corner (PLC). No difference in AP stability was found after combined ACL-PLC reconstruction versus ACL reconstruction without PLC injury.
Other Intra-articular Pathology
Bone bruises are often seen on MRI in association with ACL pathology, especially on the lateral femoral condyle and posterior lateral tibial plateau, as demonstrated in a review by Patel et al.159 This pattern of bruising is more suggestive of a multiplanar, valgus-loading ACL injury mechanism (pivot-shift) than hyperextension valgus or varus mechanisms; however, this review did not examine clinical outcomes of bone bruising.
Chondral surfaces may also be damaged when a knee is unstable, and the incidence of severe chondral injury in knees with ACL rupture is between 16% and 46%.26 Flanigan et al54 found that 30% of athletes with chondral defects had ACL insufficiency. Reasonable short-term outcomes have been found after an osteoarticular transfer system (OATS) procedure or autologous chondrocyte implantation (ACI) when combined with ACL reconstruction.26
Diagnosis of ACL Injury
A 2006 study by Benjaminse et al18 found that the Lachman test is the most reliable test for diagnosing ACL injury when considering combined sensitivity and specificity for all circumstances (including with and without anesthesia and acute vs chronic injury). The pivot shift test had the highest specificity but lacked sensitivity, especially in awake patients. Meanwhile, the anterior drawer test is better for diagnosis of chronic injuries than acute but is not sensitive enough for routine use alone.
van Eck et al213 also found the Lachman test to have the highest sensitivity for diagnosing an acute complete ACL rupture, while specificity was similar for the Lachman, anterior drawer, and pivot shift tests. When performed under anesthesia, the Lachman test had the highest sensitivity and the pivot shift test had the highest specificity. This review had some limitations, as most studies were not recent and reported sensitivity or specificity but not both. Furthermore, most studies did not compare testing in the office and during examination under anesthesia in the same study cohort.
Lopomo et al119 found that in vitro studies that have tried to quantify the pivot shift test do not accurately model clinical scenarios. Cadavers are not typically the same age as most patients with ACL tears, and application of clinical tests cannot be performed reliably in the same manner as in vivo tests. Finally, in vivo studies revealed variation in behavior between knees and testing between surgeons.
The use of instrumented measurement has also been systematically reviewed, and van Eck et al212 found that the KT-1000 arthrometer, performed with maximum manual force, has the highest sensitivity, specificity, accuracy, and positive predictive value for diagnosing ACL rupture. Finally, MRI was found by Crawford et al42 to be highly accurate in diagnosing both meniscal and ACL tears. It is the most appropriate screening tool before therapeutic arthroscopy, although a possible weakness of this study is that it did not consider the type of tear.
Nonoperative Versus Operative Management of ACL Injury
Copers Versus Noncopers
Rupture of the ACL can cause significant disability in active individuals; however, approximately one-third of this population does not experience impairment or disability and are referred to as copers.77,92 Two recent systematic reviews evaluated potential measurement tools for identifying copers, with the goal of preventing unnecessary surgical treatment.77,92 Herrington and Fowler77 found a combination of functional tests and subjective questionnaires that could improve assessment of copers, while Kaplan92 found objective differences between copers and noncopers that could be identified with screening examinations and specific algorithms. At this point, individuals wishing to return to pivoting sports are best treated with ACL reconstruction regardless of coping ability.92 Additional research is needed to better identify copers, and long-term follow-up of copers is needed to determine whether these individuals fare better than noncopers and individuals who have undergone ACL reconstruction.77
Skeletally Immature Patients
As tears of the ACL have become increasingly common in skeletally immature patients, recommendations for dealing with them have evolved. In 2006, Mohtadi and Grant132 found weak evidence for surgical treatment in this population and recommended that the surgeon wait until skeletal maturity for reconstruction if possible. Activity modification and bracing were favored as alternative modalities. Kaeding et al91 reported a low incidence of growth disturbance with both physeal-sparing as well as transphyseal techniques in Tanner stage II and III patients. There were not enough data on the transphyseal technique for Tanner stage I patients, but based on the findings with more mature patients, operative treatment was discouraged against. Vavken and Murray217 found that in a group of 476 skeletally immature patients, 5 had physeal disturbance after a transphyseal technique. Despite this, no clinically relevant deformities were noted. Moksnes et al134 described the current rates of operative management in children and found that 47% of ACL tears were accompanied by meniscal tears, of which 67% were repaired. Fourteen percent of those meniscal repairs failed; however, this review was limited by the poor quality of included studies. A meta-analysis by Ramski et al175 found that children or adolescents undergoing nonoperative or delayed ACL reconstruction were 33.7 times more likely to be clinically unstable and 12 times more likely to subsequently have medial meniscus injury than those who had surgery earlier.
Skeletally Mature Patients
A Cochrane review concluded that there was insufficient evidence from previous randomized trials to determine whether operative or nonoperative treatment of ACL injuries was more effective in adults.115 Boks et al24 found that the ACL can regain continuity after partial or complete rupture, as seen on MRI after a period of nonoperative treatment. However, there was a weak association between continuity of the ligament on MRI and clinical stability at follow-up, including functional outcome scores, and complaints. Muaidi et al138 found good short- to mid-term prognosis for nonoperatively treated ACL tears, as measured by the Lysholm score and hop-for-distance limb symmetry index. Tegner activity scores revealed that activity levels were reduced by 21% after nonoperative treatment.
Farshad et al52 performed a cost-effectiveness review and determined that ACL reconstruction was cost-effective in comparison with nonoperative treatment. Reconstructed patients also had greater levels of activity versus nonoperative groups (70.7% vs 49.7%).
Expectedly, Smith et al195 found increased stability at 1 to 10 years after ACL reconstruction compared with nonoperative treatment. However, there was no difference in stability and return to play between operative and nonoperative treatment over the long term. Furthermore, effects on the joint over time including the health of the meniscus and arthritis are mixed, and there is not enough evidence to recommend reconstruction versus nonoperative treatment based on current literature.
Despite the mixed evidence reported above, when ACL tears are associated with greater magnitudes of trauma or injury, operative treatment has shown promising results. When ACL tearing is associated with dislocation of the knee, operative treatment tends to provide improved outcomes, as shown by Frosch et al.59 Specifically, nonsurgical treatment had poor or moderate results in 70% of subjects, while repair with sutures had 40% excellent and 37.5% good results. Reconstruction had 28% excellent and 45% good results. Repair of concomitant PLC injuries also had a positive effect on clinical results, while repair of the MCL did not. Higher grade dislocations (according to the Schenck classification, Table 7) were associated with worse outcomes, although there were no significant differences in outcome between type II and III dislocations. When joint dislocation accompanied multiple-ligament injury, early surgery had a greater risk of loss of ROM and stiffness than delayed surgery. Early therapy may have prevented loss of ROM but did not reduce the rate of surgery for stiffness.135
TABLE 7.
Schenck Classification of Ligament Injurya
| Type | Description |
|---|---|
| I | Single ligament injury (ACL or PCL) |
| II | Injury to ACL and PCL |
| III | Injury to ACL, PCL, and either the LCL or MCL |
| IV | Injury to ACL, PCL, LCL, and MCL |
| V | Multiligamentous injury with periarticular fracture |
aReprinted with permission from Frosch et al.59 ACL, anterior cruciate ligament; LCL, lateral collateral ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament.
Anterior cruciate ligament injury and the subsequent need for reconstruction have been related to tibial fractures as well.23,32 Chen et al32 reviewed tibial plateau fractures and found that 21.3% of patients had an ACL injury. They found that while avulsion injuries are typically treated with arthroscopy-assisted fixation at the index procedure, midsubstance injuries are not. Bogunovic et al23 found that there is an increased rate of clinical and subjective instability with nonoperative treatment of displaced fractures, and subsequently, a need for ACL reconstruction. Furthermore, ACL reconstruction was infrequently needed when either suture or screw fixation of the fracture was performed, although instability was more common with screw compared with suture fixation.
Summary
Patients with ACL injuries can be divided into copers and noncopers based on whether they experience impairment or disability after their injury; however, more research is needed to determine whether copers have better outcomes after nonoperative management than noncopers. Several reviews have recommended nonoperative management in skeletally immature patients; however, 1 review found that nonoperative management or delayed ACL reconstruction can lead to more instability and medial meniscus injuries in this population. In skeletally mature patients, ACL reconstruction has been shown to be successful for cases with greater magnitudes of trauma or injury and in the presence of a knee dislocation; however, 1 review also found good short- to mid-term prognosis for nonoperative management.
Graft Choice
Ligamentization of ACL Autografts
A series of biologic processes that occur to free tendon graft utilized to reconstruct the ACL is termed ligamentization. Three systematic reviews examined whether the process of ligamentization does, in fact, occur,36,89,161 and 2 of these reviews evaluated this process in bone–patellar tendon–bone (BPTB) autografts.36,161 These studies concluded that ligamentization is a predictable process occurring in 3 different stages, including the early healing phase, the proliferation phase, and the maturation phase; however, there is no agreement on the timing of these stages. Furthermore, the remodeling process in humans is prolonged compared with animal studies.89 Finally, hamstring tendon (HT) autograft demonstrates a slower healing and maturation phase than BPTB autograft.161
Autograft Versus Allograft
Eleven systematic reviews, with sample sizes ranging from 410 to 5182, have compared autograft versus allograft ACL reconstruction in terms of patient outcome, laxity, and failures.¶ Six reviews compared BPTB and HT autografts to a variety of allografts.44,57,84,100,126,169 Two reviews excluded irradiated allografts84,126 and 2 included low-dose irradiation (<2 Mrad)28,57; however, none of these reviews found a difference between autografts and allografts. Two reviews that compared autografts versus allografts included a variety of sterilization methods (including radiation and ethylene glycol), of which 1 review found better outcomes with autografts and the other review found slightly more laxity with allografts, but no other significant differences in outcomes or failures were found.169,210 Lamblin et al105 compared autografts versus nonirradiated non–chemically treated allografts and found no significant differences in failure rate, outcome scores, or clinical and instrumented laxity.105 One review comparing HT autograft and soft tissue allograft found no difference between the graft types despite inclusion of irradiated allografts.44 Four reviews specifically compared BPTB autograft with BPTB allograft,84,100,103,126 with 1 review finding no difference in outcomes after excluding irradiated and chemically sterilized allografts.103 On the other hand, 3 reviews found autografts to be superior to allografts, of which 1 review did not report sterilization method,100 1 excluded irradiated allografts,84 and 1 included irradiated allografts.234
In summary, autografts offer improved outcome scores and greater patient satisfaction compared with allografts, and autografts are preferred in young, active populations. On the other hand, allograft sterilization method, specifically irradiation, has been shown to affect outcome measures and is a valid option in older, less active populations.157 Nonirradiated allografts are associated with lower failure rates compared with radiated allografts. Further research is needed to evaluate outcomes of allografts with improved sterilization methods in younger populations.
BPTB Autograft Versus HT Autograft
Numerous studies have compared BPTB autograft versus HT autograft and have found that BPTB autograft is associated with greater improvement in stability compared with HT autograft; however, there is no difference in clinical knee scores# and rate of failure.56,67,111,112,122,197 Anterior knee pain and kneeling pain occur more frequently with BPTB autograft than HT autograft,** and there is possibly a decrease in quadriceps and hamstring isokinetic muscle strength secondary to patellar tendon and HT harvest, respectively, that may persist for greater than 2 years.231 Xie et al232 found no difference in knee laxity for BPTB versus HT autografts; however, Paterno et al160 found increased laxity in females with HT autografts as well as in males and females with BPTB autografts. There may also be an association between osteoarthritis and BPTB autografts232; however, further evidence is needed, and HT graft stability is improved with 4-stranded grafts compared with 2-stranded grafts.
Two analyses of overlapping reviews comparing BPTB to HT autograft were performed to determine factors that led to differing conclusions from these reviews.166,216 Vavken and Dorotka216 suggested that these conflicts were derived from the interpretation of the pooled results and concluded that meta-analyses should be critically scrutinized like any other study. Poolman et al166 evaluated these reviews in a similar fashion and determined that the most methodologically sound meta-analysis21 found that graft harvest morbidity was lower for HT autograft, and the evidence that BPTB autografts provided better stability was weak.
Conte et al39 examined the association between HT autograft size and graft failure as well as predictors of HT autograft size. Rate of graft failure was decreased when the graft diameter was more than 8 mm in patients younger than 20 years, a population at increased risk of failure after reconstruction. Additionally, MRI and patient height were found to be preoperative predictors of HT diameter.
In summary, there is much evidence showing that BPTB autograft shows greater improvement in stability than HT autograft; however, clinical scores and rate of failure does not differ. BPTB autografts are also associated with increased anterior knee and kneeling pain.
Synthetic ACL grafts
The Ligament Augmentation and Reconstruction System (LARS) is a third-generation artificial polyester ligament made from polyethylene terephthalate (PET) designed to overcome the issues of graft failure and synovitis, which led previous generations of synthetic ligaments to fall out of favor. There have been 3 systematic reviews that evaluated LARS or other PET implants.121,139,145 Each of these reviews reported good short-term results, a low incidence of synovitis, and rerupture rates ranging from 2% to 8%. Non-PET LARS demonstrated overall poor long-term results.139 LARS results with medium-term follow-up were comparable with autograft ACL reconstruction outcomes, but long-term data are lacking despite more than 15 years of availability. Two of these reviews assessed bias and quality of the included studies and found that none of the studies included a representative sample or provided a sample size justification, and they lacked control of potential confounders.121,145
Quadriceps Tendon Autograft
There has recently been renewed interest in the utilization of quadriceps tendon for ACL autograft. A systematic review by Mulford et al140 evaluated 17 studies with a total of 1580 patients and found that quadriceps tendon autografts were associated with good clinical and functional outcomes, decreased anterior knee pain, and greater graft cross-sectional area as compared with BPTB autograft. The authors concluded that quadriceps tendon is a promising graft option; however, the current level of evidence is of poor quality and further studies are required.
Surgical Technique
Single- Versus Double-Bundle ACL Reconstruction
Multiple systematic reviews have focused on the comparison of double-bundle (DB) and single-bundle (SB) techniques for reconstruction of the ACL.†† In 2007, Steckel et al198 found that there was no clinical evidence of a difference between the 2 techniques, although there were few randomized studies at the time and no complications were reported with the DB technique. In 2008, Meredick et al128 found that KT-1000 arthrometer results for DB yielded 0.52 mm less anterior-posterior translation than did SB reconstruction, although this difference was not clinically significant. Furthermore, pivot shift testing was not significantly different between DB and SB reconstruction, although normal and near-normal results were collapsed together for analysis. Lewis et al110 also showed the SB technique to be safe and reliable based on the results of the pivot shift test (81% negative) and AP laxity tested with the Lachman (59% negative) and instrumented (77% negative) testing. Furthermore, Gadikota et al61 found no difference in AP or rotational laxity for DB versus SB ACL reconstruction. Jarvela and Suomalainen90 found that of 14 studies in their review, 7 showed improved rotational stability and 6 showed improved AP stability. van Eck et al211 compared DB versus SB reconstructions and found improved KT-1000 and pivot shift testing in both randomized and observational trials, and Lachman testing was only improved in the observational trials. However, there were no differences found in patient outcomes, and the studies included had short-term follow-up.
Tiamklang et al209 found that DB reconstructions were associated with faster return to preinjury level, better International Knee Documentation Committee (IKDC) Knee Form scores, increased knee stability, fewer new meniscal injuries, and fewer traumatic ACL ruptures versus SB reconstructions. No significant differences were found between groups for functional scores, pain, adverse events, complications, and graft failure. Similarly, 2 studies found no difference in outcome scores between DB versus SB reconstructions but noted some improvement in DB pivot shifts.106,118 Seven recent systematic reviews, summarized in Table 8, compared DB versus SB reconstructions and found that certain objective and subjective measures were more favorable for DB versus SB reconstructions, including improvements in the pivot shift test, Lachman scores, and KT-1000 scores.22,48,98,113,114,233,241
TABLE 8.
Summary Results of Systematic Reviews Published in 2013-2014 That Compared Double- Versus Single-Bundle ACL Reconstructiona
| Authors | Outcomes Found to Be More Favorable for DB vs SB Reconstruction | Outcomes That Did Not Differ for DB vs SB Reconstruction |
|---|---|---|
| Zhu et al241 | KT-1000, Lachman, IKDC | Lysholm, Tegner |
| Xu et al233 | Pivot shift, Lachman, KT-1000, IKDC objective | KT-2000, laxity rolimeter, Lysholm, Tegner, IKDC subjective |
| Kongtharvonskul et al98 | Pivot shift, IKDC objective score | KT-1000, Lysholm, Tegner, complications |
| Li et al113 | Pivot shift, KT-1000, IKDC subjective score, extension deficit, decreased graft failures | Lysholm score, objective IKDC score, flexion deficit and knee isokinetic peak torques |
| Björnsson et al22 | Pivot shift (8 of 42 studies), Lachman (4 of 17), anterior drawer (3 of 9), KT-1000 (18 of 40) Navigation: AP (3 of 17), rotation (9 of 20) | Extensor strength (9 of 10) Flexor strength (8 of 10) |
| Li et al114 | Pivot-shift, KT arthrometer grading, IKDC grading | IKDC subjective score, KT arthrometer measures, Lysholm, Tegner activity score, complications |
| Desai et al48 | KT-1000, navigated AP laxity | Pivot-shift test, Lachman, anterior drawer test, total IRER or graft failure rates |
aAP, anteroposterior, DB, double-bundle; IKDC, International Knee Documentation Committee; IRER, total internal-external rotation; SB, single-bundle.
In summary, there appears to be a small difference between DB and SB reconstruction in terms of rotational and AP stability in the hands of some surgeons. It is unclear whether these differences are clinically significant. Long-term follow-up appears to show comparable results between the techniques.
Anatomic ACL Reconstruction
van Eck et al211 conducted a systematic review that compared anatomic and nonanatomic DB versus SB ACL reconstructions. For nonanatomic reconstructions, the only significant difference in outcome measures was increased risk of extension deficit for DB versus SB. For anatomic reconstructions, KT arthrometer and pivot-shift test results showed greater improvement for DB versus SB. The authors concluded that anatomic reconstruction may be more important than the number of bundles utilized.
Femoral Tunnel Drilling Method
Alternatives to transtibial drilling have been developed to avoid the limits inherently set by transtibial approaches on femoral start point and angle.2,30,63,179 Compared with the transtibial technique, the use of an anteromedial portal for BPTB ACL reconstruction was associated with faster return to running, greater ROM, and improved Lachman and KT-1000 results at 1- to 2-year follow-up in a systematic review by Alentorn-Geli et al.2 However, activity level at 3- to 5-year and 6- to 10-year follow-up was greater for the transtibial technique versus use of an anteromedial portal. Chalmers et al30 conducted a systematic review comparing the anteromedial portal versus transtibial techniques and found improved rotatory stability in 5 of 8 studies and improved clinical outcomes in 2 of 5 studies.
Riboh et al179 found that compared with a transtibial technique, independent drilling techniques allowed the femoral tunnel position to be closer to the center of the ACL footprint. Independent drilling was associated with increased Lysholm scores and improvement in stability, as measured by the Lachman, AP testing with 134 N, and pivot shift, compared with the transtibial technique. However, there were no significant differences in IKDC objective score, Tegner activity, and the rate of graft failures for transtibial versus independent drilling techniques. One systematic review compared transtibial and rear-entry techniques of drilling the femoral tunnel and found no differences in outcome measures between techniques, although operative times may be shorter for the all-endoscopic technique.63 In summary, both the anteromedial portal and transtibial techniques produced good outcomes; however, the anteromedial portal technique has shown greater improvements in outcomes versus the transtibial technique in some studies.
Remnant Preservation
Four systematic reviews examined outcomes after ACL remnant preservation or augmentation and found no improvement in graft vascularization, outcome scores, or complication rate.83,154,155,196 While techniques for repairing the cruciate ligaments have been widely abandoned, some surgeons have recommended reconstruction without fully debriding remaining ligament tissue, which could theoretically improve vascularization or decrease tunnel widening.
Other Topics
Smith and Hing194 and Wu et al230 compared reconstructions using a tourniquet with those without one and found no significant differences in operative time, visual analogue scale (VAS) for pain, blood loss, and thigh or calf girth. A systematic review by Andersson et al6 in 2009 found that outcome was not affected by initial graft tension, ligament augmentation, choice of screw material, or use of a postoperative knee brace. Osteoarthritis was seen in 50% of patients and was noted to be increased when meniscectomy was performed at the time of reconstruction.
Femoral nerve blocks might minimize pain during the postoperative period. Mall and Wright125 found that 5 of 13 studies in their review found a significant reduction in pain after a femoral nerve block; however, the observed differences may not have been clinically relevant. Also, 2 of 13 studies found no significant difference in satisfaction of patients with femoral nerve blocks compared with controls. Last, Clifton et al37 found increased postoperative pain after use of a drain versus no drain after ACL reconstruction. However, there were no differences in blood loss or complications between these groups.
Summary
It appears that anatomic placement of the femoral tunnel is important to the function of the ACL reconstruction. A separate portal appears to aid in placement of an anatomic tunnel. Other factors do not appear to matter as much, including the number of bundles, remnant preservation, endoscopic versus rear-entry approach, or use of a tourniquet or femoral nerve block.
Fixation Methods
Graft Fixation
Recent studies of graft fixation have compared techniques for securing HT grafts versus interference fixation for BPTB autografts. Five reviews evaluated intratunnel versus extratunnel fixation of HT autografts.38,71,86,171,181 Two of these studies compared intratunnel versus extratunnel fixation of both the femoral and tibial grafts and found no differences in clinical scores, laxity, or failure between these techniques71,86; however, patient satisfaction and return to preinjury activity level was lower for extratunnel fixation of HT autografts in 1 study.86 Prodromos et al171 evaluated a variety of hybrid fixation methods including Endobutton femoral fixation with second-generation tibial fixation (defined as not involving buttons or simple staples) and found increased stability for HT graft fixation versus BPTB with interference screw fixation. A review by Colvin et al38 compared intratunnel versus extratunnel fixation for the femoral side only and found no difference in IKDC scores; however, there was a trend toward decreased failure with interference screw fixation. Finally, Saccomanno et al181 compared cortical button versus transfemoral suspensory femoral fixation and found no differences in short-term outcomes despite increased tunnel widening in the cortical button group.
Three meta-analyses compared bioabsorbable versus metal interference screws and found no differences in functional or clinical results between these types of screws.49,107,189 Compared with metal screws, bioabsorbable screws were associated with increased risk of breakage, incidence of knee joint effusion, and tunnel widening. Future studies with longer follow-up are needed to compare the long-term effects of bioabsorbable versus metal screws.
Graft Tensioning
ACL graft tensioning during fixation was evaluated by 2 systematic reviews.10,96 Both reviews found inconclusive evidence regarding the amount of tension needed for fixation and determining whether patient function is improved at any specific point of tension.
Summary
Based on current systematic reviews, there is no clinical difference in suspensory versus interference screw fixation with HT autograft, and aperture fixation may improve patient satisfaction. Also, advancements in fixation methods may offer improved stability for HT autograft; however, there is insufficient evidence to recommend specific graft tensioning during fixation. Finally, there was no clinical difference in bioabsorbable versus metal interference screw fixation, and increased tunnel widening has been shown to be associated with bioabsorbable interference screws but does not affect short-term function.
Computer-Assisted Surgery
Several systematic reviews have compared computer-assisted surgery (CAS) with nonassisted ACL reconstruction and found no significant differences in subjective testing between these groups.33,34,129 Meuffels et al129 found that tibial tunnel placement was not more accurate with CAS than when performed manually; however, 1 study found improvement in femoral tunnel position with CAS, and variation in measurement between studies prevented data from being pooled. Cheng et al33 compared radiographic outcomes for CAS versus manual ACL reconstruction in 2011 and found that both methods placed the tibial tunnel in acceptable positions in accordance with standard recommendations. Furthermore, CAS reconstructions had more anterior tibial tunnels and were less impinged than manual ACL reconstructions. Cheng et al34 also compared clinical outcomes for CAS versus manual reconstructions and found no differences in functional outcomes between these 2 methods in the short term. Furthermore, it was concluded that tunnel placement may be more accurate with CAS reconstruction, but this procedure generally increased operating time by 8 to 14 minutes and involved a more invasive technique.
Platelet-Rich Plasma
Four systematic reviews examined the effects of PRP on the healing and maturation processes of ACL reconstructions.136,190,204,218 Three of these reviews evaluated PRP in multiple soft tissue conditions, including ACL reconstruction,136,190,204 and 1 review specifically examined the effect of PRP on ACL graft healing.218 Taylor et al204 and Vavken et al218 suggested that the use of PRP during ACL reconstruction might enhance graft maturation by 20% to 30%. However, in general, these studies found insufficient evidence to determine the effectiveness of PRP on ACL reconstructions.136,190,204,218 Vavken et al218 concluded that the current level of evidence within the literature today is of low quality, with no standard PRP preparation method, application, or activation among studies.
Rehabilitation
Knee Bracing
Multiple systematic reviews have evaluated whether there is any benefit to routine brace treatment in the postoperative period after ACL reconstruction.102,117,225,228 In 2007, Wright and Fetzer225 performed a systematic review of 12 level 1 randomized controlled trials and found no evidence that braces contribute to pain control, graft stability, ROM, or protection from additional injury. The remaining authors also concluded in their respective reviews that the literature shows no added benefit from bracing in the postoperative period.
Continuous Passive Motion
Several systematic reviews have examined the effectiveness of routine continuous passive motion (CPM) for increasing ROM after ACL reconstruction; however, moderate evidence was found, suggesting no added benefit of CPM compared with standard treatment.102,117,228
Accelerated Rehabilitation, Early Weightbearing, and ROM
Three systematic reviews found that accelerated rehabilitation, early weightbearing, and early ROM are likely safe and possibly beneficial to patient outcomes.102,228,229
Home- Versus Clinic-Based Physical Therapy
Four systematic reviews have examined the effectiveness of home- versus clinic-based physical therapy after ACL reconstruction, and overall the findings are inconclusive.41,102,117,228 Kruse et al102 and Wright et al228 found some support for the effectiveness of home-based therapy. However, Lobb et al117 found no difference in the effectiveness of home- versus clinic-based therapy, and Coppola and Collins41 concluded that not enough evidence exists to determine the effectiveness of a home-based program after ACL reconstruction.
Open Chain Rehabilitation Exercises
Glass et al64 reviewed 6 randomized controlled studies that compared open chain with closed chain exercises and found no differences in laxity, pain, and function between these types of rehabilitation in patients with ACL deficiency or reconstruction. Additionally, the most appropriate timing of implementation of open chain exercises is uncertain. A systematic review by Lobb et al117 also found no differences in pain, function, and laxity for open versus closed chain exercises for ACL reconstruction rehabilitation. Grodski and Marks70 concluded that carefully planned rehabilitation programs help reduce muscle atrophy and regulate graft strain, and thus, open chain exercises in ranges where the extensors can work without harming the joint are advisable.
Cryotherapy
Raynor et al176 and Martimbianco et al127 performed meta-analyses that investigated the effectiveness and safety of cryotherapy after ACL reconstruction. Compared with placebo, Raynor et al176 found that cryotherapy was statistically significantly associated with reduced pain but was not significantly associated with ROM or postoperative drainage output. Martimbianco et al127 compared outcomes for a cryotherapy device versus ice pack, no treatment, and placebo. Pain scores at 48 hours after ACL reconstruction were significantly reduced for cryotherapy versus no therapy, suggesting that cryotherapy is safe and effective during this short-term postoperative period. However there were no other significant results.
Resistance Training
Augustsson11 systematically reviewed 6 studies that documented strength training protocols after ACL reconstruction, and it was found that only 2 studies clearly documented the postoperative strength training protocol used in their study, suggesting a need for more accurate reporting of strength training protocols. Kristensen and Franklyn-Miller101 reviewed the efficacy of resistance training for various musculoskeletal conditions, including ACL reconstruction. Low to moderate resistance training after ACL reconstruction resulted in significant increases in strength and functional ability; however, there was little to gain from high-intensity resistance training in the immediate postoperative period.
Neuromuscular and Proprioceptive Training
Cooper et al40 reviewed the effect of proprioceptive and balance training on outcomes in both ACL-deficient and ACL-reconstructed knees. Proprioceptive and balance training were associated with improvements in knee joint position sense, muscle strength, perceived knee function, and hop testing in ACL-deficient knees. Only 1 study examined ACL-reconstructed knees and found improvements in quadriceps and hamstring strength as well as proprioception. Also, there were no differences in laxity and strength for proprioceptive and balance training versus standard rehabilitation in ACL-deficient or -reconstructed knees. Zech et al238 reviewed the effects of neuromuscular and proprioceptive training for treating various musculoskeletal conditions, including ACL injuries. ACL-deficient knees showed significant improvements in knee function, function for activities of daily living, and single-leg hop testing and decreased instability after neuromuscular and proprioceptive training. Alternatively, training did not have a significant effect on outcome scores, ROM, and single-leg hop testing.
Miscellaneous Rehabilitation
van Grinsven et al215 reviewed 32 studies on evidence-based ACL rehabilitation. Based on their findings, the authors recommended accelerated rehabilitation without postoperative bracing to aid in reducing pain, swelling, and inflammation; regaining ROM; and providing strength and neuromuscular control.215 Also, patient education is an important part of the rehabilitation process. Pereira et al163 reviewed 5 studies comparing rehabilitation for BPTB versus HT grafts and found no differences between these grafts; however, the authors recommended that emphasis should be placed on knee flexion strength for HT grafts. Wasielewski et al222 systematically reviewed 8 studies that evaluated electromyographic biofeedback of the quadriceps femoris as an adjunct to therapeutic exercise in multiple knee conditions, including ACL-reconstructed knees, which showed some improvement in functional outcomes and extensor torque. However, only 2 studies examined the effect of electromyographic biofeedback in ACL-reconstructed knees, and thus, further research is warranted.
Return to Play
Rates of Return to Play
Ardern et al7,9 published 2 systematic reviews and meta-analyses that evaluated the rate of return to sports and associated factors after ACL reconstruction. Rates of return to any sport, previous level of competition, and competitive sports were 81% to 82%, 63% to 65%, and 44% to 55%, respectively; although good outcome scores were observed in at least 85% of ACL reconstructions. Fear of reinjury (19%) and functional problems of the reconstructed knee (13%) were 2 of the most common reasons for not returning to sports. Factors associated with return to preinjury level of competition were younger age, male sex, a positive psychological response favored, and symmetric single-leg hop. Patients with HT grafts were almost twice as likely as patella tendon grafts to return to any sport; however, patients with patella tendon grafts were more likely to return to their preinjury level of competition. Czuppon et al45 systematically reviewed variables associated with return to play and found weak associations between return to sport and increased quadriceps function, decreased effusion, decreased pain, increased tibial rotation, lessened kinesiophobia, and higher preoperative motivation. Warner et al221 reviewed whether return to competition after ACL reconstruction varies between sports and found that patients are more likely to return to activities such as cycling and jogging than cutting and pivoting sports such as soccer and football. However, sports-specific data are not reported frequently in the literature.
Criteria for Return to Play
Barber-Westin and Noyes14 and Harris et al72 reviewed articles evaluating criteria used to determine unrestricted return to sport after ACL reconstruction and found that 40% to 65% of articles failed to list any return-to-sport criteria. Barber-Westin and Noyes14 reported that time from surgery to return to sport was the only criterion used in 32% of studies, and 15% of studies reported time from surgery to return to sport along with subjective criteria that could not be measured. Only 13% of studies utilized objective criteria for determining return to sport, which included muscle strength, thigh circumference, general knee examination, single-leg hop tests, and Lachman examination. Only 13% of studies used more than 1 criterion for determining return to sport. Harris et al72 observed that, when reported, 76% and 67% of studies allowed return to running at 3 months and return to cutting and pivoting sports at 6 months. Return to sports without restriction was allowed by 6 (57% of studies) to 9 months (86% of studies).
Narducci et al142 and Thomee et al207 conducted systematic reviews of articles that examined the use of functional performance tests for determining return to play after ACL reconstruction. Narducci et al142 determined that there is a paucity of literature on this subject. However, the authors concluded that multiple functional performance measures may be more useful for determining readiness for return to athletic participation than a single performance measure.142 Thomee et al207 recommended a Limb Symmetry Index of 100% and a single-leg hop of 90% (compared with the contralateral limb) on 2 maximal and 1 endurance series for return to competitive, contact, and pivoting sports. For return to recreational sports and noncontact or nonpivoting sports, the Limb Symmetry Index should be at least 90% and single-leg hop should be 90% on at least 1 maximal or 1 endurance test.
Summary
There is a high rate of return to sport overall (81%-82%) and a lower rate for competitive sports (44%-55%). The 2 most common reasons for not returning to sport are fear of reinjury and functional problems of the reconstructed knee. There is a lack of uniformity in definitions of return to sport across different studies, and 40% to 65% of studies do not report any return-to-sport criteria.
Outcomes Assessment
Children and Adolescents
Frosch et al60 analyzed 55 studies that examined clinical outcomes of ACL reconstruction in children and adolescents. At a median follow-up of 40 months, 84.2% of patients had excellent or good (grades A and B) IKDC scores and a mean Lysholm score of 96.3. Complications included rerupture (3.8%) and leg-length discrepancy or angular deformity (2.1%). The rate of leg-length difference or axis deviations was 5.8% in physeal sparing techniques and 1.9% in transphyseal approaches; however, Lysholm scores did not differ between these techniques. BPTB autografts were associated with a slightly greater risk of leg-length differences or axis deviations and fewer reruptures compared with HT grafts; however, IKDC scores were normal or near normal in 80% to 85% of patients for both BPTB and HT grafts. Lastly, fixation near the joint line resulted in a slightly higher rate of leg-length difference or axis deviations compared with fixation far from the joint, and rerupture rates did not differ between these strategies.
Adults Older Than 40 Years
Brown et al27 and Legnani et al108 systematically reviewed outcomes of ACL reconstruction in adults over 40 years of age. Legnani et al108 found good to excellent results based on IKDC scores (64%-93% were good to excellent), Lysholm scores (range, 88.5-95), and Tegner scores (range, 4.1-6.6). Brown et al27 also found good to excellent results based on IKDC scores (83.6% were good to excellent), Lysholm scores (approximately 91), and Tegner scores (approximately 4.8). Graft rupture was less than 2%, instrumented side-to-side laxity was less than 3 mm in 75% of patients, and results were similar regardless of graft type. These studies concluded that ACL reconstruction over the age of 40 years can produce satisfactory results.
Sex-Based Differences
Ryan et al180 performed a systematic review and meta-analysis of studies comparing outcomes of ACL reconstruction by sex and found no significant differences between male and female patients with regard to rerupture, contralateral ACL rupture, clinical postoperative laxity, and outcome scores. de Valk et al46 performed a meta-analysis of 6 studies that examined sex-based differences in activity level after ACL reconstruction and found that in 3 studies males had increased activity levels at a minimum 1-year follow-up compared with females (P = .02). Of the remaining 3 studies, 2 showed no significant difference in activity level at 12 to 26 months, and 1 demonstrated a significantly lower activity level in females at 6 years postoperatively.
Revision Surgery
Wright et al226 performed a systematic review of 21 studies that examined outcomes of revision ACL surgery. The mean IKDC subjective score was 74.8 ± 4.4, IKDC objective scores were grade A or B in 71.1% ± 5.4%, mean Lysholm score was 82.1 ± 3.3, mean Tegner score was 6.1, and the mean Cincinnati score was 81. Overall patient satisfaction was 80%; however, return to unrestricted activity or prior level of activity was 54%. Patient-reported outcomes were inferior to those reported in the literature for primary ACL reconstructions, but the clinical relevance of these discrepancies is unknown. Objective failure (repeat revision, >5 mm of laxity compared with contralateral limb, or grades 2-3 pivot shift) occurred in 13.7% ± 2.7%, which is 3 to 4 times greater than failure rates reported in the literature for primary ACL reconstructions.
Body Mass Index
de Valk et al46 found that patients with increased baseline BMI had lower activity level after SB ACL reconstruction. Kluczynski et al97 systematically reviewed 7 studies that examined the effect of BMI on outcomes after ACL reconstruction. Four of these studies found an association between BMI and worse outcome measures, and only 3 of these studies evaluated the association between complications and BMI, but none observed significant findings.97
Surgical Timing
Smith et al193 compared outcomes for early (mean, 3 weeks postinjury) versus late (>6 weeks postinjury) ACL reconstruction and found no statistically significant differences in outcome scores, patient satisfaction, return to play, laxity, ROM, arthrofibrosis, chondral injuries, patellofemoral pain, meniscal injuries, thromboembolic episodes, or need for revision surgery. de Valk et al46 also compared early versus delayed ACL reconstruction and concluded that early reconstructions performed within 2 to 12 weeks of injury resulted in increased activity levels compared with delayed reconstructions performed beyond 12 weeks. Kwok et al104 performed a meta-analysis to compare the risk of stiffness between early and delayed ACL reconstruction with a modern accelerated rehabilitation protocol and found no statistically significant differences in stiffness, ROM, adverse events, and extension and flexion deficits. Andernord et al5 systematically reviewed 22 studies that evaluated postoperative outcomes and timing of ACL reconstruction. Eight articles found support for early (2 days to 7 months postinjury) reconstruction, but there were no differences in subjective and objective outcomes for early versus delayed (3 weeks to 24 years) ACL reconstruction in most studies. However, there was great variation in defining the interval from injury to surgery between studies, and the authors emphasized taking caution with delaying surgery given that the long-term risk of meniscal and chondral injury posed by delays in surgery is not well known.
Intra-articular Injuries
Magnussen and Spindler124 examined the association between concomitant meniscal and articular cartilage injuries and outcomes at a minimum of 5 years after ACL reconstruction. The majority of studies demonstrated increased radiographic arthritis in ACL-reconstructed knees with associated meniscus and cartilage injuries observed at the time of reconstruction. There is insufficient evidence to determine if these concomitant injuries affect clinical outcomes. Alternatively, de Valk et al46 found that patients with meniscal injuries demonstrated worse clinical outcomes at 2 to 6 years after ACL reconstruction; however, results were inconclusive regarding the association between chondral injuries and outcomes.
Psychological Factors
te Wierike et al206 systematically reviewed psychological factors and outcomes after ACL reconstruction in athletes. A greater internal locus of control and increased self-efficacy before ACL reconstruction were associated with improvements in postoperative outcomes. Athletes with low levels of fear of reinjury had better postoperative outcomes, and athletes who returned to sport had less fear of reinjury. Everhart et al51 also found patient self-confidence, optimism, self-motivation, stress, social support, and athletic self-identity to be predictive of clinical outcomes, including return to sport, rehabilitation compliance, knee pain, and knee function after ACL reconstruction.
Pivot Shift
Ayeni et al12 systematically reviewed 65 studies to determine whether the pivot shift test was associated with functional outcomes after ACL reconstruction. Forty-seven studies included pivot shift as an outcome measure, of which 40 (85%) found that the pivot shift test correlated with functional outcomes. Zaffagnini et al236 systematically reviewed 12 studies demonstrating that anatomic DB ACL reconstruction can effectively eliminate pathological translation and rotation during pivot-shift testing using quantitative measures.
Operative Versus Nonoperative Treatment
Chalmers et al31 reviewed 29 studies with at least 10-year follow-up that compared operative and nonoperative management of ACL injuries. ACL reconstruction was associated with fewer meniscal injuries and subsequent surgeries than nonoperative management; however, there were no differences in IKDC scores, Tegner scores, Lysholm scores, and radiographic arthritis between the 2 groups.
Outcome Assessment Measures
Wera et al223 performed a systematic review to determine IKDC score reporting relative to other functional scores worldwide. The most commonly reported outcome score was the Lysholm knee score, followed by the objective IKDC, subjective IKDC, and Tegner Activity Level scales. The authors recommended administering subjective and objective IKDC scores in conjunction with the Tegner activity scale after ACL reconstruction. Wang et al220 examined 24 patient-reported outcome scoring instruments for psychometric properties including reliability, validity, and responsiveness for a variety of knee conditions. For ACL reconstructions, the Cincinnati Knee Rating System (Cincinnati score), Knee Injury and Osteoarthritis Outcome Score (KOOS), and Lysholm scores are recommended for assessing patient-reported outcomes. Engelen-van Melick et al50 reviewed 6 studies to determine the most commonly used performance outcome measures 2 years after ACL reconstruction and found that concentric and isometric quadriceps and hamstring strength, limb symmetry index, and single-leg hop test were the most commonly used.
Health-Related Quality of Life
Filbay et al53 systematically reviewed 14 articles examining health-related quality of life (HRQoL) at a minimum of 5 years after ACL reconstruction and found that graft type, sex, age at surgery, and time from injury to surgery were not related to HRQoL. Revision surgery, injuries after ACL reconstruction, and severe radiographic OA were associated with reduced HRQoL scores at 5 years. At 10-year follow-up, concomitant meniscal injuries observed at the time of ACLR were associated with worse HRQoL scores.
Bone Mineral Density
Nyland et al149 examined the effects of ACL injury and treatment on bone mineral density, integrity, and mass. Eight studies reported results after ACL reconstruction or revision reconstruction, 1 evaluated suture repair, and 1 evaluated nonsurgical management. All studies reported varying reductions in bone mineral density, integrity, and mass that did not return to normal after reconstruction or rehabilitation. Reduction in bone integrity was reported most commonly at the patella, distal femur, and proximal tibia (5 studies each), the proximal femur and hip (3 studies), the calcaneus (2 studies), and the entire injured lower extremity (1 study). Bone loss was most pronounced with immobilization, limited weightbearing, and disuse, but it was also observed in 2 studies utilizing accelerated rehabilitation protocols. Two studies compared operative with nonoperative ACL management and found decreased bone mineral density at multiple sites in each group after treatment. One study also demonstrated increased bone loss in the femur, proximal tibia, and patella of patients treated 1 year after ACL reconstruction.
Postural Control, Gait, Stance, and Proprioception
Howells et al82 reviewed lower limb postural control in patients after ACL reconstruction versus healthy controls. At a mean 29-month follow-up, patients with ACL reconstructions demonstrated impaired lower limb postural control in both static and dynamic testing. Differences were most notable with backward perturbation and unstable testing platforms. Negahban et al143 also reviewed postural control after ACL reconstruction and found differences in postural control during single-leg stance in both the injured and the contralateral uninjured legs when compared with healthy controls. They reported that injury to the ACL is related to impaired postural control in both legs, which should be taken into account during rehabilitation.
Shi et al191 performed a meta-analysis evaluating proprioception and knee kinematics of ACL-reconstructed knees during level walking. Several parameters of level gait returned to normal after ACL reconstruction and rehabilitation, including step length, walking speed, proprioception, and maximum flexion angle during loading response. However, multiple parameters did not significantly improve after ACL reconstruction, including peak knee flexion angle, maximum angular knee flexion excursion during stance, peak knee flexion moment during walking, and maximum tibial rotation throughout the gait cycle. Gokeler et al66 reviewed kinematics of gait after ACL reconstruction and concluded that biomechanical differences in gait, including ROM and extension moments, are common after ACL reconstruction. These differences may be found up to 5 years after reconstruction and may never normalize. Hart et al73 examined sagittal plane knee kinetics in ACL-deficient and ACL-reconstructed limbs compared with uninjured limbs or healthy controls during functional tasks. Large effect sizes were demonstrated in walking, jogging, and stair climbing for both ACL-deficient and reconstructed knees as well as respective controls, indicating a considerable difference in sagittal plane knee kinetics with or without ACL reconstruction.
Relph et al178 conducted a meta-analysis that compared the effects of operative with nonoperative ACL management on knee joint proprioception. Proprioception was significantly worse in knees with ACL injuries than uninjured controls. Patients with ACL reconstruction demonstrated significantly improved proprioception compared with those treated nonoperatively. Gokeler et al65 reviewed proprioceptive differences between ACL-deficient and reconstructed knees and their correlation with clinical function. While proprioceptive differences exist, these differences only demonstrate low to moderate correlation with outcome scores and functional testing.
In summary, ACL injuries have been shown to be associated with impaired postural control in both legs and worse proprioception. After ACL reconstruction, proprioception may improve but biomechanical differences in gait may remain for at least 5 years or perhaps permanently after surgery.
Quadriceps and Hamstring Muscle Strength
Hart et al74 reviewed studies investigating voluntary quadriceps activation deficits after acute knee injury. Quadriceps activation deficits were present and deemed to be clinically meaningful in both ACL-deficient and reconstructed knees; however, quadriceps activation deficits were less for reconstructed compared with ACL-deficient knees. Quadriceps activation deficits are also commonly found in the contralateral uninjured limb after ACL injury and reconstruction, which may confound return-to-play considerations. Palmieri-Smith et al153 reviewed voluntary quadriceps activation after ACL reconstruction and suggested that clinicians incorporate strategies to decrease arthrogenic muscle inhibition and utilize therapy to decrease muscle atrophy, which could expedite and maximize patient recovery. Lepley and Palmieri-Smith109 reviewed 4 studies examining eccentric exercise and found that eccentric strengthening maximizes quadriceps function with initiation as early as 3 weeks after ACL reconstruction in 2 studies. Kim et al94 and Imoto et al87 reviewed studies evaluating neuromuscular electrical stimulation after ACL reconstruction. Both studies concluded that electrical stimulation combined with exercise may improve quadriceps strength more effectively than exercise alone. Imoto et al87 reported significant improvements in quadriceps strength and outcome scores 6 to 8 weeks postoperatively when electrical stimulation was utilized.
Ardern and Webster8 examined knee flexion strength after HT ACL reconstruction using single- or double-tendon harvest, and no significant differences were found for clinical outcome scores, laxity, single-leg hop, and single-leg vertical jump between groups. Isometric strength at more than 70° (1 study) and standing knee flexion angle (2 studies) were significantly decreased in the double-tendon harvest group. Petersen et al164 reviewed strength deficits after ACL reconstruction in 61 articles, of which 59 identified deficiencies in knee flexor and extensor strength when compared with healthy controls or the contralateral limb. Six studies identified deficits in hip extension, and strength deficits were greatest in the first 6 months after surgery but could persist for 2 or more years. Extension deficits were associated with patella tendon grafts, and flexion deficits were associated with HT grafts; however, flexion deficits were reduced in allograft HT reconstructions. Single-tendon harvest may preserve flexion strength more than gracilis and semitendinosus harvest. Also, given the prevalence of strength deficits, isokinetic testing is recommended before return to sport.
Arthritis
Several studies have examined long-term (>8-10 years) radiographic follow-up after ACL reconstruction and reported the prevalence of moderate to severe arthritis at 10 years after ACL reconstruction to be 27.9% and 23%, respectively.1,35 Meniscus injury and meniscectomy are 2 common risk factors of arthritis after ACL reconstruction.150 Three studies found increased rates of arthritis in patients with concomitant meniscus injuries (21%-50.4%) compared with no meniscus injury (0%-16.4%).1,35,123 The risk of developing arthritis after ACL reconstruction with concomitant partial meniscectomy was 3.5 to 5 times greater than without meniscectomy in 2 studies.35,123 One review found that ACL-injured knees had at least 3 times the risk of arthritis than uninjured contralateral knees. Operatively and nonoperatively treated knees demonstrated 3.62 times and 4.98 times the risk of developing any degree of arthritis than uninjured controls. However, ACL -reconstructed knees and nonoperatively treated knees demonstrated a risk of 4.71 times and 2.41 times, respectively, for development of moderate to severe arthritis compared with controls.
Van Ginckel et al214 examined cartilage changes on MRI up to 11 years after ACL injury. Early osteoarthritis was observed after operative and nonoperative management. ACL-reconstructed knees had more chondral change than nonsurgical knees after 1 year. Also, there is greater risk of cartilage loss in nonsurgical knees over the long term versus ACL-reconstructed knees.
Xie et al232 performed a systematic review and meta-analysis of 14 studies comparing osteoarthritis between patella tendon and HT autografts at a minimum of 5 years after reconstruction. The risk of radiographic arthritis was 61% greater for patella tendon versus HT autografts.
In summary, ACL injury has been shown to be associated with increased risk of arthritis in cases treated operatively and nonoperatively. Meniscus injury, meniscectomy, and patellar tendon autografts are risk factors for arthritis after ACL reconstruction.
Complications
Intraoperative Graft Contamination
Khan et al93 reviewed 6 laboratory studies that examined contamination of 495 ACL grafts using cultures to verify sterilization. Clorhexidine was the preferred agent for sterilization based on a high success rate (98%) in 90 specimens. Serial dilution with a polymyxin B and bacitracin solution demonstrated 100% success in 10 specimens. Normal saline solution, povidone-iodine, and a polymyxin B and bacitracin solution provided sterilization in only 60%, 48%, and 57% of specimens, respectively.
Postoperative Knee Sepsis
Several reviews have reported the incidence of septic arthritis after ACL reconstruction to range from 0.5% to 0.6%.95,187,219 Surgical irrigation and debridement combined with antibiotic therapy was the recommended treatment as opposed to antibiotics alone, which may lead to more failures.95,219 The mean number of debridements ranged from 1.52 to 1.92, with 34% to 40% of patients needing more than 1 debridement.95,187,219 Graft retention rates ranged from 77% to 85%, and failures were increased for allografts versus autografts. Mean Lysholm score at final follow-up was 80.2.95
Graft Failure
Crawford et al43 systematically reviewed 14 clinical trials that reported the rates of graft ruptures and clinical failures 10 years after ACL reconstruction. The long-term graft rupture rate was 6.2%. The rate of graft failure was 10.3%, defined as IKDC scores of C or D, instability on Lachman or pivot shift examination, and KT arthrometer laxity greater than 5 mm compared with the uninjured side.
Contralateral ACL Injury
Wright et al227 reviewed 6 studies that examined contralateral ACL injury after ACL reconstruction and found the contralateral injury rate to be 11.8% compared with an ipsilateral graft rupture rate of 5.8%. Sward et al203 systematically reviewed articles that examined the incidence and intrinsic and extrinsic risk factors of contralateral ACL injuries. The risk of sustaining a contralateral ACL injury ranged from 2% to 4%, which is greater than the risk of sustaining a first-time ACL injury. Return to a high activity level after a unilateral ACL injury was the most important risk factor for a contralateral ACL injury. However, there was inconclusive evidence to determine whether contralateral ACL injury was associated with a narrow intercondylar notch, female sex, or family history.
Hamstring Rupture
de Visser et al47 found that ACL reconstruction is a risk factor for recurrent hamstring rupture.
Miscellaneous Topics
ACL Mucoid Degeneration
Mucoid degeneration of the ACL is a rare condition that is often underdiagnosed or misdiagnosed. Lintz et al116 performed a review article of level 4 studies that examined mucoid degeneration and found that this condition arises from an initial injury to the ACL synovial lining secondary to acute trauma or chronic impingement. The authors recommended conservative arthroscopic resection of the mucoid substance and notchplasty with preservation of the ACL as opposed to complete resection with reconstruction.
Partial ACL Tears
The natural history and treatment strategy for partial ACL tears remains controversial. Pujol et al173 performed a level 4 systematic review of 12 studies that evaluated clinical and functional outcome measures after partial ACL injury. Despite good outcomes of partial ACL tears in the medium-term when patients limited sports activity, a positive pivot shift test emerged in 26% of cases, suggesting progression of laxity over time. The authors concluded that indications for the reconstruction or augmentation of partial ACL tears are therefore similar to complete ACL tears and include patients with a soft stop on Lachman test, functional instability, and those that wish to return to pivot sports.
Definitions of Acute Versus Chronic Injury
Acute and chronic injuries are not well defined within the sports medicine literature. Flint et al55 evaluated the literature in an attempt to define terms related to chronicity of several commonly treated sports injuries. With respect to the ACL literature, 77% of authors described acute injuries as those being less than 6 weeks old, and 64% described chronic tears as being at least 3 months old but typically greater than 6 months old. The variability was thought to be related to the complex nature of the injury and the fact that ACL reconstruction rarely becomes more challenging with prolonged delays.
Level of Evidence in ACL Research
Samuelsson et al185 utilized the Oxford Centre level of evidence rating system to categorize study type and level of evidence of 1510 studies on primary ACL reconstruction. The most frequent study type was a case series (32.7%) followed by randomized control trials (9.2%). The authors concluded that most therapeutic studies were low-level evidence and that there was a positive correlation between the impact factor of the journal and the mean level of evidence.
Conclusion
This systematic review provides a comprehensive summary of published systematic reviews and meta-analyses on various topics pertaining to the ACL. A large body of literature with substantial evidence has been established for several topics. The epidemiology of ACL injuries has been well researched, particularly intrinsic and extrinsic risk factors as well as the incidence of ACL injury by sport. There is also a plethora of studies on diagnostic criteria for ACL injuries as well as outcomes assessments. Many studies have compared single- and double-bundle ACL reconstructions and in general have found comparable outcomes. There is substantial evidence in the rehabilitation literature supporting the notions that (1) there is no added benefit from knee brace or CPM, (2) accelerated rehabilitation and open chain exercises may be beneficial, (3) cryotherapy is safe and effective, and (4) resistance and proprioceptive training can be beneficial after surgery. Several reviews have also shown that ACL injuries, treated operatively or nonoperatively, are associated with increased risk of knee arthritis.
Many topics are still lacking in evidence. The majority of studies evaluating associated knee injuries in patients with ACL injuries has focused on meniscus tears; however, more studies are needed to assess outcomes after multiligament tears and bone bruising in the presence of an ACL injury. Also, more studies comparing BPTB allografts versus BPTB autografts are needed because the reviews to date have shown discrepant findings. Better quality studies are also needed to assess the outcomes of synthetic grafts and quadriceps tendon autografts because the current evidence may be biased with regard to sample selection. More research is needed to assess the long-term outcomes of metal versus bioabsorbable screws. Further research is needed to determine whether copers (ie, no impairment/disability after ACL injury) have better outcomes after nonoperative management compared with noncopers, and also, more studies comparing operative versus nonoperative management in skeletally immature patients are needed because thus far the findings have been divergent. Several reviews have examined the use of PRP for ACL reconstructions; however, the current evidence is of low quality and PRP methodology varies between studies. More research comparing home- versus clinic-based physical therapy is warranted, as well as the effects of electromyographic biofeedback during physical therapy. A standardized definition of return to play is lacking from the literature, and many studies do not provide any definition of return to play. Finally, this summary of systematic reviews on the ACL can supply the surgeon with a single source for the most up-to-date synthesis of the literature.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Ralph C. Wilson Foundation.
References
- 1. Ajuied A, Wong F, Smith C, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42:2242–2252. [DOI] [PubMed] [Google Scholar]
- 2. Alentorn-Geli E, Lajara F, Samitier G, Cugat R. The transtibial versus the anteromedial portal technique in the arthroscopic bone-patellar tendon-bone anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1013–1037. [DOI] [PubMed] [Google Scholar]
- 3. Alentorn-Geli E, Mendiguch, ía J, Samuelsson K, et al. Prevention of anterior cruciate ligament injuries in sports. Part I: systematic review of risk factors in male athletes. Knee Surg Sports Traumatol Arthrosc. 2014;22:3–15. [DOI] [PubMed] [Google Scholar]
- 4. Alentorn-Geli E, Mendiguch, ía J, Samuelsson K, et al. Prevention of non-contact anterior cruciate ligament injuries in sports. Part II: systematic review of the effectiveness of prevention programmes in male athletes. Knee Surg Sports Traumatol Arthrosc. 2014;22:16–25. [DOI] [PubMed] [Google Scholar]
- 5. Andernord D, Karlsson J, Musahl V, Bhandari M, Fu FH, Samuelsson K. Timing of surgery of the anterior cruciate ligament. Arthroscopy. 2013;29:1863–1871. [DOI] [PubMed] [Google Scholar]
- 6. Andersson D, Samuelsson K, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: an assessment of randomized controlled trials. Arthroscopy. 2009;25:653–685. [DOI] [PubMed] [Google Scholar]
- 7. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–1552. [DOI] [PubMed] [Google Scholar]
- 8. Ardern CL, Webster KE. Knee flexor strength recovery following hamstring tendon harvest for anterior cruciate ligament reconstruction: a systematic review. Orthop Rev (Pavia). 2009;1(2):e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596–606. [DOI] [PubMed] [Google Scholar]
- 10. Arneja S, McConkey MO, Mulpuri K, et al. Graft tensioning in anterior cruciate ligament reconstruction: a systematic review of randomized controlled trials. Arthroscopy. 2009;25:200–207. [DOI] [PubMed] [Google Scholar]
- 11. Augustsson J. Documentation of strength training for research purposes after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1849–1855. [DOI] [PubMed] [Google Scholar]
- 12. Ayeni OR, Chahal M, Tran MN, Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20:767–777. [DOI] [PubMed] [Google Scholar]
- 13. Balazs GC, Pavey GJ, Brelin AM, Pickett A, Keblish DJ, Rue JP. Risk of anterior cruciate ligament injury in athletes on synthetic playing surfaces: a systematic review. Am J Sports Med. 2014;43:1798–1804. [DOI] [PubMed] [Google Scholar]
- 14. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697–1705. [DOI] [PubMed] [Google Scholar]
- 15. Beaufils P, Hulet C, Dhenain M, Nizard R, Nourissat G, Pujol N. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95:437–442. [DOI] [PubMed] [Google Scholar]
- 16. Belanger L, Burt D, Callaghan J, Clifton S, Gleberzon BJ. Anterior cruciate ligament laxity related to the menstrual cycle: an updated systematic review of the literature. J Can Chiropr Assoc. 2013;57:76–86. [PMC free article] [PubMed] [Google Scholar]
- 17. Benjaminse A, Gokeler A, Fleisig GS, Sell TC, Otten B. What is the true evidence for gender-related differences during plant and cut maneuvers? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2011;19:42–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Benjaminse A, Gokeler A, van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36:267–288. [DOI] [PubMed] [Google Scholar]
- 19. Benjaminse A, Welling W, Otten B, Gokeler A. Novel methods of instruction in ACL injury prevention programs, a systematic review. Phys Ther Sport. 2015;16:176–186. [DOI] [PubMed] [Google Scholar]
- 20. Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res. 2007;458:180–187. [DOI] [PubMed] [Google Scholar]
- 21. Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS. Bone–patellar tendon–bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ. 2006;332:995–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Björnsson H, Desai N, Musahl V, et al. Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:696–739. [DOI] [PubMed] [Google Scholar]
- 23. Bogunovic L, Tarabichi M, Harris D, Wright R. Treatment of tibial eminence fractures: a systematic review. J Knee Surg. 2015;28:255–262. [DOI] [PubMed] [Google Scholar]
- 24. Boks SS, Vroegindeweij D, Koes BW, Hunink MG, Bierma-Zeinstra SM. Follow-up of posttraumatic ligamentous and meniscal knee lesions detected at MR imaging: systematic review. Radiology. 2006;238:863–871. [DOI] [PubMed] [Google Scholar]
- 25. Bonanzinga T, Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Neri MP, Marcacci M. Management of combined anterior cruciate ligament-posterolateral corner tears: a systematic review. Am J Sports Med. 2013;42:1496–1503. [DOI] [PubMed] [Google Scholar]
- 26. Brophy RH, Zeltser D, Wright RW, Flanigan D. Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: incidence and treatment. Arthroscopy. 2010;26:112–120. [DOI] [PubMed] [Google Scholar]
- 27. Brown CA, McAdams TR, Harris AH, Maffulli N, Safran MR. ACL reconstruction in patients aged 40 years and older: a systematic review and introduction of a new methodology score for ACL studies. Am J Sports Med. 2013;41:2181–2190. [DOI] [PubMed] [Google Scholar]
- 28. Carey JL, Dunn WR, Dahm DL, Zeger SL, Spindler KP. A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. J Bone Joint Surg Am. 2009;91:2242–2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carson DW, Ford KR. Sex differences in knee abduction during landing: a systematic review. Sports Health. 2011;3:373–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chalmers PN, Mall NA, Cole BJ, Verma NN, Bush-Joseph CA, Bach BR., Jr Anteromedial versus transtibial tunnel drilling in anterior cruciate ligament reconstructions: a systematic review. Arthroscopy. 2013;29:1235–1242. [DOI] [PubMed] [Google Scholar]
- 31. Chalmers PN, Mall NA, Moric M, et al. Does ACL reconstruction alter natural history? A systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96:292–300. [DOI] [PubMed] [Google Scholar]
- 32. Chen XZ, Liu CG, Chen Y, Wang LQ, Zhu QZ, Lin P. Arthroscopy-assisted surgery for tibial plateau fractures. Arthroscopy. 2015;31:143–153. [DOI] [PubMed] [Google Scholar]
- 33. Cheng T, Liu T, Zhang G, Zhang X. Computer-navigated surgery in anterior cruciate ligament reconstruction: are radiographic outcomes better than conventional surgery? Arthroscopy. 2011;27:97–100. [DOI] [PubMed] [Google Scholar]
- 34. Cheng T, Zhang GY, Zhang XL. Does computer navigation system really improve early clinical outcomes after anterior cruciate ligament reconstruction? A meta-analysis and systematic review of randomized controlled trials. Knee. 2012;19:73–77. [DOI] [PubMed] [Google Scholar]
- 35. Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1967–1976. [DOI] [PubMed] [Google Scholar]
- 36. Claes S, Verdonk P, Forsyth R, Bellemans J. The “ligamentization” process in anterior cruciate ligament reconstruction: what happens to the human graft? A systematic review of the literature. Am J Sports Med. 2011;39:2476–2483. [DOI] [PubMed] [Google Scholar]
- 37. Clifton R, Haleem S, McKee A, Parker MJ. Closed suction surgical wound drainage after anterior cruciate ligament reconstruction: a systematic review of randomised controlled trials. Knee. 2007;14:348–351. [DOI] [PubMed] [Google Scholar]
- 38. Colvin A, Sharma C, Parides M, Glashow J. What is the best femoral fixation of hamstring autografts in anterior cruciate ligament reconstruction? A meta-analysis. Clin Orthop Relat Res. 2011;469:1075–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Conte EJ, Hyatt AE, Gatt CJ, Jr, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30:882–890. [DOI] [PubMed] [Google Scholar]
- 40. Cooper RL, Taylor NF, Feller JA. A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligament. Res Sports Med. 2005;13:163–178. [DOI] [PubMed] [Google Scholar]
- 41. Coppola SM, Collins SM. Is physical therapy more beneficial than unsupervised home exercise in treatment of post surgical knee disorders? A systematic review. Knee. 2009;16:171–175. [DOI] [PubMed] [Google Scholar]
- 42. Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84:5–23. [DOI] [PubMed] [Google Scholar]
- 43. Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1566–1571. [DOI] [PubMed] [Google Scholar]
- 44. Cvetanovich GL, Mascarenhas R, Saccomanno MF, et al. Hamstring autograft versus soft-tissue allograft in anterior cruciate ligament reconstruction: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy. 2014;30:1616–1624. [DOI] [PubMed] [Google Scholar]
- 45. Czuppon S, Racette BA, Klein SE, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2014;48:356–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. de Valk EJ, Moen MH, Winters M, Bakker EW, Tamminga R, van der Hoeven H. Preoperative patient and injury factors of successful rehabilitation after anterior cruciate ligament reconstruction with single-bundle techniques. Arthroscopy. 2013;29:1879–1895. [DOI] [PubMed] [Google Scholar]
- 47. de Visser HM, Reijman M, Heijboer MP, Bos PK. Risk factors of recurrent hamstring injuries: a systematic review. Br J Sports Med. 2012;46:124–130. [DOI] [PubMed] [Google Scholar]
- 48. Desai N, Bj, örnsson H, Musahl V, et al. Anatomic single- versus double-bundle ACL reconstruction: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2014;22:1009–1023. [DOI] [PubMed] [Google Scholar]
- 49. Emond CE, Woelber EB, Kurd SK, Ciccotti MG, Cohen SB. A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: a meta-analysis. J Bone Joint Surg Am. 2011;93:572–580. [DOI] [PubMed] [Google Scholar]
- 50. Engelen-van Melick N, van Cingel RE, Tijssen MP, Nijhuis-van der Sanden MW. Assessment of functional performance after anterior cruciate ligament reconstruction: a systematic review of measurement procedures. Knee Surg Sports Traumatol Arthrosc. 2013;21:869–879. [DOI] [PubMed] [Google Scholar]
- 51. Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:752–762. [DOI] [PubMed] [Google Scholar]
- 52. Farshad M, Gerber C, Meyer DC, Schwab A, Blank PR, Szucs T. Reconstruction versus conservative treatment after rupture of the anterior cruciate ligament: cost effectiveness analysis. BMC Health Serv Res. 2011;11:317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Filbay SR, Ackerman IN, Russell TG, Macri EM, Crossley KM. Health-related quality of life after anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2014;42:1247–1255. [DOI] [PubMed] [Google Scholar]
- 54. Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH. Prevalence of chondral defects in athletes’ knees: a systematic review. Med Sci Sports Exerc. 2010;42:1795–1801. [DOI] [PubMed] [Google Scholar]
- 55. Flint JH, Wade AM, Giuliani J, Rue JP. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2014;42:235–241. [DOI] [PubMed] [Google Scholar]
- 56. Forster MC, Forster IW. Patellar tendon or four-strand hamstring? A systematic review of autografts for anterior cruciate ligament reconstruction. Knee. 2005;12:225–230. [DOI] [PubMed] [Google Scholar]
- 57. Foster TE, Wolfe BL, Ryan S, Silvestri L, Kaye EK. Does the graft source really matter in the outcome of patients undergoing anterior cruciate ligament reconstruction? An evaluation of autograft versus allograft reconstruction results: a systematic review. Am J Sports Med. 2010;38:189–199. [DOI] [PubMed] [Google Scholar]
- 58. Fox AS, Bonacci J, McLean SG, Spittle M, Saunders N. What is normal? Female lower limb kinematic profiles during athletic tasks used to examine anterior cruciate ligament injury risk: a systematic review. Sports Med. 2014;44:815–832. [DOI] [PubMed] [Google Scholar]
- 59. Frosch KH, Preiss A, Heider S, et al. Primary ligament sutures as a treatment option of knee dislocations: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1502–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Frosch KH, Stengel D, Brodhun T, et al. Outcomes and risks of operative treatment of rupture of the anterior cruciate ligament in children and adolescents. Arthroscopy. 2010;26:1539–1550. [DOI] [PubMed] [Google Scholar]
- 61. Gadikota HR, Seon JK, Chen CH, Wu JL, Gill TJ, Li G. In vitro and intraoperative laxities after single-bundle and double-bundle anterior cruciate ligament reconstructions. Arthroscopy. 2011;27:849–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Gagnier JJ, Morgenstern H, Chess L. Interventions designed to prevent anterior cruciate ligament injuries in adolescents and adults: a systematic review and meta-analysis. Am J Sports Med. 2013;41:1952–1962. [DOI] [PubMed] [Google Scholar]
- 63. George MS, Huston LJ, Spindler KP. Endoscopic versus rear-entry ACL reconstruction: a systematic review. Clin Orthop Relat Res. 2007;455:158–161. [DOI] [PubMed] [Google Scholar]
- 64. Glass R, Waddell J, Hoogenboom B. The effects of open versus closed kinetic chain exercises on patients with ACL deficient or reconstructed knees: a systematic review. N Am J Sports Phys Ther. 2010;5:74–84. [PMC free article] [PubMed] [Google Scholar]
- 65. Gokeler A, Benjaminse A, Hewett TE, et al. Proprioceptive deficits after ACL injury: are they clinically relevant? Br J Sports Med. 2012;46:180–192. [DOI] [PubMed] [Google Scholar]
- 66. Gokeler A, Benjaminse A, van Eck CF, Webster KE, Schot L, Otten E. Return of normal gait as an outcome measurement in ACL reconstructed patients. A systematic review. Int J Sports Phys Ther. 2013;8:441–451. [PMC free article] [PubMed] [Google Scholar]
- 67. Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy. 2005;21:791–803. [DOI] [PubMed] [Google Scholar]
- 68. Grant JA, Tannenbaum E, Miller BS, Bedi A. Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthroscopy. 2012;28:110–122. [DOI] [PubMed] [Google Scholar]
- 69. Grimm NL, Shea KG, Leaver RW, Aoki SK, Carey JL. Efficacy and degree of bias in knee injury prevention studies: a systematic review of RCTs. Clin Orthop Relat Res. 2013;471:308–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Grodski M, Marks R. Exercises following anterior cruciate ligament reconstructive surgery: biomechanical considerations and efficacy of current approaches. Res Sports Med. 2008;16:75–96. [DOI] [PubMed] [Google Scholar]
- 71. Han DL, Nyland J, Kendzior M, Nawab A, Caborn DN. Intratunnel versus extratunnel fixation of hamstring autograft for anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:1555–1566. [DOI] [PubMed] [Google Scholar]
- 72. Harris JD, Abrams GD, Bach BR, et al. Return to sport after ACL reconstruction. Orthopedics. 2014;37:e103–e108. [DOI] [PubMed] [Google Scholar]
- 73. Hart JM, Ko JW, Konold T, Pietrosimone B. Sagittal plane knee joint moments following anterior cruciate ligament injury and reconstruction: a systematic review. Clin Biomech (Bristol, Avon). 2010;25:277–283. [DOI] [PubMed] [Google Scholar]
- 74. Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45:87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hensler D, Working ZM, Illingworth KD, Thorhauer ED, Tashman S, Fu FH. Medial portal drilling: effects on the femoral tunnel aperture morphology during anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2011;93:2063–2071. [DOI] [PubMed] [Google Scholar]
- 76. Herman K, Barton C, Malliaras P, Morrissey D. The effectiveness of neuromuscular warm-up strategies, that require no additional equipment, for preventing lower limb injuries during sports participation: a systematic review. BMC Med. 2012;10:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Herrington L, Fowler E. A systematic literature review to investigate if we identify those patients who can cope with anterior cruciate ligament deficiency. Knee. 2006;13:260–265. [DOI] [PubMed] [Google Scholar]
- 78. Herrington L, Wrapson C, Matthews M, Matthews H. Anterior cruciate ligament reconstruction, hamstring versus bone–patella tendon–bone grafts: a systematic literature review of outcome from surgery. Knee. 2005;12:41–50. [DOI] [PubMed] [Google Scholar]
- 79. Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34:490–498. [DOI] [PubMed] [Google Scholar]
- 80. Hewett TE, Myer GD, Ford KR. Reducing knee and anterior cruciate ligament injuries among female athletes: a systematic review of neuromuscular training interventions. J Knee Surg. 2005;18:82–88. [DOI] [PubMed] [Google Scholar]
- 81. Hewett TE, Zazulak BT, Myer GD. Effects of the menstrual cycle on anterior cruciate ligament injury risk: a systematic review. Am J Sports Med. 2007;35:659–668. [DOI] [PubMed] [Google Scholar]
- 82. Howells BE, Ardern CL, Webster KE. Is postural control restored following anterior cruciate ligament reconstruction? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2011;19:1168–1177. [DOI] [PubMed] [Google Scholar]
- 83. Hu J, Qu J, Xu D, Zhang T, Zhou J, Lu H. Clinical outcomes of remnant preserving augmentation in anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22:1976–1985. [DOI] [PubMed] [Google Scholar]
- 84. Hu J, Qu J, Xu D, Zhou J, Lu H. Allograft versus autograft for anterior cruciate ligament reconstruction: an up-to-date meta-analysis of prospective studies. Int Orthop. 2013;37:311–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Hwang MD, Piefer JW, Lubowitz JH. Anterior cruciate ligament tibial footprint anatomy: systematic review of the 21st century literature. Arthroscopy. 2012;28:728–734. [DOI] [PubMed] [Google Scholar]
- 86. Ilahi OA, Nolla JM, Ho DM. Intra-tunnel fixation versus extra-tunnel fixation of hamstring anterior cruciate ligament reconstruction: a meta-analysis. J Knee Surg. 2009;22:120–129. [DOI] [PubMed] [Google Scholar]
- 87. Imoto AM, Peccin S, Almeida GJ, Saconato H, Atallah AN. Effectiveness of electrical stimulation on rehabilitation after ligament and meniscal injuries: a systematic review. Sao Paulo Med J. 2011;129:414–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Jacobs CL, Hincapie CA, Cassidy JD. Musculoskeletal injuries and pain in dancers: a systematic review update. J Dance Med Sci. 2012;16:74–84. [PubMed] [Google Scholar]
- 89. Janssen RP, Scheffler SU. Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:2102–2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Jarvela T, Suomalainen P. ACL reconstruction with double-bundle technique: a review of clinical results. Phys Sportsmed. 2011;39:85–92. [DOI] [PubMed] [Google Scholar]
- 91. Kaeding CC, Flanigan D, Donaldson C. Surgical techniques and outcomes after anterior cruciate ligament reconstruction in preadolescent patients. Arthroscopy. 2010;26:1530–1538. [DOI] [PubMed] [Google Scholar]
- 92. Kaplan Y. Identifying individuals with an anterior cruciate ligament–deficient knee as copers and noncopers: a narrative literature review. J Orthop Sports Phys Ther. 2011;41:758–766. [DOI] [PubMed] [Google Scholar]
- 93. Khan M, Rothrauff BB, Merali F, Musahl V, Peterson D, Ayeni OR. Management of the contaminated anterior cruciate ligament graft. Arthroscopy. 2014;30:236–244. [DOI] [PubMed] [Google Scholar]
- 94. Kim KM, Croy T, Hertel J, Saliba S. Effects of neuromuscular electrical stimulation after anterior cruciate ligament reconstruction on quadriceps strength, function, and patient-oriented outcomes: a systematic review. J Orthop Sports Phys Ther. 2010;40:383–391. [DOI] [PubMed] [Google Scholar]
- 95. Kim SJ, Postigo R, Koo S, Kim JH. Infection after arthroscopic anterior cruciate ligament reconstruction. Orthopedics. 2014;37:477–484. [DOI] [PubMed] [Google Scholar]
- 96. Kirwan GW, Bourke MG, Chipchase L, Dalton PA, Russell TG. Initial graft tension and the effect on postoperative patient functional outcomes in anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:934–941. [DOI] [PubMed] [Google Scholar]
- 97. Kluczynski MA, Bisson LJ, Marzo JM. Does body mass index affect outcomes of ambulatory knee and shoulder surgery? Arthroscopy. 2014;30:856–865. [DOI] [PubMed] [Google Scholar]
- 98. Kongtharvonskul J, Attia J, Thamakaison S, Kijkunasathian C, Woratanarat P, Thakkinstian A. Clinical outcomes of double- vs single-bundle anterior cruciate ligament reconstruction: a systematic review of randomized control trials. Scand J Med Sci Sports. 2013;23:1–14. [DOI] [PubMed] [Google Scholar]
- 99. Kopf S, Musahl V, Tashman S, Szczodry M, Shen W, Fu FH. A systematic review of the femoral origin and tibial insertion morphology of the ACL. Knee Surg Sports Traumatol Arthrosc. 2009;17:213–219. [DOI] [PubMed] [Google Scholar]
- 100. Kraeutler MJ, Bravman JT, McCarty EC. Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med. 2013;41:2439–2448. [DOI] [PubMed] [Google Scholar]
- 101. Kristensen J, Franklyn-Miller A. Resistance training in musculoskeletal rehabilitation: a systematic review. Br J Sports Med. 2012;46:719–726. [DOI] [PubMed] [Google Scholar]
- 102. Kruse LM, Gray B, Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94:1737–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Krych AJ, Jackson JD, Hoskin TL, Dahm DL. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:292–298. [DOI] [PubMed] [Google Scholar]
- 104. Kwok CS, Harrison T, Servant C. The optimal timing for anterior cruciate ligament reconstruction with respect to the risk of postoperative stiffness. Arthroscopy. 2013;29:556–565. [DOI] [PubMed] [Google Scholar]
- 105. Lamblin CJ, Waterman BR, Lubowitz JH. Anterior cruciate ligament reconstruction with autografts compared with non-irradiated, non-chemically treated allografts. Arthroscopy. 2013;29:1113–1122. [DOI] [PubMed] [Google Scholar]
- 106. Lamsam C, Kaewpornsawan K, Luangsa-Ard J, Thephamongkhol K, Vanadurongwan B, Soparat K. Single-bundle versus double-bundle anterior cruciate ligament reconstruction: a meta-analysis. J Med Assoc Thai. 2012;95(suppl 9):S114–S121. [PubMed] [Google Scholar]
- 107. Laupattarakasem P, Laopaiboon M, Kosuwon W, Laupattarakasem W. Meta-analysis comparing bioabsorbable versus metal interference screw for adverse and clinical outcomes in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:142–153. [DOI] [PubMed] [Google Scholar]
- 108. Legnani C, Terzaghi C, Borgo E, Ventura A. Management of anterior cruciate ligament rupture in patients aged 40 years and older. J Orthop Traumatol. 2011;12:177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Lepley LK, Palmieri-Smith R. Effect of eccentric strengthening after anterior cruciate ligament reconstruction on quadriceps strength. J Sport Rehabil. 2013;22:150–156. [DOI] [PubMed] [Google Scholar]
- 110. Lewis PB, Parameswaran AD, Rue JP, Bach BR., Jr Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: a baseline assessment for consideration of double-bundle techniques. Am J Sports Med. 2008;36:2028–2036. [DOI] [PubMed] [Google Scholar]
- 111. Li S, Chen Y, Lin Z, Cui W, Zhao J, Su W. A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone–patellar tendon–bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg. 2012;132:1287–1297. [DOI] [PubMed] [Google Scholar]
- 112. Li S, Su W, Zhao J, et al. A meta-analysis of hamstring autografts versus bone-patellar tendon-bone autografts for reconstruction of the anterior cruciate ligament. Knee. 2011;18:287–293. [DOI] [PubMed] [Google Scholar]
- 113. Li X, Xu CP, Song JQ, Jiang N, Yu B. Single-bundle versus double-bundle anterior cruciate ligament reconstruction: an up-to-date meta-analysis. Int Orthop. 2013;37:213–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Li YL, Ning GZ, Wu Q, et al. Single-bundle or double-bundle for anterior cruciate ligament reconstruction: a meta-analysis. Knee. 2014;21:28–37. [DOI] [PubMed] [Google Scholar]
- 115. Linko E, Harilainen A, Malmivaara A, Seitsalo S. Surgical versus conservative interventions for ACL ruptures in adults. Cochrane Database Syst Rev. 2005;2:CD001356. [DOI] [PubMed] [Google Scholar]
- 116. Lintz F, Pujol N, Boisrenoult P, Bargoin K, Beaufils P, Dejour D. Anterior cruciate ligament mucoid degeneration: a review of the literature and management guidelines. Knee Surg Sports Traumatol Arthrosc. 2011;19:1326–1333. [DOI] [PubMed] [Google Scholar]
- 117. Lobb R, Tumilty S, Claydon LS. A review of systematic reviews on anterior cruciate ligament reconstruction rehabilitation. Phys Ther Sport. 2012;13:270–278. [DOI] [PubMed] [Google Scholar]
- 118. Longo UG, Buchmann S, Franceschetti E, Maffulli N, Denaro V. A systematic review of single-bundle versus double-bundle anterior cruciate ligament reconstruction. Br Med Bull. 2012;103:147–168. [DOI] [PubMed] [Google Scholar]
- 119. Lopomo N, Zaffagnini S, Amis AA. Quantifying the pivot shift test: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:767–783. [DOI] [PubMed] [Google Scholar]
- 120. Louw Q, Gillion N, van Niekerk SM, Morris L, Baumeister J. The effect of vision on knee biomechanics during functional activities: a systematic review. J Sci Med Sport. 2015;18:469–474. [DOI] [PubMed] [Google Scholar]
- 121. Machotka Z, Scarborough I, Duncan W, Kumar S, Perraton L. Anterior cruciate ligament repair with LARS (ligament advanced reinforcement system): a systematic review. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2011;19:462–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22:347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Magnussen RA, Spindler KP. The effect of patient and injury factors on long-term outcome after anterior cruciate ligament reconstruction. Curr Orthop Pract. 2011;22:90–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Mall NA, Wright RW. Femoral nerve block use in anterior cruciate ligament reconstruction surgery. Arthroscopy. 2010;26:404–416. [DOI] [PubMed] [Google Scholar]
- 126. Mariscalco MW, Magnussen RA, Mehta D, Hewett TE, Flanigan DC, Kaeding CC. Autograft versus nonirradiated allograft tissue for anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2014;42:492–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Martimbianco AL, Gomes da Silva BN, de Carvalho AP, Silva V, Torloni MR, Peccin MS. Effectiveness and safety of cryotherapy after arthroscopic anterior cruciate ligament reconstruction. A systematic review of the literature. Phys Ther Sport. 2014;15:261–268. [DOI] [PubMed] [Google Scholar]
- 128. Meredick RB, Vance KJ, Appleby D, Lubowitz JH. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36:1414–1421. [DOI] [PubMed] [Google Scholar]
- 129. Meuffels DE, Reijman M, Scholten RJ, Verhaar JA. Computer assisted surgery for knee ligament reconstruction. Cochrane Database Syst Rev. 2011;6:CD007601. [DOI] [PubMed] [Google Scholar]
- 130. Michaelidis M, Koumantakis GA. Effects of knee injury primary prevention programs on anterior cruciate ligament injury rates in female athletes in different sports: a systematic review. Phys Ther Sport. 2014;15:200–210. [DOI] [PubMed] [Google Scholar]
- 131. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 132. Mohtadi N, Grant J. Managing anterior cruciate ligament deficiency in the skeletally immature individual: a systematic review of the literature. Clin J Sport Med. 2006;16:457–464. [DOI] [PubMed] [Google Scholar]
- 133. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;9:CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Moksnes H, Engebretsen L, Risberg MA. The current evidence for treatment of ACL injuries in children is low: a systematic review. J Bone Joint Surg Am. 2012;94:1112–1119. [DOI] [PubMed] [Google Scholar]
- 135. Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM. Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91:2946–2957. [DOI] [PubMed] [Google Scholar]
- 136. Moraes VY, Lenza M, Tamaoki MJ, Faloppa F, Belloti JC. Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev. 2014;4:CD010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Moses B, Orchard J. Systematic review: annual incidence of ACL injury and surgery in various populations. Res Sports Med. 2012;20:157–179. [DOI] [PubMed] [Google Scholar]
- 138. Muaidi QI, Nicholson LL, Refshauge KM, Herbert RD, Maher CG. Prognosis of conservatively managed anterior cruciate ligament injury: a systematic review. Sports Med. 2007;37:703–716. [DOI] [PubMed] [Google Scholar]
- 139. Mulford JS, Chen D. Anterior cruciate ligament reconstruction: a systematic review of polyethylene terephthalate grafts. ANZ J Surg. 2011;81:785–789. [DOI] [PubMed] [Google Scholar]
- 140. Mulford JS, Hutchinson SE, Hang JR. Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:1882–1888. [DOI] [PubMed] [Google Scholar]
- 141. Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41:203–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Narducci E, Waltz A, Gorski K, Leppla L, Donaldson M. The clinical utility of functional performance tests within one-year post-ACL reconstruction: a systematic review. Int J Sports Phys Ther. 2011;6:333–342. [PMC free article] [PubMed] [Google Scholar]
- 143. Negahban H, Mazaheri M, Kingma I, van Dieen JH. A systematic review of postural control during single-leg stance in patients with untreated anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2014;22:1491–1504. [DOI] [PubMed] [Google Scholar]
- 144. Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94:2222–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Newman SD, Atkinson HD, Willis-Owen CA. Anterior cruciate ligament reconstruction with the ligament augmentation and reconstruction system: a systematic review. Int Orthop. 2013;37:321–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Noyes FR, Barber-Westin SD. Treatment of meniscus tears during anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:123–130. [DOI] [PubMed] [Google Scholar]
- 147. Noyes FR, Barber-Westin SD. Neuromuscular retraining intervention programs: do they reduce noncontact anterior cruciate ligament injury rates in adolescent female athletes? Arthroscopy. 2014;30:245–255. [DOI] [PubMed] [Google Scholar]
- 148. Noyes FR, Barber Westin SD. Anterior cruciate ligament injury prevention training in female athletes: a systematic review of injury reduction and results of athletic performance tests. Sports Health. 2012;4:36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Nyland J, Fisher B, Brand E, Krupp R, Caborn DN. Osseous deficits after anterior cruciate ligament injury and reconstruction: a systematic literature review with suggestions to improve osseous homeostasis. Arthroscopy. 2010;26:1248–1257. [DOI] [PubMed] [Google Scholar]
- 150. Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–1443. [DOI] [PubMed] [Google Scholar]
- 151. Owen JL, Campbell S, Falkner SJ, Bialkowski C, Ward AT. Is there evidence that proprioception or balance training can prevent anterior cruciate ligament (ACL) injuries in athletes without previous ACL injury? Phys Ther. 2006;86:1436–1440. [DOI] [PubMed] [Google Scholar]
- 152. Padua DA, Distefano LJ. Sagittal plane knee biomechanics and vertical ground reaction forces are modified following ACL injury prevention programs: a systematic review. Sports Health. 2009;1:165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27:405–424. [DOI] [PubMed] [Google Scholar]
- 154. Papalia R, Franceschi F, Zampogna B, Tecame A, Maffulli N, Denaro V. Surgical management of partial tears of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2014;22:154–165. [DOI] [PubMed] [Google Scholar]
- 155. Papalia R, Franceschi F, Vasta S, Di Martino A, Maffulli N, Denaro V. Sparing the anterior cruciate ligament remnant: is it worth the hassle? Br Med Bull. 2012;104:91–111. [DOI] [PubMed] [Google Scholar]
- 156. Papalia R, Osti L, Del Buono A, Denaro V, Maffulli N. Management of combined ACL-MCL tears: a systematic review. Br Med Bull. 2010;93:201–215. [DOI] [PubMed] [Google Scholar]
- 157. Park SS, Dwyer T, Congiusta F, Whelan DB, Theodoropoulos J. Analysis of irradiation on the clinical effectiveness of allogenic tissue when used for primary anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:226–235. [DOI] [PubMed] [Google Scholar]
- 158. Paszkewicz J, Webb T, Waters B, Welch McCarty C, Van Lunen B. The effectiveness of injury-prevention programs in reducing the incidence of anterior cruciate ligament sprains in adolescent athletes. J Sport Rehabil. 2012;21:371–377. [DOI] [PubMed] [Google Scholar]
- 159. Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med. 2014;44:281–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Paterno MV, Weed AM, Hewett TE. A between sex comparison of anterior-posterior knee laxity after anterior cruciate ligament reconstruction with patellar tendon or hamstrings autograft: a systematic review. Sports Med. 2012;42:135–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Pauzenberger L, Syre S, Schurz M. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013;29:1712–1721. [DOI] [PubMed] [Google Scholar]
- 162. Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. [DOI] [PubMed] [Google Scholar]
- 163. Pereira M, Vieira Nde S, Brandao Eda R, Ruaro JA, Grignet RJ, Frez AR. Physiotherapy after reconstruction of anterior cruciate ligament. Acta Ortop Bras. 2012;20:372–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Petersen W, Taheri P, Forkel P, Zantop T. Return to play following ACL reconstruction: a systematic review about strength deficits. Arch Orthop Trauma Surg. 2014;134:1417–1428. [DOI] [PubMed] [Google Scholar]
- 165. Piefer JW, Pflugner TR, Hwang MD, Lubowitz JH. Anterior cruciate ligament femoral footprint anatomy: systematic review of the 21st century literature. Arthroscopy. 2012;28:872–881. [DOI] [PubMed] [Google Scholar]
- 166. Poolman RW, Abouali JA, Conter HJ, Bhandari M. Overlapping systematic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: why are they different? J Bone Joint Surg Am. 2007;89:1542–1552. [DOI] [PubMed] [Google Scholar]
- 167. Poolman RW, Farrokhyar F, Bhandari M. Hamstring tendon autograft better than bone patellar-tendon bone autograft in ACL reconstruction: a cumulative meta-analysis and clinically relevant sensitivity analysis applied to a previously published analysis. Acta Orthop. 2007;78:350–354. [DOI] [PubMed] [Google Scholar]
- 168. Posthumus M, Collins M, September AV, Schwellnus MP. The intrinsic risk factors for ACL ruptures: an evidence-based review. Phys Sportsmed. 2011;39:62–73. [DOI] [PubMed] [Google Scholar]
- 169. Prodromos C, Joyce B, Shi K. A meta-analysis of stability of autografts compared to allografts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:851–856. [DOI] [PubMed] [Google Scholar]
- 170. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23:1320–1325.e6. [DOI] [PubMed] [Google Scholar]
- 171. Prodromos CC, Joyce BT, Shi K, Keller BL. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy. 2005;21:1202. [DOI] [PubMed] [Google Scholar]
- 172. Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17:396–401. [DOI] [PubMed] [Google Scholar]
- 173. Pujol N, Colombet P, Cucurulo T, et al. Natural history of partial anterior cruciate ligament tears: a systematic literature review. Orthop Traumatol Surg Res. 2012;98(suppl):S160–S164. [DOI] [PubMed] [Google Scholar]
- 174. Quatman CE, Quatman-Yates CC, Hewett TE. A ‘plane’ explanation of anterior cruciate ligament injury mechanisms: a systematic review. Sports Med. 2010;40:729–746. [DOI] [PubMed] [Google Scholar]
- 175. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42:2769–2776. [DOI] [PubMed] [Google Scholar]
- 176. Raynor MC, Pietrobon R, Guller U, Higgins LD. Cryotherapy after ACL reconstruction: a meta-analysis. J Knee Surg. 2005;18:123–129. [DOI] [PubMed] [Google Scholar]
- 177. Reinhardt KR, Hetsroni I, Marx RG. Graft selection for anterior cruciate ligament reconstruction: a level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am. 2010;41:249–262. [DOI] [PubMed] [Google Scholar]
- 178. Relph N, Herrington L, Tyson S. The effects of ACL injury on knee proprioception: a meta-analysis. Physiotherapy. 2014;100:187–195. [DOI] [PubMed] [Google Scholar]
- 179. Riboh JC, Hasselblad V, Godin JA, Mather RC. 3rd. Transtibial versus independent drilling techniques for anterior cruciate ligament reconstruction: a systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2013;41:2693–2702. [DOI] [PubMed] [Google Scholar]
- 180. Ryan J, Magnussen RA, Cox CL, Hurbanek JG, Flanigan DC, Kaeding CC. ACL reconstruction: do outcomes differ by sex? A systematic review. J Bone Joint Surg Am. 2014;96:507–512. [DOI] [PubMed] [Google Scholar]
- 181. Saccomanno MF, Shin JJ, Mascarenhas R, et al. Clinical and functional outcomes after anterior cruciate ligament reconstruction using cortical button fixation versus transfemoral suspensory fixation: a systematic review of randomized controlled trials. Arthroscopy. 2014;30:1491–1498. [DOI] [PubMed] [Google Scholar]
- 182. Sadoghi P, von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs. J Bone Joint Surg Am. 2012;94:769–776. [DOI] [PubMed] [Google Scholar]
- 183. Salata MJ, Gibbs AE, Sekiya JK. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38:1907–1916. [DOI] [PubMed] [Google Scholar]
- 184. Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy. 2009;25:1139–1174. [DOI] [PubMed] [Google Scholar]
- 185. Samuelsson K, Desai N, McNair E, et al. Level of evidence in anterior cruciate ligament reconstruction research: a systematic review. Am J Sports Med. 2013;41:924–934. [DOI] [PubMed] [Google Scholar]
- 186. Santamaria LJ, Webster KE. The effect of fatigue on lower-limb biomechanics during single-limb landings: a systematic review. J Orthop Sports Phys Ther. 2010;40:464–473. [DOI] [PubMed] [Google Scholar]
- 187. Saper M, Stephenson K, Heisey M. Arthroscopic irrigation and debridement in the treatment of septic arthritis after anterior cruciate ligament reconstruction. Arthroscopy. 2014;30:747–754. [DOI] [PubMed] [Google Scholar]
- 188. Serpell BG, Scarvell JM, Ball NB, Smith PN. Mechanisms and risk factors for noncontact ACL injury in age mature athletes who engage in field or court sports: a summary of the literature since 1980. J Strength Cond Res. 2012;26:3160–3176. [DOI] [PubMed] [Google Scholar]
- 189. Shen C, Jiang SD, Jiang LS, Dai LY. Bioabsorbable versus metallic interference screw fixation in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials. Arthroscopy. 2010;26:705–713. [DOI] [PubMed] [Google Scholar]
- 190. Sheth U, Simunovic N, Klein G, et al. Efficacy of autologous platelet-rich plasma use for orthopaedic indications: a meta-analysis. J Bone Joint Surg Am. 2012;94:298–307. [DOI] [PubMed] [Google Scholar]
- 191. Shi DL, Wang YB, Ai ZS. Effect of anterior cruciate ligament reconstruction on biomechanical features of knee in level walking: a meta-analysis. Chin Med J (Engl). 2010;123:3137–3142. [PubMed] [Google Scholar]
- 192. Shimokochi Y, Shultz SJ. Mechanisms of noncontact anterior cruciate ligament injury. J Athl Train. 2008;43:396–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Smith TO, Davies L, Hing CB. Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2010;18:304–311. [DOI] [PubMed] [Google Scholar]
- 194. Smith TO, Hing CB. A meta-analysis of tourniquet assisted arthroscopic knee surgery. Knee. 2009;16:317–321. [DOI] [PubMed] [Google Scholar]
- 195. Smith TO, Postle K, Penny F, McNamara I, Mann CJ. Is reconstruction the best management strategy for anterior cruciate ligament rupture? A systematic review and meta-analysis comparing anterior cruciate ligament reconstruction versus non-operative treatment. Knee. 2014;21:462–470. [DOI] [PubMed] [Google Scholar]
- 196. Song GY, Zhang H, Zhang J, et al. The anterior cruciate ligament remnant: to leave it or not? Arthroscopy. 2013;29:1253–1262. [DOI] [PubMed] [Google Scholar]
- 197. Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986–1995. [DOI] [PubMed] [Google Scholar]
- 198. Steckel H, Starman JS, Baums MH, Klinger HM, Schultz W, Fu FH. The double-bundle technique for anterior cruciate ligament reconstruction: a systematic overview. Scand J Med Sci Sports. 2007;17:99–108. [DOI] [PubMed] [Google Scholar]
- 199. Stevenson JH, Beattie CS, Schwartz JB, Busconi BD. Assessing the effectiveness of neuromuscular training programs in reducing the incidence of anterior cruciate ligament injuries in female athletes: a systematic review. Am J Sports Med. 2015;43:482–490. [DOI] [PubMed] [Google Scholar]
- 200. Stojanovic MD, Ostojic SM. Preventing ACL injuries in team-sport athletes: a systematic review of training interventions. Res Sports Med. 2012;20:223–238. [DOI] [PubMed] [Google Scholar]
- 201. Sugimoto D, Myer GD, Bush HM, Klugman MF, Medina McKeon JM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47:714–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Sugimoto D, Myer GD, McKeon JM, Hewett TE. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. Br J Sports Med. 2012;46:979–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Sward P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18:277–291. [DOI] [PubMed] [Google Scholar]
- 204. Taylor DW, Petrera M, Hendry M, Theodoropoulos JS. A systematic review of the use of platelet-rich plasma in sports medicine as a new treatment for tendon and ligament injuries. Clin J Sport Med. 2011;21:344–352. [DOI] [PubMed] [Google Scholar]
- 205. Taylor JB, Waxman JP, Richter SJ, Shultz SJ. Evaluation of the effectiveness of anterior cruciate ligament injury prevention programme training components: a systematic review and meta-analysis. Br J Sports Med. 2015;49:79–87. [DOI] [PubMed] [Google Scholar]
- 206. te Wierike SC, van der Sluis A, van den Akker-Scheek I, Elferink-Gemser MT, Visscher C. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports. 2013;23:527–540. [DOI] [PubMed] [Google Scholar]
- 207. Thomee R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1798–1805. [DOI] [PubMed] [Google Scholar]
- 208. Thompson J, Harris M, Grana WA. Patellofemoral pain and functional outcome after anterior cruciate ligament reconstruction: an analysis of the literature. Am J Orthop (Belle Mead NJ). 2005;34:396–399. [PubMed] [Google Scholar]
- 209. Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11:CD008413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Tibor LM, Long JL, Schilling PL, Lilly RJ, Carpenter JE, Miller BS. Clinical outcomes after anterior cruciate ligament reconstruction: a meta-analysis of autograft versus allograft tissue. Sports Health. 2010;2:56–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. van Eck CF, Kopf S, Irrgang JJ, et al. Single-bundle versus double-bundle reconstruction for anterior cruciate ligament rupture: a meta-analysis—does anatomy matter? Arthroscopy. 2012;28:405–424. [DOI] [PubMed] [Google Scholar]
- 212. van Eck CF, Loopik M, van den Bekerom MP, Fu FH, Kerkhoffs GM. Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of instrumented knee laxity tests. Knee Surg Sports Traumatol Arthrosc. 2013;21:1989–1997. [DOI] [PubMed] [Google Scholar]
- 213. van Eck CF, van den Bekerom MP, Fu FH, Poolman RW, Kerkhoffs GM. Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of physical examinations with and without anaesthesia. Knee Surg Sports Traumatol Arthrosc. 2013;21:1895–1903. [DOI] [PubMed] [Google Scholar]
- 214. Van Ginckel A, Verdonk P, Witvrouw E. Cartilage adaptation after anterior cruciate ligament injury and reconstruction: implications for clinical management and research? A systematic review of longitudinal MRI studies. Osteoarthritis Cartilage. 2013;21:1009–1024. [DOI] [PubMed] [Google Scholar]
- 215. van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1128–1144. [DOI] [PubMed] [Google Scholar]
- 216. Vavken P, Dorotka R. A systematic review of conflicting meta-analyses in orthopaedic surgery. Clin Orthop Relat Res. 2009;467:2723–2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Vavken P, Murray MM. Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy. 2011;27:704–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Vavken P, Sadoghi P, Murray MM. The effect of platelet concentrates on graft maturation and graft-bone interface healing in anterior cruciate ligament reconstruction in human patients: a systematic review of controlled trials. Arthroscopy. 2011;27:1573–1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Wang C, Lee YH, Siebold R. Recommendations for the management of septic arthritis after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:2136–2144. [DOI] [PubMed] [Google Scholar]
- 220. Wang D, Jones MH, Khair MM, Miniaci A. Patient-reported outcome measures for the knee. J Knee Surg. 2010;23:137–151. [DOI] [PubMed] [Google Scholar]
- 221. Warner SJ, Smith MV, Wright RW, Matava MJ, Brophy RH. Sport-specific outcomes after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1129–1134. [DOI] [PubMed] [Google Scholar]
- 222. Wasielewski NJ, Parker TM, Kotsko KM. Evaluation of electromyographic biofeedback for the quadriceps femoris: a systematic review. J Athl Train. 2011;46:543–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Wera JC, Nyland J, Ghazi C, et al. International Knee Documentation Committee knee survey use after anterior cruciate ligament reconstruction: a 2005-2012 systematic review and world region comparison. Arthroscopy. 2014;30:1505–1512. [DOI] [PubMed] [Google Scholar]
- 224. Wordeman SC, Quatman CE, Kaeding CC, Hewett TE. In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: a systematic review and meta-analysis. Am J Sports Med. 2012;40:1673–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Wright RW, Fetzer GB. Bracing after ACL reconstruction: a systematic review. Clin Orthop Relat Res. 2007;455:162–168. [DOI] [PubMed] [Google Scholar]
- 226. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94:531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93:1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part I. Continuous passive motion, early weight bearing, postoperative bracing, and home-based rehabilitation. J Knee Surg. 2008;21:217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part II. Open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. J Knee Surg. 2008;21:225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. Wu H, Chen LX, Li YL, et al. Tourniquet used in anterior cruciate ligament reconstruction: a system review. Eur J Orthop Surg Traumatol. 2014;24:999–1003. [DOI] [PubMed] [Google Scholar]
- 231. Xergia SA, McClelland JA, Kvist J, Vasiliadis HS, Georgoulis AD. The influence of graft choice on isokinetic muscle strength 4-24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:768–780. [DOI] [PubMed] [Google Scholar]
- 232. Xie X, Xiao Z, Li Q, et al. Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol. 2015;25:149–159. [DOI] [PubMed] [Google Scholar]
- 233. Xu M, Gao S, Zeng C, et al. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy. 2013;29:357–365. [DOI] [PubMed] [Google Scholar]
- 234. Yao LW, Wang Q, Zhang L, et al. Patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2015;25:355–365. [DOI] [PubMed] [Google Scholar]
- 235. Yoo JH, Lim BO, Ha M, et al. A meta-analysis of the effect of neuromuscular training on the prevention of the anterior cruciate ligament injury in female athletes. Knee Surg Sports Traumatol Arthrosc. 2010;18:824–830. [DOI] [PubMed] [Google Scholar]
- 236. Zaffagnini S, Marcheggiani Muccioli GM, Lopomo N, et al. Can the pivot-shift be eliminated by anatomic double-bundle anterior cruciate ligament reconstruction? Knee Surg Sports Traumatol Arthrosc. 2012;20:743–751. [DOI] [PubMed] [Google Scholar]
- 237. Zazulak BT, Paterno M, Myer GD, Romani WA, Hewett TE. The effects of the menstrual cycle on anterior knee laxity: a systematic review. Sports Med. 2006;36:847–862. [DOI] [PubMed] [Google Scholar]
- 238. Zech A, Hubscher M, Vogt L, Banzer W, Hansel F, Pfeifer K. Neuromuscular training for rehabilitation of sports injuries: a systematic review. Med Sci Sports Exerc. 2009;41:1831–1841. [DOI] [PubMed] [Google Scholar]
- 239. Zeng C, Cheng L, Wei J, et al. The influence of the tibial plateau slopes on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2014;22:53–65. [DOI] [PubMed] [Google Scholar]
- 240. Zeng C, Gao SG, Wei J, et al. The influence of the intercondylar notch dimensions on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:804–815. [DOI] [PubMed] [Google Scholar]
- 241. Zhu Y, Tang RK, Zhao P, Zhu SS, Li YG, Li JB. Double-bundle reconstruction results in superior clinical outcome than single-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1085–1096. [DOI] [PubMed] [Google Scholar]